Contents
What is ARDS
ARDS is short for acute respiratory distress syndrome, which is a lung condition that leads to low oxygen levels in the blood. ARDS is a buildup of fluid in the tiny air sacs in your lungs called alveoli. This means less oxygen can get to your organs, which is very dangerous and life threatening, because your body’s organs need oxygen-rich blood to work well. ARDS occurs when there is significant trauma that either affects your lungs directly or indirectly. Some examples of trauma include sepsis (a blood infection), breathing in smoke from a house fire, near-drowning, severe pneumonia, major trauma, and shock from any cause. Your body responds to this trauma with an inflammatory reaction that releases numerous natural molecules into the bloodstream. Normally, this inflammatory reaction would be protective and help you fight infection or heal from an injury. However, in some people, these inflammatory molecules lead the smallest blood vessels in the lungs to leak fluid. Fluid leaves these small vessels and goes into the alveoli. The alveoli fill with this fluid making it difficult for oxygen to get into the bloodstream.
There are about 200,000 cases of ARDS each year in the United States. Most people who develop ARDS often are very ill with another disease or have major injuries. They might already be in the hospital when they develop ARDS. ARDS is a very serious disease and even with the best medical care between 30 and 50 percent of those diagnosed with ARDS die of it. Those surviving the disease will often have long hospital stays. One of the biggest problems