The Ornish Diet
The Ornish Diet is also known as a Very-Low-Fat (VLF) diets that allow less than 15% of total calories from fat (with an equal distribution of saturated, monounsaturated, and polyunsaturated fats), 15% from protein, and 70% from carbohydrates. The Very-Low-Fat (VLF) diets are the main dietary factor in the Pritikin Diet as well. The Very-Low-Fat diet includes variations of vegetarian diets that may include eggs and dairy. Although an American Heart Association scientific statement concluded there were little long-term data to suggest that low-fat diets alone will sustain long-term weight loss, there is evidence that this diet can impact cardiovascular risk 1).
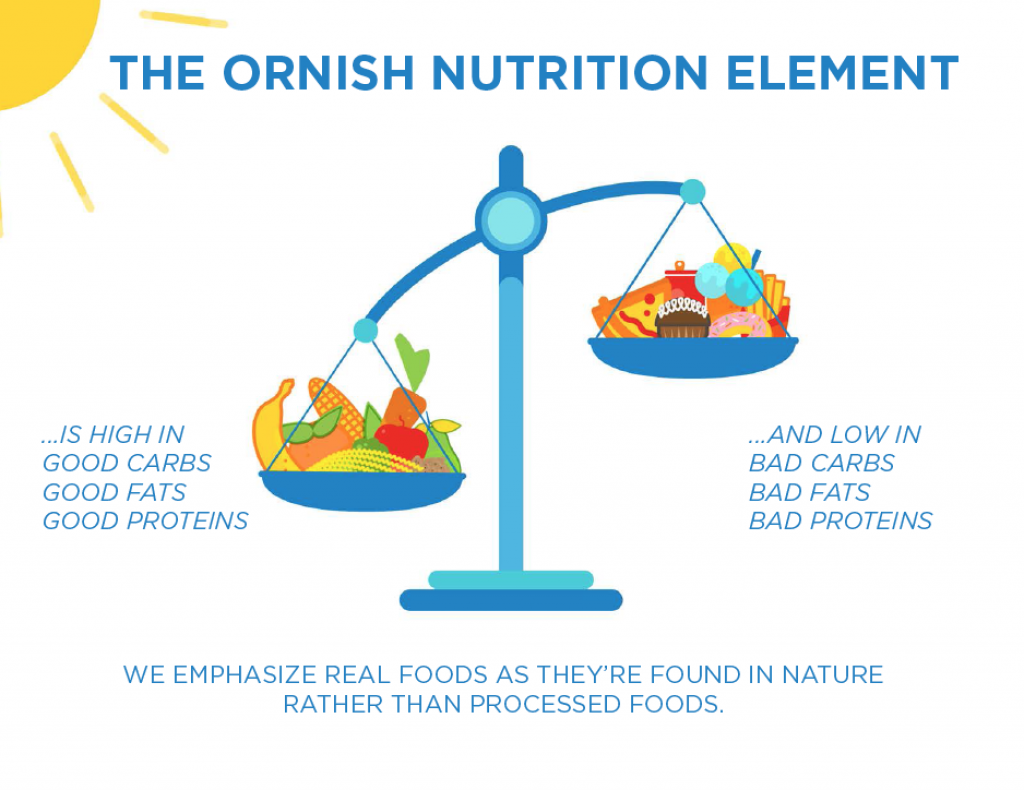
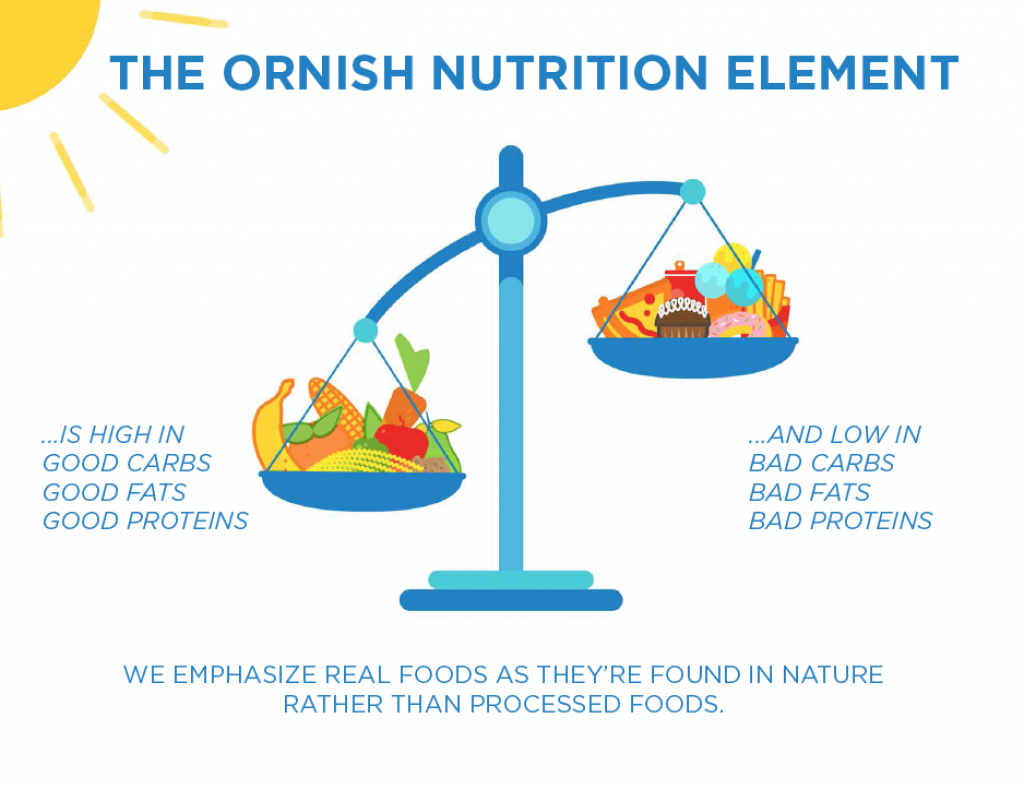
Dr. Ornish argues that protein and saturated fat increase the risk of mortality and chronic disease, therefore the fat content of your diet must be less than 10% fat with whole food and are plant-based. When comparing the Ornish diet with the highly processed, refined-carbohydrate-rich diet most Americans consume today it’s almost certainly healthier.
