Contents
What is a chalazion
Chalazion also known as meibomian cyst, is a common noninfectious obstruction of meibomian (sebaceous) tear glands. Chalazion usually presenting as eyelid swelling or painless nodule over eyelid. Chalazion affects upper eyelid more commonly than lower lid because there are more meibomian glands in the upper lid. A chalazion is a focus of granulomatous inflammation within the eyelid that originates from an obstructed meibomian gland of the tarsal plates 1. Chalazion arises from retained meibomian secretions. If acute secondary infection (e.g. Staphylococcus aureus) takes place, the lesion is known as hordeolum. Chalazion is harmless and often self limiting. However, larger chalazions may be associated with visual symptoms. Chalazion may grow to become large and can cause visual interference by deforming the cornea, leading to induced astigmatism or reduction in the superior peripheral visual field from mechanical ptosis. Chalazion affects both sex equally and occurs in all age groups.
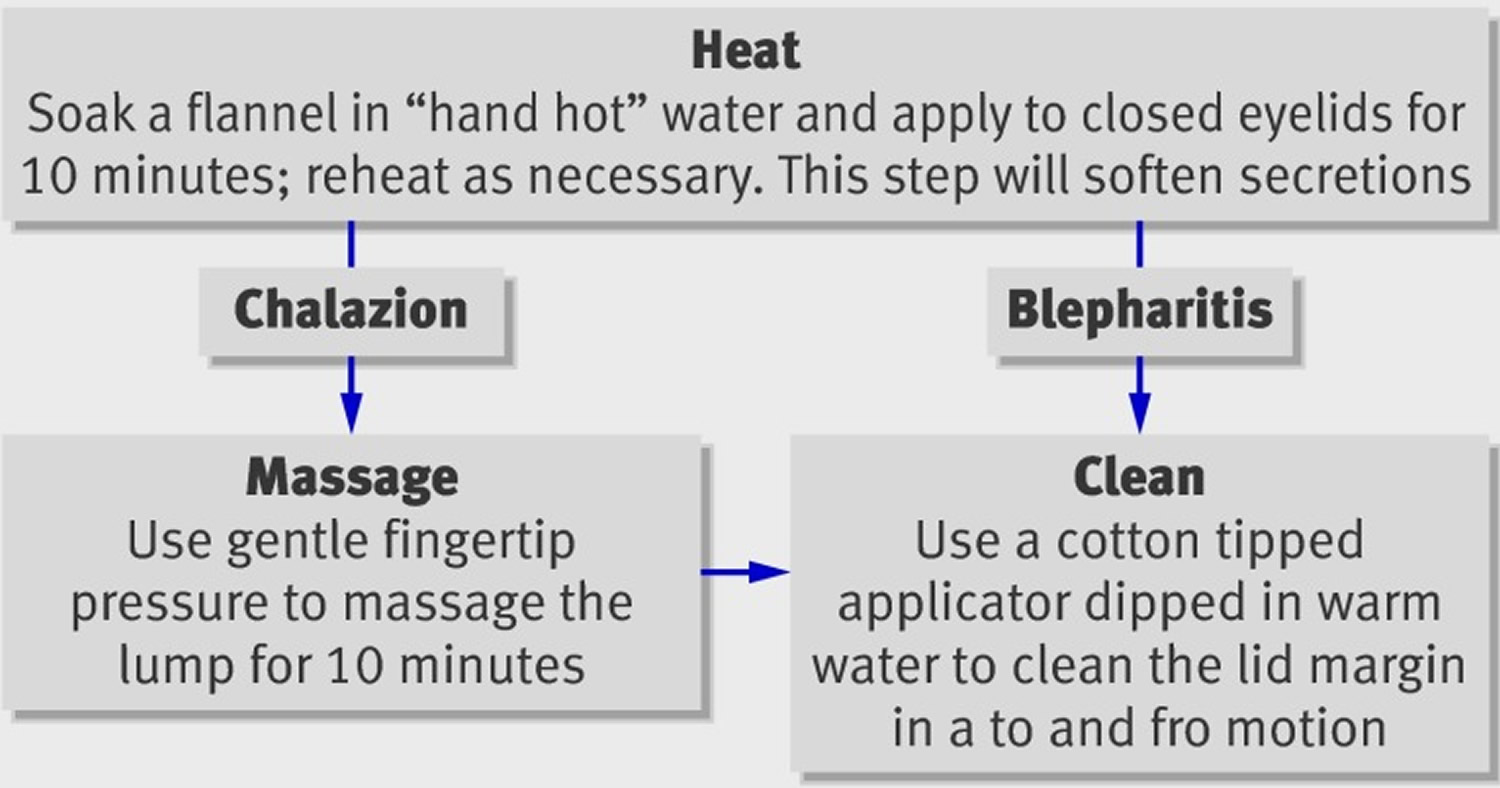
Most chalazions will respond to conservative treatment of applying heat and massage at least twice a day. Excellent prognosis could be expected. Chalazion is caused by an obstructed eyelid Meibomian glands that contains fatty material; heat softens this material, and massage disperses it. Early treatment may lead to faster resolution. Chalazion resolution often takes time and that several weeks of regular hot bathing may be required. Topical antibiotic preparations are of no benefit and should be avoided. Surgical management, involving incision and curettage or intralesional triamcinolone, should be regarded as second line treatment. Infected chalazions (hordeolums), with or without cellulitis, require oral antibiotics.
