Contents
What is female sexual dysfunction
Female sexual dysfunction is defined by the World Health Organization as “the various ways in which an individual is unable to participate in a sexual relationship…she would wish.” Female sexual dysfunction is classified into a range of disorders depending on the specific nature of the sexual difficulties a woman encounters. According to the Mayo Clinic, female sexual dysfunction is defined as “persistent, recurrent problems with sexual response, desire, orgasm or pain — that distress you or strain your relationship with your partner” 1. Female sexual dysfunction is a prevalent problem, afflicting approximately 40% of women 2, but only a small percentage of women seek medical attention. Approximately 40 million American women are affected by female sexual dysfunction 3. The National Health and Social Life Survey, a probability sample study of sexual behavior in a demographically representative cohort of U.S. adults ages 18 to 59, found that sexual dysfunction is more prevalent in women (43%) than in men (31%), and increases as women age 4. Married women have a lower risk of sexual dysfunction than unmarried women. Hispanic women consistently report lower rates of sexual problems, whereas African American women have higher rates of decreased sexual desire and pleasure than do white women. Sexual pain, however, is more likely to occur in white women. This survey was limited by its cross-sectional design and age restrictions, because women older than 60 years were excluded. Also, no adjustments were made for the effects of menopausal status or medical risk factors. Despite these limitations, the survey clearly indicates that sexual dysfunction affects many women.
Research also suggests that the majority of women experience sexual dysfunction at some point in their lives, and for many it is an ongoing or recurring issue. Female sexual dysfunction can occur at any stage of life. It can be lifelong or be acquired later in life. It can occur only in certain sexual situations or in all sexual situations.
Sexual dysfunction in women are classified by the Sexual Function Health Council of the American Foundation of Urologic Disease into 5:
- Hypoactive sexual desire disorder: The persistent or recurrent deficiency (or absence) of sexual fantasies or thoughts and/or the lack of receptivity to sexual activity.
- Sexual aversion disorder: The persistent or recurrent fear and/or aversion of sexual contact.
- Sexual arousal disorder: The persistent or recurrent inability to become sexually aroused, often characterized by inadequate vaginal lubrication for penetration.
- Orgasmic disorder: The persistent or recurrent difficulty, delay, or absence of attaining orgasm after sufficient sexual stimulation and arousal.
- Sexual pain disorder includes dyspareunia (genital pain associated with sexual intercourse); vaginismus (involuntary spasm of the vaginal musculature that causes interference with vaginal penetration), and noncoital sexual pain disorder (genital pain induced by noncoital sexual stimulation).
Each of these definitions has three additional subtypes: lifelong versus acquired; generalized versus situational; and of organic, psychogenic, mixed, or unknown causative origin.
Sexual response involves a complex interplay of physiology, emotions, experiences, beliefs, lifestyle and relationships. Disruption of any component can affect sexual desire, arousal or satisfaction, and treatment often involves more than one approach. A large survey of American women reported that 70% had experienced sexual difficulties (including inability to orgasm and not feeling like sex) in the year before the survey. Women over 50 were most likely to experience sexual difficulties, although they were common in all age groups (over 60% of women aged over 50 reported lack of interest in sex, and more than half of women aged 16-49 also reported this difficulty).
Survivors of sexual assault often experience difficulties in future sexual relationships, which may bring back difficult memories of incidents of assault. Women who are pregnant, have recently given birth or are breastfeeding are more likely to experience sexual dysfunction than those who are not. Hormonal imbalances and psychological factors both play a role for these women.
Women also often experience sexual dysfunction following menopause, which is mainly a result of hormonal imbalances.
Women suffering from female sexual dysfunction become anxious or distressed about being unable to engage in or experience sexual activity as they wish. However, other women may experience sexual difficulties (e.g. inability to orgasm) which do not cause them distress. These women do not have female sexual dysfunction. Amongst women with female sexual dysfunction, hypoactive sexual desire and orgasmic disorders are the most commonly reported. Common symptoms associated with female sexual dysfunction include diminished vaginal lubrication, pain and discomfort upon intercourse, decreased sense of arousal and difficulty in achieving orgasm.
There are many physical causes of female sexual dysfunction and these are mainly related to hormone levels and changes. Female sexual dysfunction is more typical as women age and is a progressive and widespread condition. However, female sexual dysfunction is most commonly the result of psychological factors (e.g. relationship satisfaction, depression). Even when female sexual dysfunction is the result of physical factors, psychological factors often contribute to the problem (e.g. women who have difficulty achieving adequate vaginal lubrication or find sex painful may become anxious about approaching sexual encounters, and find it even more difficult to lubricate).
Female sexual dysfunction impacts on women’s sexual functioning and on their overall sense of wellbeing. It is associated with depression and relationship satisfaction. Although it is not clear whether female sexual dysfunction causes depression and relationship satisfaction or vice versa, it is likely that, at least in some cases, female sexual dysfunction leads to depression and dissatisfaction with relationships. If you suffer from female sexual dysfunction it is also likely to affect your sexual partner, so you may both want to talk to about professional.
The effects on the partner can have important implications. For example while studies are limited, it has been shown that female sexual function can be negatively impacted on by male sexual dysfunction. A study comparing the sexual function of women with partners with erectile dysfunction to those without showed that sexual arousal, lubrication, orgasm, satisfaction, pain and total score were significantly lower in those who had partners with erectile dysfunction. Later in that study, a large proportion of the men with erectile dysfunction underwent treatment. Following treatment, sexual arousal, lubrication, orgasm, satisfaction and pain were all significantly increased. It was concluded that female sexual function is impacted by male erection status, which may improve following treatment of male sexual dysfunction.
In comparison to the overwhelming research and treatment for erectile dysfunction in males, specifically with the development of phosphodiesterase type 5 inhibitors (e.g. viagra) significantly less has been explored regarding female sexual dysfunction and treatment is primarily limited to psychological therapy. Several cardiovascular diseases have been linked with female sexual dysfunction including atherosclerosis, peripheral arterial disease and hypertension, all of which are also pathological conditions associated with aging and erectile dysfunction in men. Using animal models, scientists have expanded our understanding of female sexual dysfunction, however a tremendous amount is still to be learned in order to properly treat women suffering from female sexual dysfunction.
Progression of Female Sexual Dysfunction
Hormonal changes, which are the most common physical cause of female sexual dysfunction, tend to occur during and after childbirth and following menopause. Certain medications (e.g. antidepressants, hypertension medication) can also alter hormone levels. female sexual dysfunction is more common in women who take these medications.
Unlike in men, sexual dysfunction in women is most commonly the result of psychological factors which can arise throughout life. There is an immense amount of pressure on women in their roles as employees, wives and mothers. This can lead to stress, anxiety and fatigue, which are all more common in women who suffer from female sexual dysfunction than in those who do not. Women who are not satisfied with their relationships more commonly report female sexual dysfunction, as do those who are depressed.
Normal female sexual response
Female sexual dysfunction has both physiologic and psychological components. It is important to first understand the normal female sexual response to understand sexual dysfunction. Physiologically, sexual arousal begins in the medial preoptic, anterior hypothalamic, and limbic-hippocampal structures within the central nervous system. Electrical signals are then transmitted through the parasympathetic and sympathetic nervous systems 3.
