Contents
What is microscopic colitis
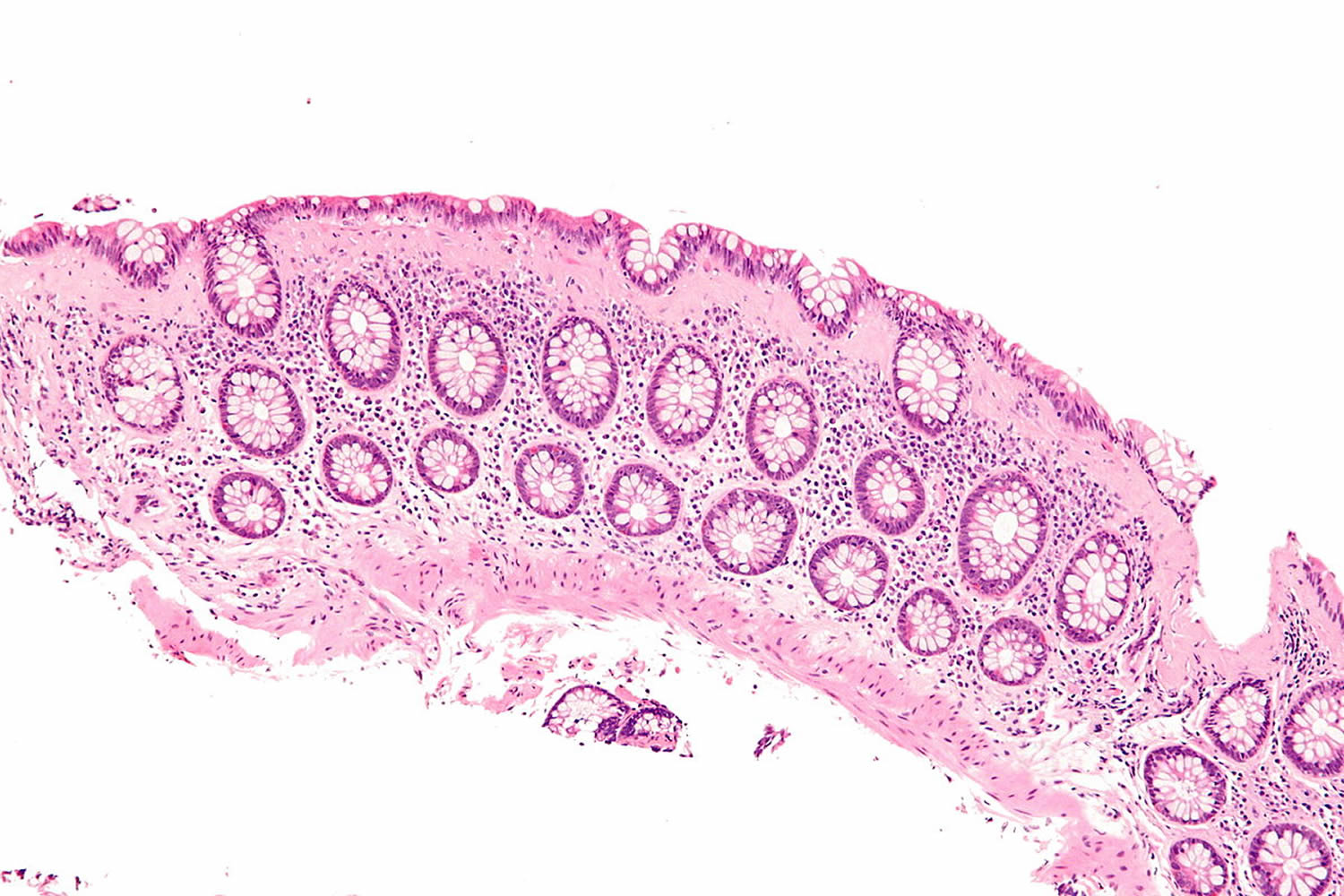
Microscopic colitis is a chronic inflammation of the colon (large intestine) that a health care provider can see only with a microscope because the tissue may appear normal with colonoscopy or flexible sigmoidoscopy 1). Inflammation is the body’s normal response to injury, irritation, or infection of tissues. Microscopic colitis is a type of inflammatory bowel disease—the general name for diseases that cause irritation and inflammation in the intestines. Microscopic colitis causes persistent watery diarrhea.
The two types of microscopic colitis are collagenous colitis and lymphocytic colitis. Health care providers often use the term microscopic colitis to describe both types because their symptoms and treatments are the same. Some scientists believe that collagenous colitis and lymphocytic colitis may be different phases of the same condition rather than separate conditions.
In both types of microscopic colitis, an increase in the number of lymphocytes, a type of white blood cell, can be seen in the epithelium—the layer of cells that lines the colon. An increase in the number of white blood cells is a sign of inflammation. The two types of colitis affect the colon tissue in slightly different ways:
- Lymphocytic colitis. The number of lymphocytes is higher, and the tissues and lining of the colon are of normal thickness.
- Collagenous colitis. The layer of collagen, a threadlike protein, underneath the epithelium builds up and becomes thicker than normal.
When looking through a microscope, the health care provider may find variations in lymphocyte numbers and collagen thickness in different parts of the colon. Researchers believe collagenous colitis and lymphocytic colitis may be different phases of the same condition. Symptoms, testing and treatment are the same for both subtypes.
Table 1. Histological key features of microscopic colitis: collagenous colitis and lymphocytic colitis
| Clinical groups | Morphology subgroups | Increased mononuclear inflammation of lamina propria | Thickness of collagenous band | Number of IELs |
|---|---|---|---|---|
| Microscopic colitis | Collagenous colitis | Moderately increased | >10 ìm | Normal/slightly increased |
| Lymphocytic colitis | Moderately increased | Normal/slightly increased | >20 IELs/100 cells |
Note: IELs, intraepithelial lymphocytes.
The reported prevalence rates of collagenous colitis and lymphocytic colitis are 42 and 69 per 100,000 persons, respectively 3) and the incidence rates of these diseases in patients under investigation for chronic diarrhea are higher, from 10% to 20% 4). Established risk factors include increasing age, with 75% of the people affected being over 50 years old 5). The ratio of women to men is 2.4 to 1, and women have a proportionally greater risk of collagenous colitis 6). A recent French study reported that the incidence of microscopic colitis was 7.9 per 100,000 inhabitants, similar to the incidence of Crohn’s disease in that population 7). Although a history of smoking is associated with transient risk, current smoking increases the risk of persistent disease 8) and collagenous colitis diagnosis at a young age 9). In addition, a history of autoimmune disease, including diabetes mellitus, rheumatoid arthritis, and celiac disease, is associated with microscopic colitis 10). Celiac disease is associated with a 50 to 70 times greater risk of microscopic colitis, especially in middle-aged women, and with severe villous atrophy 11). In a multicenter, prospective study of 433 patients with microscopic colitis or functional diarrhea, Macaigne and colleagues 12) found that microscopic colitis was associated with age over 50 years, nocturnal diarrhea, weight loss, new medications and autoimmune disease.
