What is eastern equine encephalitis
Eastern equine encephalitis is a rare illness in humans caused by the eastern equine encephalitis virus that is transmitted to humans by the bite of an infected mosquito.
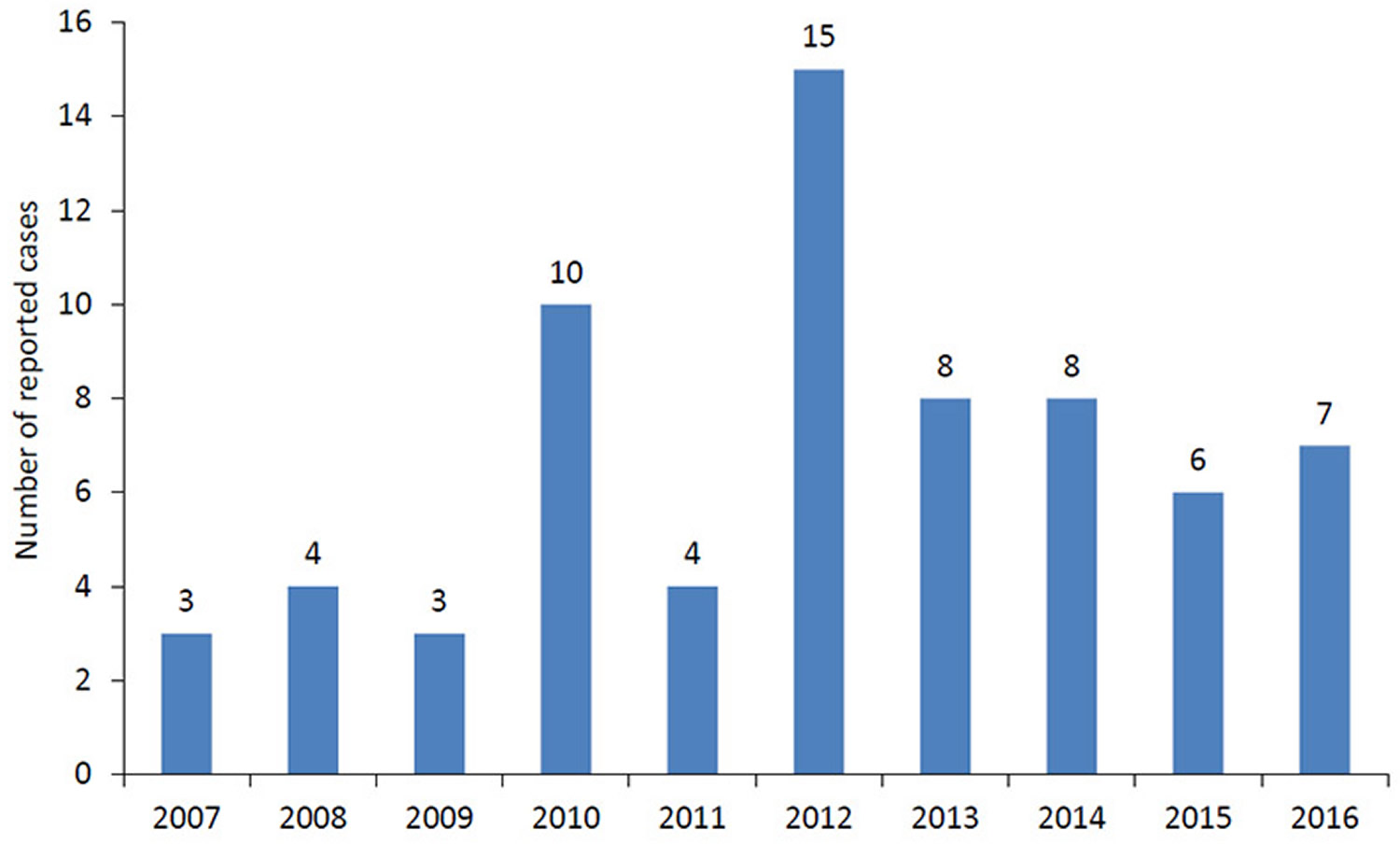
Only a few cases (~ 5-10 cases) of eastern equine encephalitis are reported in the United States each year. Most cases occur in the Atlantic and Gulf Coast states.
