Contents
What is an ectopic heartbeat
Ectopic heartbeats are early (premature) or extra heartbeats, which can cause you to have palpitations. ‘Ectopic’ means out of place. Ectopic heartbeats happen when cells away from your hearts own natural pacemaker get a little excited (or irritable) and release an electrical signal, causing an ‘extra’ or early heartbeat. There is often a tiny pause after the extra beat, giving you the sensation of a ‘missed’ heartbeat. The term ‘palpitations’ is used to describe the sensation of feeling your own heart beating. Some say this feels like a fluttering in your chest, or your heart pounding. Others describe it as feeling like a thud or movement in your chest, which you can feel in your neck or through your ear when you are lying down. Palpitations can be felt whether your heart is beating normally, quickly, slowly or irregularly.
The two most common types of ectopic heartbeats are:
- Premature Atrial Contraction – an early electrical impulse in the atria, which are the upper chambers of your heart
- Premature Ventricular Contraction – an early electrical impulse in the ventricles, which are the lower chambers of your heart.
Like most causes of palpitations, ectopic heartbeats are usually harmless and do not mean you have a serious heart condition, though exceptions exist. They generally require no treatment unless they occur very often or are very severe.
Ectopic heartbeats are rare in children without heart disease that was present at birth (congenital). Most extra heartbeats in children are premature atrial contractions. These are almost always harmless.
In adults, ectopic heartbeats are common. They are most often due to premature atrial contractions or premature ventricular contractions. Your health care provider should look into the cause when they are frequent. Most of the time no treatment is needed.