Physiologic and biochemical mediators that modulate vaginal and clitoral smooth-muscle tone and relaxation are currently under investigation. Neuropeptide Y, vasoactive intestinal polypeptide, nitric oxide synthase, cyclic guanosine monophosphate, and substance P have been found in vaginal-tissue nerve fibers. Nitric oxide is believed to mediate clitoral and labial engorgement, whereas vasoactive intestinal polypeptide, a nonadrenergic/noncholinergic neurotransmitter, may enhance vaginal blood flow, lubrication, and secretions 6.
Many changes occur in the female genitalia during sexual arousal. Increased blood flow promotes vasocongestion of the genitalia. Secretions from uterine and Bartholin glands lubricate the vaginal canal. Vaginal smooth muscle relaxation allows for lengthening and dilation of the vagina. As the clitoris is stimulated, its length and diameter increase and engorgement occurs. In addition, the labia minora promote engorgement because of increased blood flow.
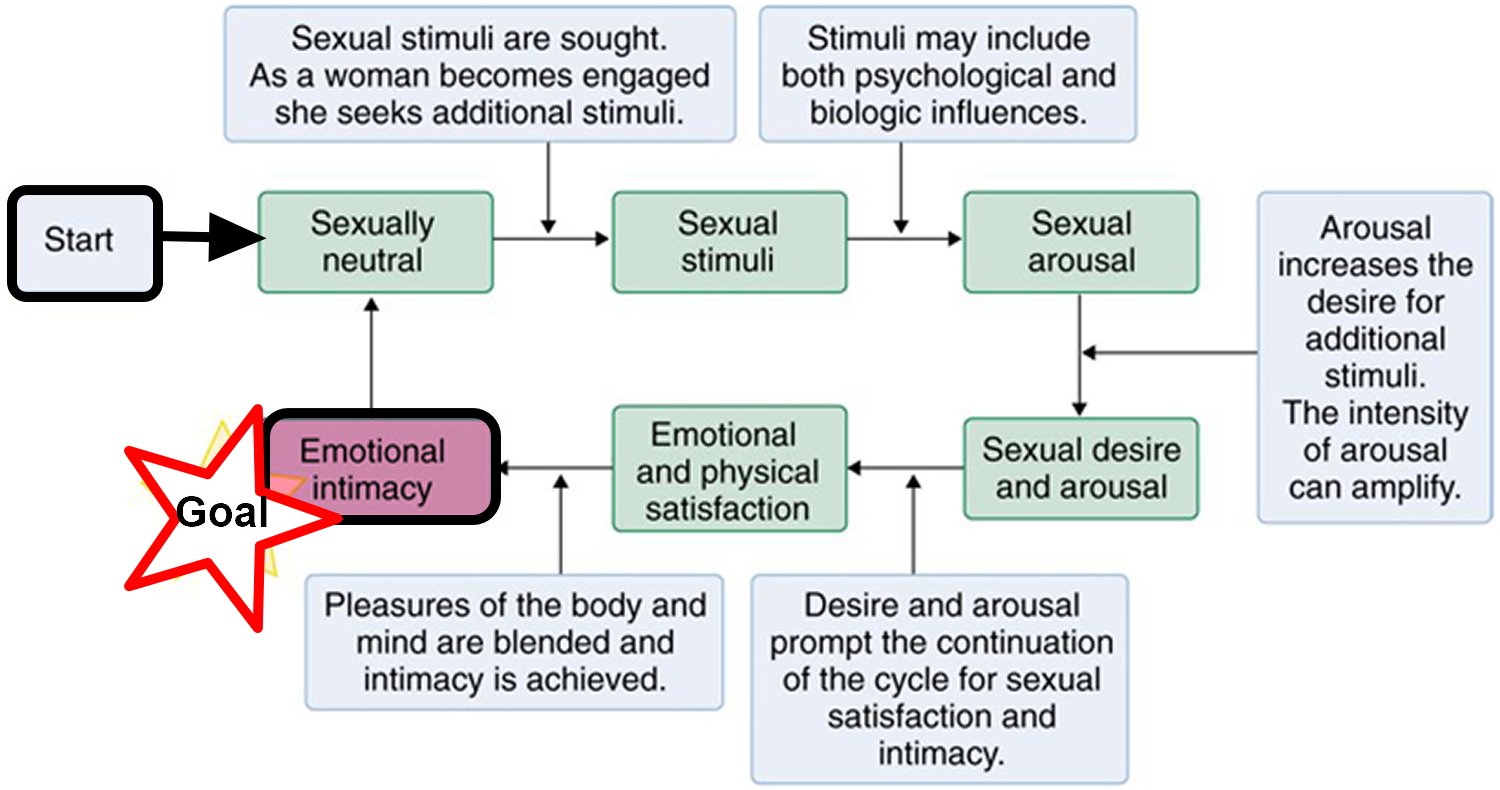
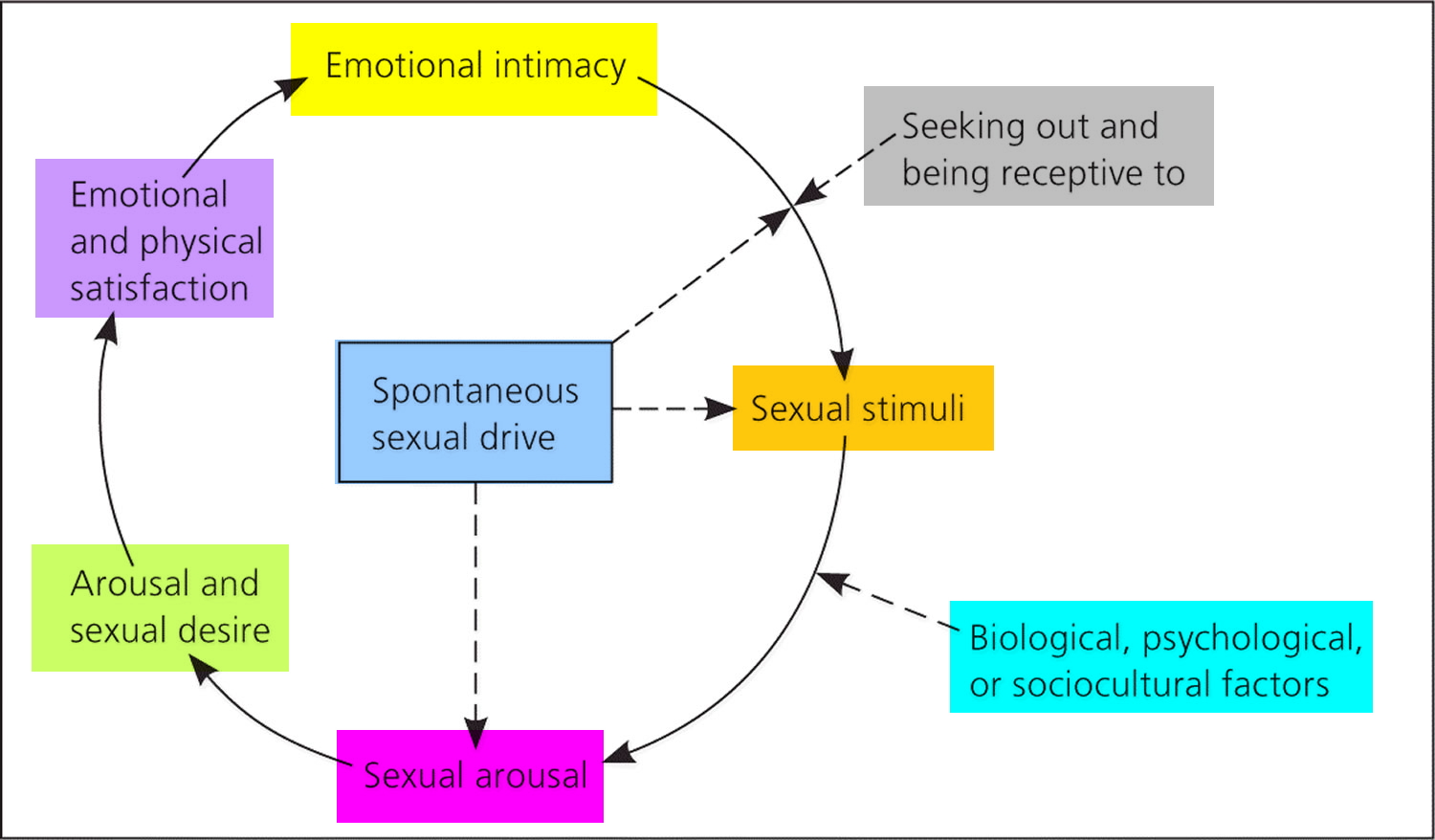
The female sexual response cycle (Figure 1) is an important educational tool that clinicians use when counseling women with sexual concerns. The cycle begins with sexual neutrality. As a woman seeks a sexual stimulus and responds to it, she becomes sexually aroused. Arousal leads to desire, thus stimulating a woman’s willingness to receive or provide additional stimuli. Emotional and physical satisfaction is gained by an increase in sexual desire and arousal. Emotional intimacy is then ultimately achieved. Various biologic and psychological factors can negatively affect this cycle, thereby leading to female sexual dysfunction.
