Contents
What is elephantiasis
Elephantiasis is a symptom of a variety of diseases that is characterized by the thickening of the skin and underlying tissues, especially in the legs, male genitals and female breasts. Some conditions having this symptom include: Elephantiasis nostras, due to longstanding chronic lymphangitis; Elephantiasis tropica or lymphatic filariasis, caused by a number of parasitic worms, particularly Wuchereria bancrofti; non-filarial elephantiasis or podoconiosis, an immune disease caused by heavy metals affecting the lymph vessels; proteus syndrome, the genetic disorder of the so-called Elephant Man 1). Podoconiosis is a type of lower limb tropical elephantiasis distinct from lymphatic filariasis. Lymphatic filariasis affects all population at risk, whereas podoconiosis predominantly affects barefoot subsistence farmers in areas with red volcanic soil 2).
Lymphatic filariasis is a parasitic disease caused by microscopic, thread-like worms. The adult worms only live in the human lymph system. The lymph system maintains the body’s fluid balance and fights infections.
Lymphatic filariasis affects over 120 million people in 73 countries throughout the tropics and sub-tropics of Asia, Africa, the Western Pacific, and parts of the Caribbean and South America.
In the Americas, only four countries are currently known to be endemic: Haiti, the Dominican Republic, Guyana and Brazil.
In the United States, Charleston, South Carolina, was the last known place with lymphatic filariasis. The infection disappeared early in the 20th century. Currently, you cannot get infected in the U.S. 3).
People with lymphatic filariasis disease can suffer from lymphedema and elephantiasis and in men, swelling of the scrotum, called hydrocele. Lymphatic filariasis is a leading cause of permanent disability worldwide. Communities frequently shun and reject women and men disfigured by the disease. Affected people frequently are unable to work because of their disability, and this harms their families and their communities.
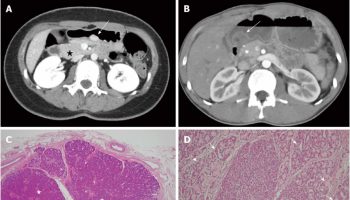
Figure 1. Wuchereria bancrofti
Footnotes:
Figure A: Microfilaria of Wuchereria bancrofti with sheath at the posterior end in a thick blood smear stained with Giemsa.
Figure B: Microfilaria of Wuchereria bancrofti in a thick blood smear stained with Giemsa.