Key facts
- Patients report a slowly enlarging lump with some variability in size on a day to day basis.
- Chalazion is painless. This allows the chalazion to be differentiated from a hordeolum (a small abscess) or infection of the meibomian (sebaceous) glands.
- Skin conditions which predispose to meibomian gland dysfunction— acne rosacea and seborrhoeic dermatitis.
- The eyes have been unusually gritty, uncomfortable, or “tired”—these symptoms point to blepharitis, which predisposes to chalazion formation. Patients with severe blepharitis also report sticky eyes, especially on waking.
- Large chalazion can occasionally exert mass effect on cornea and result in astigmatism and blurred vision.
- Acute secondary infection leading to pain that may require incision and curettage.
- Have a low threshold for referring young children with large chalazions on account of the risk of amblyopia.
- In elderly people, consider the possibility of sebaceous cell carcinoma if a chalazion fails to settle or recurs.
- Diagnosis is by clinical findings. Further workup for confirmation is usually not necessary except in recurrent cases where sebaceous gland carcinoma needed to be excluded.
- Most chalazions will respond to conservative treatment of applying heat and massage at least twice a day. Excellent prognosis could be expected.
Hordeolum vs chalazion
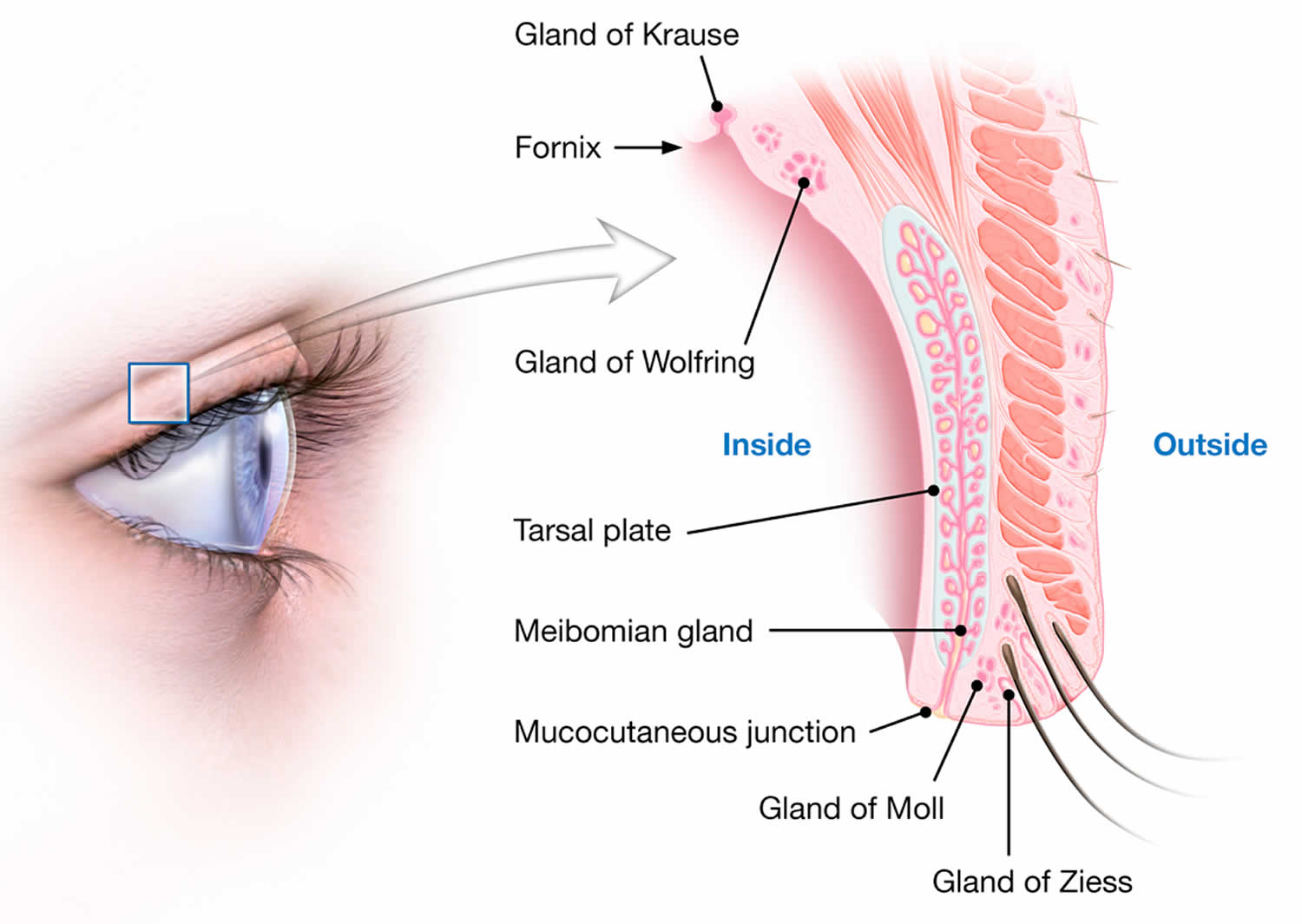
Hordeolum is an infection of the meibomian (sebaceous) glands. A chalazion is caused by noninfectious meibomian gland occlusion. Hordeolum may be on the external or internal surface of the eyelid and may lead to edema of the entire lid. An external hordeolum arises from a blockage with secondary inflammation of the Zeiss or Moll sebaceous glands of the eyelid (see Figures 2 and 3). An internal hordeolum is a secondary inflammatory response of the meibomian glands in the tarsal plate. At times, purulent material is released from the outer eyelash line in external hordeola, while internal hordeola exude on the inner conjunctival surface of eyelid. Although rare, cellulitis of the eyelid may occur if an internal hordeolum is untreated.
Hordeola are found more frequently in patients with dry eyes and chronic blepharitis (eyelid inflammation).
