Contents
What is a bundle branch block
Bundle branch block is a condition in which there’s a delay or obstruction along the pathway that electrical impulses travel to make your heart beat. The delay or blockage may occur on the pathway that sends electrical impulses to the left or the right side of the bottom chambers (ventricles) of your heart. Note that while the term bundle branch “block” is used, the affected bundle branch may or may not actually be “blocked.” In many cases, the bundle branch is not completely blocked, but instead is simply conducting the electrical impulse more slowly than the opposite bundle branch.
In bundle branch block, one or the other (or both) of these bundle branches no longer conduct electrical impulses normally. This can occur from disease or damage to one of the bundle branches, or it may occur for no apparent reason in completely healthy people. When the electrical impulse is delayed in reaching its respective ventricle, the delay shows up as a distinctive pattern on the ECG called a bundle branch block. The chief effect of a bundle branch block is to disrupt the normal, coordinated and simultaneous contraction of the two ventricles. The contraction of one ventricle (the one whose bundle branch is blocked) occurs slightly after the contraction of the other.
People with bundle branch block usually will have either right bundle branch block (RBBB) or left bundle branch block (LBBB), depending on which of the two bundle branches is affected. Sometimes both bundle branches are affected, and the bundle branch block pattern on the ECG is not clearly identifiable as either right or left bundle branch block – in this case, the bundle branch block is referred to as an intraventricular conduction delay.
People who have bundle branch block usually have either right bundle branch block (RBBB) or left bundle branch block (LBBB), depending on which of the two bundle branches is affected. In right bundle branch block (RBBB) and left bundle branch block (LBBB) cases, the QRS complex becomes wider than normal (>0.12 second or 120 millisecond or msec), since it takes longer for the electrical signal to be completely distributed across both ventricles. The shape of the QRS complex reveals which bundle branch (right or left) is conducting the electrical impulse abnormally.
Bundle branch block sometimes makes it harder for your heart to pump blood efficiently through your circulatory system.
There’s no specific treatment for bundle branch block itself. However, any underlying health condition that caused bundle branch block, such as heart disease, will need to be treated.
In most people, bundle branch block doesn’t cause any symptoms. Sometimes, people with the condition don’t even know they have a bundle branch block.
For those people who do have signs and symptoms, they may include:
- Fainting (syncope)
- Feeling as if you’re going to faint (presyncope)
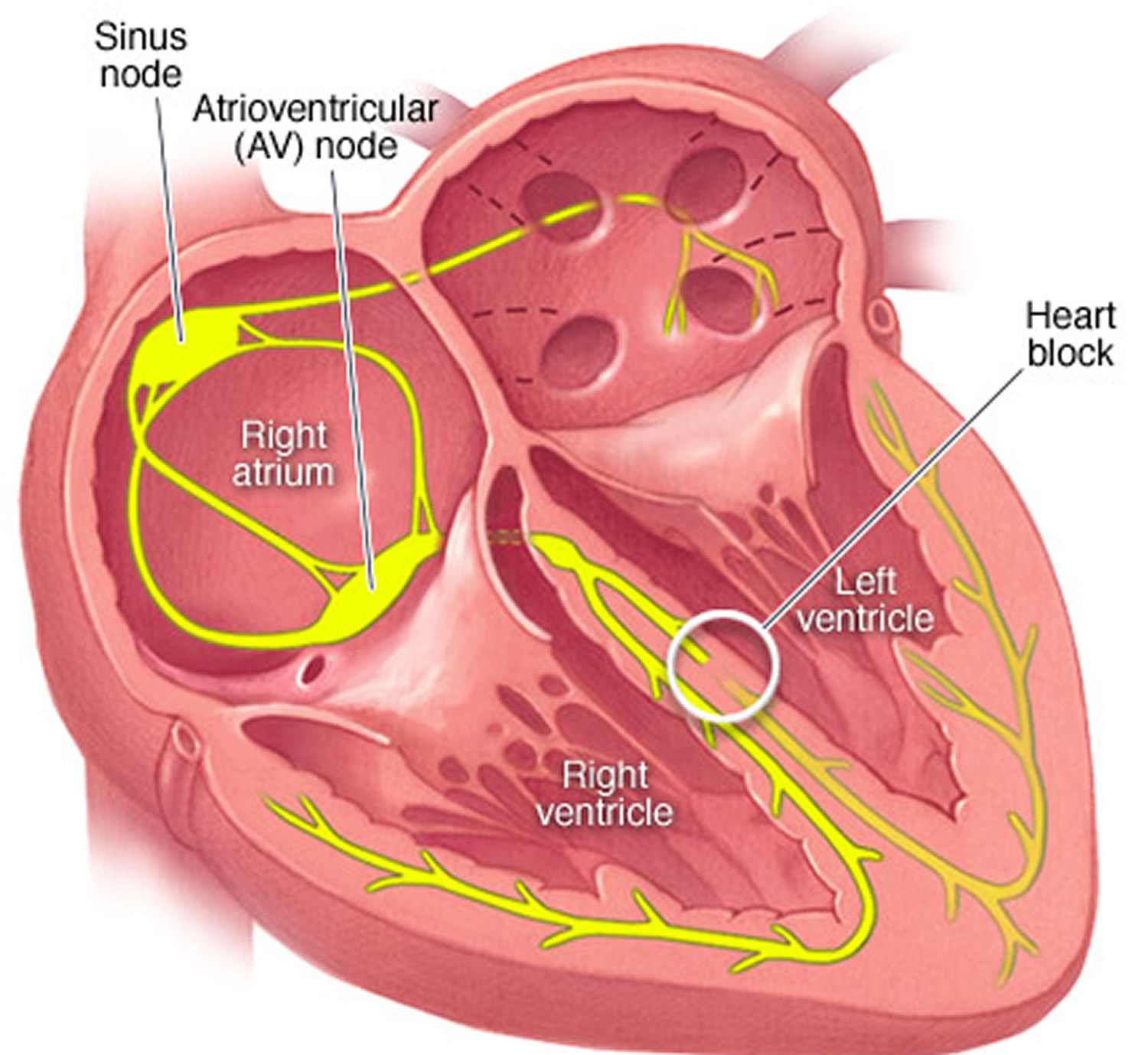
The heart’s electrical system
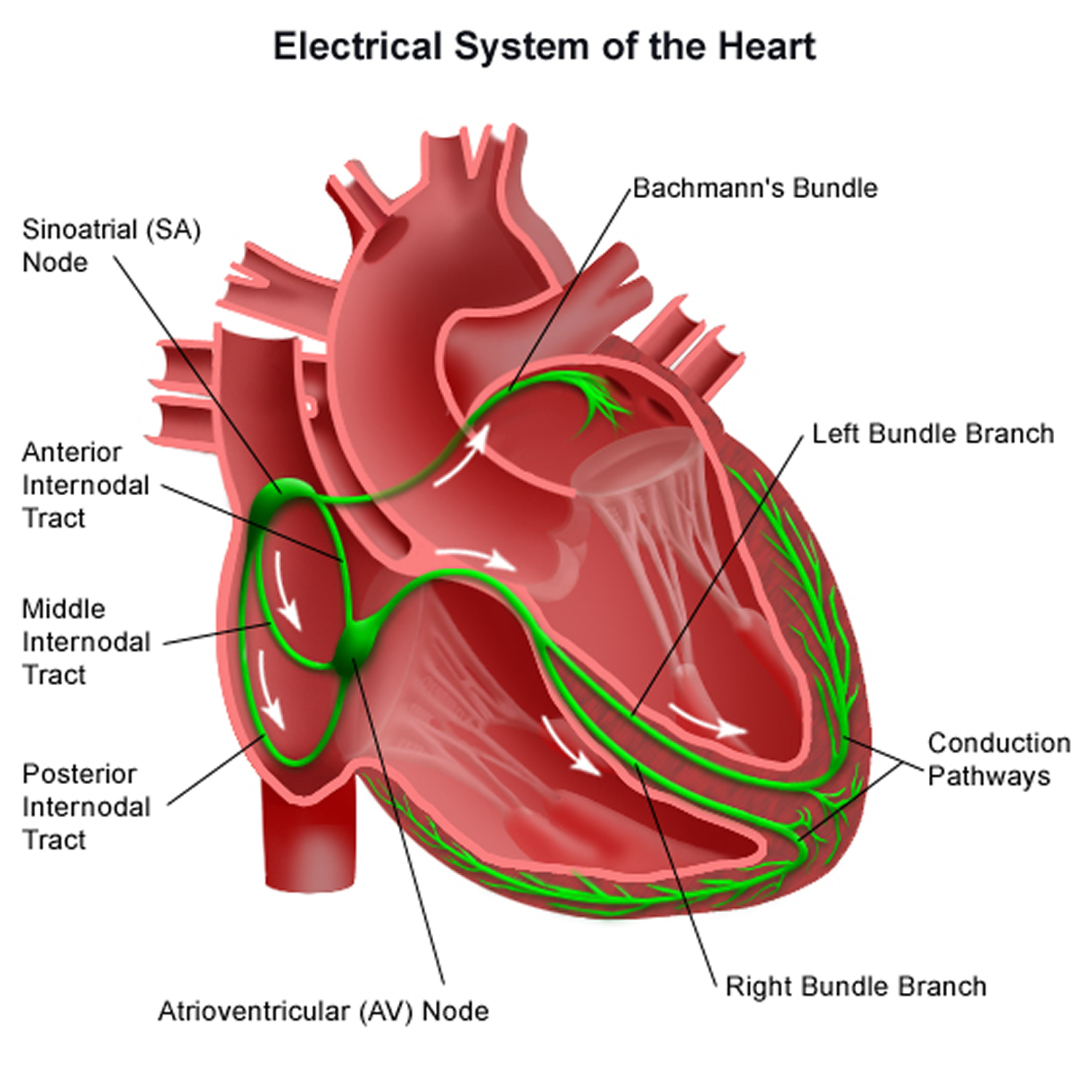
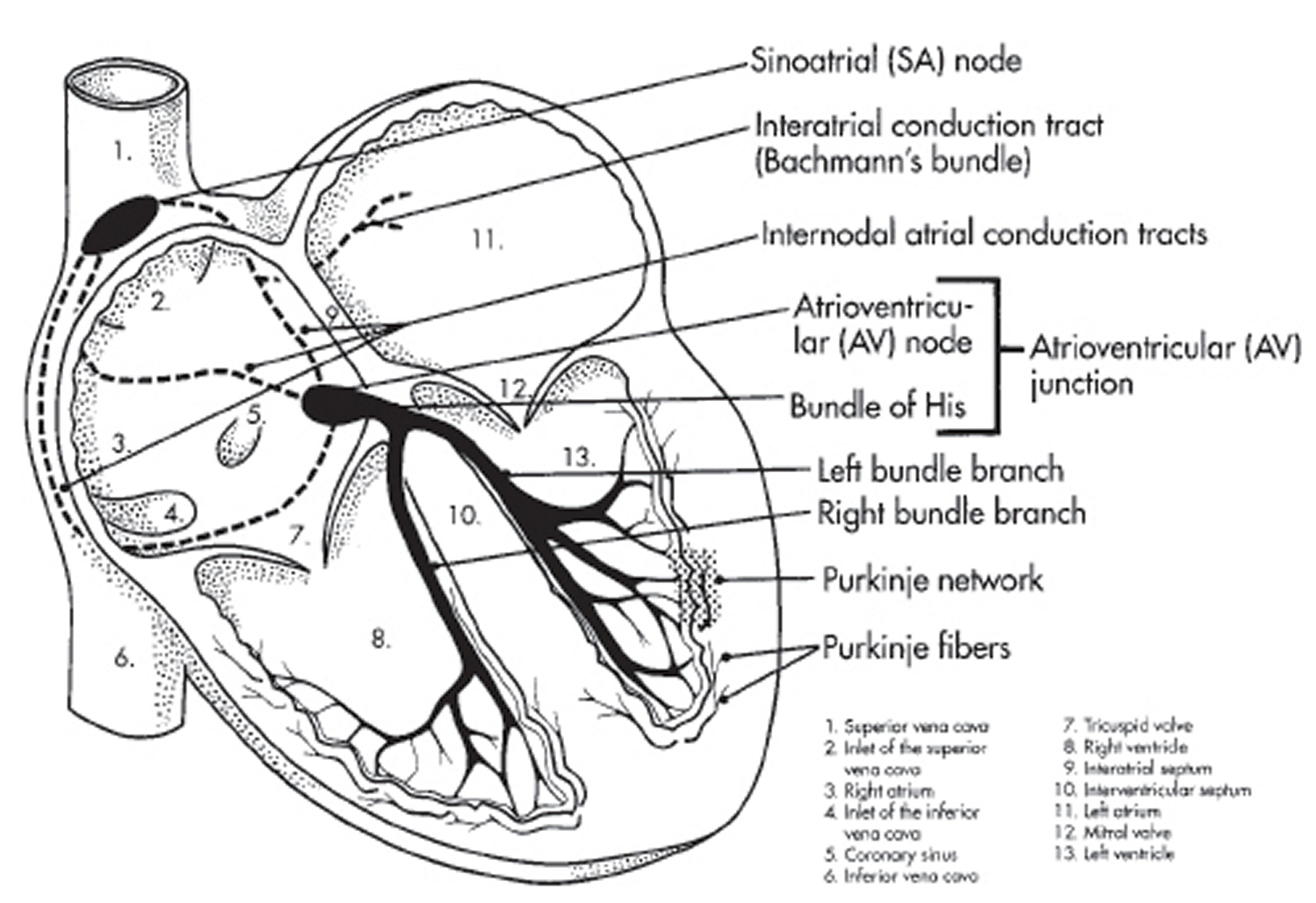
To understand the causes of heart bundle branch block problems such left bundle branch block and right bundle branch block, it helps to understand how the heart’s internal electrical system works.
