Contents
What is saccharin
Discovered in the US in 1879, saccharin is the oldest artificial sweetener or non-nutritive sweetener. Saccharin is calorie-free and 300 to 400 times sweeter than sugar. Some people find it has a bitter or metallic aftertaste. Saccharin acceptable daily intake (ADI) is 5mg/kg body weight. An acceptable daily intake (ADI) is the maximum amount considered safe to consume each day over the course of your lifetime. Diabetics depend on saccharin as a sugar replacement, and overweight people also rely on saccharin for weight control. Apatite satiety from artificial sweetness encourages reduction of calorie intake.
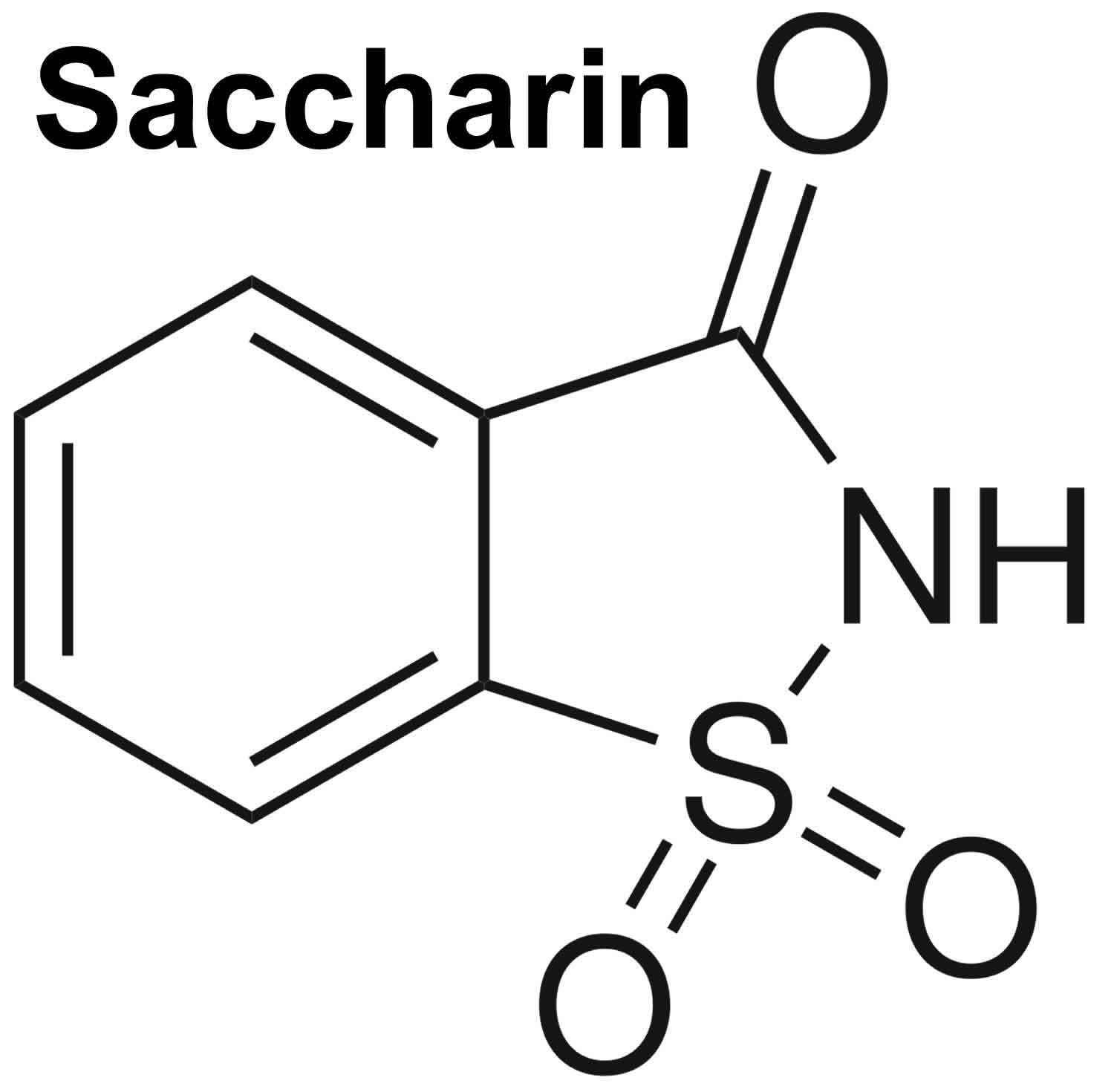
Saccharin (E 954i), sodium saccharin (E 954ii), calcium saccharin [E 954(iii)] and potassium saccharin [E 954(iv)] are authorized as a food additive in the European Union (EU) in accordance with Annex II and Annex III to Regulation (EC) No 1333/2008 1) on food additives and specific purity criteria have been defined in the Commission Regulation (EU) No 231/2012 2).