Over the last years, publications have proposed an additional subtype of microscopic colitis, microscopic colitis incomplete, comprising incomplete collagenous colitis and incomplete lymphocytic colitis 13). Microscopic colitis incomplete embraces patients with clinical features of microscopic colitis from whom biopsies fall short of fulfilling the specific histological criteria of collagenous colitis and lymphocytic colitis. Fraser 14) suggested the term “microscopic colitis not otherwise specified” for this group of patients. The histological key features of microscopic colitis and microscopic colitis incomplete are shown in Table 2.
Table 2. Histological key features of microscopic colitis (collagenous colitis and lymphocytic colitis) and MCi (collagenous colitis incomplete and lymphocytic colitis incomplete)
| Clinical groups | Morphology subgroups | Increased mononuclear inflammation of lamina propria | Thickness of collagenous band | Number of IELs |
|---|---|---|---|---|
| Microscopic colitis | Collagenous colitis | Moderately increased | >10 ìm | Normal/slightly increased |
| Lymphocytic colitis | Moderately increased | Normal/slightly increased | >20 IELs/100 cells | |
| Microscopic colitis incomplete | Collagenous colitis incomplete and lymphocytic colitis incomplete | Slightly increased | >5 and <10 ìm | >10 IELs and <20 IELs |
Note: IELs, intraepithelial lymphocytes.
As patients with microscopic colitis incomplete seem to benefit from medical treatment with a clinical response equal to patients with microscopic colitis, it has been suggested to include microscopic colitis incomplete as a subgroup of microscopic colitis 16).
The symptoms of microscopic colitis can come and go frequently. Sometimes the symptoms resolve on their own. If not, your doctor can suggest a number of effective medications.
People are more likely to get microscopic colitis if they:
- are 50 years of age or older
- are female
- have an autoimmune disease
- smoke cigarettes, especially people ages 16 to 44 17)
- use medications that have been linked to the disease
Does microscopic colitis increase the risk of colon cancer?
No. Unlike the other inflammatory bowel diseases, such as Crohn’s disease and ulcerative colitis, microscopic colitis does not increase a person’s risk of getting colon cancer. Most people are successfully treated for microscopic colitis.
Is microscopic colitis an autoimmune disease?
Scientists aren’t sure what causes microscopic colitis, but there is a strong association of microscopic colitis with autoimmune disorders, such as celiac disease, polyarthritis, and thyroid disorders (see below). Up to twenty to 60% of patients with lymphocytic colitis and 17%-40% of patients with collagenous colitis have autoimmune disease 18). In fact, histological features of Microscopic colitis in the colon are present in 30% of patients with celiac disease. While no specific genetic mutations have been identified as direct cause of Microscopic colitis, some studies have found common genetic abnormalities. For instance, there is an increased prevalence of human leukocyte antigen (HLA) DR3 DQ2 allele in patients with Microscopic colitis, and metalloproteinase 9 gene variations have been associated with collagenous colitis 19).
Autoimmune diseases associated with microscopic colitis include:
- Celiac disease—a condition in which people cannot tolerate gluten because it damages the lining of the small intestine and prevents absorption of nutrients. Gluten is a protein found in wheat, rye, and barley.
- Thyroid diseases such as:
- Hashimoto’s disease—a form of chronic, or long lasting, inflammation of the thyroid.
- Graves’ disease—a disease that causes hyperthyroidism. Hyperthyroidism is a disorder that occurs when the thyroid gland makes more thyroid hormone than the body needs.
- Rheumatoid arthritis—a disease that causes pain, swelling, stiffness, and loss of function in the joints when the immune system attacks the membrane lining the joints.
- Psoriasis—a skin disease that causes thick, red skin with flaky, silver-white patches called scales.
The colon
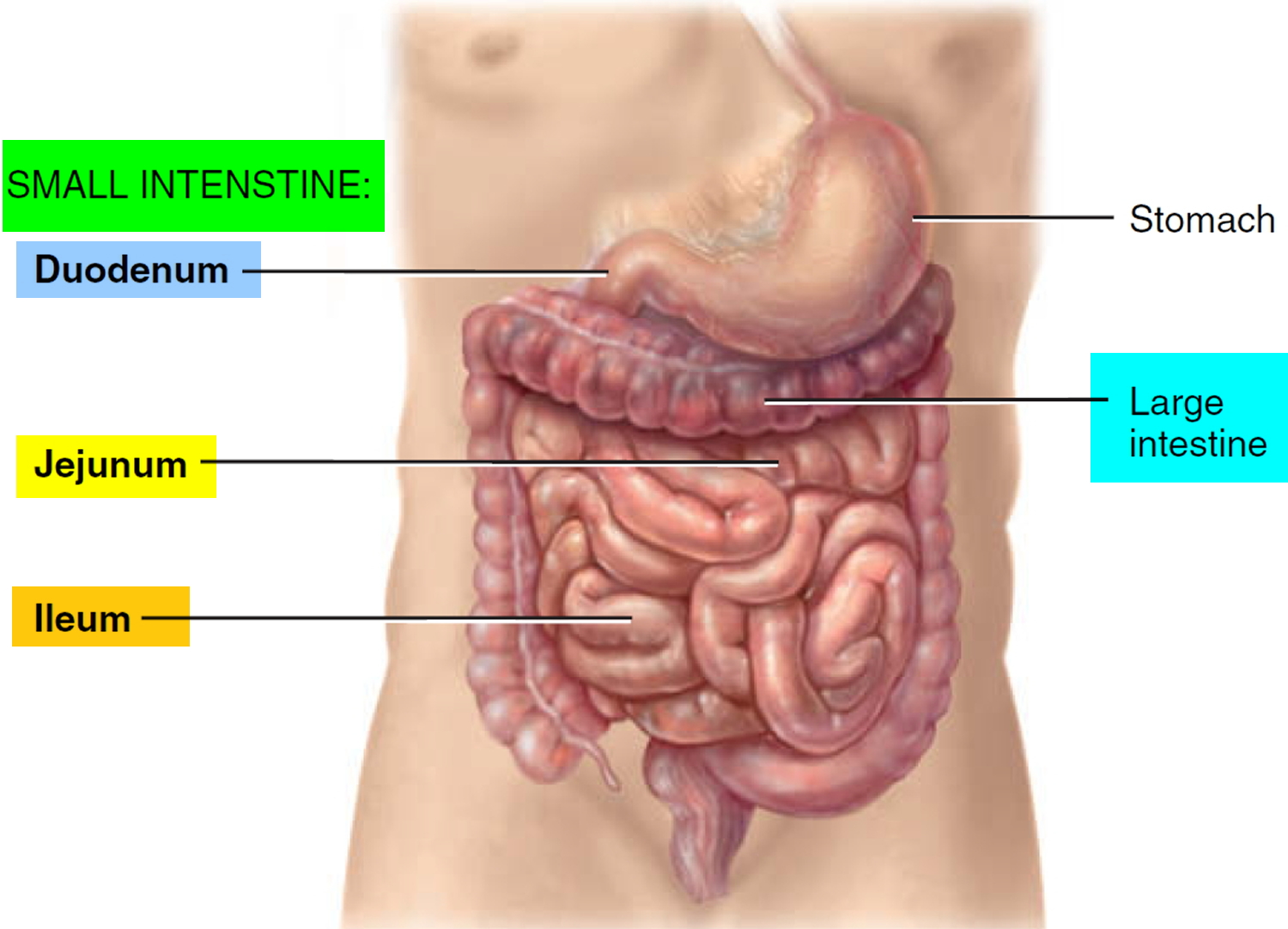
The colon is part of the gastrointestinal (GI) tract, a series of hollow organs joined in a long, twisting tube from the mouth to the anus—a 1-inch-long opening through which stool leaves the body. Organs that make up the GI tract are the:
- mouth
- esophagus
- stomach
- small intestine
- large intestine
- anus
The first part of the GI tract, called the upper GI tract, includes the mouth, esophagus, stomach, and small intestine. The last part of the GI tract, called the lower GI tract, consists of the large intestine and anus. The intestines are sometimes called the bowel.
