What is ACTH
ACTH is short for adrenocorticotropic hormone (ACTH) that is often called corticotropin, is an anterior pituitary hormone that stimulates the production of cortisol by the adrenal glands. Cortisol is a steroid hormone made by the adrenal glands (adrenal cortex) that is important for regulating glucose, protein, and lipid metabolism, suppressing the immune system’s response, and helping to maintain blood pressure.
ACTH is produced by the anterior pituitary gland. Located below the brain in the center of your head, the pituitary gland is part of the endocrine system, a network of glands that work together to produce hormones that act on organs, tissues, and other glands to regulate systems throughout the body.
Normally, ACTH levels increase when cortisol is low and fall when cortisol is high. In response to a fall in the blood cortisol level, the hypothalamus produces corticotropin-releasing hormone (CRH). This stimulates the production of ACTH by the anterior pituitary gland, which in turn stimulates the production of cortisol by the adrenal glands, small organs located at the top of each kidney. To make the appropriate amounts of cortisol, the hypothalamus, pituitary, and adrenal glands must be functioning properly.
- ACTH levels: < 10 pmol/L (dependent on time of collection) 1. ACTH levels can range between 7.2-63 pg/mL (a.m. draws) 2. No established reference values for p.m. draws.
- Plasma ACTH and cortisol levels exhibit peaks (6-8 a.m.) and troughs (11 p.m.).
- Pediatric reference values are the same as adults, as confirmed by peer reviewed literature 3.
Conditions that affect the hypothalamus, pituitary, or adrenal glands can interfere with regulating ACTH and cortisol production, increasing or decreasing how much of the hormones the glands produce. This can cause signs and symptoms associated with an excess or deficiency of cortisol. Conditions that affect ACTH include Cushing disease, Addison disease, and hypopituitarism. Some tumors found outside of the pituitary in locations such as the lungs can also increase cortisol concentrations by producing ACTH.
Disorders of cortisol production that might affect circulating ACTH concentrations include:
Hypercortisolism
- Cushing syndrome:
- Cushing disease (pituitary ACTH-producing tumor)
- Ectopic ACTH-producing tumor
- Ectopic corticotropin-releasing hormone (CRH)
- Adrenal cortisol-producing tumor