The microfilaria of Wuchereria bancrofti are sheathed and measure 240-300 µm in stained blood smears and 275-320 µm in 2% formalin. They have a gently curved body, and a tail that is tapered to a point. The nuclear column (the cells that constitute the body of the microfilaria) is loosely packed; the cells can be visualized individually and do not extend to the tip of the tail. Microfilariae circulate in the blood.
[Source 4)]Elephantiasis disease
Lymphatic filariasis, considered globally as a neglected tropical disease, is a parasitic disease caused by microscopic, thread-like worms. The adult worms only live in the human lymph system. The lymph system maintains the body’s fluid balance and fights infections. Lymphatic filariasis is spread from person to person by mosquitoes.
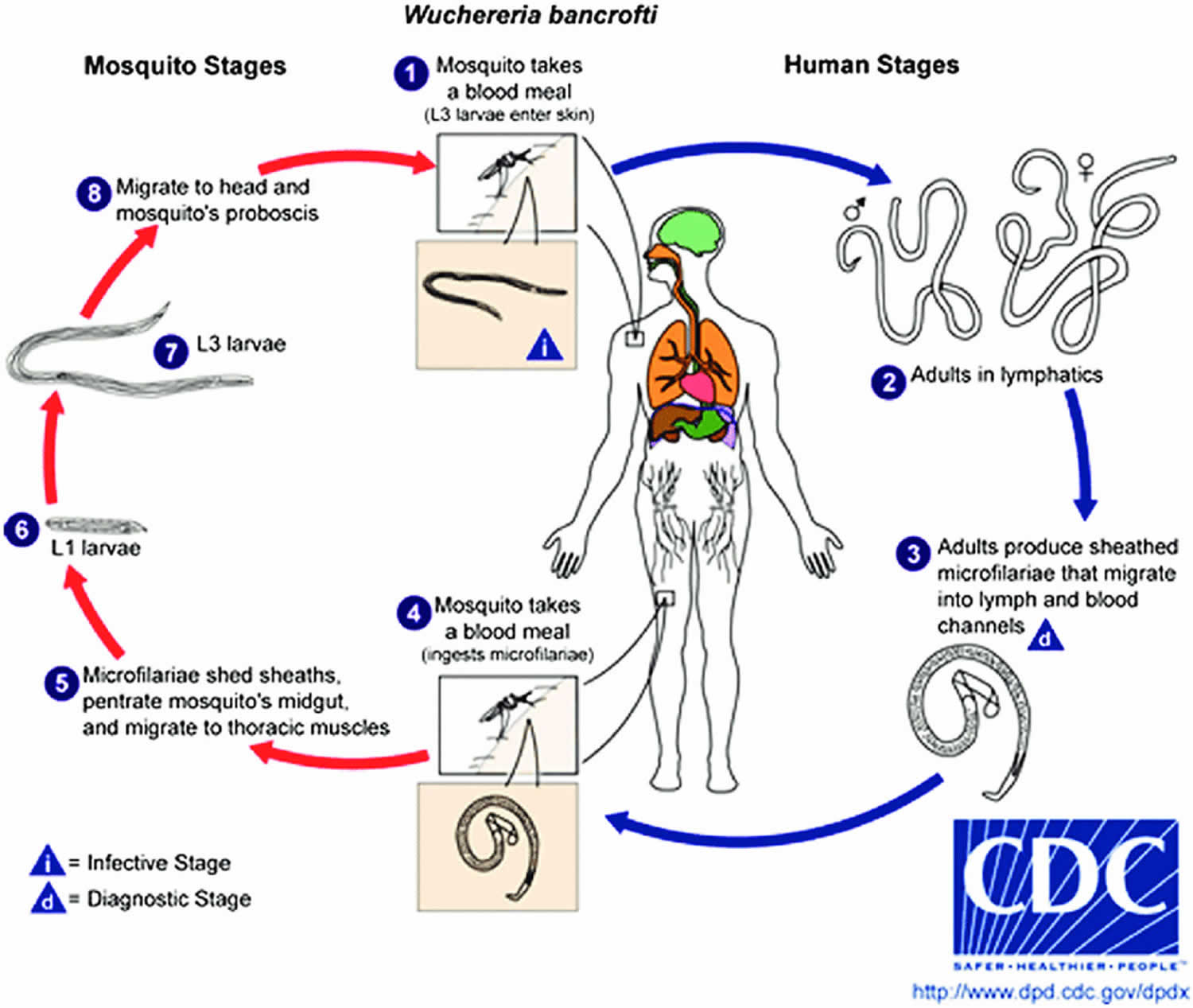
Wuchereria bancrofti life cycle
Different species of the following genera of mosquitoes are vectors of Wuchereria bancrofti filariasis depending on geographical distribution. Among them are: Culex (C. annulirostris, C. bitaeniorhynchus, C. quinquefasciatus, and C. pipiens); Anopheles (A. arabinensis, A. bancroftii, A. farauti, A. funestus, A. gambiae, A. koliensis, A. melas, A. merus, A. punctulatus and A. wellcomei); Aedes (A. aegypti, A. aquasalis, A. bellator, A. cooki, A. darlingi, A. kochi, A. polynesiensis, A. pseudoscutellaris, A. rotumae, A. scapularis, and A. vigilax); Mansonia (M. pseudotitillans, M. uniformis); Coquillettidia (C. juxtamansonia). (1) During a blood meal, an infected mosquito introduces third-stage filarial larvae onto the skin of the human host, where they penetrate into the bite wound. (2) They develop in adults that commonly reside in the lymphatics. The female worms measure 80 to 100 mm in length and 0.24 to 0.30 mm in diameter, while the males measure about 40 mm by 0.1 mm. Adults produce microfilariae measuring 244 to 296 μm by 7.5 to 10 μm, which are sheathed and have nocturnal periodicity, except the South Pacific microfilariae which have the absence of marked periodicity. (3) The microfilariae migrate into lymph and blood channels moving actively through lymph and blood. (4) A mosquito ingests the microfilariae during a blood meal. (5) After ingestion, the microfilariae lose their sheaths and some of them work their way through the wall of the proventriculus and cardiac portion of the mosquito’s midgut and reach the thoracic muscles. (6) There the microfilariae develop into first-stage larvae and (7) subsequently into third-stage infective larvae. (8) The third-stage infective larvae migrate through the hemocoel to the mosquito’s prosbocis and (1) can infect another human when the mosquito takes a blood meal.
