Contents
- What is traumatic brain injury
- How does traumatic brain injury affect the brain?
- Types of traumatic brain injury
- Traumatic brain injury causes
- Traumatic brain injury prevention
- Traumatic brain injury symptoms
- Traumatic brain injury symptoms long term
- Traumatic brain injury diagnosis
- Traumatic brain injury recovery
- Traumatic brain injury treatment
What is traumatic brain injury
Traumatic brain injury is an injury from a bump, blow, jolt, or penetrating object that disrupts normal functioning of the brain and damages the brain. The Brain Injury Association 1) defines traumatic brain injury as an alteration in brain function, or other evidence of brain pathology, caused by an external force.
Examples of a traumatic brain injury include:
- Falls
- Assaults
- Motor vehicle accidents
- Sports or recreation injuries.
- Gunshot wounds.
- Child abuse, including shaken baby syndrome.
- Military actions (blast injuries).
Centers for Disease Control and Prevention (CDC) traumatic brain injury facts 2):
- Falls are the leading cause of traumatic brain injury and recent data shows that the number of fall-related traumatic brain injuries among children aged 0-4 years and in older adults aged 75 years or older is increasing.
- Among all age groups, motor vehicle crashes and traffic-related incidents result in the largest percentage of traumatic brain injury-related deaths (31.8%) 3).
- People aged 65 years old and older have the highest rates of traumatic brain injury-related hospitalizations and death 4).
- Shaken Baby Syndrome, a form of abusive head trauma and inflicted traumatic brain injury, is a leading cause of child maltreatment deaths in the United States.
Causes of traumatic brain injury include falls, car accidents, sports-related impacts, and penetrating injuries. Half of all traumatic brain injuries are from motor vehicle accidents. Military personnel in combat zones are also at risk. However, not all blows or jolts to the head result in a traumatic brain injury. The severity of a traumatic brain injury may range from “mild” (i.e., a brief change in mental status or consciousness) to “severe” (i.e., an extended period of unconsciousness or memory loss after the injury). Most traumatic brain injuries that occur each year are mild, commonly called concussions 5). The worst traumatic brain injuries can lead to permanent brain damage or death.
Traumatic brain injury is the leading cause of death and disability in children and young adults in the United States. Traumatic brain injuries contribute to about 30% of all injury deaths 6). Every day, 153 people in the United States die from injuries that include traumatic brain injury 7). Over the past few decades preventive measures, such as seatbelts and helmets, and better critical care have substantially increased survival from severe traumatic brain injury. Those who survive a traumatic brain injury can face effects that last a few days, or the rest of their lives. Effects of traumatic brain injury can include impaired thinking or memory, movement, sensation (e.g., vision or hearing), or emotional functioning (e.g., personality changes, depression). These issues not only affect individuals but can have lasting effects on families and communities.
Traumatic brain injury is also a major concern for elderly individuals, with a high rate of death and hospitalization due to falls among people age 75 and older. Depending on the severity of injury, traumatic brain injury can have a lasting impact on quality of life for survivors of all ages – impairing thinking, decision making and reasoning, concentration, memory, movement, and/or sensation (e.g., vision or hearing), and causing emotional problems (personality changes, impulsivity, anxiety, and depression) and epilepsy.
Some symptoms of a traumatic brain injury happen immediately after the traumatic event. Others may not appear for several days or weeks.
For a mild traumatic brain injury (concussion), it’s normal to feel dizzy, nauseated, or have a headache. Other mild symptoms include:
- Ringing in your ears.
- Neck pain.
- Blurry vision.
- Confusion.
- Slow reflexes.
- Brief loss of consciousness.
In addition to these symptoms, moderate or severe traumatic brain injuries may include:
- Lasting nausea or vomiting.
- A headache that gets worse or does not go away.
- Dilated (larger than normal) pupils.
- Trouble waking up, walking, or speaking.
- Inability to awaken from sleep.
- Slurred speech.
- Weakness or numbness in your arms or legs.
- Drainage of bloody or clear fluids from your ears or nose.
- Convulsions or seizures.
- Repeated vomiting or nausea.
Mild symptoms go away after a few days or weeks. Worse traumatic brain injurys can have lasting effects. Your mood can change, making you feel angry, anxious, or sensitive. Short-term memory can be affected, as well as your ability to think and focus. You may have trouble controlling your impulses.
Traumatic brain injuries are serious. They cause damage that can be permanent. In some cases, a traumatic brain injury can lead to coma or death. Always seek medical care if you have hit your head. If your symptoms are severe, call your local emergency services number or go to the emergency room. Contact a doctor if someone you know has a head injury and acts strange.
Health care professionals use a neurological exam and imaging tests to assess traumatic brain injury. Serious traumatic brain injuries need emergency treatment. Treatment and outcome depend on how severe the injury is. Traumatic brain injury can cause a wide range of changes affecting thinking, sensation, language, or emotions. Traumatic brain injury can be associated with post-traumatic stress disorder. People with severe traumatic brain injuries usually need rehabilitation.
Recently, research has expanded from a singular focus on severe traumatic brain injury to a greater awareness about potential long-term consequences and the need to find better ways to diagnose, treat, and prevent all forms of traumatic brain injury. Many questions remain unanswered regarding the impact of traumatic brain injuries, the best treatments, and the most effective methods for promoting recovery of brain function.
Traumatic brain injury statistics
- In 2013, about 2.8 million traumatic brain injury-related emergency department visits, hospitalizations, and deaths occurred in the United States 8).
- traumatic brain injury contributed to the deaths of nearly 50,000 people.
- traumatic brain injury was a diagnosis in more than 282,000 hospitalizations and 2.5 million emergency department visits. These consisted of traumatic brain injury alone or traumatic brain injury in combination with other injuries.
- Over the span of six years (2007–2013), while rates of traumatic brain injury-related emergency department visits increased by 47%, hospitalization rates decreased by 2.5% and death rates decreased by 5%.
- In 2012, an estimated 329,290 children (age 19 or younger) were treated in U.S. emergency departments for sports and recreation-related injuries that included a diagnosis of concussion or traumatic brain injury 9).
- From 2001 to 2012, the rate of emergency department visits for sports and recreation-related injuries with a diagnosis of concussion or traumatic brain injury, alone or in combination with other injuries, more than doubled among children (age 19 or younger) 10).