with ARDS is that many patients develop additional complications while they are in the intensive care unit. Some of these complications include pneumonia, collapsed lungs, other infections, severe muscle weakness, confusion, and kidney failure.
ARDS is a serious disease that can be frightening for patients and families to endure. The outcomes tend to be better in younger patients, trauma patients and when ARDS is caused by blood transfusions. Most people will not die of the severely low oxygen levels in the blood associated with ARDS. However, the chance of dying increases dramatically if other organs begin to fail. This could include liver failure, kidney failure or severely decreased blood pressure.
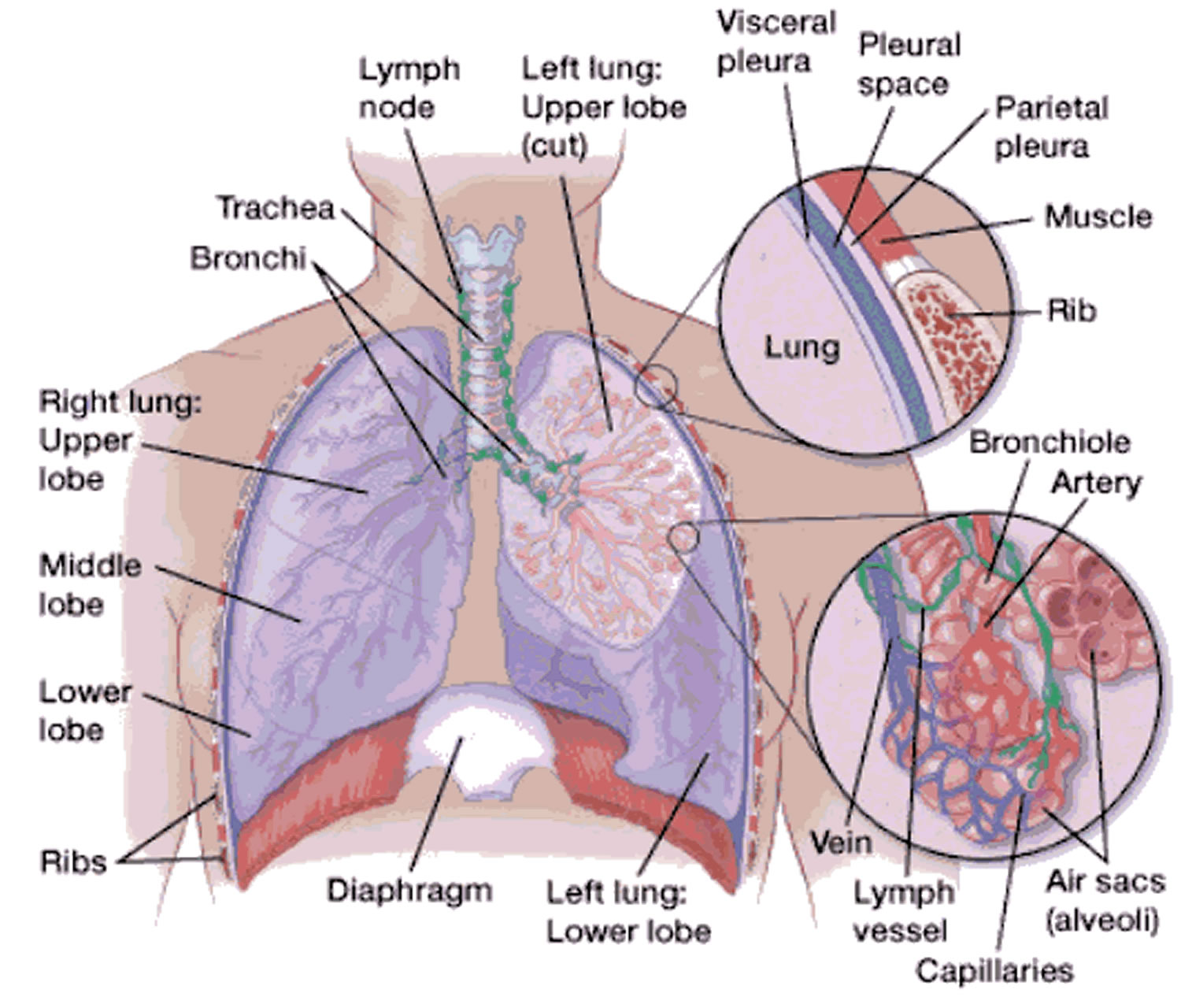
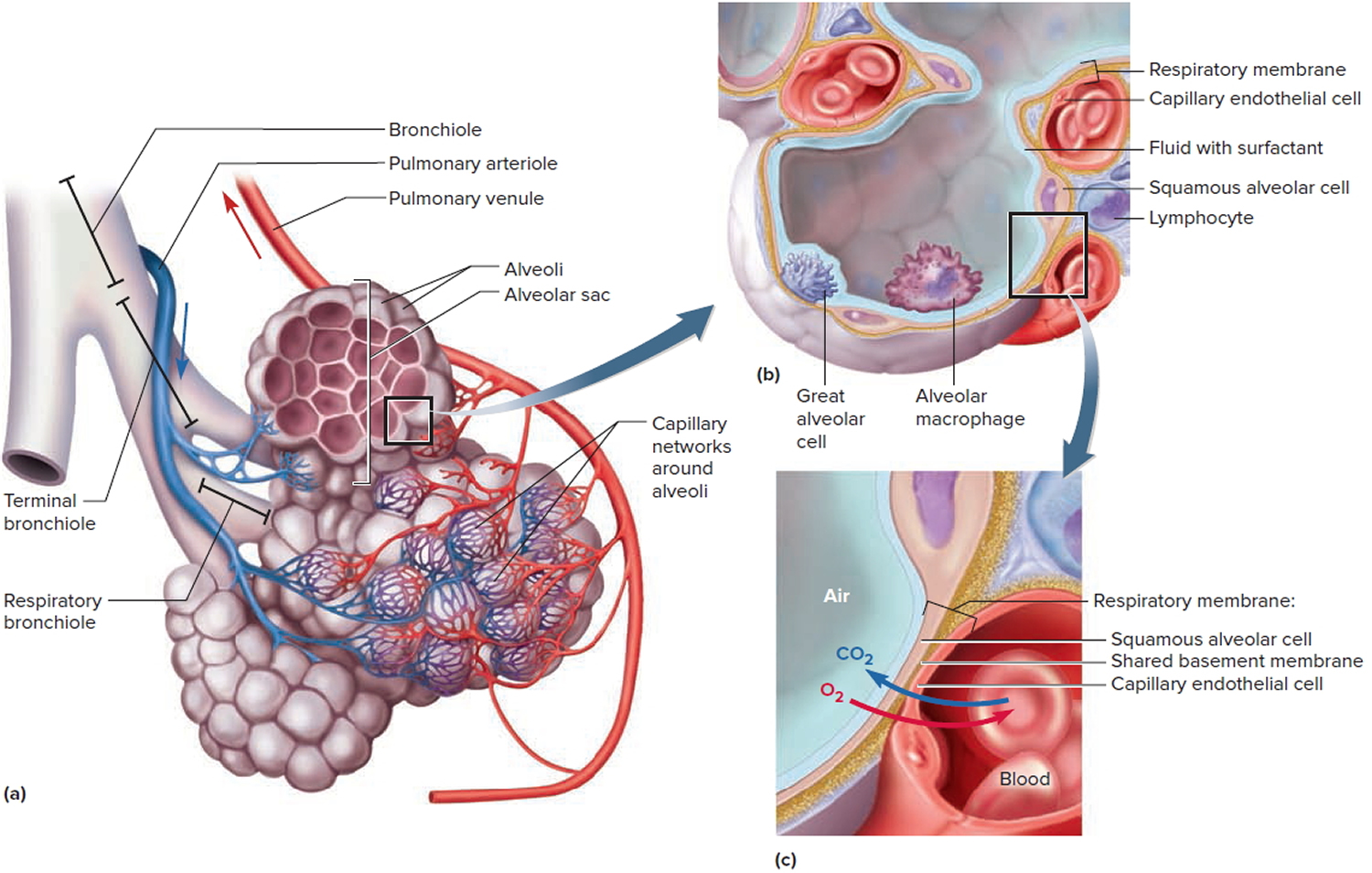
To understand ARDS, it helps to understand how the lungs work. When you breathe, air passes through your nose and mouth into your windpipe. The air then travels to your lungs’ air sacs. These sacs are called alveoli.
Small blood vessels called capillaries run through the walls of the air sacs. Oxygen passes from the air sacs into the capillaries and then into the bloodstream. Blood carries the oxygen to all parts of the body, including the body’s organs.
In ARDS, infections, injuries, or other conditions cause fluid to build up in the air sacs. The lung is damaged and a cycle of acute inflammation begins. There is damage to the alveolar wall and capillary lining, which increases leakage into the alveoli. Alveolar “surfactant” (needed to keep air spaces open) is lost or degraded, causing reduced compliance