Figure 2. Lymphatic filariasis – Wuchereria bancrofti life cycle
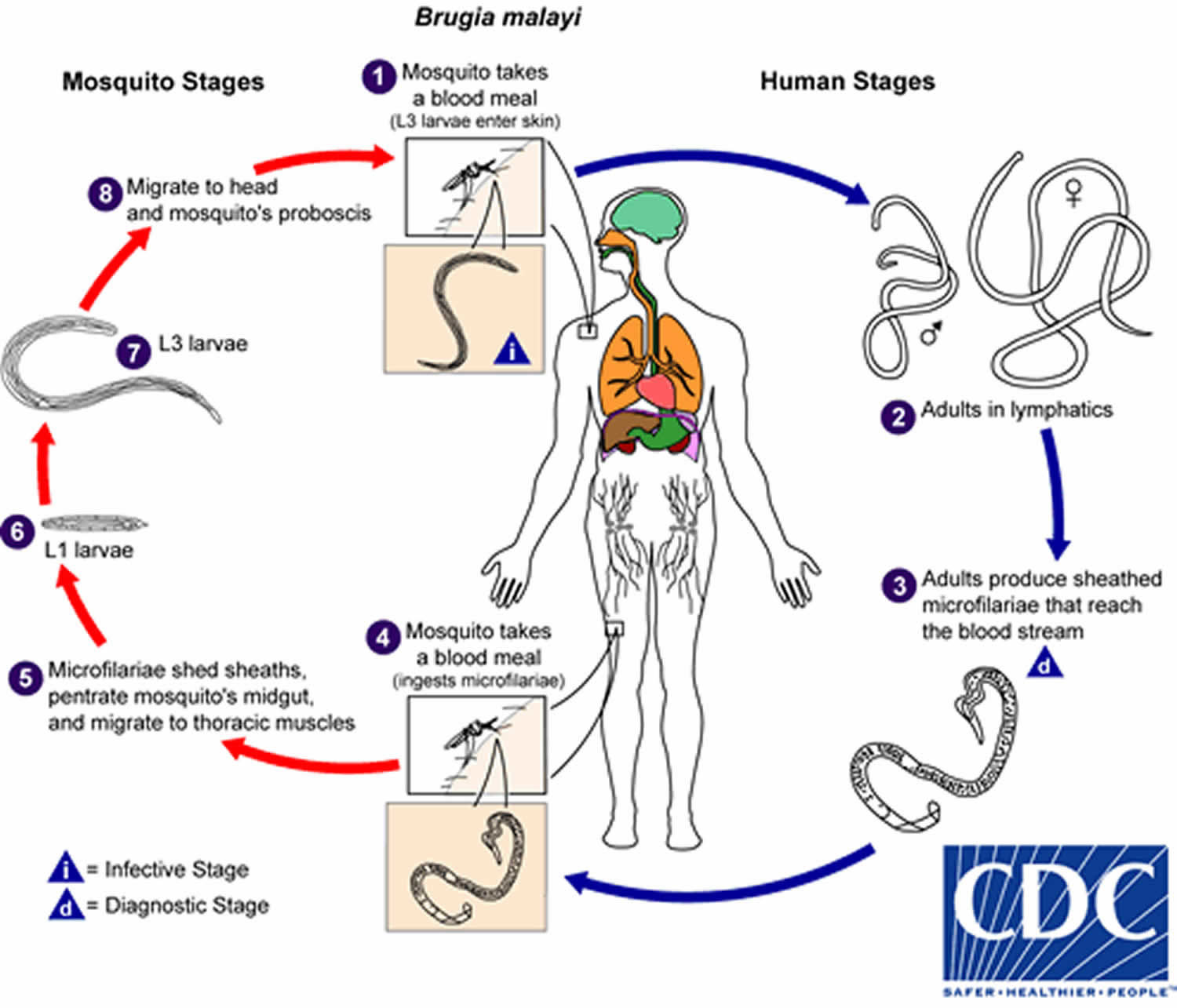
 Brugia Malayi life cycle
Brugia Malayi life cycle
The typical vector for Brugia malayi filariasis are mosquito species in the genera Mansonia and Aedes. (1) During a blood meal, an infected mosquito introduces third-stage filarial larvae onto the skin of the human host, where they penetrate into the bite wound. (2) They develop into adults that commonly reside in the lymphatics. The adult worms resemble those of Wuchereria bancrofti but are smaller. Female worms measure 43 to 55 mm in length by 130 to 170 μm in width, and males measure 13 to 23 mm in length by 70 to 80 μm in width. Adults produce microfilariae, measuring 177 to 230 μm in length and 5 to 7 μm in width, which are sheathed and have nocturnal periodicity. (3) The microfilariae migrate into lymph and enter the blood stream reaching the peripheral blood. (4) A mosquito ingests the microfilariae during a blood meal. (5) After ingestion, the microfilariae lose their sheaths and work their way through the wall of the proventriculus and cardiac portion of the midgut to reach the thoracic muscles. (6) There the microfilariae develop into first-stage larvae and (7) subsequently into third-stage larvae. (8) The third-stage larvae migrate through the hemocoel to the mosquito’s proboscis and (1) can infect another human when the mosquito takes a blood meal.
