Contents
What is Chikungunya
Chikungunya virus is an alphavirus (genus Alphavirus, family Togaviridae) that is primarily transmitted to humans by Aedes mosquitoes (predominantly Aedes aegypti and Aedes albopictus), and occasionally from mother to child 1. The risk of a person transmitting the virus to a biting mosquito or through blood is highest when the patient is viremic, usually during the first 2–6 days of illness. Maternal-fetal transmission has been documented during pregnancy; the highest risk occurs when a woman is viremic at the time of delivery. Studies have not found virus in breast milk.
Chikungunya causes the sudden onset of fever and severe joint pain. Other signs and symptoms may include fatigue, muscle pain, headache, joint swelling and rash. Signs and symptoms of chikungunya usually appear within two to seven days after being bitten by an infected mosquito. However, Chikungunya runs a limited course and rarely causes serious complications. Treatment is aimed at relieving symptoms with rest, fluids and medications — such as acetaminophen (Tylenol, others) and ibuprofen (Advil, Motrin IB, others) — to relieve joint pain and fever. Chikungunya virus disease is a nationally notifiable condition. Healthcare providers are encouraged to report suspected chikungunya cases to their state or local health department to facilitate diagnosis and mitigate the risk of local transmission 2.
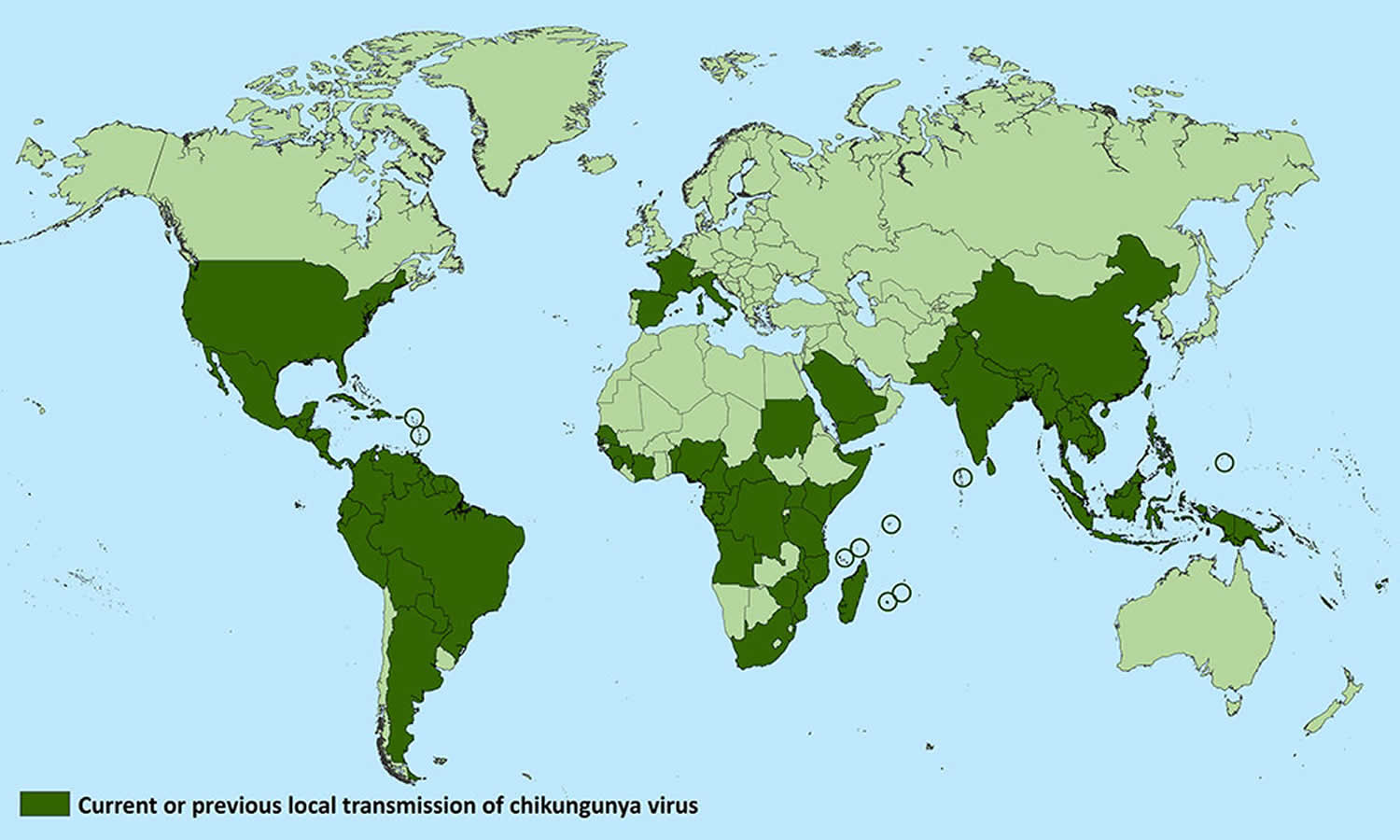
The word “chikungunya” originates from the Makonde language, spoken in Tanzania and Mozambique, meaning “that which bends up” 3; this refers to the debilitating arthralgia (joint pain) often occurring in the acute phase of infection, along with fever, myalgia (muscle pain), headache, joint swelling and rash. Although the first outbreaks were described in the 1960s, the virus was not considered a major public health problem until 2004, when it caused explosive outbreaks in the tropics 1. Prior to 2013, chikungunya virus cases and outbreaks had been identified in countries in Africa, Asia, Europe, and the Indian and Pacific Oceans. In late 2013, chikungunya virus was found for the first time in the Americas on islands in the Caribbean. By the end of 2014, more than 1.1 million suspect cases of chikungunya had been reported in the Americas 4. Since then the virus has continued to circulate and cause disease in the Americas, Southeast Asia, Pacific Islands, and Africa. There is a risk that the Chikungunya virus will be imported to new areas by infected travelers.
