Contents
- What is diabetic retinopathy
- Who is at risk of diabetic retinopathy?
- Eye Retina Anatomy
- How diabetes can affect your eyes
- Diabetic retinopathy stages
- Diabetic retinopathy signs and symptoms
- Diabetic retinopathy screening
- Diabetic retinopathy causes
- Diabetic retinopathy prevention
- Diabetic retinopathy diagnosis
- Diabetic retinopathy treatment
What is diabetic retinopathy
Diabetic retinopathy is a diabetes complication that refers to retinal changes that occur in patients with diabetes mellitus. Diabetic retinopathy can develop in anyone who has type 1 or type 2 diabetes. Diabetic retinopathy is caused by damage to the small blood vessels of the light-sensitive tissue at the back of the eye called the retina and can lead to vision loss through several different pathways. When the blood vessels in the central area of the retina (the macula) are affected, it’s known as diabetic maculopathy. Diabetic retinopathy is a complication of diabetes, caused by high blood sugar levels damaging the back of the eye (retina). Diabetic retinopathy can cause blindness if left undiagnosed and untreated. Diabetic retinopathy is extremely unusual in children with diabetes who are under the age of 12.
Diabetic retinopathy is one of the most common causes of sight loss among people of working age. However, it usually takes several years for diabetic retinopathy to reach a stage where it could threaten your sight.
At first, diabetic retinopathy may cause no symptoms or only mild vision problems. Eventually, it can cause blindness.
You can have diabetic retinopathy and not know it. This is because it often has no symptoms in its early stages. As diabetic retinopathy gets worse, you will notice symptoms such as:
- seeing an increasing number of floaters,
- having blurry vision,
- having vision that changes sometimes from blurry to clear,
- seeing blank or dark areas in your field of vision,
- having poor night vision, and
- noticing colors appear faded or washed out losing vision.
Diabetic retinopathy symptoms usually affect both eyes.
The longer you have diabetes and the less controlled your blood sugar is, the more likely you are to develop this eye complication.
To minimize your risk of developing diabetic retinopathy, people with diabetes should:
- ensure they control their blood sugar levels, blood pressure and cholesterol
- attend diabetic eye screening appointments – annual screening is offered to all people with diabetes aged 12 and over to pick up and treat any problems early on. Diabetic eye screening is specifically for diabetic retinopathy and can’t be relied upon for other conditions.
- taking your diabetes medication as prescribed
- getting medical advice quickly if you notice any changes to your vision
- maintaining a healthy weight, eating a healthy, balanced diet, exercising regularly and stopping smoking.
If you’re diagnosed with diabetic retinopathy after diabetic eye screening, lifestyle changes and/or treatment can reduce the chances of the problem progressing.
Who is at risk of diabetic retinopathy?
