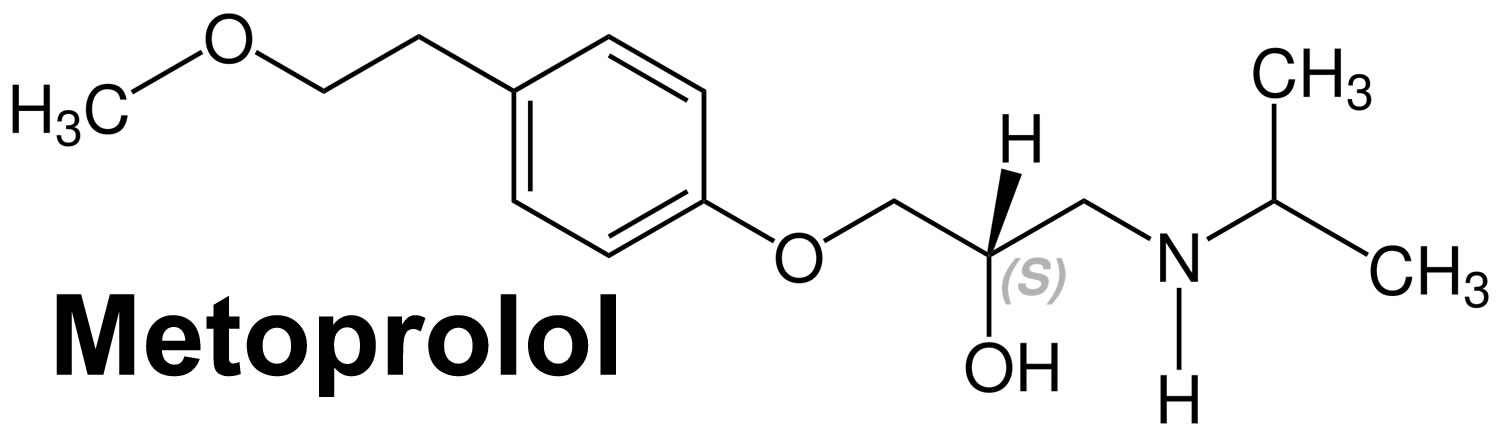
What is metoprolol
Metoprolol is used alone or in combination with other medications to treat high blood pressure (hypertension). Metoprolol also is used to prevent angina (chest pain) and to improve survival after a heart attack. Metoprolol also is used in combination with other medications to treat heart failure. Metoprolol is in a class of medications called beta blockers. It works by relaxing blood vessels and slowing heart rate to improve blood flow and decrease blood pressure.
Metoprolol comes as tablets and is only available on prescription. It’s also given by injection, but this is usually done in hospital.
Take metoprolol even if you feel well, as you will still be getting the benefits of the medicine.
High blood pressure is a common condition and when not treated, can cause damage to the brain, heart, blood vessels, kidneys and other parts of the body. Damage to these organs may cause heart disease, a heart attack, heart failure, stroke, kidney failure, loss of vision, and other problems. In addition to taking medication, making lifestyle changes will also help to control your blood pressure. These changes include eating a diet that is low in fat and salt, maintaining a healthy weight, exercising at least 30 minutes most days, not smoking, and using alcohol in moderation.
Do not stop taking metoprolol without talking to your doctor. Suddenly stopping metoprolol may cause chest pain or heart attack. Your doctor will probably decrease your dose gradually.
Key facts
- Metoprolol treats high blood pressure
- Metoprolol treats illnesses that cause an irregular heartbeat
- Metoprolol prevenst future heart disease, heart attacks and strokes
- Metoprolol prevents chest pain caused by angina
- Metoprolol prevents migraines
- Metoprolol slows down your heart rate and makes it easier for your heart to pump blood around your body.
- Your very first dose of metoprolol may make you feel dizzy, so take it at bedtime. After that, if you don’t feel dizzy, you can take it in the morning.
- Metoprolol is usually taken once or twice a day – but sometimes it’s prescribed to be taken up to 4 times a day.
- The main side effects of metoprolol are headaches, and feeling dizzy, sick or tired – these are usually mild and short-lived.