Women enter this cycle of sexual response with spontaneous sexual drive (i.e., the internal desire for sexual activity) or more commonly from a nonsexual state. A woman in a nonsexual state may engage in a sexual encounter for a number of nonsexual reasons (e.g., to please her partner, to feel emotionally connected, out of a sense of duty). Once sexual activity (with adequate stimulation) begins, the woman may experience sexual arousal, which may lead to responsive sexual desire and motivation for future sexual responsiveness 7. This model delineates spontaneous and responsive desire, normalizes the sexual experience of arousal preceding desire, and stresses emotional intimacy as a major motivator for sexual responsiveness.
Figure 1. Female sexual response cycle
Female sexual dysfunction causes
The cause of female sexual dysfunction is multifactorial, encompassing biological, psychological, relational, and sociocultural factors 8. Biological factors may impact sexual function in a variety of ways. Some chronic illnesses, such as vascular disease, diabetes mellitus, neurologic disease, heart and blood vessel (cardiovascular) disease and malignancy 9, can directly or indirectly impact sexual function (Table 1). Aging itself is associated with decreased sexual responsiveness, sexual activity, and libido 10.
Factors, often interrelated, that contribute to sexual dissatisfaction or dysfunction include:
- Physical. Any number of medical conditions, including cancer, kidney failure, multiple sclerosis, heart disease and bladder problems, can lead to sexual dysfunction. Certain medications, including some antidepressants, blood pressure medications, antihistamines and chemotherapy drugs, can decrease your sexual desire and your body’s ability to experience orgasm.
- Hormonal. Lower estrogen levels after menopause may lead to changes in your genital tissues and sexual responsiveness. A decrease in estrogen leads to decreased blood flow to the pelvic region, which can result in needing more time to build arousal and reach orgasm, as well as less genital sensation. The vaginal lining also becomes thinner and less elastic, particularly if you’re not sexually active. These factors can lead to painful intercourse (dyspareunia). Sexual desire also decreases when hormonal levels decrease. Your body’s hormone levels also shift after giving birth and during breast-feeding, which can lead to vaginal dryness and can affect your desire to have sex.
- Psychological and social. Untreated anxiety or depression can cause or contribute to sexual dysfunction, as can long-term stress and a history of sexual abuse. The worries of pregnancy and demands of being a new mother may have similar effects. Long-standing conflicts with your partner — about sex or other aspects of your relationship — can diminish your sexual responsiveness, as well. Cultural and religious issues and problems with body image also can contribute.
Table 1. Medical Conditions That Potentially Impact Female Sexual Function
| Condition | Type of dysfunction | ||||
|---|---|---|---|---|---|
| Desire | Arousal | Orgasm | Pain | Comments | |
Arthritis | + | Decreased mobility and chronic pain may impair sexual function | |||
Coronary artery disease | + | — | |||
Dermatologic conditions (e.g., vulvar lichen sclerosus, vulvar eczema, psoriasis) | + | — | |||
Diabetes mellitus | + | — | |||
Gynecologic conditions (e.g., sexually transmitted infections, endometriosis, chronic pelvic pain, pelvic pain following childbirth, pelvic organ prolapse) | + | — | |||
Hypertension | + | Impact of hypertension or treatment is unclear; one study found an association with low desire | |||
Hypothyroidism | + | + | Increased problems with lubrication and orgasm | ||
Malignancy and treatment (e.g., breast, anal, colorectal, bladder, and gynecologic cancers) | + | + | + | + | Sexual function may be directly or indirectly impacted by cancer diagnosis and treatment; factors include cancer diagnosis, disease itself, treatment (surgery, radiation, chemotherapy), and body image |
Neuromuscular disorders, spinal cord injury, multiple sclerosis | + | + | + | + | Direct impact on sexual response; indirect effect on desire may be mediated by arousal disorders or pain |
Parkinson disease, dementia, head injury | + | Desire may be increased or decreased | |||
Pituitary tumor, hyperprolactinemia | + | — | |||
Renal failure | Dialysis is associated with sexual dysfunction; no data on which type of sexual dysfunction is affected | ||||
Urinary incontinence | + | + | + | — | |
[Sources 10, 9]
Sexual problems often develop when your hormones are in flux, such as after having a baby or during menopause. Hormonal changes occurring in midlife may impact a woman’s sexual function. Menopause is marked by a decline in ovarian hormone levels, which occurs gradually in natural menopause but may be sudden if menopause occurs because of surgery, radiation, or chemotherapy. Decreased vaginal lubrication and dyspareunia are associated with low estradiol levels; however, the association between low sexual desire and lower estradiol levels has been inconsistent. Testosterone levels do not correlate with female sexual function or overall well-being, possibly because of the difficulty in accurately measuring free and total testosterone levels at the lower end of the female range 10. Although androgens are positively associated with improvements in all aspects of sexual functioning (e.g., subjective arousal, vaginal blood flow, sexual desire, orgasm), there is no lower level of testosterone that predicts sexual dysfunction, and androgen levels are not used to define an androgen deficiency syndrome in women.
Serotonin-enhancing medications have an inhibitory effect on sexual function. Sexual dysfunction induced by selective serotonin reuptake inhibitor (SSRI) use is common, with an incidence between 30% and 70%, and may include difficulty with sexual desire, arousal, and orgasm 10. Further, many other commonly prescribed medications may adversely affect sexual functioning, including antiestrogens, such as tamoxifen and aromatase inhibitors, and oral estrogens, including combined hormonal contraception (Table 2) 11.
