Contents
- What is syphilis
- How is syphilis spread?
- What is the treatment for syphilis?
- Is syphilis curable?
- Will syphilis recur?
- How common is syphilis?
- Who should be tested for syphilis?
- How can I reduce my risk of getting syphilis?
- Am I at risk for syphilis?
- I’ve been treated. Can I get syphilis again?
- I’m pregnant. How does syphilis affect my baby?
- What causes syphilis?
- Syphilis stages
- Syphilis signs and symptoms
- Syphilis diagnosis
- Syphilis treatment
- Penicillin Allergy
What is syphilis
Syphilis is a complex sexually transmitted disease (STD) or sexually transmitted infection (STI) caused by the bacteria Treponema pallidum. Syphilis can cause serious health problems if not adequately treated. Episodes of active disease occur, followed by latent periods, when the person remains infected but there are no signs or symptoms. Syphilis is transmitted from person to person by direct contact with a syphilitic sore, known as a chancre 1. Chancres can occur on or around the external genitals, in the vagina, around the anus or in the rectum, or in or around the mouth. Transmission of syphilis can occur during vaginal, anal, or oral sex. In addition, pregnant women with syphilis can transmit the infection to their unborn children.
The average time between acquisition of syphilis and the start of the first symptom is 21 days, but can range from 10 to 90 days.
Some people with syphilis have no symptoms, so you may not know you have it unless you get tested. The signs and symptoms of syphilis depend on the stage of disease. There are 4 stages of syphilis infection: primary, secondary, latent and tertiary.
Primary syphilis appears as a painless sore (ulcer) where the infection entered your body (usually around the penis, vagina, cervix, anus or mouth) and may go unnoticed. The sore is known as a chancre and this phase is known as primary syphilis. There may also be swollen lymph nodes.
Primary syphilis occurs 3 or 4 weeks after infection (although it can take up to 90 days for the sore to appear).
The sore, or sometimes multiple sores, can go unnoticed because it is usually painless and may be hidden from view in areas such as the back of the throat, vagina or anus.
These sores usually go away by themselves after 3 to 6 weeks, even with no treatment. However, even though the sore heals, if you haven’t been treated, you are still infectious and can pass it on to others.
Secondary syphilis can occur 7 to 10 weeks after the initial infection. Symptoms can last for 6 months or more and may include:
- a red rash on the palms, soles, chest or back
- fever
- enlarged glands in the armpits and groin
- sore throat
- hair loss
- weight loss
- headaches
- pain in the bones, muscles and joints
- tiredness
- ulcers in the mouth, nasal cavity or genitals
- neurological symptoms
After the initial infection, the syphilis bacteria, Treponema pallidum, can remain inactive in your body for decades before becoming active again, this is known as the latent (sleeping) syphilis stage. Generally the person with latent stage syphilis has no symptoms and it is only picked up on blood tests. If syphilis is not treated at this stage, it can remain latent or develop into tertiary syphilis. Latent syphilis is infectious within the first 12 to 24 months.
If the latent stage syphilis is left untreated, tertiary syphilis may develop 5 to 20 years after the primary infection. At the tertiary syphilis stage, the bacteria can damage almost any part of your body including your heart, brain, spinal cord, eyes and bones, resulting in heart disease, mental illness, blindness, deafness and neurological problems and can be life-threatening
Early syphilis can be cured, sometimes with a single shot (injection) of penicillin. If you’re allergic to penicillin, your doctor may suggest another antibiotic or recommend penicillin desensitization.
After you’ve been treated for syphilis, your doctor will ask you to:
- Have periodic blood tests and exams to make sure you’re responding to the usual dosage of penicillin. Your specific follow-up will depend on the stage of syphilis you’re diagnosed with.
- Avoid sexual contact with new partners until the treatment is completed and blood tests indicate the infection has been cured.
- Notify your sex partners so that they can be tested and get treatment if necessary.
- Be tested for HIV infection.
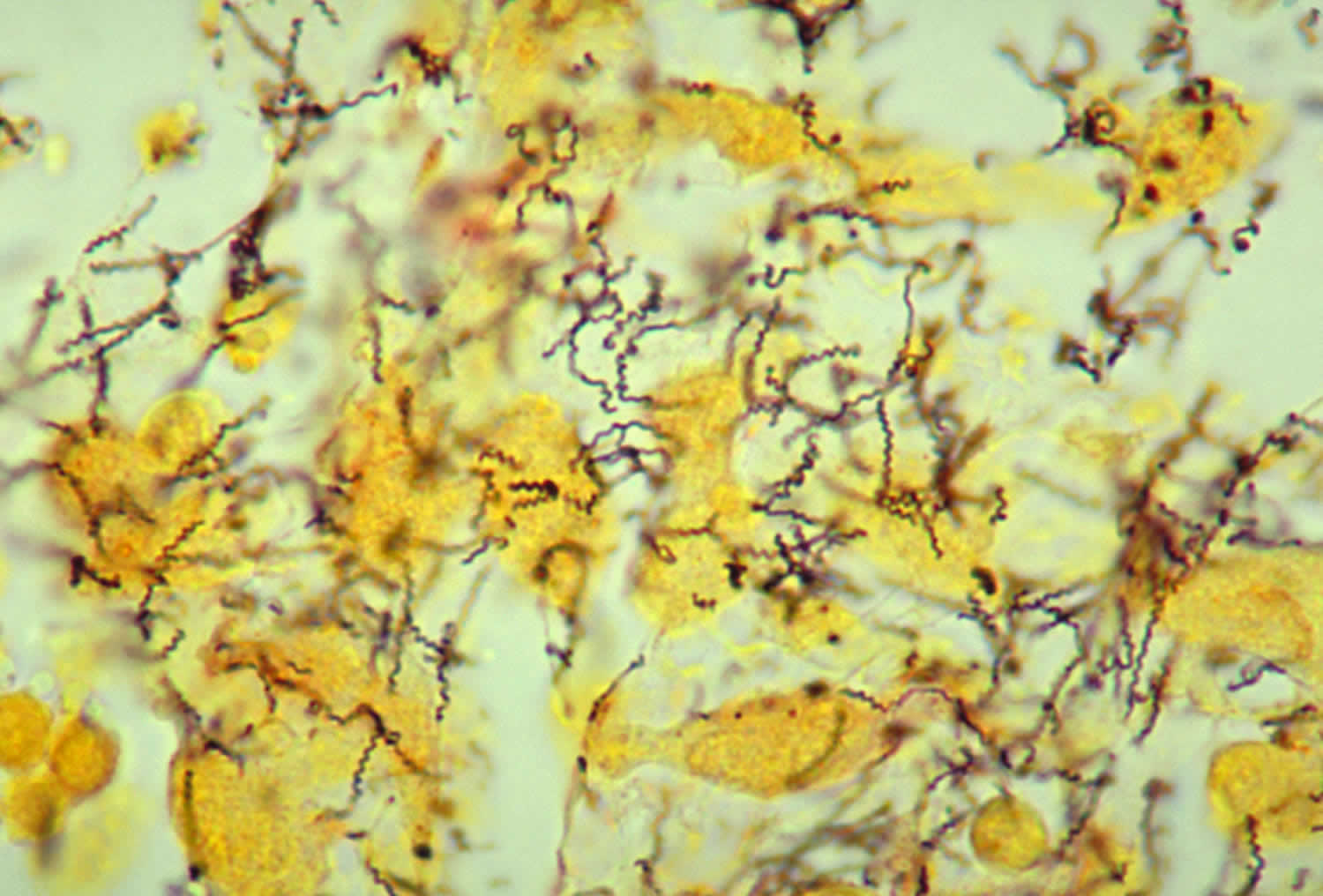
Figure 1. Treponema pallidum bacteria
Footnote: This photomicrograph depicted a tissue sample, which had been prepared using the Steiner silver stain method. The image revealed the presence of numerous, corkscrew-shaped, darkly-stained, Treponema pallidum spirochetes. Treponema pallidum is the bacterium responsible for causing syphilis.
[Source 2 ]Figure 2. Treponema pallidum bacteria
[Source 3 ]See your doctor if you or your child experiences any unusual discharge, sore or rash — particularly if it occurs in the groin area.
How is syphilis spread?
You can get syphilis by direct contact with a syphilis sore during vaginal, anal, or oral sex. Syphilis can also spread from a mother with syphilis to her unborn baby.
You cannot get syphilis through casual contact with objects, such as:
- toilet seats
- doorknobs
- swimming pools
- hot tubs
- bathtubs
- sharing clothing, or eating utensils
What is the treatment for syphilis?
There are no home remedies or over-the-counter drugs that will cure syphilis, but syphilis is easy to cure in its early stages. A single intramuscular injection of long acting Benzathine penicillin G (2.4 million units administered intramuscularly) will cure a person who has primary, secondary or early latent syphilis. Three doses of long acting Benzathine penicillin G (2.4 million units administered intramuscularly) at weekly intervals is recommended for individuals with late latent syphilis or latent syphilis of unknown duration. Treatment will kill the syphilis bacterium and prevent further damage, but it will not repair damage already done.
Selection of the appropriate penicillin preparation is important to properly treat and cure syphilis. Combinations of some penicillin preparations (e.g., Bicillin C-R, a combination of benzathine penicillin and procaine penicillin) are not appropriate treatments for syphilis, as these combinations provide inadequate doses of penicillin.
Although data to support the use of alternatives to penicillin is limited, options for non-pregnant patients who are allergic to penicillin may include doxycycline, tetracycline, and for neurosyphilis, ceftriaxone. These therapies should be used only in conjunction with close clinical and laboratory follow-up to ensure appropriate serological response and cure.
Persons who receive syphilis treatment must abstain from sexual contact with new partners until the syphilis sores are completely healed. Persons with syphilis must notify their sex partners so that they also can be tested and receive treatment if necessary.
Is syphilis curable?
Yes, syphilis can be cured with the right antibiotics from your health care provider. However, treatment might not undo any damage that the infection has already done.
Will syphilis recur?
After appropriate treatment, syphilis does not recur. However, having syphilis once does not protect a person from becoming infected again. Even following successful treatment, people can be reinfected. Patients with signs or symptoms that persist or recur or who have a sustained fourfold increase in nontreponemal test titer probably failed treatment or were reinfected. These patients should be retreated.
Because chancres can be hidden in the vagina, rectum, or mouth, it may not be obvious that a sex partner has syphilis. Unless a person knows that their sex partners have been tested and treated, they may be at risk of being reinfected by an untreated partner.
How common is syphilis?
During 2016, there were 88,042 reported new diagnoses of syphilis (all stages), compared to 39,513 estimated new diagnoses of HIV infection in 2015 and 468,514 cases of gonorrhea in 2016 4. Of syphilis cases, 27,814 were primary and secondary syphilis, the earliest and most transmissible stages of syphilis. In 2016, the majority of primary and secondary syphilis cases occurred among gay, bisexual, and other men who have sex with men. In 2016, men who have sex with men accounted for 80.6% of all primary and secondary syphilis cases among males in which sex of sex partner was known and 58% of all P&S syphilis cases overall. However, in recent years, the rate of primary and secondary syphilis has been increasing among men who have sex with men as well as heterosexual men and women.
Congenital syphilis (syphilis passed from pregnant women to their babies) continues to be a concern in the United States. During 2016, 628 cases of congenital syphilis were reported, compared to an estimated 86 cases of perinatal HIV infection during 2015. 1 In 2016, congenital syphilis rates were 8.0 times and 3.9 times higher among infants born to black and Hispanic mothers (43.1 and 20.5 cases per 100,000 live births, respectively) compared to white mothers (5.3 cases per 100,000 live births).
Who should be tested for syphilis?
Any person with signs or symptoms suggestive of syphilis should be tested for syphilis. Also, anyone with an oral, anal, or vaginal sex partner who has been recently diagnosed with syphilis should be tested for syphilis.
Some people should be tested (screened) for syphilis even if they do not have symptoms or know of a sex partner who has syphilis. Anyone who is sexually active should discuss his or her risk factors with a health care provider and ask whether he or she should be tested for syphilis or other STDs.
In addition, providers should routinely test for syphilis in persons who:
- are pregnant;
- are sexually active men who have sex with men (MSM);
- are living with HIV and are sexually active;
- are taking PrEP for HIV prevention.
How can I reduce my risk of getting syphilis?
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting syphilis:
- Being in a long-term mutually monogamous relationship with a partner who has been tested for syphilis and does not have syphilis;
- Using latex condoms the right way every time you have sex. Condoms prevent transmission of syphilis by preventing contact with a sore. Sometimes sores occur in areas not covered by a condom. Contact with these sores can still transmit syphilis.
Am I at risk for syphilis?
Any sexually active person can get syphilis through unprotected vaginal, anal, or oral sex. Have an honest and open talk with your health care provider and ask whether you should be tested for syphilis or other STDs.
- All pregnant women should be tested for syphilis at their first prenatal visit.
- You should get tested regularly for syphilis if you are sexually active and
- are a man who has sex with men;
- are living with HIV; or
- have partner(s) who have tested positive for syphilis.
I’ve been treated. Can I get syphilis again?
Having syphilis once does not protect you from getting it again. Even after you’ve been successfully treated, you can still be re-infected. Only laboratory tests can confirm whether you have syphilis. Follow-up testing by your health care provider is recommended to make sure that your treatment was successful.
It may not be obvious that a sex partner has syphilis. This is because syphilis sores can be hidden in the vagina, anus, under the foreskin of the penis, or in the mouth. Unless you know that your sex partner(s) has been tested and treated, you may be at risk of getting syphilis again from an infected sex partner.