Most persons infected with eastern equine encephalitis virus have no apparent illness. Severe cases of eastern equine encephalitis (involving encephalitis, an inflammation of the brain) begin with the sudden onset of headache, high fever, chills, and vomiting. The illness may then progress into disorientation, seizures, or coma. Eastern equine encephalitis is one of the most severe mosquito-transmitted diseases in the United States with approximately 33% mortality and significant brain damage in most survivors.
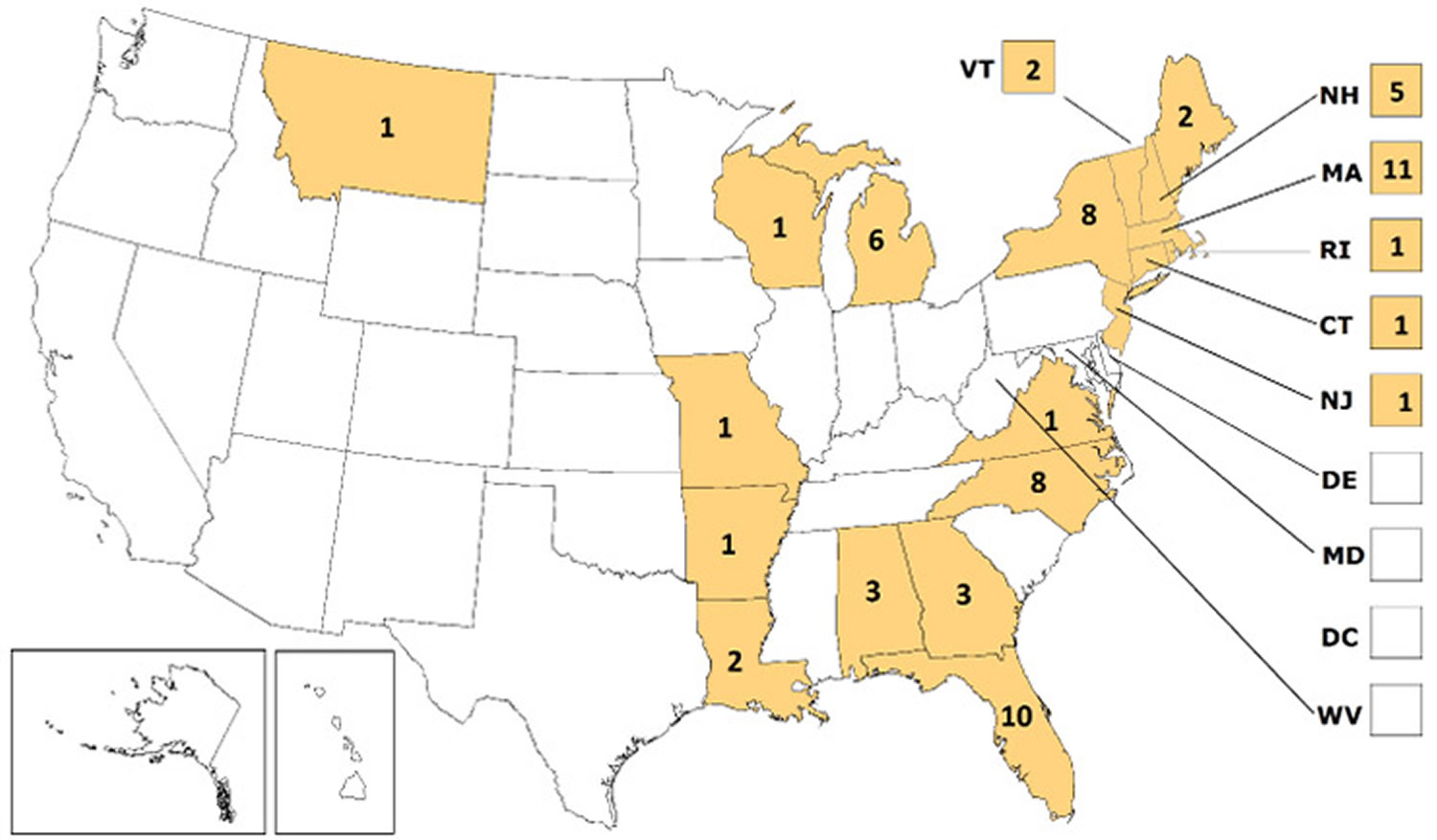
In the United States, an average of 7 human cases of eastern equine encephalitis are reported annually. Most cases of eastern equine encephalitis have been reported from Florida, Massachusetts, New York, and North Carolina. Eastern equine encephalitis virus transmission is most common in and around freshwater hardwood swamps in the Atlantic and Gulf Coast states and the Great Lakes region (see Figure 1).