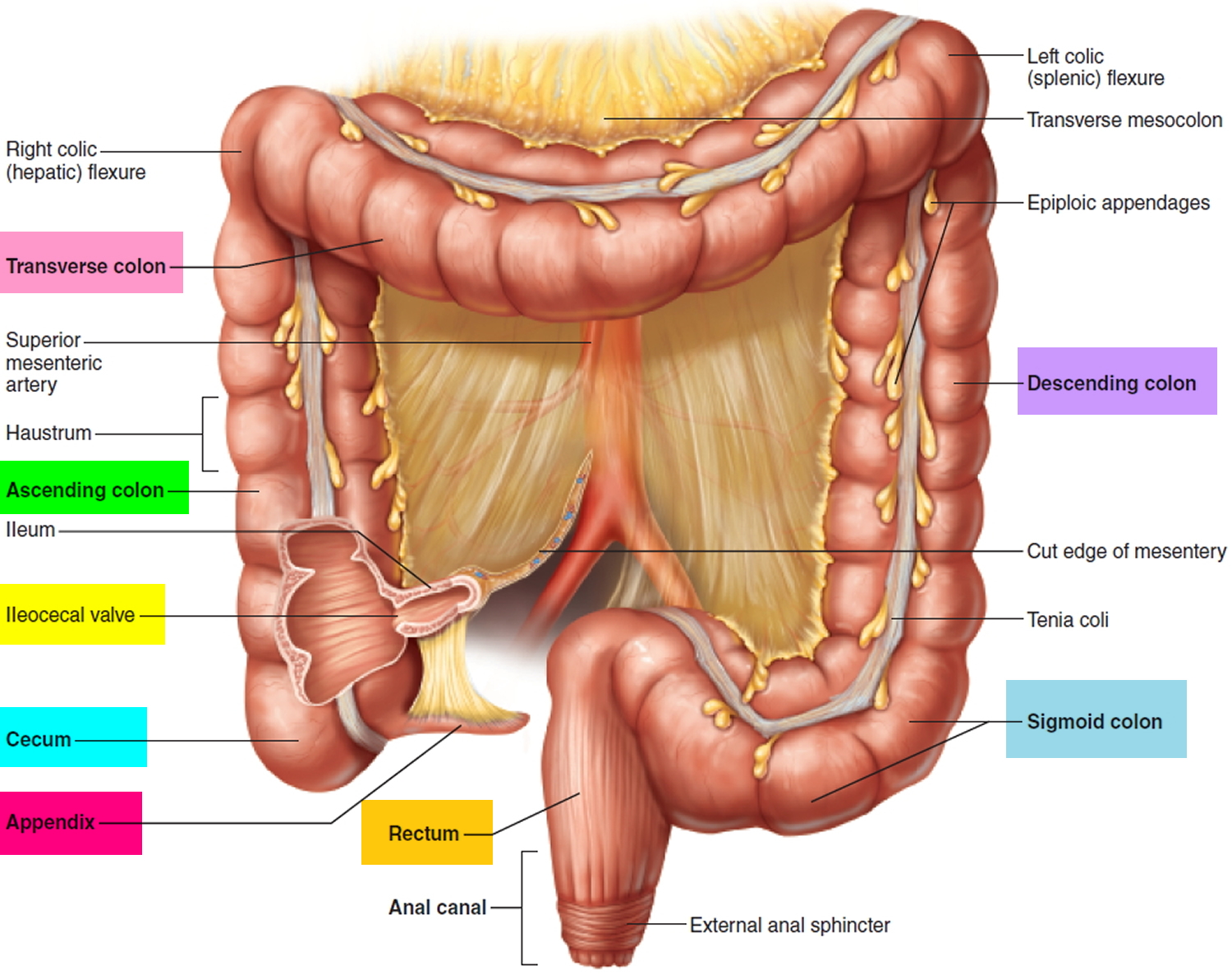
The large intestine is about 5 feet long in adults and includes the colon and rectum. The large intestine changes waste from liquid to a solid matter called stool. Stool passes from the colon to the rectum. The rectum is 6 to 8 inches long in adults and is between the last part of the colon—called the sigmoid colon—and the anus. During a bowel movement, stool moves from the rectum to the anus and out of the body.
Figure 1. Small and large intestines
Figure 2. Large intestine (colon)
Microscopic colitis causes
The exact cause of microscopic colitis is unknown. Several factors may play a role in causing microscopic colitis. However, most scientists believe that microscopic colitis results from an abnormal immune-system response to bacteria that normally live in the colon. Scientists have proposed other causes, including:
- autoimmune diseases
- medications
- infections
- genetic factors
- bile acid malabsorption
Autoimmune Diseases
Sometimes people with microscopic colitis also have autoimmune diseases—disorders in which the body’s immune system attacks the body’s own cells and organs. Autoimmune diseases associated with microscopic colitis include:
- Celiac disease—a condition in which people cannot tolerate gluten because it damages the lining of the small intestine and prevents absorption of nutrients. Gluten is a protein found in wheat, rye, and barley.
- Thyroid diseases such as:
- Hashimoto’s disease—a form of chronic, or long lasting, inflammation of the thyroid.
- Graves’ disease—a disease that causes hyperthyroidism. Hyperthyroidism is a disorder that occurs when the thyroid gland makes more thyroid hormone than the body needs.
- Rheumatoid arthritis—a disease that causes pain, swelling, stiffness, and loss of function in the joints when the immune system attacks the membrane lining the joints.
- Psoriasis—a skin disease that causes thick, red skin with flaky, silver-white patches called scales.
Medications
Researchers have not found that medications cause microscopic colitis. However, they have found links between microscopic colitis and certain medications, most commonly:
- nonsteroidal anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen
- lansoprazole (Prevacid)
- acarbose (Prandase, Precose)
- ranitidine (Tritec, Zantac)
- sertraline (Zoloft)
- ticlopidine (Ticlid)
Other medications linked to microscopic colitis include:
- carbamazepine
- clozapine (Clozaril, FazaClo)
- dexlansoprazole (Kapidex, Dexilant)
- entacapone (Comtan)
- esomeprazole (Nexium)
- flutamide (Eulexin)
- lisinopril (Prinivil, Zestril)
- omeprazole (Prilosec)
- pantoprazole (Protonix)
- paroxetine (Paxil, Pexeva)
- rabeprazole (AcipHex)
- simvastatin (Zocor)
- vinorelbine (Navelbine)
Infections
- Bacteria. Some people get microscopic colitis after an infection with certain harmful bacteria. Harmful bacteria may produce toxins that irritate the lining of the colon.
