Contents
What is hemifacial spasm
Hemifacial spasm is a neuromuscular movement disorder characterized by frequent involuntary contractions (spasms) of the muscles on one side of the face that are innervated by the facial nerve (cranial nerve 7). Hemifacial spasm prevalence has been estimated at 11 cases per 100,000 individuals 1. Hemifacial spasm occurs in both men and women, although it more frequently affects middle-aged or elderly women. Hemifacial spasm is much more common in the Asian population.
Hemifacial spasm has two forms: typical and atypical.
- In the typical hemifacial spasm, the twitching starts around the eye, usually the lower lid. As time progresses, the twitching spreads to include the whole lid, then the cheekbone area, then the lower jaw. As the progress is usually inexorable, the muscles in the neck become involved.
- In the atypical hemifacial spasm, the twitching starts in the lower face and progresses to involve the remainder of the facial muscles. It can sometimes be triggered by volitional contraction of certain facial muscles, especially puckering the lips or forcefully closing the eyes. Stressful situations or fatigue may also worsen the spasms.
The first symptom is usually an intermittent twitching of the eyelid muscle that can lead to forced closure of the eye. The spasm may then gradually spread to involve the muscles of the lower face, which may cause the mouth to be pulled to one side. Eventually the spasms involve all of the muscles on one side of the face almost continuously. Rarely, doctors see individuals with hemifacial spasm on both sides of the face. The prevalence of bilateral hemifacial spasm has been reported to be 2.6% of cases 2.
Although hemifacial spasm does not have life-threatening consequences, affected persons often suffer immensely and tend to increasingly withdraw socially. As a severe psychosocial stressor, hemifacial spasm requires timely diagnosis and therapy.
