Contents
- What is alcohol withdrawal ?
- What causes Alcohol use disorder
- Symptoms of Alcohol Use Disorder
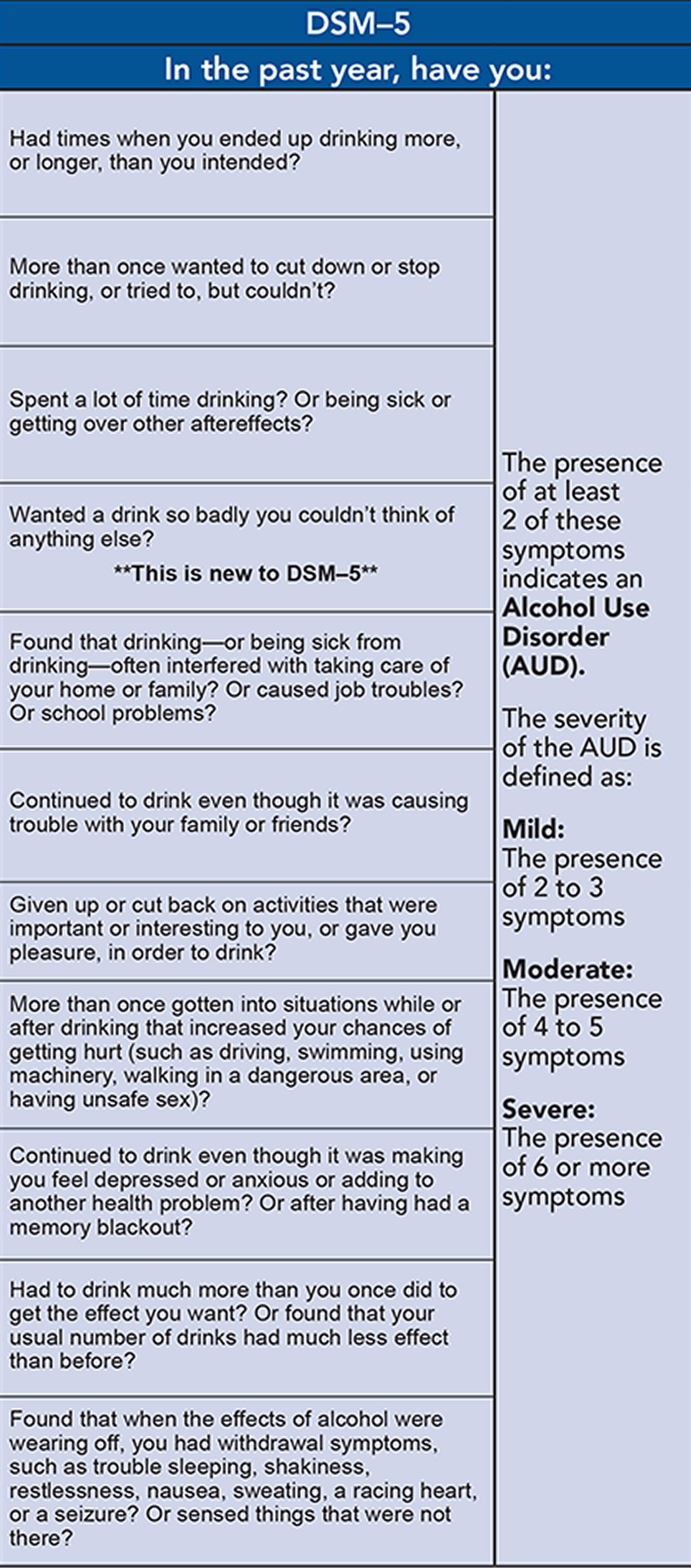
- Figure 1. Alcohol Use Disorder: American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders Definition
- Exams and Tests for Alcohol use disorder
- Treatment of Alcohol use disorder
- Support Groups for Alcohol use disorder
- FDA-Approved Medications to help people stop or reduce their drinking and avoid relapse
- Outlook (Prognosis) for Alcohol use disorder
- Possible Complications for Alcohol use disorder
- Prevention for Alcohol use disorder
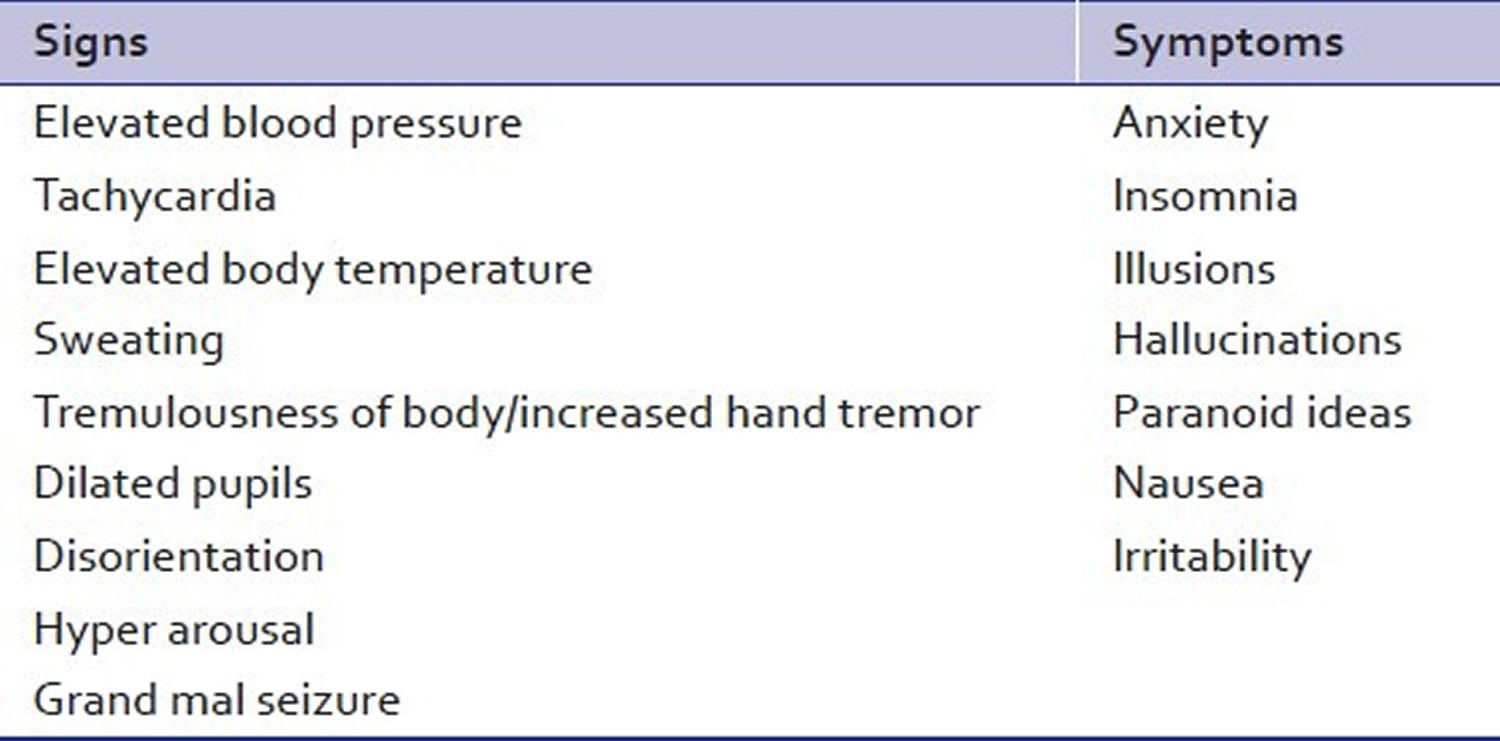
- What are the signs and symptoms of alcohol withdrawal
- How long does alcohol withdrawal last ?