- Viruses. Some scientists believe that viral infections that cause inflammation in the GI tract may play a role in causing microscopic colitis.
Genetic Factors
Some scientists believe that genetic factors may play a role in microscopic colitis. Although researchers have not yet found a gene unique to microscopic colitis, scientists have linked dozens of genes to other types of inflammatory bowel disease, including:
- Crohn’s disease—a disorder that causes inflammation and irritation of any part of the GI tract
- Ulcerative colitis—a chronic disease that causes inflammation and ulcers in the inner lining of the large intestine
Bile Acid Malabsorption
Some scientists believe that bile acid malabsorption plays a role in microscopic colitis. Bile acid malabsorption is the intestines’ inability to completely reabsorb bile acids—acids made by the liver that work with bile to break down fats. Bile is a fluid made by the liver that carries toxins and waste products out of the body and helps the body digest fats. Bile acids that reach the colon can lead to diarrhea.
Risk factors for microscopic colitis
Risk factors for microscopic colitis include:
- Age and gender. Microscopic colitis is most common in people ages 50 to 70 and more common in women than men. Some researchers suggest an association with a decrease in hormones in women after menopause.
- Autoimmune disease. People with microscopic colitis sometimes also have an autoimmune disorder, such as celiac disease, thyroid disease, rheumatoid arthritis, type 1 diabetes or psoriasis.
- Genetic link. Research suggests that there may be a connection between microscopic colitis and a family history of irritable bowel syndrome.
- Smoking. Recent research studies have shown an association between tobacco smoking and microscopic colitis, especially in people ages 16 to 44.
Some research studies indicate that using certain medications may increase your risk of microscopic colitis. But not all studies agree. Medications that may be linked to the condition include:
- Aspirin, acetaminophen (Tylenol, others) and ibuprofen (Advil, Motrin IB, others)
- Proton pump inhibitors including lansoprazole (Prevacid), esomeprazole (Nexium), pantoprazole (Protonix), rabeprazole (Aciphex), omeprazole (Prilosec) and dexlansoprazole (Dexilant)
- Acarbose (Precose)
- Flutamide
- Ranitidine (Zantac)
- Selective serotonin reuptake inhibitors (SSRIs) such as sertraline (Zoloft)
- Carbamazepine (Carbatrol, Tegretol)
- Clozapine (Clozaril, Fazaclo)
- Entacapone (Comtan)
- Paroxetine (Paxil, Pexeva)
- Simvastatin (Zocor)
Microscopic colitis prevention
Researchers do not know how to prevent microscopic colitis. However, researchers do believe that people who follow the recommendations of their health care provider may be able to prevent relapses of microscopic colitis.
Microscopic colitis symptoms
The most common symptom of microscopic colitis is chronic, watery, nonbloody diarrhea. Episodes of diarrhea can last for weeks, months, or even years. However, many people with microscopic colitis may have long periods without diarrhea. Other signs and symptoms of microscopic colitis can include:
- Chronic watery diarrhea
- A strong urgency to have a bowel movement or a need to go to the bathroom quickly
- Pain, cramping, or bloating in the abdomen—the area between the chest and the hips—that is usually mild
- Weight loss
- Fecal incontinence—accidental passing of stool or fluid from the rectum—especially at night
- Nausea
- Dehydration—a condition that results from not taking in enough liquids to replace fluids lost through diarrhea
The symptoms of microscopic colitis can come and go frequently. Sometimes, the symptoms go away without treatment.
Microscopic colitis diagnosis
A pathologist—a doctor who specializes in examining tissues to diagnose diseases—diagnoses microscopic colitis based on the findings of multiple biopsies taken throughout the colon. Biopsy is a procedure that involves taking small pieces of tissue for examination with a microscope. The pathologist examines the colon tissue samples in a lab. Many patients can have both lymphocytic colitis and collagenous colitis in different parts of their colon.
To help diagnose microscopic colitis, a gastroenterologist—a doctor who specializes in digestive diseases—begins with:
- a medical and family history
- a physical exam
The gastroenterologist may perform a series of medical tests to rule out other bowel diseases—such as irritable bowel syndrome, celiac disease, Crohn’s disease, ulcerative colitis, and infectious colitis—that cause symptoms similar to those of microscopic colitis.
These medical tests include:
- lab tests
- imaging tests of the intestines
- endoscopy of the intestines
Medical and Family History
The gastroenterologist will ask the patient to provide a medical and family history, a review of the symptoms, a description of eating habits, and a list of prescription and over-the-counter medications in order to help diagnose microscopic colitis. The gastroenterologist will also ask the patient about current and past medical conditions.
Physical Exam
A physical exam may help diagnose microscopic colitis and rule out other diseases. During a physical exam, the gastroenterologist usually:
- examines the patient’s body
- taps on specific areas of the patient’s abdomen
Lab Tests
Lab tests may include:
- blood tests
- stool tests
Blood tests. A blood test involves drawing blood at a health care provider’s office or a commercial facility and sending the sample to a lab for analysis. A health care provider may use blood tests to help look for changes in red and white blood cell counts.
Red blood cells. When red blood cells are fewer or smaller than normal, a person may have anemia—a condition that prevents the body’s cells from getting enough oxygen.
White blood cells. When the white blood cell count is higher than normal, a person may have inflammation or infection somewhere in the body.
Stool tests. A stool test is the analysis of a sample of stool. A health care provider will give the patient a container for catching and storing the stool. The patient returns the sample to the health care provider or a commercial facility that will send the sample to a lab for analysis. Health care providers commonly order stool tests to rule out other causes of GI diseases, such as different types of infections—including bacteria or parasites—or bleeding, and help determine the cause of symptoms.
Imaging Tests of the Intestines
Imaging tests of the intestines may include the following:
- computerized tomography (CT) scan
- magnetic resonance imaging (MRI)
- upper GI series
Specially trained technicians perform these tests at an outpatient center or a hospital, and a radiologist—a doctor who specializes in medical imaging—interprets the images. A patient does not need anesthesia. Health care providers use imaging tests to show physical abnormalities and to diagnose certain bowel diseases, in some cases.
CT scan. CT scans use a combination of x-rays and computer technology to create images. For a CT scan, a health care provider may give the patient a solution to drink and an injection of a special dye, called contrast medium. CT scans require the patient to lie on a table that slides into a tunnel-shaped device where the technician takes the x-rays.
MRI. MRI is a test that takes pictures of the body’s internal organs and soft tissues without using x-rays. Although a patient does not need anesthesia for an MRI, some patients with a fear of confined spaces may receive light sedation, taken by mouth. An MRI may include a solution to drink and injection of contrast medium. With most MRI machines, the patient will lie on a table that slides into a tunnel-shaped device that may be open ended or closed at one end. Some machines allow the patient to lie in a more open space. During an MRI, the patient, although usually awake, must remain perfectly still while the technician takes the images, which usually takes only a few minutes. The technician will take a sequence of images to create a detailed picture of the intestines. During sequencing, the patient will hear loud mechanical knocking and humming noises.