There is no specific treatment for eastern equine encephalitis; care is based on symptoms. You can reduce your risk of being infected with eastern equine encephalitis virus by using insect repellent, wearing protective clothing, and staying indoors while mosquitoes are most active. If you think you or a family member may have eastern equine encephalitis, it is important to consult your healthcare provider for proper diagnosis.
Figure 1. Eastern equine encephalitis virus neuroinvasive disease cases reported in the United States from year 2007–2016
Note: From 2007 through 2016, Eastern equine encephalitis virus neuroinvasive disease cases have been reported in Alabama (3), Arkansas (1), Connecticut (1), Florida (10), Georgia (3), Louisiana (2), Maine (2), Massachusetts (11), Michigan (6), Missouri (1), Montana (1), New Hampshire (5), New Jersey (1), New York (8), North Carolina (8), Rhode Island (1), Vermont (2), Virginia (1), and Wisconsin (1).
Figure 2. Eastern equine encephalitis virus neuroinvasive disease cases reported in the United States from year 2007–2016
Eastern equine encephalitis virus
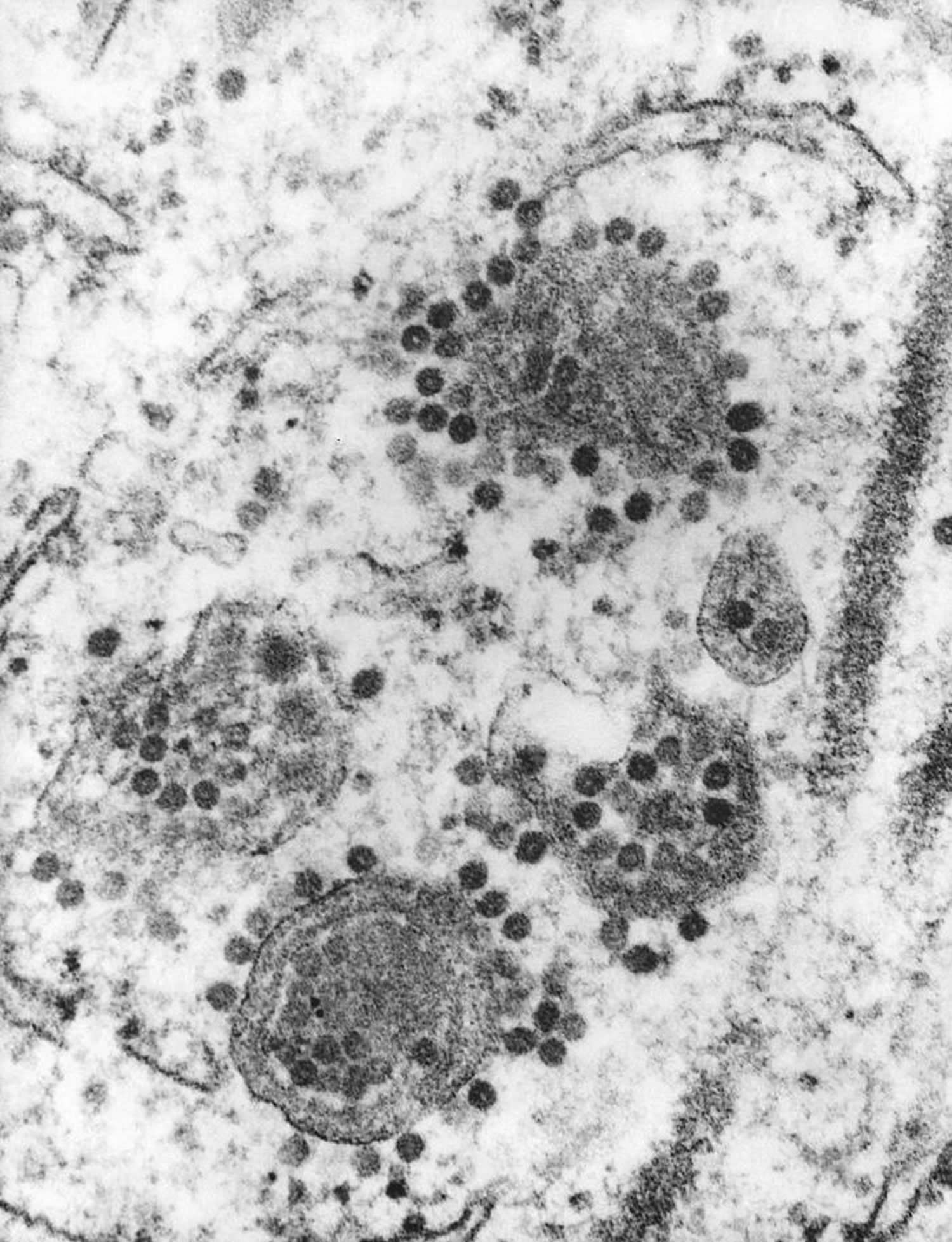
Eastern equine encephalitis virus is a member of the genus Alphavirus, family Togaviridae. Other medically important alphaviruses found in the Americas include Western equine encephalitis virus and Venezuelan equine encephalitis virus. Eastern equine encephalitis virus has a single-stranded, positive-sense RNA genome. The virus particles are spherical and have a diameter of 60-65 nm. Of the four lineages of eastern equine encephalitis virus , Group I is endemic in North America and the Caribbean and causes most human disease cases; the other three groups (IIA, IIB, and III) cause primarily equine illness in Central and South America.