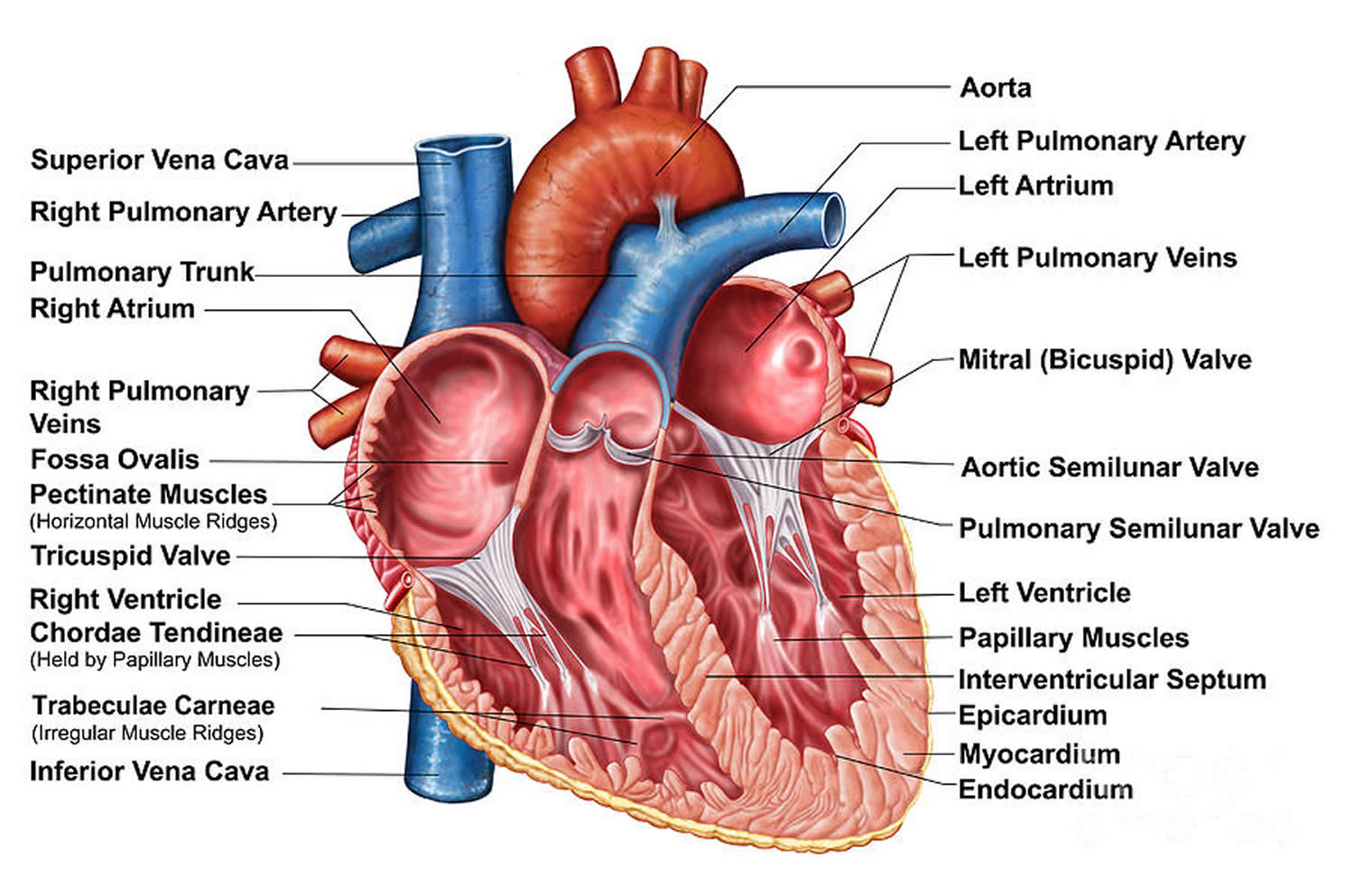
Your heart is made up of four chambers — two upper chambers (atria) and two lower chambers (ventricles). The rhythm of your heart is normally controlled by a natural pacemaker called the sinoatrial (SA) node — or sinus node — an area of specialized cells in the right atrium. The sinoatrial (SA) node produces electrical impulses that normally start each heartbeat. This natural pacemaker produces the electrical impulses that trigger the normal heartbeat. From the sinus node, electrical impulses travel across the atria to the ventricles, causing them to contract and pump blood to your lungs and body.
From the sinus node, electrical impulses travel across the atria, causing the atrial muscles to contract and pump blood into the ventricles.
The electrical impulses then arrive at a cluster of cells called the atrioventricular (AV) node — usually the only pathway for signals to travel from the atria to the ventricles. The atrioventricular (AV) node slows down the electrical signal before sending it to the ventricles. This slight delay allows the ventricles to fill with blood. When electrical impulses reach the muscles of the ventricles, they contract, causing them to pump blood either to the lungs or to the rest of the body.
Leaving the atrioventricular (AV) node, the electrical impulse penetrates the ventricles via a band of cardiac fibers called the His bundle. From the His bundle, the electrical impulse enters the two bundle branches: the right bundle branch and the left bundle branch. The right and left bundle branches distribute the electrical impulse across the right and left ventricles, respectively, causing them to beat. When the bundle branches are functioning normally, the right and left ventricles contract nearly simultaneously.
The right bundle branch, is a direct continuation of the penetrating bundle of His, originates distal to the attachment of the septal leaflet of the tricuspid valve with the membranous septum and surfaces on the right ventricular septum just below the papillary muscle of the conus. It is unbranched and proceeds toward the apex of the right ventricle along the posterior margin of the septal band, courses through the moderator band to the base of the anterior papillary muscle, and proceeds to the right ventricular free wall.
The left bundle branch originates at the crest of the muscular ventricular septum just distal to the membranous septum. It arises in a fanlike fashion that descends inferiorly along the left ventricular septal surface beneath the noncoronary cusp of the aortic valve. The left bundle branch usually branches into 3 major fascicles. The anterior fascicle is directed to the base of the anterolateral papillary muscle, the posterior fascicle is directed to the base of the posteromedial papillary muscle, and, in 60% of hearts, a central fascicle proceeds to the midseptal region. When no central fascicle is present, as in 40% of hearts, the midseptal region is supplied by radiations from the anterior fascicle or the anterior and posterior fascicles.
At the terminal aspect of each bundle branch, Purkinje fibers are interlaced on the endocardial surface of both ventricles and tend to be concentrated at the tips of the papillary muscles.
The job of the His bundle branches is to distribute the spread of the cardiac electrical impulse across the ventricles evenly, so that when the ventricles contract (to eject blood out of the heart), they do so in a coordinated and efficient fashion. The right bundle branch delivers the electrical impulse to the right ventricle, and the left bundle branch delivers the impulse to the left ventricle.
In bundle branch block, one or both of the two bundle branches are no longer transmitting the electrical impulses normally. This often occurs as a result of disease or damage to one of the bundle branches, as may happen with a myocardial infarction (heart attack) or with cardiomyopathy.
However, bundle branch block can also happen for no apparent reason in completely healthy people.
When the electrical impulse is delayed in reaching its respective ventricle, the delay shows up as a distinctive pattern on the ECG called a bundle branch block. The chief effect of a bundle branch block is that it disrupts the simultaneous contraction of the two ventricles. The contraction of one ventricle (the one that has a “blocked” bundle branch) occurs slightly after the contraction of the other, rather than at the same time.