- Table 4. Duration of Alcohol Withdrawal Syndrome
- Figure 2. Graph depicting the time course of alcohol withdrawal symptoms
- Evaluation of the Patient in Alcohol Withdrawal
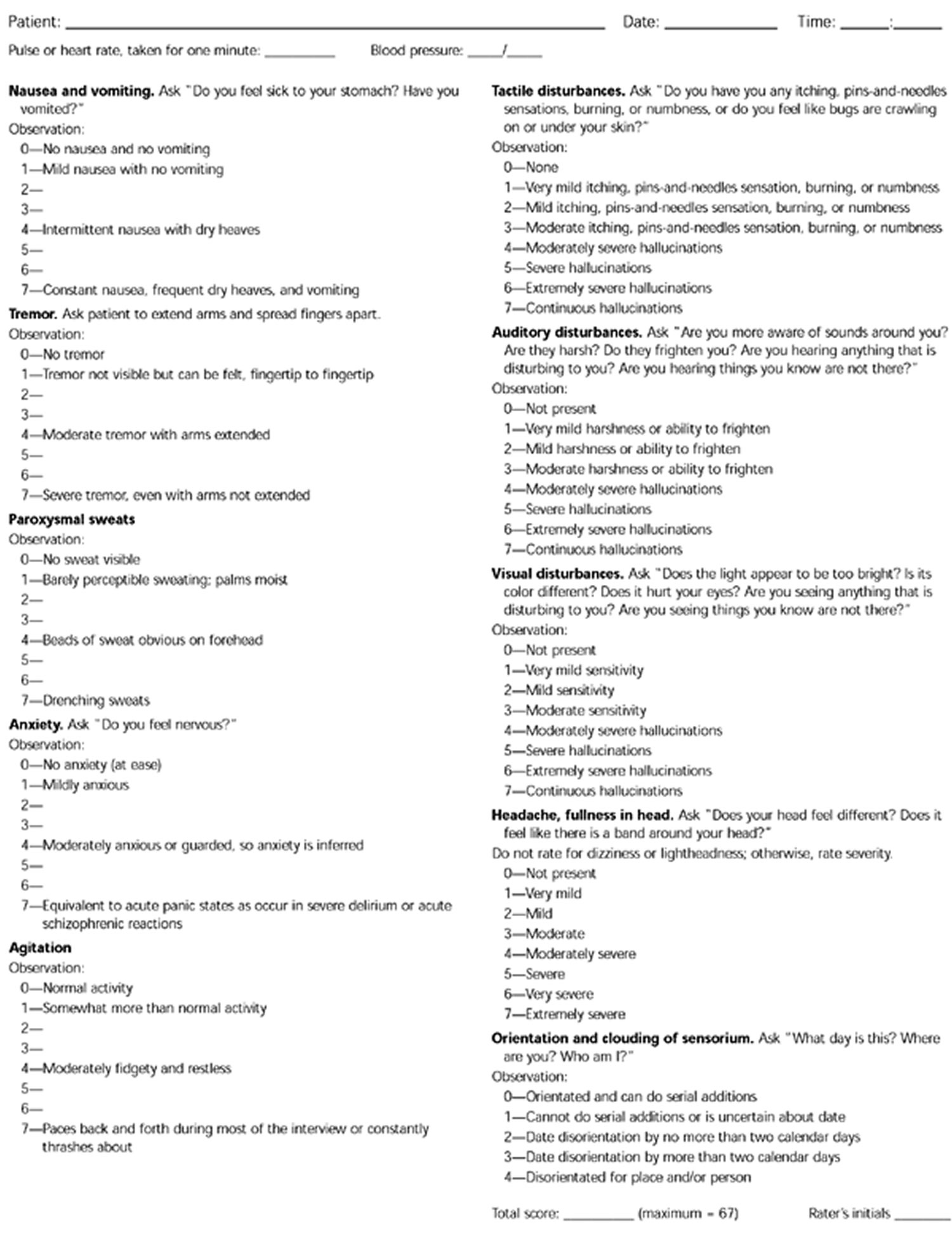
- Figure 3. Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar)
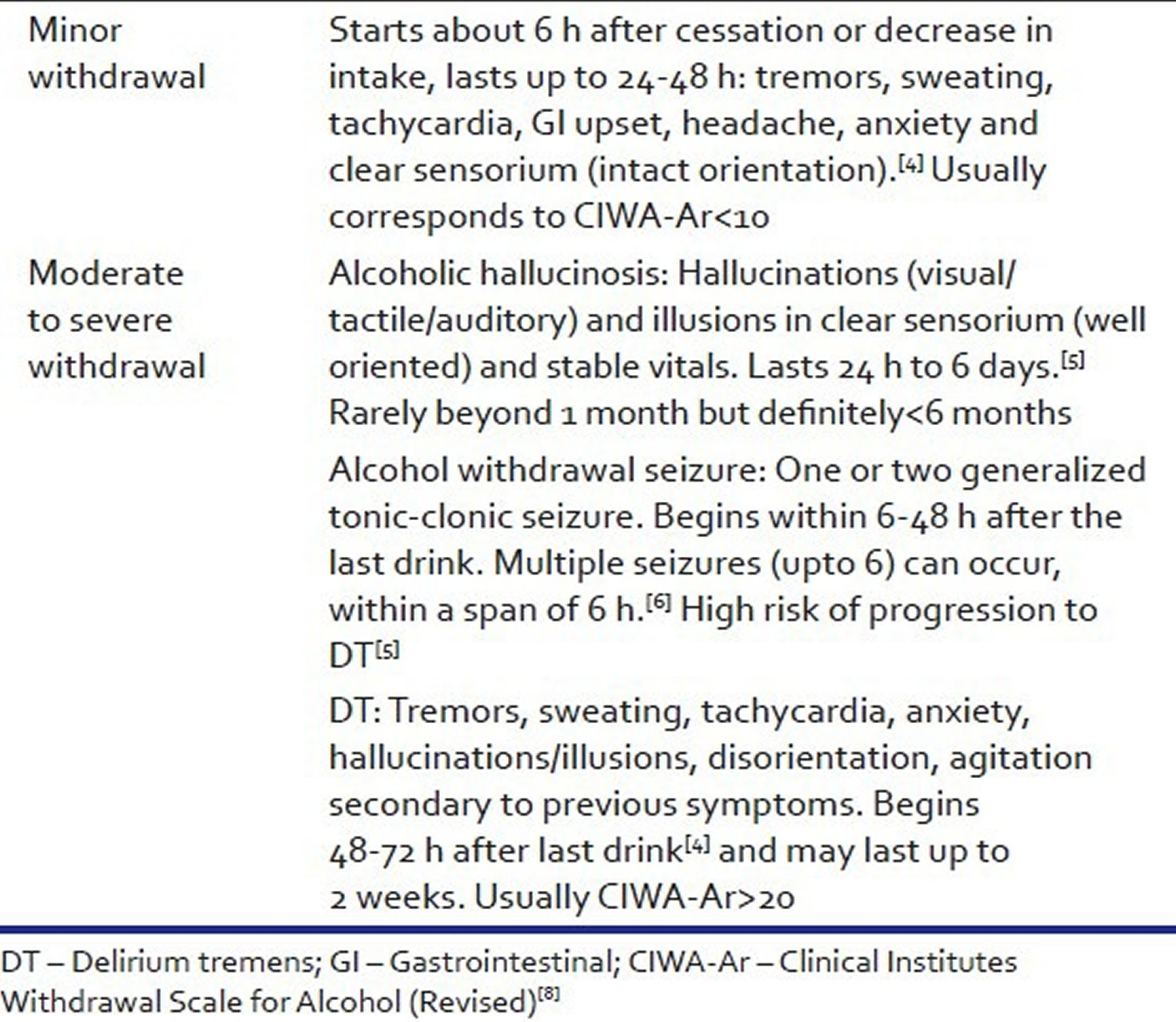
- Figure 4. Clinical descriptions of alcohol withdrawal syndromes by severity
- What is delirium tremens ?
- Alcohol withdrawal treatment
- Alcohol withdrawal medication
- What causes Alcohol use disorder
What is alcohol withdrawal ?
Prolonged alcohol consumption leads to the development of tolerance and physical dependence, which may result from compensatory functional changes in the same ion channels. Abrupt cessation of prolonged alcohol consumption unmasks these changes, leading to the alcohol withdrawal syndrome, which includes blackouts, tremors, muscular rigidity, delirium tremens, and seizures 1. Alcohol withdrawal syndrome is a distressing and life-threatening medical emergency condition associated with high mortality rates that usually affects people who are alcohol dependent when they discontinue or decrease their alcohol consumption 2, 3. The most common effects include shaking, restlessness, difficulty sleeping, nightmares, sweats, high heart rate, fever, feeling sick, vomiting, fits, hallucinations, increased agitation, tremulousness, and delirium. In severe cases, people may lose consciousness, their heart may stop, and they may die 2. It is estimated that 2 million Americans experience the symptoms of alcohol withdrawal each year 4.
The neurobiological mechanisms underlying alcohol withdrawal syndrome are complex. Alcohol is a central nervous system (CNS) depressant, influencing the inhibitory neurotransmitter gamma-aminobutyric acid (GABA). Ordinarily, the excitatory (glutamate) and inhibitory (GABA) neurotransmitters are in a state of homeostasis 5. Alcohol facilitates GABA action, causing decreased CNS excitability. In the long-term, it causes a decrease in the number of GABA receptors (down regulation). This results in the requirement of increasingly larger doses of ethanol to achieve the same euphoric effect, a phenomenon known as tolerance 5. Alcohol acts as an N-methyl-D-aspartate (NMDA) receptor antagonist, thereby reducing the CNS excitatory tone. Chronic use of alcohol leads to an increase in the number of NMDA receptors (up regulation) and production of more glutamate to maintain CNS homeostasis 5. Whether these abnormalities represent a trait- or state-dependent marker of ethanol dependence remains to be resolved 6.
With the sudden cessation of alcohol in the chronic user, the alcohol mediated central nervous system (CNS) inhibition is reduced and the glutamate mediated CNS excitation is left unopposed, resulting in a net CNS excitation. This CNS excitation results in the clinical symptoms of alcohol withdrawal in the form of autonomic over activity such as tachycardia, tremors, sweating and neuropsychiatric complications such as delirium and seizures 7.
Dopamine is another neurotransmitter involved in alcohol withdrawal states. During alcohol use and withdrawal the increase in CNS dopamine levels contribute to the clinical manifestations of autonomic hyper arousal and hallucinations 5.
Repeated episodes of withdrawal and neuroexcitation results in a lowered seizure threshold as a result of kindling predisposing to withdrawal seizures 8.
Currently, benzodiazepines are the drugs of choice for the treatment of alcohol withdrawal syndrome. These compounds potentiate GABA-A receptor signaling and act to counterbalance the hyperexcitation produced by excessive glutamate transmission. However, benzodiazepine treatment of alcohol withdrawal syndrome has substantial drawbacks, including its own host of rebound effects upon cessation of treatment and increased risk of relapse into alcohol dependence following its withdrawal. Other non-benzodiazepine compounds such as carbamazepine, gabapentin, valproic acid, topiramate, gamma-hydroxybutyric acid, baclofen, and flumazenil have been studied, but have been associated with limited clinical efficacy.
Alcohol abuse and dependence can cause serious health problems as well as interpersonal, social, interpersonal and legal consequences. Dependence on alcohol is evident by reduced control over drinking, tolerance to alcohol and withdrawal symptoms. Excessive drinking, binge drinking, and alcohol dependence were most common among men and those aged 18 to 24. Binge drinking was most common among those with annual family incomes of $75,000 or more, whereas alcohol dependence was most common among those with annual family incomes of less than $25,000 9. The prevalence of alcohol dependence was 10.2% among excessive drinkers, 10.5% among binge drinkers, and 1.3% among non-binge drinkers. A positive relationship was found between alcohol dependence and binge drinking frequency.
Excessive alcohol consumption is responsible for 88,000 deaths annually and cost the United States $223.5 billion in 2006 9. Half of these deaths and three-quarters of the economic costs are due to binge drinking (ie, ≥4 drinks for women and ≥5 drinks for men in a single occasion) 10. Binge drinking is also associated with a myriad of health and social problems (eg, violence, new HIV infections, unintended pregnancies, and alcohol dependence) 11, 12.
It is often assumed that most excessive drinkers are alcohol dependent. Because binge drinkers are at higher risk than non-binge drinkers for alcohol dependence 13 and about 18 million adult Americans have an alcohol use disorder 14. Alcohol use disorder is when your drinking causes serious problems in your life, yet you keep drinking. You may also need more and more alcohol to feel drunk. Stopping suddenly may cause withdrawal symptoms. This means that your drinking causes distress and harm. It includes alcoholism and alcohol abuse.