The reason premature atrial contractions or premature ventricular contractions can sometimes be felt as a skipped beat, is that the heart gets a premature signal to squeeze before it has had time to fill with blood. The resulting heart contraction does not produce blood flow to the body. A pause is felt, and the following heart beat is more forceful than usual. If the premature atrial contraction or premature ventricular contraction is less premature, and the heart has had time to fill with blood before receiving the early signal to squeeze, an extra beat will be felt rather than a skipped beat.
Premature heartbeats are common in healthy people of all ages. Caffeine, alcohol, stress, and fatigue may cause premature atrial contractions or premature ventricular contractions to occur more frequently. If the symptoms caused by ectopic heartbeats are bothersome, they can be treated with medications or catheter ablation.
The following may help reduce ectopic heartbeats for some people:
- Limiting caffeine, alcohol, and tobacco
- Regular exercise for people who are inactive
Most ectopic heartbeats DO NOT need to be treated. The condition is only treated if your symptoms are severe or if the extra beats occur very often.
The cause of the heartbeats, if it can be found, may also need to be treated.
Ectopic heartbeat outlook (prognosis)
In some cases, ectopic heartbeats may mean you are at greater risk for serious abnormal heart rhythms, such as ventricular tachycardia.
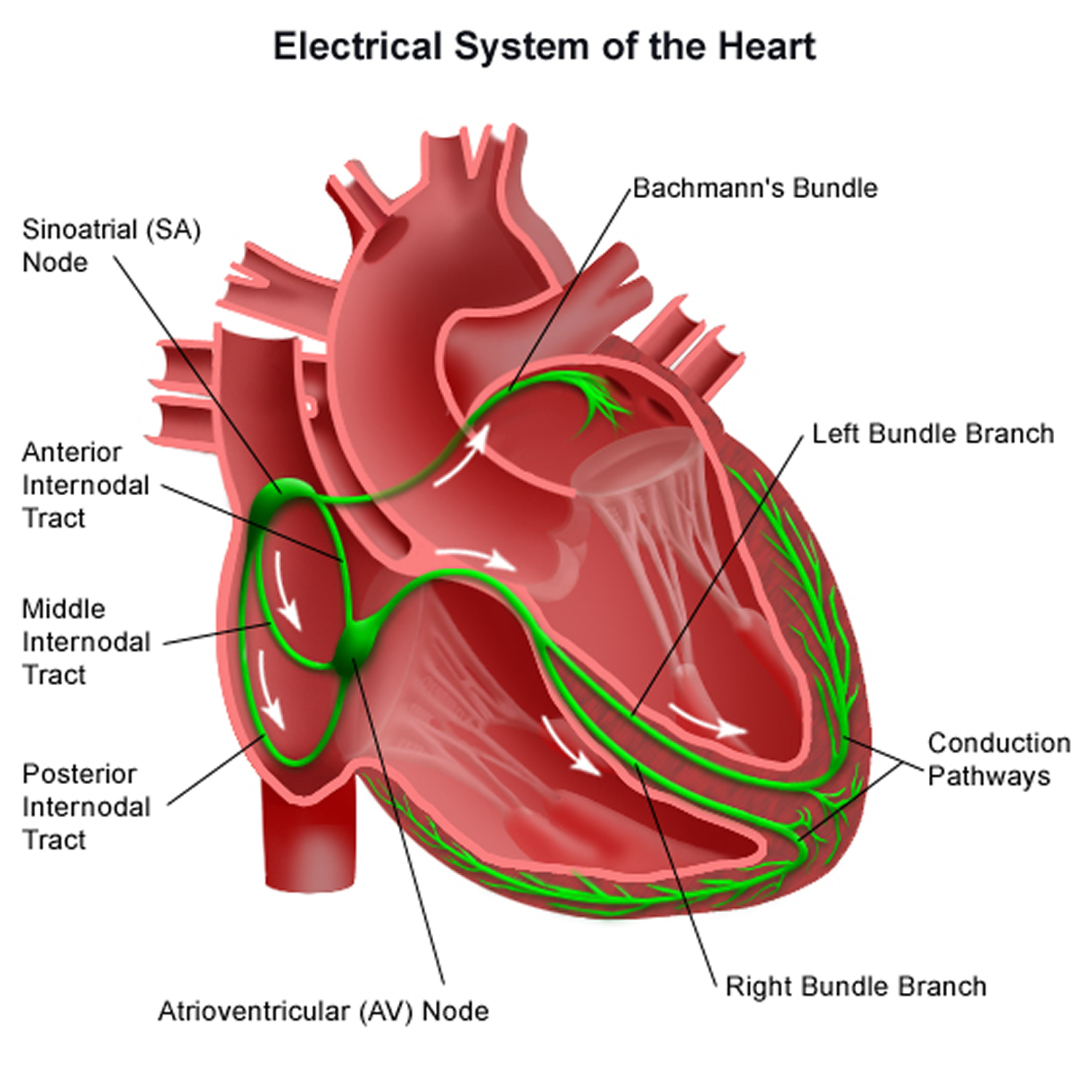
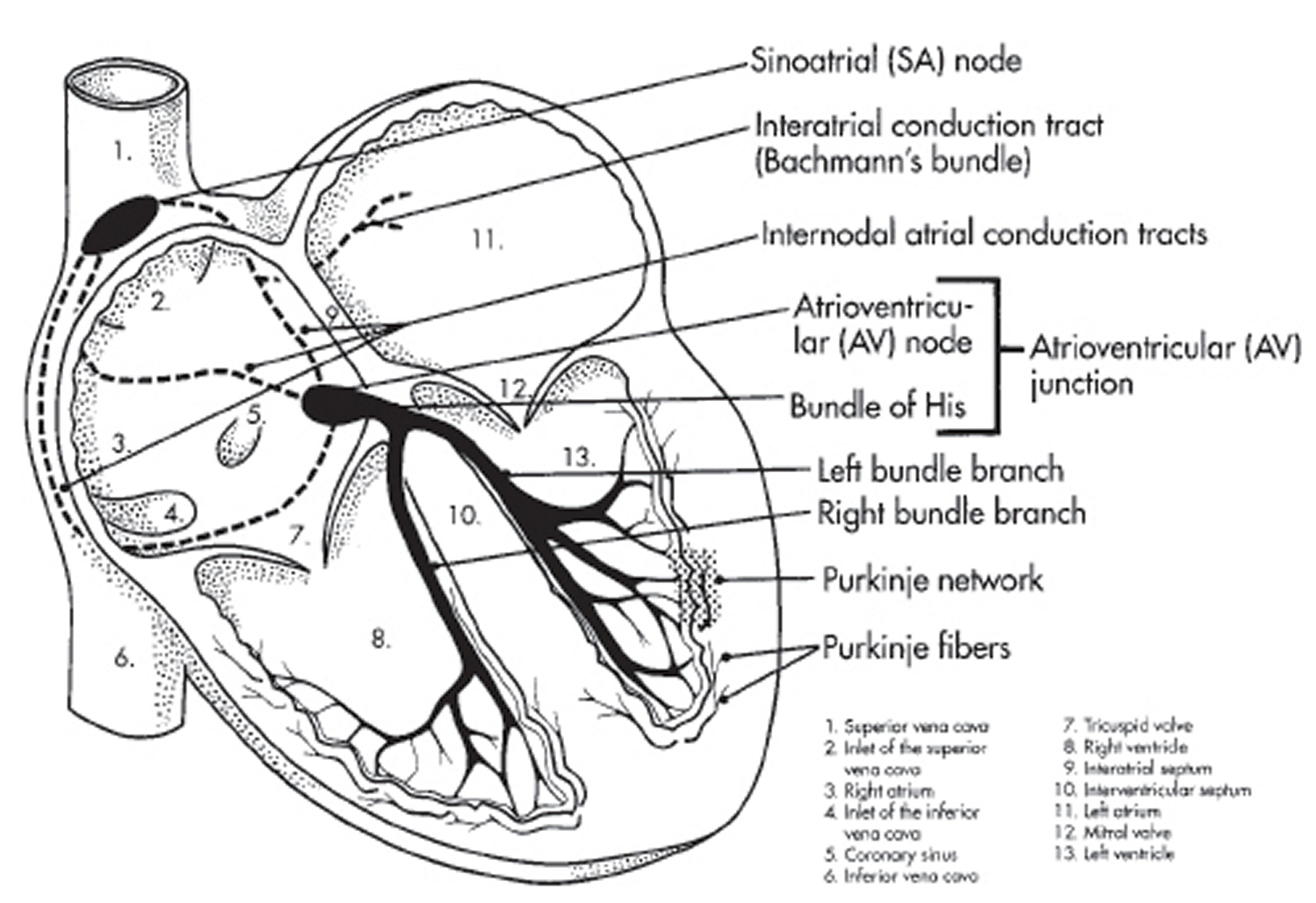
The heart’s electrical system
To understand the causes of heart rate or rhythm problems such as ectopic heartbeats, it helps to understand how the heart’s internal electrical system works.