The problem with Ornish diet is it’s claimed that protein and fat are the cause of our health and weight problem today. Which is not true based on current large observational studies that have found that diets high in fat and protein are not associated with disease and may even protect against it. Nutrition is complex but there is little evidence the world’s obesity epidemic and worsening metabolic disorders are the fault of protein or fat. If anything, our attempts to eat less fat in recent decades have made things worse !
When people vigilantly cut down on fat in the 1980s and 1990s, they replaced much of it with high-sugar and high-calorie processed foods.
During the time in which the prevalence of obesity in the U.S. nearly tripled (1970 – 2017), the percentage of calories Americans consumed from protein and fat actually dropped whereas the percentage of calories Americans ingested from carbohydrates—one of the nutrient groups Ornish says we should eat more of—increased.
Could it be that our attempts to reduce fat have in fact been part of the problem ? Some scientists think so and we believe the low-fat message promoted the obesity epidemic.
Furthermore, another aspect of the Ornish diet—avoiding all added oils and even high-fat plant foods like avocados and nuts—isn’t necessarily helpful. There’s now lots of evidence that unsaturated fat lowers blood lipids such as cholesterol and reduces heart disease 2). What’s more, a low-fat diet is, by definition, a high-carbohydrate diet. These diets tend to promote the release of insulin, the hormone that regulates blood sugar levels. In people who aren’t very physically active, high insulin levels send a signal that it’s time to store fat, which can lead to weight gain.
The Ornish Lifestyle Heart Trial 3) randomized 48 patients with moderate to severe coronary heart disease (CHD) to intensive life-style changes or usual care. The intensive life-style changes included a vegetarian diet with 7% of caloric intake coming from fat, moderate aerobic exercise, stress management training, smoking cessation, and group psychosocial support. A total of 195 coronary artery lesions were analyzed angiographically. Overall, 82% of experimental group patients had an average change toward lesion regression. At five years, there were 2.5 times fewer cardiac events in the intervention group, and the average percent diameter stenosis showed an 8% decrease in diameter, whereas the control group had 28% progression. However, the data are difficult to interpret due to the confounding effects of exercise, stress reduction, and 11-kg weight loss in the intervention group. Although the intervention seems beneficial, the small sample size and intense life-style changes raise concerns about the universal sustainability of such a program.
The Very-Low-Fat Ornish diet and intense life-style changes have significant results in terms of reducing risk factors and cardiac event rates. However, these studies are relatively small, and the programs involved may be influenced by selection bias. The programs require a motivated group of patients to undergo rigorous life-style adjustments. The VLF Ornish diet may be unnecessary if other life-style characteristics like exercise, smoking cessation, and stress management are optimized 4).
The recent multicenter PREDIMED trial also supports the notion that fat can be good rather than bad. It found that individuals assigned to eat high-fat (41 percent calories from fat), Mediterranean-style diets for nearly five years were about 30 percent less likely to experience serious heart-related problems compared with individuals who were told to avoid fat. (All groups consumed about the same amount of protein.) Protein, too, doesn’t look so evil when one considers the 2010 trial published in The New England Journal of Medicine that found individuals who had recently lost weight were more likely to keep it off if they ate more protein, along with the 2005 OmniHeart trial that reported individuals who substituted either protein or monounsaturated fat for some of their carbohydrates reduced their cardiovascular risk factors compared with individuals who did not.