The clinical diagnosis of alcohol dependence is based on criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM), Fifth Edition, and involves the assessment of warning signs such as tolerance, withdrawal, impaired control, and unsuccessful attempts to cut down 15.
- Heavy drinking was defined as 8 or more drinks per week during the past 30 days for women or 15 or more drinks per week for men 9.
- Alcohol dependence or alcoholism, is a disease that causes: 1) Craving – a strong need to drink; 2) Loss of control – not being able to stop drinking once you’ve started; 3) Physical dependence – withdrawal symptoms; 4) Tolerance – the need to drink more alcohol to feel the same effect 14.
This study 16 found that about 9 of 10 adult excessive drinkers did not meet the diagnostic criteria for alcohol dependence. About 90% of the adults who drank excessively reported binge drinking, and the prevalence of alcohol dependence was similar among excessive drinkers and binge drinkers across most sociodemographic groups 16. The prevalence of alcohol dependence also increased with the frequency of binge drinking. However, even among those who reported binge drinking 10 or more times in the past month, more than two-thirds did not meet diagnostic criteria for alcohol dependence according to their responses to the survey 16.
Too much alcohol is dangerous. Heavy drinking can increase the risk of certain cancers. It can cause damage to the liver, brain, and other organs. Drinking during pregnancy can harm your baby. Alcohol also increases the risk of death from car crashes, injuries, homicide, and suicide.
If you want to stop drinking, there is help. Start by talking to your health care provider. Treatment may include medicines, counseling, and support groups.
If you cannot stop drinking, GET HELP. There are programs that can help you stop drinking. They are called alcohol treatment programs. Your doctor or nurse can find a program to help you. Even if you have been through a treatment program before, try it again. There are also programs just for women.
Consider joining Alcoholics Anonymous or another mutual support group (see links below). Recovering people who attend groups regularly do better than those who do not. Groups can vary widely, so shop around for one that’s comfortable. You’ll get more out of it if you become actively involved by having a sponsor and reaching out to other members for assistance.
- Alcoholics Anonymous 17
- Moderation Management 18
- Secular Organizations for Sobriety 19
- SMART Recovery 20
- Women for Sobriety 21
- Al-Anon Family Groups 22
- Adult Children of Alcoholics 23
- National Council on Alcoholism and Drug Dependence 24
- National Institute on Alcohol Abuse and Alcoholism 25
- National Organization on Fetal Alcohol Syndrome 26
- Substance Abuse and Mental Health Services Administration 27
What causes Alcohol use disorder
No one knows what causes problems with alcohol. Health experts think that it may be a combination of a person’s:
- Genes
- Environment
- Psychology, such as being impulsive or having low self-esteem
Depression and anxiety often go hand in hand with heavy drinking. Studies show that people who are alcohol dependent are two to three times as likely to suffer from major depression or anxiety over their lifetime. When addressing drinking problems, it’s important to also seek treatment for any accompanying medical and mental health issues.
Drinking an excessive amount of alcohol can put you at risk for alcohol-related problems if:
- You are a man who has 15 or more drinks a week, or often have 5 or more drinks at a time
- You are a woman who has 8 or more drinks a week, or often have 4 or more drinks at a time.
One drink is defined as 12 ounces or 360 milliliters (mL) of beer (5% alcohol content), 5 ounces or 150 mL of wine (12% alcohol content), or a 1.5-ounce or 45-mL shot of liquor (80-proof, or 40% alcohol content).
If you have a parent with alcohol use disorder, you are more at risk for alcohol problems.
You also may be more likely to have problems with alcohol if you:
- Are a young adult under peer pressure
- Have depression, bipolar disorder, anxiety disorders, or schizophrenia
- Can easily obtain alcohol
- Have low self-esteem
- Have problems with relationships
- Live a stressful lifestyle
If you are concerned about your drinking, it may help to take a careful look at your alcohol use.
Symptoms of Alcohol Use Disorder
Doctors have developed a list of symptoms that a person has to have in the past year to be diagnosed with alcohol use disorder.
To assess whether you or loved one may have Alcohol Use Disorder, here are some questions to ask. In the past year, have you:
- Had times when you ended up drinking more, or longer than you intended?
- More than once wanted to cut down or stop drinking, or tried to, but couldn’t?
- Spent a lot of time drinking? Or being sick or getting over the aftereffects?
- Experienced craving — a strong need, or urge, to drink?
- Found that drinking — or being sick from drinking — often interfered with taking care of your home or family? Or caused job troubles? Or school problems?
- Continued to drink even though it was causing trouble with your family or friends?
- Given up or cut back on activities that were important or interesting to you, or gave you pleasure, in order to drink?
- More than once gotten into situations while or after drinking that increased your chances of getting hurt (such as driving, swimming, using machinery, walking in a dangerous area, or having unsafe sex)?
- Continued to drink even though it was making you feel depressed or anxious or adding to another health problem? Or after having had a memory blackout?
- Had to drink much more than you once did to get the effect you want? Or found that your usual number of drinks had much less effect than before?
- Found that when the effects of alcohol were wearing off, you had withdrawal symptoms, such as trouble sleeping, shakiness, irritability, anxiety, depression, restlessness, nausea, or sweating? Or sensed things that were not there?
If you have any of these symptoms, your drinking may already be a cause for concern. The more symptoms you have, the more urgent the need for change. A health professional can conduct a formal assessment of your symptoms to see if alcohol use disorder is present.
However severe the problem may seem, most people with alcohol use disorder can benefit from treatment. Unfortunately, less than 10 percent of them receive any treatment.
Ultimately, receiving treatment can improve an individual’s chances of success in overcoming alcohol use disorder.
Talk with your doctor to determine the best course of action for you.
Figure 1. Alcohol Use Disorder: American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders Definition
[Source 28]Exams and Tests for Alcohol use disorder
Your health care provider will:
- Examine you
- Ask about your medical and family history
- Ask about your alcohol use, and if you have any of the symptoms listed above
Your healthcare provider may order tests to check for health problems that are common in people who use alcohol. These tests may include:
- Blood alcohol level (this shows if you have recently been drinking alcohol. It does not diagnose alcohol use disorder.)
- Complete blood count
- Liver function tests
- Magnesium blood test
- Thiamin blood level
Treatment of Alcohol use disorder
Many people with an alcohol problem need to completely stop using alcohol. This is called abstinence. Having strong social and family support can help make it easier to quit drinking.
Some people are able to just cut back on their drinking. So even if you do not give up alcohol altogether, you may be able to drink less. This can improve your health and relationships with others. It can also help you perform better at work or school.
However, many people who drink too much find they can’t just cut back. Abstinence may be the only way to manage a drinking problem.
The good news is that no matter how severe the problem may seem, most people with an alcohol use disorder can benefit from some form of treatment.
Research shows that about one-third of people who are treated for alcohol problems have no further symptoms 1 year later. Many others substantially reduce their drinking and report fewer alcohol-related problems.
Ultimately, there is no one-size-fits-all solution, and what may work for one person may not be a good fit for someone else. Simply understanding the different options can be an important first step.
- Behavioral treatments. Often known as alcohol counseling or “talk therapy,” behavioral treatments also work well. Several counseling approaches are about equally effective—cognitive-behavioral, motivational enhancement, marital and family counseling, or a combination.
- Specialized, intensive treatment programs.Some people will need more intensive programs.
DECIDING TO QUIT
Like many people with an alcohol problem, you may not recognize that your drinking has gotten out of hand. An important first step is to be aware of how much you drink. It also helps to understand the health risks of alcohol.
If you decide to quit drinking, talk with your provider. Treatment involves helping you realize how much your alcohol use is harming your life and the lives those around you.
Depending on how much and how long you have been drinking, you may be at risk for alcohol withdrawal. Withdrawal can be very uncomfortable and even life threatening. If you have been drinking a lot, you should cut back or stop drinking only under the care of a doctor. Talk with your provider about how to stop using alcohol.
LONG-TERM SUPPORT
Alcohol recovery or support programs can help you stop drinking completely. These programs usually offer:
- Education about alcohol use and its effects
- Counseling and therapy to discuss how to control your thoughts and behaviors
- Physical health care
For the best chance of success, you should live with people who support your efforts to avoid alcohol. Some programs offer housing options for people with alcohol problems. Depending on your needs and the programs that are available:
- You may be treated in a special recovery center (inpatient)
- You may attend a program while you live at home (outpatient)
You may be prescribed medicines to help you quit. They are often used with long-term counseling or support groups. These medicines make it less likely that you will drink again or help limit the amount you drink.
Drinking may mask depression or other mood or anxiety disorders. If you have a mood disorder, it may become more noticeable when you stop drinking. Your provider will treat any mental disorders in addition to your alcohol treatment.
Support Groups for Alcohol use disorder
Because an alcohol use disorder can be a chronic relapsing disease, persistence is key. It is rare that someone would go to treatment once and then never drink again. More often, people must repeatedly try to quit or cut back, experience recurrences, learn from them, and then keep trying. For many, continued followup with a treatment provider is critical to overcoming problem drinking. Support groups help many people who are dealing with alcohol use and relapses.
Relapse is common among people who overcome alcohol problems. People with drinking problems are most likely to relapse during periods of stress or when exposed to people or places associated with past drinking.
Just as some people with diabetes or asthma may have flare-ups of their disease, a relapse to drinking can be seen as a temporary set-back to full recovery and not a complete failure. Seeking professional help can prevent relapse — behavioral therapies can help people develop skills to avoid and overcome triggers, such as stress, that might lead to drinking. Most people benefit from regular checkups with a treatment provider. Medications also can deter drinking during times when individuals may be at greater risk of relapse (e.g., divorce, death of a family member).
If you cannot stop drinking, GET HELP. You may have a disease called alcoholism. There are programs that can help you stop drinking. They are called alcohol treatment programs. Your doctor or nurse can find a program to help you. Even if you have been through a treatment program before, try it again. There are also programs just for women.
Consider joining Alcoholics Anonymous or another mutual support group (see links below). Recovering people who attend groups regularly do better than those who do not. Groups can vary widely, so shop around for one that’s comfortable. You’ll get more out of it if you become actively involved by having a sponsor and reaching out to other members for assistance.
