Contents
What is ectodermal dysplasia
Ectodermal dysplasia is a large group (180+) of inherited disorders characterized by a primary defect in hair, teeth, nails or sweat gland function, in addition to another abnormality in a tissue of ectodermal origin, e.g. ears, eyes, lips, mucous membranes of the mouth or nose, central nervous system 1).
The term ectoderm refers to some of the earliest cells found in a baby. Very early in development a baby, at this stage the embryo, consists of 3 types of cell – endoderm, mesoderm and ectoderm. The cells of the ectoderm is the outermost layer of cells in embryonic development and contributes to the formation of teeth, hair, nails and sweat glands as well as a few other types of cells. The term dysplasia means a change from the usual pattern of growth. Therefore, the term Ectodermal Dysplasia is a descriptive term meaning the ectoderm of certain areas fails to develop normally in an individual. All ectodermal dysplasias are present from birth and are non-progressive.
A predisposition to respiratory infections, due to a somewhat depressed immune system and to defective mucous glands in parts of the respiratory tract, is the most life threatening characteristic of this group of disorders.
Prenatal testing is available for ectodarmal dysplasia syndromes in some centers.
Unfortunately, there is no cure for ectodermal dysplasia. Instead, the goal is to successfully manage the symptoms so that the individual can lead a healthy life and have a good quality of life.
Because the symptoms vary depending on the type of ectodermal dysplasia, the treatment plan will vary with each person too. Some people will experience mild symptoms that need minor treatment while others will have extensive health issues that need complex care.
You may also want to contact ectodermal dysplasia support organizations for more information:
- National Foundation for Ectodermal Dysplasias: https://www.nfed.org/
- Ectodermal Dysplasia Society: https://edsociety.co.uk
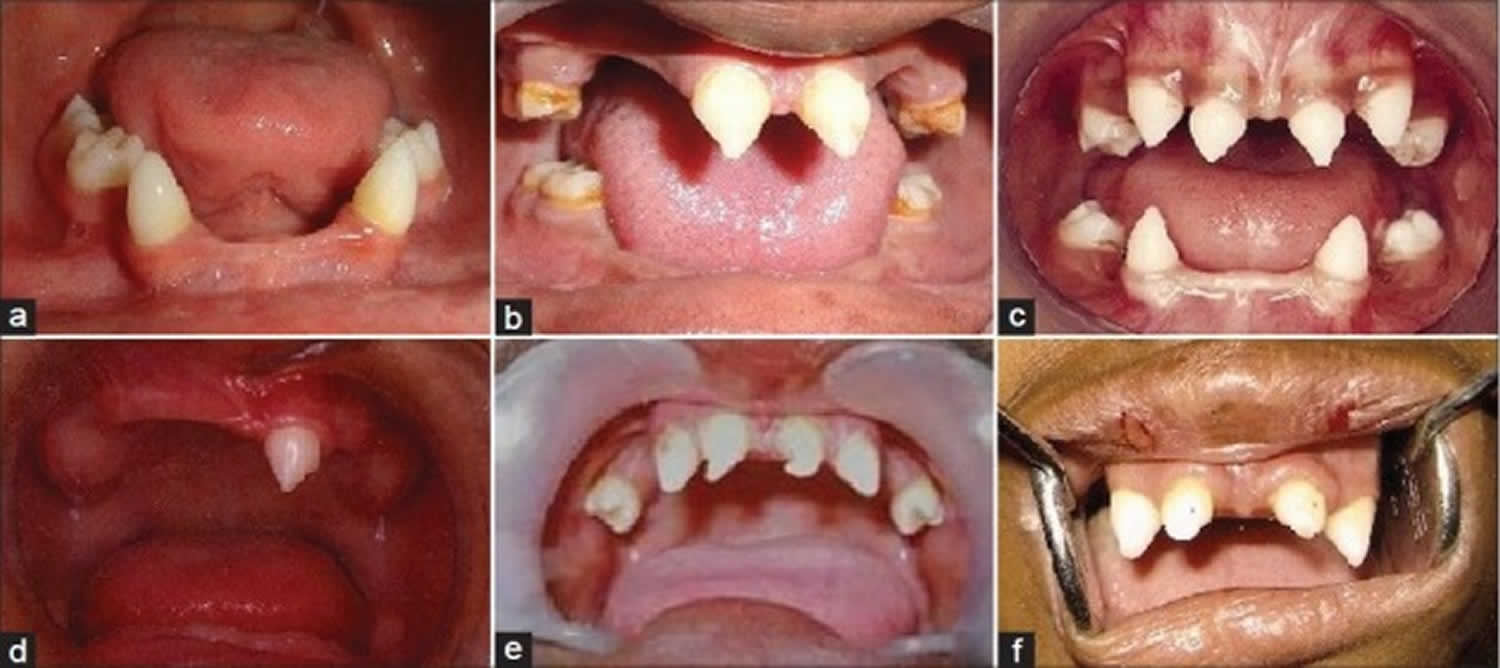
Figure 1. Ectodermal dysplasia teeth
Ectodermal dysplasia life expectancy
Hypohidrotic ectodermal dysplasia (anhidrotic ectodermal dysplasia) does not affect life expectancy, intelligence and your ability to lead a normal life.
Ectodermal dysplasia types