Risk to travelers is highest in areas experiencing ongoing epidemics of the disease (for the most updated information see the Travel Health Notices section on the Centers for Disease Control and Prevention (CDC) Travelers’ Health website at https://wwwnc.cdc.gov/travel/notices/). Most epidemics occur during the tropical rainy season and abate during the dry season. However, outbreaks in Africa have occurred after periods of drought, where open water containers in close proximity to human habitation served as vector-breeding sites. Risk of infection exists throughout the day, as the primary vector, Aedes aegypti, aggressively bites during the daytime. Aedes aegypti mosquitoes bite indoors or outdoors near a dwelling. They typically breed in domestic containers that hold water, including buckets and flower pots.
Both adults and children can become infected and symptomatic with the disease. From 2010 through 2013, 110 cases of chikungunya were identified or reported among US travelers who predominantly traveled to areas with known ongoing outbreaks. Following the outbreaks in the Americas, however, >3,500 chikungunya cases have been reported from US states through the end of April 2016. Although most were in travelers, a few cases acquired locally in the continental United States were reported in 2014 and 2015. In addition, several US territories (Puerto Rico, US Virgin Islands, and American Samoa) have reported locally acquired cases from 2014–2016.
Severe complications of chikungunya infection, including neurological disease, are being recognized increasingly 1. Chikungunya virus is now recognized as a cause of both arthritic and neurological diseases throughout the tropics.
There is no vaccine to prevent or no effective antiviral medicine to treat chikungunya virus infection. Travelers can protect themselves by preventing mosquito bites. When traveling to countries with chikungunya virus, use insect repellent, wear long sleeves and pants, and stay in places with air conditioning or that use window and door screens.
Treatment is supportive. Chikungunya infection treatment for acute supportive care include analgesics and antipyretics such as acetaminophen (Tylenol®) or paracetamol to reduce fever and pain. It is wise to avoid aspirin and NSAIDs until dengue fever has been excluded. For chronic arthralgias: nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids; chloroquine (Aralen) and hydroxychloroquine (Plaquenil) in refractory cases have been recommended 5.