- Annually, traumatic brain injury injuries cost an estimated $76 billion in direct and indirect medical expenses. These figures are likely an underestimate of the true number of traumatic brain injuries as they exclude people who did not seek medical attention at the emergency room.
- Although approximately 75 percent of brain injuries are considered mild (not life-threatening), as many as 5.3 million people in the United States are estimated to be living with the challenges of long-term traumatic brain injury-related disability.
- Not every traumatic brain injury is alike. Each injury is unique and can cause changes that affect a person for a short period of time, or sometimes permanently.
- The majority of people will completely recover from symptoms related to concussion (mild type of traumatic brain injury). However, persistent symptoms do occur for some people and may last for weeks or months. The long-term effects of traumatic brain injury may vary depending on the number and nature of “hits” to the head, the age and gender of the individual, the speed with which the person received medical attention, and genetic and other factors.
Always see your doctor if you or your child has received a blow to the head or body that concerns you or causes behavioral changes.
Seek emergency medical care if there are any signs or symptoms of traumatic brain injury following a recent blow or other traumatic injury to the head.
The terms “mild,” “moderate” and “severe” are used to describe the effect of the injury on brain function. A mild injury to the brain is still a serious injury that requires prompt attention and an accurate diagnosis.
Danger Signs in Adults
In rare cases, a person with a concussion may form a dangerous blood clot that crowds the brain against the skull. Contact your health care professional or emergency department right away if you experience these danger signs after a bump, blow, or jolt to your head or body:
- Headache that gets worse and does not go away.
- Weakness, numbness or decreased coordination.
- Repeated vomiting or nausea.
- Slurred speech.
The people checking on you should take you to an emergency department right away if you:
- Look very drowsy or cannot wake up.
- Have one pupil (the black part in the middle of the eye) larger than the other.
- Have convulsions or seizures.
- Cannot recognize people or places.
- Are getting more and more confused, restless, or agitated.
- Have unusual behavior.
- Lose consciousness.
Danger Signs in Children
Take your child to the emergency department right away if they received a bump, blow, or jolt to the head or body, and:
- Have any of the danger signs for adults listed above.
- Will not stop crying and are inconsolable.
- Will not nurse or eat.
Is a concussion a traumatic brain injury?
Yes. Medical providers may describe a concussion as a “mild” brain injury because concussions are usually not life-threatening. Even so, the effects of a concussion can be serious.
Children and teens who show or report one or more of the signs and symptoms listed below, or simply say they just “don’t feel right” after a bump, blow, or jolt to the head or body, may have a concussion or more serious brain injury.
Concussion Signs Observed
- Can’t recall events prior to or after a hit or fall.
- Appears dazed or stunned.
- Forgets an instruction, is confused about an assignment or position, or is unsure of the game, score, or opponent.
- Moves clumsily.
- Answers questions slowly.
- Loses consciousness (even briefly).
- Shows mood, behavior, or personality changes.
Concussion Symptoms Reported
- Headache or “pressure” in head.
- Nausea or vomiting.
- Balance problems or dizziness, or double or blurry vision.
- Bothered by light or noise.
- Feeling sluggish, hazy, foggy, or groggy.
- Confusion, or concentration or memory problems.
- Just not “feeling right,” or “feeling down”.
Signs and symptoms generally show up soon after the injury. However, you may not know how serious the injury is at first and some symptoms may not show up for hours or days. For example, in the first few minutes your child or teen might be a little confused or a bit dazed, but an hour later your child might not be able to remember how he or she got hurt.
You should continue to check for signs of concussion right after the injury and a few days after the injury. If your child or teen’s concussion signs or symptoms get worse, you should take him or her to the emergency department right away.
Can a person who has sustained a brain injury drink alcohol?
Alcohol consumption following a brain injury is known to reduce brain injury recovery and, consequently, is not recommended. After sustaining a brain injury, many find they are much more sensitive to the effects of alcohol – specifically its negative impact on cognition and an increase in symptoms of depression.
For these reasons, staying away from alcohol is strongly recommended to avoid further injury to the brain and to promote as much healing as possible. Please consult your physician prior to drinking any amount of alcohol after a brain injury.
How does traumatic brain injury affect the brain?
Traumatic brain injury-related damage can be confined to one area of the brain, known as a focal injury, or it can occur over a more widespread area, known as a diffuse injury. The type of injury is another determinant of the effect on the brain. Some injuries are considered primary, meaning the damage is immediate. Other consequences of traumatic brain injury can be secondary, meaning they can occur gradually over the course of hours, days, or weeks. These secondary brain injuries are the result of reactive processes that occur after the initial head trauma.
There are a variety of immediate effects on the brain, including various types of bleeding and tearing forces that injure nerve fibers and cause inflammation, metabolic changes, and brain swelling.
- Diffuse axonal injury is one of the most common types of brain injuries. Diffuse axonal injury refers to widespread damage to the brain’s white matter. White matter is composed of bundles of axons (projections of nerve cells that carry electrical impulses). Like the wires in a computer, axons connect various areas of the brain to one another. Diffuse axonal injury is the result of shearing forces, which stretch or tear these axon bundles. This damage commonly occurs in auto accidents, falls, or sports injuries. It usually results from rotational forces (twisting) or sudden deceleration. It can result in a disruption of neural circuits and a breakdown of overall communication among nerve cells, or neurons, in the brain. It also leads to the release of brain chemicals that can cause further damage. These injuries can cause temporary or permanent damage to the brain, and recovery can be prolonged.
- Concussion– a type of mild traumatic brain injury that may be considered a temporary injury to the brain but could take minutes to several months to heal. Concussion can be caused by a number of things including a bump, blow, or jolt to the head, sports injury or fall, motor vehicle accident, weapons blast, or a rapid acceleration or deceleration of the brain within the skull (such as the person having been violently shaken). The individual either suddenly loses consciousness or has sudden altered state of consciousness or awareness, and is often called “dazed” or said to have his/her “bell rung.” A second concussion closely following the first one causes further damage to the brain — the so-called “second hit” phenomenon — and can lead to permanent damage or even death in some instances.
- Hematomas — a pooling of blood in the tissues outside of the blood vessels. Hematomas can develop when major blood vessels in the head become damaged, causing severe bleeding in and around the brain. Different types of hematomas form depending on where the blood collects relative to the meninges. The meninges are the protective membranes surrounding the brain, which consist of three layers: dura mater (outermost), arachnoid mater (middle), and pia mater (innermost).