Figure 3. Eastern equine encephalitis virus (electron microscopic image revealed the presence of numerous Eastern equine encephalitis virus virions in this specimen of central nervous system tissue)
Eastern equine encephalitis transmission
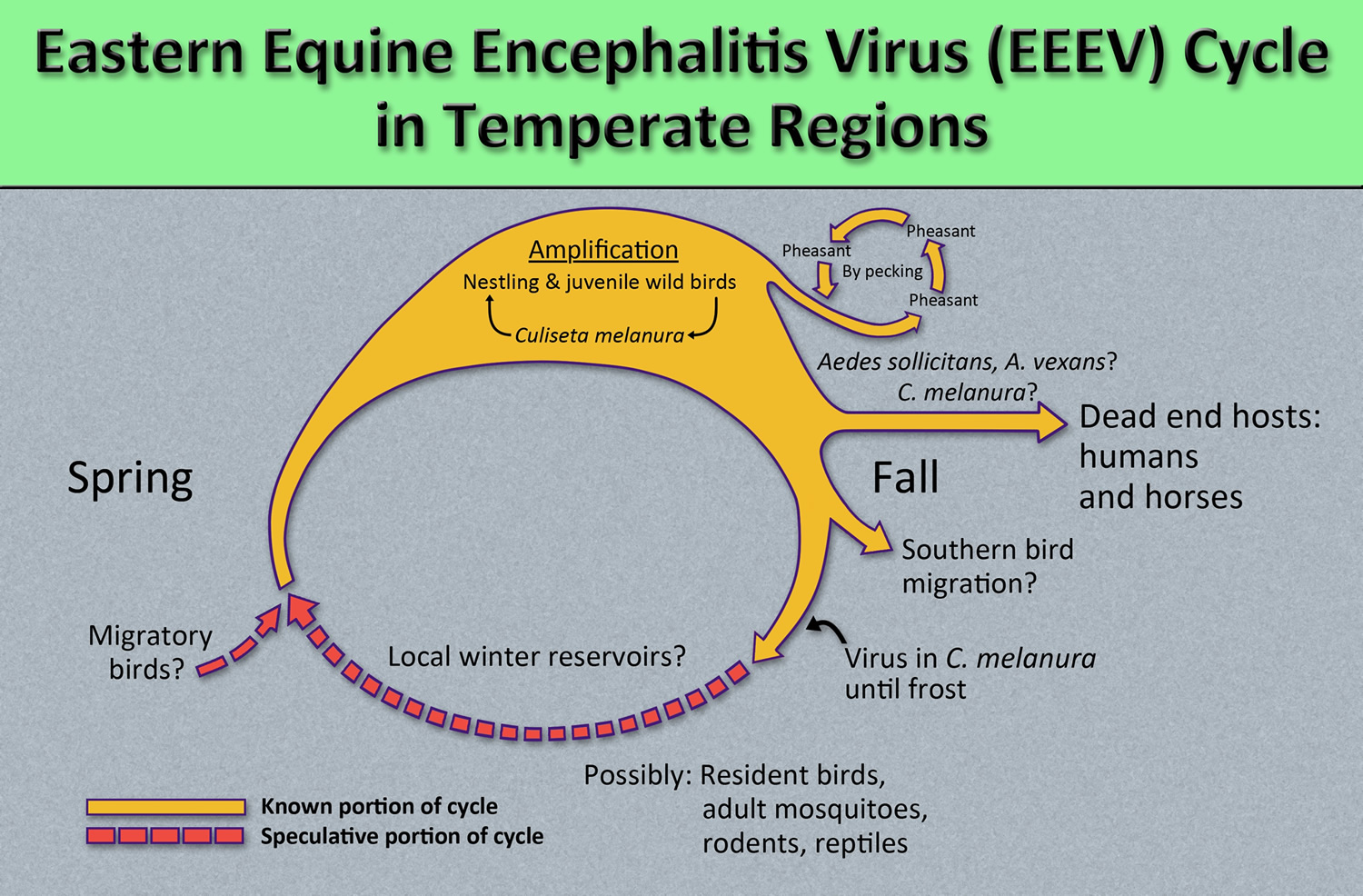
Eastern equine encephalitis virus is maintained in a cycle between Culiseta melanura mosquitoes and avian hosts in freshwater hardwood swamps. Culiseta melanura is not considered to be an important vector of eastern equine encephalitis virus to humans because it feeds almost exclusively on birds. Transmission to humans requires mosquito species capable of creating a “bridge” between infected birds and uninfected mammals such as some Aedes, Coquillettidia, and Culex species.
