Contents
- Hypervitaminosis A
- What is vitamin A?
- Hypervitaminosis A causes
- Hypervitaminosis A prevention
- Hypervitaminosis A symptoms
- Hypervitaminosis A complications
- Hypervitaminosis A diagnosis
- Hypervitaminosis A treatment
- Hypervitaminosis A prognosis
Hypervitaminosis A
Hypervitaminosis A is vitamin A toxicity that can occur from either the topical vitamin A or oral form of vitamin A 1. Each has its own set of adverse effects. Hypervitaminosis A or vitamin A toxicity is commonly related to the misuse of vitamin A dietary supplements but can also appear after an increased intake of food rich in preformed vitamin A (liver, poultry, fish, eggs and dairy products) 2, 3, 4. Oral vitamin A toxicity can be acute or chronic.
Acute oral vitamin A toxicity occurs because of the ingestion of a large amount of vitamin A (typically more than 100 times the Recommended Dietary Allowance [RDA]) over a short period of time 5. Acute vitamin A toxicity usually appears after more than 500 mg/day in adults, 100 mg/day in children or 30 mg/day in infants 1. However, these cutoff levels are decreased in individuals with heavy alcohol consumption or with kidney failure 6, 7. In addition, mild adverse effects have been observed in vitamin A supplementation (loose stools, headache, irritability, fever, nausea and vomiting), they are rare and typically resolved quickly by discontinuation of vitamin A intake 1.
The typical signs and symptoms of acute hypervitaminosis A are dry skin, cheilosis, dermatitis, joint and bone pain, severe headache, fatigue, blurred vision, nausea, dizziness, aching muscles, and coordination problems 5. A high proportion of patients also have liver test abnormalities, but these are typically mild. Jaundice is uncommon, but enlargement of the liver may be present. The presence of splenomegaly suggests that cirrhosis or portal hypertension was present at the time of initial presentation, as vitamin A is not stored in the spleen and does not cause splenomegaly on its own. In severe cases, cerebral spinal fluid pressure can increase, leading to drowsiness and, eventually, coma and even death 5.
In chronic oral vitamin A toxicity, intake is over a longer duration (regular consumption of high doses). Chronic toxicity can appear after a long-term intake of 10 mg/day of vitamin A for several months in adults and 7.5–15 mg/day in children 1. In general, vitamin A toxicity is uncommon in intakes lower than 30 mg/day (25,000–30,000 IU/day) 2.
Signs and symptoms of chronic hypervitaminosis A include low-grade fever, headache, fatigue, depression, anorexia, intestinal disturbances, hepatosplenomegaly, anemia, hypercalcemia, subcutaneous swelling, nocturia, joint and bone pain, painful muscles and skin changes such as yellowing, dryness, alopecia, and photosensitivity 5. Neuropsychiatric changes as a consequence of chronic hypervitaminosis A have also been reported 8. It was proposed that toxic levels of unbound retinyl esters (preformed vitamin A) can elicit neuropsychiatric effects, including depression, psychosis, and impulsivity 9.
Topical retinoids are creams, lotions and gels containing medicine derived from Vitamin A. The most common adverse effect of topical retinoids is skin irritation, notably skin redness (erythema), skin peeling (secondary to the hyper-proliferation of the epidermis) and discomfort 1. The most severe adverse effect of systemic retinoids is teratogenicity (major birth defects following fetal exposure during pregnancy). In addition, topical administration of retinoids can be associated with other adverse effects that include transient hypopigmentation or hyperpigmentation, psoriasis, allergic contact dermatitis and ectropion (the eyelids turned outwards) 10, 11. Importantly, retinoid overdose can cause the so-called “retinoic acid syndrome” 1. The retinoic acid syndrome manifests as acute respiratory distress with dyspnea, pleural and pericardial effusions, fever, weight gain, edema, and even multiorgan failure 12.
Getting too much preformed vitamin A usually from supplements or certain medicines can cause dizziness, nausea, headaches, liver injury, jaundice, enlargement of the liver and spleen, portal hypertension, cirrhosis, coma and even death 13. High intakes of preformed vitamin A in pregnant women can also cause birth defects in their babies. Birth abnormalities include craniofacial, cardiac, and central nervous system malformations. Women who might be pregnant should not take high doses of vitamin A supplements 13. Consuming high amounts of beta-carotene or other forms of provitamin A can turn the skin yellow-orange, but this condition is harmless. High intakes of beta-carotene do not cause birth defects or the other more serious effects caused by getting too much preformed vitamin A.
The recommended daily allowance for vitamin A is 300 to 700 mcg for children and approximately 700 to 900 mcg for adults, amounts which can be provided by a normal diet 14.
Each year, in the US alone over 60,000 cases of vitamin A toxicity are reported. Unlike the water-soluble vitamins, the fat-soluble vitamins (vitamins A, D, E and K) tend to accumulate in your body. In general, people with known chronic liver diseases should avoid ingestion of more than the minimal daily requirement of vitamin A as underlying liver disease appears to increase the susceptibility to vitamin A toxicity.
Treatment of hypervitaminosis A involves simply stopping supplements (or in rare cases, foods) that contain vitamin A. Symptoms of hypervitaminosis A may resolve within several weeks after discontinuing from ingestion of vitamin A and instituting supportive therapy. The liver injury caused by high doses of vitamin A is reversible in its early stages, but may resolve only slowly with discontinuation of vitamin A ingestion and resumption of a normal diet. Usually, portal hypertension resolves within months to years after discontinuation of the vitamin A supplement. However, in some cases, the liver injury progresses to cirrhosis, even requiring transplantation 15. Patients with increased intracranial pressure may require lumbar punctures or medications such as mannitol and diuretics for therapy. Patients with hypercalcemia may require intravenous fluids and additional therapy such as calcitonin and corticosteroids 16.
Birth defects caused by vitamin A are irreversible.