Figure 3. Lymphatic filariasis – Brugia Malayi life cycle
How is lymphatic filariasis spread?
The disease spreads from person to person by mosquito bites. When a mosquito bites a person who has lymphatic filariasis, microscopic worms circulating in the person’s blood enter and infect the mosquito. People get lymphatic filariasis from the bite of an infected mosquito. The microscopic worms pass from the mosquito through the skin, and travel to the lymph vessels. In the lymph vessels they grow into adults. An adult worm lives for about 5–7 years. The adult worms mate and release millions of microscopic worms, called microfilariae, into the blood. People with the worms in their blood can give the infection to others through mosquitoes.
Who is at risk for infection?
Repeated mosquito bites over several months to years are needed to get lymphatic filariasis. People living for a long time in tropical or sub-tropical areas where the disease is common are at the greatest risk for infection. Short-term tourists have a very low risk. An infection will show up on a blood test.
Elephantiasis symptoms
Most infected people are asymptomatic and will never develop clinical symptoms, despite the fact that the parasite damages the lymph system. These people do not know they have lymphatic filariasis unless tested. A small percentage of persons will develop lymphedema. This is caused by improper functioning of the lymph system that results in fluid collection and swelling. This mostly affects the legs, but can also occur in the arms, breasts, and genitalia. Most people develop these clinical manifestations years after being infected.
The swelling and the decreased function of the lymph system make it difficult for the body to fight germs and infections. Affected persons will have more bacterial infections in the skin and lymph system. This causes hardening and thickening of the skin, which is called elephantiasis. Many of these bacterial infections can be prevented with appropriate skin hygiene and exercise.
Men can develop hydrocele or swelling of the scrotum due to infection with one of the parasites that causes lymphatic filariasis, specifically Wuchereria bancrofti (see Figure 4).
Filarial infection can also cause tropical pulmonary eosinophilia syndrome. Cough, shortness of breath, wheezing, fever, marked eosinophilia and high serum IgE (Immunoglobulin E) concentrations, and positive antifilarial antibodies are manifestations of the tropical pulmonary eosinophilia syndrome. Peripheral microfilaremia is absent in patients with tropical pulmonary eosinophilia. Most cases of tropical pulmonary eosinophilia have been reported in long-term residents from Asia. Men 20 to 40 years old are most commonly affected.
Filarial lymphadenopathy is seen commonly in infected children; before puberty, adult worms can be detected by ultrasonography of the inguinal, crural, and axillary lymph nodes and vessels. Death of the adult worm triggers an acute inflammatory response, which progresses distally (retrograde) along the affected lymphatic vessel, usually in the limbs and is termed acute filarial lymphangitis. If present, systemic symptoms, such as headache or fever, are generally mild.
In postpubertal males, adult Wuchereria bancrofti organisms are found most commonly in the intrascrotal lymphatic vessels and can be visualized on ultrasound examination. Inflammation resulting from adult worm death, in this area, may present as funiculitis, epididymitis, or orchitis. A tender granulomatous nodule may be palpable at the site of the dead adult worms.
The chronic manifestations of lymphedema and/or hydrocele will develop in approximately 30% of lymphatic filariasis infected persons. Lymphedema mostly affects the legs, but can also occur in the arms, breasts, and genitalia. Most people develop these symptoms years after being infected. Recurrent secondary bacterial infections of the affected extremity, characterized by severe pain, fever and chills, hasten the progression of lymphedema to its advanced stage, known as elephantiasis.