- Adrenal hyperplasia (non-ACTH dependent, autonomous cortisol-producing adrenal nodules)
Hypocortisolism
- Addison disease-primary adrenal insufficiency
- Secondary adrenal insufficiency
- Pituitary insufficiency
- Hypothalamic insufficiency
- Congenital adrenal hyperplasia-defects in enzymes involved in cortisol synthesis
Figure 1. ACTH and Cortisol production and control by the hypothalamus (the Hypothalamic-Pituitary-Adrenal axis)
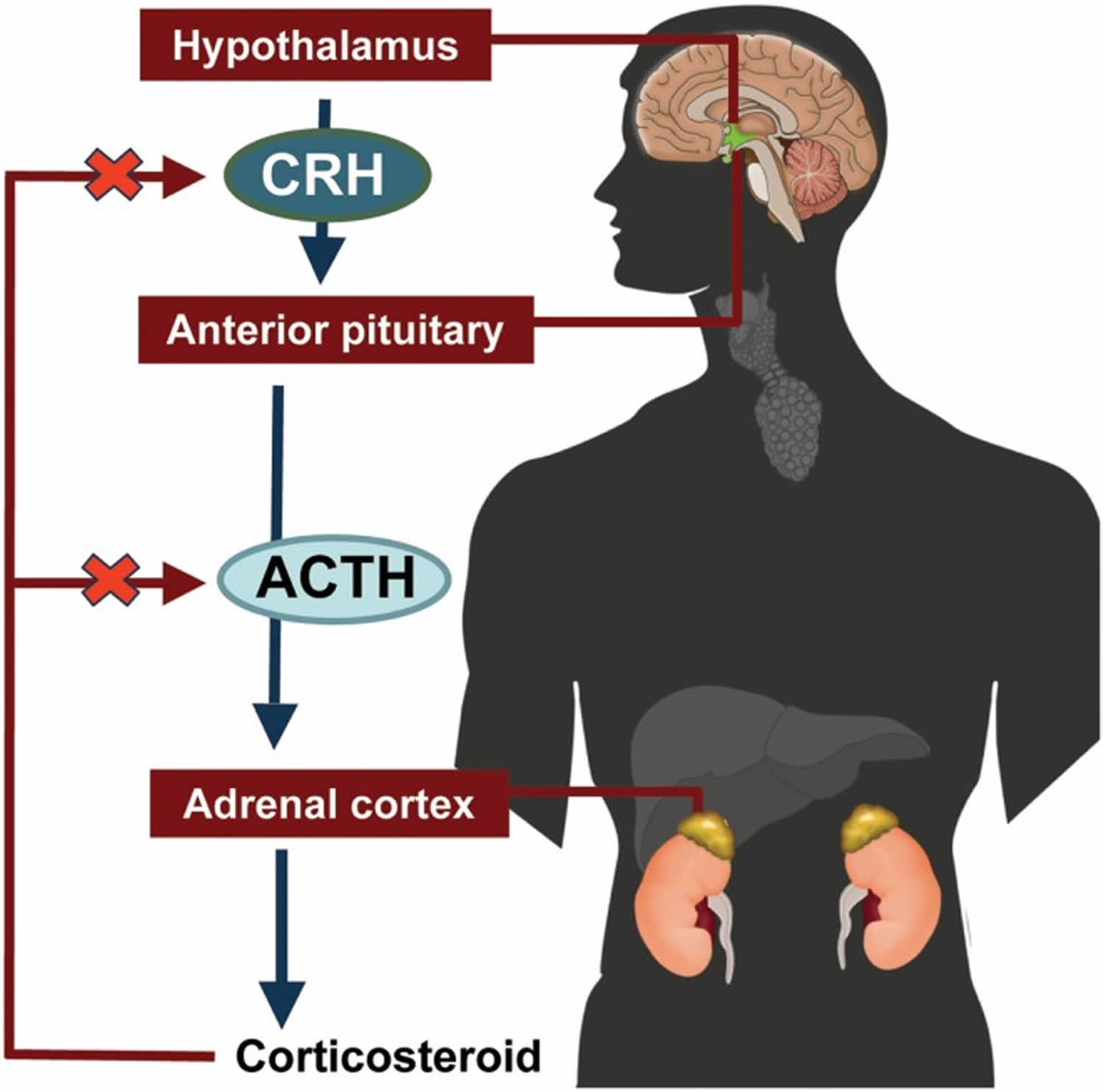 [Source 4]
[Source 4]
What is the difference between Cushing disease and Cushing syndrome?
Cushing disease is caused by a pituitary gland tumor (usually benign) that over-secretes the hormone ACTH, thus overstimulating the adrenal glands’ cortisol production. Cushing syndrome refers to the signs and symptoms associated with excess cortisol in the body, regardless of the cause. In addition to a pituitary tumor, taking steroid hormones (often used to treat cancer or autoimmune diseases), adrenal gland tumors, and ACTH-producing tumors outside the pituitary gland can cause Cushing syndrome.
ACTH deficiency
Addison’s disease
Addison’s disease develops when the outer layer of your adrenal glands (adrenal cortex) is damaged, reducing the levels of hormones (cortisol and often aldosterone) it produces.
In Addison’s disease, your adrenal glands produce too little cortisol and often insufficient levels of aldosterone as well.
Also called adrenal insufficiency, Addison’s disease occurs in all age groups and affects both sexes. Addison’s disease can be life-threatening.
Treatment for Addison’s disease involves taking hormones to replace the insufficient amounts being made by your adrenal glands, in order to mimic the beneficial effects produced by your naturally made hormones.
Addison’s disease symptoms
Addison’s disease symptoms usually develop slowly, often over several months, and may include:
- Extreme fatigue
- Weight loss and decreased appetite
- Darkening of your skin (hyperpigmentation)
- Low blood pressure, even fainting
- Salt craving
- Low blood sugar (hypoglycemia)
- Nausea, diarrhea or vomiting
- Abdominal pain
- Muscle or joint pains
- Irritability
- Depression
- Body hair loss or sexual dysfunction in women
Addisonian crisis: If you have untreated Addison’s disease, an addisonian crisis may be provoked by physical stress, such as an injury, infection or illness.