A wide variety of foods and drinks have saccharin added to them, including baked goods, chewing gum and table top sweeteners.
Saccharin is also used in cosmetic products (such as toothpaste, mouthwash and lip gloss), as well as vitamins and medications.
Saccharin is not broken down when digested. It is slowly absorbed into the system and rapidly excreted, unchanged, by the kidneys.
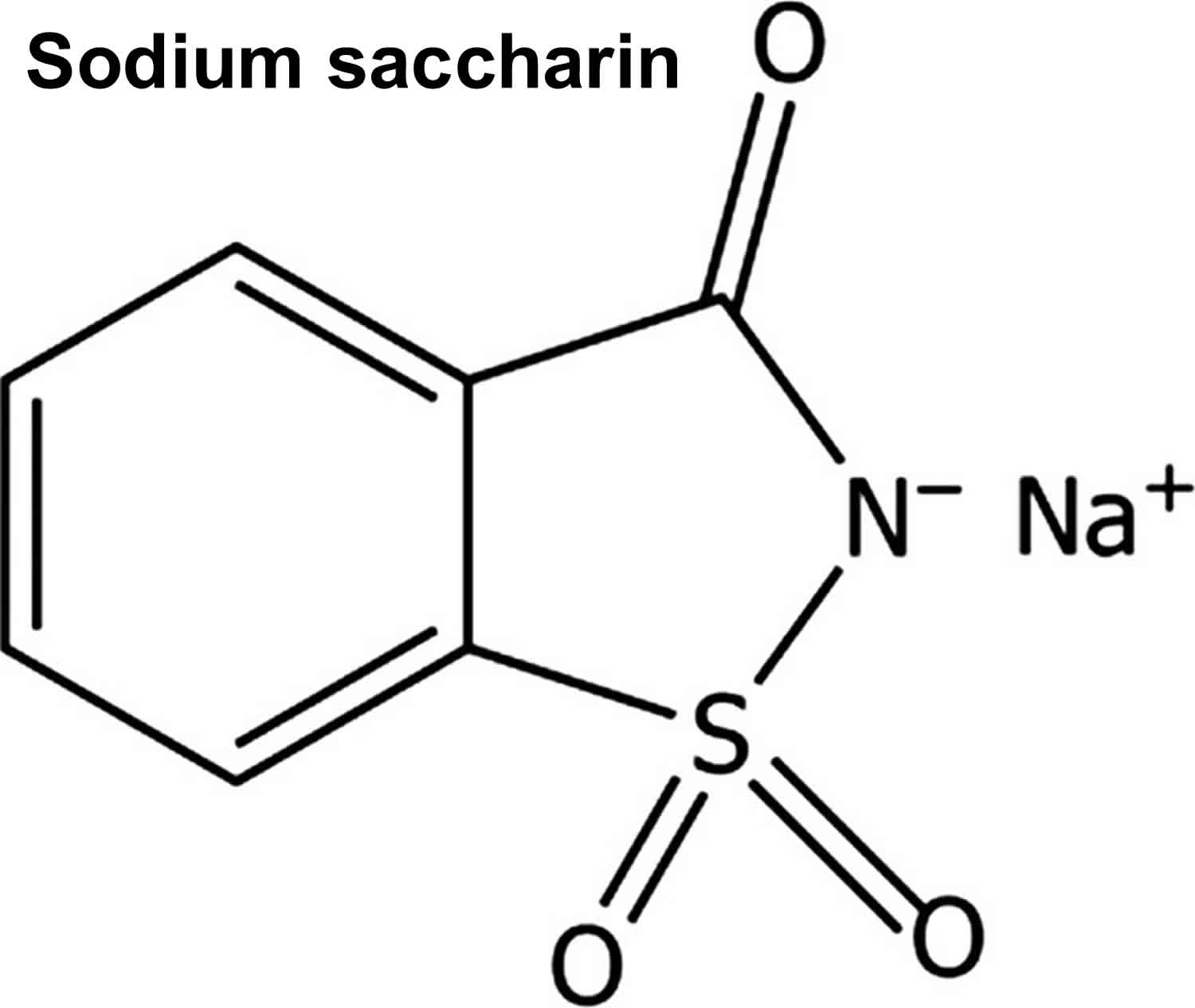
Figure 1. Sodium saccharin
Does saccharin cause cancer?