In contrast to other movement disorders, psychopathological abnormalities—for example, anxiety disorders—are no more common in patients with hemifacial spasm than in the normal population 3.
Hemifacial spasm may be caused by a facial nerve injury, or a tumor, or it may have no apparent cause. Most often hemifacial spasm is caused by a blood vessel pressing on the facial nerve at the place where it exits the brainstem. Hemifacial spasm is usually caused by an artery compressing the facial nerve at the root exit zone of the brainstem.
Untreated, hemifacial spasm symptoms will persist for life, and over time, the spasms are often progressive in terms of intensity and frequency, as well as area affected.
The therapeutic options for hemifacial spasm range from simple application of heat to medication treatment and botulinum injections to microvascular decompression surgery. 85–95% of patients obtain moderate or marked relief from local injections of botulinum toxin (botox), which must be repeated every 3 to 4 months. Alternatively, microvascular decompression has a success rate of about 85%. Drug therapy is generally not effective 4, 5. However, large studies are lacking that compare the possible therapeutic options in a randomized and controlled fashion.
Facial Nerve
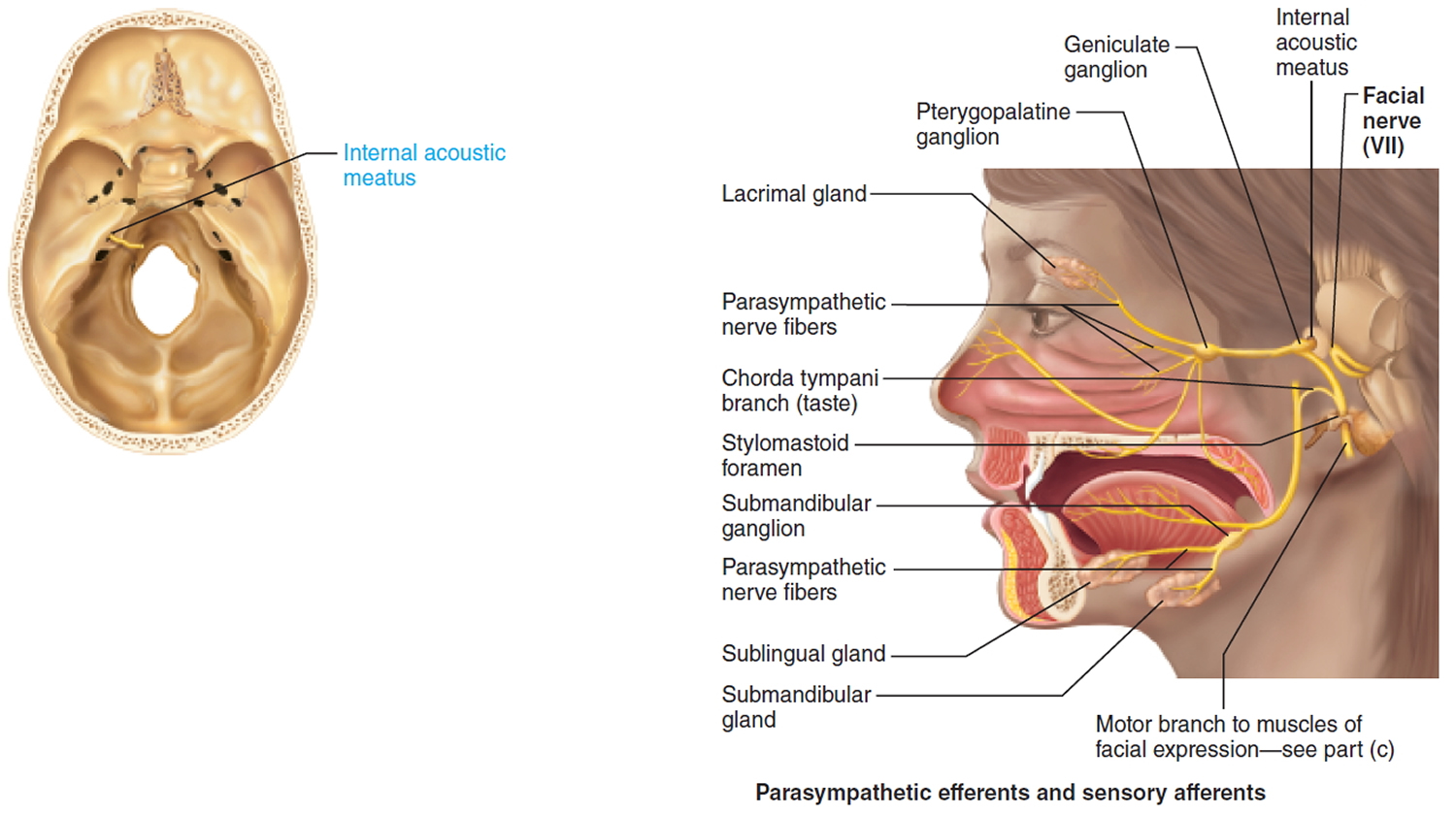
The facial nerve (cranial nerve 7) is a mixed nerve. Facial nerve is a chief somatic motor nerve to the facial muscles; parasympathetic innervation to glands; special sensory taste from the tongue.
Sensory function: Special visceral sensory from taste buds on anterior two-thirds of tongue. General somatic sensory from small patch of skin on the ear.
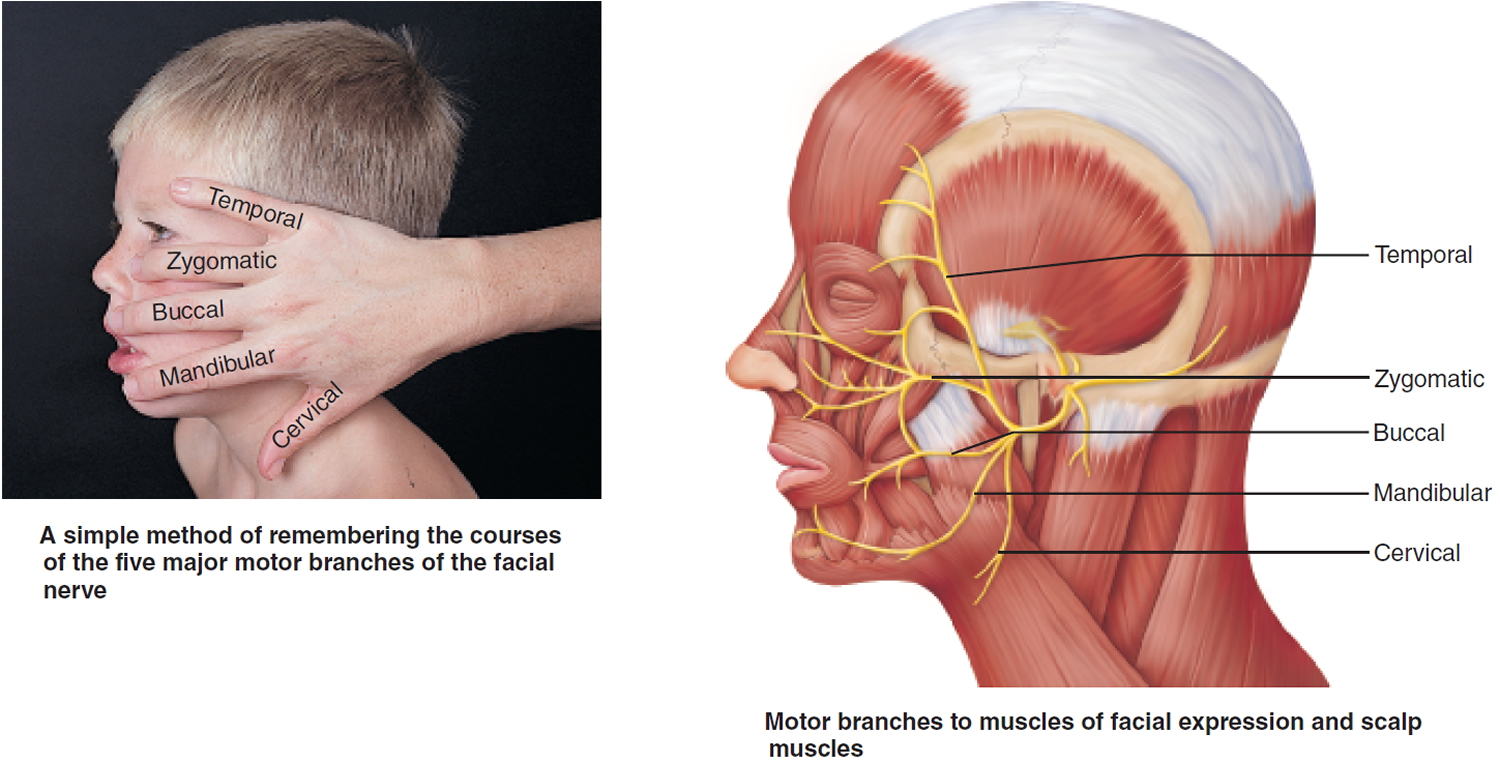
Somatic motor function: Five major branches on face: temporal, zygomatic, buccal, mandibular, and cervical, to innervate the facial muscles. Also innervates the posterior belly of digastric. Afferent proprioceptor fibers return from these muscles.