- Metoprolol also goes by the brand name Toprol, Toprol XL and Lopresor. When given by injection, it may be called by the brand name Betaloc.
How does metoprolol work?
Metoprolol is a type of medicine called a beta blocker.
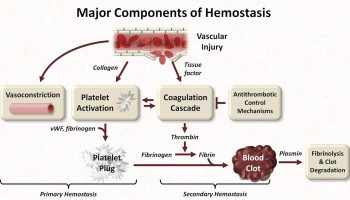
Like other beta blockers, metoprolol works by changing the way your body responds to some nerve impulses, especially in the heart. It slows down your heart rate and makes it easier for your heart to pump blood around your body.
How does it compare with other heart medicines?
Metoprolol works as well as other beta blockers for reducing blood pressure but is less likely to cause side effects. That’s because metoprolol works mainly on the heart. Other beta blockers, such as propranolol, work on the heart but affect other parts of the body as well.
There are lots of other medicines to lower blood pressure and treat chest pain that work in a different way to beta blockers. They include:
- angiotensin-converting enzyme (ACE) inhibitors – for example, ramipril and lisinopril
- angiotensin receptor blockers – for example, candesartan
- calcium channel blockers – for example, amlodipine
- diuretics (tablets that make you pee more) – for example, furosemide
Beta blockers aren’t usually the first-choice treatment for high blood pressure. The medicine your doctor prescribes depends on your age and ethnicity.
- if you’re under 55, you’ll usually be offered an ACE inhibitor or an angiotensin receptor blocker
- if you’re 55 or older, or you’re any age and of black African or Caribbean origin, you’ll usually be offered a calcium channel blocker
Sometimes you may have to try other blood-pressure-lowering medicines if you get side effects. Many people need to take a combination of different tablets.
How long does it take to work?
Metoprolol starts to work after about 2 hours, but it can take up to 1 week to fully take effect.
You may not feel any different when you take metoprolol, but this doesn’t mean it’s not working. It’s important to keep taking your medicine.
Can lifestyle changes help?
You can boost the health of your heart by making some key lifestyle changes.
- Stop smoking – smoking increases your heart rate and blood pressure. Quitting smoking brings down your blood pressure and relieves heart failure symptoms. Try to avoid secondhand smoke.
- Drink alcohol sensibly – drinking too much alcohol raises blood pressure over time. It makes heart failure worse too. Men and women shouldn’t drink more than 14 units of alcohol a week.
- Be more active – regular exercise lowers blood pressure by keeping your heart and blood vessels in good condition. It doesn’t need to be too energetic – walking every day will help.
- Eat healthily – aim to eat a diet that includes plenty of fruit and veg, wholegrains, fat-free or low-fat dairy products, and lean proteins. It’s a good idea to cut down on salt too. Eating too much salt is the biggest cause of high blood pressure – the more salt you eat, the higher your blood pressure will be. Aim for no more than 6g of salt a day.
- Manage stress – when you’re anxious or upset, your heart beats faster, you breathe more heavily and your blood pressure often goes up. Find ways to reduce stress in your life. To give your heart a rest, try napping or putting your feet up when possible. Spend time with friends and family to be social and help avoid stress.
How long will I take it for?
Treatment with metoprolol is usually long term, possibly even lifelong.
Is it safe to take for a long time?
Metoprolol is generally safe to take for a long time. In fact, it works best when you take it for a long time.
What will happen if I stop taking it?
Stopping metoprolol suddenly can make your condition worse.
Talk to your doctor if you want to stop taking metoprolol. If you’re bothered by side effects, your doctor may be able to prescribe a different medicine for your heart problems.
If you stop taking metoprolol, it will take 1 day for it to be completely out of your body.
Will I need to stop metoprolol before surgery?
Tell your doctor you’re taking metoprolol if you’re going to be put to sleep (using general anaesthetic) or have any kind of major operation.
Your doctor may advise you to stop taking metoprolol 24 hours before surgery. This is because metoprolol can lower your blood pressure too much when it’s combined with some anaesthetics.
Is there any food or drink I need to avoid?
You can eat and drink normally while taking metoprolol.