Both hordeolum and chalazion initially cause eyelid hyperemia and edema, swelling, and pain at distal eyelid margin. With time, a chalazion becomes a small nontender nodule in the eyelid center, whereas a hordeolum remains painful and localizes to an eyelid margin. Diagnosis is clinical. Treatment is primarily with hot compresses and massage at least twice a day. Both conditions improve spontaneously, but incision or, for chalazia, intralesional corticosteroids may be used to hasten resolution.
Chalazion vs stye
Stye is an infection of the sweat gland (gland of Zeiss) of the eyelid. Stye appears as a red, swollen bump that resembles a pimple in appearance. Stye is sometimes tender in its acute presentation, especially to the touch. More chronic appearance of a stye often leads to a chalazion.
Styes are similar to common acne pimples that occur elsewhere on the skin and patients may have more than one stye at the same time. They commonly develop over a few days and may drain and heal without treatment.
Staphylococcal bacteria are the most common causes of eyelid infections, but other organisms normally found on the skin may be precipitating factors.
Daily eyelid hygiene with a mild soap and warm water is necessary to reduce the incidence of styes. Eyelid and face make-up should be removed completely before going to sleep.
It is important to wash hands thoroughly before touching the skin around the eye. Patients who are susceptible to styes should carefully clean excess oils from the eyelid margin. Commercial eyelid scrubs are available and may be recommended by an eye doctor as primary prevention for styes.
Stye and chalazion may be treated by applying warm compresses to the eyelid several times per day. This helps to accelerate drainage of the lesion. Antibiotic ointments with concomittant steroid may help styes to resolve more quickly. Regular follow-up with an ophthalmologist is necessary to chronicle regression and monitor side effects from medications. In some cases, injection of triamcinolone (Kenalog) can help in resolving the lesion, although carries the risks of skin necrosis, subcutaneous fat atrophy, embolic visual loss, incomplete resolution and need for surgical removal, and skin hypo-pigmentation or hyper-pigmentation (particularly in patients with darker skin tones).