Visceral motor function (parasympathetic): Innervate the lacrimal (tear) glands, nasal and palatine glands, and the submandibular and sublingual salivary glands.
Origin: Fibers emerge from the pons, just lateral to abducens.
Pathway: Fibers enter the temporal bone via the internal acoustic meatus. Chorda tympani branches off to innervate the two salivary glands and tongue. Branch to facial muscles emerges from the temporal bone through the stylomastoid foramen and courses to lateral aspect of face. Cell bodies of sensory neurons are in geniculate ganglion. Cell bodies of postganglionic parasympathetic neurons are in pterygopalatine and submandibular ganglia on the trigeminal nerve
Figure 1. Facial nerve (Cranial nerve 7)
Hemifacial spasm prognosis
The prognosis for an individual with hemifacial spasm depends on the treatment and their response. Some individuals will become relatively free from symptoms with injection therapy. Some may require surgery. In most cases, a balance can be achieved, with tolerable residual symptoms.
Hemifacial spasm causes
The underlying cause of hemifacial spasm is in most cases an ectatic (dilated) or atypically aberrant blood vessel, which compresses the facial nerve at the place where it exits the brainstem 6. Pathoanatomically this so-called root-exit zone has some particular features: The nerve is ensheathed by an arachnoidal membrane only, without the epineurium. Furthermore, no connective tissue septa traverse the individual fascicles. This region is also the transition zone between central (oligodendroglial cells) and peripheral (Schwann cells) myelination 7. All the particular features result in increased vulnerability and therefore susceptibility to stimuli, such as compression.
The pathogenesis of hemifacial spasm by compression of the facial nerve is explained by using several theories. According to the “peripheral” hypothesis, ephaptic and ectopic excitations occur in the root-exit zone. The ephaptic impulse conduction is characterized by a pathological transfer of impulses between neighboring nerve fibers 8. Ectopic impulse conduction describes the spontaneous development of neural impulses in the compression area. By contrast, the “central” hypothesis assumes hyperexcitability of the facial motor nucleus in the brainstem 7. The explanation for patients’ relatively old age at disease onset is that in the course of life, progressive ectatic changes and elongations may affect the vessels in the cerebellopontine angle. This is particularly common in patients with arterial hypertension. Over time, this results in contact between vessel and nerve, which causes the compression. It is assumed that this leads in turn to focal demyelination, which leads to the electrophysiological processes mentioned above.
Further, albeit much rarer, causes of hemifacial spasm include all kinds of space-occupying lesions in the cerebellopontine angle—for example, Schwannomas, meningiomas, and arachnoidal cysts 9. Certain processes in the brainstem can also result in symptoms. These include gliomas, demyelinating neurological disorders such as multiple sclerosis (MS), or brainstem infarction. It has been reported that symptoms can also be triggered by Bell’s palsy owing to injury to the facial nerve 9.