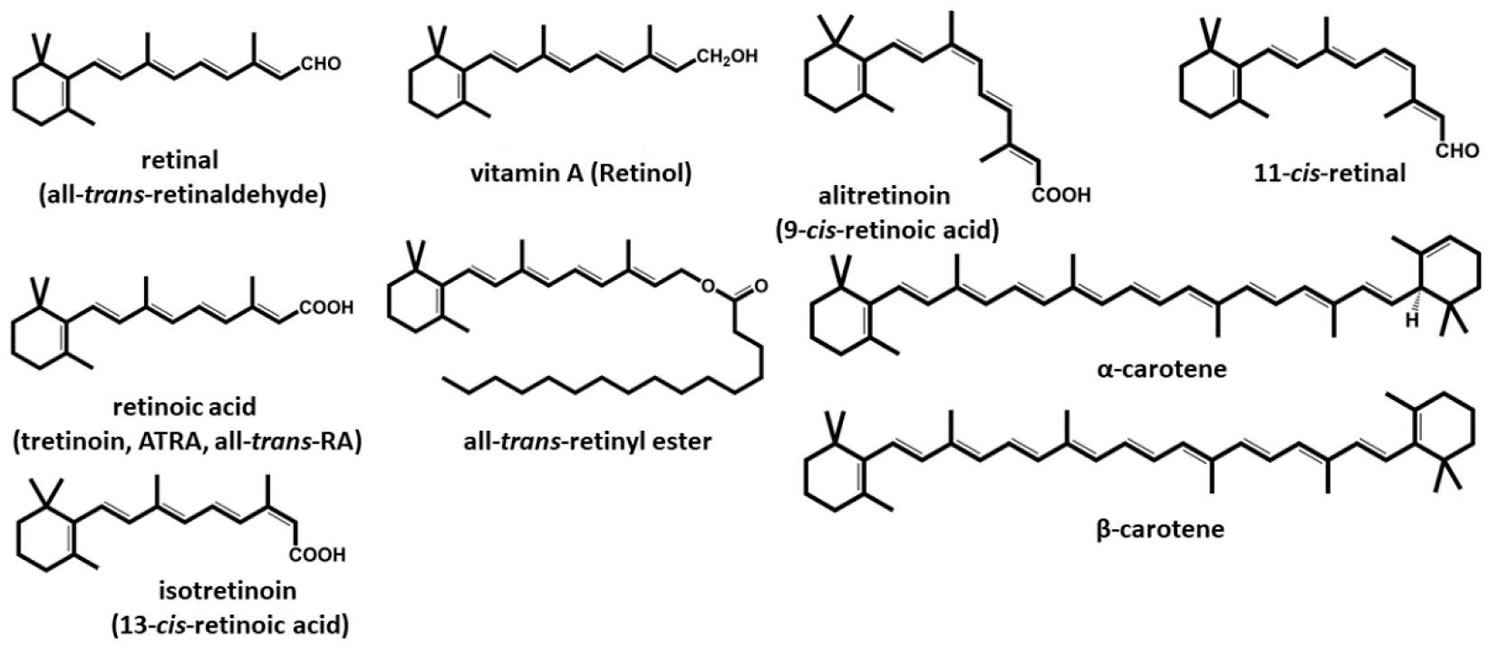
Figure 1. Vitamin A chemical structure
What is vitamin A?
Vitamin A is name of a group of fat-soluble compounds found as preformed vitamin A (retinol and its esterified form, retinyl ester) in animal products (such as fish, liver, dairy products, and eggs) and as provitamin A carotenoids (beta-carotene, alpha-carotene and beta-cryptoxanthin) in fruit and vegetables 17, 18, 19, 20, 21. Carotenoids are pigments that give yellow, orange, and red fruits and vegetables their color. Your body is able to convert some carotenoids into vitamin A. The three active forms of vitamin A in the body are retinol, retinal, and retinoic acid 22.
There are two different types of vitamin A 23.
- Preformed vitamin A (retinol and its esterified form, retinyl ester), is found in meat (especially liver), poultry, fish, eggs and dairy products.
- Provitamin A carotenoids (beta-carotene, alpha-carotene and beta-cryptoxanthin), is found in fruits, vegetables, and other plant-based products (oily fruits and red palm oil). The most common type of provitamin A carotenoids in foods and dietary supplements is beta-carotene (β-carotene). The body converts these plant pigments into vitamin A.
The human body is not able to produce vitamin A, and therefore, you need to obtain vitamin A from your diet either as preformed vitamin A or in the form of provitamin A carotenoids 1. There are more than 50 provitamin A carotenoids, but only beta-carotene (β-carotene), alpha-carotene (α-carotene), and beta-cryptoxanthin (β-cryptoxanthin) are present in significant amounts in the human diet 24. Beta-carotene (β-carotene) is the most abundant in the diet. Beta-carotene (β-carotene) is mostly ingested through red and orange vegetables and partially through the same colored fruits and green vegetables. In Europe, carrots, spinach, and tomato products are the main contributors to beta-carotene (β-carotene) intake, while beta-cryptoxanthin (β-cryptoxanthin) is most commonly taken from various citruses and citrus juices 2. Beta-cryptoxanthin (β-cryptoxanthin), as well as other carotenoids, occurs in plants both as free and esterified with fatty acids (lauric, myristic, palmitic), and these esters contribute to total vitamin A content due to their comparable bioavailability 25. Rich sources of cryptoxanthin or its esters include, in addition to the already-mentioned citruses (satsuma mandarins, tangerines, clementines, mineolas and oranges), persimmons, chili peppers and red peppers, papaya, sea buckthorn, loquat, mango and apricots 26, 27, 28, 29. Other sources of provitamin A carotenoids also include various medicinal plants and herbs, cereals, and specific vegetable oils (see Table 2 below).
Vitamin A is important for normal vision, gene expression, the immune function, embryonic development, growth, cellular communication, and male and female reproduction 4, 30, 31. Vitamin A also helps your heart, lungs, kidneys, and other organs to work properly 32.
Vitamin A is critical for vision as an essential component of rhodopsin, a protein that absorbs light in the retinal receptors, and because it supports the normal differentiation and functioning of the conjunctival membranes and cornea 19, 20, 33. Vitamin A also supports cell growth and differentiation, playing a critical role in the normal formation and maintenance of the heart, lungs, kidneys, and other organs 19.
Both provitamin A and preformed vitamin A must be metabolized intracellularly to retinal and retinoic acid, the active forms of vitamin A, to support the vitamin’s important biological functions 19, 20. Provitamin A carotenoids are plant pigments that the body converts into vitamin A in the intestine 4. The main provitamin A carotenoids in the human diet are beta-carotene, alpha-carotene, and beta-cryptoxanthin 4. Other carotenoids in food, such as lycopene, lutein, and zeaxanthin, are not converted into vitamin A and are referred to as non-provitamin A carotenoids; they might have other important activities not involving vitamin A formation 4.
Both retinyl esters and provitamin A carotenoids are converted to retinol, which is oxidized to retinal and then to retinoic acid 19. Most of the body’s vitamin A is stored in the liver in the form of retinyl esters 4.
Normally, the liver stores 80 to 90% of the body’s vitamin A. To use vitamin A, the body releases it into the circulation bound to prealbumin (transthyretin) and retinol-binding protein (RBP). Beta-carotene and other provitamin carotenoids, contained in green leafy and yellow vegetables and deep- or bright-colored fruits, are converted to vitamin A. Carotenoids are absorbed better from vegetables when they are cooked or homogenized and served with some fat (eg, oils).
The body can convert beta-carotene into vitamin A to help meet these requirements. Although there is no Recommended Dietary Allowance (RDA) for beta-carotene, the National Institutes of Health Office of Dietary Supplements recommends eating five or more servings of fruits and vegetables per day, including dark green and leafy vegetables and deep yellow or orange fruits to get appropriate amounts of beta-carotene.
Retinol activity equivalents (RAE) were developed because provitamin A carotenoids have less vitamin A activity than preformed vitamin A; 1 microgram retinol = 3.33 IU vitamin A. Or expressed differently, 1 IU vitamin A = 0.3 mcg retinol
For dietary provitamin A carotenoids (β-carotene, α-carotene, and β-cryptoxanthin), retinol activity equivalents (RAEs) have been set at 12, 24, and 24 microgram (mcg), respectively. Using mcg RAE, the vitamin A activity of provitamin A carotenoids is half the vitamin A activity assumed when using μg retinol equivalents (μg RE) 32. This change in equivalency values is based on data demonstrating that the vitamin A activity of purified β-carotene in oil is half the activity of vitamin A, and based on recent data demonstrating that the vitamin A activity of dietary β-carotene is one-sixth, rather than one-third, the vitamin activity of purified β-carotene in oil. This change in bioconversion means that a larger amount of provitamin A carotenoids, and therefore darkly colored, carotene-rich fruits and vegetables, is needed to meet the vitamin A requirement.