Horses are susceptible to eastern equine encephalitis virus infection and some cases are fatal. Eastern equine encephalitis virus infections in horses, however, are not a significant risk factor for human infection because horses (like humans) are considered to be “dead-end” hosts for the virus (i.e., the concentration of virus in their bloodstreams is usually insufficient to infect mosquitoes).
Eastern equine encephalitis virus is transmitted to humans through the bite of an infected mosquito. Human eastern equine encephalitis virus cases occur relatively infrequently, largely because the primary transmission cycle takes place in and around swampy areas where human populations tend to be limited. All residents of and visitors to areas where eastern equine encephalitis virus activity has been identified are at risk of infection. People who engage in outdoor work and recreational activities in endemic areas are at increased risk of infection. Persons over age 50 and under age 15 seem to be at greatest risk for developing severe disease when infected with eastern equine encephalitis virus. Overall, only about 4-5% of human eastern equine encephalitis virus infections result in eastern equine encephalitis. Eastern equine encephalitis virus infection is thought to confer life-long immunity against re-infection. It does not confer significant cross-immunity against other alphaviruses (e.g., western equine encephalitis virus), and it confers no cross-immunity against flaviviruses (e.g., West Nile virus) or bunyaviruses (e.g., La Crosse virus).
Figure 4. Eastern equine encephalitis virus lifecycle
Eastern equine encephalitis prevention
There is no vaccine against Eastern equine encephalitis virus for humans. Reducing exposure to mosquitoes is the best defense against infection with eastern equine encephalitis virus and other mosquito-borne viruses. There are several approaches you and your family can use to prevent and control mosquito-borne diseases.
Your best bet for preventing Eastern equine encephalitis virus and other mosquito-borne illnesses is to prevent mosquito bites and to avoid exposure to mosquitoes and eliminate standing water, where mosquitoes breed. Be aware of the Eastern equine encephalitis virus activity in your area and take action to protect yourself and your family.
- Unclog roof gutters.
- Empty unused swimming pools or empty standing water on pool covers.
- Change water in birdbaths and pet bowls regularly.
- Remove old tires or unused containers that might hold water and serve as a breeding place for mosquitoes.
- Install or repair screens on windows and doors.
To reduce your exposure to mosquitoes:
- Avoid unnecessary outdoor activity when mosquitoes are most prevalent, such as at dawn, dusk and early evening.
- Wear long-sleeved shirts and long pants when outdoors.
- Apply mosquito repellent containing an Environmental Protection Agency-registered insect repellent to your skin and clothing. Choose the concentration based on the hours of protection you need — the higher the percentage (concentration) of the active ingredient, the longer the repellent will work. Follow the directions on the package, paying special attention to recommendations for use on children.
- When outside, cover your infant’s stroller or playpen with mosquito netting.