The other problem with Ornish’s antiprotein stance is that he lumps all animal proteins together. For instance, he wrote that animal proteins have been associated with higher disease and mortality risks. However that is only true if you combine processed meats like bacon, salami, pepperoni, hot dogs with unprocessed meats. A 2010 systematic review and meta-analysis of 20 studies found consumption of processed meat was associated with an increased risk of diabetes and heart disease but eating unprocessed red meat was not. A 2014 meta-analysis similarly reported much higher mortality risks associated with processed meat compared with red meat consumption and found no problems associated with white meat. And it is worth noting that among people in the study over 65, heavy consumption of animal protein actually protected against cancer and mortality. Also the heavy protein consumers in the study were consuming nearly 30 percent more protein than the average American does. So there’s little evidence to suggest that we need to avoid protein and fat.
The patients who followed the Ornish diet also quit smoking, started exercising and attended stress management training. The people in the control group were told to do none of these things. It’s hardly surprising that quitting smoking, exercising, reducing stress and dieting—when done together—improves heart health. But fact that the participants were making all of these lifestyle changes means that we cannot make any inferences about the effect of the Ornish diet alone.
Ornish Diet vs Zone Diet vs Atkins Diet vs LEARN Diet for Weight Loss
In a 2007 study 5), where researchers randomly assigned 311 individuals to four groups: one group was assigned the high-fat, high-protein and low-carbohydrate (Atkins diet); the second was assigned Ornish’s very low-fat vegetarian diet, which requires consuming fewer than 10 percent of calories from fat; the third was assigned the Zone diet, which aims for a 40/30/30 percent distribution of carbohydrate, protein and fat (macronutrient balance); and the fourth was assigned the high-carbohydrate, low–saturated fat LEARN (for: lifestyle, exercise, attitudes, relationships, nutrition) diet. Participants were randomly assigned to follow the Atkins (n = 77), Zone (n = 79), LEARN (n = 79), or Ornish (n = 76) diets and received weekly instruction for 2 months, then an additional 10-month follow-up. Weight loss at 12 months was the primary outcome. Secondary outcomes included lipid profile (low-density lipoprotein, high-density lipoprotein, and non–high-density lipoprotein cholesterol, and triglyceride levels), percentage of body fat, waist-hip ratio, fasting insulin and glucose levels, and blood pressure. Outcomes were assessed at months 0, 2, 6, and 12. The participants all had trouble adhering to their regimens, but all lost about the same statistically significant amounts of weight, and when compared head to head, the Atkins dieters saw greater improvements in blood pressure and HDL cholesterol than the Ornish dieters did.
Results 6): Weight loss was greater for women in the Atkins diet group compared with the other diet groups at 12 months, and mean 12-month weight loss was significantly different between the Atkins and Zone diets. Mean 12-month weight loss was as follows:
- Atkins, −4.7 kg ( −6.3 to −3.1 kg),
- Zone, −1.6 kg (−2.8 to −0.4 kg),
- LEARN, −2.6 kg (−3.8 to −1.3 kg), and
- Ornish, −2.2 kg (−3.6 to −0.8 kg).
- Weight loss was not statistically different among the Zone, LEARN, and Ornish groups.
- At 12 months, secondary outcomes for the Atkins group were comparable with or more favorable than the other diet groups.
Conclusions 7): In this study, premenopausal overweight and obese women assigned to follow the Atkins diet, which had the lowest carbohydrate intake, lost more weight and experienced more favorable overall metabolic effects at 12 months than women assigned to follow the Zone, Ornish, or LEARN diets. Average weight loss across all four groups ranged from 3.5 to 10.4 pounds. The authors note that “even modest reductions in excess weight have clinically significant effects on risk factors such as triglycerides and blood pressure.” While questions remain about long-term effects and mechanisms, a low-carbohydrate, high-protein, high-fat diet may be considered a feasible alternative recommendation for weight loss.
In another study published in the Journal of American Medical Association, where a total of 160 participants were randomly assigned to either Atkins (carbohydrate restriction), Zone , Weight Watchers (calorie restriction), or Ornish (fat restriction) diet groups. After 12 months of maximum effort, participants on the Atkins Diet which had the lowest carbohydrate intake, lost more weight at 12 months than participants assigned to follow the Zone diet, and had experienced comparable or more favorable metabolic effects than those assigned to the Zone, Weight Watchers or Ornish diets. Each diet significantly reduced the low-density lipoprotein/high-density lipoprotein (HDL) cholesterol ratio by approximately 10%, with no significant effects on blood pressure or glucose at 1 year. Each popular diet modestly reduced body weight and several cardiac risk factors at 1 year. The participants all had trouble adhering to their regimens, although increased adherence was associated with greater weight loss and cardiac risk factor reductions for each diet group. While questions remain about long-term effects and mechanisms, a low-carbohydrate, high-protein, high-fat diet may be considered a feasible alternative recommendation for weight loss.
References [ + ]