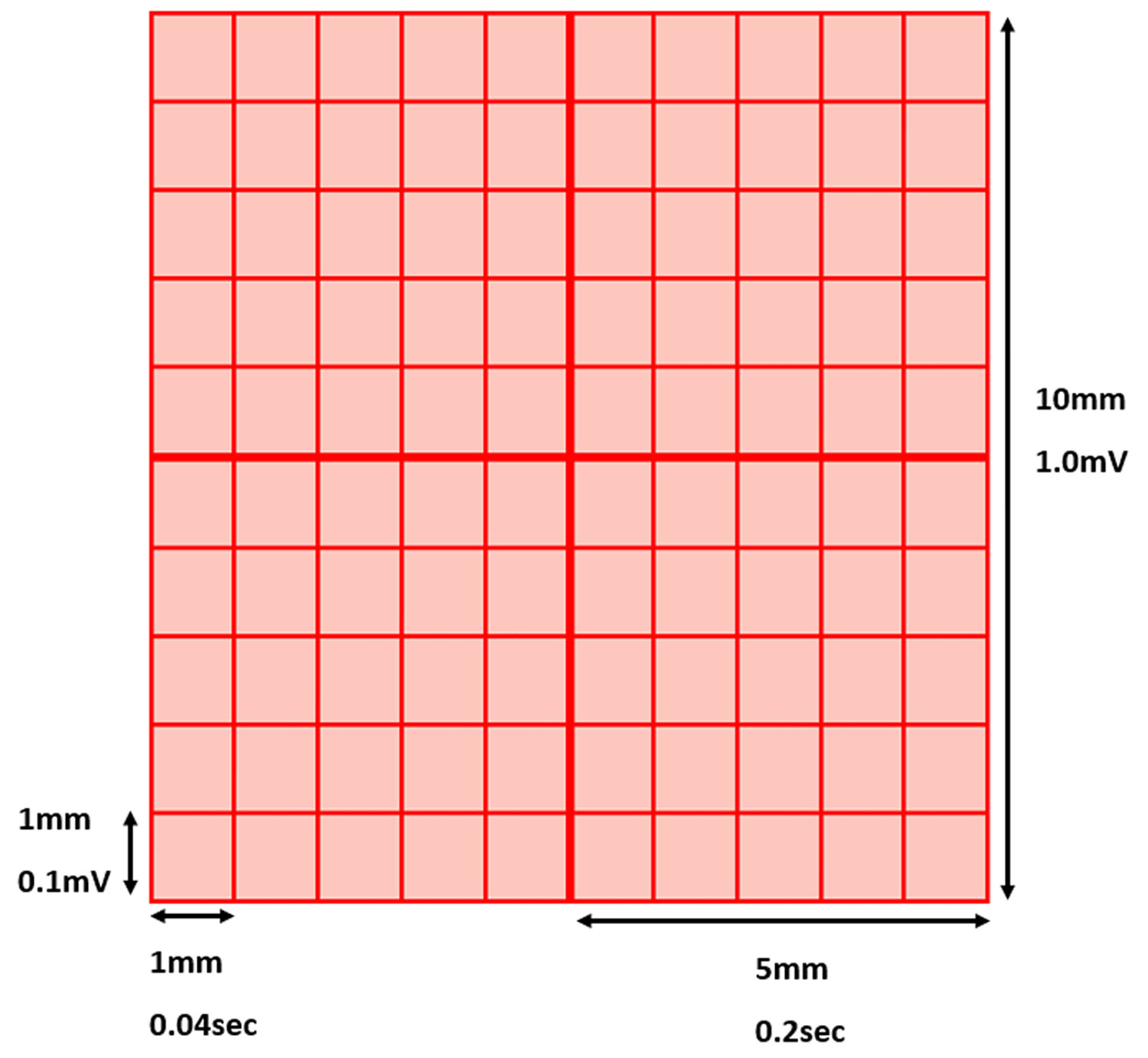
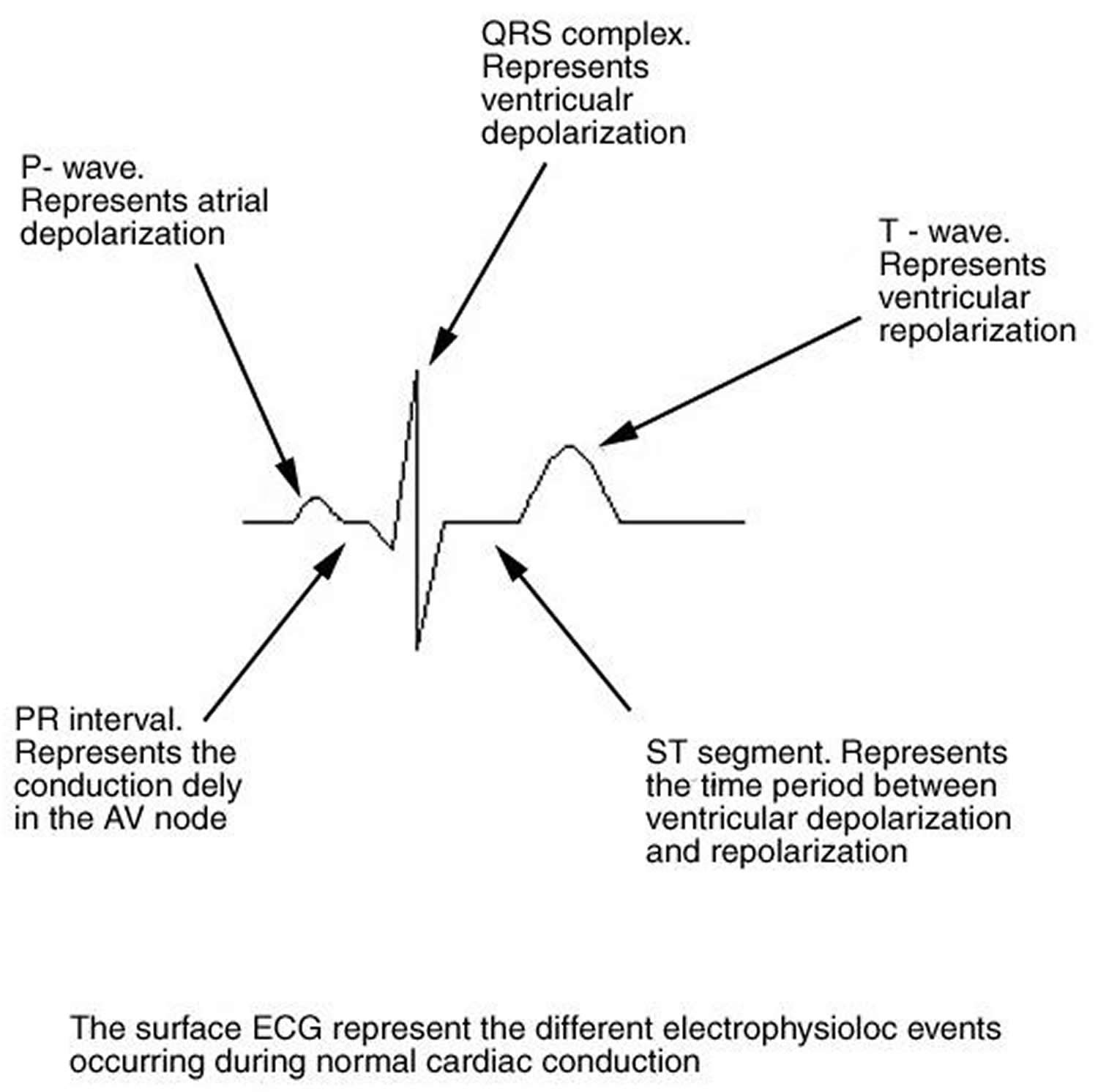
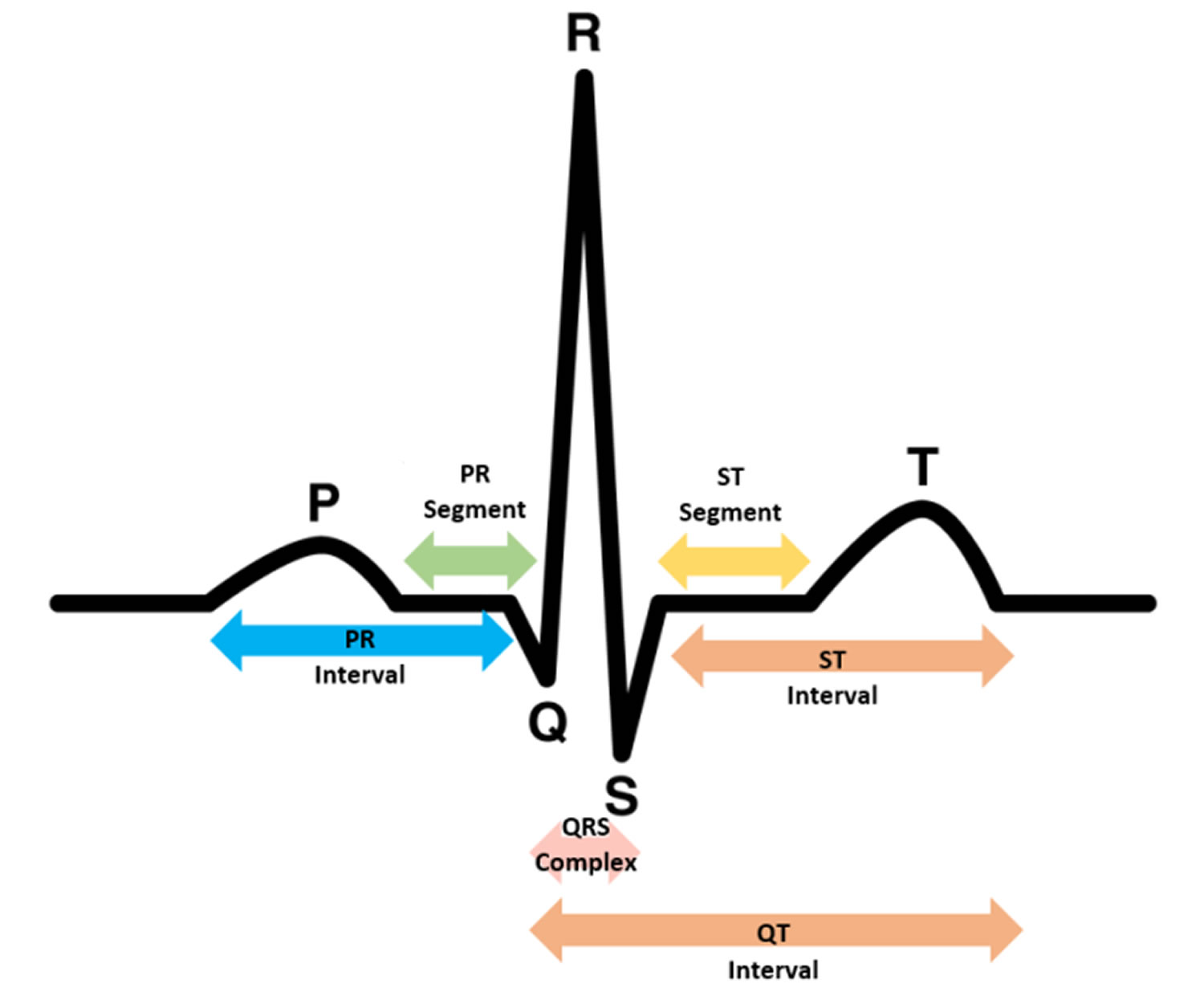
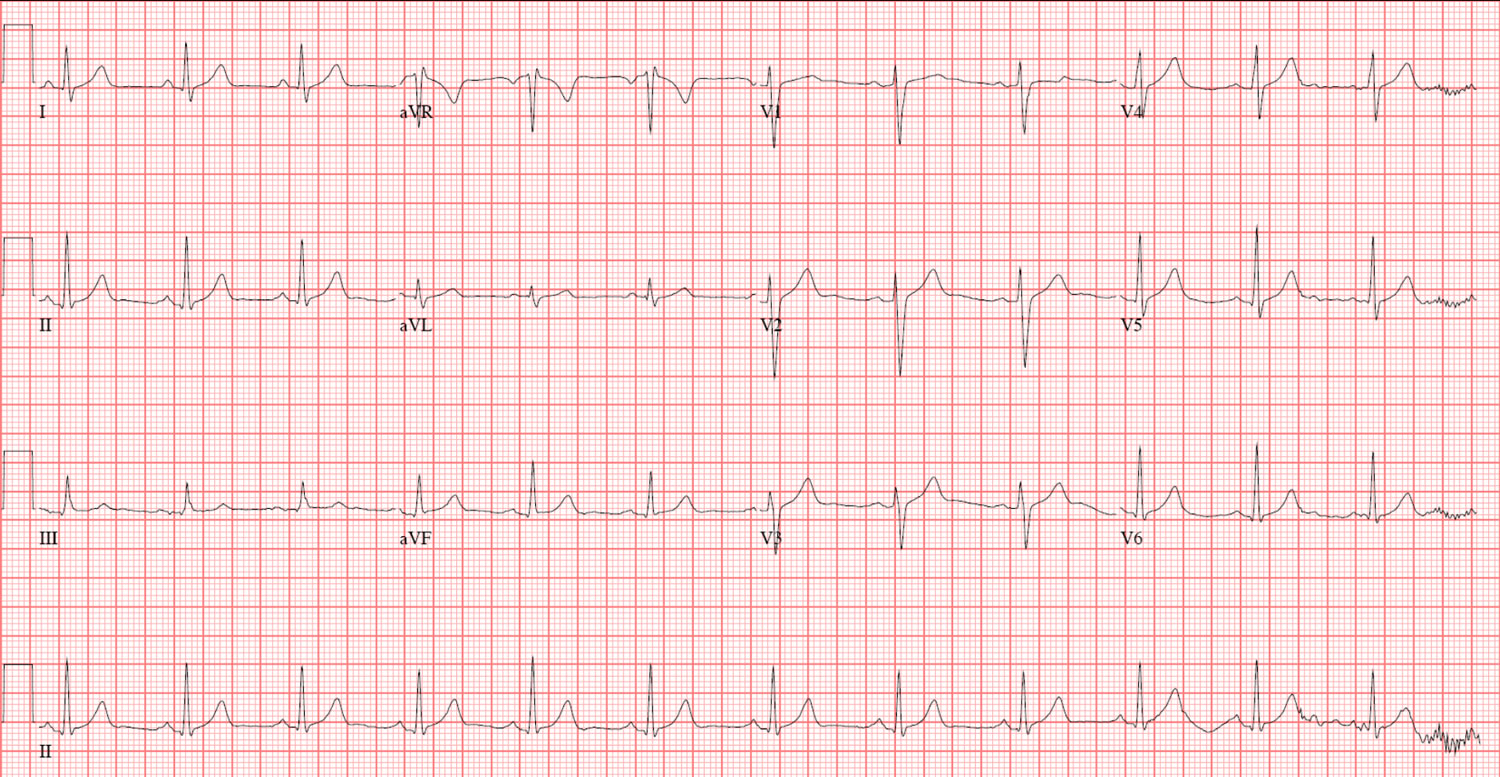
An ECG (electrocardiogram) is a visual representation of the electrical impulse as it moves through the heart. A QRS complex is what cardiologists call a certain part of an ECG (electrocardiogram), the part that shows the electrical impulse as it is being distributed by the bundle branch system throughout the ventricles (see Figure 4 below).