Acute adrenal failure (Addisonian crisis)
Sometimes, however, the signs and symptoms of Addison’s disease may appear suddenly. In acute adrenal failure (addisonian crisis), the signs and symptoms may also include:
- Pain in your lower back, abdomen or legs
- Severe vomiting and diarrhea, leading to dehydration
- Low blood pressure
- Loss of consciousness
- High potassium (hyperkalemia) and low sodium (hyponatremia)
When to see a doctor
See your doctor if you have signs and symptoms that commonly occur in people with Addison’s disease, such as:
- Darkening areas of skin (hyperpigmentation)
- Severe fatigue
- Unintentional weight loss
- Gastrointestinal problems, such as nausea, vomiting and abdominal pain
- Lightheadedness or fainting
- Salt cravings
- Muscle or joint pains
Your doctor can help determine whether Addison’s disease or some other medical condition may be causing these problems.
Addison’s disease causes
Addison’s disease results when your adrenal glands are damaged, producing insufficient amounts of the hormone cortisol and often aldosterone as well. Your adrenal glands are located just above your kidneys. As part of your endocrine system, they produce hormones that give instructions to virtually every organ and tissue in your body.
Your adrenal glands are composed of two sections. The interior (medulla) produces adrenaline-like hormones. The outer layer (cortex) produces a group of hormones called corticosteroids, which include glucocorticoids, mineralocorticoids and male sex hormones (androgens).
Some of the hormones the cortex produces are essential for life — the glucocorticoids and the mineralocorticoids.
- Glucocorticoids. These hormones, which include cortisol, influence your body’s ability to convert food fuels into energy, play a role in your immune system’s inflammatory response and help your body respond to stress.
- Mineralocorticoids. These hormones, which include aldosterone, maintain your body’s balance of sodium and potassium to keep your blood pressure normal.
- Androgens. These male sex hormones are produced in small amounts by the adrenal glands in both men and women. They cause sexual development in men, and influence muscle mass, libido and a sense of well-being in both men and women.
Primary adrenal insufficiency
Addison’s disease occurs when the cortex is damaged and doesn’t produce its hormones in adequate quantities. Doctors refer to the condition involving damage to the adrenal glands as primary adrenal insufficiency.
The failure of your adrenal glands to produce adrenocortical hormones is most commonly the result of the body attacking itself (autoimmune disease). For unknown reasons, your immune system views the adrenal cortex as foreign, something to attack and destroy.
A problem with the immune system is the most common cause of Addison’s disease in the US, accounting for 70% to 90% of cases.
The immune system is your body’s defence against infection and disease. If you’re ill, your immune system produces antibodies – a special type of protein that destroys disease-carrying organisms and toxins. These antibodies attack the cause of the illness.
However, if you develop a problem with your immune system, it can start to attack your own healthy tissues and organs. This is called an autoimmune disorder.
Addison’s disease can develop if your immune system attacks your adrenal glands and severely damages your adrenal cortex.
When 90% of the adrenal cortex is destroyed, your adrenal glands will not be able to produce enough of the steroid hormones cortisol and aldosterone. Once levels of these start decreasing, you’ll experience symptoms of Addison’s disease.
It’s not clear why some people develop this problem with their immune system, although it can run in families.
Genetics
Research has shown that some people with certain genes are more likely to develop autoimmune disorders.
It’s not clear how these genes lead to Addison’s disease and similar conditions, but it does mean your risk of developing Addison’s disease is increased if you or a close family member have another autoimmune condition, such as:
- vitiligo – a long-term condition that causes pale, white patches to develop on the skin
- type 1 diabetes – a long-term condition caused by your body not producing insulin
- underactive thyroid gland (hypothyroidism)
Other causes of adrenal gland failure may include:
- Tuberculosis (TB) is the most common cause of Addison’s disease worldwide, but it’s rare in the US. Tuberculosis (TB) is a bacterial infection that mostly affects the lungs but can also spread to other parts of your body. It can cause Addison’s disease if it damages your adrenal glands.
- Other infections of the adrenal glands such as those linked to AIDS, or fungal infections
- Spread of cancer to the adrenal glands.
- Bleeding into the adrenal glands, which may present as adrenal crisis without any preceding symptoms. Very heavy bleeding into the adrenal glands, sometimes associated with meningitis or other types of severe sepsis.