Synthetic vitamin A analogs (retinoids) are being used increasingly in dermatology. The possible protective role of beta-carotene, retinol, and retinoids against some epithelial cancers is under study. However, risk of certain cancers may be increased after beta-carotene supplementation 34.
Retinol is the form of vitamin A that causes concern. In addition to getting retinol from their diets, some people may be using synthetic retinoid preparations that are chemically similar to vitamin A to treat acne, psoriasis, and other skin conditions. These retinoid preparations have been shown to have the same negative impact on bone health as dietary retinol. Use of retinoid medications in children and teens also has been linked to delays in growth.
Retinol and carotenoid levels are typically measured in plasma or serum because blood samples are easy to collect 4. However, these levels are not always reliable indicators of vitamin A status because they do not decline until vitamin A levels in the liver and other storage sites are almost depleted and because acute and chronic infections can decrease serum and plasma retinol concentrations 4. Most vitamin A is stored in the liver, so measuring vitamin A levels in the liver is the best way to assess vitamin A adequacy 4. In clinical studies, specialized research laboratories can measure liver vitamin A reserves indirectly using isotope-dilution or dose-response methods, in which plasma levels of retinol, a tracer surrogate, or both are measured over several days after the administration of vitamin A 4.
In clinical practice, plasma retinol levels alone can be used to document significant deficiency. In general, the following conversions can be used: serum retinol 1 micromole/L = 28.6 mcg/dL.
A serum or plasma retinol concentration of 20 mcg/dL (0.70 micromoles/L) or less frequently reflects moderate vitamin A deficiency, and a serum retinol level of 10 mcg/dL (0.35 micromoles/L) or less is considered an indicator of severe vitamin A deficiency 4.
How much vitamin A do I need?
The amount of vitamin A you need depends on your age and sex. Average daily recommended amounts of preformed vitamin A and provitamin A carotenoids are listed below in micrograms (mcg) of retinol activity equivalents (RAE).
Intake recommendations for vitamin A and other nutrients are provided in the Dietary Reference Intakes (DRIs) developed by the Food and Nutrition Board (FNB) at the Institute of Medicine of the National Academies (formerly National Academy of Sciences) 35. Dietary Reference Intake (DRI) is the general term for a set of reference values used for planning and assessing nutrient intakes of healthy people. These values, which vary by age and gender, include:
- Recommended Dietary Allowance (RDA): Average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals; often used to plan nutritionally adequate diets for individuals.
- Adequate Intake (AI): Intake at this level is assumed to ensure nutritional adequacy; established when evidence is insufficient to develop an RDA.
- Estimated Average Requirement (EAR): Average daily level of intake estimated to meet the requirements of 50% of healthy individuals; usually used to assess the nutrient intakes of groups of people and to plan nutritionally adequate diets for them; can also be used to assess the nutrient intakes of individuals.
- Tolerable Upper Intake Level (UL): Maximum daily intake unlikely to cause adverse health effects.
Recommended Dietary Allowances (RDAs) for vitamin A are given as mcg of retinol activity equivalents (RAE) to account for the different bioactivities of retinol and provitamin A carotenoids (see Table 1). Because the body converts all dietary sources of vitamin A into retinol, 1 mcg of physiologically available retinol is equivalent to the following amounts from dietary sources: 1 mcg of retinol, 12 mcg of beta-carotene, and 24 mcg of alpha-carotene or beta-cryptoxanthin. From dietary supplements, the body converts 2 mcg of beta-carotene to 1 mcg of retinol.
Retinol activity equivalents (RAE) were developed because provitamin A carotenoids have less vitamin A activity than preformed vitamin A; 1 mcg retinol = 3.33 IU.
Currently, vitamin A is listed on food and supplement labels in international units (IUs) even though nutrition scientists rarely use this measure. Conversion rates between mcg RAE and IU are as follows 36:
- 1 IU retinol = 0.3 mcg RAE (retinol activity equivalents)
- 1 IU beta-carotene from dietary supplements = 0.15 mcg RAE
- 1 IU beta-carotene from food = 0.05 mcg RAE
- 1 IU alpha-carotene or beta-cryptoxanthin = 0.025 mcg RAE
However, under FDA’s new labeling regulations for foods and dietary supplements that take effect by January 1, 2020 (for companies with annual sales of $10 million or more) or January 1, 2021 (for smaller companies), vitamin A will be listed only in mcg RAE and not IUs 37.
An RAE cannot be directly converted into an IU without knowing the source(s) of vitamin A. For example, the RDA of 900 mcg RAE for adolescent and adult men is equivalent to 3,000 IU if the food or supplement source is preformed vitamin A (retinol). However, this RDA is also equivalent to 6,000 IU of beta-carotene from supplements, 18,000 IU of beta-carotene from food, or 36,000 IU of alpha-carotene or beta-cryptoxanthin from food. So a mixed diet containing 900 mcg RAE provides between 3,000 and 36,000 IU of vitamin A, depending on the foods consumed.
Table 1. Recommended Dietary Allowances (RDAs) for Vitamin A
| Life Stage | Recommended Amount |
|---|---|
| Birth to 6 months* | 400 mcg RAE |
| Infants 7–12 months* | 500 mcg RAE |
| Children 1–3 years | 300 mcg RAE |
| Children 4–8 years | 400 mcg RAE |
| Children 9–13 years | 600 mcg RAE |
| Teen boys 14–18 years | 900 mcg RAE |
| Teen girls 14–18 years | 700 mcg RAE |
| Adult men | 900 mcg RAE |
| Adult women | 700 mcg RAE |
| Pregnant teens | 750 mcg RAE |
| Pregnant women | 770 mcg RAE |
| Breastfeeding teens | 1,200 mcg RAE |
| Breastfeeding women | 1,300 mcg RAE |
Footnote: * Adequate Intake (AI), equivalent to the mean intake of vitamin A in healthy, breastfed infants.
[Source 35 ]International Units (IUs) and mcg RAE
Vitamin A is listed on the new Nutrition Facts and Supplement Facts labels in mcg RAE 38. The U.S. Food and Drug Administration (FDA) required manufacturers to use these new labels starting in January 2020, but companies with annual sales of less than $10 million may continue to use the old labels that list vitamin A in international units (IUs) until January 2021 37. To convert International Units (IUs) to mcg RAE, use the following 39:
- 1 IU retinol = 0.3 mcg RAE (retinol activity equivalents)
- 1 IU beta-carotene from dietary supplements = 0.15 mcg RAE
- 1 IU beta-carotene from food = 0.05 mcg RAE
- 1 IU alpha-carotene or beta-cryptoxanthin = 0.025 mcg RAE
RAE can only be directly converted into IUs if the source or sources of vitamin A are known. For example, the RDA of 900 mcg RAE for adolescent and adult men is equivalent to 3,000 IU if the food or supplement source is preformed vitamin A (retinol). However, this RDA is also equivalent to 6,000 IU of beta-carotene from supplements, 18,000 IU of beta-carotene from food, or 36,000 IU of alpha-carotene or beta-cryptoxanthin from food. So a mixed diet containing 900 mcg RAE provides between 3,000 and 36,000 IU of vitamin A, depending on the foods consumed.