Since both ventricles normally receive the electrical impulse at the same time, the normal QRS complex is relatively narrow (generally less than 0.1 second in duration.) The simultaneous stimulation of both ventricles depends on the electrical impulse traveling down both the right and left bundle branches at nearly the same rate of speed.
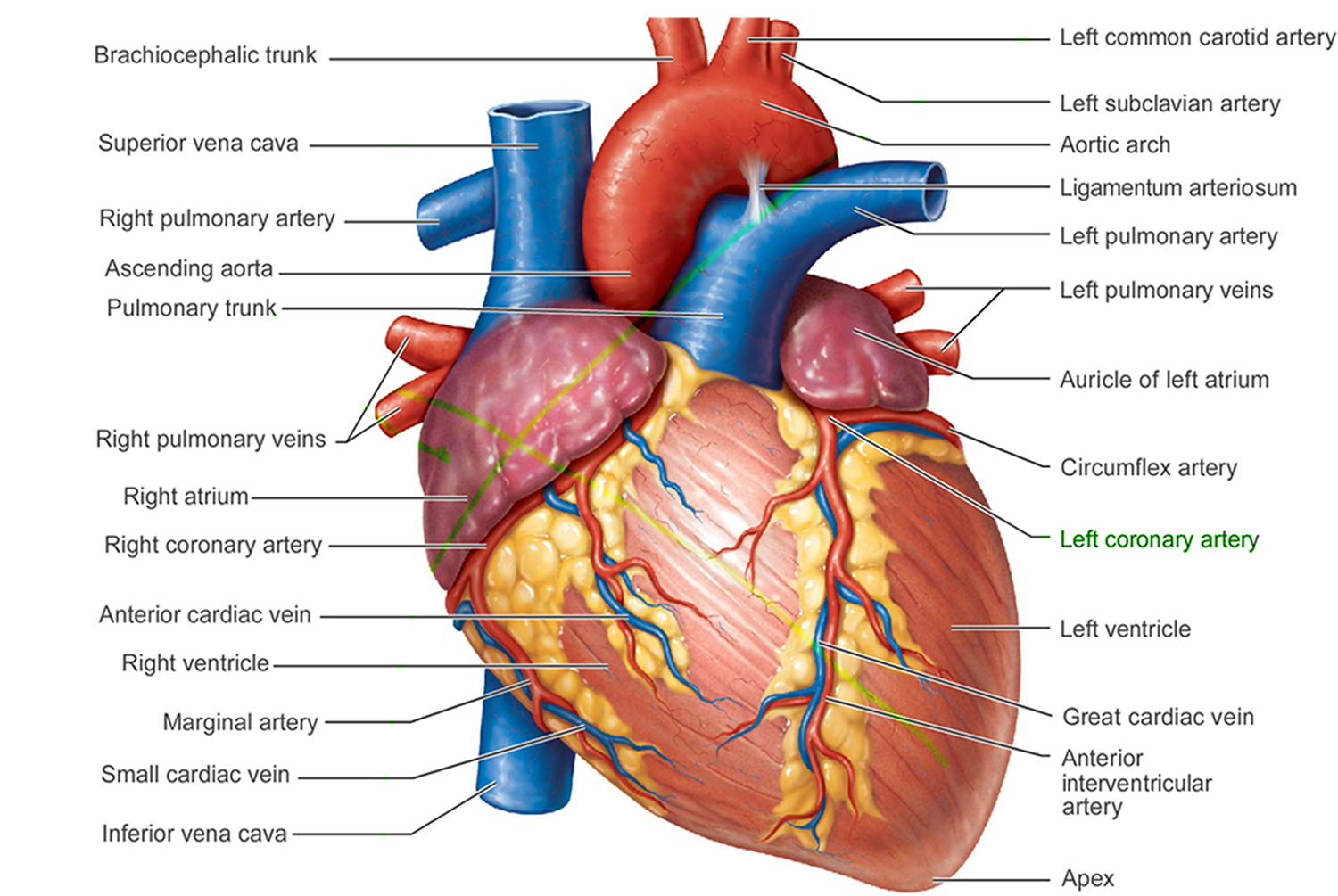
Figure 1. The anatomy of the heart
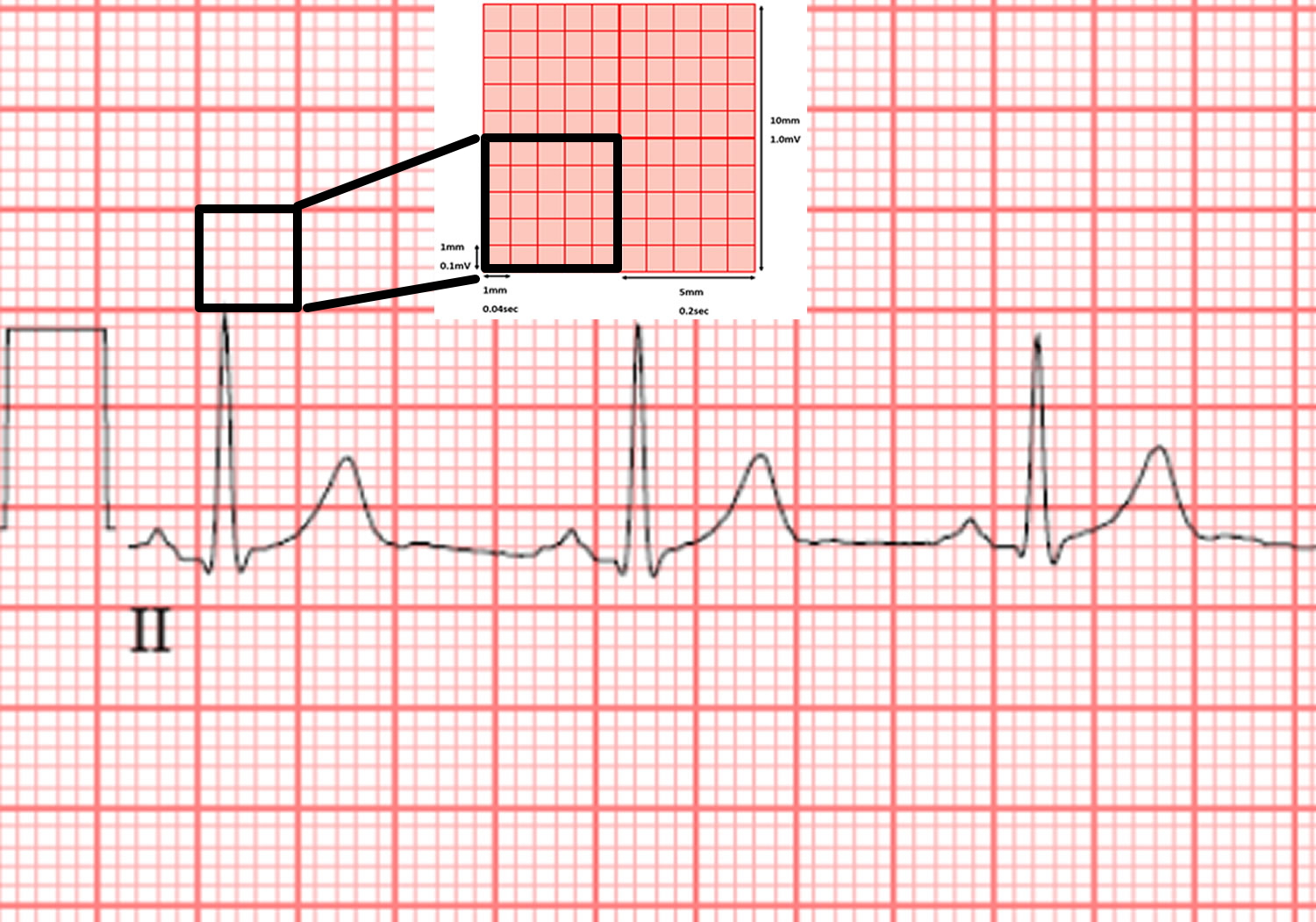
 Normal ECG
Normal ECG
The electrical impulse generated in the sinus node proceeds through the atria (reflected by the P wave on the ECG) to reach the AV node. As the impulse conducts through the AV node, conduction slows, allowing time for atrial contraction to occur before the ventricle is activated (PR segment). After the impulse passes through the compact AV node, it is rapidly conducted through the crux of the heart to the ventricles by means of the bundle of His (penetrating bundle) to the branching bundle, the bundle branches, the distal Purkinje fibers, and finally the ventricular myocardial cells (narrow QRS complex). When depolarization is complete, the ventricle repolarizes in preparation for conducting another impulse.