- Alcoholics Anonymous 17
- Moderation Management 18
- Secular Organizations for Sobriety 19
- SMART Recovery 20
- Women for Sobriety 21
- Al-Anon Family Groups 22
- Adult Children of Alcoholics 23
- National Council on Alcoholism and Drug Dependence 24
- National Institute on Alcohol Abuse and Alcoholism 25
- National Organization on Fetal Alcohol Syndrome 26
- Substance Abuse and Mental Health Services Administration 27
FDA-Approved Medications to help people stop or reduce their drinking and avoid relapse
The U.S. Food and Drug Administration (FDA) has approved three medications for treating alcohol dependence, and others are being tested to determine if they are effective 29.
- Naltrexone can help people reduce heavy drinking.
- Acamprosate makes it easier to maintain abstinence.
- Disulfiram blocks the breakdown (metabolism) of alcohol by the body, causing unpleasant symptoms such as nausea and flushing of the skin. Those unpleasant effects can help some people avoid drinking while taking disulfiram.
It is important to remember that not all people will respond to medications, but for a subset of individuals, they can be an important tool in overcoming alcohol dependence.
Of the FDA approved medications, the two newer ones (naltrexone and acamprosate) can make it easier to quit drinking by offsetting changes in the brain caused by alcoholism. They don’t make you sick if you do drink, unlike the older approved medication (disulfiram) 30.
- None of these medications is addictive. They can be combined with mutual-support groups or behavioral treatments.
Naltrexone
Naltrexone blocks opioid receptors that are involved in the rewarding effects of drinking and the craving for alcohol 31. It has been shown to reduce relapse to problem drinking in some patients. An extended release version, Vivitrol—administered once a month by injection—is also FDA-approved for treating alcoholism, and may offer benefits regarding compliance.
Acamprosate
Acamprosate (Campral®) acts on the gamma-aminobutyric acid (GABA) and glutamate neurotransmitter systems and is thought to reduce symptoms of protracted withdrawal, such as insomnia, anxiety, restlessness, and dysphoria 31. Acamprosate has been shown to help dependent drinkers maintain abstinence for several weeks to months, and it may be more effective in patients with severe dependence.
Disulfiram
Disulfiram (Antabuse®) interferes with degradation of alcohol, resulting in the accumulation of acetaldehyde, which, in turn, produces a very unpleasant reaction that includes flushing, nausea, and plapitations if a person drinks alcohol 31. The utility and effectiveness of disulfiram are considered limited because compliance is generally poor. However, among patients who are highly motivated, disulfiram can be effective, and some patients use it episodically for high-risk situations, such as social occasions where alcohol is present. It can also be administered in a monitored fashion, such as in a clinic or by a spouse, improving its efficacy.
Scientists are working to develop a larger menu of pharmaceutical treatments that could be tailored to individual needs. As more medications become available, people may be able to try multiple medications to find which they respond to best.
Certain medications already approved for other uses have shown promise for treating alcohol dependence and problem drinking:
- The anti-smoking drug varenicline (marketed under the name Chantix) significantly reduced alcohol consumption and craving among people with alcoholism.
- Gabapentin, a medication used to treat pain conditions and epilepsy, was shown to increase abstinence and reduce heavy drinking. Those taking the medication also reported fewer alcohol cravings and improved mood and sleep.
- The anti-epileptic medication topiramate was shown to help people curb problem drinking, particularly among those with a certain genetic makeup that appears to be linked to the treatment’s effectiveness.
Topiramate
Topiramate is thought to work by increasing inhibitory (GABA) neurotransmission and reducing stimulatory (glutamate) neurotransmission, although its precise mechanism of action is not known 31. Although topiramate has not yet received FDA approval for treating alcohol addiction, it is sometimes used off-label for this purpose. Topiramate has been shown in studies to significantly improve multiple drinking outcomes, compared with a placebo.
“Isn’t taking medications just trading one addiction for another?”
This is not an uncommon concern, but the short answer is “no.” All medications approved for treating alcohol dependence are non-addictive 29. These medicines are designed to help manage a chronic disease, just as someone might take drugs to keep their cholesterol or diabetes in check.
Outlook (Prognosis) for Alcohol use disorder
How well a person does depends on whether they can successfully cut back or stop drinking.
It may take several tries to stop drinking for good. If you are struggling to quit, do not give up hope. Getting treatment, if needed, along with support and encouragement from support groups and those around you can help you remain sober.
Possible Complications for Alcohol use disorder
Alcohol use disorder can increase your risk of many health problems, including:
- Bleeding in the digestive tract
- Brain cell damage
- A brain disorder called Wernicke-Korsakoff syndrome
- Cancer of the esophagus, liver, colon, breast and other areas
- Changes in the menstrual cycle
- Delirium tremens (DTs)
- Dementia and memory loss
- Depression and suicide
- Erectile dysfunction
- Heart damage
- High blood pressure
- Inflammation of the pancreas (pancreatitis)
- Liver disease, including cirrhosis
- Nerve damage
- Poor nutrition
- Sleeping problems (insomnia)
- Sexually transmitted infections (STIs)
Alcohol use also increases your risk for violence.
Drinking alcohol while you are pregnant can lead to severe birth defects in the baby. This is called fetal alcohol syndrome.
Prevention for Alcohol use disorder
The National Institute on Alcohol Abuse and Alcoholism recommends:
- Women should not drink more than 1 drink per day
- Men should not drink more than 2 drinks per day
What are the signs and symptoms of alcohol withdrawal
The spectrum of alcohol withdrawal symptoms ranges from such minor symptoms as insomnia and tremulousness to severe complications such as withdrawal seizures and delirium tremens.
Generally, the symptoms of alcohol withdrawal relate proportionately to the amount of alcoholic intake and the duration of a patient’s recent drinking habit. Most patients have a similar spectrum of symptoms with each episode of alcohol withdrawal 32.
Minor withdrawal symptoms can occur while the patient still has a measurable blood alcohol level. These symptoms may include insomnia, mild anxiety, and tremulousness. Patients with alcoholic hallucinosis experience visual, auditory, or tactile hallucinations but otherwise have a clear sensorium 32.
Withdrawal seizures are more common in patients who have a history of multiple episodes of detoxification 32. Causes other than alcohol withdrawal should be considered if seizures are focal, if there is no definite history of recent abstinence from drinking, if seizures occur more than 48 hours after the patient’s last drink, or if the patient has a history of fever or trauma.
Table 1. Common signs and symptoms of alcohol withdrawal syndrome
Table 2. Diagnostic Criteria for Alcohol Withdrawal Symptoms
A. Cessation of (or reduction in) alcohol use that has been heavy and prolonged. | |
B. Two (or more) of the following, developing within several hours to a few days after criterion A: | |
1. Autonomic hyperactivity (e.g., sweating or pulse rate greater than 100 beats per minute) | |
2. Increased hand tremor | |
3. Insomnia | |
4. Nausea or vomiting | |
5. Transient visual, tactile, or auditory hallucination s or illusions | |
6. Psychomotor agitation | |
7. Anxiety | |
8. Grand mal seizures | |
C. The symptoms in criterion B cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. | |
D. The symptoms are not due to a general medical condition and are not better accounted for by another mental disorder. | |
Alcohol withdrawal delirium, or delirium tremens, is characterized by clouding of consciousness and delirium. Episodes of delirium tremens have a mortality rate of 1 to 5 percent 34. Risk factors for developing alcohol withdrawal delirium include concurrent acute medical illness, daily heavy alcohol use, history of delirium tremens or withdrawal seizures, older age, abnormal liver function, and more severe withdrawal symptoms on presentation.
Table 3. Timing of Alcohol Withdrawal Symptoms Appearance
| Symptoms | Time of appearance after cessation of alcohol use |
|---|---|
Minor withdrawal symptoms: insomnia, tremulousness, mildanxiety, gastrointestinal upset, headache, diaphoresis, palpitations, anorexia | 6 to 12 hours |
Alcoholic hallucinosis: visual, auditory, or tactile hallucinations | 12 to 24 hours* |
Withdrawal seizures: generalized tonic-clonic seizures | 24 to 48 hours† |
Alcohol withdrawal delirium (delirium tremens): hallucinations (predominately visual), disorientation, tachycardia, hypertension, low-grade fever, agitation, diaphoresis | 48 to 72 hours‡ |
*— Symptoms generally resolve within 48 hours.
†— Symptoms reported as early as two hours after cessation.
‡— Symptoms peak at five days.
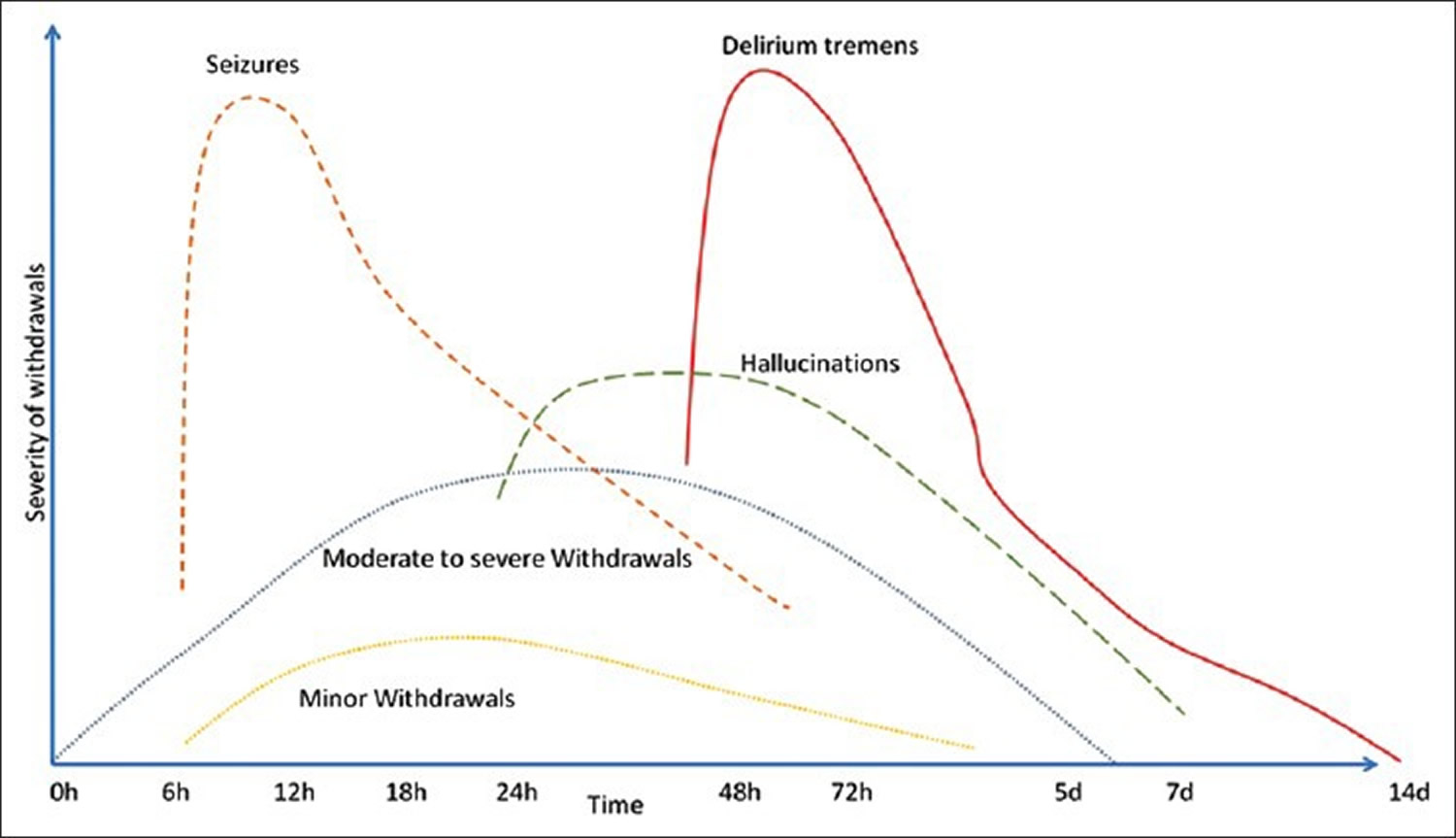
How long does alcohol withdrawal last ?