- Epidural hematomas involve bleeding into the area between the skull and the dura mater. These can occur with a delay of minutes to hours after a skull fracture damages an artery under the skull, and are particularly dangerous.
- Subdural hematomas involve bleeding between the dura and the arachnoid mater, and like epidural hematomas exert pressure on the outside of the brain . Their effects vary depending on their size and extent to which they compress the brain. They are very common in the elderly after a fall.
- Subarachnoid hemorrhage is bleeding that occurs between the arachnoid mater and the pia mater and their effects vary depending on the amount of bleeding.
- Bleeding into the brain itself is called an intracerebral hematoma and damages the surrounding tissue.
- Contusions — a bruising or swelling of the brain that occurs when very small blood vessels bleed into brain tissue. Contusions can occur directly under the impact site (i.e, a coup injury) or, more often, on the complete opposite side of the brain from the impact (i.e., a contrecoup injury). They can appear after a delay of hours to a day.
- Coup/Contrecoup lesions — contusions or subdural hematomas that occur at the site of head impact as well as directly opposite the coup lesion. Generally they occur when the head abruptly decelerates, which causes the brain to bounce back and forth within the skull (such as in a high-speed car crash). This type of injury also occurs in shaken baby syndrome, a severe head injury that results when an infant or toddler is shaken forcibly enough to cause the brain to bounce back and forth against the skull.
- Skull fractures — breaks or cracks in one or more of the bones that form the skull. They are a result of blunt force trauma and can cause damage to the underlying areas of the skull such as the membranes, blood vessels, and brain. One main benefit of helmets is to prevent skull fracture.
The first 24 hours after mild traumatic brain injury are particularly important because subdural hematoma, epidural hematoma, ontusion, or excessive brain swelling (edema) are possible and can cause further damage. For this reason doctors suggest watching a person for changes for 24 hours after a concussion.
- Hemorrhagic progression of a contusion contributes to secondary injuries. Hemorrhagic progression of a contusions occur when an initial contusion from the primary injury continues to bleed and expand over time. This creates a new or larger lesion — an area of tissue that has been damaged through injury or disease. This increased exposure to blood, which is toxic to brain cells, leads to swelling and further brain cell loss.
- Secondary damage may also be caused by a breakdown in the blood-brain barrier. The blood-brain barrier preserves the separation between the brain fluid and the very small capillaries that bring the brain nutrients and oxygen through the blood. Once disrupted, blood, plasma proteins, and other foreign substances leak into the space between neurons in the brain and trigger a chain reaction that causes the brain to swell. It also causes multiple biological systems to go into overdrive, including inflammatory responses which can be harmful to the body if they continue for an extended period of time. It also permits the release of neurotransmitters, chemicals used by brain cells to communicate, which can damage or kill nerve cells when depleted or over-expressed.
- Poor blood flow to the brain can also cause secondary damage. When the brain sustains a powerful blow, swelling occurs just as it would in other parts of the body. Because the skull cannot expand, the brain tissue swells and the pressure inside the skull rises; this is known as intracranial pressure (ICP). When the intracranial pressure becomes too high it prevents blood from flowing to the brain, which deprives it of the oxygen it needs to function. This can permanently damage brain function.
Types of traumatic brain injury
There are different types of injuries that can happen to the brain:
- A concussion occurs from a hard fall or hit to the head. It jars your brain and causes shock or trauma. Most of the time you don’t lose consciousness. You may feel dazed and off-balance. You also may have brief decreased vision or memory.
- A brain contusion is a bruise of the brain, in which swollen brain tissue mixes with blood released from broken blood vessels. Brain contusion causes bleeding in your brain and swelling. The bruise is not always visible on your skin. A contusion can occur from the brain shaking back and forth against the skull, such as from a car collision or sports accident or in shaken baby syndrome.
- A skull fracture is when the skull cracks. Sometimes broken bones cut into your brain and cause bleeding or other damage.
- An intracranial hematoma is bleeding inside the skull that collects and clots. A mass of clotted blood forms between your brain and skull. It may not show up for a few days, or even weeks, after an injury.
- Anoxia, absence of oxygen to the brain, causes damage to the brain tissue.
The most common form of traumatic brain injury is concussion 11). A concussion can happen when the head or body is moved back and forth quickly, such as during a motor vehicle accident or sports injury. Concussions are often called “mild traumatic brain injury” because they are usually not life-threatening. However, they still can cause serious problems, and research suggests that repeated concussions can be particularly dangerous 12).
Traumatic brain injury can happen to anyone, but certain groups face a greater risk for traumatic brain injury than others. traumatic brain injury among members of the military has become a particular concern in recent years because many military personnel in Iraq and Afghanistan have been exposed to such traumatic brain injury hazards as improvised explosive devices. Head and neck injuries, including severe brain trauma, have been reported in 1 out of 4 military members who were evacuated from those conflicts 13).
Traumatic brain injury injury severity can be described using several different tools:
The Glasgow Coma Scale (GCS), a clinical tool designed to assess coma and impaired consciousness, is one of the most commonly used severity scoring systems 14).
- Glasgow Coma Scale scores of 3 to 8 are classified as a severe traumatic brain injury,
- Glasgow Coma Scale scores of 9 to 12 are classified as a moderate traumatic brain injury,
- Glasgow Coma Scale scores of 13 to 15 are classified as a mild traumatic brain injury.
Other classification systems include the Abbreviated Injury Scale (AIS), the Trauma Score, and the Abbreviated Trauma Score 15). Despite their limitations, these systems are crucial to understanding the clinical management and the likely outcomes of this injury as the prognosis for milder forms of traumatic brain injurys is better than for moderate or severe traumatic brain injuries 16).
Traumatic brain injury causes
Traumatic brain injury is usually caused by a blow or other traumatic injury to the head or body. The degree of damage can depend on several factors, including the nature of the injury and the force of impact.
Common events causing traumatic brain injury include the following:
- Falls. Falls from bed or a ladder, down stairs, in the bath and other falls are the most common cause of traumatic brain injury overall, particularly in older adults and young children.
- Vehicle-related collisions. Collisions involving cars, motorcycles or bicycles — and pedestrians involved in such accidents — are a common cause of traumatic brain injury.