Currently there are over 180 different types of ectodermal dysplasias. The 180+ ectodermal dysplasias are recognized and named based on the specific combination of symptoms shown in affected individuals. The pattern of these features is important when a physician tries to make a formal diagnosis.
In some types, teeth may be missing and nails may be defective, while in another type there may be missing teeth, inability to sweat, and sparse hair. Still another may have hearing loss and defects of the enamel of the teeth. Each combination of abnormalities may be a distinct ectodermal dysplasia and will have a unique name.
These syndromes represent the largest groups of people who are registered with National Foundation for Ectodermal Dysplasias with that type.
- Ankyloblepharon-Ectodermal Defects-Cleft Lip and/or Palate (AEC) Syndrome
- Clouston Syndrome
- Ectrodactyly-Ectodermal Dysplasia-Clefting (EEC) Syndrome
- Fried Syndrome
- Goltz Syndrome
- Hypohidrotic Ectodermal Dysplasia (HED)
- Oculodentodigital Dysplasia (ODD)
- Tricho-Dento-Osseous (TDO) Syndrome
- Trichorhinophalangael (TRP) Syndrome, Type 1
- Trichorhinophalangael (TRP) Syndrome, Type 2
- Witkop Syndrome
Ectodermal Dysplasia – Type Unknown
It is possible that a person could have a combination of symptoms that is unique to them and has not yet been described in the medical literature. Or, the person is just told they are affected by ectodermal dysplasia. The doctor might not know enough about the different types to give a specific diagnosis. Or, the person was diagnosed at a time when doctors didn’t know as much about a particular type.
What is an unknown diagnosis?
There are hundreds of types of ectodermal dysplasias that have been identified and specifically named. Even still, some individuals may not receive a diagnosis of a specific type of ectodermal dysplasia.
A diagnosis can be unknown for many reasons. A few common reasons are below:
- The collection of symptoms a person is experiencing does not fit into a classic description of one ectodermal dysplasia syndrome.
- The person has not had genetic testing yet and their symptoms could fit more than one ectodermal dysplasia condition.
- Genetic testing has been done, but did not result in a diagnosis. Instead, results may have been negative (no mutations in the known genes tested causing ectodermal dysplasia) or uncertain (the gene showed a variant – or difference – but it is not known if this difference causesectodermal dysplasia or is just part of typical variation among our genes and has no effect.)