Alcohol withdrawal seizures typically occur 6 to 48 hours after discontinuation of alcohol consumption and are usually generalized tonic–clonic seizures, although partial seizures also occur 35.
Up to one third of patients with significant alcohol withdrawal may experience alcohol withdrawal seizures. Although seizures in this setting are usually self-limited, they can be associated with status epilepticus and, therefore, are potentially serious 36. In the United States, benzodiazepines are considered the drugs of choice to treat alcohol withdrawal and to prevent the occurrence of seizures 37, 38. In Europe, carbamazepine, chlormethiazole, and valproate are often used 39, 40.
Table 4. Duration of Alcohol Withdrawal Syndrome
| Drug | Peak period | Duration | Signs | Symptoms |
|---|---|---|---|---|
Alcohol | 1 to 3 days | 5 to 7 days | Elevated blood pressure, pulse and temperature, hyperarousal, agitation, restlessness, cutaneous flushing, tremors, diaphoresis, dilated pupils, ataxia, clouding of consciousness, disorientation | Anxiety, panic, paranoid delusions, illusions, visual and auditory hallucinations (often derogatory and intimidating) |
Benzodiazepines and other sedative/hypnotics | Short-acting: 2 to 4 days Long-acting: 4 to 7 days | Short-acting: 4 to 7 days Long-acting: 7 to 14 days | Increased psychomotor activity, agitation, muscular weakness, tremulousness, hyperpyrexia, diaphoresis, delirium, convulsions, elevated blood pressure, pulse and temperature, tremor of eyelids, tongue and hands | Anxiety, depression, euphoria, incoherent thoughts, hostility, grandiosity, disorientation, tactile, auditory and visual hallucinations, suicidal thoughts |
Stimulants (cocaine, amphetamines and derivatives) | 1 to 3 days | 5 to 7 days | Social withdrawal, psychomotor retardation, hypersomnia, hyperphagia | Depression, anhedonia, suicidal thoughts and behavior, paranoid delusions |
Opiates (heroin) | 1 to 3 days | 5 to 7 days | Drug seeking, mydriasis, piloerection, diaphoresis, rhinorrhea, lacrimation, diarrhea, insomnia, elevated blood pressure and pulse (mild) | Intense desire for drugs, muscle cramps, arthralgia, anxiety, nausea, vomiting, malaise |
PCP/psychedelics | Days to weeks | Days to weeks | Hyperactivity, increased pain threshold, nystagmus, hyperreflexia, hypertension and tachycardia, eyelid retraction (stare), agitation and hyperarousal, dry and erythematous skin, violent and self-destructive behaviors | Anxiety, depression, delusions, auditory and visual hallucinations, memory loss, irritable and angry mood and affect, suicidal thoughts |
PCP = phencyclidine.
Figure 2. Graph depicting the time course of alcohol withdrawal symptoms
[Source 42]Evaluation of the Patient in Alcohol Withdrawal
The history and physical examination establish the diagnosis and severity of alcohol withdrawal. Important historical data include quantity of alcoholic intake, duration of alcohol use, time since last drink, previous alcohol withdrawals, presence of concurrent medical or psychiatric conditions, and abuse of other agents. In addition to identifying withdrawal symptoms, the physical examination should assess possible complicating medical conditions, including arrhythmias, congestive heart failure, coronary artery disease, gastrointestinal bleeding, infections, liver disease, nervous system impairment, and pancreatitis. Basic laboratory investigations include a complete blood count, liver function tests, a urine drug screen, and determination of blood alcohol and electrolyte levels.
The revised Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar) scale is a validated 10-item assessment tool that can be used to quantify the severity of alcohol withdrawal syndrome, and to monitor and medicate patients going through withdrawal (Figure 2) 43, 44. Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar) scores of 8 points or fewer correspond to mild withdrawal, scores of 9 to 15 points correspond to moderate withdrawal, and scores of greater than 15 points correspond to severe withdrawal symptoms and an increased risk of delirium tremens and seizures 43.
In using the Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar), the clinical picture should be considered because medical and psychiatric conditions may mimic alcohol withdrawal symptoms. In addition, certain medications (e.g., beta blockers) may blunt the manifestation of these symptoms.
Figure 3. Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar)
Note: Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar) scores of 8 points or fewer correspond to mild withdrawal, scores of 9 to 15 points correspond to moderate withdrawal, and scores of greater than 15 points correspond to severe withdrawal symptoms and an increased risk of delirium tremens and seizures.
Figure 4. Clinical descriptions of alcohol withdrawal syndromes by severity
[Source 41]What is delirium tremens ?
Delirium tremens is a severe form of alcohol withdrawal. It involves sudden and severe mental or nervous system changes 46.
Causes of delirium tremens
Delirium tremens can occur when you stop drinking alcohol after a period of heavy drinking, especially if you do not eat enough food.
Delirium tremens may also be caused by head injury, infection, or illness in people with a history of heavy alcohol use.
It occurs most often in people who have a history of alcohol withdrawal. It is especially common in those who drink 4 to 5 pints (1.8 to 2.4 liters) of wine, 7 to 8 pints (3.3 to 3.8 liters) of beer, or 1 pint (1/2 liter) of “hard” alcohol every day for several months. Delirium tremens also commonly affects people who have used alcohol for more than 10 years.
Symptoms of delirium tremens
Symptoms most often occur within 48 to 96 hours after the last drink. But, they can occur 7 to 10 days after the last drink.
Symptoms may get worse quickly, and can include:
- Delirium, which is sudden severe confusion
- Body tremors
- Changes in mental function
- Agitation, irritability
- Deep sleep that lasts for a day or longer
- Excitement or fear
- Hallucinations (seeing or feeling things that are not really there)
- Bursts of energy
- Quick mood changes
- Restlessness, excitement
- Sensitivity to light, sound, touch
- Stupor, sleepiness, fatigue
Seizures (may occur without other symptoms of delirium tremens):
- Most common in the first 12 to 48 hours after the last drink
- Most common in people with past complications from alcohol withdrawal
- Usually generalized tonic-clonic seizures
Symptoms of alcohol withdrawal, including:
- Anxiety, depression
- Fatigue
- Headache
- Insomnia (difficulty falling and staying asleep)
- Irritability or excitability
- Loss of appetite
- Nausea, vomiting
- Nervousness, jumpiness, shakiness, palpitations (sensation of feeling the heart beat)
- Pale skin
- Rapid emotional changes
- Sweating, especially on the palms of the hands or the face
Other symptoms that may occur:
- Chest pain
- Fever
- Stomach pain
Treatment of Delirium Tremens
The goals of treatment are to:
- Save the person’s life
- Relieve symptoms
- Prevent complications
A hospital stay is needed. The health care team will regularly check:
- Blood chemistry results, such as electrolyte levels
- Body fluid levels
- Vital signs (temperature, pulse, breathing rate, blood pressure)
While in the hospital, the person will receive medicines to:
- Stay calm and relaxed (sedated) until the delirium tremens are finished
- Treat seizures, anxiety, or tremors
- Treat mental disorders, if any
Long-term preventive treatment should begin after the person recovers from delirium tremens symptoms. This may involve:
- A “drying out” period, in which no alcohol is allowed
- Total and lifelong avoidance of alcohol (abstinence)
- Counseling
- Going to support groups (such as Alcoholics Anonymous)
Treatment may be needed for other medical problems that can occur with alcohol use, including:
- Alcoholic cardiomyopathy
- Alcoholic liver disease
- Alcoholic neuropathy
- Wernicke-Korsakoff syndrome.
Outlook (Prognosis) for Delirium tremens
Delirium tremens is serious and may be life threatening. Some symptoms related to alcohol withdrawal may last for a year or more, including:
- Emotional mood swings
- Feeling tired
- Sleeplessness
Possible Complications of Delirium tremens
Complications can include:
- Injury from falls during seizures
- Injury to self or others caused by mental state (confusion/delirium)
- Irregular heartbeat, may be life threatening
- Seizures
Alcohol withdrawal treatment
Regimens used to treat alcohol withdrawal syndrome have evolved over time, taking advantage of advances in the understanding of addiction neurophysiology. There is no specific ethanol receptor 47. Much of alcohol’s acute effects on the central nervous system are mediated by its stimulation of the gamma‐aminobutyric acid (GABA) system, which is neuroinhibitory 48. Chronic alcohol use leads to habituation partly by inducing configuration changes of GABA‐A receptor subunits. This renders the GABA‐A receptor less sensitive to alcohol, barbiturates, and benzodiazepines 49. Although both GABA‐A and GABA‐B receptor activation cause increased GABA neuronal output, the GABA‐A receptor is rendered relatively less sensitive by chronic exposure to alcohol.