Eating a healthy, balanced diet can help if you have high blood pressure or a heart problem.
Can I drink alcohol with metoprolol?
Drinking alcohol can increase the risk of side effects with metoprolol. It can make you feel dizzy or lightheaded.
During the first few days of taking metoprolol, or after an increase in your dose, it’s best to stop drinking alcohol until you see how the medicine affects you.
It’s best to stop drinking alcohol if you find metoprolol makes you feel dizzy.
Will metoprolol affect my contraception?
Metoprolol won’t stop your contraception working.
However, some types of hormonal methods of contraception, such as the combined contraceptive pill and contraceptive patch, aren’t usually recommended for women with high blood pressure. Talk to your doctor if you’re taking a combined hormonal contraceptive.
Does metoprolol affect fertility in men or women?
It’s unlikely that metoprolol affects fertility in men or women. However, there’s not enough evidence to say for certain.
If you’re trying for a baby or are having problems getting pregnant while on metoprolol, speak to your doctor.
Will metoprolol affect my sex life?
Some people on metoprolol say their sex drive goes down or they can’t get an erection. However, this isn’t a common side effect and there’s not enough evidence to say for sure that metoprolol causes it.
If you’re having problems with your sex life, talk to your doctor.
Do I need to avoid playing sports?
You don’t need to stop playing sports if you take metoprolol, but don’t push yourself too much.
Regular exercise is good for you because it lowers blood pressure by keeping your heart and blood vessels in good condition. But be aware that metoprolol is not allowed in some sports if you’re competing at a high level.
Can I drive or ride a bike?
Metoprolol can make some people feel dizzy, especially when you first start taking it or after taking a bigger dose. If this happens to you, don’t drive a car, ride a bike, or use tools or machinery.
What does metoprolol do?
Metoprolol is a cardioselective competitive adrenergic beta-1 adrenergic receptor blocking agent that is commonly used to treat chest pain (angina pectoris), hypertension (high blood pressure) and heart arrhythmias. Metoprolol antagonizes beta 1-adrenergic receptors in the myocardium (heart muscle), thereby reducing the rate and force of myocardial contraction, and consequently a diminished cardiac output. Metoprolol may also reduce the secretion of renin with subsequent reduction in levels of angiotensin II thus decreasing sympathetic activation, including vasoconstriction, aldosterone secretion.
How should metoprolol be used?
Metoprolol comes as a tablet and an extended-release (long-acting) tablet to take by mouth. The regular tablet is usually taken once or twice a day with meals or immediately after meals. The extended-release tablet is usually taken once a day. To help you remember to take metoprolol, take it around the same time(s) every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take metoprolol exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
The extended-release tablet may be split. Swallow the whole or half tablets whole; do not chew or crush them.
Your doctor may start you on a low dose of metoprolol and gradually increase your dose.
Metoprolol controls high blood pressure and angina but does not cure them. Metoprolol extended-release tablets control heart failure but does not cure it. It may take a few weeks before you feel the full benefit of metoprolol. Continue to take metoprolol even if you feel well.
- You can take metoprolol with or without food, but it’s best to do the same each day.
- Swallow the tablets whole with a drink of water. Some brands have a score line to help you break the tablet and make it easier to swallow. Check the information leaflet for your brand to see if you can do this.
Who can and can’t take metoprolol
Metoprolol can be taken by adults over the age of 18.
Metoprolol isn’t suitable for everyone. To make sure it’s safe for you, tell your doctor before starting metoprolol if you have:
- had an allergic reaction to metoprolol or any other medicine in the past
- low blood pressure or a slow heart rate
- a lung disease or severe asthma
- metabolic acidosis – when there is too much acid in your blood
- an overactive thyroid (hyperthyroidism) – metoprolol may make it more difficult to recognise the warning signs of having too much thyroid hormone in your body (thyrotoxicosis)
- severe blood circulation problems in your limbs (such as Raynaud’s phenomenon), which may make your fingers and toes tingle or turn pale or blue
- liver problems
Pregnancy and breastfeeding
Metoprolol isn’t usually recommended in pregnancy.
If you’re trying to get pregnant or already are pregnant, talk to your doctor about the benefits and possible harms of taking metoprolol.