What foods provide vitamin A?
Vitamin A is found naturally in many foods and is added to some foods, such as milk and cereal. You can get recommended amounts of vitamin A by eating a variety of foods, including the following:
- Some types of fish, such as herring and salmon
- Beef liver and other organ meats (which are also high in cholesterol, so limit the amount you eat)
- Green leafy vegetables and other green, orange, and yellow vegetables, such as spinach, sweet potatoes, carrots, broccoli, and winter squash
- Fruits, including cantaloupe, mangos, and apricots
- Dairy products, such as milk and cheese
- Fortified breakfast cereals
- Eggs
Concentrations of preformed vitamin A are highest in liver and fish oils 19. Other sources of preformed vitamin A are milk and eggs, which also include some provitamin A 19. Most dietary provitamin A comes from leafy green vegetables, orange and yellow vegetables, tomato products, fruits, and some vegetable oils 19. The top food sources of vitamin A in the U.S. diet include dairy products, liver, fish, and fortified cereals; the top sources of provitamin A include carrots, broccoli, cantaloupe, and squash 33.
Table 2 suggests many dietary sources of vitamin A. The foods from animal sources in Table 2 contain primarily preformed vitamin A, the plant-based foods have provitamin A, and the foods with a mixture of ingredients from animals and plants contain both preformed vitamin A and provitamin A.
Table 2. Selected food sources of vitamin A
| Food | Micrograms (mcg) RAE per serving | Percent Daily Value* |
|---|---|---|
| Beef liver, pan fried, 3 ounces | 6582 | 731 |
| Sweet potato, baked in skin, 1 whole | 1403 | 156 |
| Spinach, frozen, boiled, ½ cup | 573 | 64 |
| Pumpkin pie, commercially prepared, 1 piece | 488 | 54 |
| Carrots, raw, ½ cup | 459 | 51 |
| Ice cream, French vanilla, soft serve, 1 cup | 278 | 31 |
| Cheese, ricotta, part skim, 1 cup | 263 | 29 |
| Herring, Atlantic, pickled, 3 ounces | 219 | 24 |
| Milk, fat free or skim, with added vitamin A and vitamin D, 1 cup | 149 | 17 |
| Cantaloupe, raw, ½ cup | 135 | 15 |
| Peppers, sweet, red, raw, ½ cup | 117 | 13 |
| Mangos, raw, 1 whole | 112 | 12 |
| Breakfast cereals, fortified with 10% of the daily value for vitamin A, 1 serving | 90 | 10 |
| Egg, hard boiled, 1 large | 75 | 8 |
| Black-eyed peas (cowpeas), boiled, 1 cup | 66 | 7 |
| Apricots, dried, sulfured, 10 halves | 63 | 7 |
| Broccoli, boiled, ½ cup | 60 | 7 |
| Salmon, sockeye, cooked, 3 ounces | 59 | 7 |
| Tomato juice, canned, ¾ cup | 42 | 5 |
| Yogurt, plain, low fat, 1 cup | 32 | 4 |
| Tuna, light, canned in oil, drained solids, 3 ounces | 20 | 2 |
| Baked beans, canned, plain or vegetarian, 1 cup | 13 | 1 |
| Summer squash, all varieties, boiled, ½ cup | 10 | 1 |
| Chicken, breast meat and skin, roasted, ½ breast | 5 | 1 |
| Pistachio nuts, dry roasted, 1 ounce | 4 | 0 |
Footnote: *DV = Daily Value. U.S. Food and Drug Administration (FDA) developed Daily Values (DVs) to help consumers compare the nutrient contents of foods and dietary supplements within the context of a total diet. The Daily Value (DV) for vitamin A is 900 mcg RAE for adults and children age 4 years and older, where 1 mcg RAE = 1 mcg retinol, 2 mcg beta-carotene from supplements, 12 mcg beta-carotene from foods, 24 mcg alpha-carotene, or 24 mcg beta-cryptoxanthin 37. FDA does not require food labels to list vitamin A content unless vitamin A has been added to the food. Foods providing 20% or more of the Daily Value (DV) are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
The U.S. Department of Agriculture’s (USDA’s) FoodData Central (https://fdc.nal.usda.gov) lists the nutrient content of many foods and provides a comprehensive list of foods containing vitamin A in IUs arranged by nutrient content (https://ods.od.nih.gov/pubs/usdandb/VitaminA-Content.pdf) and by food name (https://ods.od.nih.gov/pubs/usdandb/VitaminA-Food.pdf), and foods containing beta-carotene in mcg arranged by nutrient content (https://ods.od.nih.gov/pubs/usdandb/VitA-betaCarotene-Content.pdf) and by food name (https://ods.od.nih.gov/pubs/usdandb/VitA-betaCarotene-Food.pdf).
[Source 40 ]What kinds of vitamin A dietary supplements are available?
Vitamin A is available in dietary supplements, usually in the form of retinyl acetate or retinyl palmitate (preformed vitamin A), beta-carotene (provitamin A), or a combination of preformed and provitamin A 4. Most multivitamin-mineral supplements contain vitamin A. Dietary supplements that contain only vitamin A are also available.
The amounts of vitamin A in supplements vary widely, but 3,000 mcg RAE (333% of the DV) is common. This is due to the fact that the Daily Values (DV) used by the US Food and Drug Administration (FDA) for supplement labeling are based on the RDA established in 1968 rather than the most recent RDA, and multivitamin supplements typically provide 100% of the DV for most nutrients.
Multivitamins commonly have somewhat lower vitamin A amounts, often 750 to 1,050 mcg RAE (83% to 117% of the DV). Because retinol intakes of 5,000 IU/day (1,500 mcg RAE) may be associated with an increased risk of osteoporosis in older adults, some companies have reduced the retinol content in their multivitamin supplements to 2,500 IU (750 mcg RAE).
The absorption of preformed vitamin A esters from dietary supplements is 70–90%, and that of beta-carotene ranges from 8.7% to 65% 41, 42.
What is the tolerable upper intake level of vitamin A?
Because vitamin A is fat soluble, the body stores excess vitamin A primarily in the liver, and these vitamin A levels can accumulate. In January 2001, the Food and Nutrition Board of the US Institute of Medicine set the tolerable upper intake level (UL) of vitamin A intake for adults at 3,000 mcg RAE (10,000 IU)/day of preformed vitamin A 43, 44. The tolerable upper intake level (UL) does not apply to vitamin A derived from carotenoids (vitamin A in fruits and vegetables). The Food and Nutrition Board based these Upper Intake Levels (ULs) on the amounts associated with an increased risk of liver abnormalities in men and women, teratogenic effects, and a range of toxic effects in infants and children. The Food and Nutrition Board also considered levels of preformed vitamin A associated with decreased bone mineral density, but did not use these data as the basis for its ULs because the evidence was conflicting. The Food and Nutrition Board has not established Upper Intake Levels (ULs) for beta-carotene and other provitamin A carotenoids 45. However, the Food and Nutrition Board advises against the use of beta-carotene supplements for the general population, except as a provitamin A source to prevent vitamin A deficiency.