Anyone with type 1 diabetes or type 2 diabetes is potentially at risk of developing diabetic retinopathy.
Patients with type 1 diabetes should have their eyes examined within five years of diagnosis 1). Those with type 2 diabetes should be referred at the time of diagnosis, since nearly 30% will already have diabetic retinopathy 2). The frequency of follow-up examinations will depend on the severity of the retinopathy at diagnosis. Typically, patients with early disease require annual examination, whereas those with more advanced retinopathy or who are pregnant will need more frequent follow-up 3).
You’re at a greater risk of developing diabetic retinopathy if you:
- have had diabetes for a long time
- have a persistently high blood sugar (blood glucose) level
- have high blood pressure
- have high cholesterol
- are pregnant
- are of Asian or Afro-Caribbean background
By keeping your blood sugar, blood pressure and cholesterol levels under control, you can reduce your chances of developing diabetic retinopathy.
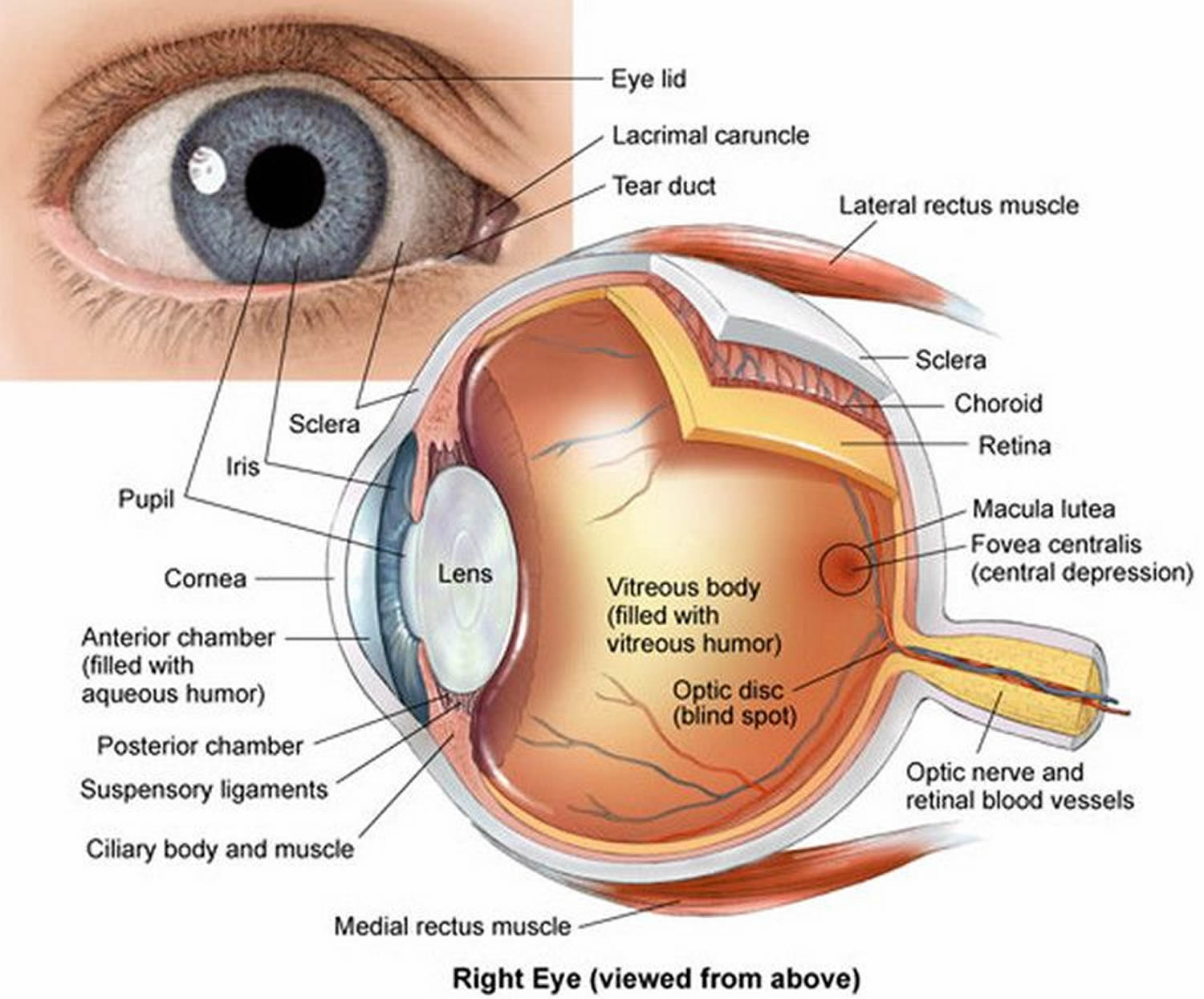
Eye Retina Anatomy
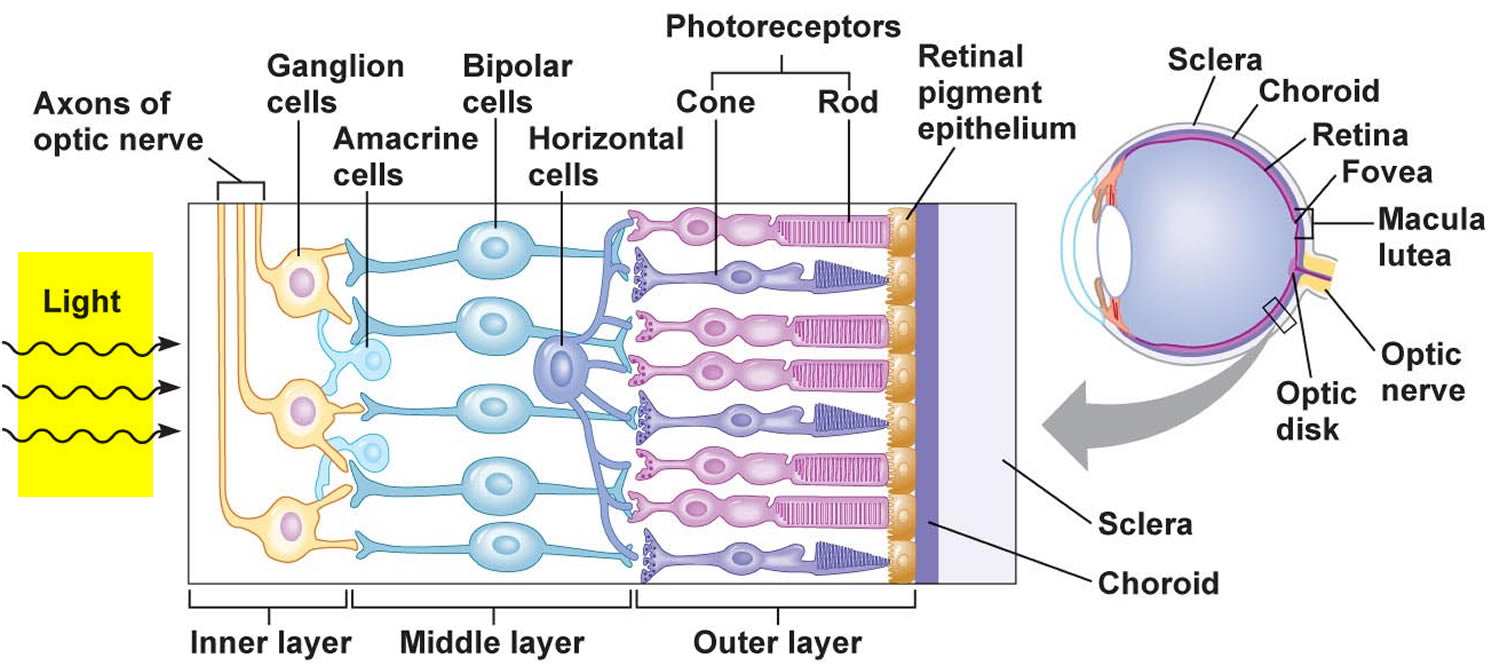
The retina is a multi-layered sheet composed of neurons, photoreceptors, and support cells. It is one of the most metabolically active organs in the body, and as a result, it is extremely sensitive to ischemia and nutrient imbalances 4). A perfused retina is a happy retina.
The outer one-third of the retina receives its blood supply from the choriocapillaris, a vascular network that lies between the retina and sclera. The inner two-thirds of the retina is supplied by branches of the central retinal artery, which comes from the ophthalmic artery (the first branch off of the internal carotid artery).
The central retinal artery exits out of the optic nerve, and its branches arch temporally both above and below the macula (the sensitive region of the retina responsible for central vision).
Figure 1. Structure of the human eye
Figure 2. The retina (inside human eye)
How diabetes can affect your eyes
The retina is the light-sensitive layer of cells at the back of the eye that converts light into electrical signals. The signals are sent to the brain and the brain turns them into the images you see.
The retina needs a constant supply of blood, which it receives through a network of tiny blood vessels. Over time, a persistently high blood sugar level can damage these blood vessels in three main stages:
- tiny bulges develop in the blood vessels, which may bleed slightly but don’t usually affect your vision – this is known as background retinopathy
- more severe and widespread changes affect the blood vessels, including more significant bleeding into the eye – this is known as pre-proliferative retinopathy
- scar tissue and new blood vessels, which are weak and bleed easily, develop on the retina – this is known as proliferative retinopathy and it can result in some loss of vision
However, if a problem with your eyes is picked up early, lifestyle changes and/or treatment can stop it getting worse.