Your doctor may recommend another medicine, such as labetalol. It’s similar to metoprolol and is often prescribed for high blood pressure in pregnancy.
Metoprolol and breastfeeding
It is usually safe to take metoprolol if you’re breastfeeding. This is because only a small amount gets into breast milk, and it’s not enough to cause any problems to your baby.
However, speak to your doctor before taking metoprolol if your baby is premature or has kidney problems.
Metoprolol special precautions
Before taking metoprolol:
- tell your doctor and pharmacist if you are allergic to metoprolol, acebutolol (Sectral), atenolol (Tenormin, in Tenoretic), betaxolol, bisoprolol (Zebeta, in Ziac), carvedilol (Coreg, Coreg CR), esmolol (Brevibloc), labetalol, nadolol (Corgard, in Corzide), pindolol, propranolol (Inderal, Inderal LA, Innopran XL, in Inderide), sotalol (Betapace, Betapace AF, Sorine), timolol, any other medications, or any of the ingredients in metoprolol tablets. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: bupropion (Aplenzin, Forfivo, Wellbutrin, Zyban), cimetidine, clonidine (Catapres), diphenhydramine (Benadryl), fluoxetine (Prozac, Sarafem, Selfemra, in Symbyax), hydroxychloroquine, paroxetine (Brisdelle, Paxil, Pexeva), propafenone (Rythmol), quinidine, ranitidine (Zantac), reserpine, ritonavir (Norvir, in Kaletra), terbinafine (Lamisil), and thioridazine. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have a slow heart rate, heart failure, problems with blood circulation, or pheochromocytoma (a tumor that develops on a gland near the kidneys and may cause high blood pressure and fast heartbeat). Your doctor may tell you not to take metoprolol.
- tell your doctor if you have or have ever had asthma or other lung diseases; heart or liver disease; diabetes; severe allergies; or hyperthyroidism (an overactive thyroid gland).
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking metoprolol, call your doctor.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking metoprolol.
- you should know that metoprolol may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
- remember that alcohol can add to the drowsiness caused by this medication.
- you should know that if you have allergic reactions to different substances, your reactions may be worse while you are using metoprolol, and your allergic reactions may not respond to the usual doses of injectable epinephrine.
Cautions with other medicines
There are some medicines that may interfere with the way metoprolol works.
Tell your doctor if you’re taking:
- other medicines for high blood pressure – the combination with metoprolol can sometimes lower your blood pressure too much, which may make you feel dizzy or faint; tell your doctor if this keeps happening as they may change your dose
- other medicines that can lower your blood pressure – these include some antidepressants, nitrates (for chest pain), baclofen (a muscle relaxant), tamsulosin (for an enlarged prostate), and co-careldopa and levodopa (for Parkinson’s disease)
- non-steroidal anti-inflammatory medicines (NSAIDs), such as ibuprofen – these medicines may increase your blood pressure, so it’s best to keep them to a minimum
- cough medicines that contain pseudoephedrine or xylometazoline
- medicines for diabetes – metoprolol may make it more difficult to recognise the warning signs of low blood sugar
- medicines for allergies – such as ephedrine, noradrenaline or adrenaline
- medicines for asthma or chronic obstructive pulmonary disease (COPD)
Mixing metoprolol with herbal remedies or supplements
There’s very little information about taking herbal remedies and supplements with metoprolol.
For safety, tell your doctor or pharmacist if you’re taking any other medicines, including herbal medicines, vitamins or supplements.
Metoprolol uses
Metoprolol is commonly used to treat chest pain (angina pectoris) and hypertension (high blood pressure).
Metoprolol is also used sometimes to prevent migraine headaches and to treat irregular heartbeat (heart arrhythmias) and movement disorders caused by medications for mental illness. Talk to your doctor about the possible risks of using this medication for your condition.
Metoprolol can help reduce your symptoms if you have too much thyroid hormone in your body (thyrotoxicosis or hyperthyroidism). You’ll usually take it together with medicines to treat an overactive thyroid.
Metoprolol may be prescribed for other uses; ask your doctor or pharmacist for more information.