I’m pregnant. How does syphilis affect my baby?
If you are pregnant and have syphilis, you can give the infection to your unborn baby. Having syphilis can lead to a low birth weight baby. It can also make it more likely you will deliver your baby too early or stillborn (a baby born dead) or of giving birth to a baby who dies shortly after birth. Untreated syphilis in pregnant women results in infant death in up to 40 percent of cases. To protect your baby, you should be tested for syphilis at least once during your pregnancy. Receive immediate treatment if you test positive.
An infected baby born alive may not have any signs or symptoms of disease. However, if not treated immediately, the baby may develop serious problems within a few weeks. Untreated babies may become developmentally delayed and can have health problems such as cataracts, deafness, or seizures, and can die. All babies born to mothers who test positive for syphilis during pregnancy should be screened for syphilis and examined thoroughly for evidence of congenital syphilis 5.
All pregnant women should be tested for syphilis at the first prenatal visit. For women who are at high risk for syphilis, live in areas of high syphilis morbidity, are previously untested, or had a positive screening test in the first trimester, the syphilis screening test should be repeated during the third trimester (28 to 32 weeks gestation) and again at delivery 5. Any woman who delivers a stillborn infant after 20 week’s gestation should also be tested for syphilis.
For pregnant women only penicillin therapy can be used to treat syphilis and prevent passing the disease to her baby; treatment with penicillin is extremely effective (success rate of 98%) in preventing mother-to-child transmission 6. Pregnant women who are allergic to penicillin should be referred to a specialist for desensitization to penicillin.
What causes syphilis?
Syphilis is caused by bacteria called Treponema pallidum (Figures 1 and 2). You can get syphilis by having sex with an infected person (coming into direct contact with a syphilis sore). It can also be passed from an infected mother to her baby during pregnancy.
Syphilis stages
Syphilis is divided into 4 stages: primary, secondary, latent, and tertiary. The signs and symptoms of syphilis depend on the stage of disease. A person with primary syphilis generally has a sore or sores at the original site of infection. These sores usually occur on or around the genitals, around the anus or in the rectum, or in or around the mouth. These sores are usually (but not always) firm, round, and painless. Symptoms of secondary syphilis include skin rash, swollen lymph nodes, and fever. The signs and symptoms of primary and secondary syphilis can be mild, and they might not be noticed. During the latent stage, there are no signs or symptoms. Tertiary syphilis is associated with severe medical problems. A doctor can usually diagnose tertiary syphilis with the help of multiple tests. It can affect the heart, brain, and other organs of the body.
Primary syphilis
During the first (primary) stage of syphilis, you may notice a single sore called chancre or multiple sores. The sore (chancre) is the location where syphilis entered your body. The chancres are usually (but not always) firm, round, and painless. Because the sore is painless, it can easily go unnoticed. These painless chancres can occur in locations that make them difficult to notice (e.g., the vagina or anus). The sore usually lasts 3 to 6 weeks and heals regardless of whether or not you receive treatment. Even after the sore goes away, you must still receive treatment. This will stop your infection from moving to the secondary stage. However, if the infected person does not receive adequate treatment, the infection progresses to the secondary stage.
- Single small firm red painless papule quickly ulcerates (chancre). Heals within 4-8 weeks without treatment, and within 1 to 2 weeks with appropriate treatment. Sores may be inside the vagina or anus and often go unnoticed.
- Unilateral enlargement of lymph nodes close to the ulcer develops about 5 weeks after acquiring infection. Inguinal lymphadenopathy arises in men with ulcers on the genitals and cervical lymphadenopathy in patients with ulcers in the mouth. If a syphilis ulcer is located in the vagina or rectum, the lymphadenopathy can be only detected by pelvic ultrasound examination.
Figure 3. Primary syphilis in men (syphilis chancre)
Figure 4. Primary syphilis in women (syphilis chancre)
Figure 5. Syphilis chancre
Secondary syphilis
During the secondary stage, you may have skin rashes and/or mucous membrane lesions. Mucous membrane lesions are sores in your mouth, vagina, or anus. This stage usually starts with a rash on one or more areas of your body. The rash can show up when your primary sore is healing or several weeks after the sore has healed. The rash can look like rough, red, or reddish brown spots on the palms of your hands and/or the bottoms of your feet. The rash usually won’t itch and it is sometimes so faint that you won’t notice it. Other symptoms you may have can include fever, swollen lymph glands, sore throat, patchy hair loss, headaches, weight loss, muscle aches, and fatigue (feeling very tired). The symptoms from this stage will go away whether or not you receive treatment. Without the right treatment, your infection will move to the latent and possibly tertiary stages of syphilis.
- Patient is very infectious during this stage.
- If left untreated or treatment has failed, about 3 weeks to 3 months after the 1st stage, a widespread skin rash occurs.
- Rash may be subtle or appear as rough, red or reddish brown papules or patches. Occurs typically on the trunk and frequently affects palms and soles. May be mistaken for other conditions. The rash does not itch. It can appear more obvious with physical activity or heat. It resolves spontaneously within several weeks but can recur during the following 2 years.
- Corymbose syphilis describes a cluster of erythematous papules around a central scaly plaque (resembling a flower).
- Patchy hair loss.
- Raw and red mucosal surfaces such as inside the mouth, throat, genital area, vagina and anus (mucous patches).
- Unilateral tonsilitis, which may be ulcerated and accompanied by cervical lymph node enlargement. Can be mistaken for common tonsilitis but does not respond to usual oral antibiotics.
- Greyish-white moist raised patches in the groin, inner thighs, armpits, umbilicus, or under breasts (condyloma lata).
- Other symptoms include fever, tiredness, muscle and joint pains, headache and swollen lymph glands.
- Other affected organs may include liver, kidneys, central nervous system (CNS), joints and eyes (resulting in visual impairment).
Figure 6. Secondary syphilis (hands rash – subtle rough, red or reddish brown papules or patches)
Figure 7. Secondary syphilis (foot rash – subtle rough, red or reddish brown papules or patches)
Figure 8. Condyloma lata gluteal fold (secondary syphilis)
Figure 9. Condyloma lata of umbilicus (secondary syphilis)
Latent syphilis
The latent (hidden) stage of syphilis is a period of time when there are no visible signs or symptoms of syphilis. Without treatment, the infected person will continue to have syphilis in their body even though there are no signs or symptoms. Early latent syphilis is latent syphilis where infection occurred within the past 12 months. Late latent syphilis is latent syphilis where infection occurred more than 12 months ago. Latent syphilis can last for years.
Early latent syphilis (first 2 years)
- Patient is infectious and can pass the infection on to partner.
- Usually normal,i.e. no signs on clinical examination.
- Continued infection found by positive treponemal antibody tests.
Late latent syphilis (after 2 years)
- Patient is non-infectious.
- Usually normal,i.e. no signs on clinical examination.
- Continued infection found by positive treponemal antibody tests
Tertiary syphilis
Most people with untreated syphilis do not develop tertiary syphilis. However, when it does happen it can affect many different organ systems. These include the heart and blood vessels, and the brain and nervous system. Tertiary syphilis is very serious and would occur 10–30 years after your infection began. In tertiary syphilis, the disease damages your internal organs and can result in death.
- Signs and symptoms may develop 3 to 10 years after initial infection, and corresponds with immunological response to the infection. Tertiary syphilis is very rare in developed countries.
- Solitary granulomatous lesions (gummas) may be found on the skin, in the mouth and throat or occur in bones. Small or large nodules or ulcers may persist for years. Skin lesions may be painless but gummas in long bones cause a deep boring pain that is worse at night.
- Brain involvement (neurosyphilis) may cause headaches, dizziness, blurred vision, mental disturbances, paralysis and dementia (general paresis). This occurs 10–30 years after infection.
- Spinal cord disease results in unsteady gait, bladder disturbance, impotence and sensory changes (tabes dorsalis) resulting in collapsed joints (Charcot’s joints) and foot ulcers.
- Other internal organs such as the heart, blood vessels, eyes, liver and blood may be damaged by infection.
Figure 10. Tertiary syphilis
Neurosyphilis and Ocular Syphilis
Without treatment, syphilis can spread to the brain and nervous system (neurosyphilis) or to the eye (ocular syphilis) or ear (otosyphilis). This can happen during any of the stages described above.
Symptoms of neurosyphilis include:
- severe headache;
- difficulty coordinating muscle movements;
- paralysis (not able to move certain parts of your body);
- numbness; and
- dementia (mental disorder).
Symptoms of ocular syphilis include changes in your vision and even blindness.
Congenital syphilis
- Congenital syphilis can be prevented by treatment prior to 16 weeks gestation.
- The risk to the fetus is greatest with early untreated maternal syphilis
- Miscarriage or stillbirth may occur.
- In the first few weeks of life, effects resemble secondary syphilis including blisters, scaly rash, mucous patches and condyloma latum (very infectious).
- Snuffles, inflamed bones, swollen liver and lymph glands are common.
- Blood changes include anemia, reduced platelets, and increased white cells.
- Late congenital syphilis often affects eyes (interstitial keratitis), ears, joints and CNS.
- Characteristic signs include Hutchinson’s teeth, typical facial appearance and bowed sabre shins.
Figure 11. Congenital syphilis
Figure 12. Congenital syphilis – Hutchinson’s teeth
Syphilis signs and symptoms
The signs and symptoms of syphilis depend on the stage of disease. The symptoms of syphilis are similar for men and women. Syphilis has been called “The Great Pretender”, as its symptoms can look like many other diseases. They’re often mild and difficult to recognize, so you may pass on the infection without knowing you have it.
Some people with syphilis have no symptoms.
The symptoms also tend to change over time and may come and go.
Symptoms can include:
- small, painless sores or ulcers that typically appear on the penis, vagina, or around the anus, but can occur in other places such as the mouth
- a blotchy red rash that often affects the palms of the hands or soles of the feet
- small skin growths (similar to genital warts) that may develop on the vulva in women or around the anus in both men and women
- white patches in the mouth
- tiredness, headaches, joint pains, a high temperature (fever), and swollen glands in your neck, groin or armpits
However, syphilis typically follows a progression of stages that can last for weeks, months, or even years.
Once infected there is an incubation period of anywhere from 10 to 90 days (on average 21 days) before any signs become apparent.
Initially, the first stage of syphilis or primary syphilis, a dusky red flat spot appears at the site of inoculation and is easily missed. Then, a painless ulcer (chancre) appears 18–21 days after initial infection. Genital sites in women affected are the cervix, vagina, vulva, and clitoris. Cervical and vaginal syphilis infections may not be recognized. In men, the chancre is easily seen on the penis. Other locations of infection are limited only by human ingenuity and imagination. Common sites are around the mouth (perioral) and between the buttocks (perianal) areas.
Chancres vary in size from a few millimeters to several centimeters. A chancre is usually painless, solitary, and shallow, with a sharp border and raised, hard edge. About 70–80% of patients have rubbery, non-tender, swollen lymph nodes, often on only one side of the groin, during the first week of infection.
If untreated, the chancre will remain present for 1 to 6 weeks. If treated, it heals without scarring in 1–2 weeks.
If you don’t treat syphilis early, it spreads from the sore into your blood. When syphilis gets into your blood, it can move into the secondary stage (secondary syphilis) and cause many problems. The most common sign is a rash. The rash is usually reddish-brown and can occur anywhere on the body (even on the palms of the hands and the soles of the feet). The rash appears 2 to 10 weeks after the appearance of the sores. Other signs of secondary syphilis include fever, swollen lymph nodes, sore throat, body aches, sores in the mouth, and fatigue.
After recovering from the secondary stage of syphilis, the disease can move into the latent stage (latent syphilis). Latent syphilis produces no symptoms, but the infection is still present in your body. Latent syphilis is infectious within the first 12 to 24 months. Generally the person with latent stage syphilis has no symptoms and it is only picked up on blood tests. If syphilis is not treated at this stage, it can remain latent or develop into tertiary syphilis.
After many years (5 to 20 years), people who have syphilis and don’t get treatment may develop the fourth stage of syphilis, called tertiary syphilis. At the tertiary syphilis stage, the bacteria can damage almost any part of your body including your heart, brain, spinal cord, eyes and bones, resulting in heart disease, mental illness, blindness, deafness and neurological problems and can be life-threatening.
Some people who have syphilis don’t have any signs of infection. In other people, the signs may be very mild. They might not even know they have it. But even if they have no signs or the signs go away on their own, the infection is still alive and can cause serious health problems many years later.
Primary stage symptoms
The first symptoms of syphilis usually develop around two or three weeks after infection, although they can start up to 90 days.
This stage of the infection is known as “primary syphilis”.
- the main symptom is a small, painless sore or ulcer called a chancre that you might not notice
- the sore will typically be on the penis, vagina, or around the anus, although they can sometimes appear in the mouth or on the lips, fingers or buttocks
- most people only have one sore, but some people have several
- you may also have swollen glands in your neck, groin or armpits
These symptoms usually pass within two to eight weeks. But if the infection isn’t treated, it may progress to a second stage.