Hemifacial spasm symptoms
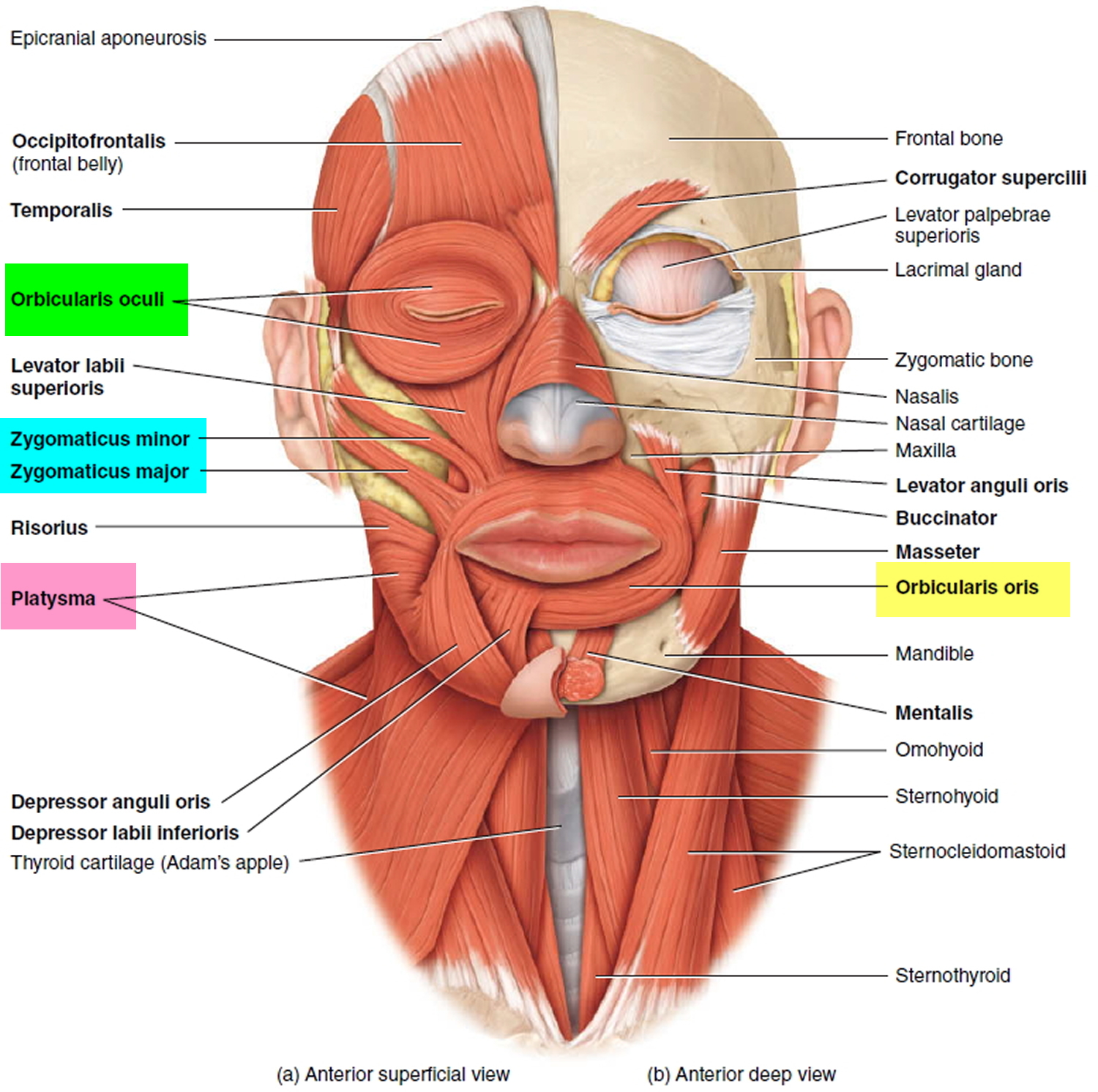
Hemifacial spasm is characterized by progressive, involuntary, irregular, clonic or tonic movements of the facial muscles innervated by the facial nerve (cranial nerve VII) 10. Typically, these symptoms are strictly unilateral. At disease onset, in many cases involuntary spasms occur in the region of the orbicularis oculi muscle, which then gradually extend into other parts of the affected half of the face. In pronounced cased, the platysma muscle is also affected (Figure 2). In most patients the symptoms persist during sleep 10. Some patients also complained of a “clicking” in the ear, which can be explained with contractions of the stapedius muscle.
Figure 2. Facial muscles (superficial and deep)
Figure 3. Hemifacial spasm – patient with pronounced right-sided hemifacial spasm and involvement of the platysma muscle is clearly visible
Patients with hemifacial spasm suffer primarily from the associated psychosocial stress. Furthermore, pronounced spasm of the orbicularis oculi muscle can impair bilateral vision, which is required for reading or driving 11. The symptoms are often accentuated by psychological tension and during speaking. In many patients, low-grade facial nerve paralysis develops after many years of hemifacial spasm.
Hemifacial spasm diagnosis
The clinical features are crucial to making a diagnosis of hemifacial spasm. To diagnose your condition, your doctor will conduct a physical examination and check for signs of hemifacial spasm. Your doctor may order imaging tests to diagnose your condition, determine the cause of your condition and develop the most appropriate treatment for your condition.
Your doctor may order electromyography (EMG) and a magnetic resonance imaging (MRI) tests. An MRI uses powerful magnets and radio waves to create detailed images of your head and determine the cause of your hemifacial spasm. Your doctor may inject a contrast dye into a blood vessel (magnetic resonance angiogram) to look for any abnormal blood vessel that may be irritating the facial nerve. MRI is also a useful modality to exclude pathological changes in the cerebellopontine angle, such as tumors or brainstem lesions. To display possible vascular compression, high-resolution, T2-weighted sequences are particularly useful—for example, an axial-plane CISS (constructive interference in steady state) sequence, since this yields images with a high contrast between cerebrospinal fluid, nerves, and vessels (Figure 4).