Metoprolol contraindications
- Metoprolol is contraindicated in sinus bradycardia, heart block greater than first degree, cardiogenic shock, and overt cardiac failure.
- Hypersensitivity to metoprolol and related derivatives, or to any of the excipients; hypersensitivity to other beta-blockers (cross sensitivity between beta-blockers can occur).
- Sick-sinus syndrome.
- Severe peripheral arterial circulatory disorders.
- Metoprolol is contraindicated in patients with a heart rate < 45 beats/min; second- and third-degree heart block; significant first-degree heart block (P-R interval ≥ 0.24 sec); systolic blood pressure < 100 mmHg; or moderate-to-severe cardiac failure.
Warnings
Heart Failure
Beta blockers, like metoprolol, can cause depression of myocardial contractility and may precipitate heart failure and cardiogenic shock. If signs or symptoms of heart failure develop, treat the patient according to recommended guidelines. It may be necessary to lower the dose of metoprolol or to discontinue it.
Ischemic Heart Disease
Do not abruptly discontinue metoprolol therapy in patients with coronary artery disease. Severe exacerbation of angina, myocardial infarction and ventricular arrhythmias have been reported in patients with coronary artery disease following the abrupt discontinuation of therapy with beta-blockers. When discontinuing chronically administered metoprolol, particularly in patients with coronary artery disease, the dosage should be gradually reduced over a period of 1 to 2 weeks and the patient should be carefully monitored. If angina markedly worsens or acute coronary insufficiency develops, metoprolol administration should be reinstated promptly, at least temporarily, and other measures appropriate for the management of unstable angina should be taken. Patients should be warned against interruption or discontinuation of therapy without the physician’s advice. Because coronary artery disease is common and may be unrecognized, it may be prudent not to discontinue metoprolol therapy abruptly even in patients treated only for hypertension.
Use During Major Surgery
Chronically administered beta-blocking therapy should not be routinely withdrawn prior to major surgery; however, the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
Bradycardia
Bradycardia, including sinus pause, heart block, and cardiac arrest have occurred with the use of metoprolol. Patients with first-degree atrioventricular block, sinus node dysfunction, or conduction disorders may be at increased risk. Monitor heart rate and rhythm in patients receiving metoprolol. If severe bradycardia develops, reduce or stop metoprolol.
Exacerbation of Bronchospastic Disease
Patients with bronchospastic disease, should, in general, not receive beta blockers, including metoprolol. Because of its relative beta1 selectivity, however, metoprolol may be used in patients with bronchospastic disease who do not respond to, or cannot tolerate, other antihypertensive treatment. Because beta1 selectivity is not absolute use the lowest possible dose of metoprolol and consider administering metoprolol in smaller doses three times daily, instead of larger doses two times daily, to avoid the higher plasma levels associated with the longer dosing interval. Bronchodilators, including beta-2 agonists, should be readily available or administered concomitantly.
Diabetes and Hypoglycemia
Beta-blockers may mask tachycardia occurring with hypoglycemia, but other manifestations such as dizziness and sweating may not be significantly affected.
Pheochromocytoma
If metoprolol is used in the setting of pheochromocytoma, it should be given in combination with an alpha blocker, and only after the alpha blocker has been initiated. Administration of beta-blockers alone in the setting of pheochromocytoma has been associated with a paradoxical increase in blood pressure due to the attenuation of beta-mediated vasodilatation in skeletal muscle.
Thyrotoxicosis
Metoprolol may mask certain clinical signs (e.g., tachycardia) of hyperthyroidism. Avoid abrupt withdrawal of beta blockade, which might precipitate a thyroid storm.
Metoprolol dose
Metoprolol comes as 2 different types of tablet: standard release and slow release (also called “sustained release” or SR).
- Standard release – releases metoprolol into your body quickly. You may need to take it several times a day depending on your dose.
- Slow release – dissolves slowly so you don’t have to take it as often. Once a day is usually enough.
Your doctor may advise you to take your first dose before bedtime because it could make you feel dizzy. If you don’t feel dizzy after the first dose, take metoprolol in the morning.
If you have metoprolol more than once a day, try to space the doses evenly throughout the day.