and lung collapse. This prevents the lungs from filling with air and moving enough oxygen into the bloodstream. The end result is an acute pulmonary edema and multi-organ failure. Other complications include pneumothorax (due to ventilation and reduced lung compliance) and secondary pneumonia.
In most cases ARDS will follow a rapid course from its development, progressing rapidly thought the various phases of edema, proliferation and later fibrosis or scarring of the airways.
As a result, the body’s organs (such as the kidneys and brain) don’t get the oxygen they need. Without oxygen, the organs may not work well or at all.
Depending on the amount of oxygen in the blood and during breathing, the severity of ARDS is classified as:
- Mild
- Moderate
- Severe
People who develop ARDS often are in the hospital for other serious health problems. Rarely, people who aren’t hospitalized have health problems that lead to ARDS, such as severe pneumonia.
The diagnosis of ARDS is based on your symptoms, vital signs, and a chest X-ray. There is no single test to confirm the diagnosis of ARDS. Patients with ARDS will have rapid onset of shortness of breath and very low oxygen levels in the blood. The chest X-ray will show fluid present in both lungs (often described as “infiltrates” by doctors reading chest X-rays). Since ARDS and some heart problems have similar symptoms, your doctor might perform certain tests to rule out a heart problem.
If you have trouble breathing, call your doctor right away. If you have severe shortness of breath, call your local emergency services number for an ambulance.