If left untreated, styes may rarely lead to more widespread infections that involve the periorbital tissues. Also, stye recurrence is common if prophylactic daily lid hygiene is not done upon resolution.
Complications of improper drainage include disruption of lash growth, eyelid deformity, or eyelid fistula.
How long does a chalazion last?
Untreated chalazion usually resolves spontaneously in weeks. However, recurrence is common.
Figure 1. Chalazion eye
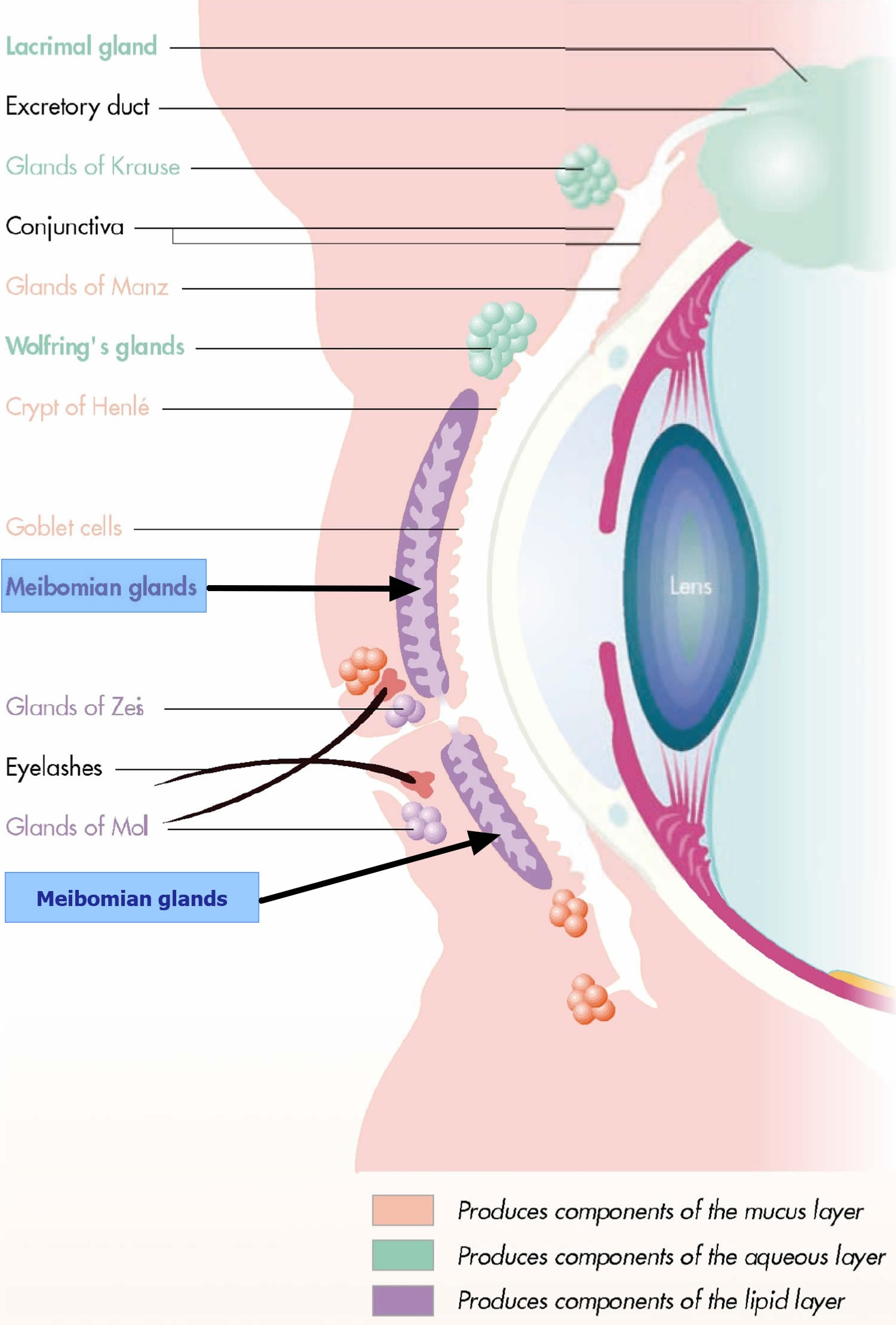
Figure 2. Eyelid anatomy