On the standard ECG paper, with standard calibration, the squares represent:
1 mm = 0.04 second (the smallest square)
5 mm = 0.2 second (5 smallest squares) = 1 big square
P Wave
- Spread of electrical impulse across atria from SA node
- Atrial depolarization
- 0.06 – 0.12 second
- Upright in I, II, aVF, V2- V6
- Inverted in aVR
- Varies in III, aVL
QRS Complex
- Spread of electrical impulse through the ventricles
- Ventricular depolarization
- <0.12 second
T Wave
- Ventricular repolarization
- <2/3 height of preceding R wave
- 0.5mm in I, II, III
- <10mm in V1 – V6
- Same direction as preceding R wave
PR Interval
- Electrical impulse spreads over atrium, through AV node and Bundle of His
- 0.12 – 0.2 second
ST Segment
- Isoelectric point. No change in electrical activity
QT Interval
- Depolarisation and repolarisation of the ventricles
U Wave
- Hypothesized to be Purkinje repolarization
- <25% of T wave
- Same direction as T wave
Heart Rate
- Count the number of small squares between two R waves
- Divide by 1500
Figure 4. Normal heart ECG
Right bundle branch block
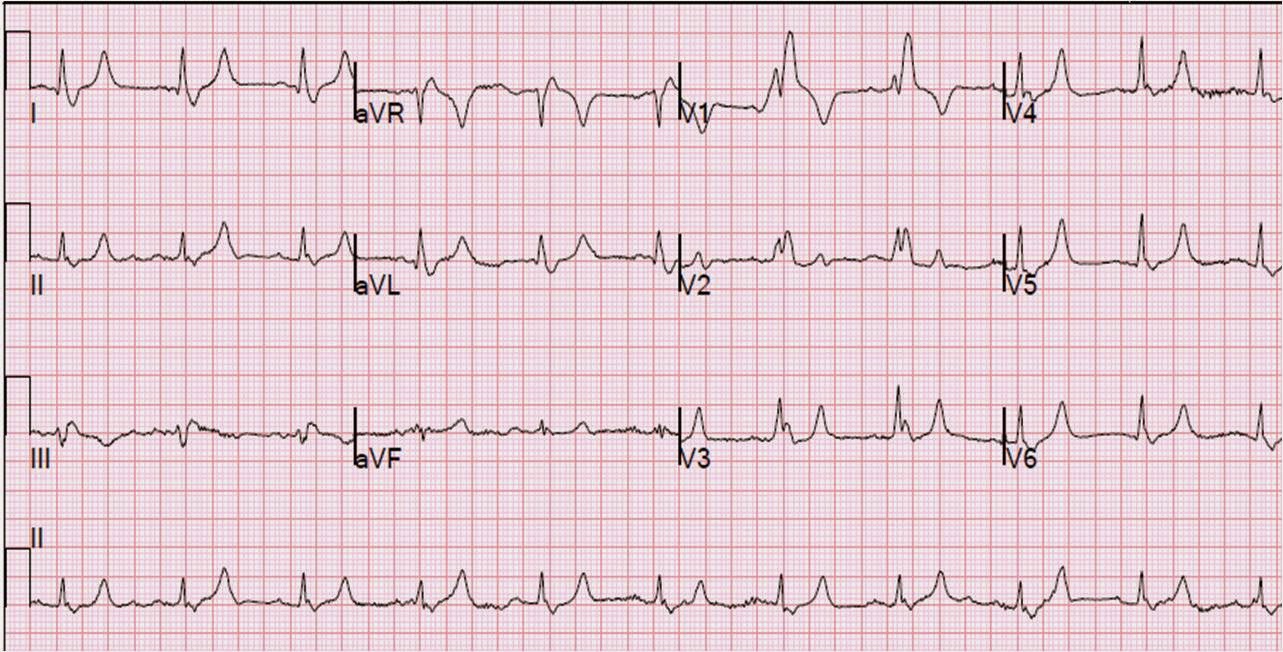
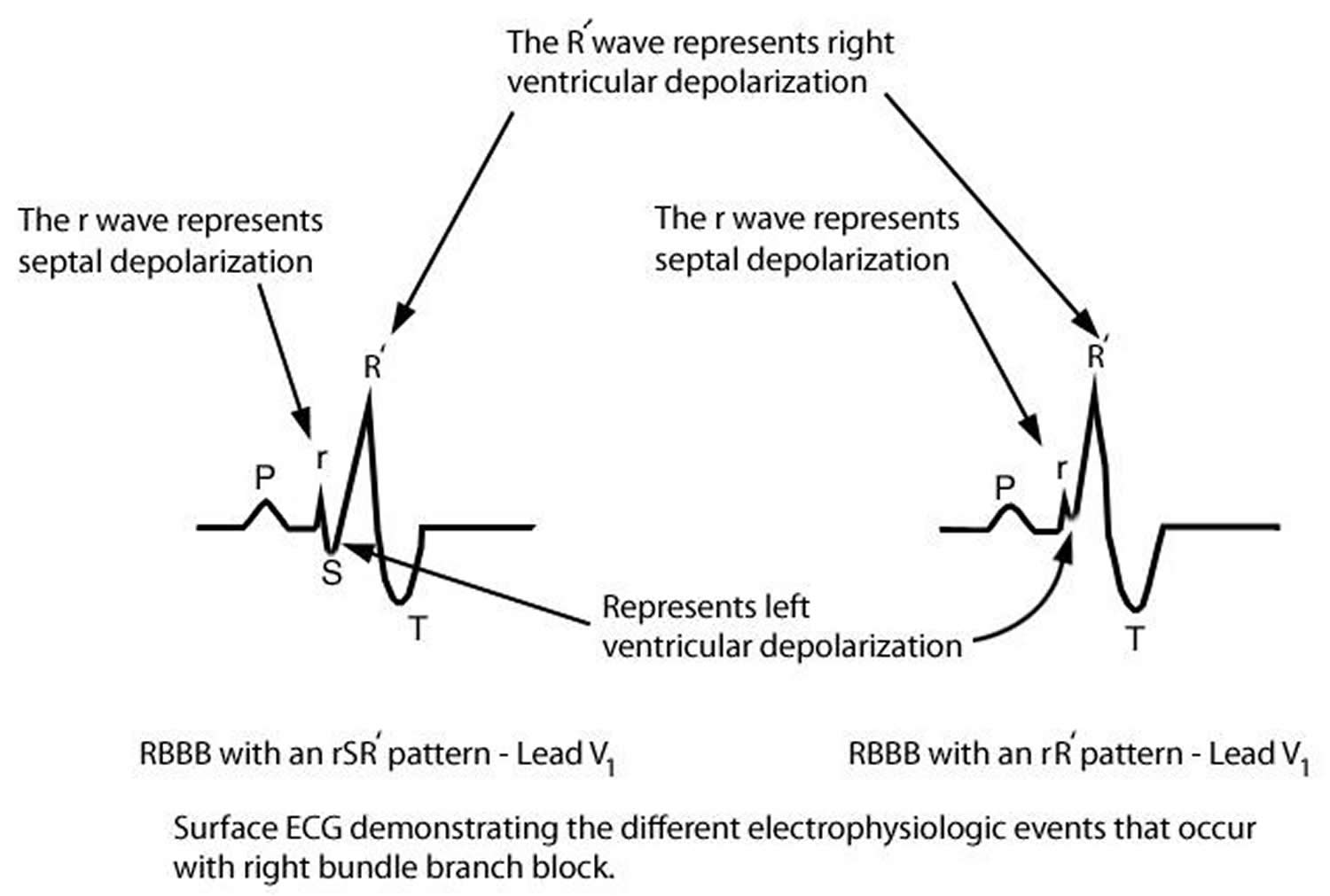
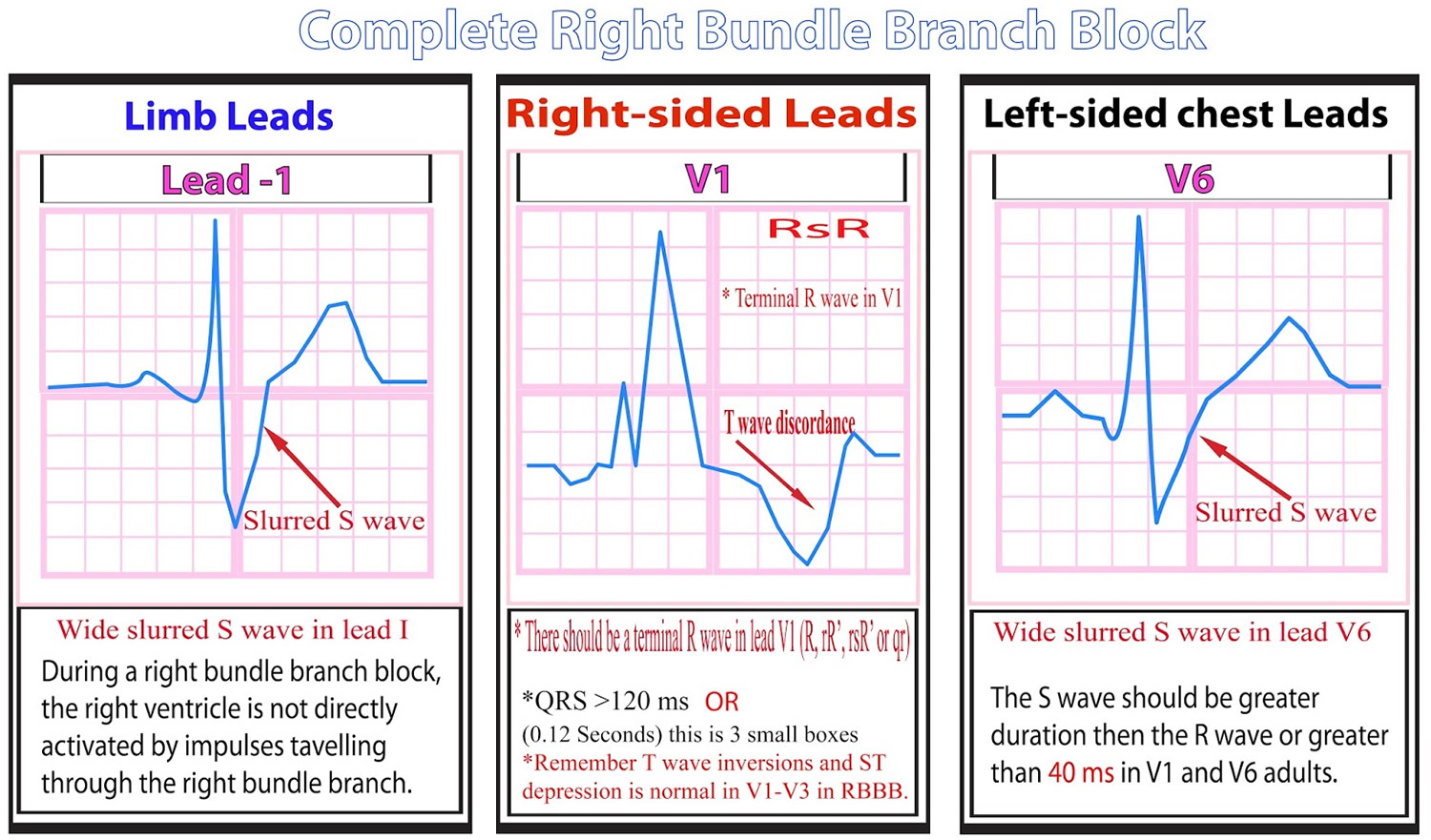
Right bundle branch block (RBBB) occurs when transmission of the electrical impulse from the bundle of His is delayed or not conducted along the right bundle branch. Conduction down the left bundle branch proceeds normally, and the interventricular septum and left ventricle rapidly depolarize in the normal fashion. Depolarization of the right ventricle occurs later and is comparatively slow, accounting for the ECG findings in right bundle branch block (see Figure 5 below). Thus, the right ventricle depolarizes by means of cell-to-cell conduction that spreads from the interventricular septum and from left ventricle to the right ventricle. This results in the characteristic right bundle branch block ECG pattern (Figure 5) compared with a normal ECG as shown in the image above (Figure 4).