Currently, alcohol withdrawal syndrome is usually managed with benzodiazepines, using variable dosing depending on the severity of withdrawal symptoms. Such symptom‐triggered treatment is generally preferred over fixed‐dose regimens 50, in part because when using this method, many cases of alcohol withdrawal syndrome can be managed with less medication. Benzodiazepine regimens using high doses have been found to be associated with substantial morbidity and prolonged hospitalizations 51, 52.
Benzodiazepines are the drugs of choice for the treatment of alcohol withdrawal syndrome 53 because these compounds potentiate GABA-A receptor signaling and act to counterbalance the hyperexcitation produced by excessive glutamate transmission. Benzodiazepines showed a protective benefit against seizures, when compared to placebo and a potentially protective benefit for many outcomes when compared with antipsychotics 53. Although benzodiazepines are protective in some animal models of alcohol withdrawal seizures 54, they do not exhibit high potency. Moreover, benzodiazepine treatment of alcohol withdrawal syndrome has substantial drawbacks, including its own host of rebound effects upon cessation of treatment and increased risk of relapse into alcohol dependence following its withdrawal 55.
Nevertheless, clinical experience demonstrates that benzodiazepines do reduce the risk of recurrent seizures in patients with an alcohol withdrawal seizure 38, so that in practice, no complete benzodiazepine resistance occurs. However, GABAA-receptor modulators, other than benzodiazepines, might be superior therapeutic agents. Chlormethiazole is a positive modulator of GABAA receptors, which has high efficacy in enhancing GABAA receptors containing α4 subunits 56 and has been shown to protect transiently against alcohol withdrawal seizures in mice withdrawn from exposure to inhaled ethanol 57. Although chlormethiazole may be a preferred agent from a theoretical point of view, it is not currently registered for sale in the United States. Other non-benzodiazepine compounds such as carbamazepine, gabapentin, valproic acid, topiramate, gamma-hydroxybutyric acid, baclofen, and flumazenil have been studied, but have been associated with limited clinical efficacy 58.
Goals of Treatment
The American Society of Addiction Medicine 34 lists three immediate goals for detoxification of alcohol and other substances:
- To provide a safe withdrawal from the drug(s) of dependence and enable the patient to become drug-free;
- To provide a withdrawal that is humane and thus protects the patient’s dignity; and
- To prepare the patient for ongoing treatment of his or her dependence on alcohol or other drugs.
General Care
Abnormalities in fluid levels, electrolyte levels, or nutrition should be corrected. Intravenous fluids may be necessary in patients with severe withdrawal because of excessive fluid loss through hyperthermia, sweating, and vomiting. Intravenous fluids should not be administered routinely in patients with less severe withdrawal, because these patients may become overhydrated.
Routine administration of magnesium sulfate has not been shown to improve withdrawal symptoms 59, but supplementation is appropriate if a patient is hypomagnesemic.
Wernicke’s Encephalopathy results from cell damage due to chronic thiamine deficiency. Wernicke’s Encephalopathy has an associated mortality of 20%, with 75% developing a permanent severe amnestic syndrome (Korsokoff’s encephalopathy) 60. This can be prevented by administering parenteral (intravenous) thiamine which achieves adequate blood thiamine level much earlier than the oral route. Allergic reactions are rare. All patients in alcohol withdrawal should receive at least 250 mg thiamine by the parenteral route once a day for the first 3-5 days 61, whereas for those with suspected Wernicke’s Encephalopathy, thiamine 500 mg/day for 3-5 days is advised. If there is clinical improvement the supplementation is continued for total of 2 weeks.[39] Concurrent administration of parenteral thiamine with glucose is advised traditionally. However, this is only to ensure that thiamine supplementation is not forgotten. Administration of glucose containing fluids before thiamine may not precipitate Wernicke’s Encephalopathy 62. Due to chronic malnutrition and gastric malabsorption that follows chronic alcohol abuse, many clinicians advise multivitamin supplements (B1 + B2 + B6 + nicotinamide + Vitamin C) in parenteral form for the initial 3-5 days 63.
Chronic alcohol use is associated with abnormal magnesium metabolism. Those with neuropathy and presenting with severe withdrawal symptoms are more likely to show low serum magnesium level 64. Oral or parenteral magnesium supplementation may benefit such patients by reducing the severity and duration of alcohol withdrawal. Routine use is not advised 65
Choice of Treatment Setting
In most patients with mild to moderate withdrawal symptoms, outpatient detoxification is safe and effective, and costs less than inpatient treatment 66, 67, 68, 69. However, certain patients should be considered for inpatient treatment regardless of the severity of their symptoms. Relative indications for inpatient alcohol detoxification are as follows: history of severe withdrawal symptoms, history of withdrawal seizures or delirium tremens, multiple previous detoxifications, concomitant psychiatric or medical illness, recent high levels of alcohol consumption, pregnancy, and lack of a reliable support network 70.
If outpatient treatment is chosen, the patient should be assessed daily. The patient and support person(s) should be instructed about how to take the withdrawal medication, the side effects of the medication, the expected withdrawal symptoms, and what to do if symptoms worsen 34, 71. Small quantities of the withdrawal medication should be prescribed at each visit; thiamine and a multivitamin also should be prescribed. Because close monitoring is not available in ambulatory treatment, a fixed-schedule regimen should be used.
Alcohol withdrawal medication
Medication can be administered using fixed-schedule or symptom-triggered regimens (Table 2) 72. With a fixed-schedule regimen, doses of a benzodiazepine are administered at specific intervals, and additional doses of the medication are given as needed based on the severity of the withdrawal symptoms. In a symptom-triggered regimen, medication is given only when the Clinical Institute Withdrawal Assessment for Alcohol score is higher than 8 points.
Benzodiazepines
Pharmacologic treatment of alcohol withdrawal syndrome involves the use of medications that are cross-tolerant with alcohol. Benzodiazepines have been shown to be safe and effective, particularly for preventing or treating seizures and delirium, and are the preferred agents for treating the symptoms of alcohol withdrawal syndrome 72.
The choice of agent is based on pharmacokinetics.
- Diazepam (Valium) and chlordiazepoxide (Librium) are long-acting agents that have been shown to be excellent in treating alcohol withdrawal symptoms. Because of the long half-life of these medications, withdrawal is smoother, and rebound withdrawal symptoms are less likely to occur.
- Lorazepam (Ativan) and oxazepam (Serax) are intermediate-acting medications with excellent records of efficacy. Treatment with these agents may be preferable in patients who metabolize medications less effectively, particularly the elderly and those with liver failure. Lorazepam is the only benzodiazepine with predictable intramuscular absorption (if intramuscular administration is necessary).
Rarely, it is necessary to use extremely high dosages of benzodiazepines to control the symptoms of alcohol withdrawal. Dosages of diazepam as high as 2,000 mg per day have been administered 73. Because clinicians often are reluctant to administer exceptionally high dosages, under-treatment of alcohol withdrawal is a common problem.
One randomized controlled trial 74 affirmed previous findings that carbamazepine is an effective alternative to benzodiazepines in the treatment of alcohol withdrawal syndrome in patients with mild to moderate symptoms. Patients in the study received 800 mg of carbamazepine on the first day, with the dosage tapered to 200 mg by the fifth day. Carbamazepine (Tegretol) also appears to decrease the craving for alcohol after withdrawal. It is not sedating and has little potential for abuse. Although carbamazepine is used extensively in Europe, its use in the United States has been limited by lack of sufficient evidence that it prevents seizures and delirium.
Several medications have shown early promise in the treatment of alcohol withdrawal. Gabapentin, which is structurally similar to GABA, has been effective in the treatment of alcohol withdrawal in small studies 75, 76. The low toxicity of gabapentin makes it a promising agent. In another study 77, the anticonvulsant agent vigabatrin, which irreversibly blocks GABA transaminase, improved withdrawal symptoms after only three days of treatment.
Vigabatrin, an anticonvulsant agent, which irreversibly blocks GABA transaminase, showed improvement in withdrawal symptoms after only three days of treatment and is a promising agent for detoxification 78.
Valproic acid significantly affects the course of alcohol withdrawal and reduces the need for treatment with a benzodiazepine 79. These two double-blind 79, 80, randomized studies showed that patients treated with Valproic acid for 4 to 7 days dropped out less frequently, had less severe withdrawal symptoms including fewer seizures, and required less oxazepam than patients receiving either carbamazepine or placebo. Although effective, Valproic acid use may be limited by side effects—somnolence, gastrointestinal disturbances, confusion, and tremor—which are similar to alcohol withdrawal symptoms, making assessment of improvement difficult.
Adjunctive Agents
Several medications may be helpful adjuncts to benzodiazepines in the treatment of alcohol withdrawal syndrome. However, these medications should not be used as monotherapy.
- Haloperidol (Haldol) can be used to treat agitation and hallucinations, although it can lower the seizure threshold.
- The use of atenolol (Tenormin) in conjunction with oxazepam has been shown to improve vital signs more quickly and to reduce alcohol craving more effectively than the use of oxazepam alone 81.
Adjunctive treatment with a beta blocker should be considered in patients with coronary artery disease, who may not tolerate the strain that alcohol withdrawal can place on the cardiovascular system.
- Clonidine (Catapres) also has been shown to improve the autonomic symptoms of withdrawal 72.
Although phenytoin (Dilantin) does not treat withdrawal seizures, it is an appropriate adjunct in patients with an underlying seizure disorder.
Table 5. Examples of Treatment Regimens for Alcohol Withdrawal
Monitoring (with no medication) | |
| |
| |
Symptom-triggered regimens | |
| |
| |
Chlordiazepoxide (Librium), 50 to 100 mg | |
Diazepam (Valium), 10 to 20 mg | |
Lorazepam (Ativan), 2 to 4 mg | |
Fixed-schedule regimen | |
| |
Chlordiazepoxide, four doses of 50 mg, then eight doses of 25 mg | |
Diazepam, four doses of 10 mg, then eight doses of 5 mg | |
Lorazepam, four doses of 2 mg, then eight doses of 1 mg | |
Provide additional medication as needed when symptoms are not controlled (i.e., the Clinical Institute Withdrawal Assessment for Alcohol score remains at least 8 to 10 points). | |
Symptom-triggered regimens have been shown to result in the administration of less total medication and to require a shorter duration of treatment 83, 84. In one randomized, double-blind controlled trial 83, patients in the symptom-triggered group received an average of 100 mg of chlordiazepoxide, whereas patients in the fixed-schedule group received an average of 425 mg. The median duration of treatment in the symptom-triggered group was nine hours, compared with 68 hours in the fixed-schedule group. Patients were excluded from the study if they had concurrent medical or psychiatric illness requiring hospitalization or seizures from any cause 83.