Key facts
- ARDS occurs when there is trauma to the lungs, either directly or indirectly.
- Most people who get ARDS are already in the hospital for trauma or illness.
- ARDS causes fluid to leak into the lungs, making it difficult to get oxygen into the blood.
- ARDS can be associated with an acute medical problem or procedure.
- The lungs usually recover and long-term lung failure after ARDS is rare.
- For people who survive ARDS, the main complications are associated with nerve and muscle damage, which causes pain and weakness. Some people also develop psychological problems, such as post-traumatic stress disorder (PTSD) and depression.
ARDS other names:
- Acute lung injury
- Adult respiratory distress syndrome
- Increased-permeability pulmonary edema
- Noncardiac pulmonary edema
In the past, ARDS was called stiff lung, shock lung, and wet lung.
How ARDS affects your body
The fluid that leaks into the lungs makes it very difficult to breathe and leads to low oxygen in the blood, or hypoxemia. The fluid in the lungs makes the lungs stiff and difficult to inflate. This increases the work it takes to breathe and get air into your lungs. When the body can’t carry out the work of breathing and has low oxygen levels, it causes respiratory failure. In order to improve the amount of oxygen and reduce the work of breathing, most ARDS patients will be placed on a ventilator to support them while the lungs heal. If the inflammation and fluid in the lung(s) persist, some patients will go on to develop scarring in the lungs. This is known as the fibrotic stage of ARDS. It is during this stage that the lung can “pop” and deflate, leading to a collapsed lung, also called a pneumothorax.
Figure 1. Lungs alveoli
Note: (a) Clusters of alveoli and their blood supply. (b) Structure of an alveolus. (c) Structure of the respiratory membrane.
ARDS survival rate
ARDS is a very serious disease and even with the best medical care between 30 and 50 percent of those diagnosed with ARDS die of it. Survival rates for ARDS vary depending on age, the underlying cause of ARDS, associated illnesses, and other factors. Moreoever, more people are surviving ARDS now than in the past. One likely reason for this is that treatment and care for the condition have improved.
Some people who survive recover completely. Others may have lasting damage to their lungs and other health problems. Those surviving the disease will often have long hospital stays. One of the biggest problems with ARDS is that many patients develop additional complications while they are in the intensive care unit (ICU). Some of these complications include pneumonia, collapsed lungs, other infections, severe muscle weakness, confusion, and kidney failure.
Researchers continue to look for new and better ways to treat ARDS.
Some people fully recover from ARDS. Others continue to have health problems. After you go home from the hospital, you may have one or more of the following problems:
- Shortness of breath. After treatment, many people who have ARDS recover close-to-normal lung function within 6 months. For others, it may take longer.
- Some people have breathing problems for the rest of their lives.
- Tiredness and muscle weakness. Being in the hospital and on a ventilator (a machine that supports breathing) can cause your muscles to weaken. You also may feel very tired following treatment.
- Depression. Many people who’ve had ARDS feel depressed for a while after treatment.
- Problems with memory and thinking clearly. Certain medicines and a low blood oxygen level can cause these problems.
These health problems may go away within a few weeks, or they may last longer. Talk with your doctor about how to deal with these issues.
Getting help
You can take steps to recover from ARDS and improve your quality of life. For example, ask your family and friends for help with everyday activities.
If you smoke, quit. Smoking can worsen lung problems. Talk to your doctor about programs and products that can help you quit. Also, try to avoid secondhand smoke and other lung irritants, such as harmful fumes.
If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking.
Go to pulmonary rehabilitation (rehab) if your doctor recommends it. Rehab might include exercise training, education, and counseling. Rehab can teach you how to return to normal activities and stay active.
Your rehab team might include doctors, nurses, and other specialists. They will work with you to create a program that meets your needs.
Emotional issues and support
Living with ARDS may cause fear, anxiety, depression, and stress. Talk about how you feel with your health care team. Talking with a professional counselor also can help. If you’re very depressed, your doctor may recommend medicines or other treatments that can improve your quality of life.