Right bundle branch block (RBBB) ECG pattern 1):
- QRS duration > 120 msec;
- Broad and/or notched R waves (rsr`, rsR` or rSR` pattern) in the right precordial leads (leads V1 and V2) and wide and/or deep S waves in leads I and V6.
The incidence of right bundle branch block increases with age. It is seen only rarely in young people (~1% of young adults), but more than 11 percent of 80-year-old people have right bundle branch block and is considered a normal finding.
Exercise-induced right bundle branch block has been rarely noted and appears to be benign 2).
In contrast to left bundle branch block (in which the stimulation of the left ventricle is delayed), right bundle branch block does not compromise overall cardiac function in any measurable way. So right bundle branch block itself is usually regarded as a benign condition that does not require any specific therapy.
However, right bundle branch block is still an important finding. Its significance lies in the fact it is often associated with some underlying cardiac or pulmonary condition. So when right bundle branch block is diagnosed, a medical evaluation is usually required.
Figure 5. Right bundle branch block ECG (RBBB)
Figure 6. Right bundle branch block ECG patterns
Right bundle branch block types
Three types of right bundle branch block have been identified in electrophysiologic studies. Proximal, or central right bundle branch block (RBBB) occurs when a conduction block is present just distal to the bundle of His in the superior aspect of the right bundle branch. This generally occurs when the proximal bundle is injured during surgery for lesions with an inlet or membranous ventricular septal defect (VSD).
Another type of right bundle branch block occurs when the impulse is interrupted between the proximal and distal aspects of the right bundle branch; this type is most commonly observed after surgical division of the moderator band during repair of tetralogy of Fallot.
Distal right bundle branch block or arborisation block is observed when distal ramifications of the right bundle are disrupted during right ventriculotomy or resection of muscle bundles in the right ventricular outflow tract. Regardless of the type of right bundle branch block, the ECG patterns remain similar.
Natural history of right bundle branch block
In general, surgically induced right bundle branch block results in no clinically significant acute hemodynamic consequences and has a benign course over the long term. In rare cases, a progression to complete heart block and sudden death is a concern, particularly if the right bundle branch block pattern is accompanied by additional evidence of substantial injury to the His-Purkinje system (eg, left anterior hemiblock, first-degree AV block). Patients who have undergone repair for tetralogy of Fallot and who have an right bundle branch block pattern with a markedly prolonged QRS duration (>180 ms) may be at increased risk for significant ventricular arrhythmias and sudden death.
Patients with right bundle branch block from other causes may have diverse natural histories depending on the underlying disease. The outcome may be benign in some forms of familial right bundle branch block, or sudden death may result if the right bundle branch block pattern on ECG is due to Brugada syndrome, arrhythmogenic right ventricular cardiomyopathy or Kearns-Sayre syndrome.
Kearns-Sayre Syndrome is a mitochondrial myopathy with the physical findings of ptosis, chronic progressive external ophthalmoplegia, and abnormal retinal pigmentation. Patients are at risk for heart block and sudden death 3). Rarely, patients present with dilated cardiomyopathy and heart failure.
Brugada syndrome is a channelopathy mediated by the SCN5A gene. The right bundle branch block pattern seen in patients with this syndrome is not actually right bundle branch block but is a function of the unusual repolarization abnormality. There are subtle differences in the QRS morphology, specifically the latter portion R’ 4). The ECG shows ST-segment elevation in leads V1-V3, and patients are at risk for sudden cardiac death. Cocaine consumption or the use of the antiarrhythmic drugs propafenone, ajmaline, flecainide or procainamide may reveal ECG findings consistent with Brugada syndrome 5).
Right bundle branch block causes
- A heart abnormality that’s present at birth (congenital) — such as atrial septal defect, a hole in the wall separating the upper chambers of the heart or ventricular septal defect (VSD)
- A heart attack (myocardial infarction)
- A viral or bacterial infection of the heart muscle (myocarditis)
- High blood pressure (hypertension)
- Pulmonary hypertension. Pulmonary hypertension, in turn, can be caused by an array of various lung disorders, including chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea.
- A blood clot in the lungs (pulmonary embolism)
- Coronary artery disease
- Valvular heart disease
- Can also happen naturally in people with a normal heart and no heart problems.
The most common cause of right bundle branch block in children is surgery associated with repair of an isolated VSD or another congenital heart disease that includes a VSD (eg, double-chambered right ventricle, AV canal, or tetralogy of Fallot). The incidence of right bundle branch block ranges from 25-81% after repair of a VSD alone to 60-100% after repair of tetralogy of Fallot. The variation of right bundle branch block after surgery is likely due to the proximity of the VSD to the His-Purkinje system, as well as the surgical technique. For example, right bundle branch block is less common with transatrial repair or exclusion ventriculotomy repair of a VSD than with other procedures.
Hereditary factors
Hereditary right bundle branch block was observed in 4 Lebanese families and has been mapped to chromosome 19 6).
A subset of patients with Brugada syndrome have mutations in SCN5A, the gene that encodes for the voltage-gated cardiac sodium channel 7).
Risk factors for right bundle branch block
In children, most cases of right bundle branch block occur after intracardiac surgery, such as congenital heart surgery associated with repair of a ventricular septal defect (VSD) and tetralogy of Fallot, as well as cardiac transplantation. Right bundle branch block has also been described in patients undergoing cardiac catheterization, particularly transcatheter closure of perimembranous VSDs and catheter ablation for ventricular tachycardia.
Right bundle branch block has been associated with cardiomyopathy, myocarditis, congestive heart failure, right ventricular systolic dysfunction, atrial septal defect (ASD), and Ebstein anomaly.
A transient form of right bundle branch may be observed in patients with premature atrial contractions (Ashman phenomenon) or supraventricular tachycardia (rate dependent right bundle branch block). This occurs when an early impulse is conducted from the atrioventricular (AV) node to the His bundle while the right bundle branch is still refractory but the left bundle is not. Conduction down the right bundle branch is therefore delayed or blocked, resulting in a transient right bundle branch block pattern on the ECG.
Transient right bundle branch block also occurs in approximately 5 percent of patients undergoing cardiac catheterization. This temporary right bundle branch block occurs when the catheter irritates the right bundle branch. This transient bundle branch block usually resolves quickly (within minutes) once the catheter is removed. However, in people who already have left bundle branch block, causing even this transient right bundle branch block will likely create temporary complete heart block, and the heart can stop beating. So, in people with left bundle branch block who are having a right-sided cardiac catheterization, sometimes a temporary pacemaker is inserted during the procedure, to assure that the heart rhythm will continue uninterrupted during the study.
Incomplete right bundle branch block has been described in children with perinatal exposure to human immunodeficiency virus (HIV) type 1 8).
Right bundle branch block prognosis
The prognosis for patients with isolated right bundle branch block is excellent because the course of right bundle branch block is generally benign.
In other patients with right bundle branch block, such as those who have undergone heart transplantation or repair of congenital heart disease and those with Brugada syndrome, Kearns-Sayre syndrome, myocarditis, or cardiomyopathy, the prognosis depends on the underlying condition causing the right bundle branch block and the morphology of the systemic ventricle.
In pediatric patients after VSD patch closure or tetralogy of Fallot repair, the presence of the right bundle branch block has been shown to cause some mechanical dyssynchrony and a tendency toward LV dilatation. Therefore, long-term follow-up of these patients has been suggested 9).
Morbidity/mortality
Surgically induced right bundle branch block is generally considered to have in no clinically significant acute hemodynamic consequences and has a benign course over the long term. However, the role of right bundle branch block in acute right ventricular dysfunction following tetralogy of Fallot repair is unknown since this is a routine postoperative finding. Patients who have undergone tetralogy of Fallot repair and have a QRS duration more than 180 milliseconds may have a long-term risk of ventricular arrhythmias and sudden death. In rare cases, if right bundle branch block is associated with injury to the proximal His-Purkinje system (e.g., left anterior hemiblock, first-degree AV block), it can progress to complete heart block and sudden death.
Patients with familial right bundle branch block may have a benign course, whereas those with right bundle branch block and Brugada syndrome, arrhythmogenic right ventricular cardiomyopathy, or Kearns-Sayre syndrome are at risk for sudden death.
Right bundle branch block complications
If right bundle branch block progresses to heart block, the patient may experience fatigue, exercise intolerance, dizziness, syncope, or sudden death. Some patients who have undergone tetralogy of Fallot repair and have a right bundle branch block pattern and a markedly prolonged QRS may be at increased risk for ventricular tachycardia or sudden death.
Right bundle branch block symptoms
Symptoms of right bundle branch block depend on the underlying cause of the right bundle branch block. In most people, bundle branch block doesn’t cause any symptoms. Sometimes, people with the condition don’t even know they have a bundle branch block.
For those people who do have signs and symptoms, they may include:
- Fainting (syncope)
- Feeling as if you’re going to faint (presyncope)
Right bundle branch block treatment
The only treatment required for isolated right bundle branch block (RBBB) is periodic follow-up and evaluation. Individuals with right bundle branch block (RBBB) and selected heart disease (untreated or following surgical treatment) may require an annual or biennial ECG to evaluate for interval changes. In these individuals, ECGs may reveal progression of the underlying conduction defect or other potential rhythm abnormalities (e.g., sinus bradycardia, supraventricular or ventricular ectopy).
Inpatient ECG telemetry may be required if patients with right bundle branch block (RBBB) are at risk for clinically significant arrhythmia.
Patients, parents, and primary medical providers should be informed that right bundle branch block per se does not typically predict specific future problems or management concerns.
Patients with right bundle branch block are not specifically limited in their activities; however, associated conditions may influence activity restrictions.