- Amyloidosis – a disease where amyloid, a protein produced by your bone marrow cells, builds up in and damages your adrenal glands
- Surgical removal of both adrenal glands (adrenalectomy) – for example, to remove a tumor
- Adrenoleukodystrophy – a rare, life-limiting inherited condition that affects the adrenal glands and nerve cells in the brain, and is mostly seen in young boys
- Certain treatments needed for Cushing’s syndrome – a collection of symptoms caused by very high levels of cortisol in the body
Secondary adrenal insufficiency
Adrenal insufficiency can also occur if your pituitary gland is diseased. The pituitary gland makes a hormone called adrenocorticotropic hormone (ACTH), which stimulates the adrenal cortex to produce its hormones. Inadequate production of ACTH can lead to insufficient production of hormones normally produced by your adrenal glands, even though your adrenal glands aren’t damaged. Secondary adrenal insufficiency can occur if your pituitary gland becomes damaged – for example, because of a tumour on the pituitary gland (pituitary adenoma). Doctors call this condition secondary adrenal insufficiency and is a separate condition to Addison’s disease.
Another more common cause of secondary adrenal insufficiency occurs when people who take corticosteroids for treatment of chronic conditions, such as asthma or arthritis, abruptly stop taking the corticosteroids.
Addison’s disease diagnosis
Your doctor will ask you about your medical history and your symptoms.
Your doctor also likely to ask if anyone in your family has an autoimmune disorder (a condition caused by a problem with their immune system).
Your doctor will examine your skin for any evidence of brownish discolouration (hyperpigmentation), particularly in certain areas, such as:
- the creases on your palm
- your elbow crease
- on any scars
- your lips and gums
However, hyperpigmentation does not occur in all cases of Addison’s disease.
You’ll also be tested for low blood pressure (hypotension) while you’re lying down and again shortly after you stand up. This is to see whether you have low blood pressure when you change position (postural or orthostatic hypotension).
Your doctor may also perform laboratory tests to determine whether you have Addison’s disease. Those lab tests include:
- Blood tests to measure your body’s hormone and mineral levels. Your doctor may check your blood before and after an injection to see if your body is responding normally to increased levels of certain hormones.
- Computerized tomography (CT) scan or magnetic resonance imaging (MRI) to look at the size of your adrenal glands or pituitary gland. These scans are similar to an X-ray.
Blood tests
If Addison’s disease is suspected, blood tests will be carried out to measure the levels of sodium, potassium and cortisol in your body. A low sodium, high potassium or low cortisol level may indicate Addison’s disease.
You may need to see a hospital hormone specialist (endocrinologist) for your blood to be tested for the following:
- a low level of the hormone aldosterone
- a high level of adrenocorticotrophic hormone (ACTH)
- a low level of glucose (sugar used for energy)
- positive adrenal antibodies (antibodies designed to attack the adrenal gland)
Any of the above could be a sign of Addison’s disease.
ACTH stimulation test
If cortisol in your blood is low or your symptoms strongly suggest Addison’s disease, you’ll need to have a ACTH stimulation test (synacthen stimulation test) to confirm the diagnosis.
Your doctor may refer you to an endocrinology unit (a unit that specializes in the study of hormones) for the test. How urgent the referral is will depend on how severe your symptoms are.
Synacthen is a man-made (synthetic) copy of the adrenocorticotrophic hormone (ACTH). ACTH is naturally produced by the pituitary gland (a pea-sized gland below the brain) to encourage the adrenal glands to release cortisol and aldosterone.
When synacthen is given, the adrenal glands should respond in the same way as they would to ACTH by releasing cortisol and other steroid hormones into the blood.
A blood sample will be taken and tested for cortisol before an injection of synacthen is given into your arm. Further blood samples will be taken to measure cortisol after 30 minutes and after 60 minutes.
If the ACTH level is high but the cortisol and aldosterone levels are low, it’s usually confirmation of Addison’s disease.
Thyroid function test
Your thyroid gland may also be tested to see if it’s working properly.
Your thyroid gland is found in your neck. It produces hormones that control your body’s growth and metabolism.
People with Addison’s disease often have an underactive thyroid gland (hypothyroidism), where the thyroid gland does not produce enough hormones.
By testing the levels of certain hormones in your blood, your endocrinologist (a specialist in hormone conditions) can determine whether you have hypothyroidism.
Scans
In some cases, your specialist may refer you for a scan of your adrenal glands – this could be a CT scan or an MRI scan.
Diagnosis during an adrenal crisis
If Addison’s disease is left untreated, it eventually leads to an adrenal crisis. This is where the symptoms of Addison’s disease appear quickly and severely.
During an adrenal crisis, there’s not enough time to perform a ACTH stimulation test (synacthen stimulation test) to confirm Addison’s disease.