Table 2. Medications Associated with Female Sexual Dysfunction
| Type of dysfunction | ||||
|---|---|---|---|---|
| Medication | Desire disorder | Arousal disorders | Orgasm disorders | |
Amphetamines and related anorectic medications | + | |||
Anticholinergics | + | |||
Antihistamines | + | |||
Cardiovascular and antihypertensive medications | ||||
Antilipids | + | |||
Beta blockers | + | |||
Clonidine | + | + | ||
Digoxin | + | + | ||
Methyldopa | + | |||
Spironolactone | + | |||
Hormonal preparations | ||||
Antiandrogens | + | + | + | |
Danazol | + | |||
Gonadotropin-releasing hormone agonists | + | |||
Gonadotropin-releasing hormone analogues | + | + | ||
Hormonal contraceptives | + | |||
Tamoxifen | + | + | ||
Ultra-low-potency contraceptives | + | + | ||
Narcotics | + | |||
Psychotropics | ||||
Antipsychotics | + | + | ||
Barbiturates | + | + | + | |
Benzodiazepines | + | + | ||
Lithium | + | + | + | |
Monoamine oxidase inhibitors | ||||
Selective serotonin reuptake inhibitors | + | + | + | |
Trazodone | + | |||
Tricyclic antidepressants | + | + | + | |
Venlafaxine | + | |||
Other | ||||
Aromatase inhibitors | + | + | ||
Chemotherapeutic agents | + | + | ||
Histamine H2 blockers and promotility agents | + | |||
Indomethacin | + | |||
Ketoconazole | + | |||
Phenytoin (Dilantin) | + | |||
Risk Factors for Female Sexual Dysfunction
While sexual dysfunction is wide spread in America, it is more common in particular groups of women.
Factors associated with sexual dysfunction in women include:
- History of sexual assault, rape or sexual coercion. This may be linked to post-traumatic stress disorder
- Pregnancy
- Childbirth in the past year
- Breastfeeding
- Menopause
- Urinary incontinence
- Vaginal prolapse
- Coronary heart disease (coronary artery disease)
- Hypertension, and hypertension medications
- Liver or kidney failure
- Cancer
- Spinal cord injury
- Neurological conditions, such as multiple sclerosis
- Depression, and antidepressant medications
- Relationship problems
- Stress
- Depression or anxiety
- Emotional or psychological stress, especially with regard to your relationship with your partner
- Fatigue
- Previous gynecological surgery, including hysterectomy and vault prolapse surgery
The most common psychological factors impacting female sexual function are depression, anxiety, distraction, negative body image, sexual abuse, and emotional neglect. Common contextual or sociocultural factors that cause or maintain sexual dysfunction include relationship discord, partner sexual dysfunction (e.g., erectile dysfunction), life stage stressors (e.g., transition into retirement, children leaving home), and cultural or religious messages that inhibit sexuality 12.
Recently, Schwarz et al 13 reported a high correlation between women with sexual dysfunction and chronic compensated heart failure. This report showed that 87% of middle-aged women with heart failure reported some degree of sexual dysfunction. More specifically, 80% of these patients reported reduced lubrication that resulted in frequent unsuccessful intercourse (76%) and 63% of the same population had difficulties achieving an orgasm. Indeed, the prevalence of sexual dysfunction in women with chronic compensated heart failure suggests a reduction in quality of life.
Sexual dysfunction associated with cancer
Between 10 and 88% of patients diagnosed with cancer experience sexual problems following diagnosis and treatment. The prevalence varies according to the location and type of cancer, and the treatment modalities used. Sexuality may be affected by chemotherapy, alterations in body image due to weight change, hair loss or surgical disfigurement, hormonal changes, and cancer treatments that directly affect the pelvic region.
Sexual problems are reported in many patients with breast and gynecological (e.g. cervical or vulval) cancer. They are also reported in patients with cancer that does not directly effect sexual organs, including lung cancer (48% of patients), Hodgkin’s disease (50%), and laryngeal (60%) and head and neck cancers (39-74%).
It is uncertain how they influence sexual function, but you may also have an increased risk if female sexual dysfunction if you have:
- Previous posterior vaginal repair
- Diabetes mellitus
- Oral contraceptive use.
Recent studies have demonstrated that diabetic women experience increased incidences of sexual dysfunction 14, including reduced sex drive, little to no arousal, vaginal dryness, difficulty in achieving orgasm and overall diminished sexual satisfaction 15. Despite these observations, correlation between female sexual dysfunction and diabetes is not without controversy. A report on the frequency of psychosexual difficulties from diabetic women found secondary sexual dysfunction was reported in 73.3% of diabetic women, however no direct association between sexual disorders and diabetic complications were found 16. These authors concluded that, in diabetic women, sexual dysfunction was prominently a psychogenic complication.
Female sexual dysfunction symptoms
Your symptoms will depend on the type or types of female sexual dysfunction you have:
- Low sexual desire. This most common of female sexual dysfunctions involves a lack of sexual interest and willingness to be sexual.
- Sexual arousal disorder. Your desire for sex might be intact, but you have difficulty with arousal or are unable to become aroused or maintain arousal during sexual activity.
- Orgasmic disorder. You have persistent or recurrent difficulty in achieving orgasm after sufficient sexual arousal and ongoing stimulation.
- Sexual pain disorder. You have pain associated with sexual stimulation or vaginal contact.
Female sexual interest/arousal disorder
The Diagnostic and Statistical Manual of Mental Disorders, 5th ed. (DSM-5), combines hypoactive sexual desire disorder and female sexual arousal disorder into a single disorder: female sexual interest/arousal disorder 17. Whereas sexual desire is the motivation to have sex, sexual arousal refers to the physiologic processes of arousal, including vaginal lubrication and genital warmth related to blood flow. Women commonly report experiencing these as part of the same process 18. The DSM-5 criteria for female sexual interest/arousal disorder are presented in Table 3 17.
It is important to determine whether the your problem with desire or arousal is a dysfunction or a normal variation of sexual response. The following examples are not considered sexual dysfunction: a woman reports little or no spontaneous desire but continues to experience responsive desire; a woman maintains spontaneous or responsive desire but reports a desire discrepancy between herself and her partner; a woman has reduced physiologic sexual arousal (e.g., decreased vaginal lubrication or genital blood flow) related to menopausal transition.