Diabetic retinopathy stages
Diabetic retinopathy develops in stages over time. There are two main stages of diabetic eye disease:
- Non-proliferative diabetic retinopathy
- Proliferative diabetic retinopathy
The word “proliferative” refers to whether or not there is neovascularization (abnormal blood vessel growth) in the retina. Early disease without neovascularization is called nonproliferative diabetic retinopathy. As the disease progresses, it may evolve into proliferative diabetic retinopathy, which is defined by the presence of neovascularization and has a greater potential for serious visual consequences.
The main stages of diabetic retinopathy are described below. You won’t necessarily experience all of these.
Non proliferative diabetic retinopathy
This is the early stage of diabetic eye disease. Many people with diabetes have it.
With non-proliferative diabetic retinopathy, tiny blood vessels leak, making the retina swell. When the macula swells, it is called macular edema. This is the most common reason why people with diabetes lose their vision.
Also with non-proliferative diabetic retinopathy, blood vessels in the retina can close off. This is called macular ischemia. When that happens, blood cannot reach the macula. Sometimes tiny particles called exudates can form in the retina. These can affect your vision too.
If you have non-proliferative diabetic retinopathy, your vision will be blurry.
Non-proliferative diabetic retinopathy is further subdivided based on retinal findings:
- Early non-proliferative diabetic retinopathy – At least one microaneurysm present on retinal exam.
- Moderate non-proliferative diabetic retinopathy – Characterized by multiple microaneurysms, dot-and-blot hemorrhages, venous beading, and/or cotton wool spots.
- Severe non-proliferative diabetic retinopathy – In the most severe stage of non-proliferative diabetic retinopathy, you will find cotton wool spots, venous beading, and severe intraretinal microvascular abnormalities. It is diagnosed using the “4-2-1 rule.” A diagnosis is made if the patient has any of the following: diffuse intraretinal hemorrhages and microaneurysms in 4 quadrants, venous beading in ≥2 quadrants, or intraretinal microvascular abnormalities in ≥1 quadrant. Within one year, 52-75% of patients falling into this category will progress to proliferative diabetic retinopathy 5).
At non-proliferative diabetic retinopathy stage:
- there’s a high risk that your vision could eventually be affected
- you’ll usually be advised to have more frequent screening appointments every three or six months to monitor your eyes