If possible, blood will be taken and tested for any of the abnormalities listed above. While you’re waiting for the results, treatment may be started with steroid injections, and fluids containing salt and glucose.
Addison’s disease treatment
If you have Addison’s disease, you’ll need to take daily prescription hormones to replace the lost hormones. This can include hydrocortisone, prednisone, or cortisone acetate. If your body is not making enough of the hormone aldosterone, your doctor may prescribe fludrocortisone. These medicines are taken every day by mouth (in pill form). This should help you to live an active life, although many people find they still need to manage their fatigue.
Your doctor may also recommend that you take a medicine called dehydroepiandrosterone. Some women who have Addison’s disease find that taking this medicine improves their mood and sex drive.
If you are experiencing an Addisonian crisis, you need immediate medical care. The treatment typically consists of intravenous (IV) injections of hydrocortisone, saline (salt water), and dextrose (sugar). These injections help restore blood pressure, blood sugar, and potassium levels to normal.
In some cases, the underlying causes of Addison’s disease can be treated. For example, tuberculosis (TB) is treated with a course of antibiotics over a period of at least 6 months.
However, most cases are caused by a problem with the immune system that cannot be cured.
Adjusting your medication
At certain times, your medication may need to be adjusted to account for any additional strain on your body. For example, you may need to increase the dosage of your medication if you experience any of the following:
- an illness or infection – particularly if you have a high temperature of 38C or above
- an accident, such as a car crash
- an operation, dental or medical procedure – such as a tooth filling or endoscopy
- strenuous exercise that’s not usually part of your daily life
This will help your body cope with the additional stress. Your endocrinologist will monitor your dosage and advise about any changes.
Over time, as you get used to the condition and learn what can trigger your symptoms, you may learn how to adjust your medication yourself. However, always consult your doctor or specialist if you’re unsure.
Emergency treatment
You and a partner or family member may be trained to administer an injection of hydrocortisone in an emergency.
This could be necessary if you go into shock after an injury, or if you experience vomiting or diarrhea and are unable to keep down oral medication. This may occur if you’re pregnant and have morning sickness. Your endocrinologist will discuss with you when an injection might be necessary.
If you need to administer emergency hydrocortisone, always call your doctor immediately afterwards. Check what out-of-hours services are available in your local area, in case the emergency is outside normal working hours.
You can also register yourself with your local ambulance service, so they have a record of your requirement for a steroid injection or tablets, if you need their assistance.
Treating adrenal crisis
Adrenal crisis, or Addisonian crisis, needs urgent medical attention. Dial 999 for an ambulance if you or someone you know are experiencing adrenal crisis.
Signs of an adrenal crisis include:
- severe dehydration
- pale, cold, clammy skin
- sweating
- rapid, shallow breathing
- dizziness
- severe vomiting and diarrhea
- severe muscle weakness
- headache
- severe drowsiness or loss of consciousness
In hospital, you’ll be given lots of fluid through a vein in your arm to rehydrate you. This will contain a mixture of salts and sugars (sodium, glucose and dextrose) to replace what your body is lacking. You’ll also be injected with hydrocortisone to replace the missing cortisol hormone.
Any underlying causes of the adrenal crisis, such as an infection, will also be treated.
Living with Addison’s disease
Many people with Addison’s disease find that taking their medication enables them to continue with their normal diet and exercise routines.
However, bouts of fatigue are also common, and it can take some time to learn how to manage these periods of low energy.
Some people find that needing to take regular doses of medication is restrictive and affects their daily life or emotional health. Missing a dose of medication, or taking it late, can also lead to exhaustion or insomnia.
Some people can develop associated health conditions, such as diabetes or an underactive thyroid, which require extra treatment and management.
You’ll usually need to have appointments with an endocrinologist every 6 to 12 months so they can review your progress and adjust your medication dose, if necessary. Your doctor can provide support and repeat prescriptions in between these visits.
Failing to take your medication could lead to a serious condition called an adrenal crisis, so you must:
- remember to collect your repeat prescriptions
- keep spare medication as necessary – for example, in the car or at work, and always carry some spare medication with you
- take your medication every day at the right time
- pack extra medication if you’re going away – usually double what you would normally need, plus your injection kit
- carry your medication in your hand luggage if you are traveling by plane, with a note from your doctor explaining why it is necessary
You could also inform close friends or colleagues of your condition. Tell them about the signs of adrenal crisis and what they should do if you experience one.