Joining a patient support group may help you adjust to living with ARDS. You can see how other people who have the same symptoms have coped with them. Talk to your doctor about local support groups or check with an area medical center.
Support from family and friends also can help relieve stress and anxiety. Let your loved ones know how you feel and what they can do to help you.
ARDS stages
The European Society of Intensive Care Medicine, endorsed by the American Thoracic Society and the Society of Critical Care Medicine, developed the Berlin Definition, a draft definition for 3 mutually exclusive categories of ARDS based on degree of hypoxemia 1:
- Mild (200 mm Hg < PaO2/FIO2 ≤ 300 mm Hg),
- Moderate (100 mm Hg < PaO2/FIO2 ≤ 200 mm Hg), and
- Severe (PaO2/FIO2 ≤ 100 mm Hg) and 4 ancillary variables for severe ARDS: radiographic severity, respiratory system compliance (≤40 mL/cm H2O), positive end-expiratory pressure (≥10 cm H2O), and corrected expired volume per minute (≥10 L/min). The 4 ancillary variables did not contribute to the predictive validity of severe ARDS for mortality and were removed from the definition.
Using the Berlin Definition, stages of mild, moderate, and severe ARDS were associated with increased mortality (27%, 32% and 45% respectively) and increased median duration of mechanical ventilation in survivors (5 days, 7 days and 9 days respectively) 1. Compared with the American-European Consensus Conference definition, the final Berlin Definition had better predictive validity for mortality 1.
ARDS signs and symptoms
ARDS may initially be diagnosed as pneumonia or pulmonary edema (fluid in the lungs from heart disease). However, your doctor may suspect ARDS if you are not getting better and have one of the known causes of ARDS.
Patients with ARDS have shortness of breath and a low blood oxygen level, often severe. They also have a cough and many have fever. Those with ARDS also have fast heart rates and rapid breathing. Occasionally, they experience chest pain, especially during inhalation. Some patients who have very low oxygen levels may have bluish coloring of nails and lips from the severely decreased oxygen levels in the blood.
Other signs and symptoms depend on the cause of ARDS. They may occur before ARDS develops. For example, if pneumonia is causing ARDS, you may have a cough and fever before you feel short of breath.
Sometimes people who have ARDS develop signs and symptoms such as low blood pressure, confusion, and extreme tiredness. This may mean that the body’s organs, such as the kidneys and heart, aren’t getting enough oxygen-rich blood.
People who develop ARDS often are in the hospital for other serious health problems. Rarely, people who aren’t hospitalized have health problems that lead to ARDS, such as severe pneumonia.
If you have trouble breathing, call your doctor right away. If you have severe shortness of breath, call your local emergency services number for an ambulance.
Complications from ARDS
If you have ARDS, you can develop other medical problems while in the hospital. The most common problems are:
- Infections. Being in the hospital and lying down for a long time can put you at risk for infections, such as pneumonia. Being on a ventilator also puts you at higher risk for infections.
- A pneumothorax (collapsed lung). This is a condition in which air or gas collects in the space around the lungs. This can cause one or both lungs to collapse. The air pressure from a ventilator can cause this condition.
- Lung scarring (pulmonary fibrosis). ARDS causes the lungs to become stiff (scarred). It also makes it hard for the lungs to expand and fill with air. Being on a ventilator also can cause lung scarring.
- Blood clots. Lying down for long periods can cause blood clots to form in your body. A blood clot that forms in a vein deep in your body is called a deep vein thrombosis. This type of blood clot can break off, travel through the bloodstream to the lungs, and block blood flow. This condition is called pulmonary embolism.
Thanks to improved treatments, more people are surviving ARDS. However, many survivors end up with potentially serious and sometimes lasting effects:
- Breathing problems. Many people with ARDS recover most of their lung function within several months to two years, but others may have breathing problems for the rest of their lives. Even people who do well usually have shortness of breath and fatigue and may need supplemental oxygen at home for a few months.