How much you take depends on why you need metoprolol and the type of tablet you’re taking.
- For high blood pressure: standard release – 50mg to 100mg twice a day; slow release – 200mg once a day
- For chest pain (angina): standard release – 50mg to 100mg 2 to 3 times a day; slow release – 200mg to 400mg once a day
- For irregular heartbeats (arrhythmias): standard release – 50mg 2 to 3 times a day
- For preventing migraine: standard release – 50mg 2 to 4 times a day, or 100mg twice a day
- For too much thyroid hormone (thyrotoxicosis): standard release – 50mg 4 times a day
Adult Dose for Hypertension
METOPROLOL TARTRATE IMMEDIATE RELEASE TABLETS:
- Initial dose: 100 mg orally per day in single or divided doses
- Maintenance dose: 100 to 450 mg orally per day
Comments:
- May increase dose at weekly, or longer, intervals.
- Doses above 450 mg per day have not been studied.
- Lower once-daily doses may not maintain full effect at the end of the 24-hour period; larger or more frequent daily doses may be required. Beta-1 selectivity diminishes as the dose is increased.
METOPROLOL SUCCINATE EXTENDED RELEASE TABLETS:
- Initial dose: 25 to 100 mg orally once a day
- Maintenance dose: 100 to 400 mg orally once a day
Comments:
- May increase dose at weekly, or longer, intervals.
- Doses above 400 mg per day have not been studied.
Adult Dose for Angina Pectoris
Initial dose:
- Metoprolol tartrate immediate release tablets: 50 mg orally twice a day
- Metoprolol succinate extended release tablets: 100 mg orally once a day
Maintenance dose: 100 to 400 mg per day
Comments:
- Increase dose at weekly intervals until optimum clinical response has been obtained or pronounced slowing of heart rate occurs.
- Doses above 400 mg per day have not been studied.
Adult Dose for Myocardial Infarction
- Use: Treatment of hemodynamically stable patients with definite or suspected acute myocardial infarction to reduce cardiovascular mortality. Treatment with the IV formulation can be initiated as soon as the patient’s clinical condition allows. Alternatively, treatment can begin within 3 to 10 days of the acute event.
Metoprolol tartrate:
- Early Treatment:
- Initial dose: 5 mg IV every 2 minutes as tolerated for 3 doses
- Patients tolerant of full IV dose (15 mg): 50 mg orally every 6 hours starting 15 minutes after the last IV dose and continued for 48 hours
- Patients intolerant of full IV dose (15 mg): 25 or 50 mg orally every 6 hours depending on the degree of intolerance starting 15 minutes after the last IV dose or as soon as their clinical condition allows
- Late Treatment:
- Maintenance dose: 100 mg orally twice a day
Comments:
Patients with contraindications to treatment during the early phase of suspected or definite myocardial infarction, patients who appear not to tolerate the full early treatment, and patients in whom the physician wishes to delay therapy for any other reason should be started on 100 mg orally twice a day as soon as their clinical condition allows.
Continue therapy for at least 3 months; efficacy beyond 3 months has not been conclusively established; data from studies with other beta blockers suggest a treatment duration of 1 to 3 years.
Adult Dose for Congestive Heart Failure
- Use: Treatment of stable, symptomatic New York Heart Association (NYHA) Class II or III heart failure of ischemic, hypertensive, or cardiomyopathic origin.
METOPROLOL SUCCINATE EXTENDED RELEASE TABLETS:
- 25 mg orally once a day (12.5 mg orally once a day in patients with more severe heart failure); double dose every 2 weeks to highest tolerated dose or up to 200 mg orally once a day
Comments: Initial titration difficulty should not preclude later attempts to introduce this drug.
Pediatric Dose for Hypertension
METOPROLOL SUCCINATE EXTENDED RELEASE TABLETS:
6 Years or Older:
- Initial dose: 1 mg/kg orally once a day (not to exceed 50 mg orally once a day)
- Maximum dose: 2 mg/kg (or 200 mg) orally once a day
Renal Dose Adjustments
- No adjustment recommended
Liver Dose Adjustments
- Initiate at low doses and titrate gradually according to clinical response.
What should I do if I forget a dose?