Secondary stage symptoms
Symptoms of secondary syphilis include:
- a blotchy red rash that can appear anywhere on the body, but often develops on the palms of the hands or soles of the feet
- small skin growths (similar to genital warts) – on women these often appear on the vulva and for both men and women they may appear around the anus
- white patches in the mouth
- flu-like symptoms, such as tiredness, headaches, joint pains and a high temperature (fever)
- swollen glands
- occasionally, patchy hair loss
Skin rashes and/or mucous membrane lesions (sores in the mouth, vagina, or anus) mark the second stage of symptoms. This stage typically starts with the development of a rash on one or more areas of the body. Rashes associated with secondary syphilis can appear when the primary chancre is healing or several weeks after the chancre has healed. The rash usually does not cause itching. The characteristic rash of secondary syphilis may appear as rough, red, or reddish brown spots both on the palms of the hands and the bottoms of the feet. However, rashes with a different appearance may occur on other parts of the body, sometimes resembling rashes caused by other diseases. Sometimes rashes associated with secondary syphilis are so faint that they are not noticed. Large, raised, gray or white lesions, known as condyloma lata, may develop in warm, moist areas such as the mouth, underarm or groin region. In addition to rashes, symptoms of secondary syphilis may include fever, swollen lymph glands, sore throat, patchy hair loss, headaches, weight loss, muscle aches, and fatigue. The symptoms of secondary syphilis will go away with or without treatment within a few weeks, although they may come and go over several months before they disappear. However, without treatment, the infection will progress to the latent and possibly tertiary stage of disease.
Latent stage symptoms
You’ll still be infected even if you don’t have symptoms. This is known as “latent syphilis” and it can last for decades and lead to serious problems if not treated.
The latent (hidden) stage of syphilis is a period of time when there are no visible signs or symptoms of syphilis. Without treatment, the infected person will continue to have syphilis in their body even though there are no signs or symptoms. Early latent syphilis is latent syphilis where infection occurred within the past 12 months. Late latent syphilis is latent syphilis where infection occurred more than 12 months ago. Latent syphilis can last for years.
It’s still possible to pass on the infection during this stage, although this usually only happens within two years of becoming infected.
Tertiary syphilis
Without treatment, a syphilis infection can last for years or decades without causing any symptoms. Tertiary syphilis is rare and develops in a subset of untreated syphilis infections;, it can appear 10–30 years after infection was first acquired, and it can be fatal. Tertiary syphilis can affect multiple organ systems, including the brain, nerves, eyes, heart, blood vessels, liver, bones, and joints. Symptoms of tertiary syphilis vary depending on the organ system affected.
People with tertiary syphilis may experience:
- meningitis
- strokes
- dementia symptoms
- loss of co-ordination
- numbness
- vision problems or blindness
- heart problems
Syphilis is still treatable at this stage, but it’s sometimes not possible to reverse any damage that’s already been done.
Neurosyphilis
Syphilis can invade the nervous system at any stage of infection, and causes a wide range of symptoms, including headache, altered behavior, difficulty coordinating muscle movements, paralysis, sensory deficits, and dementia 7, 8. This invasion of the nervous system is called “neurosyphilis”.
- Early neurosyphilis: Cerebrospinal fluid (CSF) abnormalities can occur in 50 to 60% of persons with early syphilis and are of unknown significance in the absence of neurologic signs or symptoms 9, 10. The most common manifestation of early neurosyphilis is meningeal syphilis, which usually occurs weeks to months (and almost always within a year) after initial infection 7. Symptomatic syphilitic meningitis often resembles aseptic meningitis, and symptoms may include fever, headache, and stiff neck; with basilar involvement, cranial nerve abnormalities can develop, particularly cranial nerves 2, 6, and 8 7. Meningovascular syphilis typically develops 5 to 12 years after initial infection, but it can occur earlier. Meningovascular syphilis, which results from Treponema pallidum infection and inflammation of small and medium central nervous system blood vessels, most often manifests as a stroke-like syndrome with seizures 11.
- Late neurosyphilis: Late forms of neurosyphilis usually occur multiple years or even decades (typically at least 15 years) after infection 7, 12. In the modern era, this type of neurosyphilis is rarely seen. Clinical manifestations include general paresis and tabes dorsalis but can present with a wide variety of neurologic symptoms, including dementia 7, 8.
Ocular syphilis
Like neurosyphilis, ocular syphilis can occur at any stage of infection 12. Ocular syphilis can involve almost any part of the eye, but the most common clinical presentation is uveitis—anterior, posterior, or panuveitis 13, 14. Symptoms associated with ocular syphilis may occur with or without neurosyphilis include vision changes, decreased visual acuity, and permanent blindness 15, 13, 14. Other described ocular syphilis signs and symptoms include lid involvement, episcleritis, vitritis, papillitis, interstitial keratitis, retinitis, and optic neuritis 14. The clinical presentation of ocular syphilis can have significant overlap with other infectious and noninfectious eye diseases. People with syphilis who have ocular complaints should have a complete cranial nerve evaluation and receive a referral to an ophthalmologist for an immediate evaluation 16. In addition, if any cranial nerve abnormalities are present, a lumbar puncture should be performed with cerebrospinal fluid analysis to determine if concomitant neurosyphilis is present 16.
Clinicians should be aware of ocular syphilis and screen for visual complaints in any patient at risk for syphilis (e.g., men who have sex with men, persons living with HIV, others with risk factors and persons with multiple or anonymous partners).
Otosyphilis
Otic involvement from T. pallidum infection can occur at any stage of syphilis, and persons with otosyphilis usually present with hearing loss, tinnitus, or vertigo, or a combination of these manifestations 17, 18. The hearing loss with otosyphilis is typically sensorineural and can involve one or both ears 17, 18. Otosyphilis can develop with other syphilis manifestations, including neurosyphilis or ocular syphilis. Thus, individuals with suspected or diagnosed otosyphilis should undergo an initial screening evaluation for neurosyphilis and ocular syphilis 18. Poeple with a suspected diagnosis of otosyphilis should receive a referral for an immediate evaluation by an otolaryngologist 16. Individuals with a positive serologic test for syphilis who have isolated auditory symptoms and a normal neurologic examination do not require lumbar puncture with cerebrospinal fluid examination 16.
Congenital syphilis
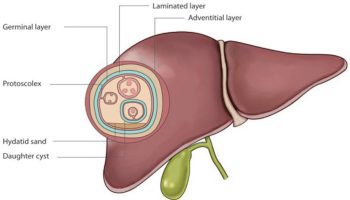
Congenital syphilis occurs when Treponema pallidum is transmitted from a pregnant woman with syphilis to her fetus 19, 20. Less often, perinatal transmission of Treponema pallidum can occur at the time of the delivery if the newborn has contact with maternal genital lesions 19, 20. Transmission to the fetus in pregnancy can occur during any stage of syphilis, but the risk is much higher with primary or secondary syphilis, especially if the mother acquires Treponema pallidum in the third trimester of pregnancy 21. Fetal infection can occur during any trimester of pregnancy. For pregnant women only penicillin therapy can be used to treat syphilis and prevent passing the disease to her baby; treatment with penicillin is extremely effective (success rate of 98%) in preventing mother-to-child transmission 6. Pregnant women who are allergic to penicillin should be referred to a specialist for desensitization to penicillin.
All pregnant women should be tested for syphilis at the first prenatal visit. For women who are at high risk for syphilis, live in areas of high syphilis morbidity, are previously untested, or had a positive screening test in the first trimester, the syphilis screening test should be repeated during the third trimester (28 to 32 weeks gestation) and again at delivery 5. Any woman who delivers a stillborn infant after 20 week’s gestation should also be tested for syphilis.
Depending on how long a pregnant woman has been infected, she may have a high risk of having a stillbirth or of giving birth to a baby who dies shortly after birth. Untreated syphilis in pregnant women results in infant death in up to 40 percent of cases.
An infected baby born alive may not have any signs or symptoms of disease 21, 22, 23. However, if not treated immediately, the baby may develop serious problems within a few weeks. Untreated babies may become developmentally delayed, have seizures, or die. All babies born to mothers who test positive for syphilis during pregnancy should be screened for syphilis and examined thoroughly for evidence of congenital syphilis 5.
Congenital syphilis is traditionally classified as either early or late disease 24. Early manifestations occur within the first two years of life, and late manifestations occur after two years of age. Although infants with congenital syphilis most often display some early manifestations, some do not have clinical manifestations of active disease at the time of birth or early in life. Accordingly, regardless of symptoms, all neonates with a reactive serologic test for syphilis or who are at risk for congenital should undergo a thorough examination for signs or symptoms of congenital syphilis, as well as testing for HIV 16.
- Early congenital syphilis: Early congenital syphilis is usually defined as manifestations of syphilis in infants and children younger than 2 years of age, with more common abnormalities that include the following 19, 25:
- Rhinitis and nasal discharge
- Hepatosplenomegaly
- Jaundice
- Bone involvement (osteochondritis, diaphyseal osteomyelitis, and periostitis)
- Skin rash (begins as a maculopapular rash and may progress to form bullous or desquamating lesions)
- Ophthalmic disorders (cataracts, glaucoma, interstitial keratitis, optic neuritis, chorioretinitis, and pigmentary chorioretinopathy)
- Generalized lymphadenopathy
- Hematologic abnormalities (anemia and thrombocytopenia)
- Neurologic (pseudoparalysis of an extremity)
- Late congenital syphilis: Late congenital syphilis is generally defined as manifestations of syphilis in children older than 2 years of age, which typically result from scarring and chronic inflammatory changes from persistent infection and inflammation, and may manifest with one or more of the following disorders 19, 25, 26:
- Facial changes (frontal bossing due to periostitis, saddle deformity of the nose due to destruction of cartilage)
- Perforation of the hard palate
- Abnormal tooth development such as Hutchinson’s teeth and mulberry molars
- Bone abnormalities (shortened maxilla, tibial thickening [saber shins])
- Ophthalmic disorders (interstitial keratitis, glaucoma, optic atrophy)
- Deafness
Syphilis diagnosis
Syphilis can be diagnosed by testing samples of:
- Blood. Blood tests can confirm the presence of antibodies that the body produces to fight infection. The antibodies to the syphilis-causing bacteria remain in your body for years, so the test can be used to determine a current or past infection.
- Cerebrospinal fluid (CSF). If it’s suspected that you have nervous system complications of syphilis, your doctor may also suggest collecting a sample of cerebrospinal fluid through a lumbar puncture.
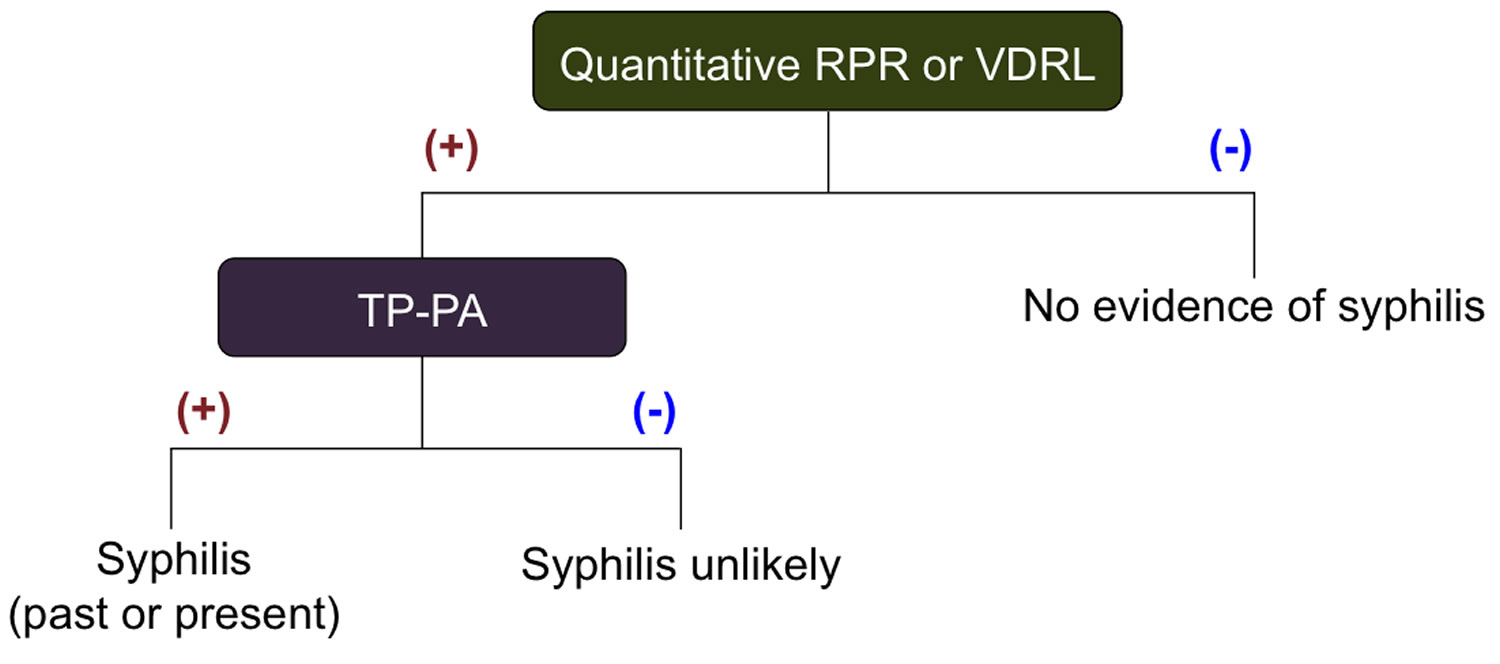
The definitive method for diagnosing syphilis is visualizing the Treponema pallidum bacterium via darkfield microscopy. This technique is rarely performed today. Diagnoses are thus more commonly made using blood tests. There are two types of blood tests available for syphilis: 1) nontreponemal blood tests and 2) treponemal blood tests. Both types of tests are needed to confirm a diagnosis of syphilis.