Your heart is made up of four chambers — two upper chambers (atria) and two lower chambers (ventricles). The rhythm of your heart is normally controlled by a natural pacemaker called the sinoatrial (SA) node — or sinus node — an area of specialized cells in the right atrium. The sinoatrial (SA) node produces electrical impulses that normally start each heartbeat. This natural pacemaker produces the electrical impulses that trigger the normal heartbeat. From the sinus node, electrical impulses travel across the atria to the ventricles, causing them to contract and pump blood to your lungs and body.
From the sinus node, electrical impulses travel across the atria, causing the atrial muscles to contract and pump blood into the ventricles.
The electrical impulses then arrive at a cluster of cells called the atrioventricular (AV) node — usually the only pathway for signals to travel from the atria to the ventricles.
The atrioventricular (AV) node slows down the electrical signal before sending it to the ventricles. This slight delay allows the ventricles to fill with blood. When electrical impulses reach the muscles of the ventricles, they contract, causing them to pump blood either to the lungs or to the rest of the body.
When anything disrupts this complex system, it can cause the heart to beat too fast (tachycardia), too slow (bradycardia) or with an irregular rhythm.
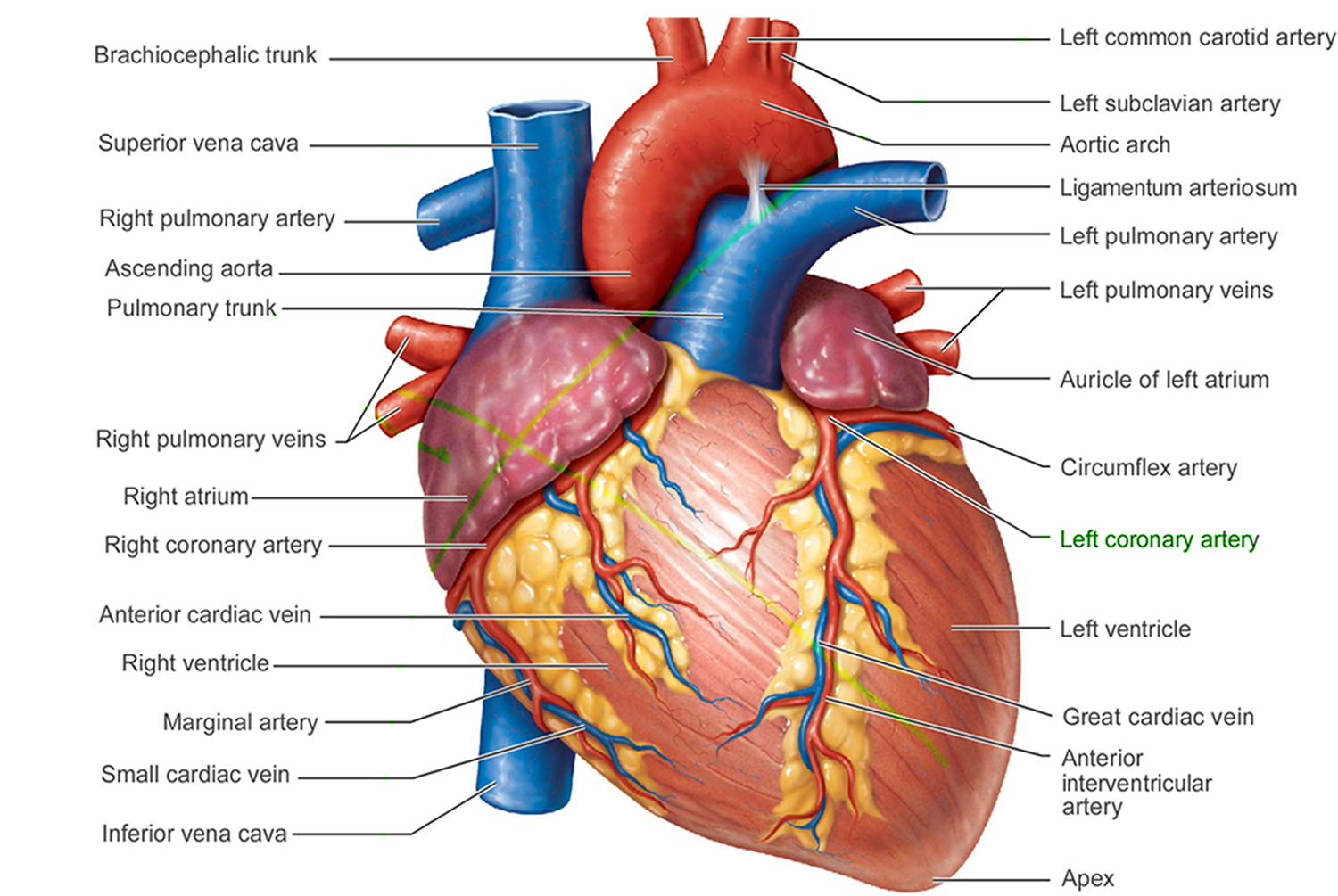
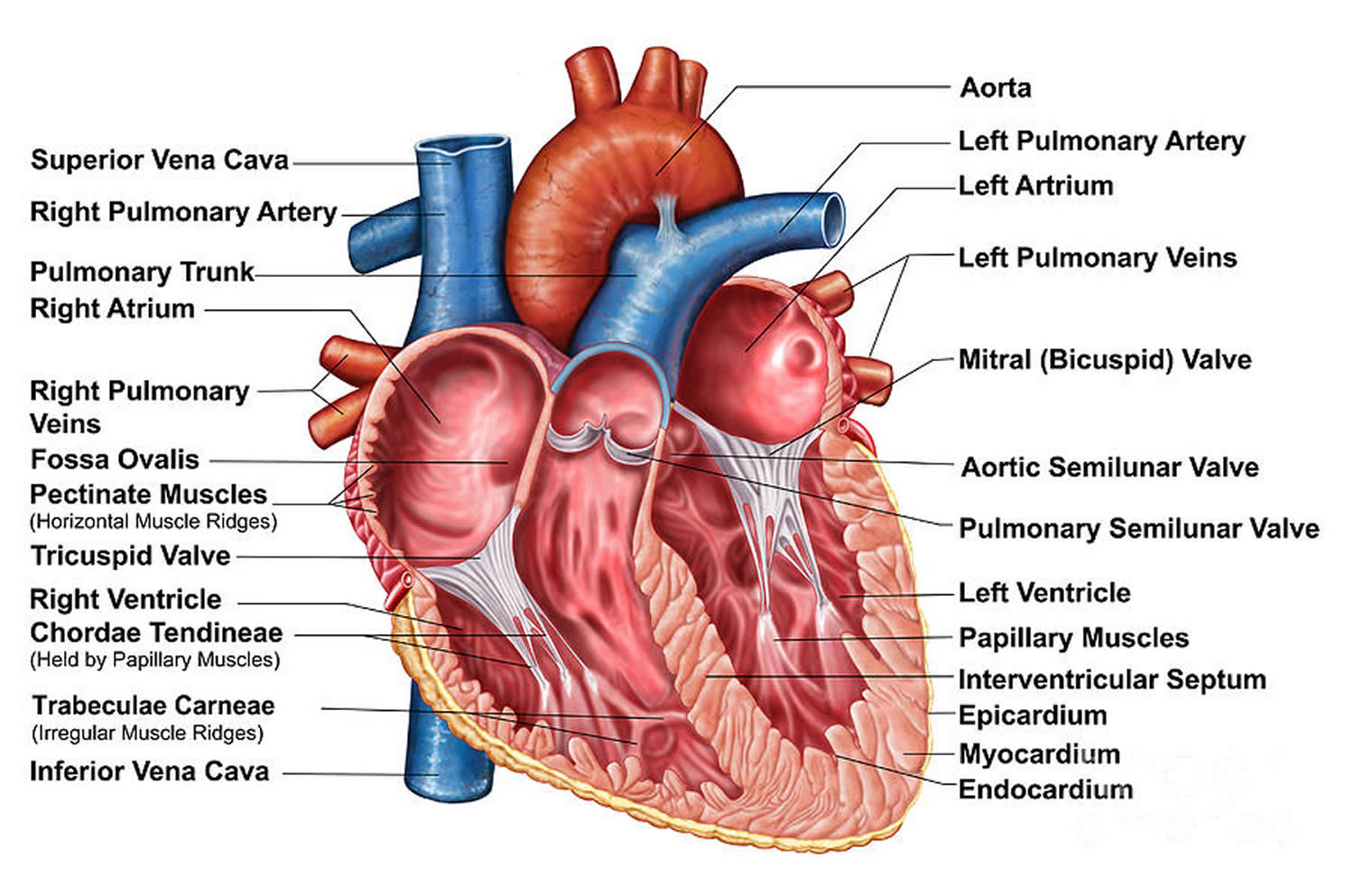
Figure 1. The anatomy of the heart
Premature Atrial Contraction
Premature atrial contractions (premature atrial contractions), also known as atrial premature complexes or atrial premature beats, are a common cardiac dysrhythmia characterized by premature heartbeats originating in the atria. While the sinoatrial node typically regulates the heartbeat during normal sinus rhythm, premature atrial contractions occur when another region of the atria depolarizes before the sinoatrial node and thus triggers a premature heartbeat. The exact cause of premature atrial contractions is unclear; while several predisposing conditions exist, premature atrial contractions commonly occur in healthy young and elderly people without heart disease, and by themselves are not considered an abnormal finding. premature atrial contractions found in healthy young are more likely to lead to other heart conditions or even death. Elderly people that get premature atrial contractions usually don’t need any further attention besides follow ups due to unclear evidence. premature atrial contractions are often completely asymptomatic and may be noted only with Holter monitoring, but occasionally they can be perceived as a skipped beat or a jolt in the chest. In most cases, no treatment other than reassurance is needed for premature atrial contractions, although medications such as beta blockers can reduce the frequency of symptomatic premature atrial contractions.