- Recommended Dietary Allowance (RDA) is the average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals; often used to plan nutritionally adequate diets for individuals.
- Retinol activity equivalents (RAE) were developed because provitamin A carotenoids have less vitamin A activity than preformed vitamin A; 1 microgram retinol = 3.33 IU vitamin A. Or expressed differently, 1 IU vitamin A = 0.3 mcg retinol
Table 3. Tolerable Upper Intake Levels (ULs) for Preformed Vitamin A
| Age | Male | Female | Pregnancy | Lactation |
|---|---|---|---|---|
| Birth to 12 months | 600 mcg | 600 mcg | ||
| 1–3 years | 600 mcg | 600 mcg | ||
| 4–8 years | 900 mcg | 900 mcg | ||
| 9–13 years | 1,700 mcg | 1,700 mcg | ||
| 14–18 years | 2,800 mcg | 2,800 mcg | 2,800 mcg | 2,800 mcg |
| 19+ years | 3,000 mcg | 3,000 mcg | 3,000 mcg | 3,000 mcg |
Footnotes: These tolerable upper intake levels (ULs) apply only to products from animal sources and supplements whose vitamin A comes entirely from retinol or its ester forms, such as retinyl palmitate. However, many dietary supplements (such as multivitamins) do not provide all of their vitamin A in retinol or its ester forms. For example, the vitamin A in some supplements consists partly or entirely of beta-carotene. In such cases, the percentage of retinol or retinyl ester in the supplement should be used to determine whether an individual’s vitamin A intake exceeds the UL. For example, a supplement whose label indicates that the product contains 3,000 mcg RAE vitamin A and that 60% of this vitamin A comes from beta-carotene (and therefore 40% comes from retinol or retinyl ester) provides 1,200 mcg RAE of preformed vitamin A. That amount is above the UL for children from birth to 8 years but below the UL for older children and adults.
[Source 46 ]Hypervitaminosis A causes
Because vitamin A is fat soluble, the body stores excess amounts, primarily in the liver, and these levels can accumulate 40. Although excess preformed vitamin A can have significant toxicity also known as hypervitaminosis A, large amounts of beta-carotene and other provitamin A carotenoids are not associated with major adverse effects 47. Vitamin A toxicity is more commonly associated with abuse of vitamin A supplements than with health intervention programs. Vitamin A toxic reactions may also be provoked by consuming liver products rich in vitamin A or excess administration of vitamin A preparations. The amount of vitamin A required to cause toxicity among individuals varies depending on age and liver function.
Acute hypervitaminosis A may occur with a single ingestion of 25,000 IU/kg or more. However, this cutoff level is decreased in individuals with heavy alcohol consumption or with kidney failure 6, 7. Signs and symptoms include nausea, vomiting, diarrhea, dizziness, lethargy, drowsiness, increased intracranial pressure, and skin changes such as erythema, pruritus, or desquamation.
Chronic hypervitaminosis A may occur with excessive ingestion of 4000 IU/kg or more daily for 6-15 months. Signs and symptoms include low-grade fever, headache, fatigue, anorexia, intestinal disturbances, hepatosplenomegaly, anemia, hypercalcemia, subcutaneous swelling, nocturia, joint and bone pain, and skin changes such as yellowing, dryness, alopecia, and photosensitivity. Neuropsychiatric changes as a consequence of chronic hypervitaminosis A have also been reported 8. It was proposed that toxic levels of unbound retinyl esters (preformed vitamin A) can elicit neuropsychiatric effects, in-cluding depression, psychosis, and impulsivity 9.
The manifestations of hypervitaminosis A depend on the size and rapidity of the excess vitamin A intake. The symptoms of hypervitaminosis A following sudden, massive intakes of vitamin A, as with Arctic explorers who ate polar bear liver, are acute 48. The symptoms of acute hypervitaminosis A are drowsiness, sluggishness, irritability or irresistible desire to sleep and severe headache and vomiting 48. During the second 24 hours, the skin of the patients began to peel around the mouth, beginning in spots and gradually spreading over larger areas. In some cases the peeling was confined to the face, but in several it was general. Lindhard 49 also described three other cases in which the skin peeled from head to foot after eating polar bear liver. The Norwegian explorer Nansen [1924] has mentioned that on two occasions he ate small amounts of bear liver without ill effects. It seems probable therefore that vitamin A toxicity only occur when large quantities are consumed.
Chronic intakes of excess vitamin A lead to increased intracranial pressure (pseudotumor cerebri), dizziness, nausea, headaches, skin irritation, pain in joints and bones, coma, and even death 19. Although hypervitaminosis A can be due to excessive dietary intakes, the condition is usually a result of consuming too much preformed vitamin A from supplements or therapeutic retinoids 20. When people consume too much vitamin A, their tissue levels take a long time to fall after they discontinue their intake, and the resulting liver damage is not always reversible.
Observational studies have suggested an association between high intakes of preformed vitamin A (more than 1,500 mcg daily—only slightly higher than the RDA), reduced bone mineral density, and increased fracture risk 50. However, the results of studies on this risk have been mixed, so the safe retinol intake level for this association is unknown.
Total intakes of preformed vitamin A that exceed the Upper Intake Level (UL) and some synthetic retinoids used as topical therapies (such as isotretinoin and etretinate) can cause congenital birth defects 19. These birth defects can include malformations of the eye, skull, lungs, and heart 33. Women who might be pregnant should not take high doses of vitamin A supplements 19.
Unlike preformed vitamin A, beta-carotene is not known to be teratogenic or lead to reproductive toxicity 18. And even large supplemental doses (20–30 mg/day) of beta-carotene or diets with high levels of carotenoid-rich food for long periods are not associated with toxicity. The most significant effect of long-term, excess beta-carotene is carotenodermia, a harmless condition in which the skin becomes yellow-orange 18. This condition can be reversed by discontinuing beta-carotene ingestion.
Supplementation with beta-carotene, with or without retinyl palmitate, for 5–8 years has been associated with an increased risk of lung cancer and cardiovascular disease in current and former male and female smokers and in male current and former smokers occupationally exposed to asbestos 51. In the The Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study 52, beta-carotene supplements (20 mg daily) were also associated with increased mortality, mainly due to lung cancer and ischemic heart disease. The CARET study 51 ended early, after the investigators found that daily beta-carotene (30 mg) and retinyl palmitate (7,500 mcg RAE [25,000 IU]) supplements increased the risk of lung cancer and cardiovascular disease mortality.
Hypervitaminosis A prevention
How much vitamin A you need depends on your age and sex. Other factors, such as pregnancy and your overall health, are also important. Ask your provider what amount is best for you.
To avoid hypervitaminosis A, don’t take more than the recommended daily allowance of vitamin A.
Some people take vitamin A and beta carotene supplements in the belief it will help prevent cancer. This may lead to chronic hypervitaminosis A if people take more than is recommended.
Hypervitaminosis A symptoms
Excess natural or synthetic vitamin A levels or hypervitaminosis A may result in a wide array of adverse effects. Hypervitaminosis A is more commonly associated with abuse of vitamin A supplements than with health intervention programs. Toxic reactions may also be provoked by consuming liver products rich in vitamin A or excess administration of vitamin A preparations. The amount of vitamin A required to cause toxicity among individuals varies depending on age and hepatic function.