Left bundle branch block
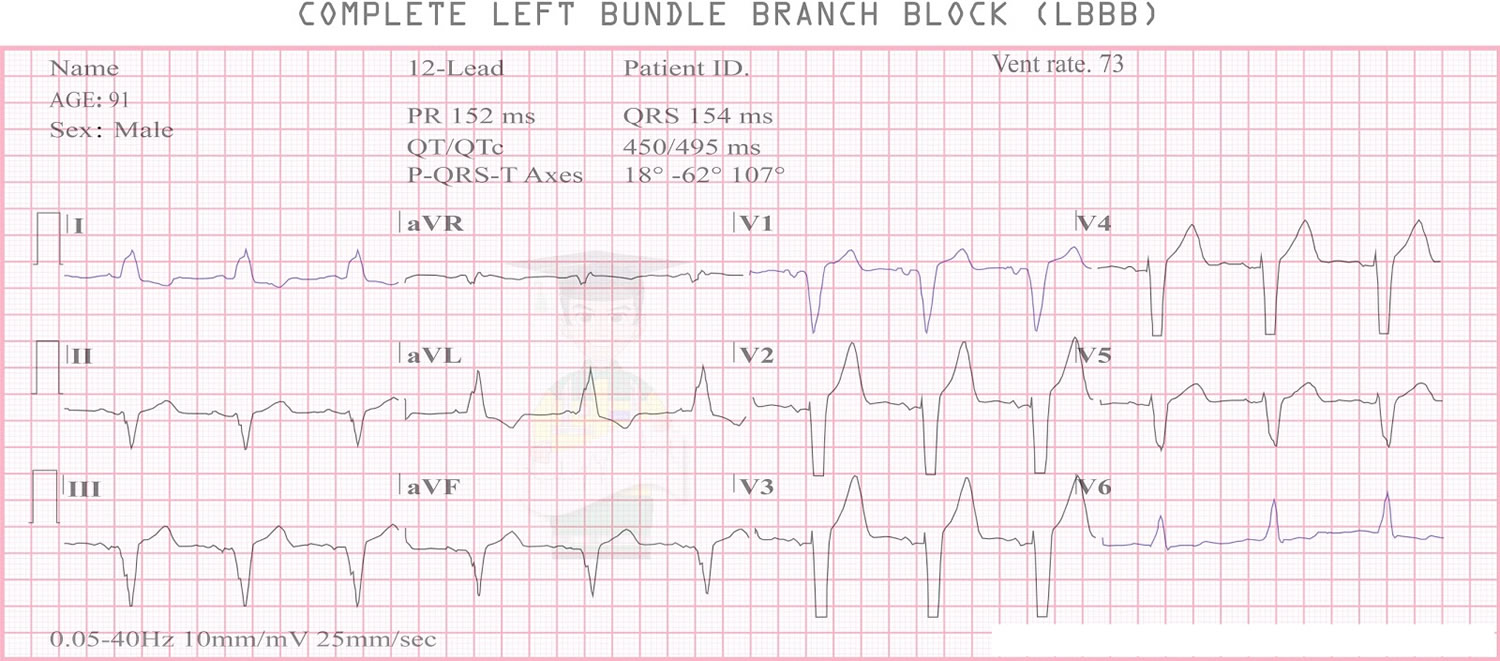
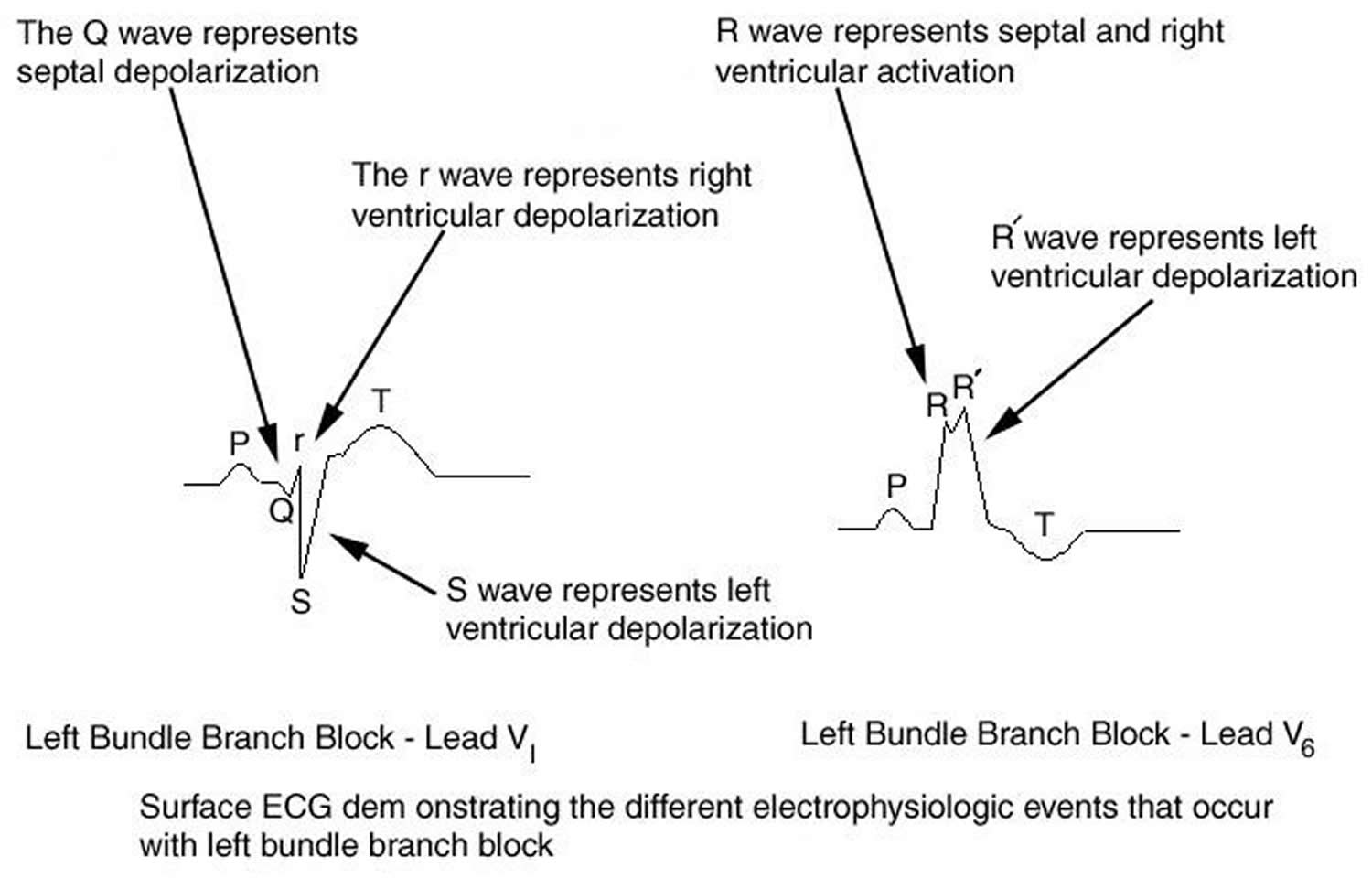
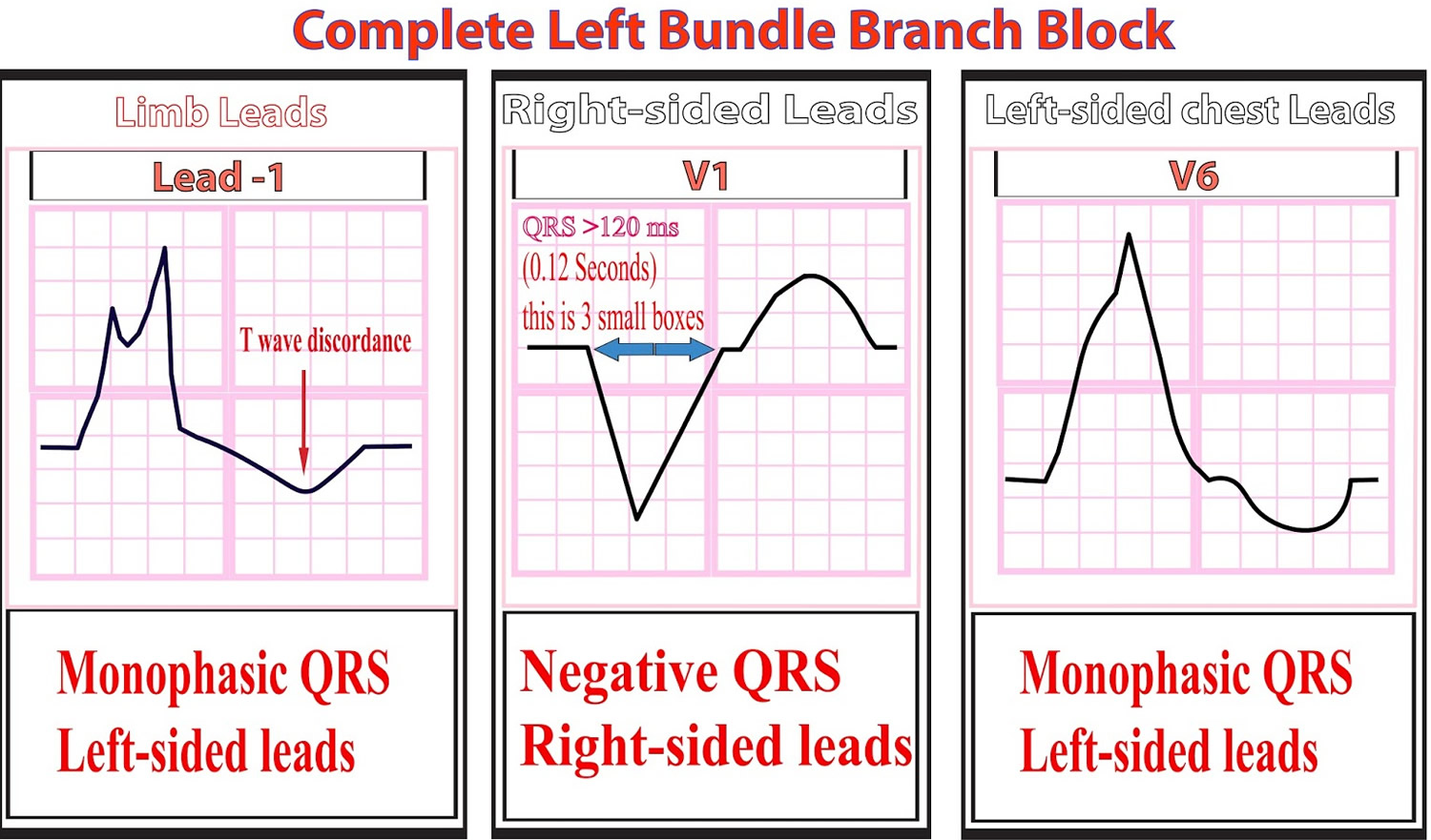
Left bundle branch block (LBBB) occurs when transmission of the cardiac electrical impulse is delayed or fails to be conducted along the rapidly conducting fibers of the main left bundle branch or in both left anterior and posterior fascicles 10). Thus, the left ventricle slowly depolarizes by means of cell-to-cell conduction that spreads from the right ventricle to the left ventricle. This results in the characteristic ECG pattern shown in the image below.
Left bundle branch block is not a benign entity for two different reasons:
- First, left bundle branch block most often occurs as a result of some underlying heart problem. So when it is found, it is quite likely that some significant underlying cardiac condition is also present.
- Second, the left bundle branch block itself can cause the heart to work less efficiently in people who have certain types of heart disease.
Left bundle branch block mainly affects older adults. It is found in less than 1 percent of people under the age of 50; in contrast, nearly 6 percent of 80-year-olds have left bundle branch block.
Most people with left bundle branch block have some form of underlying heart disease. In the Framingham study, subjects who developed left bundle branch block had an average age of 62, and had a significantly increased incidence of hypertension, dilated cardiomyopathy, or coronary artery disease (coronary heart disease). In fact, during the course of the the Framingham study, 89 percent of the people who developed left bundle branch block were subsequently diagnosed with some form of significant cardiovascular disease.
What this means is that anyone, of any age, who is found to have left bundle branch block should have a cardiac evaluation to look for underlying heart disease.