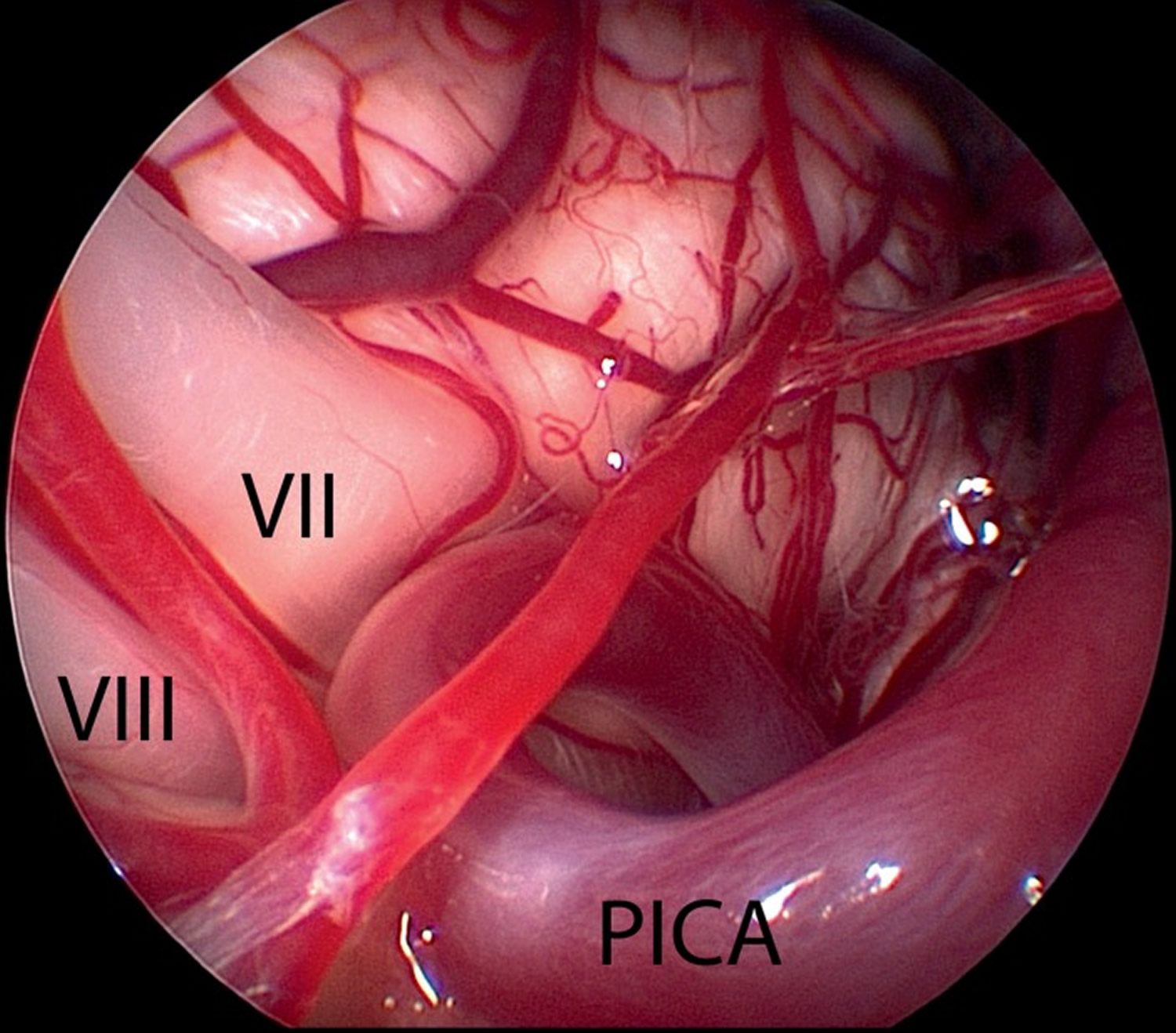
In most cases, the compression is caused by the inferior posterior cerebellar artery (PICA) or the inferior anterior cerebellar artery (AICA) 1. The compression is rarely caused by the vertebral artery (VA) or a combination of these arteries. In very rare cases, the compression can also be caused by a vein.