If you miss a dose of metoprolol, take it as soon as you remember, unless it is nearly time for your next dose. In this case, just leave out the missed dose and take your next dose as normal.
Never take 2 doses at the same time. Never take an extra dose to make up for a forgotten one.
If you often forget doses, it may help to set an alarm to remind you. You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
What if I take too much?
Taking too much metoprolol can slow down your heart rate and make it difficult to breathe. It can also cause dizziness and trembling.
The amount of metoprolol that can lead to an overdose varies from person to person.
If you take too much metoprolol by accident, call your doctor or go to your nearest hospital accident and emergency department straight away.
If you need to go to hospital, don’t drive yourself – get someone else to drive you or call an ambulance.
Take the metoprolol packet, or the leaflet inside it, with you plus any remaining medicine.
Metoprolol side effects
Like all medicines, metoprolol can cause side effects, but many people have no side effects or only minor ones. Side effects often improve as your body gets used to the medicine.
Common side effects
These common side effects happen in more than 1 in 100 people. They’re usually mild and short-lived.
Talk to your doctor or pharmacist if the side effects bother you or last more than a few days:
- headaches
- feeling tired, dizzy or weak
- cold hands or feet
- feeling sick (nausea)
- stomach ache
- dizziness or lightheadedness
- tiredness
- depression
- nausea
- dry mouth
- stomach pain
- vomiting
- gas or bloating
- heartburn
- constipation
- rash or itching
- runny nose
Serious side effects
It’s rare, but some people have serious side effects when taking metoprolol.
Call a doctor straight away if you have:
- shortness of breath, wheezing and tightening of the chest – these can be signs of lung problems
- shortness of breath with a cough that gets worse when you exercise (like walking up stairs), swollen ankles or legs, chest pain, an irregular heartbeat – these are signs of heart problems
- fast heart rate, high temperature (38 °C and above), trembling and confusion – these are signs of thyrotoxicosis (too much thyroid hormone in the blood)
- yellow skin, or the whites of your eyes turn yellow – these can be signs of liver problems
Serious allergic reaction
In rare cases, metoprolol may cause a serious allergic reaction.
A serious allergic reaction is an emergency. Contact a doctor straight away if you think you or someone around you is having a serious allergic reaction.
The warning signs of a serious allergic reaction are:
- getting a skin rash – this may include itchy, red, swollen, blistered or peeling skin
- wheezing
- tightness in the chest or throat
- having trouble breathing or talking
- swelling of the mouth, face, lips, tongue or throat
These are not all the side effects of metoprolol. Metoprolol may cause other side effects. For a full list, see the leaflet inside your medicine packet.
Call your doctor if you have any unusual problems while taking metoprolol.
Symptoms of overdose may include the following:
- dizziness
- fainting
- difficulty breathing or swallowing
- swelling of the hands, feet, ankles, or lower legs
How to cope with side effects
What to do about:
- Headaches – make sure you rest and drink plenty of fluids. Don’t drink too much alcohol. Ask your pharmacist to recommend a painkiller. Headaches usually go away after the first week of taking metoprolol. Talk to your doctor if the headaches are severe or last longer than a week.
- Feeling tired, dizzy or weak – if metoprolol makes you feel dizzy or weak, stop what you’re doing, and sit or lie down until you feel better. Don’t drive or use tools or machinery if you’re feeling tired. Don’t drink alcohol. It will make you feel worse.
- Cold hands or feet – put your hands or feet under warm running water, massage them, and wiggle your fingers and toes. Don’t smoke or have drinks with caffeine in – these can make your blood vessels narrower and restrict your blood flow. Smoking also makes your skin colder. Try wearing mittens (they’re warmer than gloves) and warm socks. Don’t wear tight watches or bracelets.
- Feeling sick – stick to simple meals and don’t eat rich or spicy food. It might help to take your metoprolol after you’ve eaten. If you’re being sick, try frequent small sips of water.
- Stomach ache – try to rest and relax. It can help to eat and drink slowly, and have smaller and more frequent meals. Putting a heat pad or covered hot water bottle on your tummy may also help. If you are in a lot of pain, speak to your pharmacist or doctor.