Upper GI series. This test is an x-ray exam that provides a look at the shape of the upper GI tract. A patient should not eat or drink before the procedure, as directed by the health care provider. Patients should ask their health care provider about how to prepare for an upper GI series. During the procedure, the patient will stand or sit in front of an x-ray machine and drink barium, a chalky liquid. Barium coats the upper GI tract so the radiologist and gastroenterologist can see the organs’ shapes more clearly on x-rays. A patient may experience bloating and nausea for a short time after the test. For several days afterward, barium liquid in the GI tract causes white or light-colored stools. A health care provider will give the patient specific instructions about eating and drinking after the test.
Endoscopy of the Intestines
Endoscopy of the intestines may include:
- colonoscopy with biopsy
- flexible sigmoidoscopy with biopsy
- upper GI endoscopy with biopsy
A gastroenterologist performs these tests at a hospital or an outpatient center.
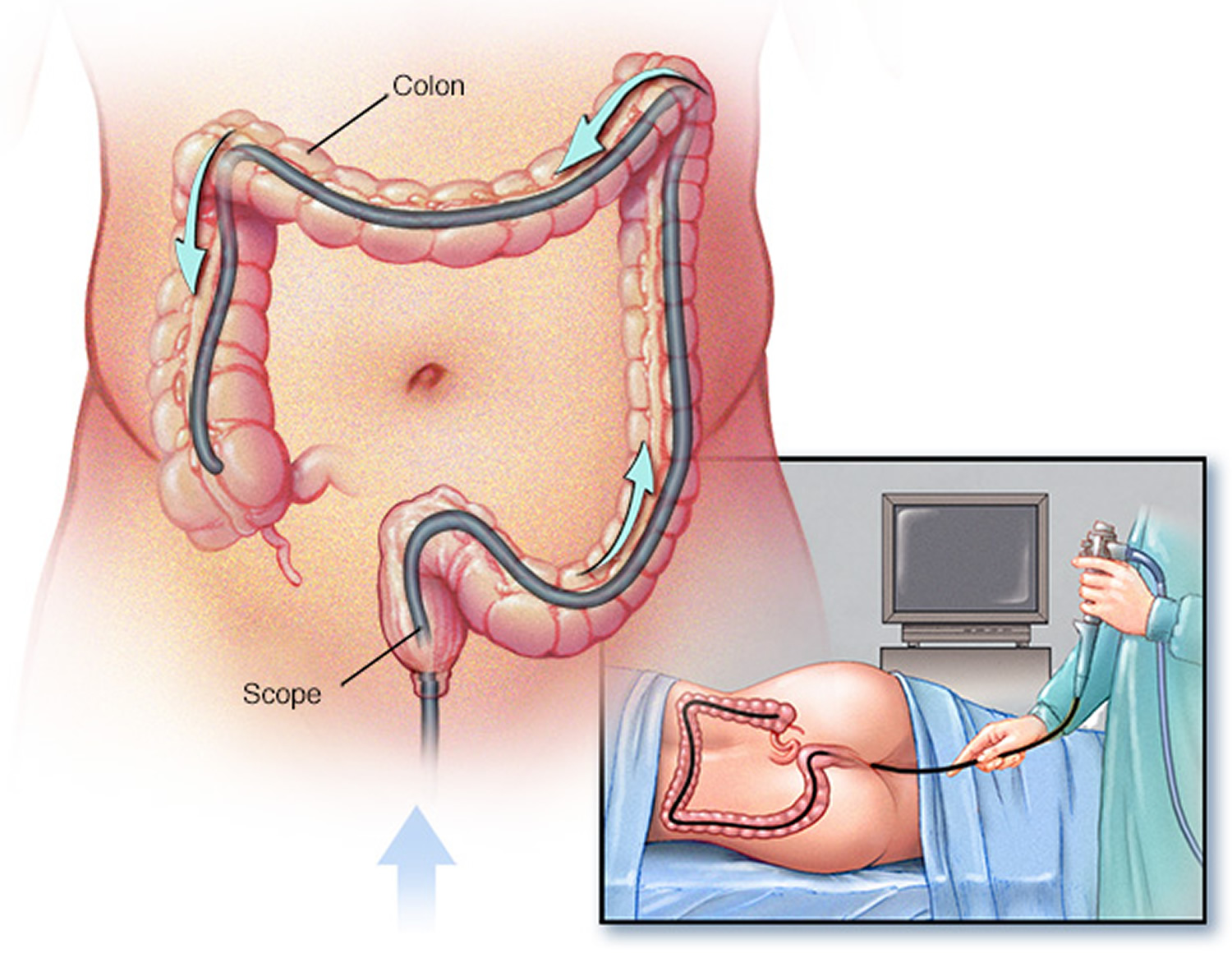
Colonoscopy with biopsy. Colonoscopy is a test that uses a long, flexible, narrow tube with a light and tiny camera on one end, called a colonoscope or scope, to look inside the rectum and entire colon. In most cases, light anesthesia and pain medication help patients relax for the test. The medical staff will monitor a patient’s vital signs and try to make him or her as comfortable as possible. A nurse or technician places an intravenous (IV) needle in a vein in the arm or hand to give anesthesia.
For the test, the patient will lie on a table while the gastroenterologist inserts a colonoscope into the anus and slowly guides it through the rectum and into the colon. The scope inflates the large intestine with air to give the gastroenterologist a better view. The camera sends a video image of the intestinal lining to a computer screen, allowing the gastroenterologist to carefully examine the tissues lining the colon and rectum. The gastroenterologist may move the patient several times and adjust the scope for better viewing. Once the scope has reached the opening to the small intestine, the gastroenterologist slowly withdraws it and examines the lining of the colon and rectum again. A colonoscopy can show irritated and swollen tissue, ulcers, and abnormal growths such as polyps—extra pieces of tissue that grow on the lining of the intestine. If the lining of the rectum and colon appears normal, the gastroenterologist may suspect microscopic colitis and will biopsy multiple areas of the colon.
A health care provider will provide written bowel prep instructions to follow at home before the test. The health care provider will also explain what the patient can expect after the test and give discharge instructions.