Other ectodermal dysplasia types
- Ackerman Syndrome
- Acrorenal Field Defect, Ectodermal Dysplasia, and Lipoatrophic Diabetes
- Acto-Dermato-Ungual-Lacrimal-Tooth Syndrome
- Ameloonychohypohidrotic Syndrome
- Ankyloblepharon-Ectodermal Defects-Cleft Lip/Palate (AEC)
- Anonychia with Flexural Pigmentation
- Anonychia-Onychodystrophy with Brachydactyly Type B and Ectrodactyly
- Arthrogryposis and Ectodermal Dysplasia
- Basan Syndrome
- Blepharocheilodontic Syndrome
- Book (Dysplasia) Syndrome
- Brachymetapody-Anodontia-Hypotrichosis-Albinoidism
- Cahmr Syndrome
- Cardiofaciocutaneous Syndrome
- Cartilage-Hair Hypoplasia
- Chands
- Cleft Lip/Palate-Ectodermal Dysplasia Syndrome
- Clouston Syndrome
- Coffin-Siris Syndrome
- Cooks Syndrome
- Corneodermatoosseous Syndrome
- Cranioectodermal Dysplasia 1
- Deafness with Anhidrotic Ectodermal Dysplasia
- Deafness, Conductive, with Ptosis and Skeletal Anomalies
- Deafness, Congenital, and Onychodystrophy, Autosomal Dominant
- Deafness, Onychodstrophy, Osteodystrophy, Mental Retardation, and Seizures Syndrome
- Dermatoosteolysis, Kirghizian Type
- Dermoodontodysplasia
- Dubowitz Syndrome
- Dyskeratosis Congenita
- Dyskeratosis Congenita, Autosomal Dominant, 1
- Dyskeratosis Congenita, Autosomal Recessive, 1
- Ectodermal Dysplasia 4, Hair/Nail Type
- Ectodermal Dysplasia and Neurosensory Deafness
- Ectodermal Dysplasia Syndrome with Distinctive Facial Appearances and Preaxial Polydactyly of Feet
- Ectodermal Dysplasia with Adrenal Cyst
- Ectodermal Dysplasia with Mental Retardation and Syndactyly
- Ectodermal Dysplasia with Natal Teeth, Turnpenny Type
- Ectodermal Dysplasia, Anhidrotic, With Immunodeficiency, Osteopetrosis, and Lymphedema
- Ectodermal Dysplasia, Ectrodactyly, and Macular Dystrophy Syndrome
- Ectodermal Dysplasia, Hidrotic, Christianson-Fourie Type
- Ectodermal Dysplasia, Trichoodontoonychial Type
- Ectodermal Dysplasia/Skin Fragility Syndrome
- Ectrodactyly and Ectodermal Dysplasia without Cleft Lip/Palate
- Ectrodactyly, Ectodermal Dysplasia, and Cleft Lip/Palate (EEC) Syndrome 1
- Focal Dermal Hypoplasia / Goltz Syndrome
- Focal Facial Dermal Dysplasia 1, Brauer Type
- Focal Facial Dermal Dysplasia 2, Brauer-Setleis Type
- Focal Facial Dermal Dysplasia 3
- Gapo Syndrome
- Gorlin-Chaudhry-Moss Syndrome
- Hallermann-Streiff Syndrome
- Hearing Loss, Sensorineural, With Enamel Hypoplasia and Nail Defects
- Hypertrichosis, Congenital Generalized, With or Without Gingival Hyperplasia
- Hypohidrotic Ectodermal Dysplasia with Hypothyroidism and Agenesis of the Corpus Callosum
- Hypohidrotic Ectodermal Dysplasia, Autosomal Dominant
- Hypohidrotic Ectodermal Dysplasia, Autosomal Recessive
- Hypohidrotic Ectodermal Dysplasia, With Hypothyroidism and Ciliary Dyskinesia
- Hypohidrotic Ectodermal Dysplasia, With Immune Deficiency
- Hypohidrotic Ectodermal Dysplasia, X-Linked
- Hypotrichosis, Congenital, With Juvenile Macular Dystrophy
- Hypotrichosis-Osteolysis-Periodontitis-Palmoplantar Keratoderma Syndrome
- IFAP Syndrome With or Without Bresheck Syndrome
- Incontinentia Pigmenti
- Johanson-Blizzard Syndrome
- Johnson Neuroectodermal Syndrome
- Keratitis-Ichthyosis-Deafness Syndrome, Autosomal Dominant
- Kohlschutter-Tonz Syndrome