- Depression. Most ARDS survivors also report going through a period of depression, which is treatable.
- Problems with memory and thinking clearly. Sedatives and low levels of oxygen in the blood can lead to memory loss and cognitive problems after ARDS. In some cases, the effects may lessen over time, but in others, the damage may be permanent.
- Tiredness and muscle weakness. Being in the hospital and on a ventilator can cause your muscles to weaken. You also may feel very tired following treatment.
ARDS causes
The mechanical cause of ARDS is fluid leaked from the smallest blood vessels in the lungs into the tiny air sacs where blood is oxygenated. Normally, a protective membrane keeps this fluid in the vessels. Severe illness or injury, however, can cause damage to the membrane, leading to the fluid leakage of ARDS.
The causes of ARDS are divided into two categories: direct or indirect injuries to the lung. Some of the direct injuries to the lung include pneumonia, breathing stomach contents into the lung (also known as aspiration), near drowning, lung bruising from trauma (such as a car accident) and smoke inhalation from a house fire.
The indirect injuries to the lung include inflammation of the pancreas, severe infection (also known as sepsis), blood transfusions, burns, and medication reactions.
Direct Lung Injury
Conditions that can directly injure the lungs include:
- Pneumonia. This is an infection in the lungs.
- Breathing in harmful fumes or smoke.
- Inhaling vomited stomach contents from the mouth.
- Using a ventilator. This is a machine that helps people breathe; rarely, it can injure the lungs.
- Nearly drowning.
Indirect Lung Injury
Conditions that can indirectly injure the lungs include:
- Sepsis. This is a condition in which bacteria infect the bloodstream.
- Severe bleeding caused by an injury to the body or having many blood transfusions.
- An injury to the chest or head, such as a severe blow.
- Pancreatitis. This is a condition in which the pancreas becomes irritated or infected. The pancreas is a gland that releases enzymes and hormones.
- Fat embolism. This is a condition in which fat blocks an artery. A physical injury, like a broken bone, can lead to a fat embolism.
- Drug reaction.
Fortunately, most patients with the problems listed above will not develop ARDS. It is not known why some will.
The most common underlying causes of ARDS include:
- Sepsis. The most common cause of ARDS is sepsis, a serious and widespread infection of the bloodstream.
- Inhalation of harmful substances. Breathing high concentrations of smoke or chemical fumes can result in ARDS, as can inhaling (aspirating) vomited stomach contents from the mouth or near-drowning episodes.
- Severe pneumonia. Severe cases of pneumonia usually affect all five lobes of the lungs.
- Severe bleeding caused by an injury to the body.
- Head, chest or other major injury. Accidents, such as falls or car crashes, can directly damage the lungs or the portion of the brain that controls breathing.
- Others.
- Pancreatitis (inflammation of the pancreas);
- Massive blood transfusions and burns;
- Diabetic ketoacidosis (acidic pH level in blood due to the body breaking down ketones instead of sugar);
- Hypersensitivity reactions;
- Drugs reactions due to aspirin, heroin or paraquat;
- Multiple blood transfusions;
- Malaria;
- Acute liver failure;
- Obstetric complications: Problems during pregnancy or delivery such as preeclampsia;
- Cardiac surgery and other complicated surgeries.
It’s not clear why some very sick or seriously injured people develop ARDS and others don’t. Researchers are trying to find out why ARDS develops and how to prevent it.
Risk factors for developing ARDS
People at risk for ARDS have a condition or illness that can directly or indirectly injure their lungs.
While it is not clear who will develop ARDS, there are a few factors that may increase the risk for ARDS. These factors include:
- A history of cigarette smoking
- Oxygen use for a pre-existing lung condition
- Recent high-risk surgery
- Obesity
- Low protein in the blood
- Alcohol abuse
- Recent chemotherapy
ARDS diagnosis
Your doctor will diagnose ARDS based on your medical history, a physical exam, and test results.