Stage one: background retinopathy
This means that tiny bulges (microaneurysms) have appeared in the blood vessels in the back of your eyes (retina), which may leak small amounts of blood. This is very common in people with diabetes.
At this stage:
- your sight isn’t affected, although you’re at a higher risk of developing vision problems in the future
- you don’t need treatment, but you’ll need to take care to prevent the problem getting worse – read more about preventing diabetic retinopathy
- the chances of it progressing to the stages below within three years is over 25% if both of your eyes are affected
Hyperglycemia results in damage to retinal capillaries. This weakens the capillary walls and results in small outpouchings of the blood vessel lumens, known as microaneurysms. Microaneurysms eventually rupture to form hemorrhages deep within the retina, confined by the internal limiting membrane. Because of their dot-like appearance, they are called “dot-and-blot” hemorrhages. The weakened vessels also become leaky, causing fluid to seep into the retina. Fluid deposition under the macula, or macular edema, interferes with the macula’s normal function and is a common cause of vision loss in those with diabetic retinopathy. Resolution of fluid lakes can leave behind sediment, similar to a receding river after a flood. This sediment is composed of lipid byproducts and appears as waxy, yellow deposits called hard exudates. As non-proliferative diabetic retinopathy progresses, the affected vessels eventually become obstructed. This obstruction may cause infarction of the nerve fiber layer, resulting in fluffy, white patches called cotton wool spots.
Stage two: pre-proliferative retinopathy
This means that more severe and widespread changes are seen in the retina, including bleeding into the retina.
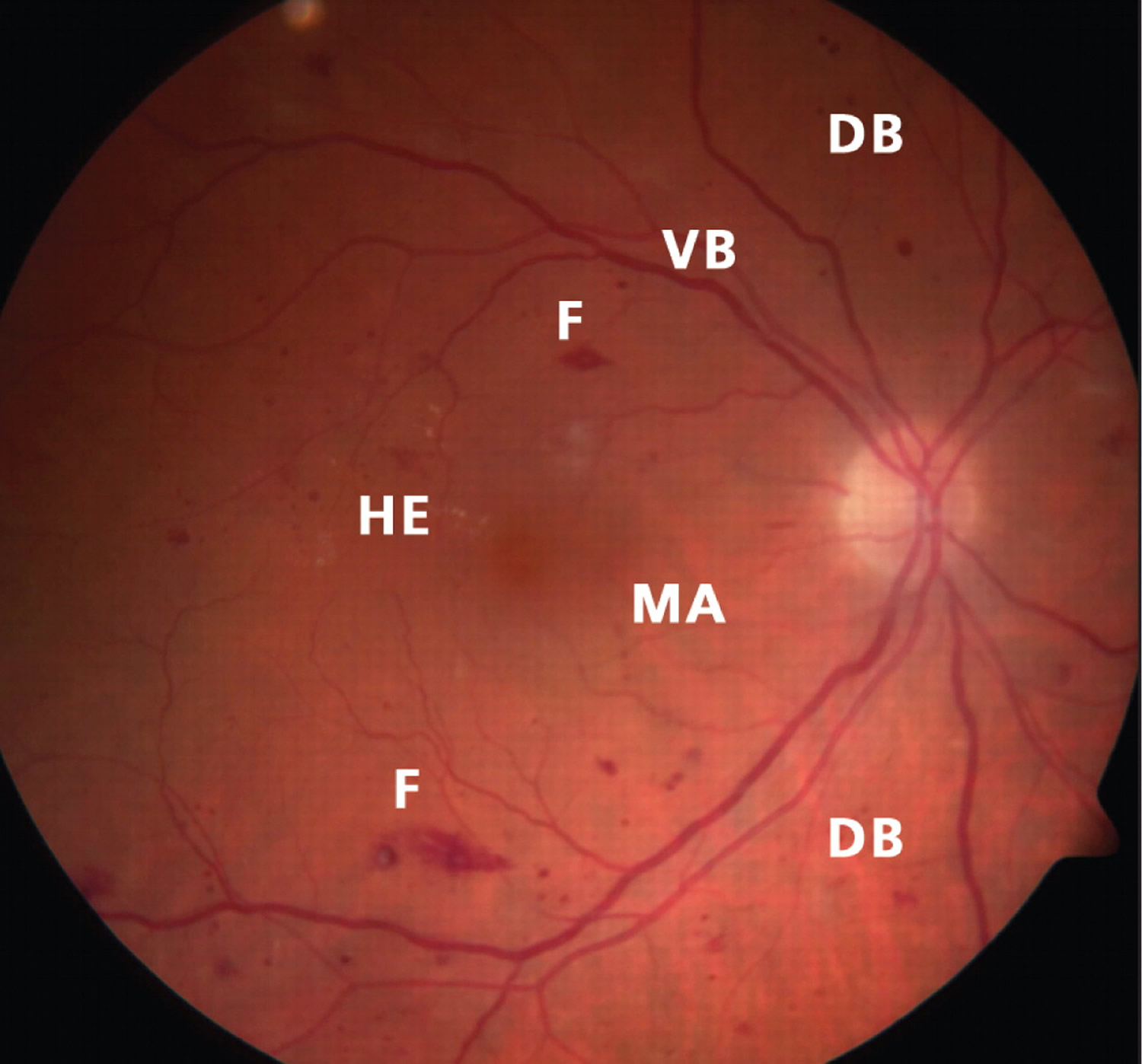
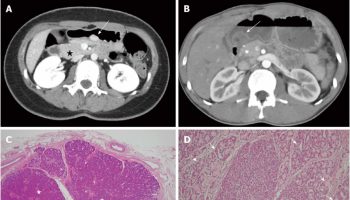
Figure 3. Nonproliferative diabetic retinopathy (right eye)
Footnote: Retina of the right eye showing characteristic features of nonproliferative diabetic retinopathy, including dot-blot hemorrhages (DB), flame-shaped hemorrhages (F), hard exudates (HE), micro-aneurysms (MA) and venous beading (VB).
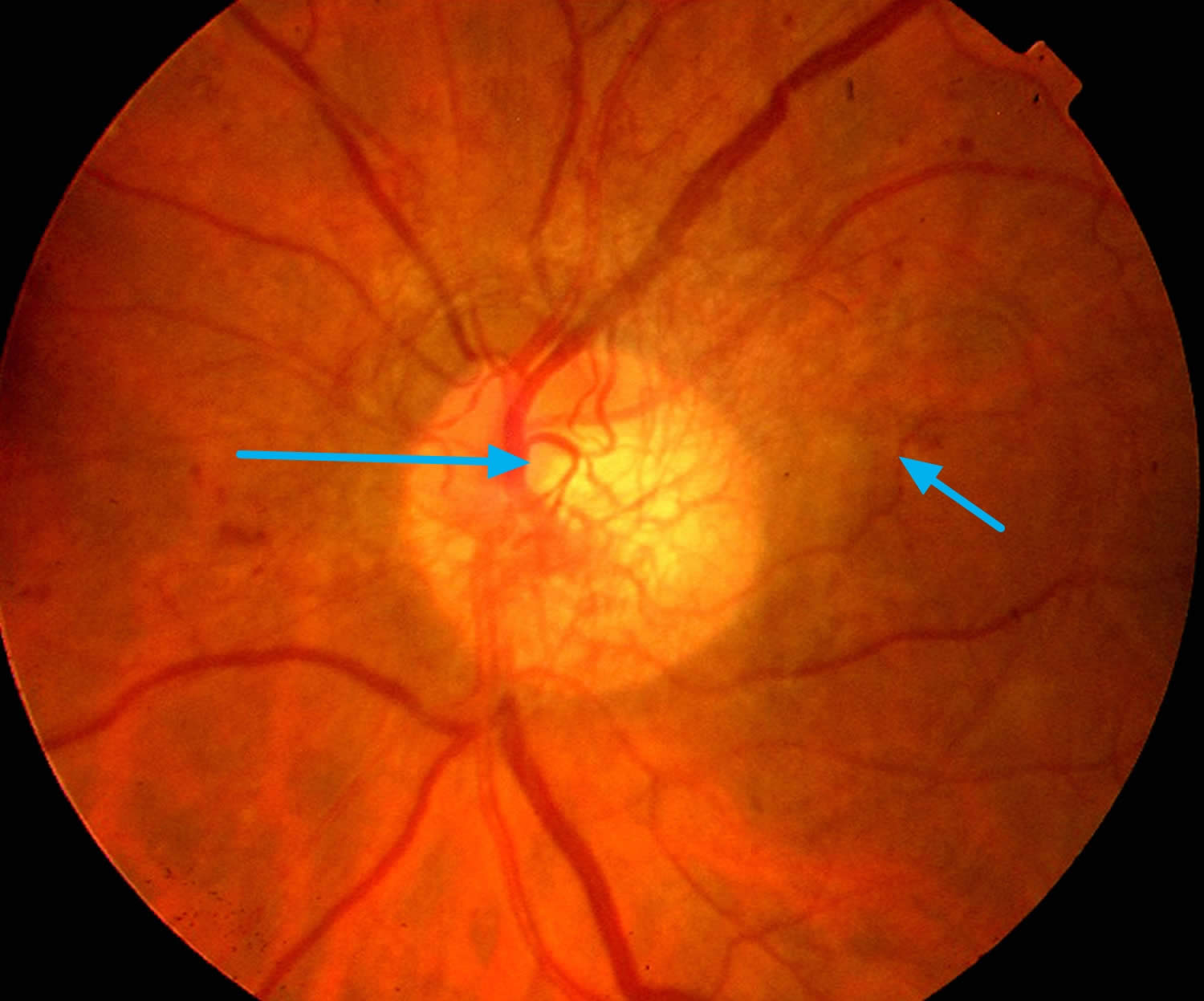
[Source 6)]Proliferative diabetic retinopathy
Proliferative diabetic retinopathy is the more advanced stage of diabetic eye disease. It happens when the retina starts growing new blood vessels. This is called neovascularization. These fragile new vessels often bleed into the vitreous. If they only bleed a little, you might see a few dark floaters. If they bleed a lot, it might block all vision.