Figure 3. Colonoscopy
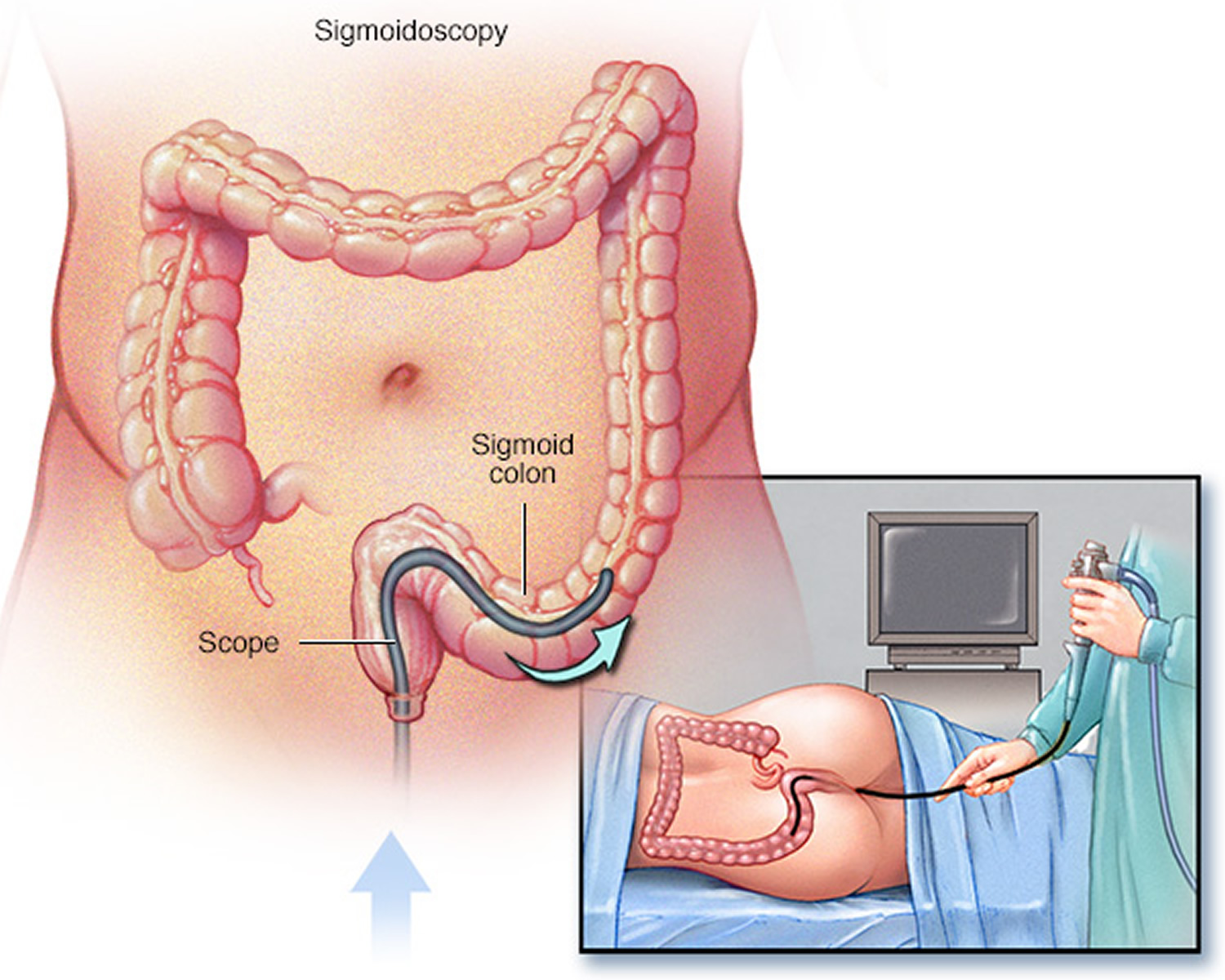
Flexible sigmoidoscopy with biopsy. Flexible sigmoidoscopy is a test that uses a flexible, narrow tube with a light and tiny camera on one end, called a sigmoidoscope or scope, to look inside the rectum and the sigmoid colon. A patient does not usually need anesthesia.
For the test, the patient will lie on a table while the gastroenterologist inserts the sigmoidoscope into the anus and slowly guides it through the rectum and into the sigmoid colon. The scope inflates the large intestine with air to give the gastroenterologist a better view. The camera sends a video image of the intestinal lining to a computer screen, allowing the gastroenterologist to carefully examine the tissues lining the sigmoid colon and rectum. The gastroenterologist may ask the patient to move several times and adjust the scope for better viewing. Once the scope reaches the end of the sigmoid colon, the gastroenterologist slowly withdraws it while carefully examining the lining of the sigmoid colon and rectum again.
The gastroenterologist will look for signs of bowel diseases and conditions such as irritated and swollen tissue, ulcers, and polyps. If the lining of the rectum and colon appears normal, the gastroenterologist may suspect microscopic colitis and will biopsy multiple areas of the colon.
A health care provider will provide written bowel prep instructions to follow at home before the test. The health care provider will also explain what the patient can expect after the test and give discharge instructions.
Figure 4. Sigmoidoscopy
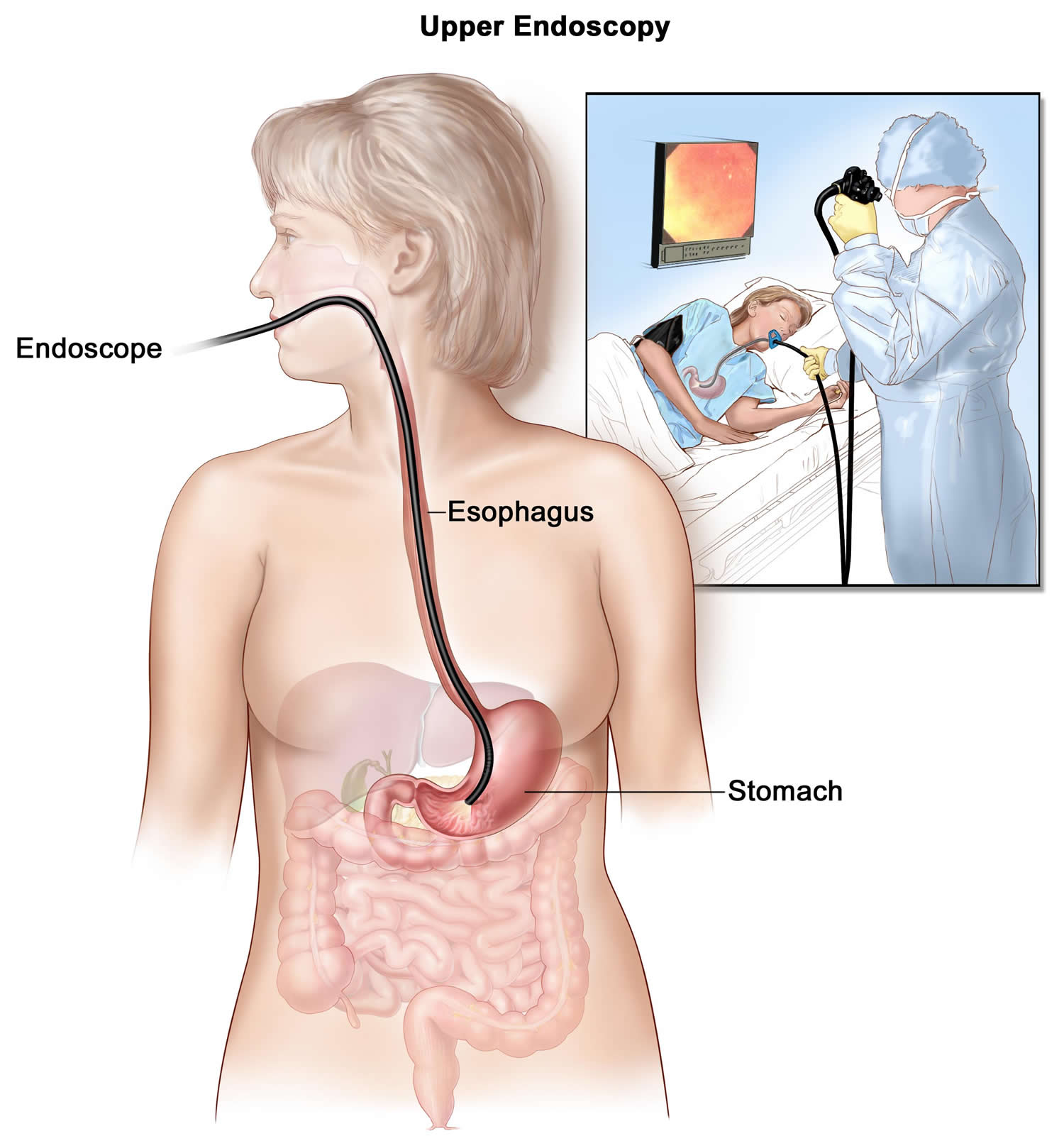
Upper GI endoscopy with biopsy. Upper GI endoscopy is a test that uses a flexible, narrow tube with a light and tiny camera on one end, called an endoscope or a scope, to look inside the upper GI tract. The gastroenterologist carefully feeds the endoscope down the esophagus and into the stomach and first part of the small intestine, called the duodenum. A small camera mounted on the endoscope transmits a video image to a monitor, allowing close examination of the intestinal lining. A health care provider may give a patient a liquid anesthetic to gargle or may spray anesthetic on the back of the patient’s throat. A health care provider will place an IV needle in a vein in the arm or hand to administer sedation. Sedatives help patients stay relaxed and comfortable. This test can show blockages or other conditions in the upper small intestine. A gastroenterologist may biopsy the lining of the small intestine during an upper GI endoscopy.