Hypervitaminosis A symptoms may include:
- Abnormal softening of the skull bone (in infants and children)
- Blurred vision
- Bone pain or swelling
- Bulging of the soft spot in an infant’s skull (fontanelle)
- Changes in alertness or consciousness
- Decreased appetite
- Dizziness
- Double vision (in young children)
- Drowsiness
- Hair changes, such as hair loss and oily hair
- Headache
- Irritability
- Liver damage
- Nausea
- Poor weight gain (in infants and children)
- Skin changes, such as cracking at corners of the mouth, higher sensitivity to sunlight, oily skin, peeling, itching, and yellow color to the skin
- Vision changes
- Vomiting
Acute hypervitaminosis A may occur with a single ingestion of 25,000 IU/kg or more. Signs and symptoms include nausea, vomiting, diarrhea, dizziness, lethargy, drowsiness, increased intracranial pressure, and skin changes such as erythema, pruritus, or desquamation.
Chronic hypervitaminosis A may occur with excessive ingestion of 4000 IU/kg or more daily for 6-15 months. Signs and symptoms include low-grade fever, headache, fatigue, anorexia, intestinal disturbances, hepatosplenomegaly, anemia, hypercalcemia, subcutaneous swelling, nocturia, joint and bone pain, and skin changes such as yellowing, dryness, alopecia, and photosensitivity. Neuropsychiatric changes as a consequence of chronic hypervitaminosis A have also been reported 8. It was proposed that toxic levels of unbound retinyl esters (preformed vitamin A) can elicit neuropsychiatric effects, in-cluding depression, psychosis, and impulsivity 9.
To convert International Units (IUs) to mcg RAE, use the following 39:
- 1 IU retinol = 0.3 mcg RAE (retinol activity equivalents)
- 1 IU beta-carotene from dietary supplements = 0.15 mcg RAE
- 1 IU beta-carotene from food = 0.05 mcg RAE
- 1 IU alpha-carotene or beta-cryptoxanthin = 0.025 mcg RAE
RAE can only be directly converted into IUs if the source or sources of vitamin A are known. For example, the RDA of 900 mcg RAE for adolescent and adult men is equivalent to 3,000 IU if the food or supplement source is preformed vitamin A (retinol) or if the supplement source is beta-carotene. This RDA is also equivalent to 18,000 IU beta-carotene from food or to 36,000 IU alpha-carotene or beta-cryptoxanthin from food. Therefore, a mixed diet containing 900 mcg RAE provides between 3,000 and 36,000 IU vitamin A, depending on the foods consumed.
Vitamin A is highly teratogenic if taken during pregnancy. Retinoids affect the expression of homeobox gene Hoxb-1, which regulates axial patterning of the embryo. Birth abnormalities include craniofacial, cardiac, and central nervous system malformations. Therefore, treatment with vitamin A should be avoided in pregnant patients except in areas where vitamin A deficiency is prevalent. In this circumstance, supplementation should not exceed 10,000 IU daily 16.
Of note, mild adverse effects have been observed with vitamin A given with immunization. Symptoms include loose stools, headache, irritability, fever, nausea, and vomiting. These side effects are rare and typically resolved within 24 to 48 hours 53.
Vitamin A Toxicity in Infants and Children
There are numerous case reports of infants, toddlers, and children who have demonstrated toxic effects due to excess vitamin A intakes for months to years. Of particular concern are intracranial (bulging fontanel) and skeletal abnormalities that can result in infants given vitamin A doses of 5,500 to 6,750 μg/day 54. The clinical presentation of vitamin A toxicity in infants and young children varies widely. The more commonly recognized signs and symptoms include skeletal abnormalities, bone tenderness and pain, increased intracranial pressure, desquamation, brittle nails, mouth fissures, alopecia, fever, headache, lethargy, irritability, weight loss, vomiting, and hepatomegaly 55. Furthermore, tolerance to excess vitamin A intake also appears to vary 56. Carpenter and coworkers 56 described two boys who developed hypervitaminosis A by age 2 years for one and by age 6 years for the other. Both were given chicken liver that supplied about 690 μg/day of vitamin A and various supplements that supplied another 135 to 750 μg/day. An older sister who had been treated similarly remained completely healthy.
Hypervitaminosis A complications
Hypervitaminosis A complications can include:
- Very high calcium level
- Failure to thrive (in infants)
- Kidney damage due to high calcium
- Liver damage
Taking too much vitamin A during pregnancy may cause birth defects. Talk to your health care provider about eating a proper diet while you are pregnant.
Consuming high amounts of beta-carotene or other forms of provitamin A can turn the skin yellow-orange, but this condition is harmless. High intakes of beta-carotene do not cause birth defects or the other more serious effects caused by getting too much preformed vitamin A.
Hypervitaminosis A diagnosis
These tests may be done if a high vitamin A level is suspected:
- Bone x-rays
- Blood calcium test
- Cholesterol test
- Liver function test
- Blood test to check vitamin A level
- Blood test to check other vitamin levels
Diagnosis of vitamin A toxicity is clinical. Blood vitamin levels correlate poorly with toxicity. However, if clinical diagnosis is equivocal, laboratory testing may help. In vitamin A toxicity, fasting serum retinol levels may increase from normal (28 to 86 mcg/dL [1 to 3 mcmol/L]) to > 100 mcg/dL (> 3.49 mcmol/L), sometimes to > 2000 mcg/dL (> 69.8 mcmol/L). Hypercalcemia is common.
The plasma retinol concentration is not a reliable estimate of the vitamin A requirement because of its insensitive relationship between liver concentration and there is no noninvasive marker available for the assessment of vitamin A excess 15.
Differentiating vitamin A toxicity from other disorders may be difficult. Carotenosis may also occur in severe hypothyroidism and anorexia nervosa, possibly because carotene is converted to vitamin A more slowly.
Histologically, hypervitaminosis A causes hepatocyte injury, necrosis, stellate cell hyperplasia and subsequent fibrosis resulting in perisinusoidal, pericentrilobular and periportal scarring causing sinusoidal dilatation and obstruction thusimpairing hepatic venous outflow and consequently leading to noncirrhotic portal hypertension 57.
Hypervitaminosis A treatment
Treatment involves simply stopping supplements (or rarely, foods) that contain vitamin A. Most of the signs and symptoms of hypervitaminosis A (acute retinoid toxicity, hypertriglyceridemia, skin and central nervous system symptoms) may resolve within several weeks after discontinuing from ingestion of vitamin A and instituting supportive therapy. Some of these symptoms, such as skin desquamation, remain evident for several months. The liver injury caused by high doses of vitamin A is reversible in its early stages, but may resolve only slowly with discontinuation of vitamin A ingestion and resumption of a normal diet. Usually, portal hypertension resolves within months to years after discontinuation of the vitamin A supplement. However, in some cases, the liver injury progresses to cirrhosis, even requiring transplantation 15. Patients with increased intracranial pressure may require lumbar punctures or medications such as mannitol and diuretics for therapy. However, irreversible central nervous system consequences may occur 58, 59. Eye dryness following hypervitaminosis A is managed with eye drops. Patients with hypercalcemia may require intravenous fluids and additional therapy such as calcitonin and corticosteroids 16.