These new blood vessels can form scar tissue. Scar tissue can cause problems with the macula or lead to a detached retina.
Proliferative diabetic retinopathy is very serious, and can steal both your central and peripheral (side) vision.
The retina has a high metabolic requirement, so with continued ischemia, retinal cells respond by releasing angiogenic signals such as vascular endothelial growth factor (VEGF). Angiogenic factors, like vascular endothelial growth factor (VEGF), stimulate growth of new retinal blood vessels to bypass the damaged vessels. This is referred to as neovascularization. In proliferative diabetic retinopathy, the fibrovascular proliferation extends beyond the internal limiting membrane. This may sound like a good idea, but the new vessels are leaky, fragile, and often misdirected. They may even grow off the retina and into the vitreous. As the vitreous shrinks with age, it pulls on these fragile vessels and can cause them to tear, resulting in a vitreous hemorrhage and sudden vision loss. These vessels may also scar down, forming strong anchors between the retina and vitreous causing traction on the retina. If enough force is created, a tractional retinal detachment may occur. This is another mechanism by which DR can cause sudden vision loss. If the retina is not re-attached soon, especially if the macula is involved, vision may be permanently compromised.
While the effects of neovascularization in proliferative diabetic retinopathy can be devastating, the most common cause of vision loss in diabetics is macular edema. Macular edema can occur in non-proliferative diabetic retinopathy, but it is more common in more severe cases of diabetic retinopathy due to the leakiness of the new blood vessels 7).
Diabetics can also have problems located more anteriorly in the eye. The angiogenic molecules that are produced by the retina may float anteriorly, causing neovascularization of the iris. These vessels can grow into the angle of the anterior chamber where the trabecular meshwork, the drain of the eye, resides. This can obstruct outflow of aqueous fluid, raising intraocular pressure and causing acute glaucoma.
Figure 4. Proliferative diabetic retinopathy (key funduscopic feature of proliferative diabetic retinopathy is neovascularizaton, seen here around the optic disk)
Proliferative retinopathy
This means that new blood vessels and scar tissue have formed on your retina, which can cause significant bleeding and lead to retinal detachment (where the retina pulls away from the back of the eye).
At this stage:
- there’s a very high risk you could lose your vision
- treatment will be offered to stabilize your vision as much as possible, although it won’t be possible to restore any vision you’ve lost
Diabetic maculopathy
In some cases, the blood vessels in the part of the eye called the macula (the central area of the retina) can also become leaky or blocked. This is known as diabetic maculopathy.
If this is detected:
- there’s a high risk that your vision could eventually be affected
- you may be advised to have more frequent specialized testing to monitor your eyes
- you may be referred to a hospital specialist to discuss treatments that can help stop the problem getting worse
Diabetic retinopathy signs and symptoms
You won’t usually notice diabetic retinopathy in the early stages, as it doesn’t tend to have any obvious symptoms until it’s more advanced.
However, early signs of the condition can be picked up by taking photographs of the eyes during diabetic eye screening.
Contact your doctor or diabetes care team immediately if you experience:
- gradually worsening vision
- sudden vision loss
- shapes floating in your field of vision (floaters)
- blurred or patchy vision
- eye pain or redness
These symptoms don’t necessarily mean you have diabetic retinopathy, but it’s important to get them checked out. Don’t wait until your next screening appointment.
Diabetic retinopathy screening
Screening is a way of detecting diabetic retinopathy early before you notice any changes to your vision. Diabetic retinopathy doesn’t usually cause any noticeable symptoms in the early stages.
Diabetic eye screening test involves examining the back of the eyes and taking photographs. Depending on your result, you may be advised to return for another appointment a year later, attend more regular appointments, or discuss treatment options with a specialist.
Everyone with diabetes who is 12 years old or over is invited for eye screening once a year. Diabetic eye screening is a key part of diabetes care. People with diabetes are at risk of damage from diabetic retinopathy, a condition that can lead to sight loss if it’s not treated.
Diabetic eye screening is offered because:
- diabetic retinopathy doesn’t tend to cause any symptoms in the early stages
- diabetic retinopathy can cause permanent blindness if not diagnosed and treated promptly
- screening can detect problems in your eyes before they start to affect your vision
- if problems are caught early, treatment can help prevent or reduce vision loss
If diabetic retinopathy is detected early enough, treatment can stop it getting worse. Otherwise, by the time symptoms become noticeable, it can be much more difficult to treat. This is why the diabetic eye screening programme was introduced.
Diabetic eye screening test takes about half an hour and involves examining the back of the eyes and taking photographs of the retina.
If you have sight problems in between screening appointments, such as sudden vision loss or a deterioration in your vision, seek immediate medical advice. Don’t wait until your next screening appointment.
What happens during diabetic eye screening
The screening appointment should last about 30 minutes.
When you arrive, the procedure will be explained to you. If you have any questions, ask the healthcare professional who is treating you.
You’ll be given eye drops to enlarge your pupils, which takes between 15 and 20 minutes, and photographs of your retina will be taken.
There will be a flash of light each time a photograph is taken, but the camera won’t touch your eye. Although the light is bright, it shouldn’t be uncomfortable.
The eye drops may cause your eyes to sting slightly, and after about 15 minutes your vision will be blurred. You may find it difficult to focus on objects that are close to you.
Depending on the type of eye drops used, the blurring can last between two and six hours. You won’t be able to drive home from your appointment, so you may want to bring someone with you.
After the screening procedure, you may also find that everything looks very bright. You may want to take a pair of sunglasses to wear afterwards.
Side effects
In very rare cases, the eye drops can cause a sudden pressure increase within the eye. This requires prompt treatment at an eye unit.
The symptoms of a pressure increase are:
- pain or severe discomfort in your eye
- redness of the white of your eye
- constantly blurred vision, sometimes with rainbow halos around lights
If you experience any of these symptoms after screening, go back to the screening centre or your nearest accident and emergency (A&E) department.