On an electrocardiogram (ECG), premature atrial contractions are characterized by an abnormally shaped P wave. Since the premature beat initiates outside the sinoatrial node, the associated P wave appears different from those seen in normal sinus rhythm. Typically, the atrial impulse propagates normally through the atrioventricular node and into the cardiac ventricles, resulting in a normal, narrow QRS complex. However, if the atrial beat is premature enough, it may reach the atrioventricular node during its refractory period, in which case it will not be conducted to the ventricle and there will be no QRS complex following the P wave.
Figure 4. Premature atrial contraction ECG
Premature Ventricular Contraction
Premature ventricular contractions are extra heartbeats that is initiated by Purkinje fibers in the ventricles rather than by the sinoatrial node, the normal heartbeat initiator. These extra beats disrupt your regular heart rhythm, sometimes causing you to feel a fluttering or a skipped beat in your chest. The electrical events of the heart detected by the electrocardiogram (ECG) allow a premature ventricular contraction to be easily distinguished from a normal heart beat. Although a premature ventricular contraction can be a sign of decreased oxygenation to the heart muscle, often premature ventricular contractions are benign and may even be found in otherwise healthy hearts.
A premature ventricular contraction may be perceived as a “skipped beat” or felt as palpitations in the chest. In a normal heartbeat, the ventricles contract after the atria have helped to fill them by contracting; in this way the ventricles can pump a maximized amount of blood both to the lungs and to the rest of the body. In a premature ventricular contraction, the ventricles contract first and before the atria have optimally filled the ventricles with blood, which means that circulation is inefficient. However, single beat premature ventricular contraction abnormal heart rhythms do not usually pose a danger and can be asymptomatic in healthy individuals. A premature ventricular contraction is a type of ectopic heartbeat.
Figure 5. Premature ventricular contraction ECG
Premature ventricular contractions are common — they occur in many people. They’re also called:
- Premature ventricular complexes
- Ventricular premature beats
- Ventricular extrasystoles
If you have occasional premature ventricular contractions, but you’re otherwise healthy, there’s probably no reason for concern, and no need for treatment. If you have frequent premature ventricular contractions or underlying heart disease, you might need treatment.
Premature ventricular contraction causes
Premature ventricular contractions are abnormal contractions that begin in the ventricles. These extra contractions usually beat sooner than the next expected regular heartbeat. And they often interrupt the normal order of pumping, which is the atria first, then the ventricles.
Why do extra heartbeats occur?
The reasons aren’t always clear. Certain triggers, heart diseases or changes in the body can make cells in the ventricles electrically unstable. Heart disease or scarring may also cause electrical impulses to be misrouted.
Premature ventricular contractions can be associated with:
- Certain medications, including decongestants and antihistamines
- Alcohol or illegal drugs
- Increased levels of adrenaline in the body that may be caused by caffeine, tobacco, exercise or anxiety
- Injury to the heart muscle from coronary artery disease, congenital heart disease, high blood pressure or heart failure
Risk factors for premature ventricular contraction
The following can increase your risk of premature ventricular contractions:
- Caffeine , tobacco, alcohol and illicit drugs
- Exercise — if you have certain types of premature ventricular contractions
- High blood pressure (hypertension)
- Anxiety
- Heart disease, including congenital heart disease, coronary artery disease, heart attack, heart failure and a weakened heart muscle (cardiomyopathy)
Premature ventricular contraction symptoms
Premature ventricular contractions often cause few or no symptoms. But you might feel an odd sensation in your chest, such as:
- Fluttering
- Pounding or jumping
- Skipped beats or missed beats
- Increased awareness of your heartbeat
Premature ventricular contraction complications
Having frequent premature ventricular contractions or certain patterns of them might increase your risk of developing heart rhythm problems (arrhythmias) or weakening of the heart muscle (cardiomyopathy).
Rarely, when accompanied by heart disease, frequent premature contractions can lead to chaotic, dangerous heart rhythms and possibly sudden cardiac death.
Premature ventricular contractions diagnosis
An electrocardiogram (ECG) can detect the extra beats and identify the pattern and source.
Electrocardiogram
Depending on the frequency and timing of your premature ventricular contractions, different types of ECG testing options are available.