- Leukomelanoderma, Infantilism, Mental Retardation, Hypodontia, Hypotrichosis
- Limb-Mammary Syndrome
- Marshall Syndrome
- Mohr Syndrome
- Monilethrix
- Mucoepithelial Hysplasia, Hereditary
- Naegeli Syndrome
- Oculodentodigital Dysplasia
- Oculotrichodysplasia
- Odonoonychodermal Dysplasia
- Ondontomicronychial Dysplasia
- Onychotrichodysplasia and Neutropenia
- Orofaciodigital Syndrome I
- Pachyonychia Congenita 1
- Pachyonychia Congenita 2
- Palmoplantar Keratoderma and Congenital Alopecia 2
- Palmoplantar Keratoderma and Congenital Alopecia, Autosomal Dominant
- Papillon-Lefevre Syndrome
- Pili Torti and Developmental Delay
- Pilodental Dysplasia with Refractive Errors
- Poikiloderma with Neutropenia
- Polyposis, Skin Pigmentation, Alopecia, and Fingernail Changes
- Rapp-Hodgkin Syndrome
- Rosselli-Gulienetti Syndrome
- Rothmund-Thomson Syndrome
- Sabinas Brittle Hair Syndrome
- Saethre-Chotzen Syndrome
- Scalp-Ear-Nipple Syndrome
- Schinzel-Giedion Midface Retraction Syndrome
- Schopf-Schulz-Passarge Syndrome
- Sener Syndrome
- Short-Limb Skeletal Dysplasia with Severe Combined Immunodeficiency
- Teeth, Congenital Absence of, with Taurodontia and Sparse Hair
- Tetramelic Deficiencies, Ectodermal Dysplasia, Deformed Ears, and Other Abnormalities
- Thumb Deformity and Alopecia
- Trichodental Dysplasia
- Trichodentoosseous Syndrome
- Trichoodontoonychial Dysplasia with Bone Deficiency
- Trichorhinophalangeal Syndrome, Type I
- Trichorhinophalangeal Syndrome, Type II
- Trichorhinophalangeal Syndrome, Type III
- Trichothiodystrophy 1, Photosensitive
- Trichothiodystrophy 2, Photosensitive
- Trichothiodystrophy 3, Photosensitive
- Trichothiodystrophy 4, Nonphotosensitive
- Trichothiodystrophy 5, Nonphotosensitive
- Ulnar-Mammary Syndrome
- Uncombable Hair, Retinal Pigmentary Dystrophy, Dental Anomalies, and Brachydactyly
- Weyers Acrofacial Dysostosis
- Witkop Syndrome
- Woolly Hair, Hypotrichosis, Everted Lower Lip, and Outstanding Ears
Hypohidrotic ectodermal dysplasia
Hypohidrotic ectodermal dysplasia (anhidrotic ectodermal dysplasia) is one of about 180 types of ectodermal dysplasia in humans 2). Before birth, these disorders result in the abnormal development of structures including the skin, hair, nails, teeth, and sweat glands.
Hypohidrotic ectodermal dysplasia is the most common form of ectodermal dysplasia in humans. It is estimated to affect at least 1 in 17,000 people worldwide 3).
Most people with anhidrotic ectodermal dysplasia have a reduced ability to sweat (hypohidrosis) because they have fewer sweat glands than normal or their sweat glands do not function properly 4). Sweating is a major way that the body controls its temperature; as sweat evaporates from the skin, it cools the body. An inability to sweat can lead to a dangerously high body temperature (hyperthermia), particularly in hot weather. In some cases, hyperthermia can cause life-threatening medical problems.
Affected individuals tend to have sparse scalp and body hair (hypotrichosis). The hair is often light-colored, brittle, and slow-growing. This condition is also characterized by absent teeth (hypodontia) or teeth that are malformed. The teeth that are present are frequently small and pointed.