However, birth defects in the fetus of a mother who has taken megadoses of vitamin A are not reversible.
Most people fully recover.
Hypervitaminosis A prognosis
Most people fully recover from hypervitaminosis A. The liver injury caused by high doses of vitamin A is reversible in its early stages, but may resolve only slowly with discontinuation of vitamin A ingestion and resumption of a normal diet. Usually, portal hypertension resolves within months to years after discontinuation of the vitamin A supplement. However, in some cases, the liver injury progresses to cirrhosis, even requiring transplantation 15. Patients with increased intracranial pressure may require lumbar punctures or medications such as mannitol and diuretics for therapy. Patients with hypercalcemia may require intravenous fluids and additional therapy such as calcitonin and corticosteroids 16. Birth defects caused by vitamin A are irreversible.
- Carazo A, Macáková K, Matoušová K, Krčmová LK, Protti M, Mladěnka P. Vitamin A Update: Forms, Sources, Kinetics, Detection, Function, Deficiency, Therapeutic Use and Toxicity. Nutrients. 2021 May 18;13(5):1703. doi: 10.3390/nu13051703[↩][↩][↩][↩][↩][↩][↩]
- Beltrán-de-Miguel B., Estévez-Santiago R., Olmedilla-Alonso B. Assessment of dietary vitamin A intake (retinol, α-carotene, β-carotene, β-cryptoxanthin) and its sources in the National Survey of Dietary Intake in Spain (2009–2010) Int. J. Food Sci. Nutr. 2015;66:706–712. doi: 10.3109/09637486.2015.1077787[↩][↩][↩]
- Trumbo P., Yates A.A., Schlicker S., Poos M. Dietary reference intakes: Vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. J. Am. Diet. Assoc. 2001;101:294–301. doi: 10.1016/S0002-8223(01)00078-5[↩]
- Blaner WS. Vitamin A and Provitamin A Carotenoids. In: Marriott BP, Birt DF, Stallings VA, Yates AA, eds. Present Knowledge in Nutrition. 11th ed. Cambridge, Massachusetts: Wiley-Blackwell; 2020:73-91.[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Vitamin A. [Updated 2020 Nov 4]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548165[↩][↩][↩][↩]
- Jing J., Isoherranen N., Robinson-Cohen C., Petrie I., Kestenbaum B.R., Yeung C.K. Chronic Kidney Disease Alters Vitamin A Homeostasis via Effects on Hepatic RBP4 Protein Expression and Metabolic Enzymes. Clin. Transl. Sci. 2016;9:207–215. doi: 10.1111/cts.12402[↩][↩]
- Clugston R.D., Blaner W.S. The adverse effects of alcohol on vitamin A metabolism. Nutrients. 2012;4:356–371. doi: 10.3390/nu4050356[↩][↩]
- O’Donnell J. Polar hysteria: An expression of hypervitaminosis A.Am JTher. 2004;11(6):507–16.[↩][↩][↩]
- Mawson A. Mefloquine use, psychosis, and violence: A retinoid toxicityhypothesis.Med Sci Monitor. 2013;19:579–83.[↩][↩][↩]
- Layton A. The use of isotretinoin in acne. Dermatoendocrinology. 2009;1:162–169. doi: 10.4161/derm.1.3.9364[↩]
- Kuenzli S, Saurat JH. Retinoids for the treatment of psoriasis: outlook for the future. Curr Opin Investig Drugs. 2001 May;2(5):625-30.[↩]
- Patatanian E., Thompson D.F. Retinoic acid syndrome: A review. J. Clin. Pharm. Ther. 2008;33:331–338. doi: 10.1111/j.1365-2710.2008.00935.x[↩]
- Vitamin A. https://ods.od.nih.gov/factsheets/VitaminA-Consumer[↩][↩]
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Vitamin A. [Updated 2013 Dec 3]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548165 [↩]
- García-Muñoz P, Bernal-Bellido C, Marchal-Santiago A, et al. Liver cir-rhosis from chronic hypervitaminosis A resulting in a liver transplantation:A case report.Transpl Proc. 2019;51(1):90–1.[↩][↩][↩][↩]
- Challem JJ. Teratogenicity of high vitamin A intake. N Engl J Med. 1996 May 2;334(18):1196-7.[↩][↩][↩][↩]
- D’Ambrosio D.N., Clugston R.D., Blaner W.S. Vitamin A metabolism: An update. Nutrients. 2011;3:63–103. doi: 10.3390/nu3010063[↩]
- Johnson EJ, Russell RM. Beta-Carotene. In: Coates PM, Betz JM, Blackman MR, et al., eds. Encyclopedia of Dietary Supplements. 2nd ed. London and New York: Informa Healthcare; 2010:115-20.[↩][↩][↩]
- Ross CA. Vitamin A. In: Coates PM, Betz JM, Blackman MR, et al., eds. Encyclopedia of Dietary Supplements. 2nd ed. London and New York: Informa Healthcare; 2010:778-91.[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Ross A. Vitamin A and Carotenoids. In: Shils M, Shike M, Ross A, Caballero B, Cousins R, eds. Modern Nutrition in Health and Disease. 10th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2006:351-75.[↩][↩][↩][↩]
- Kam R.K., Deng Y., Chen Y., Zhao H. Retinoic acid synthesis and functions in early embryonic development. Cell. Biosci. 2012;2:11. doi: 10.1186/2045-3701-2-11[↩]
- Vitamin A. https://lpi.oregonstate.edu/mic/vitamins/vitamin-A[↩]
- National Institute of Health. Vitamin A. https://ods.od.nih.gov/factsheets/VitaminA-HealthProfessional[↩]
- Kelly M.E., Ramkumar S., Sun W., Colon Ortiz C., Kiser P.D., Golczak M., von Lintig J. The Biochemical Basis of Vitamin A Production from the Asymmetric Carotenoid β-Cryptoxanthin. ACS Chem. Biol. 2018;13:2121–2129. doi: 10.1021/acschembio.8b00290[↩]
- Ma G., Zhang L., Iida K., Madono Y., Yungyuen W., Yahata M., Yamawaki K., Kato M. Identification and quantitative analysis of β-cryptoxanthin and β-citraurin esters in Satsuma mandarin fruit during the ripening process. Food Chem. 2017;234:356–364. doi: 10.1016/j.foodchem.2017.05.015[↩]
- Maiani G., Castón M.J., Catasta G., Toti E., Cambrodón I.G., Bysted A., Granado-Lorencio F., Olmedilla-Alonso B., Knuthsen P., Valoti M., et al. Carotenoids: Actual knowledge on food sources, intakes, stability and bioavailability and their protective role in humans. Mol. Nutr. Food Res. 2009;53(Suppl. 12):S194–S218. doi: 10.1002/mnfr.200800053[↩]
- Jiao Y., Reuss L., Wang Y. β-Cryptoxanthin: Chemistry, Occurrence, and Potential Health Benefits. Curr. Pharmacol. Rep. 2019;5:20–34. doi: 10.1007/s40495-019-00168-7[↩]
- Breithaupt D.E., Bamedi A. Carotenoid esters in vegetables and fruits: A screening with emphasis on beta-cryptoxanthin esters. J. Agric. Food Chem. 2001;49:2064–2070. doi: 10.1021/jf001276t[↩]