Table 3. DSM-5 Criteria for Female Sexual Interest/Arousal Disorder
A. Lack of, or significantly reduced, sexual interest/arousal, as manifested by at least three of the following: | |
1. Absent/reduced interest in sexual activity. | |
2. Absent/reduced sexual/erotic thoughts or fantasies. | |
3. No/reduced initiation of sexual activity, and typically unreceptive to a partner’s attempts to initiate. | |
4. Absent/reduced sexual excitement/pleasure during sexual activity in almost all or all (approximately 75%–100%) sexual encounters (in identified situational contexts or, if generalized, in all contexts). | |
5. Absent/reduced sexual interest/arousal in response to any internal or external sexual/erotic cues (e.g., written, verbal, visual). | |
6. Absent/reduced genital or nongenital sensations during sexual activity in almost all or all (approximately 75%–100%) sexual encounters (in identified situational contexts or, if generalized, in all contexts). | |
B. The symptoms in Criterion A have persisted for a minimum duration of approximately 6 months. | |
C. The symptoms in Criterion A cause clinically significant distress in the individual. | |
D. The sexual dysfunction is not better explained by a nonsexual mental disorder or as a consequence of severe relationship distress (e.g., partner violence) or other significant stressors and is not attributable to the effects of a substance/medication or another medical condition. | |
Specify whether: | |
Lifelong: The disturbance has been present since the individual became sexually active. | |
Acquired: The disturbance began after a period of relatively normal sexual function. | |
Specify whether: | |
Generalized: Not limited to certain types of stimulation, situations, or partners. | |
Situational: Only occurs with certain types of stimulation, situations, or partners. | |
Specify current severity | |
Mild: Evidence of mild distress over the symptoms in Criterion A. | |
Moderate: Evidence of moderate distress over the symptoms in Criterion A. | |
Severe: Evidence of severe or extreme distress over the symptoms in Criterion A. | |
Female Orgasmic Disorder
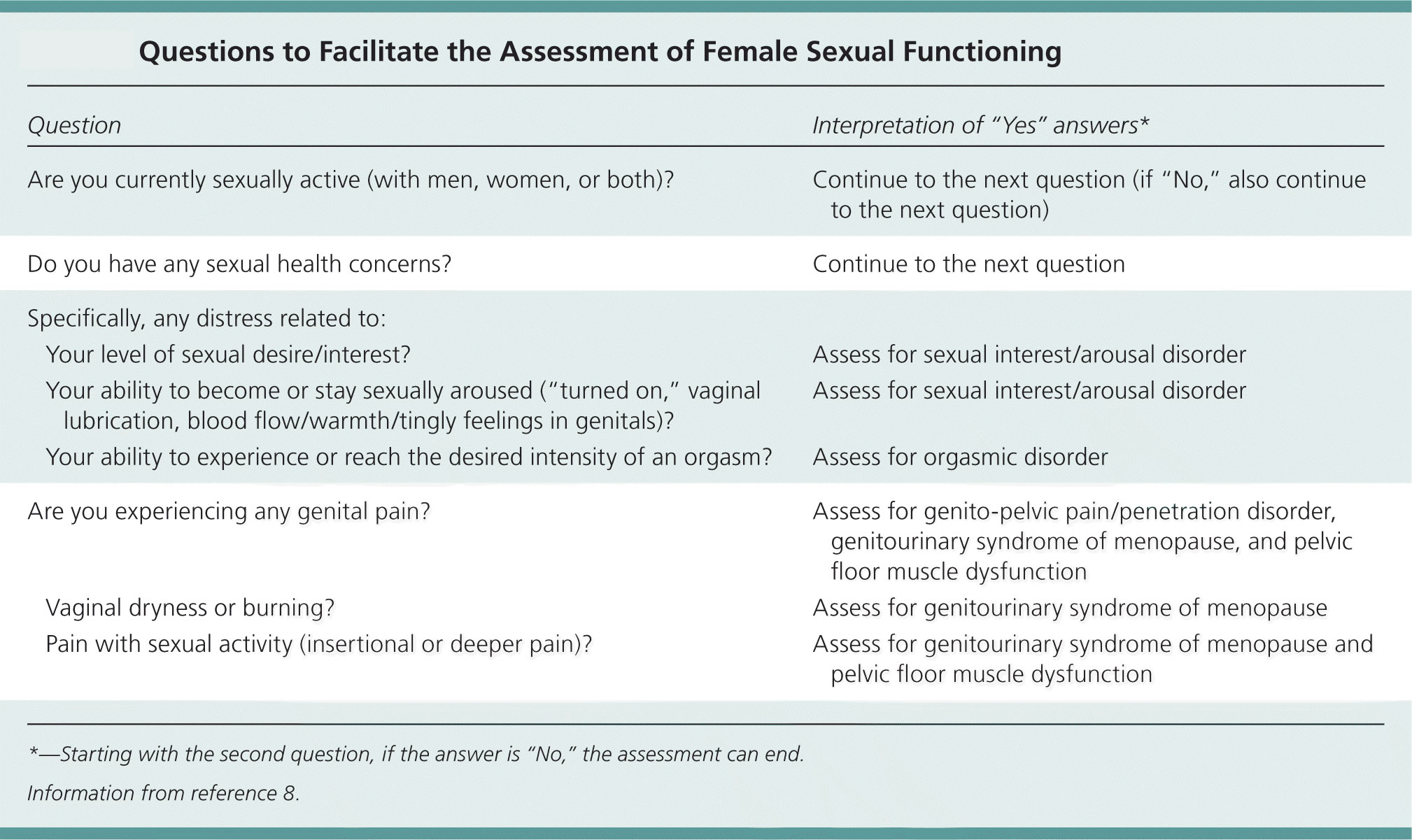
DSM-5 criteria for female orgasmic disorder include a marked delay in orgasm, infrequency or absence of orgasm, or less intense orgasm for at least six months in 75% to 100% of sexual interactions 17. Establishing the presence of orgasm is important, because many women may not know whether they have experienced orgasm 19. The next step is determining whether these problems are causing distress. About one-half of women who do not consistently reach orgasm during sexual activity do not report distress 20. If distress exists, the assessment follows the biopsychosocial model with the addition of several key questions that will assist in treatment planning: Is this a change in previous orgasmic functioning? Does this difficulty occur during self-stimulation, partnered sexual activity, or both? Does this difficulty occur across different sexual activities (e.g., oral, manual, vaginal penetration) and with different sex partners? (see Female sexual dysfunction diagnosis questionnaire below including Figure 2)
Orgasmic difficulties may be lifelong (present since sexual debut) or acquired (starting after a period of no dysfunction). Lifelong anorgasmia may suggest the patient is unfamiliar or uncomfortable with self-stimulation or sexual communication with her partner, or lacks adequate sex education 21. Delayed or less intense orgasms may be related to decreased genital blood flow and dulled genital sensations occurring naturally with aging. These examples are not considered sexual dysfunction.
The clinician should determine whether orgasmic difficulties occur only with certain types of stimulation, situations, or partners. If the patient reports difficulty during partnered sexual activity but not with self-stimulation, it may be the result of inadequate sexual stimulation 19. Biological factors requiring assessment and treatment include medical conditions and use of medications that impact sexual functioning 19.
Genito-Pelvic Pain/Penetration Disorder
In the DSM-5, vaginismus and dyspareunia are combined in genito-pelvic pain/penetration disorder. This disorder of sexual pain is defined as fear or anxiety, marked tightening or tensing of the abdominal and pelvic muscles, or actual pain with vaginal penetration that is persistent or recurrent for at least six months. This may be lifelong or acquired after a period of no dysfunction 17. The clinician should determine if the pain occurs with initial vaginal penetration, deeper penetration, or both.
Female sexual dysfunction diagnosis
Assessment of female sexual dysfunction is best approached using a biopsychosocial model (Figure 2), and should include a sexual history and physical examination. Table 4 includes important questions to ask patients during a sexual functioning assessment 22.
To diagnose female sexual dysfunction, your doctor will:
- Discuss your sexual and medical history. You might be uneasy talking with your doctor about such personal matters, but your sexuality is a key part of your well-being. An accurate diagnosis of female sexual dysfunction requires a thorough medical and sexual history. Issues such as sexual preference, domestic violence, fears of pregnancy, human immunodeficiency virus, and sexually transmitted diseases must be discussed. In addition, specific details of the actual dysfunction, identifying causes, medical or gynecologic conditions, and psychosocial information must be obtained. Female sexual dysfunction is often multifactorial, and the presence of more than one dysfunction should be ascertained. Patients may be able to provide insight into the cause or causes of the problem; however, various tools are available to assist with obtaining a good sexual history. The Female Sexual Function Index is one such example 23. This questionnaire contains 19 questions and categorizes sexual dysfunction in the domains of desire, arousal, lubrication, orgasm, satisfaction, and pain. The FSFI and other similar questionnaires can be filled out before the appointment time to expedite the process. The more forthcoming you can be about your sexual history and current problems, the better your chances of finding an effective approach to treating them. To get a copy of the Female Sexual Function Index Questionnaire please go here: http://www.fsfiquestionnaire.com/FSFI%20questionnaire2000.pdf
- Perform a pelvic exam. During the exam, your doctor checks for physical changes that affect your sexual enjoyment, such as thinning of your genital tissues, decreased skin elasticity, scarring or pain.