Questions about artificial sweeteners and cancer arose when early studies showed that cyclamate in combination with saccharin caused bladder cancer in laboratory animals 3). Studies in laboratory rats during the early 1970s linked saccharin with the development of bladder cancer, especially in male rats. After being suspected of causing bladder cancer in rats, the Canadian government banned saccharin as a food additive in 1977 (although restricted access to saccharin as a table top sweetener was maintained). The US government also warned that it could cause cancer.
Since then, many studies have disproved any link to cancer. The results from subsequent carcinogenicity studies (studies that examine whether a substance can cause cancer) of these sweeteners have not provided clear evidence of an association with cancer in humans. Similarly, studies of other U.S. Food and Drug Administration (FDA)-approved sweeteners have not demonstrated clear evidence of an association with cancer in humans.
Mechanistic studies (studies that examine how a substance works in the body) have shown that these results apply only to rats. Human epidemiology studies (studies of patterns, causes, and control of diseases in groups of people) have shown no consistent evidence that saccharin is associated with bladder cancer incidence. Because the bladder tumors seen in rats are due to a mechanism not relevant to humans and because there is no clear evidence that saccharin causes cancer in humans, saccharin was delisted in 2000 from the U.S. National Toxicology Program’s Report on Carcinogens, where it had been listed since 1981 as a substance reasonably anticipated to be a human carcinogen (a substance known to cause cancer) 4). In terms of saccharin dosage, humans would need to drink the equivalent of 800 twelve-ounce diet sodas with saccharin daily to reach the carcinogenic doses that induced rat bladder cancer 5). Experimentally, no harmful effects on humans were observed with consumption of 5 g saccharin daily over 5 months 6). To produce tumors in rats, saccharin is administered in grams per kilo, compared with the milligrams per kilo used when saccharin acts as a sweetener for humans. In a 3000-calorie North American diet, daily consumption approaching 0.5 g (500 mg) by a single individual is highly unlikely 7).
The European Scientific Committee for Food (SCF) re-evaluated the safety of saccharin in 1995 8) and concluded that saccharin did not pose a cancer risk to people. It stated: “While it is unlikely that the tumours in the male rat bladder are of relevance for man, it has not been possible to unequivocally demonstrate this”.
After a complete evaluation of the evidence in 1999, the International Agency for Research on Cancer (IARC) concluded that saccharin could no longer be considered a possible carcinogen in people 9).
Canada lifted the ban on saccharin in 2014 10). Health Canada’s Food Directorate completed a detailed safety assessment of a food additive, saccharin and its salts, specifically calcium saccharin, potassium saccharin and sodium saccharin, concluded that saccharin and its salts are permitted for sale, as saccharin sweeteners, under specific conditions prescribed in Part E of the Food and Drug Regulations. These conditions allow pharmacies to sell saccharin and its salts as sweeteners that can be used by consumers. As no safety concerns were raised through this assessment, it is the intention of Health Canada to enable the food additive use of saccharin and its salts. Health Canada’s evaluation of the available scientific data also supports the safety of saccharin, calcium saccharin, potassium saccharin and sodium saccharin for use in table-top sweeteners. Health Canada intends to propose to modify the List of Permitted Sweeteners and amend Part E of the Food and Drug Regulations in order to enable the use of saccharin, calcium saccharin, potassium saccharin and sodium saccharin as food additives in table-top sweeteners.
However, some health groups maintain that infants, children and pregnant women should avoid it due to the possibility of having an allergic reaction, although there is no evidence to back this up.
Saccharin during pregnancy
No relevant published information was not found regarding the use of saccharin during pregnancy. However, information is available on non-nutritive sweeteners or artificial sweeteners (e.g., aspartame, sucralose, acesulfame K, saccharin, xylitol and steviol glycosides) as a group. Non-nutritive sweeteners or artificial sweeteners are increasingly being consumed by children and pregnant women around the world, yet their long-term health impact is unclear 11).