- Violence. Gunshot wounds, domestic violence, child abuse and other assaults are common causes. Shaken baby syndrome is a traumatic brain injury in infants caused by violent shaking.
- Sports injuries. Traumatic brain injuries may be caused by injuries from a number of sports, including soccer, boxing, football, baseball, lacrosse, skateboarding, hockey, and other high-impact or extreme sports. These are particularly common in youth.
- Explosive blasts and other combat injuries. Explosive blasts are a common cause of traumatic brain injury in active-duty military personnel. Although how the damage occurs isn’t yet well-understood, many researchers believe that the pressure wave passing through the brain significantly disrupts brain function. Traumatic brain injury also results from penetrating wounds, severe blows to the head with shrapnel or debris, and falls or bodily collisions with objects following a blast.
Risk factors for traumatic brain injury
The people most at risk of traumatic brain injury include:
- Children, especially newborns to 4-year-olds
- Young adults, especially those between ages 15 and 24
- Adults age 60 and older
- Males in any age group
Among traumatic brain injury-related deaths in 2013 17):
- Rates were highest for persons 75 years of age and older.
- The leading cause of traumatic brain injury-related death varied by age.
- Falls were the leading cause of death for persons 65 years of age or older.
- Intentional self-harm was the leading cause of death for persons 25-64 years of age.
- Motor vehicle crashes were the leading cause of death for persons 5-24 years of age.
- Assaults were the leading cause of death for children ages 0-4 years.
Among non-fatal traumatic brain injury-related injuries in 2013 18):
- Hospitalization rates were highest among persons 75 years of age and older.
- Rates of emergency department visits were highest for persons 75 years of age and older and children 0-4 years of age.
- Falls were the leading cause of traumatic brain injury-related emergency department visits for all but one age group.
- Being struck by or against an object was the leading cause of traumatic brain injury-related emergency department visits for persons 15 to 24 years of age.
- The leading cause of traumatic brain injury-related hospitalizations varied by age:
- Falls were the leading cause among children 0-14 years of age and adults 45 years of age and older.
- Motor vehicle crashes were the leading cause of hospitalizations for adolescents and persons 15-44 years of age.
Traumatic brain injury prevention
Follow these tips to reduce the risk of brain injury:
- Seat belts and airbags. Always wear a seat belt in a motor vehicle. A small child should always sit in the back seat of a car secured in a child safety seat or booster seat that is appropriate for his or her size and weight.
- Alcohol and drug use. Don’t drive under the influence of alcohol or drugs, including prescription medications that can impair the ability to drive.
- Helmets. Wear a helmet while riding a bicycle, skateboard, motorcycle, snowmobile or all-terrain vehicle. Also wear appropriate head protection when playing baseball or contact sports, skiing, skating, snowboarding or riding a horse.
- Avoid dangerous sports and activities.
Preventing falls
The following tips can help older adults avoid falls around the house:
- Install handrails in bathrooms
- Put a nonslip mat in the bathtub or shower
- Remove area rugs
- Install handrails on both sides of staircases
- Improve lighting in the home
- Keep stairs and floors clear of clutter
- Get regular vision checkups
- Get regular exercise
Preventing head injuries in children
The following tips can help children avoid head injuries:
- Install safety gates at the top of a stairway
- Keep stairs clear of clutter
- Install window guards to prevent falls
- Put a nonslip mat in the bathtub or shower
- Use playgrounds that have shock-absorbing materials on the ground
- Make sure area rugs are secure
- Don’t let children play on fire escapes or balconies
Traumatic brain injury symptoms
Traumatic brain injury can have wide-ranging physical and psychological effects. Some signs or symptoms may appear immediately after the traumatic event, while others may appear days or weeks later.
Mild traumatic brain injury
The signs and symptoms of mild traumatic brain injury (concussion) may include:
Physical symptoms
- Loss of consciousness for a few seconds to a few minutes
- No loss of consciousness, but a state of being dazed, confused or disoriented
- Headache
- Nausea or vomiting
- Fatigue or drowsiness
- Problems with speech
- Difficulty sleeping
- Sleeping more than usual, sleep less than usual or trouble falling asleep
- Dizziness
- Balance problems
- Feeling tired, having no energy
Sensory symptoms
- Sensory problems, such as blurred vision, ringing in the ears, a bad taste in the mouth or changes in the ability to smell
- Sensitivity to light or sound
Cognitive or mental symptoms
- Memory or concentration problems
- Mood changes or mood swings
- Feeling depressed or anxious
- Difficulty thinking clearly
- Feeling slowed down
- Difficulty concentrating
- Difficulty remembering new information
Some of these symptoms may appear right away. Others may not be noticed for days or months after the injury, or until the person resumes their everyday life. Sometimes, people do not recognize or admit that they are having problems. Others may not understand their problems and how the symptoms they are experiencing impact their daily activities.
The signs and symptoms of a concussion can be difficult to sort out. Early on, problems may be overlooked by the person with the concussion, family members, or doctors. People may look fine even though they are acting or feeling differently.
Moderate to severe traumatic brain injuries
Moderate to severe traumatic brain injuries can include any of the signs and symptoms of mild injury, as well as these symptoms that may appear within the first hours to days after a head injury:
Physical symptoms
- Loss of consciousness from several minutes to hours
- Persistent headache or headache that worsens
- Repeated vomiting or nausea
- Convulsions or seizures
- Dilation of one or both pupils of the eyes
- Clear fluids draining from the nose or ears
- Inability to awaken from sleep
- Weakness or numbness in fingers and toes
- Loss of coordination
Cognitive or mental symptoms
- Profound confusion
- Agitation, combativeness or other unusual behavior
- Slurred speech
- Coma and other disorders of consciousness
Effects on consciousness
A traumatic brain injury can cause problems with arousal, consciousness, awareness, alertness, and responsiveness. Generally, there are four abnormal states that can result from a severe traumatic brain injury:
- Brain death – The lack of measurable brain function and activity after an extended period of time is called brain death and may be confirmed by studies that show no blood flow to the brain.Coma – A person in a coma is totally unconscious, unaware, and unable to respond to external stimuli such as pain or light. Coma generally lasts a few days or weeks after which an individual may regain consciousness, die, or move into a vegetative state.
- Vegetative state – A result of widespread damage to the brain, people in a vegetative state are unconscious and unaware of their surroundings. However, they can have periods of unresponsive alertness and may groan, move, or show reflex responses. If this state lasts longer than a few weeks it is referred to as a persistent vegetative state.