Countries and territories where chikungunya cases have been reported
[Source 6]Chikungunya disease modes of transmission
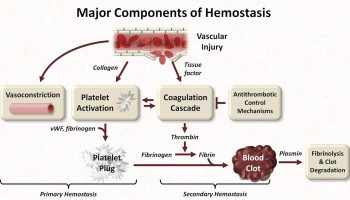
Chikungunya virus is primarily transmitted to humans through the bites of infected mosquitoes of the Aedes spp., predominantly Aedes aegypti and Aedes albopictus. Humans are the primary host of chikungunya virus during epidemic periods. Blood-borne transmission is possible; cases have been documented among laboratory personnel handling infected blood and a health care worker drawing blood from an infected patient. Rare in utero transmission has been documented mostly during the second trimester. Intrapartum transmission has also been documented when the mother was viremic around the time of delivery. Studies have not found chikungunya virus in breast milk and there have been no reports to date of infants acquiring chikungunya virus infection through breastfeeding. Because the benefits of breastfeeding likely outweigh the risk of chikungunya virus infection in breastfeeding infants, mothers should be encouraged to breastfeed even if they are infected with chikungunya virus or live in an area with ongoing virus transmission.
The risk of a person transmitting the virus to a biting mosquito or through blood is highest when the patient is viremic during the first week of illness.
Chikungunya virus is spread by infected mosquitoes, usually the Aedes albopictus (Figure 2) and Aedes aegypti (Figure 3) varieties.
Chikungunya virus are mainly transmitted by the bite of infected Aedes aegypti mosquitoes; an invasive, domestic species with tropical and subtropical worldwide distribution that originated in Africa.
Aedes albopictus, which is another invasive species originally from Asia.
These mosquitoes bite during the day, most often early in the morning or in the early evening before dusk.
They’re often found living around sources of stagnant water in built-up areas, such as wells, water storage tanks or old car tyres.
Through mosquito bites
- Chikungunya virus is transmitted to people through mosquito bites. Mosquitoes become infected when they feed on a person already infected with the virus. Infected mosquitoes can then spread the virus to other people through bites.
- Chikungunya virus is most often spread to people by Aedes aegypti and Aedes albopictus mosquitoes. These are the same mosquitoes that transmit dengue virus. They bite during the day and at night.
Rarely, from mother to child
- Chikungunya virus is transmitted rarely from mother to newborn around the time of birth.
- To date, no infants have been found to be infected with chikungunya virus through breastfeeding. Because of the benefits of breastfeeding, mothers are encouraged to breastfeed even in areas where chikungunya virus is circulating.
Rarely, through infected blood
- In theory, the virus could be spread through a blood transfusion. To date, there are no known reports of this happening.