Medical history
Your doctor will ask whether you have or have recently had conditions that could lead to ARDS.
Your doctor also will ask whether you have heart problems, such as heart failure. Heart failure can cause fluid to build up in your lungs.
Physical Exam
ARDS may cause abnormal breathing sounds, such as crackling. Your doctor will listen to your lungs with a stethoscope to hear these sounds.
He or she also will listen to your heart and look for signs of extra fluid in other parts of your body. Extra fluid may mean you have heart or kidney problems.
Your doctor will look for a bluish color on your skin and lips. A bluish color means your blood has a low level of oxygen. This is a possible sign of ARDS.
Diagnostic Tests
You may have ARDS or another condition that causes similar symptoms. To find out, your doctor may recommend one or more of the following tests.
Initial Tests
The first tests done are:
- An arterial blood gas test. This blood test measures the oxygen level in your blood using a sample of blood taken from an artery. A low blood oxygen level might be a sign of ARDS.
- Chest x ray. This test creates pictures of the structures in your chest, such as your heart, lungs, and blood vessels. A chest x ray can show whether you have extra fluid in your lungs.
- Blood tests, such as a complete blood count, blood chemistries, and blood cultures. These tests help find the cause of ARDS, such as an infection.
- A sputum culture. This test is used to study the spit you’ve coughed up from your lungs. A sputum culture can help find the cause of an infection.
Other Tests
Other tests used to diagnose ARDS include:
- Chest computed tomography scan, or chest CT scan. This test uses a computer to create detailed pictures of your lungs. A chest CT scan may show lung problems, such as fluid in the lungs, signs of pneumonia, or a tumor.
- Heart tests that look for signs of heart failure. Heart failure is a condition in which the heart can’t pump enough blood to meet the body’s needs. This condition can cause fluid to build up in your lungs. Your doctor may recommend heart tests such as:
- Electrocardiogram. This painless test tracks the electrical activity in your heart. It involves attaching several wired sensors to your body.
- Echocardiogram. A sonogram of the heart, this test can reveal problems with the structures and the function of your heart.
ARDS treatment
ARDS is treated in a hospital’s intensive care unit (ICU). Because there is no direct cure for ARDS, treatment focuses on supporting the patient while the lung heals. ARDS will often worsen in the first few days following the diagnosis before the lung begins to heal. The goal of this supportive care is to keep enough oxygen in the blood to prevent further damage to your body and to treat whatever caused ARDS in the first place. Another important part of the care for ARDS is to prevent and manage complications related to being in an intensive care unit. Current treatment approaches focus on improving blood oxygen levels and providing supportive care. Doctors also will try to pinpoint and treat the underlying cause of the condition.
Oxygen therapy
All patients with ARDS will require oxygen therapy. One of the main goals of treating ARDS is to provide oxygen to your lungs and other organs (such as your brain and kidneys). Your organs need oxygen to work properly.
Oxygen usually is given through nasal prongs or a mask that fits over your mouth and nose. However, if your oxygen level doesn’t rise or it’s still hard for you to breathe, your doctor will give you oxygen through a breathing tube to be supported by a ventilator. Your doctor will insert the flexible breathing tube through your mouth or nose and into your trachea or windpipe.
Before inserting the tube, your doctor will squirt or spray a liquid medicine into your throat (and possibly your nose) to make it numb. Your doctor also will give you medicine through an intravenous (IV) line in your bloodstream to make you sleepy and relaxed.
The breathing tube will be connected to a machine that supports breathing (a ventilator). The ventilator will fill your lungs with oxygen-rich air.
Your doctor will adjust the ventilator as needed to help your lungs get the right amount of oxygen. This also will help prevent injury to your lungs from the pressure of the ventilator.