Another trial 84 yielded similar results, with patients in the fixed-schedule group receiving an average of 231.4 mg of oxazepam and those in the symptom-triggered group receiving an average of 37.5 mg. Of the patients in the symptom-triggered group, 61 percent did not receive any oxazepam. This trial excluded persons with major psychiatric, cognitive, or medical comorbidities.
The use of symptom-triggered therapy requires training of the clinical staff. If this training has not been provided, fixed-schedule pharmacotherapy should be used 72.
Patient Follow-Up
Treatment of alcohol withdrawal syndrome should be followed by treatment for alcohol dependence. Treatment of withdrawal alone does not address the underlying disease of addiction and therefore offers little hope for long-term abstinence.
In the outpatient setting, brief interventions are helpful in patients with alcohol abuse 85, but more intense interventions are required in patients with alcohol dependence. The anticonvulsant topiramate (Topamax) has been shown to be an effective adjunctive medication to decrease alcohol consumption and increase abstinence in alcohol-dependent patients 86.
Some patients achieve dramatic results by joining 12-step groups such as Alcoholics Anonymous and Narcotics Anonymous. Other patients benefit from stays in comprehensive treatment facilities, which offer a combination of a 12-step model, cognitive-behavior therapy, and family therapy. The treatment of alcohol withdrawal syndrome should be supplemented by an individualized, comprehensive treatment program, or at least as many elements of such a program as the patient can tolerate and afford.
- Management of drug and alcohol withdrawal. Kosten TR, O’Connor PG. N Engl J Med. 2003 May 1; 348(18):1786-95. https://www.ncbi.nlm.nih.gov/pubmed/12724485/[↩]
- Liu J, Wang LN. Baclofen for alcohol withdrawal. Cochrane Database of Systematic Reviews 2017, Issue 8. Art. No.: CD008502. DOI: 10.1002/14651858.CD008502.pub5. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD008502.pub5/full[↩][↩]
- Long-term mortality of patients admitted to the hospital with alcohol withdrawal syndrome. Campos J, Roca L, Gude F, Gonzalez-Quintela A. Alcohol Clin Exp Res. 2011 Jun; 35(6):1180-6. https://www.ncbi.nlm.nih.gov/pubmed/21352245/[↩]
- Alcohol withdrawal syndrome. Bayard M, McIntyre J, Hill KR, Woodside J Jr. Am Fam Physician. 2004 Mar 15; 69(6):1443-50. http://www.aafp.org/afp/2004/0315/p1443.html[↩]
- Kattimani S, Bharadwaj B. Clinical management of alcohol withdrawal: A systematic review. Industrial Psychiatry Journal. 2013;22(2):100-108. doi:10.4103/0972-6748.132914. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085800/[↩][↩][↩][↩]
- Increased glutamatergic neurotransmission and oxidative stress after alcohol withdrawal. Tsai GE, Ragan P, Chang R, Chen S, Linnoila VM, Coyle JT. Am J Psychiatry. 1998 Jun; 155(6):726-32. https://www.ncbi.nlm.nih.gov/pubmed/9619143/[↩]
- The neurobiology of addiction: a neuroadaptational view relevant for diagnosis. Koob GF. Addiction. 2006 Sep; 101 Suppl 1():23-30. https://www.ncbi.nlm.nih.gov/pubmed/16930158/[↩]
- Update on the neurobiology of alcohol withdrawal seizures. Rogawski MA. Epilepsy Curr. 2005 Nov-Dec; 5(6):225-30. https://www.ncbi.nlm.nih.gov/pubmed/16372057/[↩]
- Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD. Economic costs of excessive alcohol consumption in the U.S., 2006. Am J Prev Med 2011;41(5):516–24. https://www.ncbi.nlm.nih.gov/pubmed/22011424[↩][↩][↩]
- US Department of Health and Human Services. NIAAA Council approves binge drinking definition. Rockville (MD): National Institute on Alcohol Abuse and Alcoholism; 2004. http://pubs.niaaa.nih.gov/publications/newsletter/winter2004/newsletter_number3.pdf[↩]
- Rehm J, Baliunas D, Borges GL, Graham K, Irving H, Kehoe T, et al. The relation between different dimensions of alcohol consumption and burden of disease: an overview. Addiction 2010;105(5):817–43. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3306013/[↩]
- Hingson RW, Zha W. Age of drinking onset, alcohol use disorders, frequent heavy drinking, and unintentionally injuring oneself and others after drinking. Pediatrics 2009;123(6):1477–84. https://www.ncbi.nlm.nih.gov/pubmed/19482757[↩]
- Dawson DA. Drinking patterns among individuals with and without DSM-IV alcohol use disorders. J Stud Alcohol 2000;61(1):111–20. https://www.ncbi.nlm.nih.gov/pubmed/10627104[↩]
- U.S. National Library of Medicine. Alcoholism and Alcohol Abuse. https://medlineplus.gov/alcoholismandalcoholabuse.html[↩][↩]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Fourth edition. Washington (DC): American Psychiatric Association; 1994.[↩]
- Centers for Disease Control and Prevention. Prevalence of Alcohol Dependence Among US Adult Drinkers, 2009–2011. https://www.cdc.gov/pcd/issues/2014/14_0329.htm[↩][↩][↩]
- Alcoholics Anonymous. http://www.aa.org/[↩][↩]
- Moderation Management. http://www.moderation.org/[↩][↩]
- Secular Organizations for Sobriety. http://www.sossobriety.org/[↩][↩]
- SMART Recovery. http://www.smartrecovery.org/[↩][↩]
- Women for Sobriety. http://womenforsobriety.org[↩][↩]
- Al-Anon Family Groups. https://al-anon.org/[↩][↩]
- Adult Children of Alcoholics. http://www.adultchildren.org/[↩][↩]
- National Council on Alcoholism and Drug Dependence. https://www.ncadd.org/[↩][↩]
- National Institute on Alcohol Abuse and Alcoholism. https://www.niaaa.nih.gov/[↩][↩]
- National Organization on Fetal Alcohol Syndrome. http://www.nofas.org/[↩][↩]
- Substance Abuse and Mental Health Services Administration. https://www.findtreatment.samhsa.gov/[↩][↩]
- American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. Alcohol Use Disorder. https://pubs.niaaa.nih.gov/publications/dsmfactsheet/dsmfact.htm[↩]
- National Institute on Alcohol Abuse and Alcoholism. Treatment for Alcohol Problems: Finding and Getting Help. https://pubs.niaaa.nih.gov/publications/Treatment/treatment.htm[↩][↩]
- National Institutes of Health. Rethinking Drinking. Professional help. https://www.rethinkingdrinking.niaaa.nih.gov/Thinking-about-a-change/support-for-quitting/Professional-Help.aspx [↩]
- National Institute on Drug Abuse. Alcohol Addiction: Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition). https://www.drugabuse.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition/evidence-based-approaches-to-drug-addiction-treatment/pharmacotherapi-1[↩][↩][↩][↩]
- Am Fam Physician. 2004 Mar 15;69(6):1443-1450. Alcohol Withdrawal Syndrome. http://www.aafp.org/afp/2004/0315/p1443.html[↩][↩][↩][↩][↩]
- Miller NS, Gold MS. Management of withdrawal syndromes and relapse prevention in drug and alcohol dependence. Am Fam Physician. 1998;58:139–46. http://www.aafp.org/afp/1998/0701/p139.html[↩]
- Kasser C, Geller A, Howell E, Wartenberg A. Detoxification: principles and protocols. American Society of Addiction Medicine. http://www.asam.org[↩][↩][↩]
- Mattson RH. Seizures associated with alcohol use and alcohol withdrawal. In: Feldman B, editor. Epilepsy:Diagnosis and Management. Boston: Little Brown; 1983. pp. 325–332.[↩]
- Status epilepticus related to alcohol abuse. Alldredge BK, Lowenstein DH. Epilepsia. 1993 Nov-Dec; 34(6):1033-7. https://www.ncbi.nlm.nih.gov/pubmed/8243353/[↩]
- Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. Mayo-Smith MF. JAMA. 1997 Jul 9; 278(2):144-51. https://www.ncbi.nlm.nih.gov/pubmed/9214531/[↩]
- Lorazepam for the prevention of recurrent seizures related to alcohol. D’Onofrio G, Rathlev NK, Ulrich AS, Fish SS, Freedland ES. N Engl J Med. 1999 Mar 25; 340(12):915-9. https://www.ncbi.nlm.nih.gov/pubmed/10094637/[↩][↩]
- Chlormethiazole: current status in the treatment of the acute ethanol withdrawal syndrome. Majumdar SK. Drug Alcohol Depend. 1991 May; 27(3):201-7. https://www.ncbi.nlm.nih.gov/pubmed/1884662/[↩]
- The management of alcohol withdrawal using chlormethiazole. Morgan MY. Alcohol Alcohol. 1995 Nov; 30(6):771-4. https://www.ncbi.nlm.nih.gov/pubmed/8679018/[↩]
- Am Fam Physician. 1998 Jul 1;58(1):139-146. Management of Withdrawal Syndromes and Relapse Prevention in Drug and Alcohol Dependence. http://www.aafp.org/afp/1998/0701/p139.html[↩][↩]
- Haber NL, Proude E, Lopatko O. Guidelines for the Treatment of Alcohol Problems. Ch. 5. Sydney, NSW: Ageing DoHa; 2009. Alcohol withdrawal management.[↩]
- Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of alcohol withdrawal: the revised Clinical Institute Withdrawal Assessment for Alcohol scale (CIWA-Ar). Br J Addict. 1989;84:1353–7.[↩][↩]
- Reoux JP, Miller K. Routine hospital alcohol detoxification practice compared to symptom triggered management with an Objective Withdrawal Scale (CIWA-Ar). Am J Addict. 2000;9:135–44.[↩]
- Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of alcohol withdrawal: the revised Clinical Institute Withdrawal Assessment for Alcohol Scale (CIWA-Ar). Br J Addict 1989;84:1353–7.[↩]
- U.S. National Library of Medicine. Medline Plus. Delirium tremens. https://medlineplus.gov/ency/article/000766.htm[↩]
- Balashov AM. GABA‐system and alcohol: does an “ethanol receptor” exist? Review. Zh Nevrol Psikhiatr Im S S Korsakova.2007;Suppl 1:56–62.[↩]
- Wang LL,Yang AK,He SM, et al.Identification of molecular targets associated with ethanol toxicity and implications in drug development.Curr Pharm Des.2010;16(11):1313–1355.[↩]
- Addolorato G,Leggio L,Agabio R,Colombo G,Gasbarrini G.Baclofen: a new drug for the treatment of alcohol dependence.Int J Clin Pract.2006;60(8):1003–1008.[↩]
- Daeppen J‐B,Gache P,Landry U, et al.Symptom‐triggered vs fixed‐schedule doses of benzodiazepine for alcohol withdrawal.Arch Intern Med.2002;162(10):1117–1121.[↩]
- Cawley MJ.Short‐term lorazepam infusion and concern for propylene glycol toxicity: case report and review.Pharmacother.2001;21(9):1140–1144.[↩]
- Kollef MH,Levy NT,Ahrens TS,Schaff R,Prentice D,Sherman G.The use of continuous IV sedation is associated with prolongation of mechanical ventilation.Chest.1998;114:541–548.[↩]
- Efficacy and safety of pharmacological interventions for the treatment of the Alcohol Withdrawal Syndrome. Amato L, Minozzi S, Davoli M. Cochrane Database Syst Rev. 2011 Jun 15; (6):CD008537. https://www.ncbi.nlm.nih.gov/pubmed/21678378/[↩][↩]
- Effects of lorazepam treatment for multiple ethanol withdrawals in mice. Becker HC, Veatch LM. Alcohol Clin Exp Res. 2002 Mar; 26(3):371-80. https://www.ncbi.nlm.nih.gov/pubmed/11923591/[↩]
- GABA systems, benzodiazepines, and substance dependence. Malcolm RJ. J Clin Psychiatry. 2003; 64 Suppl 3():36-40. https://www.ncbi.nlm.nih.gov/pubmed/12662132/[↩]
- Activity of chlormethiazole at human recombinant GABA(A) and NMDA receptors. Usala M, Thompson SA, Whiting PJ, Wafford KA. Br J Pharmacol. 2003 Nov; 140(6):1045-50. https://www.ncbi.nlm.nih.gov/pubmed/14530209/[↩]
- Action of chlormethiazole in a model of ethanol withdrawal. Green AR, Davies EM, Little HJ, Whittington MA, Cross AJ. Psychopharmacology (Berl). 1990; 102(2):239-42. https://www.ncbi.nlm.nih.gov/pubmed/2177205/[↩]
- New developments for the pharmacological treatment of alcohol withdrawal syndrome. A focus on non-benzodiazepine GABAergic medications. Leggio L, Kenna GA, Swift RM. Prog Neuropsychopharmacol Biol Psychiatry. 2008 Jul 1; 32(5):1106-17. https://www.ncbi.nlm.nih.gov/pubmed/18029075/[↩]
- Wilson A, Vulcano B. A double-blind, placebo-controlled trial of magnesium sulfate in the ethanol withdrawal syndrome. Alcohol Clin Exp Resp. 1984;8:542–5.[↩]
- The natural history and pathophysiology of Wernicke’s Encephalopathy and Korsakoff’s Psychosis. Thomson AD, Marshall EJ. Alcohol Alcohol. 2006 Mar-Apr; 41(2):151-8. https://www.ncbi.nlm.nih.gov/pubmed/16384871/[↩]
- B Vitamin deficiency and neuropsychiatric syndromes in alcohol misuse. Cook CC, Hallwood PM, Thomson AD. Alcohol Alcohol. 1998 Jul-Aug; 33(4):317-36. https://www.ncbi.nlm.nih.gov/pubmed/9719389/[↩]
- Thiamine before glucose to prevent Wernicke encephalopathy: examining the conventional wisdom. Hack JB, Hoffman RS. JAMA. 1998 Feb 25; 279(8):583-4. https://www.ncbi.nlm.nih.gov/pubmed/9486750/[↩]
- The Royal College of Physicians report on alcohol: guidelines for managing Wernicke’s encephalopathy in the accident and Emergency Department. Thomson AD, Cook CC, Touquet R, Henry JA, Royal College of Physicians, London. Alcohol Alcohol. 2002 Nov-Dec; 37(6):513-21. https://www.ncbi.nlm.nih.gov/pubmed/12414541/[↩]
- MAGNESIUM METABOLISM IN ALCOHOLISM. SULLIVAN JF, LANKFORD HG, SWARTZ MJ, FARRELL C. Am J Clin Nutr. 1963 Nov; 13():297-303. https://www.ncbi.nlm.nih.gov/pubmed/14080503/[↩]
- Management of alcohol withdrawal delirium. An evidence-based practice guideline. Mayo-Smith MF, Beecher LH, Fischer TL, Gorelick DA, Guillaume JL, Hill A, Jara G, Kasser C, Melbourne J, Working Group on the Management of Alcohol Withdrawal Delirium, Practice Guidelines Committee, American Society of Addiction Medicine. Arch Intern Med. 2004 Jul 12; 164(13):1405-12. https://www.ncbi.nlm.nih.gov/pubmed/15249349/[↩]
- Abbott PJ, Quinn D, Knox L. Ambulatory medical detoxification for alcohol. Am J Drug Alcohol Abuse. 1995;21:549–63.[↩]
- Hayashida M, Alterman AI, McLellan AT, O’Brien CP, Purtill JJ, Volpicelli JR, et al. Comparative effectiveness and costs of inpatient and outpatient detoxification of patients with mild-to-moderate alcohol withdrawal syndrome. N Engl J Med. 1989;320:358–65.[↩]
- Hayashida M, Alterman A, McLellan T, Mann S, Maany I, O’Brien C. Is inpatient medical alcohol detoxification justified: results of a randomized, controlled study. NIDA Res Monogr. 1988;81:19–25.[↩]
- Stockwell T, Bolt L, Milner I, Russell G, Bolderston H, Pugh P. Home detoxification from alcohol: its safety and efficacy in comparison with inpatient care. Alcohol Alcohol. 1991;26:645–50[↩]
- Myrick H, Anton RF. Treatment of alcohol withdrawal. Alcohol Health Res World. 1998;22:38–43.[↩]
- Myrick H, Anton RF. Clinical management of alcohol withdrawal. CNS Spectr. 2000;5:22–32.[↩]
- Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA. 1997;278:144–51.[↩][↩][↩][↩]
- Wolf KM, Shaughnessy AF, Middleton DB. Prolonged delirium tremens requiring massive doses of medication. J Am Board Fam Pract. 1993;6:502–4.[↩]
- Malcolm R, Myrick H, Roberts J, Wang W, Anton RF, Ballenger JC. The effects of carbamazepine and lorazepam on single versus multiple previous alcohol withdrawals in an outpatient randomized trial. J Gen Intern Med. 2002;17:349–55.[↩]
- Myrick H, Malcolm R, Brady KT. Gabapentin treatment of alcohol withdrawal. Am J Psychiatry. 1998;155:1632.[↩]
- Bozikas V, Petrikis P, Gamvrula K, Savvidou I, Karavatos A. Treatment of alcohol withdrawal with gabapentin. Prog Neuropsychopharmacol Biol Psychiatry. 2002;26:197–9.[↩]
- Stuppaeck CH, Deisenhammer EA, Kurz M, Whitworth AB, Hinterhuber H. The irreversible gamma-aminobutyrate transaminase inhibitor vigabatrin in the treatment of the alcohol withdrawal syndrome. Alcohol Alcohol. 1996;31:109–11.[↩]
- The irreversible gamma-aminobutyrate transaminase inhibitor vigabatrin in the treatment of the alcohol withdrawal syndrome. Stuppaeck CH, Deisenhammer EA, Kurz M, Whitworth AB, Hinterhuber H. Alcohol Alcohol. 1996 Jan; 31(1):109-11. https://www.ncbi.nlm.nih.gov/pubmed/8672169/[↩]
- Divalproex sodium in alcohol withdrawal: a randomized double-blind placebo-controlled clinical trial. Reoux JP, Saxon AJ, Malte CA, Baer JS, Sloan KL. Alcohol Clin Exp Res. 2001 Sep; 25(9):1324-9. https://www.ncbi.nlm.nih.gov/pubmed/11584152/[↩][↩]
- Update on anticonvulsants for the treatment of alcohol withdrawal. Malcolm R, Myrick H, Brady KT, Ballenger JC. Am J Addict. 2001; 10 Suppl():16-23. https://www.ncbi.nlm.nih.gov/pubmed/11268817/[↩]
- Horwitz RI, Gottlieb LD, Kraus ML. The efficacy of atenolol in the outpatient management of the alcohol withdrawal syndrome. Results of a randomized clinical trial. Arch Intern Med. 1989;149:1089–93.[↩]
- Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA 1997;278:148.[↩]
- Saitz R, Mayo-Smith MF, Roberts MS, Redmond HA, Bernard DR, Calkins DR. Individualized treatment for alcohol withdrawal. A randomized double-blind controlled trial. JAMA. 1994;272:519–23.[↩][↩][↩]
- Daeppen JB, Gache P, Landry U, Sekera E, Schweizer V, Gloor S, et al. Symptom-triggered vs fixed-schedule doses of benzodiazepine for alcohol withdrawal: a randomized treatment trial. Arch Intern Med. 2002;162:1117–21.[↩][↩]
- Fleming MF, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice for problem alcohol drinkers. A randomized controlled trial in community-based primary care practices. JAMA. 1997;277:1039–45.[↩]
- Johnson BA, AitDaoud N, Bowden CL, DiClemente CC, Roache JD, Lawson K, et al. Oral topiramate for treatment of alcohol dependence: a randomised controlled trial. Lancet. 2003;361:1677–85.[↩]