Filarial hydrocele is thought to be the consequence of lymphatic damage caused by adult worms. Chyluria, which results from rupture of dilated lymphatics into the renal pelvis, can occur as a manifestation of bancroftian filariasis. Microscopic hematuria and proteinuria are also found in lymphatic filariasis infected patients.
Figure 4. Elephantiasis involving the scrotum
Figure 5. Elephantiasis involving a leg
What causes elephantiasis
Lymphatic filariasis is caused by nematodes (roundworms) that inhabit the lymphatic vessels and lymph nodes of a human host. There are three different filarial species that can cause lymphatic filariasis in humans. Most of the infections worldwide are caused by Wuchereria bancrofti. In Asia, the disease can also be caused by Brugia malayi and Brugia timori.
The infection spreads from person to person by mosquito bites. The adult worm lives in the human lymph vessels, mates, and produces millions of microscopic worms, also known as microfilariae. Microfilariae circulate in the person’s blood and infect the mosquito when it bites a person who is infected. Microfilariae grow and develop in the mosquito. When the mosquito bites another person, the larval worms pass from the mosquito into the human skin, and travel to the lymph vessels. They grow into adult worms, a process that takes 6 months or more. An adult worm lives for about 5–7 years. The adult worms mate and release millions of microfilariae into the blood. People with microfilariae in their blood can serve as a source of infection to others.
A wide range of mosquitoes can transmit the parasite, depending on the geographic area. In Africa, the most common vector is Anopheles and in the Americas, it is Culex quinquefasciatus. Aedes and Mansonia can transmit the infection in the Pacific and in Asia.
Many mosquito bites over several months to years are needed to get lymphatic filariasis. People living for a long time in tropical or sub-tropical areas where the disease is common are at the greatest risk for infection. Short-term tourists have a very low risk.
Programs to eliminate lymphatic filariasis are under way in more than 50 countries. These programs are reducing transmission of the filarial parasites and decreasing the risk of infection for people living in or visiting these communities.
Elephantiasis nostras verrucosa
Elephantiasis nostras verrucosa is a rare, disfiguring complication of longstanding chronic lymphedema 6). Elephantiasis nostras verrucosa is characterized by marked edema of the affected extremity, generalized thickening and lichenification of the skin 7). Disruption of the lymphatic system after trauma, surgery or radiation is the most common cause of chronic lymphedema. Recurrent soft tissue infections also induce fibrosis and worsen the condition 8). Congenital, traumatic or surgical disruption of lymphatic vessels, venous stasis, radiation, neoplastic obstruction, portal hypertension, obesity and congestive heart failure are the precipitating factors of this disease 9). The diagnosis is based on the history and the peculiar skin changes. Treatment options include use of elastic bandages, pneumatic stockings, mechanical massage, oral retinoids and surgery. The goal of the therapy is to re-establish function and to reduce physical disability. Oral retinoids were used successfully in some case series. For refractory cases, microsurgical lymphovenous anastomosis can be used. Amputation should be the last option.
Figure 6. Elephantiasis nostras verrucosa
Footnote: A 49-year-old woman with morbid obesity and hypertension presented with extensive areas of redness and weeping sores on her legs. She had an 8-year history of chronic venous stasis and lymphedema.
[Source 10)]Lymphatic filariasis diagnosis
The standard method for diagnosing active infection is the identification of microfilariae in a blood smear by microscopic examination. The microfilariae that cause lymphatic filariasis circulate in the blood at night (called nocturnal periodicity). Blood collection should be done at night to coincide with the appearance of the microfilariae, and a thick smear should be made and stained with Giemsa or hematoxylin and eosin. For increased sensitivity, concentration techniques can be used.
Serologic techniques provide an alternative to microscopic detection of microfilariae for the diagnosis of lymphatic filariasis. Patients with active filarial infection typically have elevated levels of antifilarial IgG4 in the blood and these can be detected using routine assays.
Because lymphedema may develop many years after infection, lab tests are most likely to be negative with these patients.
Diagnostic findings
Microscopy
Lymphatic filariasis is usually identified by the finding of microfilaria in peripheral blood smears (thick or thin) stained with Giemsa or hematoxylin-and-eosin. For increased sensitivity, concentration techniques can be used. These include centrifugation of the blood sample lysed in 2% formalin (Knott’s technique), or filtration through a Nucleopore® membrane. Microfilariae of Wuchereria and Brugia exhibit a nocturnal periodicity and an accurate diagnosis is best achieved on smears collected at night (10 PM-2 AM). Adults may be identified in biopsy specimens of lymphatic tissue.