A presumptive diagnosis of syphilis requires use of two tests: a nontreponemal test (i.e., Venereal Disease Research Laboratory [VDRL] or Rapid Plasma Reagin [RPR]) and a treponemal test (i.e., fluorescent treponemal antibody absorbed [FTA-ABS] tests, the Treponema pallidum passive particle agglutination [TP-PA] assay, various enzyme immunoassays [EIAs], chemiluminescence immunoassays, immunoblots, or rapid treponemal assays). Although many treponemal-based tests are commercially available, only a few are approved for use in the United States. Use of only one type of serologic test is insufficient for diagnosis and can result in false-negative results in persons tested during primary syphilis and false-positive results in persons without syphilis. False-positive nontreponemal test results can be associated with various medical conditions and factors unrelated to syphilis, including other infections (e.g., HIV), autoimmune conditions, immunizations, pregnancy, injection-drug use, and older age 27. Therefore, persons with a reactive nontreponemal test should always receive a treponemal test to confirm the diagnosis of syphilis.
Nontreponemal test antibody titers might correlate with disease activity and are used to follow treatment response. Results should be reported quantitatively. A fourfold change in titer, equivalent to a change of two dilutions (e.g., from 1:16 to 1:4 or from 1:8 to 1:32), is considered necessary to demonstrate a clinically significant difference between two nontreponemal test results obtained using the same serologic test. Sequential serologic tests in individual patients should be performed using the same testing method (VDRL or RPR), preferably by the same laboratory. The VDRL and RPR are equally valid assays, but quantitative results from the two tests cannot be compared directly because RPR titers frequently are slightly higher than VDRL titers. Nontreponemal test titers usually decline after treatment and might become nonreactive with time; however, in some persons, nontreponemal antibodies can persist for a long period of time, a response referred to as the “serofast reaction.” Most patients who have reactive treponemal tests will have reactive tests for the remainder of their lives, regardless of treatment or disease activity. However, 15%–25% of patients treated during the primary stage revert to being serologically nonreactive after 2–3 years 28. Treponemal antibody titers do not predict treatment response and therefore should not be used for this purpose.
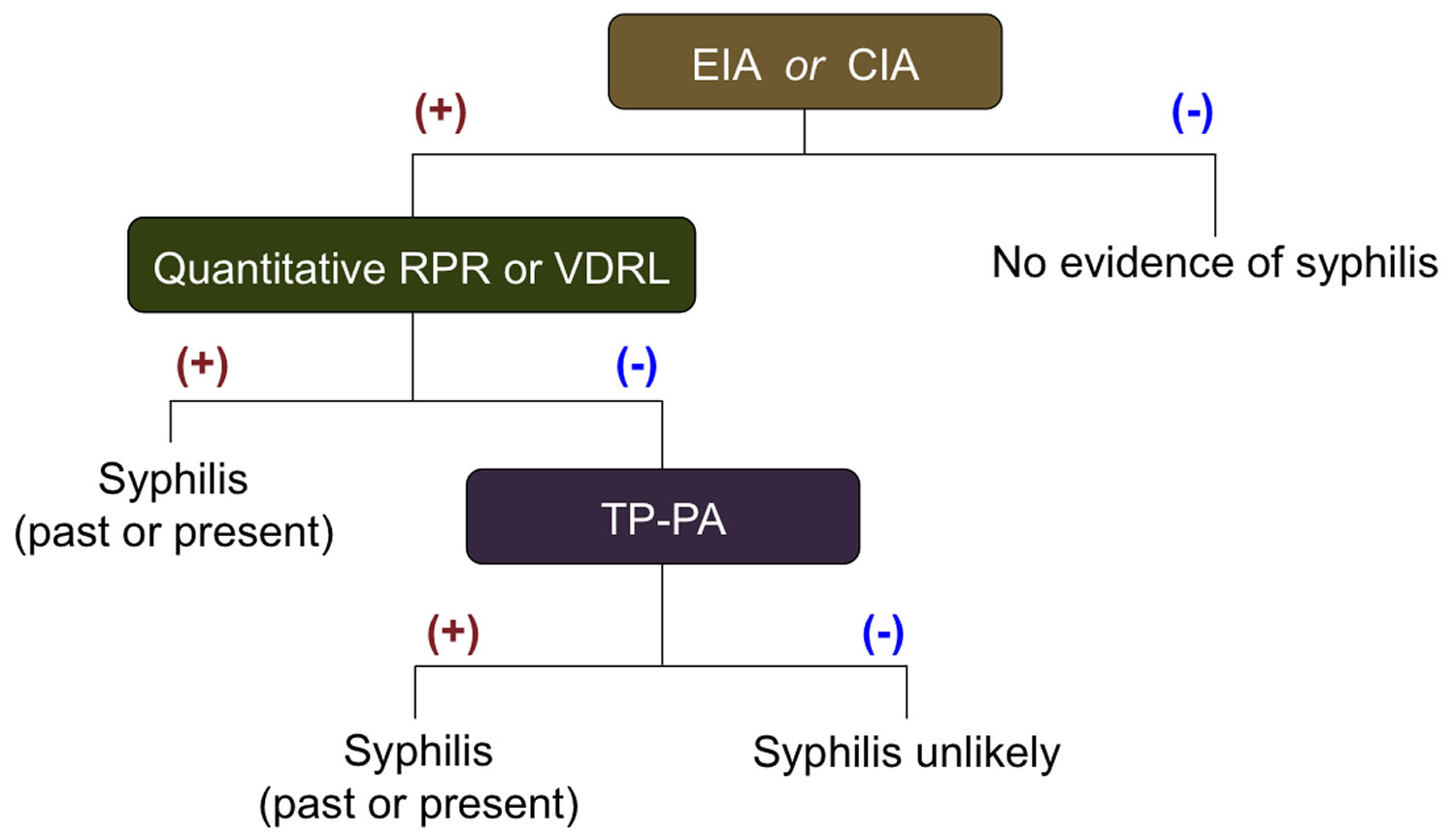
Some clinical laboratories are screening samples using treponemal tests, typically by EIA or chemiluminescence immunoassays 29. This reverse screening algorithm for syphilis testing can identify persons previously treated for syphilis, those with untreated or incompletely treated syphilis, and persons with false-positive results that can occur with a low likelihood of infection. Persons with a positive treponemal screening test should have a standard nontreponemal test with titer performed reflexively by the laboratory to guide patient management decisions. If the nontreponemal test is negative, the laboratory should perform a different treponemal test (preferably one based on different antigens than the original test) to confirm the results of the initial test. If a second treponemal test is positive, persons with a history of previous treatment will require no further management unless sexual history suggests likelihood of re-exposure. In this instance, a repeat nontreponemal test in 2–4 weeks is recommended to evaluate for early infection. Those without a history of treatment for syphilis should be offered treatment. Unless history or results of a physical examination suggest a recent infection, previously untreated persons should be treated for late latent syphilis. If the second treponemal test is negative and the epidemiologic risk and clinical probability for syphilis are low, further evaluation or treatment is not indicated. Two studies demonstrate that high quantitative index values from treponemal EIA/CIA tests correlate with TPPA positivity; however, the range of optical density values varies among different treponemal immunoassays, and the clinical significance of these findings warrant further investigation 30.
For most persons with HIV infection, serologic tests are accurate and reliable for diagnosing syphilis and following a patient’s response to treatment. However, atypical nontreponemal serologic test results (i.e., unusually high, unusually low, or fluctuating titers) might occur regardless of HIV-infection status. When serologic tests do not correspond with clinical findings suggestive of early syphilis, presumptive treatment is recommended for persons with risk factors for syphilis, and use of other tests (e.g., biopsy and PCR) should be considered.
Further testing is warranted for persons with clinical signs of neurosyphilis (e.g., cranial nerve dysfunction, auditory or ophthalmic abnormalities, meningitis, stroke, acute or chronic altered mental status, and loss of vibration sense). Laboratory testing is helpful in supporting the diagnosis of neurosyphilis; however, no single test can be used to diagnose neurosyphilis in all instances. The diagnosis of neurosyphilis depends on a combination of cerebrospinal fluid (CSF) tests (CSF cell count or protein and a reactive CSF-VDRL) in the presence of reactive serologic test results and neurologic signs and symptoms. CSF laboratory abnormalities are common in persons with early syphilis and are of unknown significance in the absence of neurologic signs or symptoms 31. CSF-VDRL is highly specific but insensitive. In a person with neurologic signs or symptoms, a reactive CSF-VDRL (in the absence of blood contamination) is considered diagnostic of neurosyphilis. When CSF-VDRL is negative despite the presence of clinical signs of neurosyphilis, reactive serologic test results, and abnormal CSF cell count and/or protein, neurosyphilis should be considered. In this instance, additional evaluation using FTA-ABS testing on CSF may be warranted. The CSF FTA-ABS test is less specific for neurosyphilis than the CSF-VDRL but is highly sensitive. Neurosyphilis is highly unlikely with a negative CSF FTA-ABS test, especially among persons with nonspecific neurologic signs and symptoms 32.
Among persons with HIV infection, CSF leukocyte count usually is elevated (>5 white blood cell count [WBC]/mm³). Using a higher cutoff (>20 WBC/ mm³) might improve the specificity of neurosyphilis diagnosis 33.
Figure 13. Standard syphilis screening algorithm
Abbreviation: TP-PA =Treponema pallidum-Particle agglutination
[Source 34 ]Figure 14. Reverse Sequence Syphilis Screening Algorithm
Abbreviations:
- Treponema pallidum-specific enzyme immunoassay (EIA) or chemiluminescence immunoassay (CIA)
- VDRL = Venereal Disease Research Laboratory
- RPR = Rapid Plasma Reagin
- FTA-ABS = Fluorescent Treponemal Antibody Absorbed
- TP-PA =Treponema pallidum-Particle agglutination
- ELISA= Enzyme Linked Immunoassay
Syphilis blood test
Nontreponemal tests
Nontreponemal tests [e.g., Venereal Disease Research Laboratory (VDRL) and Rapid Plasma Reagin (RPR)] are simple, inexpensive, and are often used for screening. However, they are not specific for syphilis, can produce false-positive results, and, by themselves, are insufficient for diagnosis. Venereal Disease Research Laboratory (VDRL) and Rapid Plasma Reagin (RPR) tests should each have their antibody titer results reported quantitatively. Persons with a reactive nontreponemal test should always receive a treponemal test to confirm a syphilis diagnosis. This sequence of testing (nontreponemal, then treponemal test) is considered the “classical” testing algorithm.
Treponemal tests
Treponemal tests (e.g., FTA-ABS, TP-PA, various EIAs, chemiluminescence immunoassays, immunoblots, and rapid treponemal assays) detect antibodies that are specific for syphilis. Treponemal antibodies appear earlier than nontreponemal antibodies and usually remain detectable for life, even after successful treatment. If a treponemal test is used for screening and the results are positive, a nontreponemal test with titer should be performed to confirm diagnosis and guide patient management decisions. Based on the results, further treponemal testing may be indicated. This sequence of testing (treponemal, then nontreponemal test) is considered the “reverse” sequence testing algorithm. Reverse sequence testing can be more convenient for laboratories, but its clinical interpretation is problematic, as this testing sequence can identify persons previously treated for syphilis, those with untreated or incompletely treated syphilis, and persons with false-positive results that can occur with a low likelihood of infection 36.
Special note: Because untreated syphilis in a pregnant woman can infect and possibly kill her developing baby, every pregnant woman should have a blood test for syphilis. All women should be screened at their first prenatal visit. For patients who belong to communities and populations with high prevalence of syphilis and for patients at high risk, blood tests should also be performed during the third trimester (at 28–32 weeks) and at delivery.
All infants born to mothers who have reactive nontreponemal and treponemal test results should be evaluated for congenital syphilis. A quantitative nontreponemal test should be performed on infant serum and, if reactive, the infant should be examined thoroughly for evidence of congenital syphilis. Suspicious lesions, body fluids, or tissues (e.g., umbilical cord, placenta) should be examined by darkfield microscopy, PCR testing, and/or special stains. Other recommended evaluations may include analysis of cerebrospinal fluid by Venereal Disease Research Laboratory (VDRL), cell count and protein, complete blood count with differential and platelet count, and long-bone radiographs.
Latent Syphilis
Latent syphilis is defined as syphilis characterized by seroreactivity without other evidence of primary, secondary, or tertiary disease. Persons who have latent syphilis and who acquired syphilis during the preceding year are classified as having early latent syphilis, a subset of latent syphilis. Persons can receive a diagnosis of early latent syphilis if, during the year preceding the diagnosis, they had 1) a documented seroconversion or a sustained (>2 week) fourfold or greater increase in nontreponemal test titers; 2) unequivocal symptoms of primary or secondary syphilis; or 3) a sex partner documented to have primary, secondary, or early latent syphilis. In addition, for persons with reactive nontreponemal and treponemal tests whose only possible exposure occurred during the previous 12 months, early latent syphilis can be assumed. In the absence of these conditions, an asymptomatic person should be considered to have latent syphilis. Nontreponemal serologic titers usually are higher early in the course of syphilis infection. However, early latent syphilis cannot be reliably diagnosed solely on the basis of nontreponemal titers. All persons with latent syphilis should have careful examination of all accessible mucosal surfaces (i.e., the oral cavity, perianal area, perineum and vagina in women, and underneath the foreskin in uncircumcised men) to evaluate for mucosal lesions.