- Standard ECG. Sensors (electrodes) are attached to your chest and limbs to create a graphical record of the electrical signals traveling through your heart. This brief test usually is done in a clinic or hospital setting.
If you have infrequent premature ventricular contractions, they may not be detected during the brief time a standard ECG is being done. In such cases, you may need to use a portable monitoring device for 24 hours or more to capture any abnormal rhythms. Common types of portable ECGs include:
- Holter monitor. You carry this device in your pocket or in a pouch on a belt or shoulder strap. It automatically records your heart’s activity for 24 or 48 hours, which provides your doctor with an extended look at your heart rhythms.
- Event recorder. This device can be carried in your pocket or worn on a belt or shoulder strap for home monitoring of your heart’s activity. When you feel symptoms, you push a button, and a brief ECG strip recording is made. The recorder, which can be used for several weeks, allows your doctor to see your heart rhythm at the time of your symptoms.
- Exercise stress ECG. This test uses electrocardiography to record your heart’s electrical activity while you walk on a treadmill or pedal an exercise bike. It can help determine whether exercise triggers your premature ventricular contractions.
Premature ventricular contractions treatment
For most people, premature ventricular contractions with an otherwise normal heart won’t need treatment. However, if you have frequent premature ventricular contractions, your doctor might recommend treatment.
In some cases, if you have heart disease that could lead to more-serious rhythm problems, you might need the following:
- Lifestyle changes. Eliminating common premature ventricular contraction triggers — such as caffeine or tobacco — can decrease the frequency and severity of your symptoms.
- Medications. Beta blockers — which are often used to treat high blood pressure and heart disease — can suppress premature contractions. Other medications, such as calcium channel blockers, or anti-arrhythmic drugs, such as amiodarone (Pacerone) or flecainide (Tambocor), also might be used if you have ventricular tachycardia or frequent premature ventricular contractions that interfere with your heart’s function.
- Radiofrequency catheter ablation. For premature ventricular contractions that don’t respond to lifestyle changes or medications, your doctor might recommend ablation therapy. This procedure uses radiofrequency energy to destroy the area of heart tissue that is causing your irregular contractions.
Home remedies
The following self-care strategies can help control premature ventricular contractions and improve your heart health:
- Track your triggers. If you have frequent symptoms, you might want to take note of your symptoms and your activities. This can help identify substances or actions that may trigger premature ventricular contractions.
- Modify your substance use. Caffeine, alcohol, tobacco and other recreational drugs are known triggers of premature ventricular contractions. Reducing or avoiding these substances can reduce your symptoms.
- Manage stress. Anxiety can trigger abnormal heartbeats. If you think anxiety is contributing to your condition, try stress-reduction techniques, such as biofeedback, meditation or exercise, or talk to your doctor about anti-anxiety medications.
Ectopic heartbeat causes
The reasons for ectopic heartbeat aren’t always clear. Certain triggers, heart diseases or changes in the body can make cells in the atria and ventricles electrically unstable. Heart disease or scarring may also cause electrical impulses to be misrouted.
Common triggers of heart palpitations include:
- strenuous exercise
- not getting enough sleep
- drinks containing caffeine, such as coffee, tea and energy drinks
- alcohol
- smoking
- illegal drugs, such as cocaine, heroin, amphetamines, ecstasy and cannabis
- rich or spicy foods
- changes in the blood, such as a low potassium level (hypokalemia)
- decrease in blood supply to the heart
- when the heart is enlarged
In these cases, the palpitations should go away on their own. Avoiding these triggers may help stop them coming back.
Thousands of substances may affect the heart’s electrical system and change its ability to pump blood through the body. Many illegal, prescription and over-the-counter drugs, as well as alcohol, tobacco, certain foods and other substances, can affect the electrical signals that trigger the heartbeat.
Caffeine, Diet and Heart Arrhythmias
Caffeine is the most common substance linked with abnormal heart rhythms (arrhythmias). Some people feel heart palpitations (fast heartbeats) when they drink coffee or tea or eat chocolate. Red wine and eating too much can bring about symptoms in others. These rhythm problems are rarely serious.
Substance Abuse: Drugs and Inhalants
Abusing legal or illegal drugs can lead to dangerous arrhythmias.
Alcohol
Small amounts (no more than one drink a day) of alcohol may lower the risk of heart problems and increase “good” cholesterol (HDL cholesterol). But for some people, alcohol can cause heart rhythm disturbances. Alcohol abuse is a major risk factor for High Blood Pressure, cardiomyopathy (weak heart muscle), heart failure and stroke.
Tobacco
Tobacco (cigarettes) causes more heart and blood vessel disease, stroke and heart-related deaths than all illegal drugs combined. It contributes to as much as one-third of all heart disease.
Dietary Supplements and Over-the-Counter Medications
Some herbs and other substances used in over-the-counter remedies are believed to improve abnormal heart rhythms. Others can make them worse or interfere with heart medications. Diet pills can be especially dangerous. Patients should always talk to a healthcare provider before taking any medication or supplement.