Medical alert bracelets
It’s also a good idea to wear a medical alert bracelet or necklace that informs people you have Addison’s disease.
After a serious accident, such as a car crash, a healthy person produces more cortisol. This helps you cope with the stressful situation and additional strain on your body that results from serious injury. As your body cannot produce cortisol, you’ll need a hydrocortisone injection to replace it and prevent an adrenal crisis.
Wearing a medical alert bracelet will inform any medical staff treating you about your condition and what medication you require.
Medical alert bracelets or necklaces are pieces of jewellery engraved with your medical condition and an emergency contact number. They are available from a number of retailers.
ACTH test
This test measures the amount of ACTH in the blood. ACTH blood tests are used, usually in conjunction with cortisol tests, to help detect, diagnose, and monitor conditions associated with excessive or deficient cortisol in the body. These conditions include:
- Cushing disease: excess cortisol that is due to an ACTH-producing tumor in the pituitary gland (usually a benign tumor)
- Cushing syndrome: refers to the symptoms and signs associated with excess cortisol; in addition to Cushing disease, Cushing syndrome may be due to an adrenal tumor, adrenal hyperplasia, the use of steroid medications, or due to an ACTH-producing tumor located outside the pituitary (ectopic), such as in the lungs.
- Addison disease (primary adrenal insufficiency): decreased cortisol production due to adrenal gland damage
- Secondary adrenal insufficiency: decreased cortisol production because of pituitary dysfunction
- Hypopituitarism: pituitary dysfunction or damage that leads to decreased (or no) hormone production by the pituitary, including ACTH production
Measuring both ACTH and cortisol can help to differentiate among some of these conditions because the level of ACTH normally changes in the opposite direction to the level of cortisol.
If abnormal levels are detected, a healthcare practitioner will do additional testing to help confirm the findings and help determine the cause.
While ACTH is still used to diagnose adrenal insufficiency (Addison disease), the ACTH stimulation test is the preferred diagnostic test, when available.
Taking certain medications such as any steroid, oral, inhaled, topical or eye drop may cause abnormal results. Megestrol acetate can also cause abnormal results. Mifepristone (RU486) is a glucocorticoid receptor antagonist and, as such, likely causes changes to ACTH levels.
Stress may increase ACTH secretion.
ACTH has also been used therapeutically as a drug to treat multiple sclerosis and infantile spasms.
When is ACTH test ordered?
An ACTH test may be ordered after a cortisol test reveals abnormal results and when someone has signs or symptoms associated with excess or deficient cortisol.
Too much cortisol can cause symptoms that include:
- Obesity, with majority of the weight on the trunk of the body and not the arms and legs
- Fat collection between the shoulders
- Rounded, red face
- Fragile and thin skin
- Purple lines on the abdomen
- Muscle weakness
- Acne
- Skin infections
- Increased body hair
- Fatigue
These are often accompanied by findings such as high blood pressure, low potassium, high bicarbonate, high glucose levels, and sometimes diabetes.
People with insufficient cortisol production may exhibit symptoms such as:
- Muscle weakness
- Fatigue
- Weight loss
- Increased skin pigmentation, even in areas not exposed to the sun
- Loss of appetite
- Diarrhea, nausea and vomiting
- Dizziness
- Salt cravings
These are often accompanied by findings such as low blood pressure, low blood glucose, low sodium, high potassium, and high calcium.
Symptoms suggestive of hypopituitarism typically include several of the following:
- Loss of appetite
- Fatigue
- Irregular menstrual cycle
- Dysfunction of sex organs (hypogonadism)
- Decreased sex drive
- Frequent nighttime urination
- Unexplained weight loss
- Hot flashes
- Cold sensitivity
When the condition is due to a pituitary tumor (usually benign), the affected person may also have symptoms associated with the compression of nearby cells and nerves. For example, the tumor can cause a change in a pattern of headaches. It can also affect the nerves controlling vision, causing symptoms such as “tunnel vision” (inability to see things off to the side), loss of vision to some localized areas, or double vision.
How is ACTH test performed?
A blood sample is drawn by needle from a vein in the arm.
Is any test preparation needed to ensure the quality of the sample?
- Your healthcare provider may request that you fast overnight before testing. Blood is typically drawn in the morning, about 8 a.m.