Congenital syphilis
The diagnosis of congenital syphilis can be difficult, as maternal nontreponemal and treponemal IgG (immunoglobulin G) antibodies can be transferred through the placenta to the fetus, complicating the interpretation of reactive serologic tests for syphilis in neonates. Therefore, treatment decisions frequently must be made on the basis of 1) identification of syphilis in the mother; 2) adequacy of maternal treatment; 3) presence of clinical, laboratory, or radiographic evidence of syphilis in the neonate; and 4) comparison of maternal (at delivery) and neonatal nontreponemal serologic titers using the same test, preferably conducted by the same laboratory. Any neonate at risk for congenital syphilis should receive a full evaluation and testing for HIV infection.
All neonates born to mothers who have reactive nontreponemal and treponemal test results should be evaluated with a quantitative nontreponemal serologic test [Rapid Plasma Reagin (RPR) or Venereal Disease Research Laboratory (VDRL)] performed on the neonate’s serum, because umbilical cord blood can become contaminated with maternal blood and yield a false-positive result, and Wharton’s jelly within the umbilical cord can yield a false-negative result. Conducting a treponemal test (i.e., TP-PA, FTA-ABS, EIA, or CIA) on neonatal serum is not recommended because it is difficult to interpret. No commercially available immunoglobulin M (IgM) test can be recommended.
All neonates born to women who have reactive serologic tests for syphilis should be examined thoroughly for evidence of congenital syphilis (e.g., nonimmune hydrops, jaundice, hepatosplenomegaly, rhinitis, skin rash, and pseudoparalysis of an extremity). Pathologic examination of the placenta or umbilical cord using specific staining (e.g., silver) or a T. pallidum PCR test using a CLIA-validated test should be considered; DFA-TP reagents are not available. Darkfield microscopic examination or PCR testing of suspicious lesions or body fluids (e.g., bullous rash and nasal discharge) also should be performed. In addition to these tests, for stillborn infants, skeletal survey demonstrating typical osseous lesions might aid in the diagnosis of congenital syphilis.
The following scenarios describe the congenital syphilis evaluation and treatment of neonates born to women who have reactive serologic tests for syphilis during pregnancy. Maternal history of infection with T. pallidum and treatment for syphilis must be considered when evaluating and treating the neonate for congenital syphilis in most scenarios, except when congenital syphilis is proven or highly probable (See Scenario 1).
Scenario 1: Proven or highly probable congenital syphilis
Any neonate with:
- an abnormal physical examination that is consistent with congenital syphilis;
OR - a serum quantitative nontreponemal serologic titer that is fourfold higher than the mother’s titer;*
OR - a positive darkfield test or PCR of lesions or body fluid(s).
* The absence of a fourfold or greater titer for a neonate does not exclude congenital syphilis.
Recommended Evaluation
- CSF analysis for VDRL, cell count, and protein **
- Complete blood count (CBC) and differential and platelet count
- Other tests as clinically indicated (e.g., long-bone radiographs, chest radiograph, liver-function tests, neuroimaging, ophthalmologic examination, and auditory brain stem response).
**CSF test results obtained during the neonatal period can be difficult to interpret; normal values differ by gestational age and are higher in preterm infants. Values as high as 25 white blood cells (WBCs) /mm3 and/or protein of 150 mg/dL might occur among normal neonates; lower values (i.e., 5 WBCs/mm³ and protein of 40 mg/dL) might be considered the upper limits of normal. Other causes of elevated values should be considered when an infant is being evaluated for congenital syphilis.
Scenario 2: Possible Congenital Syphilis
Any neonate who has a normal physical examination and a serum quantitative nontreponemal serologic titer equal to or less than fourfold the maternal titer and one of the following:
- mother was not treated, inadequately treated, or has no documentation of having received treatment;
OR - mother was treated with erythromycin or a regimen other than those recommended in these guidelines (i.e., a nonpenicillin G regimen);††
OR - mother received recommended treatment <4 weeks before delivery.
†† A women treated with a regimen other than recommended in these guidelines should be considered untreated.
Recommended Evaluation
- CSF analysis for Venereal Disease Research Laboratory (VDRL), cell count, and protein**
- CBC, differential, and platelet count
- Long-bone radiographs
A complete evaluation is not necessary if 10 days of parenteral therapy is administered, although such evaluations might be useful. For instance, a lumbar puncture might document CSF abnormalities that would prompt close follow-up. Other tests (e.g., CBC, platelet count, and bone radiographs) can be performed to further support a diagnosis of congenital syphilis.
**CSF test results obtained during the neonatal period can be difficult to interpret; normal values differ by gestational age and are higher in preterm infants. Values as high as 25 white blood cells (WBCs) /mm3 and/or protein of 150 mg/dL might occur among normal neonates; lower values (i.e., 5 WBCs/mm³ and protein of 40 mg/dL) might be considered the upper limits of normal. Other causes of elevated values should be considered when an infant is being evaluated for congenital syphilis.
Scenario 3: Congenital Syphilis less likely
Any neonate who has a normal physical examination and a serum quantitative nontreponemal serologic titer equal to or less than fourfold the maternal titer and both of the following are true:
- mother was treated during pregnancy, treatment was appropriate for the stage of infection, and treatment was administered >4 weeks before delivery and
mother has no evidence of reinfection or relapse.
Recommended Evaluation
No evaluation is recommended.
Persons with HIV Infection
Interpretation of treponemal and nontreponemal serologic tests for persons with HIV infection is the same as for the HIV-uninfected patient. Although rare, unusual serologic responses have been observed among persons with HIV infection who have syphilis; although most reports have involved post-treatment serologic titers that were higher than expected (high serofast) or fluctuated, false-negative serologic test results and delayed appearance of seroreactivity have also been reported 37.
When clinical findings are suggestive of syphilis but serologic tests are nonreactive or their interpretation is unclear, alternative tests (e.g., biopsy of a lesion, darkfield examination, and PCR of lesion material) might be useful for diagnosis. Neurosyphilis should be considered in the differential diagnosis of neurologic signs and symptoms in persons with HIV infection.
Syphilis treatment
Penicillin G, administered parenterally, is the preferred drug for treating persons in all stages of syphilis 38. The preparation used (i.e., benzathine, aqueous procaine, or aqueous crystalline), dosage, and length of treatment depend on the stage and clinical manifestations of the disease. Treatment for late latent syphilis and tertiary syphilis require a longer duration of therapy, because organisms theoretically might be dividing more slowly (the validity of this rationale has not been assessed). Longer treatment duration is required for persons with latent syphilis of unknown duration to ensure that those who did not acquire syphilis within the preceding year are adequately treated.
Selection of the appropriate penicillin preparation is important, because Treponema pallidum can reside in sequestered sites (e.g., the CNS and aqueous humor) that are poorly accessed by some forms of penicillin. Combinations of benzathine penicillin, procaine penicillin, and oral penicillin preparations are not considered appropriate for the treatment of syphilis. Reports have indicated that practitioners have inadvertently prescribed combination benzathine-procaine penicillin (Bicillin C-R) instead of the standard benzathine penicillin product (Bicillin L-A) widely used in the United States. Practitioners, pharmacists, and purchasing agents should be aware of the similar names of these two products to avoid using the inappropriate combination therapy agent for treating syphilis 39.
The effectiveness of penicillin for the treatment of syphilis was well established through clinical experience even before the value of randomized controlled clinical trials was recognized. Therefore, nearly all recommendations for the treatment of syphilis are based not only on clinical trials and observational studies, but many decades of clinical experience.
The Jarisch-Herxheimer reaction is an acute febrile reaction frequently accompanied by headache, myalgia, fever, and other symptoms that can occur within the first 24 hours after the initiation of any therapy for syphilis. Patients should be informed about this possible adverse reaction and how to manage it if it occurs. The Jarisch-Herxheimer reaction occurs most frequently among persons who have early syphilis, presumably because bacterial burdens are higher during these stages. Antipyretics can be used to manage symptoms, but they have not been proven to prevent this reaction. The Jarisch-Herxheimer reaction might induce early labor or cause fetal distress in pregnant women, but this should not prevent or delay therapy.
Primary and Secondary Syphilis Treatment
Parenteral penicillin G has been used effectively to achieve clinical resolution (i.e., the healing of lesions and prevention of sexual transmission) and to prevent late sequelae. However, no comparative trials have been conducted to guide the selection of an optimal penicillin regimen. Substantially fewer data are available for nonpenicillin regimens.
Recommended Regimen for Adults*
- Benzathine penicillin G 2.4 million units IM in a single dose
*Recommendations for treating syphilis in persons with HIV infection and pregnant women are discussed below.
Available data demonstrate that use of additional doses of benzathine penicillin G, amoxicillin, or other antibiotics do not enhance efficacy when used to treat primary and secondary syphilis, regardless of HIV status 40.
Recommended Regimen for Infants and Children
- Benzathine penicillin G 50,000 units/kg IM, up to the adult dose of 2.4 million units in a single dose
Infants and children aged >1 month who receive a diagnosis of syphilis should have birth and maternal medical records reviewed to assess whether they have congenital or acquired syphilis (see Congenital Syphilis). Infants and children aged ≥1 month with primary and secondary syphilis should be managed by a pediatric infectious-disease specialist and evaluated for sexual abuse (e.g., through consultation with child-protection services).
Other Management Considerations
All persons who have primary and secondary syphilis should be tested for HIV infection. In geographic areas in which the prevalence of HIV is high, persons who have primary or secondary syphilis should be retested for acute HIV in 3 months if the first HIV test result was negative.
Persons who have syphilis and symptoms or signs suggesting neurologic disease (e.g., cranial nerve dysfunction, meningitis, stroke, and hearing loss) or ophthalmic disease (e.g., uveitis, iritis, neuroretinitis, and optic neuritis) should have an evaluation that includes CSF analysis, ocular slit-lamp ophthalmologic examination, and otologic examination. Treatment should be guided by the results of this evaluation.
Invasion of CSF by Treponema pallidum accompanied by CSF laboratory abnormalities is common among adults who have primary or secondary syphilis 31. In the absence of clinical neurologic findings, no evidence supports variation from the recommended treatment regimen for primary and secondary syphilis. Symptomatic neurosyphilis develops in only a limited number of persons after treatment with the penicillin regimens recommended for primary and secondary syphilis. Therefore, unless clinical signs or symptoms of neurologic or ophthalmic involvement are present, routine CSF analysis is not recommended for persons who have primary or secondary syphilis.
Jarisch-Herxheimer Reaction
The Jarisch-Herxheimer reaction is a self-limited reaction associated with initiation of anti-treponemal therapy that most often occurs in persons treated for early syphilis, presumably because bacterial burdens are higher during these stages. The Jarisch-Herxheimer reaction is characterized by fever, malaise, nausea, vomiting, and less frequently, chills and exacerbation of a secondary syphilis rash 41. This reaction almost always occurs within 24 hours after initiating antimicrobial therapy and usually resolves within 24 hours. For patients who develop a Jarisch-Herxheimer reaction, the clinician should clarify this reaction is not an allergic reaction to penicillin. It occurs more frequently after treatment with penicillin and treatment of early syphilis, especially at the secondary stage. Antipyretics can be used to manage symptoms associated with the Jarisch-Herxheimer reaction, but they do not prevent this reaction.
Follow-Up
Clinical and serologic evaluation should be performed at 6 and 12 months after treatment; more frequent evaluation might be prudent if follow-up is uncertain or if repeat infection is a concern. Serologic response (i.e., titer) should be compared with the titer at the time of treatment. However, assessing serologic response to treatment can be difficult, and definitive criteria for cure or failure have not been well established. In addition, nontreponemal test titers might decline more slowly for persons previously treated for syphilis 42.
Persons who have signs or symptoms that persist or recur and those with at least a fourfold increase in nontreponemal test titer persisting for >2 weeks likely experienced treatment failure or were re-infected. These persons should be retreated and reevaluated for HIV infection. Because treatment failure usually cannot be reliably distinguished from reinfection with Treponema pallidum, a CSF analysis also should be performed; treatment should be guided by CSF findings.
Failure of nontreponemal test titers to decline fourfold within 6–12 months after therapy for primary or secondary syphilis might be indicative of treatment failure. However, clinical trial data have demonstrated that 15%–20% of persons with primary and secondary syphilis treated with the recommended therapy will not achieve the fourfold decline in nontreponemal titer used to define response at 1 year after treatment 42. Serologic response to treatment appears to be associated with several factors, including the person’s stage of syphilis (earlier stages are more likely to decline fourfold and become negative) and initial nontreponemal antibody titers (lower titers are less likely to decline fourfold than higher titers) 42. Optimal management of persons who have less than a fourfold decline in titers after treatment of syphilis is unclear. At a minimum, these persons should receive additional clinical and serologic follow-up and be evaluated for HIV infection. If additional follow-up cannot be ensured, retreatment is recommended. Because treatment failure might be the result of unrecognized CNS infection, CSF examination can be considered in such situations.
For retreatment, weekly injections of benzathine penicillin G 2.4 million units IM for 3 weeks is recommended, unless CSF examination indicates that neurosyphilis is present (see Neurosyphilis). Serologic titers might not decline despite a negative CSF examination and a repeated course of therapy 43. In these circumstances, although the need for additional therapy or repeated CSF examinations is unclear, it is not generally recommended.
Latent Syphilis Treatment
Because latent syphilis is not transmitted sexually, the objective of treating persons in this stage of disease is to prevent complications and transmission from a pregnant woman to her fetus. Although clinical experience supports the effectiveness of penicillin in achieving this goal, limited evidence is available to guide choice of specific regimens or duration.