Your screening results
Both you and your doctor should receive a letter letting you know your results.
You won’t get the results immediately as the photographs need to be studied by a number of different healthcare professionals, including someone who is trained in identifying and grading retinopathy.
Diabetic eye screening test results may show either:
- no retinopathy
- background retinopathy – also called stage one retinopathy
- degrees of referable retinopathy – this means retinopathy that requires referral to an eye specialist for further assessment and treatment
You may need to have a further assessment if:
- the photographs aren’t clear enough to give an accurate result
- you have retinopathy that could affect your sight and follow-up treatment is needed
- you have retinopathy that needs to be checked more than once a year
- other eye conditions are detected, such as glaucoma (a group of eye conditions that affect vision) or cataracts (cloudy patches in the lens of the eye)
If your results show no retinopathy or background retinopathy, you’ll be invited back for another screening appointment a year later.
You can also reduce your risk of developing diabetic retinopathy in the future by controlling your blood sugar levels and blood pressure.
If screening detects signs that diabetic retinopathy or maculopathy is threatening your sight, you’ll be given information about how far the condition has progressed. This will determine the type of treatment you receive.
If you have questions about your results, contact your local diabetic eye screening service. Their details should be on the letter you received from them.
Diabetic eye screening in pregnancy
If you have diabetes and become pregnant, you’ll need special care as there are risks to both mother and baby associated with the condition.
You’ll be offered additional tests for diabetic retinopathy at or soon after your first antenatal clinic visit, and also after 28 weeks of pregnancy.
If the early stages of retinopathy are found at the first screening, you’ll also be offered another test between 16 and 20 weeks of pregnancy.
If serious retinopathy is found at any screening, you’ll be referred to an eye specialist.
Some women who don’t have diabetes can develop hyperglycaemia (high blood sugar) during pregnancy. This is known as gestational diabetes.
Pregnant women who develop gestational diabetes aren’t offered screening for diabetic retinopathy.
Diabetic retinopathy causes
Although the exact pathophysiology of diabetic retinopathy is unknown, hyperglycemia is thought to cause endothelial damage, selective loss of pericytes, and basement membrane thickening, all of which contribute to leaky, incompetent blood vessels.
The risk of diabetic retinopathy is directly related to the duration of diabetes and the severity of hyperglycemia 8).
- Among patients with type 1 diabetes, 25%, 60% and 80% will have retinopathy after 5, 10 and 15 years of disease 9).
- Among patients with type 2 diabetes, 40% who use insulin and 24% who do not use insulin will have retinopathy at five years; the proportions will increase to 84% and 53%, respectively, at 19 years 10).
- Poor glycemic control, smoking, hyperlipidemia, hypertension, anemia and nephropathy are associated with progression of diabetic retinopathy.
Strict control of blood glucose levels and blood pressure remain key strategies for decreasing the risk of diabetic retinopathy or slowing its progression
Studies from the Diabetes Control and Complications Trial Research Group and the United Kingdom Prospective Diabetes Study Group both showed significant reductions in the development of diabetic retinopathy among patients who intensely controlled their blood glucose levels 11). Control of blood pressure and serum lipid levels can slow the progression of the retinopathy.
Diabetic retinopathy prevention
You can reduce your risk of developing diabetic retinopathy, or help stop it getting worse, by keeping your blood sugar levels, blood pressure and cholesterol levels under control.
This can often be done by making healthy lifestyle choices, although some people will also need to take medication.
Healthy lifestyle
Adopting a few lifestyle changes can improve your general health and reduce your risk of developing retinopathy. These include:
- eating a healthy, balanced diet – in particular, try to cut down on salt, fat and sugar
- losing weight if you’re overweight – you should aim for a BMI (body mass index) of 18.5-24.9; use the BMI calculator to work out your BMI
- BMI Calculator Adults. https://www.cdc.gov/healthyweight/assessing/bmi/adult_BMI/english_bmi_calculator/bmi_calculator.html
- BMI Calculator Children. https://www.cdc.gov/healthyweight/bmi/calculator.html
- exercising regularly – aim to do at least 150 minutes of moderate-intensity activity, such as walking or cycling, a week; doing 10,000 steps a day can be a good way to reach this target
- stopping smoking if you smoke
- not exceeding the recommended alcohol limits – men and women are advised not to regularly drink more than 14 alcohol units a week
You may also be prescribed medication to help control your blood sugar level (such as insulin or metformin), blood pressure (such as ACE inhibitors) and/or cholesterol level (such as statins).
Know your blood sugar, blood pressure and cholesterol levels
It can be easier to keep your blood sugar levels, blood pressure and cholesterol levels under control if you know what level they are and monitor them regularly.
The lower you can keep them, the lower your chances of developing retinopathy are. Your diabetes care team can let you know what your target levels should be.