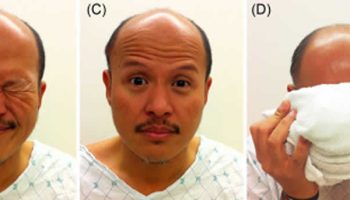
Hypohidrotic ectodermal dysplasia is associated with distinctive facial features including a prominent forehead, thick lips, and a flattened bridge of the nose. Additional features of this condition include thin, wrinkled, and dark-colored skin around the eyes; chronic skin problems such as eczema; and a bad-smelling discharge from the nose (ozena).
Hypohidrotic ectodermal dysplasia causes
Mutations in the EDA, EDAR, and EDARADD genes cause hypohidrotic ectodermal dysplasia 5).
The EDA, EDAR, and EDARADD genes provide instructions for making proteins that work together during embryonic development. These proteins form part of a signaling pathway that is critical for the interaction between two cell layers, the ectoderm and the mesoderm. In the early embryo, these cell layers form the basis for many of the body’s organs and tissues. Ectoderm-mesoderm interactions are essential for the formation of several structures that arise from the ectoderm, including the skin, hair, nails, teeth, and sweat glands.
Mutations in the EDA, EDAR, or EDARADD gene prevent normal interactions between the ectoderm and the mesoderm and impair the normal development of hair, sweat glands, and teeth. The improper formation of these ectodermal structures leads to the characteristic features of hypohidrotic ectodermal dysplasia.
Inheritance pattern
Hypohidrotic ectodermal dysplasia may be inherited in one of three patterns:
- X-linked recessive, ninety-five percent of randomly selected individuals with hypohidrotic ectodermal dysplasia have the X-linked recessive form.
- Autosomal recessive,
- Autosomal dominant.
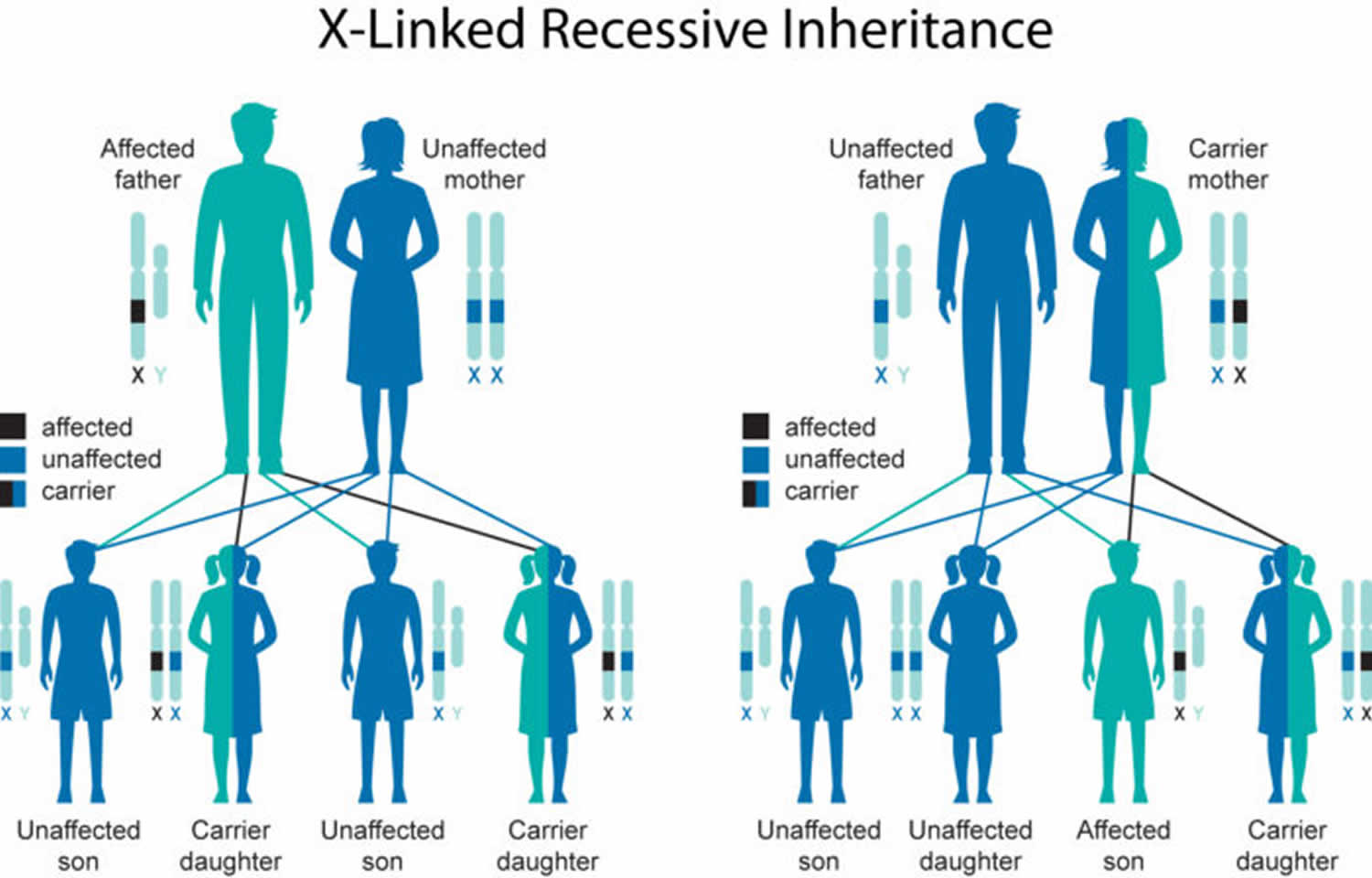
Hypohidrotic ectodermal dysplasia has several different inheritance patterns. Most cases are caused by mutations in the EDA gene, which are inherited in an X-linked recessive pattern. A condition is considered X-linked if the mutated gene that causes the disorder is located on the X chromosome, one of the two sex chromosomes. In males (who have only one X chromosome), one altered copy of the gene in each cell is sufficient to cause the condition. In females (who have two X