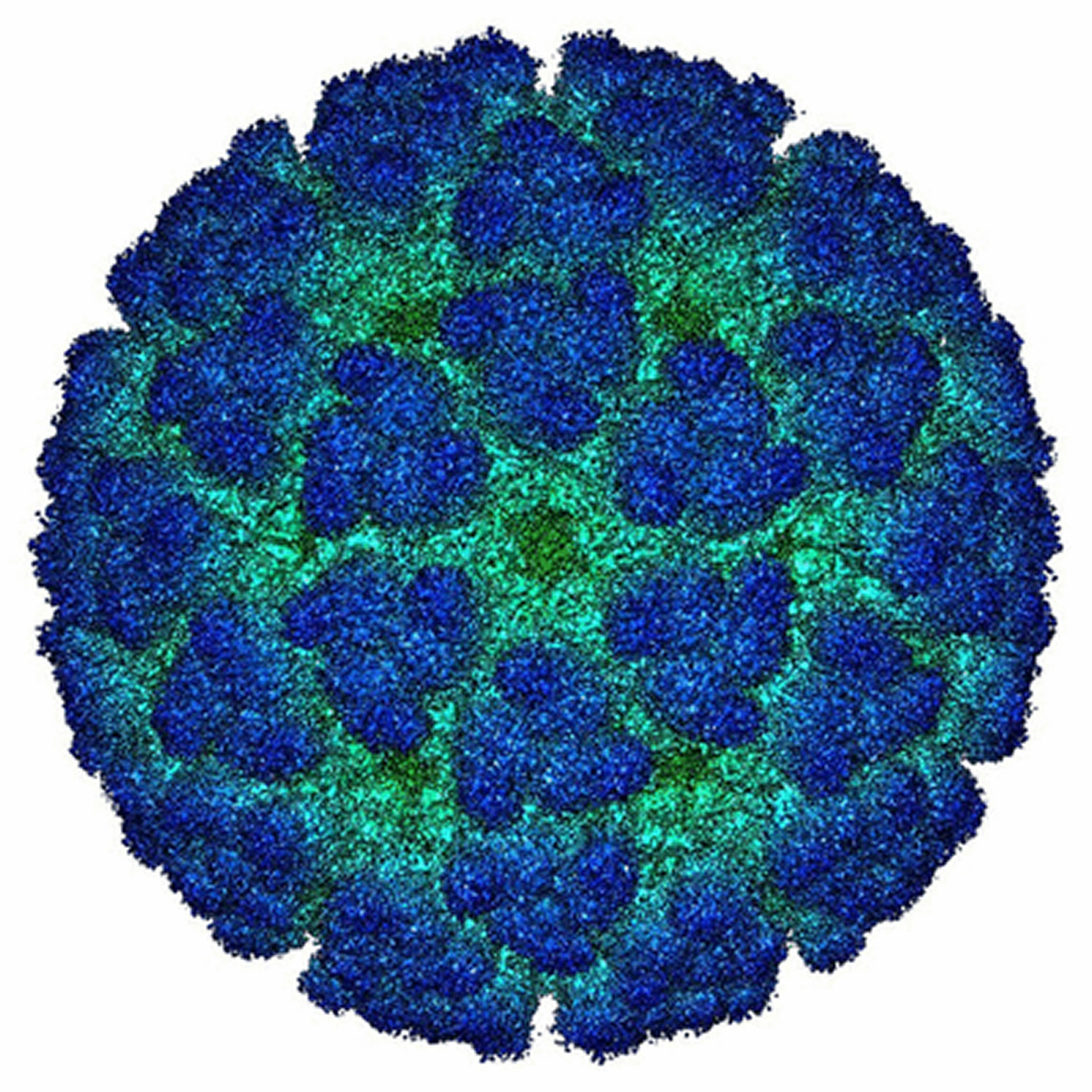
Figure 1. Chikungunya virus
[Source 7]Figure 2. Chikungunya mosquito (Aedes albopictus)
Figure 3. Chikungunya mosquito (Aedes aegypti)
There is no widely vaccine available against chikungunya virus and there are no specific medications to treat a chikungunya virus infection. This makes prevention the most important step, and prevention means avoiding mosquito bites if you live in or travel to an endemic area.
Reduce mosquito habitat. The mosquitoes that carry the chikungunya virus typically live in and around houses, breeding in standing water that can collect in such things as used automobile tires. You can help lower mosquito populations by eliminating habitats where they lay their eggs. At least once a week, empty and clean containers that hold standing water, such as planting containers, animal dishes and flower vases. Keep standing water containers covered between cleanings.
The best way to reduce mosquitoes is to eliminate the places where the mosquito lays her eggs, like artificial containers that hold water in and around the home. Outdoors, clean water containers like pet and animal watering containers, flower planter dishes or cover water storage barrels. Look for standing water indoors such as in vases with fresh flowers and clean at least once a week.
The adult mosquitoes like to bite inside as well as around homes, during the day and at night when the lights are on. To protect yourself, use repellent on your skin while indoors or out. When possible, wear long sleeves and pants for additional protection. Also, make sure window and door screens are secure and without holes. If available, use air-conditioning.