Figure 3. Upper Eyelid anatomy
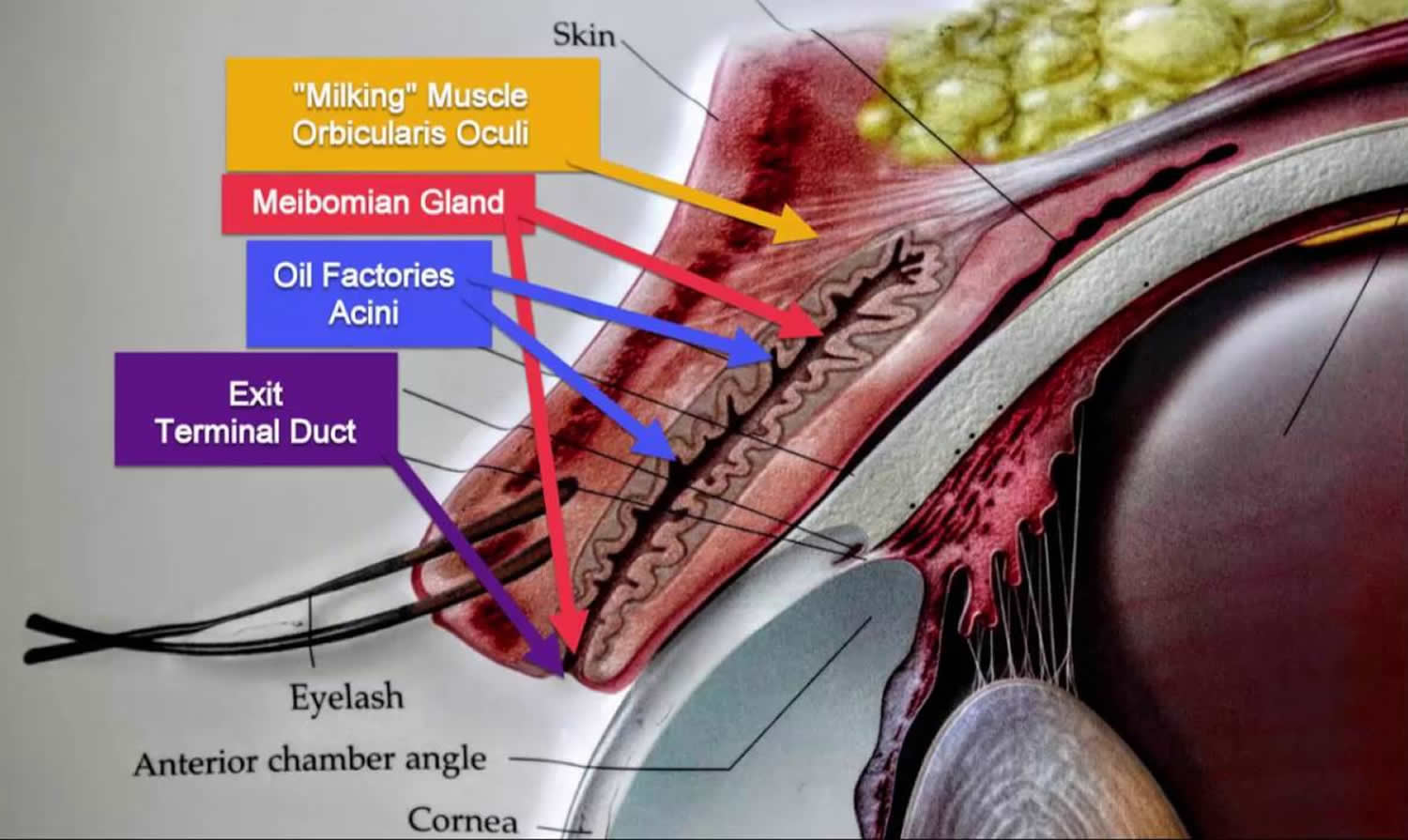
Meibomian glands
Meibomian glands are sebaceous tear glands located in the tarsal plate of eyelid. Meibomian glands secretion includes polar and non-polar lipids, which are components of tear film. If the outflow of Meibomian glands sebaceous secretions is obstructed, the oily secretions are retained and may leak into the adjacent tissue, which will in turn induce chronic granulomatous inflammatory response leading to formation of lipogranuloma or chalazion.