Few studies have investigated the effects of prenatal non-nutritive sweeteners exposure on obesity-related outcomes in offspring (Table 1). Two recent studies in Canada 12) and Denmark 13) have reported a positive and apparently sex-specific association between daily artificially-sweetened beverage consumption during pregnancy and higher BMI-z scores in male offspring, while a third study in the US found no association 14). There is an emerging body of evidence from human and animal studies suggesting that early-life exposure to non-nutritive sweeteners may have adverse effects on cardio-metabolic health and development 15). However, current evidence remains inconclusive due to the lack of randomized controlled trials, lack of evidence from low and middle-income countries, limitations of observational studies, and lack of mechanistic studies 16). It is difficult to draw firm conclusions regarding the global impact of non-nutritive sweeteners during pregnancy and childhood due to the lack of data on consumption trends, inconsistencies between observational studies, paucity of evidence from low and middle-income countries, and lack of well-designed randomized controlled trials examining prenatal and early-life exposure to non-nutritive sweeteners. Further research is needed to address the limitations of existing studies and critically evaluate the impact of early-life non-nutritive sweeteners exposure. Limited studies in rodents provide complementary evidence on this topic, but these have rarely examined prenatal exposure separately from postnatal exposure, and most have used extreme doses that may not be relevant to humans 17).
Given the increasing popularity of non-nutritive sweeteners among all segments of the population, including pregnant women and children, further research is urgently needed to address this global knowledge gap. Considering the established detrimental effects of dietary sugars and the current uncertainty regarding non-nutritive sweeteners, limiting both is likely the most appropriate recommendation to pregnant women and children at this time, until higher quality evidence is available 18).
Table 1. Summary of human studies evaluating non-nutritive sweetener (NNS) exposure during pregnancy and obesity-related outcomes in offspring.
| Study, Year | Setting, Year of Study Enrollment/Baseline Intake, Study Name | n | Timing of Prenatal NNS Exposure | Duration of Follow Up | NNS Type, Measure, Method of Assessment | Confounders/Covariates Considered, and Comparators for RCTs | Outcomes in Offspring | Main Finding |
|---|---|---|---|---|---|---|---|---|
| Randomized Controlled Trials | ||||||||
| Nakai et al., 2008 19) | Japan, unspecified | 107 pregnant women | 6th month of pregnancy to 9 months postpartum | 13 months | Xylitol gum, 1 pellet at least 4x/day | Maternal age, oral examination (DMFT); child birthweight, sex. Comparator: no gum | Birth weight (examined as a covariate) | No association of infant birth weight and daily maternal xylitol gum |
| Maslova et al., 2013 20) | Denmark, 1996, DNBC | 60,466 pregnant women | Prenatal; 25th week pregnancy | 7 years | ASB, servings, validated FFQ | Maternal BMI, total energy intake, parity, smoking, exercise, gestational weight gain, education and occupation, breastfeeding duration; child gestational age, sex | Birth weight (examined as a covariate) | No association of infant birth weight with maternal ASB intake |
| Prospective Cohort Studies | ||||||||
| Azad et al., 2016 21) | Canada, 2009, CHILD | 2686 pregnant women | Prenatal exposure | 1 year | ASB, servings, validated FFQ | Maternal BMI, total energy intake, diet quality, age, education, smoking, diabetes; infant gestational age, sex, birth weight; breastfeeding duration, timing of solid food introduction | BMI z-score, overweight | Higher infant BMI and risk of overweight with daily maternal ASB consumption (males only) |
| Gillman et al., 2017 22) | USA, 1999, Project Viva | 1078 pregnant women without gestational diabetes | Prenatal exposure | 6.6–10.9 years | ASB, servings, validated FFQ | Maternal BMI, age, race, education, smoking, parity; household income; child age, sex | Adiposity (BMI z-score, fat mass index, skinfolds), central adiposity (skinfold ratio, WC) | No association of child adiposity with maternal ASB intake |
| Zhu et al., 2017 23) | Denmark, 1996, DNBC | 918 pregnant women with gestational diabetes | Prenatal exposure | 7 years | ASB, servings, validated FFQ | Maternal BMI, energy intake and diet quality, age, employment level, smoking, physical activity; infant sex, breastfeeding duration; child ASB/SSB consumption, physical activity | ||
Footnote: Studies sorted by year of publication. Bold text indicates main direction of association between non-nutritive sweeteners exposure and obesity-related outcome.