If someone in your house is ill with chikungunya virus, take extra precautions to prevent mosquitoes from biting the patient and going on to bite others in the household. Sleep under a mosquito bed net, eliminate mosquitoes you find indoors and wear repellent!
List of repellant products approved by the EPA : https://www.epa.gov/insect-repellents/find-repellent-right-you
The following can reduce your risk of being bitten:
- use insect repellent – products containing 50% DEET are most effective, but lower concentrations (15-30% DEET) should be used in children, and alternatives to DEET should be used in children younger than two months
- wear loose but protective clothing – mosquitoes can bite through tight-fitting clothes; trousers, long-sleeved shirts, and socks and shoes (not sandals) are ideal
- sleep under a mosquito net – ideally one that has been treated with insecticide
- be aware of your environment – mosquitoes that spread chikungunya virus breed in standing water in urban areas
- stay in air-conditioned or well-screened housing. The mosquitoes that carry the chikungunya virus are most active from dawn to dusk, but they can also bite at night.
It’s a good idea to speak to your doctor, practice nurse or a travel clinic before traveling to get specific advice about what you can do to avoid chikungunya virus and other travel illnesses.
Travelers at increased risk for more severe disease, including travelers with underlying medical conditions and women who are late in their pregnancy (as their unborn infants are at increased risk), may consider avoiding travel to areas with ongoing outbreaks. If travel is unavoidable, emphasize the need for protective measures against mosquito bites.
Chikungunya symptoms
The majority of people infected with chikungunya virus become symptomatic. The incubation period is typically 3–7 days (range, 1–12 days). The disease is most often characterized by acute onset of fever (typically >39°C [102°F]) and polyarthralgia. Joint symptoms are usually bilateral and symmetric, and can be severe and debilitating. Other symptoms may include headache, myalgia, arthritis, conjunctivitis, nausea/vomiting, or maculopapular rash.
Acute symptoms typically resolve within 7–10 days. Rare complications include uveitis, retinitis, myocarditis, hepatitis, nephritis, bullous skin lesions, hemorrhage, meningoencephalitis, myelitis, Guillain-Barré syndrome, and cranial nerve palsies. Persons at risk for severe disease include neonates exposed intrapartum, older adults (e.g., > 65 years), and persons with underlying medical conditions (e.g., hypertension, diabetes, or cardiovascular disease). Some patients might have relapse of rheumatologic symptoms (e.g., polyarthralgia, polyarthritis, tenosynovitis) in the months following acute illness. Studies report variable proportions of patients with persistent joint pains for months to years. Mortality is rare and occurs mostly in older adults.
Chikungunya virus symptoms:
- Most people infected with chikungunya virus will develop some symptoms.
- Symptoms usually begin 3–7 days after being bitten by an infected mosquito.
- The most common symptoms are fever and joint pain (especially in small joints).
- Other symptoms may include headache, muscle pain, joint swelling, or rash.
- Chikungunya disease does not often result in death, but the symptoms can be severe and disabling.
- Most patients feel better within a week. In some people, the joint pain may persist for months.
- People at risk for more severe disease include newborns infected around the time of birth, older adults (≥65 years), and people with medical conditions
- such as high blood pressure, diabetes, or heart disease.
- Once a person has been infected, he or she is likely to be protected from future infections.
The symptoms of chikungunya are similar to those of dengue and Zika, diseases spread by the same mosquitoes that transmit chikungunya.
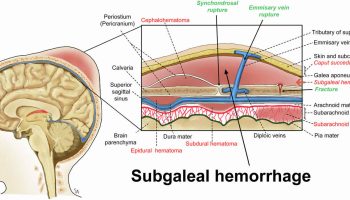
Pregnant women have symptoms and outcomes similar to those of other people, and most chikungunya virus infections that occur during pregnancy will not result in the virus being transmitted to the fetus. However, when intrapartum transmission occurs, it can result in complications for the baby, including neurologic disease, hemorrhagic symptoms, and myocardial disease 4. There are also rare reports of spontaneous abortions after maternal infection during the first trimester.