You’ll use the breathing tube and ventilator until you can breathe on your own. If you need a ventilator for more than a few days, your doctor may do a tracheotomy. Although there is no set time, after about 7 to 14 days, your doctors may need to surgically place a tube that is surgically placed directly into the windpipe through the neck called tracheostomy. The tracheostomy procedure involves making a small cut in your neck to create an opening to the windpipe. This tube is not permanent and can easily be removed once the patient no longer needs the ventilator. The tracheostomy breathing tube would only be placed if your doctors felt it would take longer than a few weeks to remove the patient from the ventilator.
Prone positioning
Hospitalized patients are typically in bed on their backs. However, lying face down (prone) may help improve oxygen levels in the blood and increase survival in patients with ARDS. This can be a very complicated task that takes an entire team to accomplish, and some patients may be too sick for this treatment. There are specialized beds designed to help position patients in the intensive care unit face down and, although they are convenient, they are not absolutely necessary for this therapy.
Supportive Care
Supportive care refers to treatments that help relieve symptoms, prevent complications, or improve quality of life. Supportive approaches used to treat ARDS include:
- Medicines to help you relax, relieve discomfort, and treat pain.
- Ongoing monitoring of heart and lung function (including blood pressure and gas exchange).
- Nutritional support. People who have ARDS often suffer from malnutrition. Thus, extra nutrition may be given through a feeding tube.
- Treatment for infections. People who have ARDS are at higher risk for infections, such as pneumonia. Being on a ventilator also increases the risk of infections. Doctors use antibiotics to treat pneumonia and other infections.
- Prevention of blood clots. Lying down for long periods can cause blood clots to form in the deep veins of your body. These clots can travel to your lungs and block blood flow (a condition called pulmonary embolism). Blood-thinning medicines and other treatments, such as compression stocking (stockings that create gentle pressure up the leg), are used to prevent blood clots.
- Prevention of intestinal bleeding. People who receive long-term support from a ventilator are at increased risk of bleeding in the intestines. Medicines can reduce this risk.
- Fluids. You may be given fluids to improve blood flow through your body and to provide nutrition. Your doctor will make sure you get the right amount of fluids. Fluids usually are given through an IV line inserted into one of your blood vessels.
Sedation and medications to prevent movement
It is uncomfortable and painful to be supported by a ventilator. This often leads to restlessness and agitation, which can cause even more problems for the lungs. In order to keep comfortable and prevent this, the patient may need sedation to remain calm. There are medications called paralytics that can temporarily prevent patients from moving. Because the side effects related to these medications are significant, the risks and benefits need to be closely considered.
Fluid management
Sometimes doctors will give patients with ARDS a medication called a diuretic to help increase urination. This removes fluid from the body and can help prevent fluid from building up in the lungs. This must be done carefully, because too much fluid removal can lead to low blood pressure or kidney problems.
Extracorporeal membrane oxygenation (ECMO)
Extracorporeal membrane oxygenation (ECMO) is a very complicated treatment that takes blood outside of your body and pumps it through a membrane that adds oxygen and removes carbon dioxide and then returns the blood to your body. This is a high-risk therapy with many complications. It is not suitable for every patient with ARDS.
Recovering from ARDS
What to expect
It is important to note that people can survive ARDS. Most patients will not require oxygen on a long-term basis and will regain most of their lung function. Some people who survive ARDS struggle with weakness, which might mean they end up in the hospital more frequently or need to seek out therapy, such as pulmonary rehabilitation, to regain their strength.
Finding support
Facing ARDS may cause fear, anxiety, depression, and stress for both patients and their loved ones. Joining a support group may help you adjust to your condition. You can see how other people who have the same symptoms have coped with them. Talk to your doctor about local support groups, or check with an area medical center.
Support from family and friends also can help relieve stress and anxiety. Let your loved ones know how you feel and what they can do to help you.
The American Lung Association recommends patients and caregivers join their Living with Lung Disease Support Community (https://www.inspire.com/groups/american-lung-association-lung-disease/) to connect with others facing this disease. You can also call the Lung Association’s Lung Helpline at 1-800-586-4872 to talk to a trained respiratory professional who can help answer your questions and connect you with support.