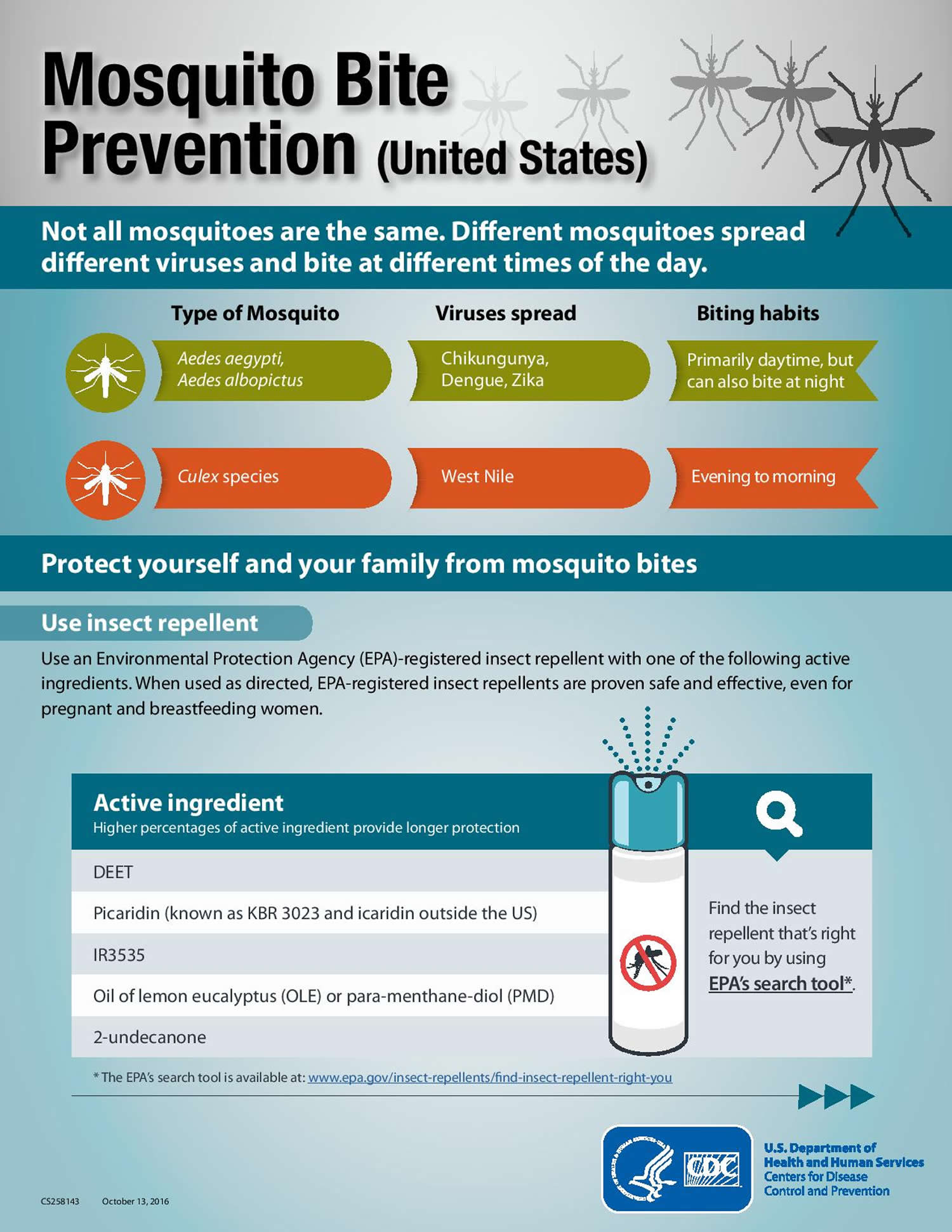
Prevent Mosquito Bites
Use Insect Repellent
Use Environmental Protection Agency (EPA)-registered insect repellents with one of the active ingredients below 1). When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women.
- DEET
- Picaridin (known as KBR 3023 and icaridin outside the US)
- IR3535
- Oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD)
- 2-undecanone
Find the insect repellent that’s right for you by using EPA’s search tool (https://www.epa.gov/insect-repellents/find-repellent-right-you).