Prescription Drugs
While most medications prescribed by doctors are beneficial to health, some can cause serious side effects. Certain medications commonly prescribed for arrhythmias, heart disease and High Blood Pressure can themselves cause problems, including heart rhythm disturbances. Patients should watch for symptoms and discuss any changes with a doctor or healthcare provider.
Substances in the Environment and Workplace
Hundreds of substances in the environment can cause arrhythmias, heart disease and death. In general, the people at greatest risk are those who handle or come into contact with dangerous substances in the workplace. Some of the substances that can cause problems are: automobile emissions, cigarette smoke, pollution from industrial plants, paint thinners and propane gas.
Emotional or psychological triggers
Heart palpitations are also often caused by emotions or psychological issues, such as:
- excitement or nervousness
- stress or anxiety
- panic attacks – an overwhelming sense of anxiety or fear, accompanied by feeling sick, sweating, trembling and palpitations
Breathing exercises and panic attack tips may help if you’re feeling stressed, anxious or panicky.
Medication
Palpitations can occasionally be triggered by some types of:
- asthma inhalers, such as salbutamol and ipratropium bromide
- high blood pressure (hypertension) medicines, such as hydralazine and minoxidil
- antihistamines, such as terfenadine
- antibiotics, such as clarithromycin and erythromycin
- antidepressants, such as citalopram and escitalopram
- antifungal medicines, such as itraconazole
Speak to your doctor if you think medication may be causing your palpitations. But don’t stop taking a prescribed treatment without first getting medical advice.
Hormone changes
Heart palpitations in women can sometimes be the result of hormonal changes that occur during:
- periods
- pregnancy
- the menopause – when a woman stops having periods and is no longer able to get pregnant naturally
In these cases, the palpitations are usually temporary and not a cause for concern.
Risk factors for ectopic heartbeats
The following can increase your risk of ectopic heartbeats:
- Caffeine , tobacco, alcohol and illicit drugs
- Exercise — if you have certain types of premature ventricular contractions
- High blood pressure (hypertension)
- Anxiety
- Heart disease, including congenital heart disease, coronary artery disease, heart attack, heart failure and a weakened heart muscle (cardiomyopathy)
Ectopic heartbeats complications
Having frequent premature ventricular contractions or certain patterns of them might increase your risk of developing heart rhythm problems (arrhythmias) or weakening of the heart muscle (cardiomyopathy).
Rarely, when accompanied by heart disease, frequent premature contractions can lead to chaotic, dangerous heart rhythms and possibly sudden cardiac death.
Ectopic heartbeat symptoms
Ectopic heartbeats often cause few or no symptoms. But you might feel an odd sensation in your chest, such as:
- Feeling your heartbeat (palpitations)
- Feeling like your heart stopped or skipped a beat
- Feeling of occasional, forceful beats
- Fluttering
- Pounding or jumping
- Skipped beats or missed beats
- Increased awareness of your heartbeat.
Ectopic heartbeat diagnosis
A physical exam may show an occasional uneven pulse. If the ectopic heartbeats DO NOT occur very often, your provider may not find them during a physical exam.
Blood pressure is most often normal.
An electrocardiogram (ECG) can detect the extra beats and identify the pattern and source.
Electrocardiogram
Depending on the frequency and timing of your ectopic heartbeats, different types of ECG testing options are available.
- Standard ECG. Sensors (electrodes) are attached to your chest and limbs to create a graphical record of the electrical signals traveling through your heart. This brief test usually is done in a clinic or hospital setting. If you have infrequent ectopic heartbeats, they may not be detected during the brief time a standard ECG is being done. In such cases, you may need to use a portable monitoring device for 24 hours or more to capture any abnormal rhythms.
Often, no further testing is needed when your ECG is normal and the symptoms are not severe or worrisome.
If your doctor wants to know more about your heart rhythm, he or she may order:
- A monitor that you wear that records and stores your heart rhythm for 24 to 48 hours (Holter monitor)
- A recording device that you wear, and records your heart rhythm whenever you feel a skipped beat
Common types of portable ECGs include:
- Holter monitor. You carry this device in your pocket or in a pouch on a belt or shoulder strap. It automatically records your heart’s activity for 24 or 48 hours, which provides your doctor with an extended look at your heart rhythms.
- Event recorder. This device can be carried in your pocket or worn on a belt or shoulder strap for home monitoring of your heart’s activity. When you feel symptoms, you push a button, and a brief ECG strip recording is made. The recorder, which can be used for several weeks, allows your doctor to see your heart rhythm at the time of your symptoms.
- Exercise stress ECG. This test uses electrocardiography to record your heart’s electrical activity while you walk on a treadmill or pedal an exercise bike. It can help determine whether exercise triggers your ectopic heartbeats.
- An echocardiogram may be ordered if your doctor suspects problems with the size or structure of your heart are the cause.