See your healthcare provider if you develop the symptoms described above and have visited an area where chikungunya is found.
If you have recently traveled, tell your healthcare provider when and where you traveled.
Your healthcare provider may order blood tests to look for chikungunya or other similar viruses like dengue and Zika.
Chikungunya neuronal complications
In chikungunya‐associated neurological disease, the clinician must be vigilant for other complications in the same patient, a pattern also described in dengue but rarely in Zika infection. Amongst 99 cases of chikungunya‐associated neurological disease described in a study in India, 69 also had other complications involving, for example, the renal, hepatic, and respiratory systems 8. These patients should be managed using a multidisciplinary approach.
Table 1. List of neurological syndromes and syndromes and diseases associated with chikungunya virus
| Described More Frequently | Described Less Frequently |
|---|---|
| Encephalopathy and encephalitis | Seizures with or without fever |
| Myelopathy and myelitis | Behavioural changes |
| Encephalomyelopathy | Sensorineural hearing loss |
| Myeloneuropathy | Stroke |
| Encephalomyeloneuropathy | Cerebellitis |
| Guillain‐Barré syndrome | Meningism |
| Acute disseminated encephalomyelitis | Third nerve palsy |
| Neonatal hypotonia | Encephaloneuropathy |
| Neuro‐ocular disease (uveitis, retinitis, optic neuritis) | Carpal tunnel syndrome |
| Bilateral total ophthalmoplegia | |
| Mild encephalitis with a reversible lesion of the splenium | |
| Bickerstaff brainstem encephalitis–Miller Fisher syndrome–Guillain‐Barré syndrome overlap |
Adults and Children (Transmission Directly Via Mosquito Bite)
Encephalitis is the most commonly reported neurological complication associated with chikungunya; encephalitis has a worse prognosis than encephalopathy alone; a CSF pleocytosis is not always seen.
In myelitis associated with chikungunya, CSF pleocytosis and magnetic resonance imaging changes are not always seen.
Guillain‐Barré syndrome associated with chikungunya follows a similar course compared with other infections such as Campylobacter jejuni; most patients recover after immunomodulatory treatment.
Disease of both the central and peripheral nervous systems in the same patient can be seen in association with chikungunya infection.
Ophthalmological complications associated with chikungunya have been reported both at the time of infection and up to 12 wk after; some reports describe treating with steroids, recovery is variable.
Neonates (Mothers to Babies Transmission)
Neonates born to mothers experiencing symptoms of chikungunya infection near the time of delivery require admission and observation for signs of vertical transmission for at least 7 d postpartum, as they may be asymptomatic for the first few days of life.
Neonates born to mothers infected outside of the peripartum period are usually unaffected by chikungunya virus.
Caesarean section does not appear to be protective in vertical transmission of chikungunya.
Neonates infected with chikungunya should be followed up for at least 2 years, regardless of symptoms in the first week of life; the neurodevelopment of those without clinical encephalopathy at birth can still be affected.
Chikungunya diagnosis
Chikungunya virus infection should be considered in patients with acute onset of fever and polyarthralgia, especially travelers who recently returned from areas with known virus transmission. Preliminary diagnosis is based on the patient’s clinical features, places and dates of travel, and activities.
The differential diagnosis of chikungunya virus infection varies based on place of residence, travel history, and exposures. Dengue and chikungunya viruses are transmitted by the same mosquitoes and have similar clinical features. The two viruses can circulate in the same area and can cause occasional co-infections in the same patient. Chikungunya virus infection is more likely to cause high fever, severe arthralgia, arthritis, rash, and lymphopenia, while dengue virus infection is more likely to cause neutropenia, thrombocytopenia, hemorrhage, shock, and death. It is important to rule out dengue virus infection because proper clinical management of dengue can improve outcome.
Clinical laboratory findings can include lymphopenia, thrombocytopenia, elevated creatinine, and elevated hepatic transaminases.