Recommended Regimens for Adults*
Early Latent Syphilis
- Benzathine penicillin G 2.4 million units IM in a single dose
Available data demonstrate that additional doses of benzathine penicillin G, amoxicillin, or other antibiotics in early latent syphilis do not enhance efficacy, regardless of HIV infection 44
Late Latent Syphilis or Latent Syphilis of Unknown Duration
- Benzathine penicillin G 7.2 million units total, administered as 3 doses of 2.4 million units IM each at 1-week intervals
Recommended Regimens for Infants and Children
Early Latent Syphilis
- Benzathine penicillin G 50,000 units/kg IM, up to the adult dose of 2.4 million units in a single dose
Late Latent Syphilis
- Benzathine penicillin G 50,000 units/kg IM, up to the adult dose of 2.4 million units, administered as 3 doses at 1-week intervals (total 150,000 units/kg up to the adult total dose of 7.2 million units)
Infants and children aged ≥1 month diagnosed with latent syphilis should be managed by a pediatric infectious-disease specialist and receive a CSF examination. In addition, birth and maternal medical records should be reviewed to assess whether these infants and children have congenital or acquired syphilis. For those with congenital syphilis, treatment should be undertaken as described in the congenital syphilis section in this document. Those with acquired latent syphilis should be evaluated for sexual abuse (e.g., through consultation with child protection services). These regimens are for penicillin nonallergic children who have acquired syphilis and who have normal CSF examination results.
Latent Syphilis among Persons with HIV Infection
Recommended Regimen for Early Latent Syphilis
- Benzathine penicillin G, 2.4 million units IM in a single dose
Recommended Regimen for Late Latent Syphilis
- Benzathine penicillin G, at weekly doses of 2.4 million units for 3 weeks
Other Management Considerations
If a person misses a dose of penicillin in a course of weekly therapy for latent syphilis, the appropriate course of action is unclear. Clinical experience suggests that an interval of 10–14 days between doses of benzathine penicillin for latent syphilis might be acceptable before restarting the sequence of injections (i.e., if dose 1 is given on day 0, dose 2 is administered between days 10 and 14). Pharmacologic considerations suggest that an interval of 7–9 days between doses, if feasible, might be more optimal 45. Missed doses are not acceptable for pregnant women receiving therapy for latent syphilis 46. Pregnant women who miss any dose of therapy must repeat the full course of therapy.
Follow-Up
Quantitative nontreponemal serologic tests should be repeated at 6, 12, and 24 months. A CSF examination should be performed if 1) a sustained (>2 weeks) fourfold increase or greater in titer is observed, 2) an initially high titer (≥1:32) fails to decline at least fourfold within 12–24 months of therapy, or 3) signs or symptoms attributable to syphilis develop. In such circumstances, patients with CSF abnormalities should be treated for neurosyphilis. If the CSF examination is negative, retreatment for latent syphilis should be administered. Serologic titers might fail to decline despite a negative CSF examination and a repeated course of therapy, especially if the initial nontreponemal titer is low (<1:8); in these circumstances, the need for additional therapy or repeated CSF examinations is unclear but is generally not recommended. Serologic and clinical monitoring should be offered along with a reevaluation for HIV infection.
Management of Sex Partners
Sexual transmission of Treponema pallidum is thought to occur only when mucocutaneous syphilitic lesions are present. Such manifestations are uncommon after the first year of infection. Persons exposed sexually to a person who has primary, secondary, or early latent syphilis should be evaluated clinically and serologically and treated according to the following recommendations:
- Persons who have had sexual contact with a person who receives a diagnosis of primary, secondary, or early latent syphilis within 90 days preceding the diagnosis should be treated presumptively for early syphilis, even if serologic test results are negative.
- Persons who have had sexual contact with a person who receives a diagnosis of primary, secondary, or early latent syphilis >90 days before the diagnosis should be treated presumptively for early syphilis if serologic test results are not immediately available and the opportunity for follow-up is uncertain. If serologic tests are negative, no treatment is needed. If serologic tests are positive, treatment should be based on clinical and serologic evaluation and stage of syphilis.
- In some areas or populations with high rates of syphilis, health departments recommend notification and presumptive treatment of sex partners of persons with late latent syphilis who have high nontreponemal serologic test titers (i.e., >1:32), because high titers might be indicative of early syphilis. These partners should be managed as if the index case had early syphilis.
- Long-term sex partners of persons who have late latent syphilis should be evaluated clinically and serologically for syphilis and treated on the basis of the evaluation’s findings.
- The following sex partners of persons with syphilis are considered at risk for infection and should be confidentially notified of the exposure and need for evaluation: partners who have had sexual contact within 1) 3 months plus the duration of symptoms for persons who receive a diagnosis of primary syphilis, 2) 6 months plus duration of symptoms for those with secondary syphilis, and 3) 1 year for persons with early latent syphilis.
Expedited Partner Therapy
There is insufficient data to support the use of expedited partner therapy in management of syphilis contacts. Accordingly, use of expedited partner therapy is not recommended for sexual contacts of persons diagnosed with syphilis. Transmission of Treponema pallidum is highly unlikely in persons when more than 1 year has elapsed since the time of infection.
Primary and Secondary Syphilis among Persons with HIV Infection
Recommended Regimen
- Benzathine penicillin G, 2.4 million units IM in a single dose
Available data demonstrate that additional doses of benzathine penicillin G, amoxicillin, or other antibiotics in primary and secondary syphilis do not result in enhanced efficacy 44.
Persons with HIV infection who have early syphilis might be at increased risk for neurologic complications 47 and might have higher rates of serologic treatment failure with recommended regimens. The magnitude of these risks is not defined precisely, but is likely small. Although long-term (>1 year) comparative data are lacking, no treatment regimens for syphilis have been demonstrated to be more effective in preventing neurosyphilis in persons with HIV infection than the syphilis regimens recommended for persons without HIV infection 48. Careful follow-up after therapy is essential. The use of antiretroviral therapy as per current guidelines might improve clinical outcomes in persons with HIV infection and syphilis 49.
Syphilis During Pregnancy
Penicillin G is the only known effective antimicrobial for preventing maternal transmission to the fetus and treating fetal infection 50. Evidence is insufficient to determine optimal, recommended penicillin regimens 51.
Recommended Regimen
- Pregnant women should be treated with the penicillin regimen appropriate for their stage of infection.
Other Management Considerations
- Some evidence suggests that additional therapy is beneficial for pregnant women. For women who have primary, secondary, or early latent syphilis, a second dose of benzathine penicillin 2.4 million units IM can be administered 1 week after the initial dose 52.
- When syphilis is diagnosed during the second half of pregnancy, management should include a sonographic fetal evaluation for congenital syphilis. However, this evaluation should not delay therapy. Sonographic signs of fetal or placental syphilis (i.e., hepatomegaly, ascites, hydrops, fetal anemia, or a thickened placenta) indicate a greater risk for fetal treatment failure 53; cases accompanied by these signs should be managed in consultation with obstetric specialists. Evidence is insufficient to recommend specific regimens for these situations.
- Women treated for syphilis during the second half of pregnancy are at risk for premature labor and/or fetal distress if the treatment precipitates the Jarisch-Herxheimer reaction 54. These women should be advised to seek obstetric attention after treatment if they notice any fever, contractions, or decrease in fetal movements. Stillbirth is a rare complication of treatment, but concern for this complication should not delay necessary treatment. No data are available to suggest that corticosteroid treatment alters the risk for treatment-related complications in pregnancy.
- Missed doses are not acceptable for pregnant women receiving therapy for late latent syphilis 46. Pregnant women who miss any dose of therapy must repeat the full course of therapy.
- All women who have syphilis should be offered testing for HIV infection.
Follow-Up
Coordinated prenatal care and treatment are vital. At a minimum, serologic titers should be repeated at 28–32 weeks’ gestation and at delivery. Serologic titers can be checked monthly in women at high risk for reinfection or in geographic areas in which the prevalence of syphilis is high. Providers should ensure that the clinical and antibody responses are appropriate for the patient’s stage of disease, although most women will deliver before their serologic response to treatment can be assessed definitively. Inadequate maternal treatment is likely if delivery occurs within 30 days of therapy, clinical signs of infection are present at delivery, or the maternal antibody titer at delivery is fourfold higher than the pretreatment titer.
Congenital syphilis treatment
Proven or highly probable congenital syphilis Recommended Regimens
- Aqueous crystalline penicillin G 100,000–150,000 units/kg/day, administered as 50,000 units/kg/dose IV every 12 hours during the first 7 days of life and every 8 hours thereafter for a total of 10 days
OR
- Procaine penicillin G 50,000 units/kg/dose IM in a single daily dose for 10 days
If more than 1 day of therapy is missed, the entire course should be restarted. Data are insufficient regarding the use of other antimicrobial agents (e.g., ampicillin). When possible, a full 10-day course of penicillin is preferred, even if ampicillin was initially provided for possible sepsis. The use of agents other than penicillin requires close serologic follow-up to assess adequacy of therapy.
Possible Congenital Syphilis Recommended Regimens
- Aqueous crystalline penicillin G 100,000–150,000 units/kg/day, administered as 50,000 units/kg/dose IV every 12 hours during the first 7 days of life and every 8 hours thereafter for a total of 10 days
OR
- Procaine penicillin G 50,000 units/kg/dose IM in a single daily dose for 10 days
OR
- Benzathine penicillin G 50,000 units/kg/dose IM in a single dose
Before using the single-dose benzathine penicillin G regimen, the complete evaluation (i.e., CSF examination, long-bone radiographs, and CBC with platelets) must be normal, and follow-up must be certain. If any part of the infant’s evaluation is abnormal or not performed, if the CSF analysis is uninterpretable because of contamination with blood, or if follow-up is uncertain, a 10-day course of penicillin G is required. If the neonate’s nontreponemal test is nonreactive and the provider determines that the mother’s risk of untreated syphilis is low, treatment of the neonate with a single IM dose of benzathine penicillin G 50,000 units/kg for possible incubating syphilis can be considered without an evaluation.
Neonates born to mothers with untreated early syphilis at the time of delivery are at increased risk for congenital syphilis, and the 10-day course of penicillin G may be considered even if the complete evaluation is normal and follow-up is certain.
Congenital Syphilis Less Likely – Recommended Regimen
- Benzathine penicillin G 50,000 units/kg/dose IM in a single dose*
*Another approach involves not treating the infant, but rather providing close serologic follow-up every 2-3 months for 6 months for infants whose mother’s nontreponemal titers decreased at least fourfold after appropriate therapy for early syphilis or remained stable for low-titer, latent syphilis (e.g., VDRL <1:2; RPR <1:4).
Congenital Syphilis Unlikely Recommended Regimen
- No treatment is required, but infants with reactive nontreponemal tests should be followed serologically to ensure the nontreponemal test returns to negative (see Follow-Up). Benzathine penicillin G 50,000 units/kg as a single IM injection might be considered, particularly if follow-up is uncertain and the neonate has a reactive nontreponemal test.
Follow-Up
All neonates with reactive nontreponemal tests should receive careful follow-up examinations and serologic testing (i.e., a nontreponemal test) every 2–3 months until the test becomes nonreactive. In the neonate who was not treated because congenital syphilis was considered less likely or unlikely, nontreponemal antibody titers should decline by age 3 months and be nonreactive by age 6 months, indicating that the reactive test result was caused by passive transfer of maternal IgG antibody. At 6 months, if the nontreponemal test is nonreactive, no further evaluation or treatment is needed; if the nontreponemal test is still reactive, the infant is likely to be infected and should be treated. Treated neonates that exhibit persistent nontreponemal test titers by 6–12 months should be re-evaluated through CSF examination and managed in consultation with an expert. Retreatment with a 10-day course of a penicillin G regimen may be indicated. Neonates with a negative nontreponemal test at birth and whose mothers were seroreactive at delivery should be retested at 3 months to rule out serologically negative incubating congenital syphilis at the time of birth. Treponemal tests should not be used to evaluate treatment response because the results are qualitative and passive transfer of maternal IgG treponemal antibody might persist for at least 15 months.
Neonates whose initial CSF evaluations are abnormal should undergo a repeat lumbar puncture approximately every 6 months until the results are normal. A reactive CSF Venereal Disease Research Laboratory (VDRL) test or abnormal CSF indices that persist and cannot be attributed to other ongoing illness requires retreatment for possible neurosyphilis and should be managed in consultation with an expert.
Tertiary Syphilis
Tertiary syphilis refers to gummas and cardiovascular syphilis but not to neurosyphilis. Persons who are not allergic to penicillin and have no evidence of neurosyphilis should be treated with the following regimen.
Recommended Regimen
Tertiary Syphilis with Normal CSF Examination
- Benzathine penicillin G 7.2 million units total, administered as 3 doses of 2.4 million units IM each at 1-week intervals
Other Management Considerations
All persons who have tertiary syphilis should be tested for HIV infection and should receive a CSF examination before therapy is initiated. Persons with CSF abnormalities should be treated with a neurosyphilis regimen. Some providers treat all persons who have cardiovascular syphilis with a neurosyphilis regimen. These persons should be managed in consultation with an infectious-disease specialist. Limited information is available concerning clinical response and follow-up of persons who have tertiary syphilis.