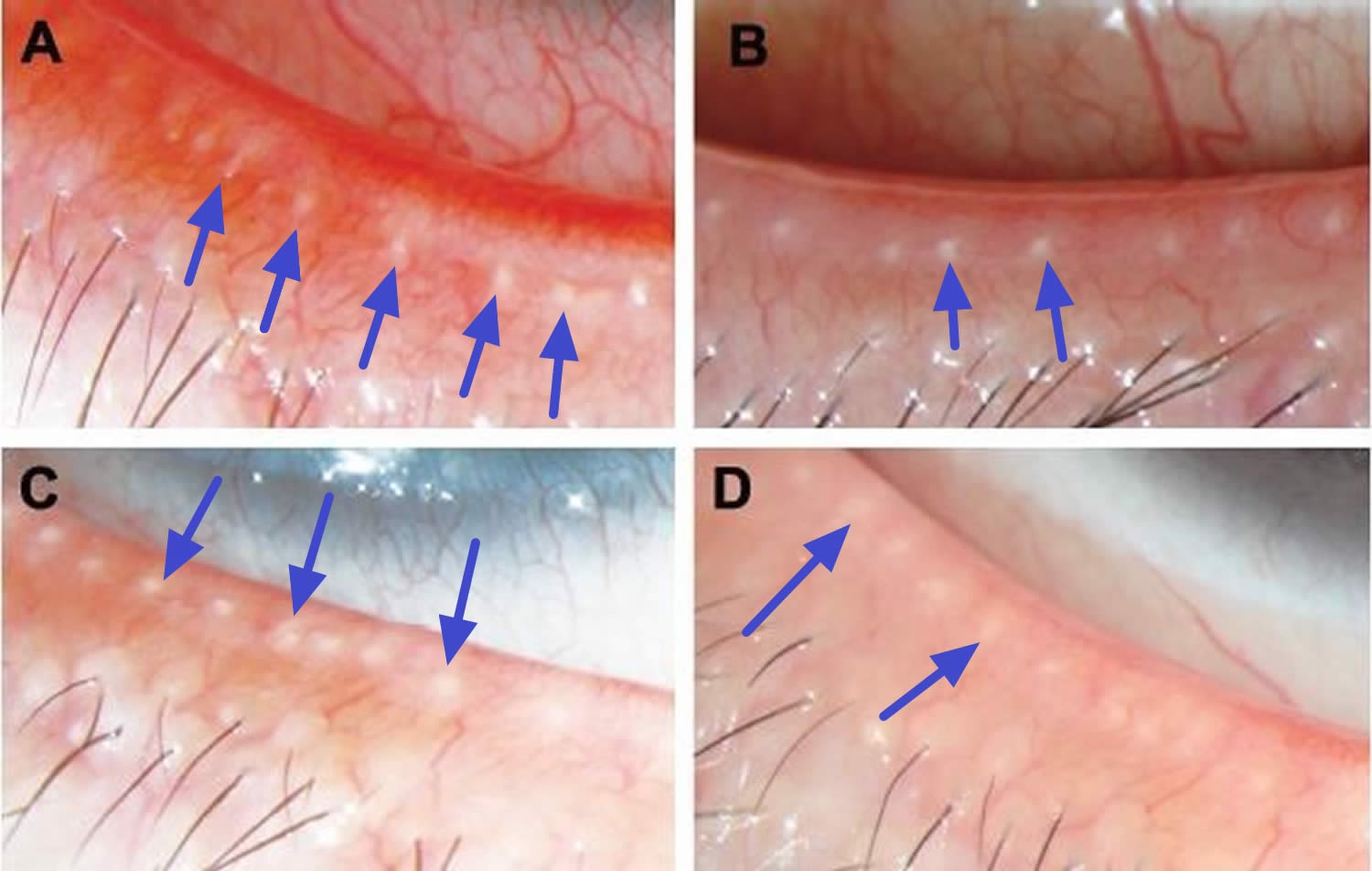
Figure 4. Meibomian glands
Figure 5. Meibomian gland openings on eyelids
Chalazion symptoms
Patient usually presents with gradually enlarging eyelid nodule, eyelid discomfort or even painful swelling if secondary infection occurs (hordeolum). Many patients would have history of similar eyelid swelling in the past.