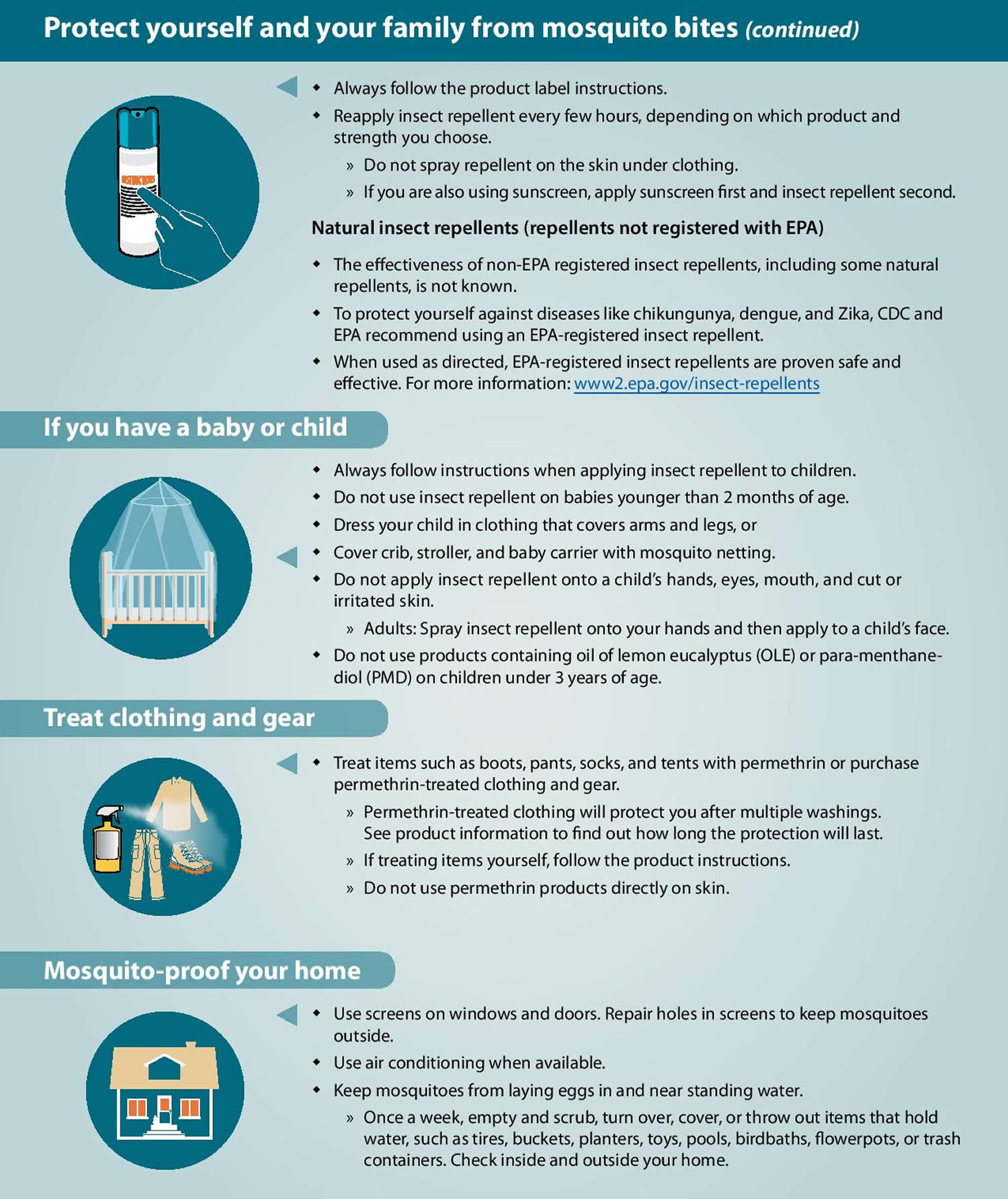
Tips for Everyone
- Always follow the product label instructions.
- Reapply insect repellent as directed.
- Do not spray repellent on the skin under clothing.
- If you are also using sunscreen, apply sunscreen first and insect repellent second.
Tips for Babies & Children
- Always follow instructions when applying insect repellent to children.
- Do NOT use insect repellent on babies younger than 2 months old.
- Do NOT apply insect repellent onto a child’s hands, eyes, mouth, and cut or irritated skin.
- Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- Do NOT use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
Natural insect repellents (repellents not registered with EPA)
- Scientists do not know the effectiveness of non-EPA registered insect repellents, including some natural repellents.
- To protect yourself against diseases spread by mosquitoes, CDC and EPA recommend using an EPA-registered insect repellent.
- Choosing an EPA-registered repellent ensures the EPA has evaluated the product for effectiveness.
Protect your baby or child
- Dress your child in clothing that covers arms and legs.
- Cover crib, stroller, and baby carrier with mosquito netting.
Wear long-sleeved shirts and long pants
- Treat items, such as boots, pants, socks, and tents, with permethrin* or buy permethrin-treated clothing and gear.