chromosomes), a mutation must be present in both copies of the gene to cause the disorder. Males are affected by X-linked recessive disorders much more frequently than females. A characteristic of X-linked inheritance is that fathers with X-linked disorders can transmit the gene to all their daughters, who are carriers, but never to their sons (because the sons inherit the Y chromosome from their father).
In X-linked recessive inheritance, a female with one altered copy of the gene in each cell is called a carrier. In about 70 percent of cases, carriers of hypohidrotic ectodermal dysplasia experience some features of the condition. These signs and symptoms are usually mild and include a few missing or abnormal teeth, sparse hair, and some problems with sweat gland function. Some carriers, however, have more severe features of this disorder.
If a woman is a carrier of an X-linked ectodermal dysplasia, there is a 50% chance that each son will be affected and a 50% chance that each daughter will be a carrier, like the mother.
Figure 2. Hypohidrotic ectodermal dysplasia X-linked recessive inheritance pattern
The remaining 5% have either the autosomal recessive or autosomal dominant form of hypohidrotic ectodermal dysplasia. Less commonly, hypohidrotic ectodermal dysplasia results from mutations in the EDAR or EDARADD gene. EDAR mutations can have an autosomal dominant or autosomal recessive pattern of inheritance, and EDARADD mutations have an autosomal recessive pattern of inheritance. Autosomal dominant inheritance means one copy of the altered gene in each cell is sufficient to cause the disorder. Autosomal recessive inheritance means two copies of the gene in each cell are altered. Most often, the parents of an individual with an autosomal recessive disorder are carriers of one copy of the altered gene but do not show signs and symptoms of the disorder.
Ectodermal dysplasia signs and symptoms
The signs and symptoms of ectodermal dysplasia differ markedly between the different types of the condition and depend on the structures that are affected. Signs and symptoms are not usually apparent in newborns and may not be picked up till infancy or childhood.