Abbreviations: ASB = artificially-sweetened beverage; BMI = body mass index; CHILD = Canadian Healthy Infant Longitudinal Development; DMFT = decayed, missing, and filled teeth; DNBC = Danish National Birth Cohort; FFQ = food frequency questionnaire; GA = gestational age; NNS = non-nutritive sweetener; SES = socioeconomic status; SSB = sugar-sweetened beverage.
[Source 24) ]Is saccharin safe?
Saccharin, an artificial sweetener, has been previously assessed for safety by the Joint Food and Agriculture Organization of the United Nations (FAO)/World Health Organization (WHO) Expert Committee on Food Additives (JECFA) 25). The Scientific Committee on Food (SCF) expressed an opinion on saccharin and its sodium, potassium and calcium salts 26). Both Committees established an acceptable daily intake (ADI) of 5 mg/kg body weight per day for saccharin and its calcium, potassium and sodium salts. The Scientific Panel on Food Additives, Flavoring, Processing Aids and Materials in Contact with Food (AFC) expressed an opinion on the presence of 1,2‐benzisothiazolin‐3‐one as an impurity in saccharin used as a food additive and concluded that it is not of concern at the level detected ranging between 40 and 800 mg/kg 27). In 2012, the European Food Safety Authority Panel on Food Contact Materials, Flavorings, Enzymes and Processing Aids (CEF) evaluated sodium salt (saccharin, sodium salt) for use in food contact materials, as additive in polyesters, and concluded that it is not of safety concern for the consumer 28).
In 1999, the International Agency for Research on Cancer 29) concluded that saccharin and its salts are not classifiable as to their carcinogenicity to humans (Group 3).
The absorption, distribution, metabolism and excretion of saccharin and its salts has been reviewed by the Joint Food and Agriculture Organization of the United Nations (FAO)/World Health Organization (WHO) Expert Committee on Food Additives (JECFA) 30). The summary below is based on this JECFA assessment.
Depending on the pH, saccharin may exist in the non‐ionised form (at acidic pH) or in the ionized form (saccharin anion). The non‐ionized form is readily absorbed in the stomach of species with low pH (e.g. guinea pig, rabbit), whereas the saccharin anion is slowly absorbed in the stomach of species with a higher pH (e.g. rat) or in the intestines. In humans and rat, saccharin is slowly absorbed in the intestines and rapidly excreted in the urine. Urinary excretion is considered a measure of gastrointestinal absorption, whereas fecal excretion is an indicator of unabsorbed saccharin 31).
Following a single oral dose to adult rats, saccharin was found to be distributed to most organs with the highest concentrations in the organs of elimination (kidney and bladder) followed by the plasma. There is no evidence of bioaccumulation of saccharin in any tissue 32). Only when dietary administration to rats exceeded 5% of the diet was there any accumulation of saccharin in plasma and tissues, due to decreased renal clearance.
Based on studies reviewed by Renwick 33) and summarized by JECFA 34), saccharin does not undergo any detectable metabolism in humans, rats, guinea‐pigs, rabbits or monkeys. Studies in humans and rats indicate that the majority of saccharin administered in the diet (80–85%) is slowly absorbed and rapidly excreted unchanged in the urine. When [3‐14C]‐saccharin was administered orally to rats, 56–87% of the labelled dose was excreted in the urine and 10–40% in the faeces during 7 days. More than 99% of the urinary 14C was unchanged saccharin. Comparative metabolic profiles of a dog, rabbit, guinea pig and hamster indicated that there was little difference in the pattern due to animal species or dose level 35).
Considering the similarity of the metabolic profile of dog, rabbit, guinea pig and hamster, it is not expected that sodium saccharin behaves in a different way in pigs and calves.
Toxicological studies
The data available on the toxicity of saccharin have been reviewed by JECFA 36) and the Scientific Committee of Food 37).