Neurosyphilis Treatment
CNS involvement can occur during any stage of syphilis, and CSF laboratory abnormalities are common in persons with early syphilis, even in the absence of clinical neurologic findings. No evidence exists to support variation from recommended treatment for syphilis at any stage for persons without clinical neurologic findings, with the exception of tertiary syphilis. If clinical evidence of neurologic involvement is observed (e.g., cognitive dysfunction, motor or sensory deficits, ophthalmic or auditory symptoms, cranial nerve palsies, and symptoms or signs of meningitis or stroke), a CSF examination should be performed.
Syphilitic uveitis or other ocular manifestations (e.g., neuroretinitis and optic neuritis) can be associated with neurosyphilis. A CSF examination should be performed in all instances of ocular syphilis, even in the absence of clinical neurologic findings. Ocular syphilis should be managed in collaboration with an ophthalmologist and according to the treatment and other recommendations for neurosyphilis, even if a CSF examination is normal. In instances of ocular syphilis and abnormal CSF test results, follow-up CSF examinations should be performed to assess treatment response.
Recommended Regimen
Neurosyphilis and Ocular Syphilis
- Aqueous crystalline penicillin G 18–24 million units per day, administered as 3–4 million units IV every 4 hours or continuous infusion, for 10–14 days
If compliance with therapy can be ensured, the following alternative regimen might be considered.
Alternative Regimen
- Procaine penicillin G 2.4 million units IM once daily, PLUS Probenecid 500 mg orally four times a day, both for 10–14 days
The durations of the recommended and alternative regimens for neurosyphilis are shorter than the duration of the regimen used for latent syphilis. Therefore, benzathine penicillin, 2.4 million units IM once per week for up to 3 weeks, can be considered after completion of these neurosyphilis treatment regimens to provide a comparable total duration of therapy.
Penicillin Allergy
Limited data suggest that ceftriaxone 2 g daily either IM or IV for 10–14 days can be used as an alternative treatment for persons with neurosyphilis 55. Cross-sensitivity between ceftriaxone and penicillin can occur, but the risk for penicillin cross-reactivity between third-generation cephalosporins is negligible 56 (see Management of Persons Who Have a History of Penicillin Allergy). If concern exists regarding the safety of ceftriaxone for a patient with neurosyphilis, skin testing should be performed (if available) to confirm penicillin allergy and, if necessary, penicillin desensitization in consultation with a specialist is recommended. Other regimens have not been adequately evaluated for treatment of neurosyphilis.
Other Management Considerations
The following are other considerations in the management of persons who have neurosyphilis:
- All persons who have neurosyphilis should be tested for HIV.
- Although systemic steroids are used frequently as adjunctive therapy for otologic syphilis, such drugs have not been proven to be beneficial.
Follow-Up
If CSF pleocytosis was present initially, a CSF examination should be repeated every 6 months until the cell count is normal. Follow-up CSF examinations also can be used to evaluate changes in the CSF-Venereal Disease Research Laboratory (VDRL) or CSF protein after therapy; however, changes in these two parameters occur more slowly than cell counts, and persistent abnormalities might be less important 49. Leukocyte count is a sensitive measure of the effectiveness of therapy. If the cell count has not decreased after 6 months, or if the CSF cell count or protein is not normal after 2 years, retreatment should be considered. Limited data suggest that in immunocompetent persons and persons with HIV infection on highly active antiretroviral therapy, normalization of the serum RPR titer predicts normalization of CSF parameters following neurosyphilis treatment 49.
Penicillin Allergy
Infants and children who require treatment for congenital syphilis but who have a history of penicillin allergy or develop an allergic reaction presumed secondary to penicillin should be desensitized and then treated with penicillin (see Management of Persons with a History of Penicillin Allergy). Skin testing remains unavailable for infants and children because the procedure has not been standardized for this age group. Data are insufficient regarding the use of other antimicrobial agents (e.g., ceftriaxone) for congenital syphilis in infants and children. If a nonpenicillin G agent is used, close clinical, serologic, and CSF follow-up is required in consultation with an expert.
Management of Persons Who Have a History of Penicillin Allergy
No proven alternatives to penicillin are available for treating neurosyphilis, congenital syphilis, or syphilis in pregnant women. Penicillin also is recommended, whenever possible, for persons with HIV infection. The prevalence of reported penicillin allergy in the United States is about 8%–10% 57 and might be higher in hospitalized persons 58. The prevalence of reported penicillin allergy in developing countries is unknown; however, limited data suggest that penicillin is one of the most frequently reported allergies in some developing countries 59. Of persons reporting penicillin allergy, 10%–15% have a positive skin test suggestive of a penicillin allergy; these persons are at risk for an immunoglobulin E (IgE)-mediated allergic response to penicillin such as urticaria, angioedema, or anaphylaxis (i.e., upper airway obstruction, bronchospasm, or hypotension) 56. Re-administration of penicillin to patients with a history of IgE-mediated hypersensitivity reactions can cause severe, immediate reactions. Because anaphylactic reactions to penicillin can be fatal, every effort should be made to avoid administering penicillin to penicillin-allergic persons, unless they undergo induction of drug tolerance (also referred to as “desensitization”) to temporarily eliminate IgE-mediated hypersensitivity. However, many persons with a reported history of penicillin allergy likely have had other types of adverse drug reactions or have lost their sensitivity to penicillin over time and can safely be treated with penicillin.
Penicillin skin testing with the major and minor determinants of penicillin can reliably identify persons at high risk for IgE-mediated reactions to penicillin 60. Although the testing reagents are easily generated, only the major determinant (benzylpenicilloyl poly-L-lysine [Pre-Pen]) and penicillin G have been available commercially. These two tests identify an estimated 90%–99% of the allergic patients. However, because skin testing without the minor determinants would still fail to identify 1%–10% of allergic persons and because serious or fatal reactions can occur among these minor-determinant–positive persons, caution should be exercised when the full battery of skin-test reagents is not available (Table 1) 61. Manufacturers are working on a minor determinant mixture, but at the time of publication, no such product has been cleared by FDA for use in the United States. Penicillin skin testing has been used in a variety of settings to improve antibiotic use 62.
Table 1. Skin-test reagents for identifying persons at risk for adverse reactions to penicillin
Major Determinant
- Benzylpenicilloyl poly-L-lysine (PrePen) (AllerQuest, Plainville Connecticut) (6 x 10–5M)
Minor Determinant Precursors*
- Benzylpenicillin G (10–2M, 3.3 mg/mL, 10,000 units/mL)
- Benzylpenicilloate (10–2M, 3.3 mg/mL)
- Benzylpenicilloate (or penicilloyl propylamine) (10–2M, 3.3 mg/mL)
Positive Control
- Commercial histamine for scratch testing (1.0 mg/mL)
Negative Control
- Diluent (usually saline) or allergen diluent
Footnote: * Aged penicillin is not an adequate source of minor determinants. Penicillin G should either be freshly prepared or come from a fresh-frozen source.
[Source 63]Some studies have reported cross-reactivity rates as high as 10% among persons with a history of penicillin allergy who take cephalosporins. However, more recent studies indicate a lower rate (<2.5%) of cross reactivity between these drugs 56. Risk is highest with first-generation cephalosporins and cephalosporins that have similar R-group side chains to specific penicillins 64. The risk for penicillin cross-reactivity between most second-generation (cefoxitin) and all third generation cephalosporins (cefixime and ceftriaxone) is negligible 56; cefoxitin, cefixime, and ceftriaxone do not have an R group side chain similar to penicillin G.
Recommendations
Persons with a history of severe non-IgE-mediated reactions (e.g., Stevens-Johnson syndrome, toxic epidermal necrolysis, interstitial nephritis, and hemolytic anemia) are not candidates for skin testing or challenge and should avoid penicillins indefinitely. If the full battery of skin-test reagents is available, including both major and minor determinants (see Penicillin Allergy Skin Testing), persons who report a history of penicillin reaction and who are skin-test negative can receive conventional penicillin therapy. Persons with positive skin test results should be desensitized before initiating treatment.
If the full battery of skin-test reagents, including the minor determinants, is not available, skin testing should be conducted using the major determinant (Pre-Pen) and penicillin G. Those persons who have positive test results should be desensitized. For persons with negative skin tests, a subsequent observed challenge to the penicillin of choice is recommended. In addition, for persons with a history of severe or recent suspected IgE-mediated reactions to penicillin with negative skin testing, the penicillin of choice should be given by graded challenge. If the major determinant is not available for skin testing, all persons with a history suggesting IgE-mediated reactions to penicillin (e.g., anaphylaxis, angioedema, bronchospasm, or urticaria) should be desensitized in a hospital setting. In persons with reactions not likely to be IgE-mediated, outpatient-monitored graded challenges can be considered.
Penicillin Allergy Skin Testing
Persons at high risk for anaphylaxis, including those who 1) have a history of penicillin-related anaphylaxis or other IgE-mediated reactions, asthma, or other diseases that would make anaphylaxis more dangerous or 2) are being treated with beta-adrenergic blocking agents should be tested with 100-fold dilutions of the full-strength skin-test reagents before being tested with full-strength reagents. In these situations, testing should be performed in a monitored setting in which treatment for an anaphylactic reaction is available. If possible, antihistamines (e.g., chlorpheniramine maleate, fexofenadine, diphenhydramine HCL, and hydroxyzine) should not have been taken within the 5 days before skin testing.
Procedures
Dilute the antigens in saline either 100-fold for preliminary testing (if the patient has had a IgE- mediated reaction to penicillin) or 10-fold (if the patient has had another type of immediate, generalized reaction to penicillin within the preceding year). Pre-Pen is provided full-strength (6 x 10–5 meq penicilloyl) in a single dose ampoule. Penicillin G is diluted to 10,000 IU/ml in saline and aliquoted in sterile vials that remain stable for at least 6 months if frozen.
Epicutaneous (Prick) Tests
Duplicate drops of skin-test reagent are placed on the volar surface of the forearm. The underlying epidermis is pierced with a 26-gauge needle without drawing blood. An epicutaneous test is positive if the average wheal diameter after 15 minutes is ≥4 mm larger than that of negative controls; otherwise, the test is negative. The histamine controls should be positive to ensure that results are not falsely negative because of the effect of antihistaminic drugs.
Intradermal Test
If epicutaneous tests are negative, duplicate 0.02-mL intradermal injections of negative control and antigen solutions are made into the volar surface of the forearm by using a 26- or 27-gauge needle on a syringe. The margins of the wheals induced by the injections should be marked with a ball point pen. An intradermal test is positive if the average wheal diameter 15 minutes after injection is >2 mm larger than the initial wheal size and also is >2 mm larger than the histamine controls. Otherwise, the tests are negative. If the duplicates are discordant, a second set of duplicate tests can be used to resolve the ambiguity.
Desensitization
Persons who have a positive skin test to one of the penicillin determinants can be desensitized (Table 2). This is a straightforward, relatively safe procedure that can be performed orally or intravenously. Modified protocols might be considered based on an individual’s symptoms, drug of choice, and route of administration 65. Although the two approaches have not been compared, oral desensitization is regarded as safer and easier to perform. Desensitization should occur in a hospital setting because serious IgE-mediated allergic reactions can occur; the procedure can usually be completed in approximately 4–12 hours, after which time the first dose of penicillin is administered. After desensitization, penicillin should be maintained continuously for the duration of the course of therapy. Once the course is completed, if penicillin is required in the future, the desensitization procedure should be repeated.
Table 2. Oral desensitization protocol for persons with a positive skin test*
| Penicillin V suspension dose† | Amount§ (units/mL) | mL | Units | Cumulative dose (units) |
|---|---|---|---|---|
| 1 | 1,000 | 0.1 | 100 | 100 |
| 2 | 1,000 | 0.2 | 200 | 300 |
| 3 | 1,000 | 0.4 | 400 | 700 |
| 4 | 1,000 | 0.8 | 800 | 1,500 |
| 5 | 1,000 | 1.6 | 1,600 | 3,100 |
| 6 | 1,000 | 3.2 | 3,200 | 6,300 |
| 7 | 1,000 | 6.4 | 6,400 | 12,700 |
| 8 | 10,000 | 1.2 | 12,000 | 24,700 |
| 9 | 10,000 | 2.4 | 24,000 | 48,700 |
| 10 | 10,000 | 4.8 | 48,000 | 96,700 |
| 11 | 80,000 | 1.0 | 80,000 | 176,700 |
| 12 | 80,000 | 2.0 | 160,000 | 336,700 |
| 13 | 80,000 | 4.0 | 320,000 | 656,700 |
| 14 | 80,000 | 8.0 | 640,000 | 1,296,700 |
Footnotes:
* Observation period was 30 minutes before parenteral administration of penicillin.
† Interval between doses, 15–30 minutes; elapsed time, 4–8 hours; cumulative dose, 1.3 million units.
§ The specific amount of drug was diluted in approximately 30 mL of water and then administered orally.