Ectodermal dysplasia typically affects the four organs primarily involved in the following ways:
- Hair
- Scalp and body hair may be thin, sparse, and light in color
- Hair may be coarse, excessively brittle, curly or even twisted
- Nails
- Fingernails and toenails may be thick, abnormally shaped, discoloured, ridged, slow growing, or brittle
- Sometimes nails may be absent
- Cuticles may be prone to infection
- Teeth
- Abnormal tooth development resulting in missing teeth or growth of teeth that are peg-shaped or pointed
- Tooth enamel is also defective
- Dental treatment is necessary and children as young as 2 years may need dentures
- Sweat glands
- Eccrine sweat glands may be absent or sparse so that sweat glands function abnormally or not at all
- Without normal sweat production, the body cannot regulate temperature properly
- Children may experience recurrent high fever that may lead to seizures and neurological problems
- Overheating is a common problem, particularly in warmer climates
Other signs and symptoms include:
- Lightly pigmented skin, in some cases red or brown pigment may be present. Skin can be thick over the palms and soles and is prone to cracking, bleeding and infection.
- Skin may be dry and is prone to rashes and infection.
- Dry eyes occur due to lack of tears. Cataracts and visual defects may also occur.
- Abnormal ear development may cause hearing problems.
- Cleft palate/lip.
- Missing fingers or toes (digits).
- Respiratory infections due to lack of normal protective secretions of the mouth and nose.
- Noses may have a thick mucus secretion (“nasal rocks”) or foul smelling nasal discharge from chronic nasal infections.
- Throats may have sparse saliva, causing problems with tasting, lubricating, chewing and swallowing foods.
- Lack of breast development and infertility.
- Allergies and immunodeficiencies, such as increased frequencies of asthma, allergies, eczema or rhinitis symptoms
- Gastrointestinal issues, such as constipation
- Growth issues, such as small stature, prominent forehead, saddle nose, decreased breast development in females, and height and weight deficits beginning at an early age and persisting throughout adolescence
What causes ectodermal dysplasia
Ectodermal dysplasias are a group of approximately 180 related diseases that result from faulty development of the ectodermal germ cell layer during embryogenesis. Because of the phenomenon of induction, derivatives of other cell layers may be affected. The exact genetic and biochemical defects are unknown, and are thought to vary from one form of the disorder to another.
The various syndromes have different inheritance patterns. Anhidrotic (hypohidrotic) ectodermal dysplasia, for example, usually involves an X-linked recessive inheritance, with partial manifestation in females. However, it may also be transmitted as an autosomal dominant or recessive trait. X-linked recessive disorders are conditions that are coded on the X chromosome. Females have two X chromosomes, but males have one X chromosome and one Y chromosome. Therefore, in females, disease traits on the X chromosome can be masked by the normal gene on the other X chromosome. Since males only have one X chromosome, if they inherit a gene for a disease present on the X, it will be expressed. Men with X-linked disorders transmit the gene to all their daughters, who are carriers, but never to their sons. Women who are carriers of an X-linked disorder have a 50 percent risk of transmitting the carrier condition to their daughters, and a 50 percent risk of transmitting the disease to their sons. Syndromes with this pattern tend to be more severe.
The Rapp-Hodgkin Syndrome, by comparison, is an autosomal dominant disorder. In dominant disorders, a single copy of the disease gene (received from either the mother or father) will be expressed “dominating” the other normal gene and resulting in the appearance of the disease. The risk of transmitting the disorder from affected parent to offspring is 50 percent for each pregnancy regardless of the sex of the resulting child.
The gene for one form of ectodermal dysplasia known as Hypohidrotic Ectodermal Dysplasia (HED) has been located. Researchers plan to study the function of the gene and investigate the role of the proteins that are encoded by the H.E.D. gene. This gene identification will lead to a test for carrier status.
Ectodermal dysplasia diagnosis
Most forms of ectodermal dysplasia are diagnosed clinically. Some cases of ectodermal dysplasia is apparent at birth. In other cases, a parent or doctor may only begin to suspect that a problem exists later on when, for example, the baby’s teeth fail to develop normally. Because missing teeth is one of the cardinal features of many of the syndromes, it is often the dentist who makes the diagnosis and referrals.