Your doctor may also refer you to a counselor or therapist specializing in sexual and relationship problems.
Figure 2. Biopsychosocial model of female sexual dysfunction
[Source 22]Table 4. Questions to Facilitate the Assessment of Female Sexual Functioning
| Question | Interpretation of “Yes” answers* | |
|---|---|---|
Are you currently sexually active (with men, women, or both)? | Continue to the next question (if “No,” also continue to the next question) | |
Do you have any sexual health concerns? | Continue to the next question | |
Specifically, any distress related to: | ||
Your level of sexual desire/interest? | Assess for sexual interest/arousal disorder | |
Your ability to become or stay sexually aroused (“turned on,” vaginal lubrication, blood flow/warmth/tingly feelings in genitals)? | Assess for sexual interest/arousal disorder | |
Your ability to experience or reach the desired intensity of an orgasm? | Assess for orgasmic disorder | |
Are you experiencing any genital pain? | Assess for genito-pelvic pain/penetration disorder, genitourinary syndrome of menopause, and pelvic floor muscle dysfunction | |
Vaginal dryness or burning? | Assess for genitourinary syndrome of menopause | |
Pain with sexual activity (insertional or deeper pain)? | Assess for genitourinary syndrome of menopause and pelvic floor muscle dysfunction | |
*—Starting with the second question, if the answer is “No,” the assessment can end.
Female sexual dysfunction treatment
Keep in mind that sexual dysfunction is a problem only if it bothers you. If it doesn’t bother you, there’s no need for treatment.
Because female sexual dysfunction has many possible symptoms and causes, treatment varies. It’s important for you to communicate your concerns and understand your body and its normal sexual response. Also, your goals for your sex life are important in determining treatment and evaluating progress.
Women with sexual concerns most often benefit from a combined treatment approach that addresses medical as well as relationship and emotional issues.
Nonmedical treatment for female sexual dysfunction
To treat sexual dysfunction, your doctor might recommend that you start with these strategies:
- Talk and listen. Open communication with your partner makes a world of difference in your sexual satisfaction. Even if you’re not used to talking about your likes and dislikes, learning to do so and providing feedback in a nonthreatening way sets the stage for greater intimacy.
- Practice healthy lifestyle habits. Go easy on alcohol — drinking too much can blunt your sexual responsiveness. Be physically active — regular physical activity can increase your stamina and elevate your mood, enhancing romantic feelings. Learn ways to decrease stress so you can focus on and enjoy your sexual experience.
- Seek counseling. Talk with a counselor or therapist who specializes in sexual and relationship problems. Therapy often includes education about how to optimize your body’s sexual response, ways to enhance intimacy with your partner, and recommendations for reading materials or couples exercises.
- Use a lubricant. A vaginal lubricant may be helpful during intercourse if you have vaginal dryness or pain during sex.
- Try a device. Arousal may be enhanced with stimulation of the clitoris. Use a vibrator to provide clitoral stimulation. Although some women find clitoral vacuum suction devices helpful for enhancing sexual arousal, those devices can be expensive and no more effective than a vibrator.
Female sexual dysfunction medication
Effective treatment for sexual dysfunction often requires addressing an underlying medical condition or hormonal change. A prescription medication for premenopausal women with low sexual desire, known as flibanserin (Addyi), also offers a treatment option.
To treat sexual dysfunction tied to a medical condition, your doctor might recommend that you:
- Adjust or change medication that has sexual side effects
- Treat a thyroid problem or other hormonal condition
- Optimize treatment for depression or anxiety
- Try strategies for relieving pelvic pain or other pain problems
Treating female sexual dysfunction linked to a hormonal cause might include:
- Estrogen therapy. Localized estrogen therapy comes in the form of a vaginal ring, cream or tablet. This therapy benefits sexual function by improving vaginal tone and elasticity, increasing vaginal blood flow and enhancing lubrication.
- Androgen therapy. Androgens include testosterone. Testosterone plays a role in healthy sexual function in women as well as men, although women have much lower amounts of testosterone.
- Androgen therapy for sexual dysfunction is controversial. Some studies show a benefit for women who have low testosterone levels and develop sexual dysfunction; other studies show little or no benefit.
The risks of hormone therapy may vary, depending on whether estrogen is given alone or with a progestin, your age, the dose and type of hormone, and health issues such as your risks of heart and blood vessel disease and cancer. Talk with your doctor about benefits and risks. In some cases, hormonal therapy might require close monitoring by your doctor.
Flibanserin (Addyi)
Originally developed as an antidepressant, flibanserin (Addyi) is approved by the Food and Drug Administration as a treatment for low sexual desire in premenopausal women.
A daily pill, Addyi may boost sex drive in women who experience low sexual desire and who find the experience distressing. Potentially serious side effects include low blood pressure, sleepiness, nausea, fatigue, dizziness and fainting, particularly if the drug is mixed with alcohol. Experts recommend that you stop taking the drug if you don’t notice an improvement in your sex drive after eight weeks.
Menopause
Sexual health concerns are common in natural or surgically induced menopause, particularly sexual pain related to genitourinary syndrome of menopause. A Cochrane review showed that hormone therapy (estrogen alone or in combination with a progestogen) was associated with a small to moderate improvement in sexual function, especially pain, in symptomatic or early menopausal women 24. Estrogen treatment is highly effective for genitourinary syndrome of menopause and related dyspareunia; local vaginal estrogen is preferred if vaginal dryness is the primary concern 25. Ospemifene (Osphena) is a selective estrogen receptor modulator that has been shown to improve the vaginal maturation index, vaginal pH, and symptoms of vaginal dryness 26. The U.S. Food and Drug Administration (FDA) has approved it for treatment of moderate to severe dyspareunia. The route of administration of estrogen can impact sexual function. Oral estrogens increase sex hormone–binding globulin, which reduces available free testosterone and may thereby adversely impact sexual function, whereas transdermal estrogens have no such effect 11.
Women with genitourinary syndrome of menopause and sexual pain may have dysfunctional pelvic floor muscles, which may become tense or tight as a result of ongoing vaginal dryness and discomfort or pain with sexual activity 27. Pelvic floor physical therapy may benefit these women 27.
Randomized controlled trials involving naturally or surgically menopausal women with low sexual desire or arousal have shown improvements in sexual function with transdermal testosterone therapy (with or without concomitant estrogen therapy) 28. However, overall, data on the benefit of testosterone therapy are limited and inconsistent 29. The Endocrine Society suggests considering a three- to six-month trial of testosterone therapy for postmenopausal women with low sexual desire associated with distress. However, because of the lack of long-term data on safety and effectiveness, it does not recommend routine testosterone treatment for women with low androgen levels related to hypopituitarism, bilateral oophorectomy, or adrenal insufficiency 29. Testosterone therapy is not FDA-approved for use in women, and using testosterone formulations made for men is discouraged. If therapy is initiated, clinical evaluation and laboratory monitoring of testosterone levels are suggested to evaluate for overuse and signs of hyperandrogenism (e.g., acne, hair growth) 29.