[Source 66]- Syphilis – CDC Fact Sheet (Detailed). https://www.cdc.gov/std/syphilis/stdfact-syphilis-detailed.htm[↩]
- https://phil.cdc.gov/Details.aspx?pid=21621[↩]
- Izard J, Renken C, Hsieh CE, Desrosiers DC, Dunham-Ems S, La Vake C, Gebhardt LL, Limberger RJ, Cox DL, Marko M, Radolf JD. Cryo-electron tomography elucidates the molecular architecture of Treponema pallidum, the syphilis spirochete. J Bacteriol. 2009 Dec;191(24):7566-80. doi: 10.1128/JB.01031-09[↩]
- Centers for Disease Control and Prevention.Sexually Transmitted Disease Surveillance, 2016. Atlanta, GA: Department of Health and Human Services; September 2017. https://www.cdc.gov/std/stats16/default.htm[↩]
- Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2015 MMWR, 64(RR-3) (2015) https://www.cdc.gov/std/tg2015/default.htm[↩][↩][↩][↩]
- Alexander, J.M., et al., Efficacy of treatment for syphilis in pregnancy. Obstet Gynecol, 1999. 93(1): p. 5-8.[↩][↩]
- Marra CM. Neurosyphilis. Continuum (Minneap Minn). 2015 Dec;21(6 Neuroinfectious Disease):1714-28. doi: 10.1212/CON.0000000000000250[↩][↩][↩][↩][↩]
- Ho EL, Lukehart SA. Syphilis: using modern approaches to understand an old disease. J Clin Invest. 2011 Dec;121(12):4584-92. doi: 10.1172/JCI57173[↩][↩]
- Rolfs RT, Joesoef MR, Hendershot EF, Rompalo AM, Augenbraun MH, Chiu M, Bolan G, Johnson SC, French P, Steen E, Radolf JD, Larsen S. A randomized trial of enhanced therapy for early syphilis in patients with and without human immunodeficiency virus infection. The Syphilis and HIV Study Group. N Engl J Med. 1997 Jul 31;337(5):307-14. doi: 10.1056/NEJM199707313370504[↩]
- Lukehart SA, Hook EW 3rd, Baker-Zander SA, Collier AC, Critchlow CW, Handsfield HH. Invasion of the central nervous system by Treponema pallidum: implications for diagnosis and treatment. Ann Intern Med. 1988 Dec 1;109(11):855-62. doi: 10.7326/0003-4819-109-11-855[↩]
- Hook EW 3rd, Marra CM. Acquired syphilis in adults. N Engl J Med. 1992 Apr 16;326(16):1060-9. doi: 10.1056/NEJM199204163261606[↩]
- Ghanem KG, Ram S, Rice PA. The Modern Epidemic of Syphilis. N Engl J Med. 2020 Feb 27;382(9):845-854. doi: 10.1056/NEJMra1901593[↩][↩]
- Woolston SL, Dhanireddy S, Marrazzo J. Ocular Syphilis: a Clinical Review. Curr Infect Dis Rep. 2016 Nov;18(11):36. doi: 10.1007/s11908-016-0542-9[↩][↩]
- Spoor TC, Wynn P, Hartel WC, Bryan CS. Ocular syphilis. Acute and chronic. J Clin Neuroophthalmol. 1983 Sep;3(3):197-203.[↩][↩][↩]
- Moradi A, Salek S, Daniel E, Gangaputra S, Ostheimer TA, Burkholder BM, Leung TG, Butler NJ, Dunn JP, Thorne JE. Clinical features and incidence rates of ocular complications in patients with ocular syphilis. Am J Ophthalmol. 2015 Feb;159(2):334-43.e1. doi: 10.1016/j.ajo.2014.10.030[↩]
- Syphilis. https://www.cdc.gov/std/treatment-guidelines/syphilis.htm[↩][↩][↩][↩][↩]
- Ramchandani MS, Litvack JR, Marra CM. Otosyphilis: A Review of the Literature. Sex Transm Dis. 2020 May;47(5):296-300. doi: 10.1097/OLQ.0000000000001155[↩][↩]
- Theeuwen, H., Whipple, M. and Litvack, J.R. (2019), Otosyphilis: Resurgence of an Old Disease. The Laryngoscope, 129: 1680-1684. https://doi.org/10.1002/lary.27635[↩][↩][↩]
- Medoro AK, Sánchez PJ. Syphilis in Neonates and Infants. Clin Perinatol. 2021 Jun;48(2):293-309. doi: 10.1016/j.clp.2021.03.005[↩][↩][↩][↩]
- Peeling RW, Mabey D, Kamb ML, Chen XS, Radolf JD, Benzaken AS. Syphilis. Nat Rev Dis Primers. 2017 Oct 12;3:17073. doi: 10.1038/nrdp.2017.73[↩][↩]
- Syphilis. https://www.cdc.gov/std/statistics/2020/overview.htm#Syphilis[↩][↩]
- Rac MW, Revell PA, Eppes CS. Syphilis during pregnancy: a preventable threat to maternal-fetal health. Am J Obstet Gynecol. 2017 Apr;216(4):352-363. doi: 10.1016/j.ajog.2016.11.1052[↩]
- Rathbun KC. Congenital syphilis. Sex Transm Dis. 1983 Apr-Jun;10(2):93-9. doi: 10.1097/00007435-198304000-00009[↩]
- Lafond RE, Lukehart SA. Biological basis for syphilis. Clin Microbiol Rev. 2006 Jan;19(1):29-49. doi: 10.1128/CMR.19.1.29-49.2006[↩]
- Cremin BJ, Fisher RM. The lesions of congenital syphilis. Br J Radiol. 1970 May;43(509):333-41. doi: 10.1259/0007-1285-43-509-333[↩][↩]
- Fiumara NJ, Lessell S. Manifestations of Late Congenital Syphilis: An Analysis of 271 Patients. Arch Dermatol. 1970;102(1):78–83. doi:10.1001/archderm.1970.04000070080012[↩]
- CDC, Association of Public Health Laboratories. Laboratory diagnostic testing for Treponema pallidum, Expert Consultation Meeting Summary Report, January 13-15, 2009, Atlanta, GA. https://www.aphl.org/programs/infectious_disease/std/Documents/ID_2009Jan_Laboratory-Guidelines-Treponema-pallidum-Meeting-Report.pdf[↩]
- Romanowski B, Sutherland R, Fick GH, et al. Serologic response to treatment of infectious syphilis. Ann Intern Med 1991;114:1005–9.[↩]
- CDC. Discordant results from reverse sequence syphilis screening–five laboratories, United States, 2006-2010. MMWR Morbid Mortal Wkly Rep 2011;60:133–7.[↩]
- Park IU, Chow JM, Bolan G, et al. Screening for syphilis with the treponemal immunoassay: analysis of discordant serology results and implications for clinical management. J Infect Dis 2011;204:1297–304.[↩]
- Lukehart SA, Hook EW, III, Baker-Zander SA, et al. Invasion of the central nervous system by Treponema pallidum: implications for diagnosis and treatment. Ann Intern Med 1988;109:855–62.[↩][↩]
- Jaffe HW, Larsen SA, Peters M, et al. Tests for treponemal antibody in CSF. Arch Intern Med 1978;138:252–5.[↩]
- Marra CM, Maxwell CL, Smith SL, et al. Cerebrospinal fluid abnormalities in patients with syphilis: association with clinical and laboratory features. J Infect Dis 2004;189:369–76.[↩]
- Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. Syphilis. MMWR Recomm Rep. 2015;64(No. RR-3):1-137.[↩]
- Centers for Disease Control and Prevention (CDC). Discordant results from reverse sequence syphilis screening–five laboratories, United States, 2006-2010. MMWR Morb Mortal Wkly Rep. 2011;60:133-7.[↩]
- Centers for Disease Control and Prevention. Discordant results from reverse sequence syphilis screening–five laboratories, United States, 2006-2010. MMWR Morb Mortal Wkly Rep, 2011. 60(5): p. 133-7. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6005a1.htm[↩]
- Kingston AA, Vujevich J, Shapiro M, et al. Seronegative secondary syphilis in 2 patients coinfected with human immunodeficiency virus. Arch Dermatol 2005;141:431–3.[↩]
- Syphilis. 2015 Sexually Transmitted Diseases Treatment Guidelines. https://www.cdc.gov/std/tg2015/syphilis.htm[↩]
- CDC. Inadvertent use of Bicillin® C-R to treat syphilis infection-Los Angeles, California, 1999-2004. MMWR Morbid Mortal Wkly Rep 2005;54:217–9.[↩]
- Workowski KA, Bachmann LH, Chan PA, Johnston CM, Muzny CA, Park I, Reno H, Zenilman JM, Bolan GA. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm Rep. 2021 Jul 23;70(4):1-187. doi: 10.15585/mmwr.rr7004a1[↩]
- Brown ST. Adverse reactions in syphilis therapy. J Am Vener Dis Assoc. 1976;3:172-6.[↩]
- Sena AC, Wolff M, Martin DH, et al. Predictors of serological cure and Serofast State after treatment in HIV-negative persons with early syphilis. Clin Infect Dis 2011;53:1092–9.[↩][↩][↩]
- Sena AC, Wolff M, Behets F, et al. Response to therapy following retreatment of serofast early syphilis patients with benzathine penicillin. Clin Infect Dis 2013;56:420–2.[↩]
- Taiwan HIV and Syphilis Study Group. Comparison of effectiveness of 1 dose versus 3 doses of benzathine penicillin in treatment of early syphilis in HIV-infected patients: multicenter, prospective observational study in Taiwan [Abstract# S-119]. Presented at: the 20th Conference on Retroviruses and Opportunistic Infections (CROI 2013); March 3-6, 2013; Atlanta, GA.[↩][↩]
- Hagdrup HK, Lange Wantzin G, Secher L, et al. Penicillin concentrations in serum following weekly injections of benzathine penicillin G. Chemotherapy 1986;32:99–101.[↩]
- Nathan L, Bawdon RE, Sidawi JE, et al. Penicillin levels following the administration of benzathine penicillin G in pregnancy. Obstet Gynecol 1993;82:338–42.[↩][↩]
- CDC. Symptomatic early neurosyphilis among HIV-positive men who have sex with men–four cities, United States, January 2002-June 2004. MMWR Morb Mortal Wkly Rep 2007;56:625–8.[↩]
- Rolfs RT, Joesoef MR, Hendershot EF, et al. The Syphilis and HIV Study Group. A randomized trial of enhanced therapy for early syphilis in patients with and without human immunodeficiency virus infection. N Engl J Med 1997;337:307–14.[↩]
- Marra CM, Maxwell CL, Tantalo LC, et al. Normalization of serum rapid plasma reagin titer predicts normalization of cerebrospinal fluid and clinical abnormalities after treatment of neurosyphilis. Clin Infect Dis 2008;47:893–9.[↩][↩][↩]
- Alexander JM, Sheffield JS, Sanchez PJ, et al. Efficacy of treatment for syphilis in pregnancy. Obstet Gynecol 1999;93:5–8.[↩]
- Walker GJ. Antibiotics for syphilis diagnosed during pregnancy. Cochrane Database Syst Rev 2001:CD001143.[↩]
- Hawkes S, Matin N, Broutet N, et al. Effectiveness of interventions to improve screening for syphilis in pregnancy: a systematic review and meta-analysis. Lancet Infect Dis 2011;11:684–91.[↩]
- Hollier LM, Harstad TW, Sanchez PJ, et al. Fetal syphilis: clinical and laboratory characteristics. Obstet Gynecol 2001;97:947–53.[↩]
- Klein VR, Cox SM, Mitchell MD, et al. The Jarisch-Herxheimer reaction complicating syphilotherapy in pregnancy. Obstet Gynecol 1990;75(3 Pt 1):375–80.[↩]
- Shann S, Wilson J. Treatment of neurosyphilis with ceftriaxone. Sex Transm Infect 2003;79:415–6.[↩]
- Ahmed KA, Fox SJ, Frigas E, et al. Clinical outcome in the use of cephalosporins in pediatric patients with a history of penicillin allergy. International Arch Allergy Immunol 2012;158:405–10.[↩][↩][↩][↩]
- Albin S, Agarwal S. Prevalence and characteristics of reported penicillin allergy in an urban outpatient adult population. Allergy Asthma Proc 2014;35:489–94.[↩]
- Lee CE, Zembower TR, Fotis MA, et al. The incidence of antimicrobial allergies in hospitalized patients: implications regarding prescribing patterns and emerging bacterial resistance. Arch Intern Med 2000;160:2819–22.[↩]
- Jares EJ, Sanchez-Borges M, Cardona-Villa R, et al. Multinational experience with hypersensitivity drug reactions in Latin America. Ann Allergy Asthma Immunol 2014;113:282–9.[↩]
- Wong BB, Keith PK, Waserman S. Clinical history as a predictor of penicillin skin test outcome. Annals Asthma Allergy Immunol 2006;97:169–74.[↩]
- Macy E, Ngor EW. Safely diagnosing clinically significant penicillin allergy using only penicilloyl-poly-lysine, penicillin, and oral amoxicillin. J Allergy Clin Immunol Pract 2013;1:258–63.[↩]
- Raja AS, Lindsell CJ, Bernstein JA, et al. The use of penicillin skin testing to assess the prevalence of penicillin allergy in an emergency department setting. Annals Emerg Med 2009;54:72–7.[↩]
- Saxon A, Beall GN, Rohr AS, Adelman DC. Immediate hypersensitivity reactions to beta-lactam antibiotics. Ann Intern Med 1987;107:204–15.[↩]
- Vega JM, Blanca M, Garcia JJ, et al. Immediate allergic reactions to amoxicillin. Allergy 1994;49:317–22.[↩]
- Legere HJ, 3rd, Palis RI, Rodriguez Bouza T, et al. A safe protocol for rapid desensitization in patients with cystic fibrosis and antibiotic hypersensitivity. Journal of Cystic Fibrosis 2009;8:418–24.[↩]
- Wendel GO, Jr, Stark BJ, Jamison RB, Melina RD, Sullivan TJ. Penicillin allergy and desensitization in serious infections during pregnancy. N Engl J Med 1985;312:1229–32.[↩]