- Minimally conscious state – People with severely altered consciousness who still display some evidence of self-awareness or awareness of one’s environment (such as following simple commands, yes/no responses).
Children’s traumatic brain injury symptoms
Infants and young children with brain injuries might not be able to communicate headaches, sensory problems, confusion and similar symptoms. In a child with traumatic brain injury, you may observe:
- Change in eating or nursing habits
- Unusual or easy irritability
- Persistent crying and inability to be consoled
- Change in ability to pay attention
- Change in sleep habits
- Seizures
- Sad or depressed mood
- Drowsiness
- Loss of interest in favorite toys or activities
Traumatic brain injury symptoms long term
Several complications can occur immediately or soon after a traumatic brain injury. Severe injuries increase the risk of a greater number and more-severe complications.
Potential affects of severe traumatic brain injury
A non-fatal severe traumatic brain injury may result in an extended period of unconsciousness (coma) or amnesia after the injury. For individuals hospitalized after a traumatic brain injury, almost half (43%) have a related disability one year after the injury 19). A traumatic brain injury may lead to a wide range of short- or long-term issues affecting:
- Cognitive Function (e.g., attention and memory)
- Motor function (e.g., extremity weakness, impaired coordination and balance)
- Sensation (e.g., hearing, vision, impaired perception and touch)
- Emotion (e.g., depression, anxiety, aggression, impulse control, personality changes)
Approximately 5.3 million Americans are living with a traumatic brain injury-related disability and the consequences of severe traumatic brain injury can affect all aspects of an individual’s life 20). This can include relationships with family and friends, as well as their ability to work or be employed, do household tasks, drive, and/or participate in other activities of daily living.
Altered consciousness
Moderate to severe traumatic brain injury can result in prolonged or permanent changes in a person’s state of consciousness, awareness or responsiveness. Different states of consciousness include:
- Coma. A person in a coma is unconscious, unaware of anything and unable to respond to any stimulus. This results from widespread damage to all parts of the brain. After a few days to a few weeks, a person may emerge from a coma or enter a vegetative state.
- Vegetative state. Widespread damage to the brain can result in a vegetative state. Although the person is unaware of surroundings, he or she may open his or her eyes, make sounds, respond to reflexes, or move. It’s possible that a vegetative state can become permanent, but often individuals progress to a minimally conscious state.
- Minimally conscious state. A minimally conscious state is a condition of severely altered consciousness but with some signs of self-awareness or awareness of one’s environment. It is sometimes a transitional state from a coma or vegetative condition to greater recovery.
- Brain death. When there is no measurable activity in the brain and the brainstem, this is called brain death. In a person who has been declared brain dead, removal of breathing devices will result in cessation of breathing and eventual heart failure. Brain death is considered irreversible.
Physical complications
- Seizures. Some people with traumatic brain injury will develop seizures. The seizures may occur only in the early stages, or years after the injury. Recurrent seizures are called post-traumatic epilepsy.
- Fluid buildup in the brain (hydrocephalus). Cerebrospinal fluid may build up in the spaces in the brain (cerebral ventricles) of some people who have had traumatic brain injuries, causing increased pressure and swelling in the brain.
- Infections. Skull fractures or penetrating wounds can tear the layers of protective tissues (meninges) that surround the brain. This can enable bacteria to enter the brain and cause infections. An infection of the meninges (meningitis) could spread to the rest of the nervous system if not treated.
- Blood vessel damage. Several small or large blood vessels in the brain may be damaged in a traumatic brain injury. This damage could lead to a stroke, blood clots or other problems.
- Headaches. Frequent headaches are very common after a traumatic brain injury. They may begin within a week after the injury and could persist as long as several months.
- Vertigo. Many people experience vertigo, a condition characterized by dizziness, after a traumatic brain injury.
Sometimes, any or several of these symptoms might linger for a few weeks to a few months after a traumatic brain injury. This is currently referred to as persistent post-concussive symptoms. When a combination of these symptoms last for an extended period of time, this is generally referred to as post-concussion syndrome.
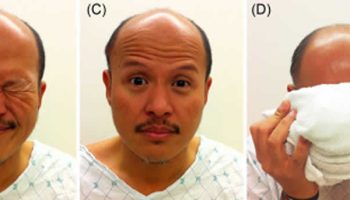
Traumatic brain injuries at the base of the skull can cause nerve damage to the nerves that emerge directly from the brain (cranial nerves). Cranial nerve damage may result in:
- Paralysis of facial muscles or losing sensation in the face
- Loss of or altered sense of smell
- Loss of or altered sense of taste
- Loss of vision or double vision
- Swallowing problems
- Dizziness
- Ringing in the ear
- Hearing loss
Intellectual problems
Many people who have had a significant brain injury will experience changes in their thinking (cognitive) skills. It may be more difficult to focus and take longer to process your thoughts. Traumatic brain injury can result in problems with many skills, including:
Cognitive problems
- Memory
- Learning
- Reasoning
- Judgment
- Attention or concentration
Executive functioning problems
- Problem-solving
- Multitasking
- Organization
- Planning
- Decision-making
- Beginning or completing tasks
Communication problems
Language and communications problems are common following traumatic brain injuries. These problems can cause frustration, conflict and misunderstanding for people with a traumatic brain injury, as well as family members, friends and care providers.
Communication problems may include:
Cognitive problems
- Difficulty understanding speech or writing
- Difficulty speaking or writing
- Inability to organize thoughts and ideas
- Trouble following and participating in conversations
Social problems
- Trouble with turn taking or topic selection in conversations
- Problems with changes in tone, pitch or emphasis to express emotions, attitudes or subtle differences in meaning
- Difficulty understanding nonverbal signals
- Trouble reading cues from listeners
- Trouble starting or stopping conversations
- Inability to use the muscles needed to form words (dysarthria)
Behavioral changes
People who’ve experienced brain injury often experience changes in behaviors. These may include:
- Difficulty with self-control
- Lack of awareness of abilities
- Risky behavior
- Difficulty in social situations
- Verbal or physical outbursts
Emotional changes
Emotional changes may include:
- Depression
- Anxiety
- Mood swings
- Irritability
- Lack of empathy for others
- Anger
- Insomnia
Sensory problems
Problems involving senses may include:
- Persistent ringing in the ears
- Difficulty recognizing objects
- Impaired hand-eye coordination
- Blind spots or double vision
- A bitter taste, a bad smell or difficulty smelling
- Skin tingling, pain or itching
- Trouble with balance or dizziness
Degenerative brain diseases
Research suggests that repeated or severe traumatic brain injuries might increase the risk of degenerative brain diseases. But, this risk can’t be predicted for an individual — and researchers are still investigating if, why and how traumatic brain injuries might be related to degenerative brain diseases.