Laboratory diagnosis is generally accomplished by testing serum or plasma to detect virus, viral nucleic acid, or virus-specific immunoglobulin M (IgM) and neutralizing antibodies. Viral culture may detect virus in the first 3 days of illness; however, chikungunya virus should be handled under biosafety level (BSL) 3 conditions. During the first 8 days of illness, chikungunya viral RNA can often be identified in serum. Chikungunya virus antibodies normally develop toward the end of the first week of illness. Therefore, to definitively rule out the diagnosis, convalescent-phase samples should be obtained from patients whose acute-phase samples test negative.
Laboratory testing
Contact your state health department or the the Centers for Disease Control and Prevention (CDC) for more information and to facilitate testing.
- Chikungunya testing is performed at CDC, several state health departments, and one commercial laboratory
- Contact your state health department for more information and to facilitate testing
Evaluate serum or plasma by:
- Viral culture to detect virus in first 3 days of illness
- RT-PCR to detect viral RNA in first 8 days of illness
- Serology to detect IgM, IgG, and neutralizing antibodies that develop toward the end of the first week of illness (≥4 days post illness onset)
Test results are normally available 4 to 14 days after specimen receipt. Reporting times for test results may be longer during summer months when arbovirus activity increases. Receipt of a hard copy of the results will take at least 2 weeks after testing is completed. Initial serological testing will be performed using IgM-capture ELISA and IgG ELISA. If the initial results are positive, further confirmatory testing will be performed and it may delay the reporting of final results. ALL RESULTS WILL BE SENT TO THE APPROPRIATE STATE HEALTH DEPARTMENT. Notify your state health department of any direct submissions to CDC.
Chikungunya treatment
There is no vaccine to prevent or medicine to treat chikungunya virus.
Treat the chikungunya symptoms:
- Get plenty of rest.
- Drink fluids to prevent dehydration.
- Take medicine such as acetaminophen (Tylenol®) or paracetamol to reduce fever and pain.
- Do not take aspirin and other non-steroidal anti-inflammatory drugs (NSAIDS until dengue can be ruled out to reduce the risk of bleeding).
- If you are taking medicine for another medical condition, talk to your healthcare provider before taking additional medication.
If you have chikungunya, prevent mosquito bites for the first week of your illness
- During the first week of infection, chikungunya virus can be found in the blood and passed from an infected person to a mosquito through mosquito bites.
- An infected mosquito can then spread the virus to other people.
- Mehta R, Gerardin P, de Brito CAA, Soares CN, Ferreira MLB, Solomon T. The neurological complications of chikungunya virus: A systematic review. Reviews in Medical Virology. 2018;28(3):e1978. doi:10.1002/rmv.1978. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5969245/[↩][↩][↩][↩]
- Chikungunya Virus. https://www.cdc.gov/chikungunya/index.html[↩]
- Robinson MC. An epidemic of virus disease in Southern Province, Tanganyika Territory, in 1952‐53. I. Clinical features. Trans R Soc Trop Med Hyg. 1955;49(1):28‐32.[↩]
- Chikungunya. Chapter 3 – Infectious Diseases Related to Travel. https://wwwnc.cdc.gov/travel/yellowbook/2018/infectious-diseases-related-to-travel/chikungunya[↩][↩]
- World Health Organization. Guidelines on clinical management of chikungunya fever. October 2008. http://www.wpro.who.int/mvp/topics/ntd/Clinical_Mgnt_Chikungunya_WHO_SEARO.pdf[↩]
- Chikungunya Virus Geographic Distribution. https://www.cdc.gov/chikungunya/geo/[↩]
- Chikungunya Virus. https://microbewiki.kenyon.edu/index.php/Chikungunya_Virus[↩]
- Tandale BV, Sathe PS, Arankalle VA, et al. Systemic involvements and fatalities during chikungunya epidemic in India, 2006. J Clin Virol. 2009;46(2):145‐149.[↩]