- Discrete mass within the lid present for two or more weeks.
On examination of the eyelid, a solitary, non-tender nodule should be noted in the tarsal plate. Eversion of eyelid may help identifying the lesion if it is not apparent over skin surface.
Chalazion causes
Chronic granulomatous reaction in the eyelid induced by retained sebaceous secretions from meibomian gland. Histology of the lesion will reveal cells characterizing chronic granulomatous inflammation, namely multinucleated giant cells and epithelioid cells (lipid-laden macrophages in this case). Lymphocytes and plasma cells may also be present.
Risk factors
History or blepharitis, rosacea, prior chalazion, or any type of eyelid inflammation. Other factors can be uncorrected refractive errors and uncontrolled diabetes, long hours of work on computers.
Chalazion prevention
Regular massage and warm compresses can help in drainage of the sebaceous secretion and therefore decrease occurrence or recurrence of chalazion. Maintaining good lid hygiene may also be beneficial.
Prevention also relies on management of blepharitis and its causes. Twice daily lid hygiene (heating and cleaning), on a long term basis, to those with obvious blepharitis. Blepharitis is a chronic condition and that flare-ups can be managed with regular lid hygiene. Lid hygiene also reduces the likelihood of a gland becoming obstructed. Your doctor may prescribe a course of tetracycline (doxycycline 50-100 mg once daily or lymecycline 408 mg once daily for at least three months) for blepharitis that is severe or associated with rosacea. Erythromycin is a good alternative in children and pregnancy.
Chalazion diagnosis
Clinical diagnosis is usually based on patient’s history and appearance of the lesion.
Diagnostic procedures
Slit-lamp examination to assess the condition of the meibomian glands (which often show diffuse inspissation of yellowish contents from the eyelid margin orifices). The eyelid should be everted to exclude other pathologies, such as a retained foreign body, or tarsal cyst.
Laboratory test is usually not necessary. Microscopy of the materials from chalazion shows chronic inflammatory cells and occasionally acute inflammatory cells such as polymorphs.
Chalazion treatment
Small, asymptomatic chalazion can be left untreated. Conservative treatment including lid massage, warm compression and steroid eyedrops can also be used. However, with administration of topical or local steroid agents, the intraocular pressure (IOP) should be monitored.
Topical antibiotics eyedrops is useful if lesion is associated with inflammatory conditions such as blepharitis. Direct injection of steroid (triamcinolone, kenalog) with lidocaine into the lesion may be preferable for lesions in close proximity to the vulnerable lacrimal apparatus where surgical drainage is difficult. Steroid injection leads to resolution in most cases; repeated injection can be given 1-2 weeks later if lesion persists. However, patients should be aware that intralesional steroid injection carries the risks of skin necrosis, subcutaneous fat atrophy, embolic visual loss, incomplete resolution and need for surgical removal, and skin hypo-pigmentation or hyper-pigmentation (particularly in patients with darker skin tones). Transconjunctival steroid injection may lead to local skin depigmentation or atrophy of skin.
Figure 6. Chalazion treatment at home
Medical therapy
Prophylactic systemic tetracyclines (such as doxycycline) can be considered in recurrent cases. There may be a role for topical antibiotics prophylaxis with macrolide antibiotics (such as erythromycin ointment or Azithromycin gel).
Chalazion surgery
Surgical treatment may be considered in case of unresolved chalazion or large and symptomatic chalazion. Incision and curettage is the treatment of choice.
Local anaethestic agent is injected to the area surrounding the lesion. Eyelid is then everted with special clamp and incision is made through conjunctiva. Contents of chalazion are curetted, and tarsus may be minimally resected if indicated. The incision is left open with clean margins to allow for drainage of any residual material within the lesion. Since the operation is done at the inner side of eyelid, no scar will be seen over the anterior aspect of the lid.
Preferably, specimens obtained during the procedure should be sent to pathology and obtain and final read, to rule out other dangerous diagnoses.
Surgical follow up
Patient may be seen again in several weeks, or follow-up as required. The inflamed lid may still take several weeks to completely resolve.
- Arbabi EM, Kelly RJ, Carrim ZI. Chalazion. The BMJ. 2010;341:c4044. doi:10.1136/bmj.c4044. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2974575/[↩]