Figure 5. Upper GI endoscopy
Microscopic colitis treatment
Treatment depends on the severity of symptoms. The gastroenterologist will:
- review the medications the person is taking
- make recommendations to change or stop certain medications
- recommend that the person quit smoking
The gastroenterologist may prescribe medications to help control symptoms. Medications are almost always effective in treating microscopic colitis. The gastroenterologist may recommend eating, diet, and nutrition changes. In rare cases, the gastroenterologist may recommend surgery.
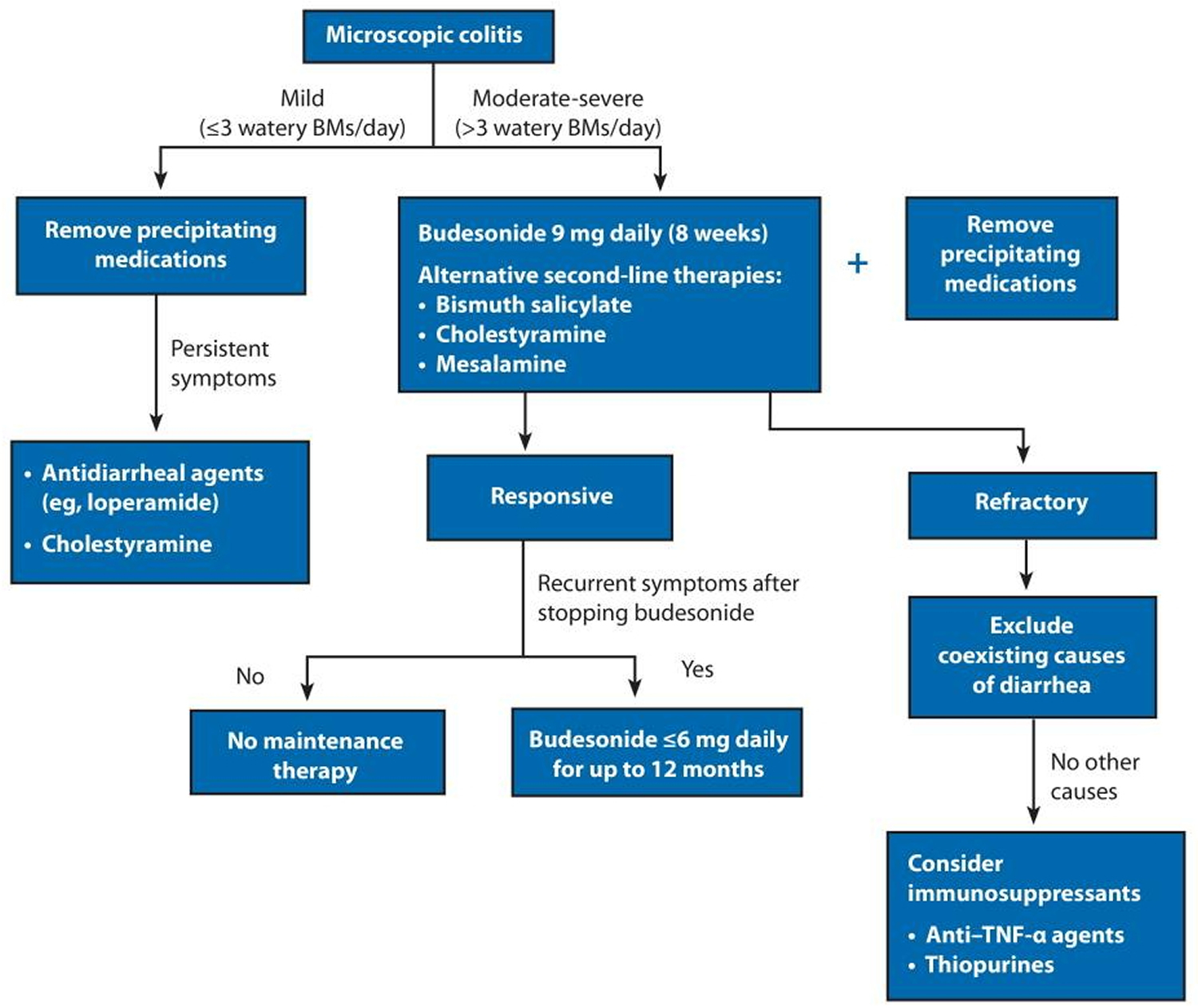
Figure 6. An algorithm of diagnostic and therapeutic recommendations for patients with microscopic colitis
Note: BMs, bowel movements; TNF, tumor necrosis factor
[Source 20)]Medications
The gastroenterologist may prescribe one or more of the following:
- antidiarrheal medications such as bismuth subsalicylate (Kaopectate, Pepto-Bismol), diphenoxylate/atropine (Lomotil), and loperamide
- corticosteroids such as budesonide (Entocort) and prednisone
- anti-inflammatory medications such as mesalamine and sulfasalazine (Azulfidine)
- cholestyramine resin (Locholest, Questran)—a medication that blocks bile acids
- antibiotics such as metronidazole (Flagyl) and erythromycin
- immunomodulators such as mercaptopurine (Purinethol), azathioprine (Azasan, Imuran), and methotrexate (Rheumatrex, Trexall)
- anti-TNF therapies such as infliximab (Remicade) and adalimumab (Humira)
Corticosteroids are medications that decrease inflammation and reduce the activity of the immune system. These medications can have many side effects. Scientists have shown that budesonide is safer, with fewer side effects, than prednisone. Most health care providers consider budesonide the best medication for treating microscopic colitis.
Patients with microscopic colitis generally achieve relief through treatment with medications, although relapses can occur. Some patients may need long-term treatment if they continue to have relapses.