Antigen Detection
Antigen detection using an immunoassay for circulating filarial antigens constitutes a useful diagnostic approach because sensitivity for detection of microfilariae can be low and variable. Unlike microfilariae with nocturnal periodicity, filarial antigens can be detected in blood samples collected at any time of day. A rapid format immunochromatographic test has been shown to be a useful and sensitive tool for the detection of Wuchereria bancrofti antigen and is being used widely by lymphatic filariasis elimination programs. Currently, this test is not licensed for use in the United States and cannot be used for patient diagnosis.
Elephantiasis treatment
Patients currently infected with the parasite
Diethylcarbamazine (DEC) is the drug of choice in the United States. The drug kills the microfilaria and some of the adult worms. Diethylcarbamazine (DEC) has been used world-wide for more than 50 years. Because this infection is rare in the U.S., the drug is no longer approved by the Food and Drug Administration (FDA) and cannot be sold in the U.S. Physicians can obtain the medication from CDC after confirmed positive lab results. CDC gives the physicians the choice between 1 or 12-day treatment of DEC (6 mg/kg/day). One day treatment is generally as effective as the 12-day regimen. For tropical pulmonary eosinophilia, a longer DEC treatment course of 14-21 days is generally recommended. Diethylcarbamazine (DEC) is generally well tolerated. Side effects are in general limited and depend on the number of microfilariae in the blood. The most common side effects are dizziness, nausea, fever, headache, or pain in muscles or joints.
Diethylcarbamazine (DEC) should not be administered to patients who may also have onchocerciasis as DEC can worsen onchocercal eye disease. In patients with loiasis, DEC can cause serious adverse reactions, including encephalopathy and death. The risk and severity of the adverse reactions are related to Loa loa microfilarial density.
The drug ivermectin kills only the microfilariae, but not the adult worm; the adult worm is responsible for the pathology of lymphedema and hydrocele.
Some studies have shown adult worm killing with treatment with doxycycline (200mg/day for 4–6 weeks).
Patients with clinical symptoms
Lymphedema and elephantiasis are not indications for diethylcarbamazine (DEC) treatment because most people with lymphedema are not actively infected with the filarial parasite.
To prevent the lymphedema from getting worse, patients should ask their physician for a referral to a lymphedema therapist so they can be informed about some basic principles of care such as hygiene, exercise and treatment of wounds.
Patients with hydrocele may have evidence of active infection, but typically do not improve clinically following treatment with diethylcarbamazine (DEC). The treatment for hydrocele is surgery.
Lymphoedema treatment
Lymphedema is an ongoing condition that has no known cure. The main goal of treatment is to reduce the swelling and keep it to a minimum. It is very important to treat lymphedema in its early stages to prevent further swelling and complications such as infection. If a cause is found then the cause needs to be treated, e.g. cancer.
For patients with mild to moderate swelling of their limbs a treatment regimen called Complex Physical (Lymphatic/Lymphedema) Therapy (C.P.T./C.L.T.) is recommended. This regimen consists of 4 main parts.
- Skin care – this involves keeping the skin clean to reduce infection, the use of emollients to restore and maintain skin suppleness, and keratolytics to remove hard, dead skin.
- Simple lymphatic drainage – this is a gentle massage technique that uses simple hand movements to try to move the swelling out of the affected area. The patient, relative or caregiver is taught the technique.
- Compression bandaging, sleeve or stocking to help prevent swelling from building up in the limb again.
- Exercise and movement – specially designed programme to supplement the massage and help by maximizing lymph drainage without over exertion
For people with more severe swelling, additional treatments are usually recommended. These include:
- Manual Lymphatic Drainage – specialized form of massage carried out by a trained therapist to move the skin in specific directions based on the underlying anatomy and physiology of the lymphatic system.
- Multi-Layer Lymphedema Bandaging – multi-layer system of compression bandages
- Drug therapy – research is ongoing as to the effectiveness of drug therapy in lymphedema. Benzopyrenes including flavonoids have been used. Coumarin use has been discontinued due to hepatic toxicity.
- Surgery – rarely performed but may be of benefit for eyelid or genital swelling. Only surgeons who have experience with lymphedema and the lymphatic system should perform surgery.
The National Lymphedema Network website (http://www.lymphnet.org/) lists certified lymphedema therapists and lymphedema organizations in the U.S.
References [ + ]