A degenerative brain disorder can cause gradual loss of brain functions, including:
- Alzheimer’s disease, which primarily causes the progressive loss of memory and other thinking skills
- Parkinson’s disease, a progressive condition that causes movement problems, such as tremors, rigidity and slow movements
- Dementia pugilistica — most often associated with repetitive blows to the head in career boxing — which causes symptoms of dementia and movement problems
Traumatic brain injury diagnosis
Traumatic brain injuries are usually emergencies and consequences can worsen rapidly without treatment. Doctors usually need to assess the situation quickly.
Glasgow Coma Scale
Glasgow Coma Scale 15-point test helps a doctor or other emergency medical personnel assess the initial severity of a brain injury by checking a person’s ability to follow directions and move their eyes and limbs. The coherence of speech also provides important clues.
Abilities are scored from 3 to 15 in the Glasgow Coma Scale. Higher scores mean less severe injuries (Total Normal Glasgow Coma Score is 15 out of 15).
Measurements for Level of traumatic brain injury
Health care providers sometimes rank the person’s level of consciousness, memory loss, and Glasgow Coma Scale score.
- A traumatic brain injury is considered Mild if:
- The person was not unconscious or was unconscious for less than 30 minutes.
- Memory loss lasted less than 24 hours.
- Glasgow Coma Scale scores of 13 to 15
- A traumatic brain injury is considered Moderate if:
- The person was unconscious for more than 30 minutes and up to 24 hours.
- Memory loss lasted anywhere from 24 hours to 7 days.
- Glasgow Coma Scale scores of 9 to 12
- A traumatic brain injury is considered Severe if:
- The person was unconscious for more than 24 hours.
- Memory loss lasted more than 7 days.
- Glasgow Coma Scale scores of 3 to 8
Table 1. Glasgow Coma Scale
| Under 4 years of age | Above 4 years of age | ||
| Response | Score | Response | Score |
| Eye opening | Eye opening | ||
| Spontaneously | 4 | Spontaneously | 4 |
| To verbal stimuli | 3 | To verbal stimuli | 3 |
| To painful stimuli | 2 | To painful stimuli | 2 |
| No response to pain | 1 | No response to pain | 1 |
| Best verbal response | Best verbal response | ||
| Orientated and converses | 5 | Appropriate words or social smile, fixes, follows | 5 |
| Confused and converses | 4 | Cries but consolable; less than usual words | 4 |
| Inappropriate words | 3 | Persistently irritable | 3 |
| Incomprehensible sounds | 2 | Moans to pain | 2 |
| No response to pain | 1 | No response to pain | 1 |
| Best motor response | Best motor response | ||
| Obeys verbal commands | 6 | Spontaneous or obeys verbal commands | 6 |
| Localises to stimuli | 5 | Localizes to stimuli | 5 |
| Withdraws to stimuli | 4 | Withdraws to stimuli | 4 |
| Abnormal flexion to pain (decorticate) | 3 | Abnormal flexion to pain (decorticate) | 3 |
| Abnormal extension to pain (decerebrate) | 2 | Abnormal extension to pain (decerebrate) | 2 |
| No response to pain | 1 | No response to pain | 1 |
Information about the injury and symptoms
If you saw someone sustain an injury or arrived immediately after an injury, you may be able to provide medical personnel with information that’s useful in assessing the injured person’s condition.
Answers to the following questions may be beneficial in judging the severity of injury:
- How did the injury occur?
- Did the person lose consciousness?
- How long was the person unconscious?
- Did you observe any other changes in alertness, speaking, coordination or other signs of injury?
- Where was the head or other parts of the body struck?
- Can you provide any information about the force of the injury? For example, what hit the person’s head, how far did he or she fall, or was the person thrown from a vehicle?
- Was the person’s body whipped around or severely jarred?
Speech and Language Tests
A speech-language pathologist completes a formal evaluation of speech and language skills, including an oral motor evaluation of the strength and coordination of the muscles that control speech, understanding and use of grammar and vocabulary, as well as reading and writing 21).
- Social communication skills are evaluated with formal tests and role-playing scenarios.
- If a patient has problems with swallowing, the speech-language pathologist will make recommendations regarding management and treatment to ensure that the individual is able to swallow safely and receive adequate nutrition.
Cognition and Neuropsychological Tests
- Cognition describes the processes of thinking, reasoning, problem solving, information processing, and memory.
- Most patients with severe traumatic brain injury suffer from cognitive disabilities, including the loss of many higher level mental skills.
- Neuropsychological assessments are often used to obtain information about cognitive capabilities.
- These tests are specialized task-oriented evaluations of human brain-behavior relationships, evaluating higher cognitive functioning as well as basic sensory-motor processes 22).
- Testing by a neuropsychologist can assess the individual’s cognitive, language, behavioral, motor, and executive functions and provide information regarding the need for rehabilitative services 23).
- For this assessment, a neuropsychologist reviews the case history and hospital records of the patient, and interviews the patient and his/her family.
- The neuropsychologist acquires information about the “person” the individual was before the injury, based on aspects like school performance, habits, and lifestyle, in order to detail which abilities remain unchanged as well as areas of the brain that are adversely affected by the injury and how the injury is expected to impact the individual’s life 24).
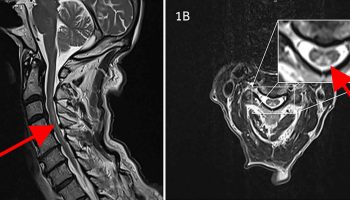
Imaging tests
Health care providers may also use tests that take images of a person’s brain. These include, but are not limited to:
- Computerized tomography (CT) scan. This test is usually the first performed in an emergency room for a suspected traumatic brain injury. A CT scan uses a series of X-rays to create a detailed view of the brain. A CT scan can quickly visualize fractures and uncover evidence of bleeding in the brain (hemorrhage), blood clots (hematomas), bruised brain tissue (contusions), and brain tissue swelling.