Two‐generation study in rat
The Joint Food and Agriculture Organization of the United Nations (FAO)/World Health Organization (WHO) Expert Committee on Food Additives (JECFA) based the assessment on a two‐generation feeding study in rats with sodium saccharin at 1%, 3%, 4%, 5%, 6.25% and 7.5% of the diet 38). Although no adverse effect on survival was observed up to the highest dose (7.5%), at levels of 3% and higher the animals showed a marked disturbance in homeostasis, with a dose‐related decrease in body weight gain despite increased food consumption. This effect was related to inhibitory effects of saccharin on carbohydrate and protein digestion. No relevant toxicological effects were observed at 1%, which was taken as the no observed adverse effect level (NOAEL). On the basis of this NOAEL of 1% (corresponding to 500 mg/kg body weight per day) and the application of an uncertainty factor of 100, JECFA allocated a group acceptable daily intake (ADI) of 5 mg/kg body weight to saccharin and its calcium, potassium and sodium salts 39). Bladder tumors induced by sodium saccharin were observed in male rats only. According to JECFA, ‘it would be inappropriate to consider the bladder tumors induced in male rats by sodium saccharin to be relevant to the assessment of a toxicological hazard in humans’. In addition, epidemiological studies on saccharin did not show any evidence that saccharin ingestion increased the incidence of bladder tumors in human populations.
The same two‐generation, long‐term study in rat was assessed by the Scientific Committee of Food 40). The Scientific Committee of Food considered the bladder tumors induced by saccharin to be specific for the male rat and not equally relevant for female rats and mice, hamsters and monkeys, and not relevant for humans. As the increase in the tumors incidence at 1% supplementation level was not statistically significant and there were no compound‐related effects in either the grade or incidence of any lesions in the 1% group, the Scientific Committee of Food concluded that a dose of 1% sodium saccharin in the diet should be taken as the NOAEL for bladder tumors in the male rat. Based on this NOAEL of 1% in the diet (500 mg/kg body weight per day) and the application of a 100‐fold uncertainty factor, an acceptable daily intake (ADI) of 5 mg/kg body weight was established 41).
Genotoxicity and carcinogenicity
Subsequent to the JECFA and Scientific Committee of Food evaluations, International Agency for Research on cancer (IARC) reviewed human and animal carcinogenicity data together with the available information on mutagenicity and genotoxicity of saccharin and its salts 42).
Based upon this analysis and review of all available studies, International Agency for Research on cancer (IARC) reached the following overall conclusions 43):
- there is inadequate evidence in humans for the carcinogenicity of saccharin salts used as sweeteners;
- there is inadequate evidence in experimental animals for the carcinogenicity of saccharin (acid form) and calcium saccharin;
- there is sufficient evidence in experimental animals for the carcinogenicity of sodium saccharin.
The International Agency for Research on cancer (IARC) concluded that ‘sodium saccharin produces urothelial bladder tumors in rats by a non‐DNA‐reactive mechanism that involves the formation of a urinary calcium phosphate‐containing precipitate, cytotoxicity and enhanced cell proliferation. This mechanism is not relevant to humans because of critical interspecies differences in urine composition’ 44).
Safety for the consumer
A group acceptable daily intake (ADI) of 5 mg saccharin/kg body weight per day was allocated by JECFA 45) and the Scientific Committee of Food 46) for saccharin and its calcium, potassium and sodium salts when used in food. Therefore, it is necessary to consider the potential contribution of residues in tissues from animals administered saccharin in feed to the overall exposure of consumers. Although no studies on residues in food from animal origin were submitted, the metabolic data suggest that there is no evidence of accumulation in any tissue and that tissue accumulation can occur but only at doses far in excess of those proposed for animal feed. The possibility that residues will be present in tissues from animals fed with sodium saccharin cannot be excluded; however, it is considered unlikely that any residues would cause consumer exposure to saccharin to exceed the acceptable daily intake (ADI), even considering that some consumers may be exposed up to 2.5 mg/kg body weight (half of the ADI) using saccharin as a sweetener 47).
Conclusions on safety for the consumer
No concern for the consumer would result from the use of sodium saccharin in feed and water for drinking at the dose considered safe for the target species.
Safety for the environment
An environmental risk assessment of saccharin indicates that the proposed use level of 150 mg sodium saccharin/kg feed for pigs for fattening and veal calves is unlikely to have detrimental effects on the terrestrial and freshwater compartments.
The high mobility and relative persistence of saccharin and the high persistency of its degradation product 4‐hydroxysaccharin indicate that groundwater contamination above 0.1 μg/L is likely to occur.
References [ + ]