Figure 4. MRI showing a loop of the posterior inferior cerebellar artery (Arrow A) which compresses the facial nerve (Arrow B), where it exists the brainstem
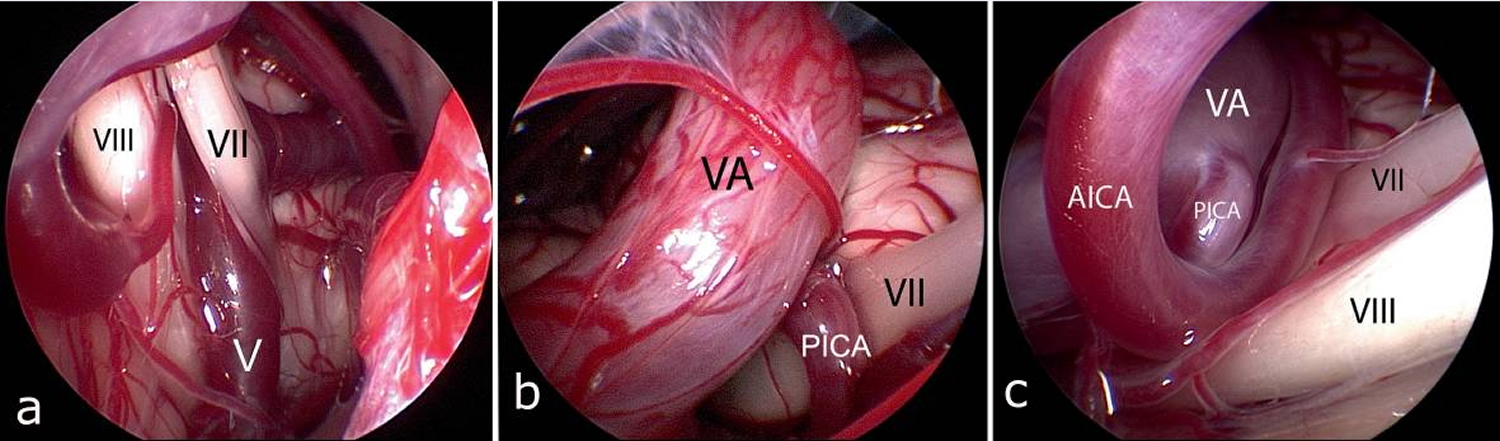
[Source 1]Figure 5. Endoscopic image showing facial nerve (VII) being compressed by a loop of the posterior inferior cerebellar artery (PICA) (same patient as in Figure 4 above) [VII = facial nerve, VIII = cochlear nerve]
[Source 1]Figure 6. Endoscopic image showing different forms of vascular compression of the facial nerve (VII) [VII = facial nerve, VIII = cochlear nerve]
Note:
(a) In this case the compression is caused by a vein (V) in close proximity to the brainstem (VII = facial nerve, VIII = cochlear nerve)
(b) Here, the compression is caused by a combination of the vertebral artery (VA) and posterior inferior cerebellar artery (PICA). (VII = facial nerve)
(c) The compression is caused by a combination of vertebral artery (VA), the descending posterior inferior cerebellar artery (PICA), and the anterior inferior cerebellar artery (AICA)
Hemifacial spasm treatment
Since hemifacial spasm has a low incidence and prevalence, large studies are lacking that compare the possible therapeutic options in a randomized and controlled fashion. An indication for treatment exists when a patient feels impaired in his/her quality of life by the disease or if functional impairments—for example, of the visual field—are present.
Local botox (botulinum-toxin) injection is a safe and well-tolerated symptomatic treatment for hemifacial spasm. In the long term, however, lasting relief can only be achieved by microvascular decompression, a microsurgical intervention with a relatively low risk and a high success rate.
Surgical treatment in the form of microvascular decompression, which relieves pressure on the facial nerve, will relieve hemifacial spasm in many cases. This intervention has significant potential side-effects, so risks and benefits have to be carefully balanced. Other treatments include injections of botulinum toxin into the affected areas, which is the most effective therapy and the only one used in most cases.
The drugs used to treat hemifacial spasm include carbamazepine, clonazepam, and baclofen, as well as newer anticonvulsive drugs, such as gabapentin. Reportedly, success has been poor, sporadic, and not sustained 5. For this reason, medication therapy has been assessed as unsatisfactory in most studies 4 and is used only for very mild forms of the disease. It should also be mentioned that some patients are notably affected by adverse effects, such as fatigue, exhaustion, and poor performance.
Botox for hemifacial spasm
Botulinum toxin (botox) is a neurotoxin that paralyses the muscles by irreversibly blocking the cholinergic signal transmission at the presynaptic nerve endings 12. Since the early 1980s it has been used for local injection therapy for hemifacial spasm. Since then botox treatment has become the standard symptomatic treatment for the condition. This treatment reportedly results in notable to moderate alleviation of symptoms in 85% to 95% of patients 13. Common adverse effects include temporary mild weakness of the face (23%), the occurrence of double vision (17%), headache, dry eye, and drooping of the eyelid or mouth (15%) 14. Nausea, allergic reactions, and antibodies to botox have been observed less often.
The crucial disadvantage of this treatment modality is its limited effectiveness; the injections have to be repeated at intervals of 3–4 months 13. The treatment is merely symptomatic. Furthermore, patients treated for many years have reported a reduction in the effectiveness of botox after a few years.
Altogether, however, botulinum injection is a minimally invasive option to alleviate the symptoms of hemifacial spasm that has few side effects and can be given on an outpatient basis.
For certain groups of patients, local botox injection is the only effective symptomatic treatment option. This is mainly the case when surgery is out of the question—for example, in patients put at high risk by anesthesia or those patients whose symptoms are not caused by vascular compression.
Hemifacial spasm surgery
Microvascular decompression surgery. In this surgery, your surgeon makes an opening in your skull and opens the covering of your brain (dura) to expose the facial nerve as it leaves the brainstem.