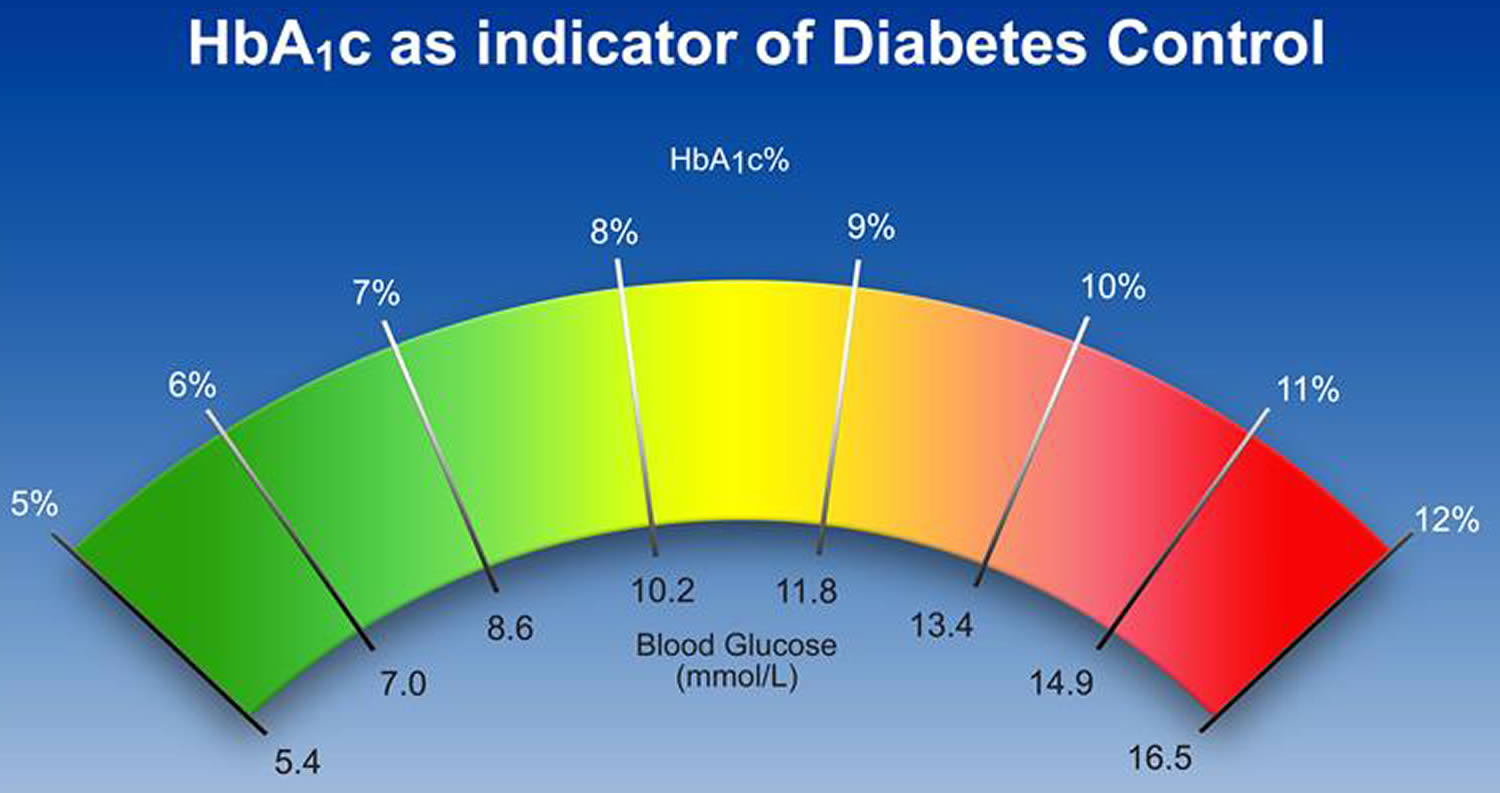
Blood sugar
If you check your blood sugar level at home, it should be 4 to 10mmol/l . The level can vary throughout the day, so try to check it at different times.
The check done at your doctor surgery is a measure of your average blood sugar level over the past few weeks. You should know this number, as it is the most important measure of your diabetes control.
It’s called HbA1c, and for most people with diabetes it should be around 48 mmol/l or 6.5%.
Figure 5. HbA1c chart
Table 1. HbA1c and Blood Glucose Levels
| HbA1c (%) | HbA1c (mmol/mol) | Ave. Blood Glucose (mmol/L) |
|---|---|---|
| 13 | 119 | 18 mmol/L |
| 12 | 108 | 17 mmol/L |
| 11 | 97 | 15 mmol/L |
| 10 | 86 | 13 mmol/L |
| 9 | 75 | 12 mmol/L |
| 8 | 64 | 10 mmol/L |
| 7 | 53 | 8 mmol/L |
| 6 | 42 | 7 mmol/L |
| 5 | 31 | 5 mmol/L |
Blood pressure
You can ask for a blood pressure test at your doctor or you can buy a blood pressure monitor to use at home. Blood pressure is measured in millimeters of mercury (mmHg) and is given as two figures.
If you have diabetes, you’ll normally be advised to aim for a blood pressure reading of no more than 120/80mmHg, or less than 130/80mmHg if you have diabetes complications , such as eye damage. A blood pressure less than 120/80 mmHg is normal. A blood pressure of 140/90 mmHg or more is too high. People with levels in between 120/80 and 140/90 have a condition called prehypertension, which means they are at high risk for high blood pressure.
Here are some easy tips to help reduce your blood pressure:
- Work with your health care provider to find a treatment plan that’s right for you.
- Eat whole-grain breads and cereals.
- Try herbs and spices instead of salt to flavor foods.
- Check food labels and choose foods with less than 400 mg of sodium per serving.
- Lose weight or take steps to prevent weight gain.
- Limit alcohol consumption and consult your health care provider about whether it is safe to drink alcohol at all.
- If you smoke, get help to quit.
- Ask your health care provider about medications to help reduce high blood pressure. Samples of these types of medications include ACE inhibitors, ARBs, beta blockers, calcium channel blockers and diuretics.
Table 2. Desirable Blood Pressure Levels
| Normal | systolic: less than 120 mmHg diastolic: less than 80mmHg |
|---|---|
| At risk (prehypertension) | systolic: 120–139 mmHg diastolic: 80–89 mmHg |
| High | systolic: 140 mmHg or higher diastolic: 90 mmHg or higher |
Cholesterol
Your cholesterol level can be measured with a simple blood test carried out by your doctor. The result is given in millimoles per liter of blood (mmol/l) or milligrams per deciliter (mg/dL).
If you have diabetes, you’ll normally be advised to aim for a total blood cholesterol level of no more than 4 mmol/l or 155 mg/dl.
Table 3. Desirable Cholesterol Levels
| Total cholesterol | Less than 200 mg/dL or 5.17 mmol/l |
| LDL (“bad”) cholesterol | Less than 100 mg/dL or 2.58 mmol/l |
| HDL (“good”) cholesterol | Higher than 40 mg/dL or 1.0 mmol/l |
| Triglycerides | Less than 150 mg/dL or 1.7 mmol/l |
Diabetic retinopathy diagnosis
Drops will be put in your eye to dilate (widen) your pupil. This allows your ophthalmologist to look through a special lens to see the inside of your eye.