- Permethrin-treated clothing will protect you after multiple washings. See product information to find out how long the protection will last.
- If treating items yourself, follow the product instructions.
- Do NOT use permethrin products directly on skin.
*In some places, such as Puerto Rico, where permethrin products have been used for years in mosquito control efforts, mosquitoes have become resistant to it. In areas with high levels of resistance, use of permethrin is not likely to be effective.
Take steps to control mosquitoes inside and outside your home
- Use screens on windows and doors. Repair holes in screens to keep mosquitoes outside.
- Use air conditioning when available.
- Sleep under a mosquito bed net if air conditioned or screened rooms are not available or if sleeping outdoors.
- Once a week, empty and scrub, turn over, cover, or throw out items that hold water, such as tires, buckets, planters, toys, pools, birdbaths, flowerpots, or trash containers. Check inside and outside your home. Mosquitoes lay eggs near water.
Figure 5. Eastern equine encephalitis virus prevention
Eastern equine encephalitis vaccine
No human vaccine against eastern equine encephalitis virus infection or specific antiviral treatment for clinical eastern equine encephalitis virus infections is available. Patients with suspected eastern equine encephalitis should be evaluated by a healthcare provider, appropriate serologic and other diagnostic tests ordered, and supportive treatment provided.
Eastern equine encephalitis symptoms
The incubation period for Eastern equine encephalitis virus disease (the time from infected mosquito bite to onset of illness) ranges from 4 to 10 days. Eastern equine encephalitis virus infection can result in one of two types of illness, systemic or encephalitic (involving swelling of the brain, referred to below as eastern equine encephalitis). The type of illness will depend on the age of the person and other host factors. It is possible that some people who become infected with eastern equine encephalitis virus may be asymptomatic (will not develop any symptoms).
Systemic infection has an abrupt onset and is characterized by chills, fever, malaise, arthralgia, and myalgia. The illness lasts 1 to 2 weeks, and recovery is complete when there is no central nervous system involvement. In infants, the encephalitic form is characterized by abrupt onset; in older children and adults, encephalitis is manifested after a few days of systemic illness. Signs and symptoms in encephalitic patients are fever, headache, irritability, restlessness, drowsiness, anorexia, vomiting, diarrhea, cyanosis, convulsions, and coma.
Approximately a third of all people with eastern equine encephalitis die from the disease. Death usually occurs 2 to 10 days after onset of symptoms but can occur much later. Of those who recover, many are left with disabling and progressive mental and physical sequelae, which include can range from minimal brain dysfunction to severe intellectual impairment, personality disorders, seizures, paralysis, and cranial nerve dysfunction. Many patients with severe sequelae die within a few years.
Eastern equine encephalitis diagnosis
Eastern equine encephalitis diagnosis is based on tests of blood or spinal fluid. These tests typically look for antibodies that the body makes against the viral infection.
Cerebrospinal fluid (CSF) findings include neutrophil-predominant pleocytosis and elevated protein levels; glucose levels are normal. Brain lesions are typical of encephalomyelitis and include neuronal destruction and vasculitis, which is perivascular and parenchymous at the cortex, midbrain, and brain stem. There is minimal involvement of the spinal cord.
Eastern equine encephalitis virus is difficult to isolate from clinical samples; almost all isolates (and positive PCR results) have come from brain tissue or CSF. Serologic testing remains the primary method for diagnosing eastern equine encephalitis virus infection. Combined with a consistent clinical presentation in an endemic area, a rapid and accurate diagnosis of acute neuroinvasive eastern equine encephalitis virus disease can be made by the detection of eastern equine encephalitis virus-specific IgM antibody in serum or CSF. Eastern equine encephalitis virus IgM tests are available commercially, in some state health department laboratories, and at CDC. A positive eastern equine encephalitis virus IgM test result should be confirmed by neutralizing antibody testing of acute- and convalescent-phase serum specimens at a state public health laboratory or CDC.
All eastern equine encephalitis virus disease cases should be reported to local public health authorities. Reporting can assist local, state and national authorities to recognize outbreaks of this rare disease and to institute control measures to limit future infections.
Eastern equine encephalitis treatment
There is no specific treatment for eastern equine encephalitis. Antibiotics are not effective against viruses, and no effective anti-viral drugs have been discovered. Severe illnesses are treated by supportive therapy which may include hospitalization, respiratory support, IV fluids, and prevention of other infections.
References [ + ]