Hypoactive Sexual Desire
Desire disorders are often multifactorial and may be difficult to treat effectively. For many women, lifestyle issues such as finances, careers, and family commitments may greatly contribute to the problem. In addition, medications or another type of sexual dysfunction (i.e., pain) may contribute to the dysfunction. Individual or couple counseling may be of benefit because there is no medical treatment geared toward this specific disorder.
Hormone replacement therapy can affect sexual desire. Estrogen may benefit menopausal or perimenopausal women. It can enhance clitoral sensitivity, increase libido, improve vaginal atrophy, and decrease dyspareunia. In addition, estrogen can improve vasomotor symptoms, mood disorders, and symptoms of urinary frequency and urgency 30. Progesterone is necessary for women with intact uterus using estrogen; however, it may negatively affect mood and contribute to decreased sexual desire.
Testosterone appears to directly influence sexual desire, but data are controversial regarding its replacement in androgen-deficient premenopausal women. Indications for testosterone replacement include premature ovarian failure, symptomatic premenopausal testosterone deficiency, and symptomatic postmenopausal testosterone deficiency (includes natural, surgical, or chemotherapy-induced deficiency) 30. Currently, however, there is no national guideline for testosterone replacement in women with sexual dysfunction. In addition, there is no consensus regarding what are considered normal or therapeutic levels of testosterone therapy for women 31.
Before initiating therapy, potential side effects and risks of treatment should be discussed. Androgenic side effects can occur in 5% to 35% of women taking testosterone and they include acne, weight gain, hirsutism, clitorimegaly, deepening of the voice, and lowering of high-density lipoprotein cholesterol 32. Baseline levels of lipids, testosterone (free and total), and liver function enzymes should be obtained in addition to a mammogram and Pap smear if indicated.
Postmenopausal women may benefit from 0.25 to 2.5 mg of methyltestosterone (Android, Methitest, Testred, Virilon) or up to 10 mg of micronized oral testosterone. Doses are adjusted according to symptom control and side effects. Methyltestosterone is also available in combination with estrogen (Estratest, Estratest HS). Some women may benefit from topical methyltestosterone or testosterone propionate compounded with petroleum jelly in a 1% to 2% formula. This ointment can be applied up to three times per week 33. It is important to periodically monitor liver function, lipids, testosterone levels, and androgenic side effects during treatment.
There are various over-the-counter herbal products that advertise improvement in female sexual dysfunction and restoration of hormone levels. Although evidence is conflicting, many of these products lack sufficient scientific studies required to support the manufacturer’s claims of efficacy and safety 34. Patients should be cautioned about the potential for side effects and drug-to-drug interactions with these products.
Tibolone is a synthetic steroid with tissue-specific estrogenic, progestogenic and androgenic properties. It has been used in Europe for the past 20 years in the prevention of postmenopausal osteoporosis and in the treatment of menopausal symptoms, including sexual dysfunction. It is not yet available in the United States, but is actively being studied 35.
Sexual Pain Disorder
Sexual pain can be classified as superficial, vaginal, or deep. Superficial pain is often caused by vaginismus, anatomic abnormalities, or irritative conditions of the vaginal mucosa. Vaginal pain can be caused by friction as a result of inadequate lubrication. Deep pain can be muscular in nature or associated with pelvic disease 31. The type(s) of pain a woman experiences can dictate therapy, thereby making an aggressive approach to an accurate diagnosis imperative. The use of lubricants, vaginal estrogens, topical lidocaine, moist heat to the genital area, NSAIDs, physical therapy, and positional changes may help to minimize discomfort during intercourse. Sex therapy may benefit women with vaginismus because it is often triggered by a history of sexual abuse or trauma.
Sexual Arousal Disorder
Inadequate stimulation, anxiety, and urogenital atrophy may contribute to arousal disorder. A pilot study of 48 women with arousal disorder showed that sildenafil (Viagra) significantly improved subjective and physiologic parameters of the female sexual response 36. Other treatment options for arousal disorder include lubricants, vitamin E and mineral oils, increased foreplay, relaxation, and distraction techniques. Estrogen replacement may benefit postmenopausal women, because urogenital atrophy is one of the most common causes of arousal disorder in this age group.
Orgasmic Disorder
Women with orgasmic disorders often respond well to therapy. Sex therapists encourage women to enhance stimulation and minimize inhibition. Pelvic muscle exercises can improve muscle control and sexual tension, whereas the use of masturbation and vibrators can increase stimulation. The use of distraction (i.e., background music, fantasy, and so forth, can also help minimize inhibition) 33.
Potential treatments that need more research
More research is needed before these agents might be recommended for treatment of female sexual dysfunction:
Tibolone. Tibolone is a synthetic steroid drug used in Europe and Australia for treatment of postmenopausal osteoporosis. Due to concerns over increased risk of breast cancer and stroke in women taking tibolone, the drug isn’t approved by the Food and Drug Administration for use in the U.S.
Phosphodiesterase inhibitors. This group of medications has proved successful in treating erectile dysfunction in men, but the drugs don’t work nearly as well in treating female sexual dysfunction. Studies looking into the effectiveness of these drugs in women show inconsistent results.
One drug, sildenafil (Viagra), may prove beneficial for some women who have sexual dysfunction as a result of taking selective serotonin reuptake inhibitors (SSRIs), a class of drugs used to treat depression. Don’t take sildenafil if you use nitroglycerin for angina — a type of chest pain caused by reduced blood flow to the heart.
Issues surrounding female sexual dysfunction are usually complex, so even the best medications aren’t likely to work if other emotional or social factors remain unresolved.
Lifestyle and home remedies
To boost your sexual health, find ways to be comfortable with your sexuality, improve your self-esteem and accept your body. Try practicing these healthy lifestyle habits:
- Avoid excessive alcohol. Drinking too much blunts sexual responsiveness.
- Don’t smoke. Cigarette smoking restricts blood flow throughout your body. Less blood reaches your sexual organs, which means you could experience decreased sexual arousal and orgasmic response.
- Be physically active. Regular aerobic exercise increases your stamina, improves your body image and elevates your mood. This can help you feel more romantic, more often.
- Make time for leisure and relaxation. Learn ways to decrease stress, and allow yourself to relax amid the stresses of your daily life. Being relaxed can enhance your ability to focus on your sexual experiences and may help you attain more satisfying arousal and orgasm.
Alternative medicine
More research is needed, but promising therapies for improving sexual satisfaction include:
- Mindfulness. This type of meditation is based on having an increased awareness and acceptance of living in the present moment. You focus on what you experience during meditation, such as the flow of your breath. You can observe your thoughts and emotions but let them pass without judgment. Some research shows that mindfulness practiced during the course of group therapy improved many aspects of sexual response and reduced personal distress in women with desire and arousal disorders.
- Acupuncture. Acupuncture involves the insertion of extremely thin needles into your skin at strategic points on your body. Acupuncture may have positive effects on women with certain sexual dysfunctions, but more study is needed.
- Yoga. During yoga, you perform a series of postures and controlled breathing exercises to promote a flexible body and a calm mind. Certain subsets of yoga aim to channel the body’s sexual energy and improve sexual functioning. Very little data exist on the benefits of yoga on sexual functioning. However, the practice of yoga is associated with improved psychological well-being and overall health.