Your doctor may do fluorescein angiography to see what is happening with your retina. Yellow dye (called fluorescein) is injected into a vein, usually in your arm. The dye travels through your blood vessels. A special camera takes photos of the retina as the dye travels throughout its blood vessels. This shows if any blood vessels are blocked or leaking fluid. It also shows if any abnormal blood vessels are growing.
Optical coherence tomography (OCT) is another way to look closely at the retina. A machine scans the retina and provides detailed images of its thickness. This helps your doctor find and measure swelling of your macula.
Diabetic retinopathy treatment
Your treatment is based on what your ophthalmologist sees in your eyes. Treatment options may include:
Managing your diabetes
The most important part of your treatment is to keep your diabetes under control.
In the early stages of diabetic retinopathy, controlling your diabetes can help prevent vision problems developing.
In the more advanced stages, when your vision is affected or at risk, keeping your diabetes under control can help stop the condition getting worse. Sometimes, good sugar control can even bring some of your vision back. Controlling your blood pressure keeps your eye’s blood vessels healthy.
Controlling your blood sugar and blood pressure can stop vision loss. Carefully follow the diet your nutritionist has recommended. Take the medicine your diabetes doctor prescribed for you.
Treatments for advanced diabetic retinopathy
For diabetic retinopathy that is threatening or affecting your sight, the main treatments are:
- laser treatment – to treat the growth of new blood vessels at the back of the eye (retina) in cases of proliferative diabetic retinopathy, and to stabilize some cases of maculopathy
- eye injections – to treat severe maculopathy that’s threatening your sight
- eye surgery – to remove blood or scar tissue from the eye if laser treatment isn’t possible because retinopathy is too advanced
Laser treatment
Laser treatment is used to treat new blood vessels at the back of the eyes in the advanced stages of diabetic retinopathy. Laser surgery can also help shrink blood vessels and prevent them from growing again. This is done because the new blood vessels tend to be very weak and often cause bleeding into the eye. Laser surgery is also used to help seal off leaking blood vessels. This can reduce swelling of the retina.
Sometimes more than one treatment is needed.
Treatment can help stabilize the changes in your eyes caused by your diabetes and stop your vision getting any worse, although it won’t usually improve your sight.
Laser treatment:
- involves shining a laser into your eyes – you’ll be given local anaesthetic drops to numb your eyes; eye drops are used to widen your pupils and special contact lenses are used to hold your eyelids open and focus the laser onto your retina
- normally takes around 20-40 minutes
- is usually carried out on an outpatient basis, which means you won’t need to stay in hospital overnight
- may require more than one visit to a laser treatment clinic
- isn’t usually painful, although you may feel a sharp pricking sensation when certain areas of your eye are being treated
Laser treatment side effects
After treatment, you may have some side effects for a few hours. These can include:
- blurred vision – you won’t be able to drive until this passes, so you’ll need to arrange for a friend or relative to drive you home, or take public transport
- increased sensitivity to light – it might help to wear sunglasses until your eyes have adjusted
- aching or discomfort – over-the-counter painkillers, such as paracetamol, should help
Possible complications
You should be told about the risks of treatment in advance. Potential complications include:
- reduced night or peripheral (side) vision – some people may have to stop driving as a result of this
- bleeding into the eye or objects floating in your vision (floaters)
- being able to “see” the pattern made by the laser on the back of your eye for a few months
- a small, but permanent, blind spot close to the center of your vision
Get medical advice if you notice that your sight gets worse after treatment.
Eye injections
In some cases of diabetic maculopathy, injections of a medicine called anti-VEGF may be given directly into your eyes to prevent new blood vessels forming at the back of the eyes and reduce swelling of the macula, slowing vision loss and perhaps improving vision.
The main medicines used are called ranibizumab (Lucentis) and aflibercept (Eylea). These can help stop the problems in your eyes getting worse, and may also lead to an improvement in your vision.
During treatment:
- the skin around your eyes will be cleaned and covered with a sheet
- small clips will be used to keep your eyes open
- you’ll be given local anaesthetic drops to numb your eyes
- a very fine needle is carefully guided into your eyeball and the injection is given
The injections are usually given once a month to begin with. Once your vision starts to stabilize, they’ll be stopped or given less frequently.
Injections of steroid medication may sometimes be given instead of anti-VEGF injections, or if the anti-VEGF injections don’t help.
Your doctor will recommend how many injections you will need over time.
Risks and side effects of anti-VEGF eye injections
Possible risks and side effects of anti-VEGF injections include:
- eye irritation or discomfort
- bleeding inside the eye
- floaters or a feeling of having something in your eye
- watery or dry, itchy eyes
There’s also a risk that the injections could cause blood clots to form, which could lead to a heart attack or stroke. This risk is small, but it should be discussed with you before you give your consent to treatment.
The main risk with steroid injections is increased pressure inside the eye.
Eye surgery
Surgery may be carried out to remove some of the vitreous humour from the eye. This is the transparent, jelly-like substance that fills the space behind the lens of the eye.
The operation, known as vitreoretinal surgery or vitrectomy, may be needed if:
- a large amount of blood has collected in your eye
- there’s extensive scar tissue that’s likely to cause, or has already caused, retinal detachment
During the procedure, the surgeon will make a small incision in your eye before removing some of the vitreous humour, removing any scar tissue and using a laser to prevent a further deterioration in your vision.
Vitreoretinal surgery (vitrectomy) is usually carried out under local anaesthetic and sedation. This means you will not experience any pain or have any awareness of the surgery being performed.
After the procedure
You should be able to go home on the same day or the day after your surgery.
For the first few days, you may need to wear a patch over your eye. This is because activities such as reading and watching television can quickly tire your eye to begin with.
You will probably have blurred vision after the operation. This should improve gradually, although it may take several months for your vision to fully return to normal.
Your surgeon will advise you about any activities you should avoid during your recovery.
Risks and side effects of vitrectomy
Possible risks of vitreoretinal surgery include:
- developing a cataract
- further bleeding into the eye
- retinal detachment
- fluid build-up in the cornea (outer layer at the front of the eye)
- infection in the eye
There’s also a small chance that you will need further retinal surgery afterwards. Your surgeon will explain the risks to you.
References [ + ]