Specimen Required
Patient Preparation: For 12 hours before this test do not take multivitamins or dietary supplements containing biotin (vitamin B7), which is commonly found in hair, skin, and nail supplements and multivitamins.
Specimen Volume: 1 mL
Collection Instructions:
- Morning (6 a.m.-10:30 a.m.) specimen is desirable.
- Collect with a pre-chilled EDTA tube and transport to the laboratory on ice.
- Spin down in a refrigerated centrifuge within 2 hours and immediately separate plasma from cells.
- Immediately freeze plasma.
Additional Information:
- Separate specimens should be submitted when multiple tests are ordered.
What does abnormal ACTH test result mean?
In many cases, the interpretation of the results can be complex. Levels of both ACTH and cortisol vary throughout the day. Normally, ACTH will be at its highest level in the morning and lowest at night. It will stimulate cortisol production, which will follow the same daily pattern but will rise after ACTH does and fall to its lowest level very late in the evening. Conditions that affect the production of ACTH and cortisol often disrupt this diurnal variation.
- ACTH levels: < 10 pmol/L (dependent on time of collection). ACTH levels can range between 7.2-63 pg/mL (a.m. draws). No established reference values for p.m. draws.
- Plasma ACTH and cortisol levels exhibit peaks (6-8 a.m.) and troughs (11 p.m.).
- Pediatric reference values are the same as adults, as confirmed by peer reviewed literature.
Results of ACTH and cortisol tests are often evaluated together. The table below indicates the common patterns of ACTH and cortisol seen with different diseases involving the adrenal and pituitary glands.
| Disease | Cortisol | ACTH |
|---|---|---|
| Cushing disease (pituitary tumor producing ACTH) | Increased | Increased |
| Adrenal tumor | Increased | Decreased |
| “Ectopic” ACTH (ACTH made by a tumor outside the pituitary, usually in the lung) | Increased | Increased |
| Addison disease (underactive or damaged adrenal glands) | Decreased | Increased |
| Hypopituitarism | Decreased | Decreased or normal |
An increased ACTH result can mean that a person has Cushing disease, Addison disease, overactive, tumor-forming endocrine glands (multiple endocrine neoplasia), or ectopic ACTH-producing tumors.
A decreased ACTH result can be due to an adrenal tumor, steroid medication, or hypopituitarism.
It is impossible to reliably distinguish Cushing disease and ectopic ACTH from cortisol and ACTH measurement alone. A variety of other tests are often used to assist healthcare practitioners in making this distinction. Testing the change in the level of cortisol when certain drugs are given to stimulate or suppress hormone production often helps the healthcare practitioner make the right diagnosis.
Interpretation of abnormal ACTH results
ACTH concentrations vary considerably depending on physiological conditions. Therefore, ACTH results should always be evaluated with simultaneously measured cortisol concentrations.
- In a patient with hypocortisolism (low cortisol), an elevated adrenocorticotropic hormone (ACTH) indicates primary adrenal insufficiency, whereas a value that is not elevated is consistent with secondary adrenal insufficiency from a pituitary or hypothalamic cause.
- In a patient with hypercortisolism (Cushing syndrome), a suppressed value is consistent with a cortisol-producing adrenal adenoma or carcinoma, primary adrenal micronodular hyperplasia, or exogenous corticosteroid use.
- Normal or elevated ACTH in a patient with Cushing syndrome puts the patient in the ACTH-dependent Cushing syndrome category. This is due to either an ACTH-producing pituitary adenoma or ectopic production of ACTH (bronchial carcinoid, small cell lung cancer, others). Further diagnostic studies such as dexamethasone suppression testing, corticotropin-releasing hormone stimulation testing, petrosal sinus sampling, and imaging studies are usually necessary to define the ACTH source.
Cautions
In very rare instances of the ectopic adrenocorticotropic hormone (ACTH) syndrome, the elevated ACTH may be biologically active but not detected by the immunometric assay.
Samples should not be taken from patients receiving therapy with high biotin or vitamin B7 doses (ie, >5 mg/day) until at least 12 hours following the last biotin administration.
Falsely elevated values may occur in plasma from patients who have developed human antimouse antibodies or heterophilic antibodies.
In rare cases, interference due to extremely high titers of antibodies to analyte-specific antibodies, streptavidin, or ruthenium can occur.
Under ACTH 1-24 medication, ACTH measurement is not recommended, due to negative interference with the sandwich assay.