Coping and support
At each stage of your life, you may experience changes in sexual desire, arousal and satisfaction. To better adapt:
- Understand your body and what makes for a healthy sexual response. The more you and your partner know about the physical aspects of your body and how it functions, the better able you’ll be to find ways to ease sexual difficulties.
- Gather information. Ask your doctor or look for educational materials to learn how issues such as aging, illnesses, pregnancy, menopause and medicines might affect your sex life.
- Communicate openly with your partner. Be flexible in your approach to intimacy with your partner. Continue to engage in the areas of intimacy that are working well for the two of you.
- Accept changes that occur. Explore new aspects of your sexuality during times of transition to improve your sexual experiences.
Sexual response often has as much to do with your feelings for your partner as it does with physical sexual stimuli. Reconnect and discover each other again.
- Female sexual dysfunction. https://www.mayoclinic.org/diseases-conditions/female-sexual-dysfunction/symptoms-causes/syc-20372549[↩]
- Allahdadi KJ, Tostes RCA, Webb RC. Female Sexual Dysfunction: Therapeutic Options and Experimental Challenges. Cardiovascular & hematological agents in medicinal chemistry. 2009;7(4):260-269. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3008577/[↩]
- Berman JR, Berman L, Goldstein I: Female sexual dysfunction: Incidence, pathophysiology, evaluation, and treatment options. Urology 1999; 54:385-391.[↩][↩]
- Laumann EO, Paik A, Rosen RC: Sexual dysfunction in the United States: Prevalence and predictors. JAMA 1999;281:537-544.[↩]
- Basson R, Berman JR, Burnett A, et al: Report of the international consensus development conference on female sexual dysfunction: Definitions and classifications. J Urol 2000;163:888-893.[↩]
- Park K, Moreland RB, Goldstein I, et al: Sildenafil inhibits phosphodiesterase type 5 in human clitoral corpus cavernosum smooth muscle. Biochem Biophys Res Commun 1998;249:612-617.[↩]
- Brotto L, Luria M. Sexual interest/arousal disorder in women. In: Binik Y, Hall KS, eds. Principles and Practice of Sex Therapy. 5th ed. New York, NY: Guilford Press; 2014:17–41.[↩]
- Clayton AH, Groth J. Etiology of female sexual dysfunction. Womens Health (Lond Engl). 2013;9(2):135–137.[↩]
- Bitzer J, Giraldi A, Pfaus J. Sexual desire and hypoactive sexual desire disorder in women. Introduction and overview. Standard operating procedure (SOP Part 1). J Sex Med. 2013;10(1):36–49.[↩][↩]
- Kingsberg SA, Rezaee RL. Hypoactive sexual desire in women. Menopause. 2013;20(12):1284–1300.[↩][↩][↩][↩]
- Buster JE. Managing female sexual dysfunction. Fertil Steril. 2013;100(4):905–915.[↩][↩][↩]
- Brotto LA, Bitzer J, Laan E, Leiblum S, Luria M. Women’s sexual desire and arousal disorders [published correction appears in J Sex Med. 2010;7(2 pt 1):856]. J Sex Med. 2010;7(1 pt 2):586–614.[↩]
- The prevalence and clinical relevance of sexual dysfunction in women and men with chronic heart failure. Schwarz ER, Kapur V, Bionat S, Rastogi S, Gupta R, Rosanio S. Int J Impot Res. 2008 Jan-Feb; 20(1):85-91. https://www.ncbi.nlm.nih.gov/pubmed/17882230/[↩]
- Olarinoye J, Olarinoye A. Determinants of sexual function among women with type 2 diabetes in a Nigerian population. J Sex Med. 2008;5:878. https://www.ncbi.nlm.nih.gov/pubmed/18069996[↩]
- Fatemi SS, Taghavi SM. Evaluation of sexual function in women with type 2 diabetes mellitus. Diab Vasc Dis Res. 2009;6:38. https://www.ncbi.nlm.nih.gov/pubmed/19156627[↩]
- Newman AS, Bertelson AD. Sexual dysfunction in diabetic women. J Behav Med. 1986;9:261. https://www.ncbi.nlm.nih.gov/pubmed/3746898[↩]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.[↩][↩][↩][↩][↩]
- Carvalheira AA, Brotto LA, Leal I. Women’s motivations for sex: exploring the diagnostic and statistical manual, fourth edition, text revision criteria for hypoactive sexual desire and female sexual arousal disorders. J Sex Med. 2010;7(4 pt 1):1454–1463.[↩]
- Graham C. Orgasm disorders in women. In: Binik YM, Hall KS, eds. Principles and Practice of Sex Therapy. 5th ed. New York, NY: Guilford Press; 2014:89–111.[↩][↩][↩]
- Shifren JL, Monz BU, Russo PA, Segreti A, Johannes CB. Sexual problems and distress in United States women: prevalence and correlates. Obstet Gynecol. 2008;112(5):970–978.[↩]
- Laan E, Rellini AH, Barnes T; International Society for Sexual Medicine. Standard operating procedures for female orgasmic disorder: consensus of the International Society for Sexual Medicine. J Sex Med. 2013;10(1):74–82.[↩]
- Latif EZ, Diamond MP. Arriving at the diagnosis of female sexual dysfunction. Fertil Steril. 2013;100(4):898–904.[↩][↩][↩]
- Rosen R: The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 2000; 26:191-208.[↩]
- Nastri CO, Lara LA, Ferriani RA, Rosa-E-Silva AC, Figueiredo JB, Martins WP. Hormone therapy for sexual function in perimenopausal and post-menopausal women. Cochrane Database Syst Rev. 2013;(6):CD009672.[↩]
- Basson R, Wierman ME, van Lankveld J, Brotto L. Summary of the recommendations on sexual dysfunctions in women. J Sex Med. 2010;7(1 pt 2):314–326.[↩]
- Management of symptomatic vulvovaginal atrophy: 2013 position statement of The North American Menopause Society. Menopause. 2013;20(9):888–902.[↩]
- Rosenbaum TY. Musculoskeletal pain and sexual function in women. J Sex Med. 2010;7(2 pt 1):645–653.[↩][↩]
- Davis SR, Worsley R. Androgen treatment of postmenopausal women. J Steroid Biochem Mol Biol. 2014;142:107–114.[↩]
- Wierman ME, Arlt W, Basson R, et al. Androgen therapy in women: a reappraisal: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2014;99(10):3489–3510.[↩][↩][↩]
- Berman JR, Goldstein I: Female sexual dysfunction. Urol Clin North Am 2001;28:405-416.[↩][↩]
- Phillips NA. Female sexual dysfunction: Evaluation and treatment. Am Fam Physician 2000;62:127-136, 141-142.[↩][↩]
- Slayden SM: Risks of menopausal androgen supplementation. Semin Reprod Endocrinol 1998;16:145-152.[↩]
- Phillips NA: The clinical evaluation of dyspareunia. Int J Impot Res 1998;10(Suppl 2):S117-S120.[↩][↩]
- Aschenbrenner D: Avlimil taken for female sexual dysfunction. A J Nurs 2004;104:27-29.[↩]
- Modelska K, Cummings S: Female sexual dysfunction in postmenopausal women: Systematic review of placebo-controlled trials. Am J Obstet Gynecol 2003;188:286-293.[↩]
- Berman JR, Berman LA, Lin A, et al: Effect of sildenafil on subjective and physiologic parameters of the female sexual response in women with sexual arousal disorder. J Sex Marital Ther 2001;27:411-420.[↩]