Randomized, controlled trials and meta-analyses favor budesonide for induction of clinical remission 21). A Cochrane systematic review reported budesonide to induce and to maintain response in collagenous colitis over 6 months with a number needed to treat of 2 per outcome. A minority of patients achieve histologic remission. Similar response rates were seen in lymphocytic colitis to induce response and a number needed to treat of 3 22). Budesonide improves quality-of-life scores using the gastrointestinal quality-of-life index 23). American Gastroenterological Association guidelines recommend an 8-week course of budesonide as first-line therapy for induction of clinical remission based on a meta-analysis of 6 studies showing a net beneficial effect and 152% increase in the likelihood of remission over 6 to 8 months 24). Data supporting the use of oral prednisolone for induction of remission are modest, so its use is not recommended as first-line treatment, particularly considering the side-effect burden associated with corticosteroids. An analysis of 17 patients treated with prednisolone vs 63 with budesonide showed lower remission rates and increased relapse with prednisolone 25).
Clinical relapse after stopping budesonide is common and reported in 40% to 81% as soon as 2 weeks after withdrawal 26). Analysis of predictors of recurrence identified risk factors, including older patients (>60 years), longer duration of symptoms (>12 months), and high daily stool frequency (>5/day). Maintenance therapy with oral budesonide may be required to restore quality of life and maintain clinical remission in a proportion of patients 27). Maintenance therapy with 4.5 mg of budesonide daily was associated with maintenance of remission, sustained improvement in quality-of-life scores for collagenous colitis patients, and nonserious adverse effects in 7 of 44 patients 28). Little research has examined the success rates of budesonide for maintenance of remission in lymphocytic colitis. Although minimal side effects have been reported in microscopic colitis during budesonide therapy 29), the association between long-term budesonide use and reduced bone density scores in Crohn’s disease 30) underlines the importance of monitoring bone health in these patients. For maintenance, the lowest effective dose of budesonide should be used. Consideration should also be given to the specific budesonide formulation used. The preferred form of budesonide is absorbed in the ileum and right colon, rather than the alternative, which is associated with mainly left colon absorption and, hence, may be less effective in microscopic colitis 31).
The American Gastroenterological Association recommends that treatment with mesalamine or bismuth subsalicylate should be considered over no treatment when budesonide is contraindicated or fails 32). Treatment with bismuth subsalicylate was associated with favorable clinical outcomes in a small open-label study of lymphocytic colitis and collagenous colitis resulting in clinical and histologic responses 33). Clinical efficacy studies of mesalamine have yielded mixed results, finding this therapy inferior to budesonide for induction of remissio 34). Although mesalamine is recommended as second-line therapy in microscopic colitis, the clinical data available do not strongly support this recommendation. In lymphocytic colitis, mesalamine in combination with cholestyramine did not significantly increase the likelihood of achieving clinical remission, although in collagenous colitis, dual therapy was associated with a greater chance of remission than mesalamine alone. The modest increased response was offset by adverse effects 35). Despite morphologically normal distal ileum, bile acid malabsorption has been identified in approximately 40% of microscopic colitis patients in 2 studies, with induction of clinical remission following cholestyramine in 19 of 22 patients with abnormal 75Se-homocholic acid taurine scans 36). In the absence of bile acid malabsorption, there is weak evidence for clinical response to cholestyramine. These recommendations (Figure 6 above) are limited by a lack of controlled clinical trials for these drugs, with the exception of bismuth and budesonide, and some mixed results and methodologies in the available data. Standard antidiarrheal agents, including loperamide, may have a role in controlling symptoms in patients with mild clinical disease. Symptomatic improvement may also be provided by the elimination of dietary secretagogues such as caffeine, lactose, and fats.
Refractory microscopic colitis
Some patients may have persistent symptoms despite medical therapy. In these individuals, coexistent conditions such as celiac disease should be first excluded. If contraindicated, or relapse occurs despite budesonide maintenance, immunomodulators (azathioprine and 6-mercaptopurine) are reasonably efficacious in microscopic colitis, although their use may be limited by intolerance in approximately one-third of patients in this setting 37). Methotrexate has been used with mixed results in retrospective and prospective analyses, although inadequate power may have influenced the outcome 38). Similarly, calcineurin inhibitors have been used in individual reports and were well tolerated, but only 1 patient achieved complete response. These drugs are not currently recommended in refractory microscopic colitis 39).
A case series points to the use of anti–TNF-α agents in refractory disease 40). Excellent early response rates have been reported, with a reduction of daily stool frequency of up to 90% and sustained remission in a proportion of patients 41). One analysis over almost 20 years included 10 patients treated with anti–TNF-α therapy for a median of 4 months, and reported that a proportion of patients achieved partial response to anti–TNF-α therapy. Long-term use in microscopic colitis may not be necessary if a precipitating agent such as a PPI has been identified and discontinued 42).
Colectomy and consequent diversion of the fecal stream have been used to treat a small cohort of patients with medically refractory microscopic colitis. A case of lymphocytic colitis 43) and a case of collagenous colitis 44) successfully treated with colectomy and subsequent fashioning of ileal J-pouch have been reported. Although histologic remission does not always coexist with clinical remission after medical therapy, diversion of the fecal stream resolves histologic changes, which recur after ileostomy reversal 45).
Microscopic colitis diet
To help reduce symptoms, a health care provider may recommend the following dietary changes:
- avoid foods and drinks that contain caffeine or artificial sugars
- drink plenty of liquids to prevent dehydration during episodes of diarrhea
- eat a milk-free diet if the person is also lactose intolerant
- eat a gluten-free diet
People should talk with their health care provider or dietitian about what type of diet is right for them.
A few studies have investigated the potential benefit of probiotics in microscopic colitis without evidence of clinical efficacy to date after treatment with Lactobacillus acidophilus and Bifidobacterium animalis subsp lactis 46). In a study that randomized 26 patients to receive placebo or Boswellia serrata extract, patients with collagenous colitis showed some clinical response, but the lack of histologic response combined with no improved quality-of-life scores means that this approach cannot be currently recommended 47). Further clinical trials would be useful to determine whether probiotics have a place within the clinical paradigm.
Surgery
When the symptoms of microscopic colitis are severe and medications aren’t effective, a gastroenterologist may recommend surgery to remove the colon. Surgery is a rare treatment for microscopic colitis. The gastroenterologist will exclude other causes of symptoms before considering surgery.
Home remedies
Changes to your diet may help relieve diarrhea that you experience with microscopic colitis. Try to:
- Drink plenty of fluids. Water is best, but fluids with added sodium and potassium (electrolytes) may help as well. Try drinking broth or watered-down fruit juice. Avoid beverages that are high in sugar or sorbitol or contain alcohol or caffeine, such as coffee, tea and colas, which may aggravate your symptoms.
- Choose soft, easy-to-digest foods. These include applesauce, bananas, melons and rice. Avoid high-fiber foods such as beans and nuts, and eat only well-cooked vegetables. If you feel as though your symptoms are improving, slowly add high-fiber foods back to your diet.
- Eat several small meals rather than a few large meals. Spacing meals throughout the day may ease diarrhea.
- Avoid irritating foods. Stay away from spicy, fatty or fried foods and any other foods that make your symptoms worse.
References [ + ]