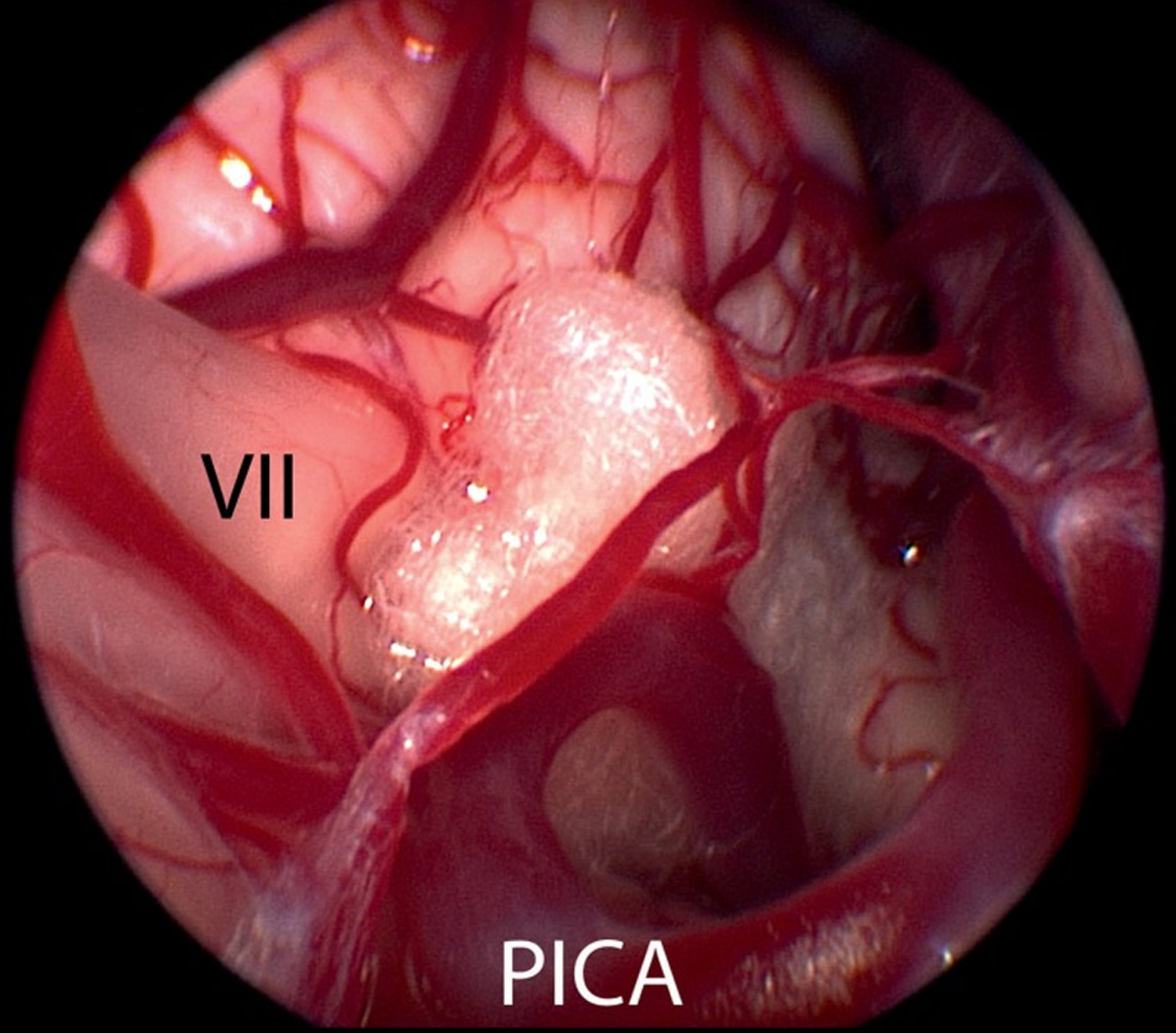
Your surgeon locates the blood vessel pressing on or irritating the facial nerve and puts a spongelike material between the nerve and blood vessel, removing the pressure on the nerve. This surgery often can relieve hemifacial spasm.
Figure 7. After microsurgical dissection of the vessel from the facial nerve, a teflon sponge is placed between brainstem and vessel, in order to permanently prevent vascular compression (VII = facial nerve, PICA = posterior inferior cerebellar artery)
[Source 1]The literature has reported an average success rate of the surgery of 80% to 88% within the first postoperative year 15. At follow-up, the success rate (that is, a reduction in spasms by more than 90%) was 83% at 6 months and 87% at 18 months. In patients with a small improvement in symptoms, or none at all, the reason for the lack of success was mostly individual anatomy, such as large-caliber veins or arteries running between the facial nerve and the vestibulocochlear nerve, or extremely elongated and ectatic vertebral arteries in a small perimedullary space. The recurrence rate of 4% is consistent with other studies 16.
As for every surgical procedure, certain risks exist for microvascular decompression. The main risk is temporary or permanent hearing impairment, even to the extent of unilateral deafness. The risk reported in larger studies was 1.5% to 8% 16, 17. The risk for permanent facial paralysis reported in the literature is 0.7% to 0.9%. Delayed facial paralysis is more common [in 3% to 8% of cases 15]. The function of the facial nerve is initially completely intact after the procedure. After a mean of 12 days, however, acute high-grade paralysis of the facial muscles can develop on the operated side. One of the possible causes associated with this is the possible reactivation of Herpes zoster. Ultimately, however, the etiology of the delayed facial paralysis has not been identified to date 18. The symptoms recede completely over time in nearly all patients. The perioperative risk for life-threatening complications in the context of microvascular decompression—such as space-occupying hemorrhages or cerebellar or brainstem infarctions—is less than 1%.