- Magnetic resonance imaging (MRI). An MRI uses powerful radio waves and magnets to create a detailed view of the brain. This test may be used after the person’s condition stabilizes, or if symptoms don’t improve soon after the injury.
Intracranial pressure monitor
Tissue swelling from a traumatic brain injury can increase pressure inside the skull and cause additional damage to the brain. Doctors may insert a probe through the skull to monitor this pressure.
Traumatic brain injury recovery
Most people with a concussion (mild traumatic brain injury) feel better within a couple of weeks. However for some, symptoms will last for a month or longer. Concussion symptoms may appear during the normal healing process or as you get back to your regular activities. If there are any symptoms that concern you or are getting worse, be sure to seek medical care as soon as possible.
In some cases, repeated blows to the head can cause chronic traumatic encephalopathy (CTE) – a progressive neurological disorder associated with a variety of symptoms, including cognition and communication problems, motor disorders, problems with impulse control and depression, confusion, and irritability. Chronic traumatic encephalopathy occurs in those with extraordinary exposure to multiple blows to the head and as a delayed consequence after many years. Studies of retired boxers have shown that repeated blows to the head can cause a number of issues, including memory problems, tremors, and lack of coordination and dementia. Recent studies have demonstrated rare cases of chronic traumatic encephalopathy in other sports with repetitive mild head impacts (e.g., soccer, wrestling, football, and rugby). A single, severe traumatic brain injury also may lead to a disorder called post-traumatic dementia, which may be progressive and share some features with chronic traumatic encephalopathy. Studies assessing patterns among large populations of people with traumatic brain injury indicate that moderate or severe traumatic brain injury in early or mid-life may be associated with increased risk of dementia later in life.
Other factors that influence recovery
Genes
Evidence suggests that genetics play a role in how quickly and completely a person recovers from a traumatic brain injury. For example, researchers have found that apolipoprotein E ε4 (ApoE4) — a genetic variant associated with higher risks for Alzheimer’s disease — is associated with worse health outcomes following a traumatic brain injury. Much work remains to be done to understand how genetic factors, as well as how specific types of head injuries in particular locations, affect recovery processes. It is hoped that this research will lead to new treatment strategies and improved outcomes for people with traumatic brain injury.
Age
Studies suggest that age and the number of head injuries a person has suffered over his or her lifetime are two critical factors that impact recovery. For example, traumatic brain injury-related brain swelling in children can be very different from the same condition in adults, even when the primary injuries are similar. Brain swelling in newborns, young infants, and teenagers often occurs much more quickly than it does in older individuals. Evidence from very limited chronic traumatic encephalopathy studies suggest that younger people (ages 20 to 40) tend to have behavioral and mood changes associated with chronic traumatic encephalopathy, while those who are older (ages 50+) have more cognitive difficulties.
Compared with younger adults with the same traumatic brain injury severity, older adults are likely to have less complete recovery. Older people also have more medical issues and are often taking multiple medications that may complicate treatment (e.g., blood-thinning agents when there is a risk of bleeding into the head). Further research is needed to determine if and how treatment strategies may need to be adjusted based on a person’s age.
Researchers are continuing to look for additional factors that may help predict a person’s course of recovery.
1. Rest
You should take it easy the first few days after the injury when symptoms are more severe.
- Early on, limit physical and thinking/remembering activities to avoid symptoms getting worse.
- Avoid activities that put you at risk for another injury to the head and brain.
- Get a good night’s sleep and take naps during the day as needed.
2. Light Activity
As you start to feel better, gradually return to regular (non-strenuous) activities.
- Find relaxing activities at home. Avoid activities that put you at risk for another injury to the head and brain.
- Return to work gradually. If symptoms do not worsen during an activity, then this activity is OK for you. If symptoms worsen, cut back on that activity until it is tolerated.
- Get maximum nighttime sleep. (Avoid screen time and loud music before bed, sleep in a dark room, and keep to a fixed bedtime and wake up schedule.)
- Reduce daytime naps or return to a regular daytime nap schedule.
3. Moderate Activity
When symptoms are mild and nearly gone, you can return to most regular activities.
- Take breaks only if concussion symptoms worsen.
- Return to a regular work schedule.
4. Back to Regular Activity
Recovery from a concussion is when you’re able to do all of your regular activities without experiencing any symptoms.
Also, be sure to:
- Schedule a follow up appointment for your doctor.
- Ask your doctor about safe over-the-counter or prescription medications to help with symptoms (e.g., Ibuprofen or acetaminophen for headache).
- Limit the number of soft drinks or caffeinated items to help you rest.
Post-Concussive Syndrome
While most people with a concussion feel better within a couple of weeks, some will have symptoms for months or longer. Talk with you health care provider if your concussion symptoms do not go away or if they get worse after they return to your regular activities.
If your concussion symptoms that last weeks to months after the injury, your medical provider may talk to you about post-concussive syndrome. While rare after only one concussion, post-concussive syndrome is believed to occur most commonly in patients with a history of multiple concussions.
There are many people who can help you and your family as you recover. You do not have to do it alone. Keep talking with your medical provider, family members, and loved ones about how you’re feeling. If you do not think you’re getting better, tell your medical provider.
What steps should I take to feel better?
Making short-term changes to your daily activities can help you get back to a regular routine more quickly. As you begin to feel better, you can slowly remove these changes. Use your symptoms to guide return to normal activities. If your symptoms do not worsen during an activity then this activity is OK for them. If symptoms worsen, you should cut back on how much you can do that activity without experiencing symptoms. It is important to remember that each concussion and each person is unique, so your recovery should be customized based on your symptoms.
Recovery Delays
Factors that might delay recovery include your child having:
- a history of a previous concussion or other brain injury,
- neurological or mental health disorders,
- learning difficulties, and/or
- family and social stressors.
Traumatic brain injury treatment
Traumatic brain injury treatment is based on the severity of the injury.
Mild traumatic brain injury
Mild traumatic brain injuries (concussions) usually require no treatment other than rest and over-the-counter pain relievers to treat a headache. However, a person with a mild traumatic brain injury usually needs to be monitored closely at home for any persistent, worsening or new symptoms. He or she may also have follow-up doctor appointments.