Patients taking glucocorticoids may have suppressed levels of ACTH with an apparent high level of cortisol. This may be due to cross-reactivity with the cortisol immunoassays. If exogenous Cushing is suspected, a cortisol level determined by liquid chromatography-tandem mass spectrometry (LC-MS/MS) (eg, CINP / Cortisol, Serum, LC-MS/MS) should be used with the ACTH level for the interpretation.
Values obtained with different assay methods or kits may be different and cannot be used interchangeably. Test results cannot be interpreted as absolute evidence for the presence or absence of malignant disease.
ACTH stimulation test
ACTH stimulation test or Synacthen stimulation test or Cosyntropin stimulation test or Cortrosyn stimulation test, is the optimal test for diagnosing primary adrenal insufficiency or Addison’s disease, according to guidelines from the Endocrine Society. ACTH (cosyntropin) stimulation test measures how well the adrenal glands respond to the hormone ACTH. ACTH is a hormone produced in the pituitary gland that stimulates the adrenal glands to release cortisol. ACTH stimulation test involves measuring the level of cortisol in a person’s blood before and after an injection of synthetic ACTH. If the adrenal glands are functional, cortisol blood levels will rise in response to the ACTH stimulation. If they are damaged or non-functional, then their response to ACTH will be minimal. This rapid screening test may be ordered along with a baseline ACTH test and, if abnormal, may be followed with a 1 to 3 day prolonged ACTH stimulation test to help differentiate between primary and secondary adrenal insufficiency.
ACTH stimulation test preparation
Do not eat, chew gum, or drink anything except for water after midnight the night before the test. Your health care provider will tell you if you should stop taking any medications before the test and will give you information about the test.
ACTH stimulation test procedure
Your health care provider will insert a small tube into a vein (IV) in your arm an hour before the test starts. Using an IV catheter avoids repeated needle sticks. The corticotropin-releasing hormone (CRH) will be given through the catheter.
Once the corticotropin-releasing hormone (CRH) is given, it travels through the bloodstream and causes the pituitary gland to secrete another hormone, adrenocorticotropic hormone (ACTH). The ACTH then travels to the adrenal glands and causes them to release cortisol. During the test, blood samples will be taken at specific times to measure changes in cortisol levels over time.
Just after the corticotropin-releasing hormone (CRH) is given, you may feel a sensation of warmth that can last for up to 30 minutes. You may have a metallic taste in your mouth which can last for some time and then go away. There are no known delayed or long-lasting side effects from corticotropin-releasing hormone (CRH).
The ACTH stimulation test will last about an hour.
Along with the blood tests, sometimes you may also have a urinary free cortisol test or urinary 17-ketosteroids test in which the urine is collected over a 24-hour period.
After the procedure
Most likely, your health care provider will remove the IV after the last blood draw. Once the test is completed, you may then eat and resume your usual activities.
If you have questions about this test, please ask. Your nurse and doctor are ready to assist you at all times.
ACTH stimulation test results interpretation
Normal Results
An increase in cortisol after stimulation by ACTH is normal. Blood cortisol after ACTH stimulation should be greater than 18 – 20 mcg/dL, depending on the dose of cosyntropin used.
Note: mcg/dL = micrograms per deciliter
The examples above are common measurements for results for these tests. Normal value ranges may vary slightly among different laboratories. Some labs use different measurements or may test different specimens.Talk to your doctor about the meaning of your specific test results.
What Abnormal Results Mean
ACTH stimulation test is helpful in determining if you have:
- Acute adrenal crisis
- Addison’s disease, when the adrenal glands do not produce enough cortisol
- Low pituitary function
- Pituitary tumors
- ACTH. Findling JW, Raff H. Endocrinol Metab Clin North Am 2001; 30: 729-747.[↩]
- Demers LM: In Tietz Textbook of Clinical Chemistry and Molecular Diagnostics, 2006; pp 2014-2027[↩]
- Petersen KE: ACTH in normal children and children with pituitary and adrenal diseases. I. Measurement in plasma by radioimmunoassay-basal values. Acta Paediatr Scand 1981;70:341-345[↩]
- Ross AP, Ben-Zacharia A, Harris C, Smrtka J. Multiple Sclerosis, Relapses, and the Mechanism of Action of Adrenocorticotropic Hormone. Frontiers in Neurology. 2013;4:21. doi:10.3389/fneur.2013.00021. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3591751/[↩]