- Schlatterer J., Breithaupt D.E. Cryptoxanthin Structural Isomers in Oranges, Orange Juice, and Other Fruits. J. Agric. Food Chem. 2005;53:6355–6361. doi: 10.1021/jf050362w[↩]
- Ross A. Vitamin A. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. Modern Nutrition in Health and Disease. 11th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2014:260-77.[↩]
- Institute of Medicine. Food and Nutrition Board. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. Washington, DC: National Academy Press; 2000. https://nap.nationalacademies.org/read/9810/chapter/1[↩]
- Institute of Medicine, US Panel on Micronutrients. Dietary reference intakes for vitamin A, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. National Academies Press. Washington, DC, 2001. PMID: 25057538 www.ncbi.nlm.nih.gov/pubmed/25057538.[↩][↩]
- Solomons NW. Vitamin A. In: Bowman B, Russell R, eds. Present Knowledge in Nutrition. 9th ed. Washington, DC: International Life Sciences Institute; 2006:157-83.[↩][↩][↩]
- Merck Sharp & Dohme Corp, Merck Manual. Vitamin A. https://www.merckmanuals.com/professional/nutritional-disorders/vitamin-deficiency,-dependency,-and-toxicity/vitamin-a#v884887[↩]
- Institute of Medicine. Food and Nutrition Board. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington, DC: National Academy Press; 2001.[↩][↩]
- Otten JJ, Hellwig JP, Meyers LD, eds. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. Washington, DC: The National Academies Press; 2006.[↩]
- Food Labeling: Revision of the Nutrition and Supplement Facts Labels and Serving Sizes of Foods That Can Reasonably Be Consumed at One Eating Occasion; Dual-Column Labeling; Updating, Modifying, and Establishing Certain Reference Amounts Customarily Consumed; Serving Size for Breath Mints; and Technical Amendments; Proposed Extension of Compliance Dates. https://www.federalregister.gov/documents/2017/10/02/2017-21019/food-labeling-revision-of-the-nutrition-and-supplement-facts-labels-and-serving-sizes-of-foods-that[↩][↩][↩]
- Food Labeling: Revision of the Nutrition and Supplement Facts Labels. https://www.federalregister.gov/documents/2016/05/27/2016-11867/food-labeling-revision-of-the-nutrition-and-supplement-facts-labels[↩]
- Converting Units of Measure for Folate, Niacin, and Vitamins A, D, and E on the Nutrition and Supplement Facts Labels: Guidance for Industry. https://www.fda.gov/media/129863/download[↩][↩]
- Vitamin A. https://ods.od.nih.gov/factsheets/VitaminA-HealthProfessional[↩][↩]
- Haskell MJ. The challenge to reach nutritional adequacy for vitamin A: β-carotene bioavailability and conversion–evidence in humans. Am J Clin Nutr. 2012 Nov;96(5):1193S-203S. doi: 10.3945/ajcn.112.034850[↩]
- Tanumihardjo SA, Russell RM, Stephensen CB, Gannon BM, Craft NE, Haskell MJ, Lietz G, Schulze K, Raiten DJ. Biomarkers of Nutrition for Development (BOND)-Vitamin A Review. J Nutr. 2016 Sep;146(9):1816S-48S. doi: 10.3945/jn.115.229708[↩]
- Food and Nutrition Board, Institute of Medicine. Vitamin A. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington, D.C.: National Academy Press; 2001:65-126. https://nap.nationalacademies.org/read/10026/chapter/6[↩]
- Institute of Medicine. Food and Nutrition Board. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington, DC: National Academy Press; 2001. https://www.nap.edu/read/10026/chapter/1[↩]
- Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. https://www.nap.edu/read/9810/chapter/1[↩]
- Institute of Medicine. Food and Nutrition Board. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington, DC: National Academy Press; 2001. https://nap.nationalacademies.org/read/10026/chapter/1[↩]
- Grune T, Lietz G, Palou A, Ross AC, Stahl W, Tang G, Thurnham D, Yin SA, Biesalski HK. Beta-carotene is an important vitamin A source for humans. J Nutr. 2010 Dec;140(12):2268S-2285S. doi: 10.3945/jn.109.119024[↩]
- Rodahl K, Moore T. The vitamin A content and toxicity of bear and seal liver. Biochem J. 1943 Jul;37(2):166-8. doi: 10.1042/bj0370166 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1257872/pdf/biochemj00974-0009.pdf[↩][↩]
- Lindhard,J.[1913]. Med”.Gronland,41,461.[↩]
- Ribaya-Mercado JD, Blumberg JB. Vitamin A: is it a risk factor for osteoporosis and bone fracture? Nutr Rev. 2007 Oct;65(10):425-38. doi: 10.1111/j.1753-4887.2007.tb00268.x[↩]
- Goodman GE, Thornquist MD, Balmes J, Cullen MR, Meyskens FL Jr, Omenn GS, Valanis B, Williams JH Jr. The Beta-Carotene and Retinol Efficacy Trial: incidence of lung cancer and cardiovascular disease mortality during 6-year follow-up after stopping beta-carotene and retinol supplements. J Natl Cancer Inst. 2004 Dec 1;96(23):1743-50. doi: 10.1093/jnci/djh320[↩][↩]
- Alpha-Tocopherol, Beta Carotene Cancer Prevention Study Group. The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. N Engl J Med. 1994 Apr 14;330(15):1029-35. doi: 10.1056/NEJM199404143301501[↩]
- Chea EP, Lopez MJ, Milstein H. Vitamin A. [Updated 2020 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482362[↩]
- Persson B, Tunell R, Ekengren K. 1965. Chronic vitamin A intoxication during the first half year of life. Acta Paediatr Scand 54:49–60. https://www.ncbi.nlm.nih.gov/pubmed/14248225[↩]
- Bush ME, Dahms BB. 1984. Fatal hypervitaminosis A in a neonate. Arch Pathol Lab Med 108:838–842. https://www.ncbi.nlm.nih.gov/pubmed/6548125[↩]
- Carpenter TO, Pettifor JM, Russell RM, Pitha J, Mobarhan S, Ossip MS, Wainer S, Anast CS. 1987. Severe hypervitaminosis A in siblings: Evidence of variable tolerance to retinol intake. J Pediatr 111:507–512. https://www.ncbi.nlm.nih.gov/pubmed/3655980[↩][↩]
- Sy, Alexander & Kumar, Smriti & Steinberg, Jonathan & Garcia-Buitrago, Monica & Benitez, Leopoldo. (2020). Liver Damage due to Hypervitaminosis. ACG Case Reports Journal. 7. e00431. 10.14309/crj.0000000000000431[↩]
- Lowe N.J., David M. New retinoids for dermatologic diseases. Uses and toxicity. Dermatol. Clin. 1988;6:539–552. doi: 10.1016/S0733-8635(18)30632-6[↩]
- Setty O.H., Misra U.K. Effect of heparin on vitamin A induced hyperlipidemia in rats. Int. J. Vitam. Nutr. Res. 1981;51:325–330.[↩]