Ectopic heartbeat treatment
For most people, ectopic heartbeats with an otherwise normal heart won’t need treatment. However, if you have frequent ectopic heartbeats, your doctor might recommend treatment.
In some cases, if you have heart disease that could lead to more-serious rhythm problems, you might need the following:
- Lifestyle changes. Eliminating common ectopic heartbeat triggers — such as caffeine or tobacco — can decrease the frequency and severity of your symptoms.
- Medications. Beta blockers — which are often used to treat high blood pressure and heart disease — can suppress premature contractions. Other medications, such as calcium channel blockers, or anti-arrhythmic drugs, such as amiodarone (Pacerone) or flecainide (Tambocor), also might be used if you have ventricular tachycardia or frequent ectopic heartbeats that interfere with your heart’s function.
- Radiofrequency catheter ablation. For ectopic heartbeats that don’t respond to lifestyle changes or medications, your doctor might recommend ablation therapy. This procedure uses radiofrequency energy to destroy the area of heart tissue that is causing your irregular contractions.
Home remedies
The following self-care strategies can help control ectopic heartbeats and improve your heart health:
- Track your triggers. If you have frequent symptoms, you might want to take note of your symptoms and your activities. This can help identify substances or actions that may trigger premature ventricular contractions.
- Modify your substance use. Caffeine, alcohol, tobacco and other recreational drugs are known triggers of premature ventricular contractions. Reducing or avoiding these substances can reduce your symptoms.
- Manage stress. Anxiety can trigger abnormal heartbeats. If you think anxiety is contributing to your condition, try stress-reduction techniques, such as biofeedback, meditation or exercise, or talk to your doctor about anti-anxiety medications.
Ectopic heartbeat exercise
Physical activity can help reduce your risk of heart disease. It can also help you control your weight, reduce blood pressure and cholesterol and improve your mental health – helping you to look and feel great.
1. Start small
If 150 minutes of physical activity a week seems like a lot, don’t worry. You can break it down into ten minute sessions throughout the day and build up from there. Why not try our 10 minute workout? You can do it from the comfort of your own living room.
2. Be realistic about your goals
Set yourself realistic goals that are specific and achievable. For example, set a goal to walk 30 minutes every day or learn how to swim.
3. Make exercise part of your day
Plan a time to do some physical activity that fits in with the rest of your day and try keeping an activity diary to help monitor your progress and success. If you miss a day, don’t worry – just make sure you start again the next day.
4. Keep moving
Remember, everyday activities count, so look out for opportunities to be active during the day.
For example, use the stairs instead of the escalators, walk to the local shop rather than taking the car and do some stretches when watching TV. Every ten minutes counts!
5. You don’t have to go it alone
Involve friends and family to make activities more fun, sociable and enjoyable. Go jogging with a friend and support and motivate each other, take the children swimming or join an exercise class.
6. Make sure you get plenty of variety
Make a list of enjoyable activities, such as dancing and yoga, and place them in a jar. Pick a different activity to do each week. By varying your activities, you are less likely to get bored and lose interest.
7. Set reminders where you can see them
Prompt yourself to be more physically active by keeping reminders around the house. Put Post-it notes on the fridge door or by the kettle, place your cycling helmet on your dressing table or put your walking shoes near the door.
8. Keep an eye on your progress
You can use a pedometer to count the number of steps you walk each day. It’s easy to use. All you need is a good pair of shoes and you are ready to take a step in the right direction, so you can push yourself to go that bit further next time you exercise.
Walking is an ideal activity as it’s free and easy to do anywhere. You could walk your children to school and back every day, take the dog for a walk or find a local park and go walking with a friend.
9. Reward yourself
Recognize when you achieve your goals. Think of things that you could reward yourself with, like a copy of your favorite magazine, a new pair of trainers or a massage.
Finding the energy to workout after a long day at work can be a struggle. Try these tips to keep your energy going strong so you can Move More.
Power Up to Move More
Do you have trouble staying energized for your post-workday workout? We feel you! Try these tips to keep your energy going strong so you can Move More.
- Hydrate: Drink water throughout the day and especially before, during and after physical activity.
- Fuel Up: When your energy is starting to lag, snack on healthy carbs, like vegetables, fruits and whole grains.
- Fight Fatigue: Alternate sitting and standing during the day. Wear comfy shoes you can easily walk in, or use insoles to keep your legs and feet feeling fine.
- Refresh: Try stress-relieving activity breaks, like lunchtime walks, meditation and yoga to rejuvenate and refresh anytime.
- Breathe: Practice breathing deeply by inhaling through your nose and exhaling through your mouth slowly to deliberately send more oxygen to your brain and body.
- Eat for Energy: Avoid eating saturated fats or too much protein throughout the day. They digest more slowly and can take away oxygen and energy-delivering blood from your muscles.
- Don’t Wait: Make it a habit to go right from work or school to your workout or activity. If you stop at home, you may be tempted to skip it.
- Refuel: Refuel after your sweat sesh with lean protein, healthy carbs and plenty of water so your body can recover more quickly.