That evaluation should include at least an echocardiogram, and if risk factors are present for coronary artery disease, a stress/thallium study should also be strongly considered. The most common cardiovascular disorders found in the setting of left bundle branch block (LBBB) include hypertension, coronary artery disease, heart failure, hypertrophic cardiomyopathy, or valvular heart disease.
If no heart disease is found after a thorough cardiac evaluation in a person with left bundle branch block, especially in people under 50, the prognosis turns out to be quite good. In these cases, the left bundle branch block is best thought of as a benign, incidental ECG finding.
In left bundle branch block, the heart’s two ventricles are being stimulated by the cardiac electrical impulse in sequence, instead of simultaneously. That is, the left ventricle is stimulated only after the right ventricle is stimulated. Thus, left bundle branch block causes a loss of normal coordination between the two ventricles, which decreases the efficiency of the heart beat. The heart has to work harder to achieve its normal pumping capacity.
In young, healthy people with left bundle branch block, and even in older people with left bundle branch block who may have mild heart disease, the drop-off in cardiac efficiency appears to be pretty trivial, and current evidence indicates that left bundle branch block itself does not pose a problem in these people.
However, in people who have heart failure and a left ventricular ejection fraction which is reduced to less than 35 percent, left bundle branch block can produce a significant drop-off in cardiac efficiency. This reduced efficiency can accelerate the deterioration of heart failure, and make symptoms significantly worse.
Figure 7. Left bundle branch block ECG (LBBB)
Figure 8. Left bundle branch block ECG pattern
Left bundle branch block types
Complete left bundle branch block occurs when the electrical impulse is delayed or interrupted in either the main left bundle branch or in both the anterior and posterior fascicles. Conduction down the right bundle branch normally proceeds, and the right ventricle depolarizes in the normal fashion. In complete left bundle branch block, conduction from the right ventricle passes first to the interventricular septum, then to the anterior and posterior portions of the left ventricle, and finally to the left lateral free wall. Delayed left ventricular depolarization accounts for the ECG findings in left bundle branch block.
Incomplete left bundle branch block occurs in 2 forms, each called hemiblock. In left anterior hemiblock, transmission of the electrical impulse proceeds normally along the main left bundle branch and the posterior fascicle, but it is blocked or delayed in the anterior fascicle. This blockage results in delayed activation of the anterior portion of the left ventricle. In left anterior hemiblock, the duration of the QRS complex may be of normal or only slightly prolonged duration because of normal rapid conduction down the right and left main bundle and the left posterior fascicle. In addition, the QRS complex is directed superiorly in the frontal plane. This is called left axis deviation, although the term superior axis deviation most accurately describes the finding. Furthermore, QRS axis is normally to the left; therefore, the term left axis deviation makes little semantic sense.
With left posterior hemiblock, transmission of the electrical impulse proceeds normally along the main left bundle branch and the anterior fascicle, but it is blocked in the posterior fascicle. This blockage results in delayed activation of the posterior left ventricle. The QRS complex is again of normal or only slightly prolonged duration and inscribes a rightward axis in the frontal plane. Left posterior hemiblock is rarely observed in children, and diagnosis is difficult because of the common association of right axis deviation in children with congenital heart disease and right ventricular hypertrophy.
Left bundle branch block causes
- Heart disease
- Thickened, stiffened or weakened heart muscle (left ventricular hypertrophic cardiomyopathy)
- A viral or bacterial infection of the heart muscle (myocarditis)
- High blood pressure (hypertension)
- Ageing of the electrical pathway in your heart.
- Anatomic malformations and abnormalities of the conduction system (e.g., as is observed in Lenegre disease).
- Left bundle branch block has been observed after surgery in the left ventricular outflow tract, septal myectomy, alcohol septal ablation, replacement of the aortic valve, and transcatheter closure of perimembranous ventricular septal defects.
- Left bundle branch block is also observed in patients with left ventricular hypertrophy, left ventricular noncompaction and neuromuscular disease, progressive conduction system disease, myocarditis 11), cardiomyopathy 12), hemochromatosis, sclerodegenerative diseases, myocardial infarction, aortic valve endocarditis, rheumatic fever with aortic valve involvement, perinatal exposure to HIV type 1 13), Wolff-Parkinson-White Syndrome (when the abnormal conduction pathway enters the right ventricle), and acute pulmonary embolism 14).
- The left bundle branch block pattern, or rather, left ventricular conduction delay, also occurs in patients with Wolff-Parkinson-White Syndrome in whom the abnormal conduction pathway enters the right ventricle.
- Some patients may demonstrate a left bundle branch block pattern during supraventricular tachycardia (ie, rate-dependent bundle branch block).
Left bundle branch block may occur in as many as 20% of individuals after aortic valve replacement.
Left bundle branch block in children is associated with cardiovascular disease or surgery and is not observed in the general population.
Risk factors for left anterior hemiblock
Risk factors for left anterior hemiblock (LAH) include the following:
- Left anterior hemiblock has been associated with coronary artery disease, left ventricular hypertrophy, cardiomyopathy, tetralogy of Fallot repair, ventricular septal defect repair, septal myectomy, subvalvar aortic resection, and an anomalous origin of the left coronary artery from the pulmonary artery.
- Left anterior hemiblock may be present in patients with autosomal dominant bundle branch disease and has been associated with lentiginosis.
- Among congenital heart defects, left anterior hemiblock is characteristic of endocardial cushion defects, such as ostium primum atrial septal defect complex and complete AV canal, an abnormality frequently seen in patients with Down syndrome. Left anterior hemiblock occurs in endocardial cushion defects because of congenital absence or hypoplasia of the left anterior division. Left anterior hemiblock has also been described in Noonan syndrome.
- Patients with endocardial cushion defects ( ostium primum atrial septal defect, complete AV canal), tricuspid atresia, double-outlet right ventricle, and certain forms of a functional single ventricle have left anterior hemiblock that may reflect absent, hypoplastic, or abnormally coursing left bundle fascicles rather than an anterior hemiblock per se.
Risk factors for left posterior hemiblock
Left posterior hemiblock is observed after congenital heart surgery and in patients with congenital aortic stenosis, endocarditis, or diphtheritic myocarditis.
Left bundle branch block prognosis
Progression to complete heart block or sudden death is rare, and the prognosis depends on associated systemic or cardiovascular disease more than the left bundle branch block itself. Biventricular pacing may improve clinically significant and progressive morbidity associated with concomitant congestive heart failure.
Patients with left bundle branch block, left axis deviation, and first-degree heart block or left bundle branch block associated with near-syncope or syncope require close follow-up and/or electrophysiologic study. In adults, left bundle branch block can disturb coronary perfusion of the left anterior descending coronary artery by shortening the duration of diastolic flow.
As noted, if left bundle branch block progresses to complete heart block, the patient may have syncope or suddenly die.
Left bundle branch block symptoms
In most people, bundle branch block doesn’t cause any symptoms. Sometimes, people with the condition don’t even know they have a bundle branch block.
For those people who do have signs and symptoms, they may include:
- Fainting (syncope)
- Feeling as if you’re going to faint (presyncope)
Left bundle branch block treatment
Patients with left bundle branch block (LBBB) require complete cardiac evaluation, and those with left bundle branch block and near-syncope or syncope may require a pacemaker. Guidelines for device-based therapy of cardiac rhythm abnormalities have been established and revised by the American College of Cardiology and American Heart Association 15).
Continuous telemetry may be considered if the LBBB might be associated with other arrhythmias.
Progression from left anterior hemiblock to high degrees of block is unusual, and patients require only observation.
Activity restrictions
Activity restrictions primarily depend on the underlying cardiac cause of the left bundle branch block pattern and on whether the patient develops important arrhythmias (bradycardia, tachycardia) during prolonged exertion.
Surgical Care
Patients with congestive heart failure and intrinsic left bundle branch block or left bundle branch block due to chronic right ventricular pacing may benefit from cardiac resynchronization therapy (CRT); however, the improvement in clinical or echocardiographic parameters varies and is, at times, unpredictable 16).
Further Outpatient Care
Left bundle branch block may rarely progress to complete heart block and sudden death. In these patients, prognosis depends on the associated cardiac disease more than the left bundle branch block itself. Yearly evaluation, including ECG, is recommended, with follow-up more frequent than this if indicated by underlying cardiac disease and changes in patient’s clinical course and symptoms.
Patients with left bundle branch block, left axis deviation, and first-degree heart block or left bundle branch block and near-syncope or complete syncope require close follow-up care. They should be referred for consultation with an electrophysiologist and possibly pacemaker insertion.
Patients with left bundle branch block need evaluation at regular intervals for possible left ventricular dysfunction. This may happen years after the onset of left bundle branch block.
Risk factors for bundle branch block
Risk factors for bundle branch block include:
- Increasing age. Bundle branch block is more common in older adults than in people who are middle-aged.
- Underlying health problems. People who have high blood pressure or heart disease are more likely to have bundle branch block than people without those conditions.
Bundle branch block complications
The main complication of bundle branch block is a slow heart rate, which can sometimes cause fainting.
People who have a heart attack and develop a bundle branch block have a higher chance of complications, including sudden cardiac death, than do people who have heart attacks and don’t develop a bundle branch block.
Because bundle branch block affects the electrical activity of your heart, it can sometimes complicate the accurate diagnosis of other heart conditions, especially heart attacks, and lead to delays in proper management of those problems.
Bundle branch block symptoms
In most cases, bundle branch block does not produce symptoms. However, in severe bundle branch block the ability of the electrical impulse to reach either ventricle may become quite tenuous. In these cases, the impulse may suddenly become completely blocked from reaching the ventricles, leading to complete heart block — which can produce syncope or sudden cardiac death.
Sometimes the presence of bundle branch block may indicate the presence of an underlying cardiac problem. So when a bundle branch block is identified, most doctors will recommend a noninvasive cardiac evaluation (most often, an echocardiogram).
Bundle branch block diagnosis
Tests that may be used to diagnose a bundle branch block or the underlying problem causing it include:
- Electrocardiogram (ECG). An electrocardiogram records the electrical impulses in your heart through wires attached to the skin on your chest and other locations on your body. Abnormalities may indicate the presence of bundle branch block, as well as which side is being affected.
- Echocardiogram. An echocardiogram can be used to pinpoint an underlying condition that caused the bundle branch block. This test uses sound waves to produce images of the heart, allowing your doctor to see your heart in motion. An echocardiogram provides detailed images of the heart’s structure and shows the thickness of your heart muscle and whether your heart valves are moving normally.
Bundle branch block treatment
Most people with bundle branch block are symptom-free and don’t need treatment.
However, if you have an underlying heart condition causing bundle branch block, treatment of the underlying condition is recommended. Treatment of underlying conditions may involve using medications to reduce high blood pressure or lessen the effects of heart failure, or the use of a coronary angioplasty to open up the artery leading to your heart.
Additionally, depending on your symptoms and whether you have other heart problems, your doctor might also recommend:
- A pacemaker. For some people with bundle branch block and a history of fainting, doctors may recommend implanting a pacemaker. A pacemaker is a compact device implanted under the skin of your upper chest (internal pacemaker) with two wires that connect to the right side of your heart. The pacemaker provides electrical impulses when needed to keep your heart beating regularly.
- Cardiac resynchronization. Also known as biventricular pacing, this procedure is similar to having a pacemaker implanted. However, in cardiac resynchronization, there’s a third wire that’s connected to the left side of the heart so the device can keep both sides in proper rhythm.
References [ + ]