Doctors usually assess all the ectodermal structures and then try to match the collection of abnormalities to those previously identified in other individuals. Sometimes this is very difficult and a precise diagnosis is not always possible.
For the subtypes of ectodermal dysplasia in which the abnormal gene is known, it is possible to screen DNA to find the specific gene mutation in an affected individual. This usually involves providing a blood sample from a vein in the arm taken from the affected child and both parents. From the blood cells, DNA can be isolated and then screened for mutations.
DNA testing for ectodermal dysplasias is not available in most hospitals. Screening is carried out in a relatively small number of diagnostic or research laboratories and doctors or genetic counselors often have to screen the internet to track down where the necessary screening can be done.
Prenatal testing is possible for some forms of ectodermal dysplasia although this needs to be discussed very carefully with genetic counselors. If the specific gene mutation(s) is/are known then it is usually possibly to have a DNA-based test at about 11 weeks’ into the pregnancy. Results usually take 2-4 days to come back. If the genetic abnormality is not known then a very few other forms of ectodermal dysplasia can be tested for prenatally (e.g. using ultrasound) but this is relevant to only a minority of families.
Clinical Diagnosis
A physician or dentist can make a clinical diagnosis of ectodermal dysplasia. This is based on the medical signs a person displays in a physical examination along with the symptoms they report. The doctor will then try to sort out which of the ectodermal derivatives are involved, as ectodermal dysplasias involve more than one. They’ll also look for abnormalities in organs that are not part of the ectodermal derivatives, such as ectrodactyly (malformations of the hand) or short stature.
The physician will also obtain a family history in an attempt to determine an inheritance pattern. The way that the condition is inherited is often an important factor for correct diagnosis.
Genetic Testing
A clinical diagnosis for ectodermal dysplasia is subjective. It’s an educated opinion formed after a doctor examines one or more members of a family. Genetic testing, in many cases, confirms the doctor’s suspicions. Genetic testing searches for changes in your genes that cause medical problems like ectodermal dysplasias.
However, there’s not a universal test that can identify all types of ectodermal dysplasia. Once a doctor suspects a certain type of ectodermal dysplasia, he or she may request a genetic test to confirm the diagnosis. The request is specific, asking the appropriate laboratory to test for a specific gene. If the changed form of the gene is present, the suspicion is confirmed, and diagnosis is certain.
Genes have been found for many of the ectodermal dysplasia but not for all. Genetic testing is now available for 60 types of ectodermal dysplasias. Find out if there’s a genetic test available for your type of ectodermal dysplasia here https://juyhw1n8m4a3a6yng24eww91-wpengine.netdna-ssl.com/wp-content/uploads/2016/06/Ectodermal-Dysplasias-With-Identified-Genes-and-Genetic-Testing.pdf
You may also want to contact ectodermal dysplasia support organizations for more information:
- National Foundation for Ectodermal Dysplasias: https://www.nfed.org/
- Ectodermal Dysplasia Society: https://edsociety.co.uk
Ectodermal dysplasia treatment
There is no specific treatment for ectodermal dysplasia. Management of the condition is by treating the various symptoms. Patients often need to be treated by a team of doctors and dentists, rather than a sole practitioner.
- Patients with abnormal or no sweat gland function should live in cooler climates or in places with air conditioning at home, school and work. Cooling water baths or sprays may be useful in maintaining a normal body temperature.
- Over the counter creams may relieve skin discomfort.
- Artificial tears can be used to prevent damage to the cornea in patients with defective tear production. Saline sprays can also be helpful.
- Saline irrigation of the nasal mucosa may help to remove purulent debris and prevent infection.
- Early dental evaluation and intervention is essential.
- Surgical procedures such as repairing a cleft palate may lessen facial deformities and improve speech.
- Wigs may be worn to improve the appearance of patients with little or no hair.
Most people with ectodermal dysplasia can lead a full and productive life once they understand how to manage their condition. Special attention must be paid to children if sweating and mucous production abnormalities are present. Recurrent high fevers may lead to seizures and neurological problems.
References [ + ]