- Rosenstengel C, Matthes M, Baldauf J, Fleck S, Schroeder H. Hemifacial Spasm: Conservative and Surgical Treatment Options. Deutsches Ärzteblatt International. 2012;109(41):667-673. doi:10.3238/arztebl.2012.0667. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3487151/[↩][↩][↩][↩][↩][↩]
- Felício AC, Godeiro-Junior Cde O, Borges V, Silva SM, Ferraz HB. Bilateral hemifacial spasm: a series of 10 patients with literature review. Parkinsonism Relat Disord. 2008;14:154–156. https://www.ncbi.nlm.nih.gov/pubmed/17702626[↩]
- Scheidt CE, Schuller B, Rayki O, Kommerell G, Deuschl G. Relative absence of psychopathology in benign essential blepharospasm and hemifacial spasm. Neurology. 1996;47:43–45. https://www.ncbi.nlm.nih.gov/pubmed/8710122[↩]
- Barker FG, 2nd, Jannetta PJ, Bissonette DJ, Shields PT, Larkins MV, Jho HD. Microvascular decompression for hemifacial spasm. J Neurosurg. 1995;82:201–210. https://www.ncbi.nlm.nih.gov/pubmed/7815147[↩][↩]
- Wang A, Jankovic J. Hemifacial spasm: clinical findings and treatment. Muscle Nerve. 1998;21:1740–1747. https://www.ncbi.nlm.nih.gov/pubmed/9843077[↩][↩]
- Girard N, Poncet M, Caces F, Tallon Y, Chays A, Martin-Bouyer P, Magnan J, Raybaud C. Three-dimensional MRI of hemifacial spasm with surgical correlation. Neuroradiology. 1997;39:46–51. https://www.ncbi.nlm.nih.gov/pubmed/9121649[↩]
- Nielsen VK. Electrophysiology of the facial nerve in hemifacial spasm: ectopic/ephaptic excitation. Muscle Nerve. 1985;8:545–555. https://www.ncbi.nlm.nih.gov/pubmed/2995804[↩][↩]
- Møller AR. Vascular compression of cranial nerves: II: pathophysiology. Neurol Res. 1999;21:439–443. https://www.ncbi.nlm.nih.gov/pubmed/10439424[↩]
- Yaltho TC, Jankovic J. The many faces of hemifacial spasm: differential diagnosis of unilateral facial spasms. Mov Disord. 2011;26:1582–1592. doi: 10.1002/mds.23692. https://www.ncbi.nlm.nih.gov/pubmed/21469208[↩][↩]
- Wang A, Jankovic J. Hemifacial spasm: clinical findings and treatment. Muscle Nerve. 1998;21:1740–1747 https://www.ncbi.nlm.nih.gov/pubmed/9843077[↩][↩]
- Wilkins RH. Hemifacial spasm: a review. Surg Neurol. 1991;36:251–277. https://www.ncbi.nlm.nih.gov/pubmed/1948626[↩]
- Jitpimolmard S, Tiamkao S, Laopaiboon M. Long term results of botulinum toxin type A (Dysport) in the treatment of hemifacial spasm: a report of 175 cases. J Neurol Neurosurg Psychiatry. 1998;64:751–757. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2170133/[↩]
- Simpson DM, Blitzer A, Brashear A, et al. Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Assessment: Botulinum neurotoxin for the treatment of movement disorders (an evidence-based review): report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2008;70:1699–1706. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5565261/[↩][↩]
- Yoshimura DM, Aminoff MJ, Tami TA, Scott AB. Treatment of hemifacial spasm with botulinum toxin. Muscle Nerve. 1992;15:1045–1049. https://www.ncbi.nlm.nih.gov/pubmed/1518513[↩]
- Dannenbaum M, Lega BC, Suki D, Harper RL, Yoshor D. Microvascular decompression for hemifacial spasm: long-term results from 114 operations performed without neurophysiological monitoring. J Neurosurg. 2008;109:410–415. https://www.ncbi.nlm.nih.gov/pubmed/18759569[↩][↩]
- Yuan Y, Wang Y, Zhang SX, Zhang L, Li R, Guo J. Microvascular decompression in patients with hemifacial spasm: report of 1200 cases. Chin Med J (Engl) 2005;118:833–836. https://www.ncbi.nlm.nih.gov/pubmed/15989764[↩][↩]
- Jo KW, Kim JW, Kong DS, Hong SH, Park K. The patterns and risk factors of hearing loss following microvascular decompression for hemifacial spasm. Acta Neurochir (Wien) 2011;153:1023–1030. Epub 2011 Jan 15. https://www.ncbi.nlm.nih.gov/pubmed/21240531[↩]
- Lovely TJ, Getch CC, Jannetta PJ. Delayed facial weakness after microvascular decompression of cranial nerve VII. Surg Neurol. 1998;50:449–452. https://www.ncbi.nlm.nih.gov/pubmed/9842870[↩]