There is no clear timeline for a safe return to normal activities although there are guidelines such as those from:
- the American Academy of Neurology (https://www.aan.com/Guidelines/Home/GetGuidelineContent/586) and
- the American Medical Society for Sports Medicine (https://journals.lww.com/acsm-msse/Fulltext/2012/12000/The_Team_Physician_and_the_Return_to_Play.25.aspx) to help determine when athletes can return to practice or competition.
Further research is needed to better understand the effects of mild traumatic brain injury on the brain and to determine when it is safe to resume normal activities.
Your doctor will indicate when a return to work, school or recreational activities is appropriate. It’s best to limit physical or thinking (cognitive) activities that make things worse until your doctor advises that it’s OK. Most people return to normal routines gradually.
Even after symptoms resolve entirely, people should return to their daily activities gradually. Brain functionality may still be limited despite an absence of outward symptoms. Very little is known about the long-term effects of concussions on brain function.
Preventing future concussions is critical. While most people recover fully from a first concussion within a few weeks, the rate of recovery from a second or third concussion is generally slower.
In the days or weeks after a concussion, a minority of individuals may develop post-concussion syndrome. People can develop post-concussion syndrome even if they never lost consciousness. The symptoms include headache, fatigue, cognitive impairment, depression, irritability, dizziness and balance trouble, and apathy. These symptoms usually improve without medical treatment within one to a few weeks but some people can have longer lasting symptoms.
In some cases of moderate to severe traumatic brain injury, persistent symptoms may be related to conditions triggered by imbalances in the production of hormones required for the brain to function normally. Hormone imbalances can occur when certain glands in the body, such as the pituitary gland, are damaged over time as result of the brain injury. Symptoms of these hormonal imbalances include weight loss or gain, fatigue, dry skin, impotence, menstrual cycle changes, depression, difficulty concentrating, hair loss, or cold intolerance. When these symptoms persist 3 months after their initial injury or when they occur up to 3 years after the initial traumatic brain injury, people should speak with a health care provider about their condition.
Moderate to severe traumatic brain injuries
Emergency care for moderate to severe traumatic brain injuries focuses on making sure the person has enough oxygen and an adequate blood supply, maintaining blood pressure, and preventing any further injury to the head or neck.
People with severe injuries may also have other injuries that need to be addressed. Additional treatments in the emergency room or intensive care unit of a hospital will focus on minimizing secondary damage due to inflammation, bleeding or reduced oxygen supply to the brain.
Medications
Medications to limit secondary damage to the brain immediately after an injury may include:
- Diuretics. These drugs reduce the amount of fluid in tissues and increase urine output. Diuretics, given intravenously to people with traumatic brain injury, help reduce pressure inside the brain.
- Anti-seizure drugs. People who’ve had a moderate to severe traumatic brain injury are at risk of having seizures during the first week after their injury. An anti-seizure drug may be given during the first week to avoid any additional brain damage that might be caused by a seizure. Continued anti-seizure treatments are used only if seizures occur.
- Coma-inducing drugs. Doctors sometimes use drugs to put people into temporary comas because a comatose brain needs less oxygen to function. This is especially helpful if blood vessels, compressed by increased pressure in the brain, are unable to supply brain cells with normal amounts of nutrients and oxygen.
Surgery
Emergency surgery may be needed to minimize additional damage to brain tissues. Surgery may be used to address the following problems:
- Removing clotted blood (hematomas). Bleeding outside or within the brain can result in a collection of clotted blood (hematoma) that puts pressure on the brain and damages brain tissue.
- Repairing skull fractures. Surgery may be needed to repair severe skull fractures or to remove pieces of skull in the brain.
- Bleeding in the brain. Head injuries that cause bleeding in the brain may need surgery to stop the bleeding.
- Opening a window in the skull. Surgery may be used to relieve pressure inside the skull by draining accumulated cerebral spinal fluid or creating a window in the skull that provides more room for swollen tissues.
Rehabilitation
Most people who have had a significant brain injury will require rehabilitation. They may need to relearn basic skills, such as walking or talking. The goal is to improve their abilities to perform daily activities.
Therapy usually begins in the hospital and continues at an inpatient rehabilitation unit, a residential treatment facility or through outpatient services. The type and duration of rehabilitation is different for everyone, depending on the severity of the brain injury and what part of the brain was injured.
Rehabilitation specialists may include:
- Physiatrist, a doctor trained in physical medicine and rehabilitation, who oversees the entire rehabilitation process, manages medical rehabilitation problems and prescribes medication as needed
- Occupational therapist, who helps the person learn, relearn or improve skills to perform everyday activities
- Physical therapist, who helps with mobility and relearning movement patterns, balance and walking
- Speech and language pathologist, who helps the person improve communication skills and use assistive communication devices if necessary
- Neuropsychologist, who assesses cognitive impairment and performance, helps the person manage behaviors or learn coping strategies, and provides psychotherapy as needed for emotional and psychological well-being
- Social worker or case manager, who facilitates access to service agencies, assists with care decisions and planning, and facilitates communication among various professionals, care providers and family members
- Rehabilitation nurse, who provides ongoing rehabilitation care and services and who helps with discharge planning from the hospital or rehabilitation facility
- Traumatic brain injury nurse specialist, who helps coordinate care and educates the family about the injury and recovery process
- Recreational therapist, who assists with time management and leisure activities
- Vocational counselor, who assesses the ability to return to work and appropriate vocational opportunities and who provides resources for addressing common challenges in the workplace.
Coping and support
A number of strategies can help a person with traumatic brain injury cope with complications that affect everyday activities, communication and interpersonal relationships. Depending on the severity of injury, a family caregiver or friend may need to help implement the following approaches:
- Join a support group. Talk to your doctor or rehabilitation therapist about a support group that can help you talk about issues related to your injury, learn new coping strategies and get emotional support.
- Write things down. Keep a record of important events, people’s names, tasks or other things that are difficult to remember.
- Follow a routine. Keep a consistent schedule, keep things in designated places to avoid confusion and take the same routes when going to frequently visited destinations.
- Take breaks. Make arrangements at work or school to take breaks as needed.
- Alter work expectations or tasks. Appropriate changes at work or school may include having instructions read to you, allowing more time to complete tasks or breaking down tasks into smaller steps.
- Avoid distractions. Minimize distractions such as loud background noise from a television or radio.
- Stay focused. Work on one task at a time.
References [ + ]