Contents
- What is menstruation
- How does my menstrual cycle affect my health?
- When does a girl usually get her first period?
- What is a normal amount of bleeding during my period?
- How often should I change my pad, tampon, menstrual cup, sponge, or period panties?
- What is toxic shock syndrome?
- How long is a typical menstrual cycle?
- How does my menstrual cycle change as I get older?
- How long does a woman usually have periods?
- Why should I keep track of my menstrual cycle?
- How can I keep track of my menstrual cycle?
- What is ovulation?
- How do I know if I’m ovulating?
- Menstruation cycle
- What are symptoms of menstruation
- When is menstrual bleeding abnormal?
- Menstruation problems
- What causes menstruation problems
- Menstruation problems diagnosis
- Common treatments for menstrual problems
What is menstruation
Menstruation often called your “period”, is normal vaginal bleeding that occurs as part of a woman’s monthly menstrual cycle. Every month, your body prepares the uterus lining for pregnancy. If no pregnancy occurs, the uterus, or womb, sheds the uterine lining through the small opening in your cervix and pass out of your body through your vagina. The menstrual blood is partly blood and partly tissue from inside the uterus. It passes out of your body through your vagina.
Your menstrual cycle is the monthly hormonal cycle a female’s body goes through to prepare for pregnancy. Your menstrual cycle is counted from the first day of your period up to the first day of your next period. Your hormone levels (estrogen and progesterone) usually change throughout the menstrual cycle and can cause menstrual symptoms.
During the monthly menstrual cycle, the uterus lining builds up to prepare for pregnancy. If you do not get pregnant, estrogen and progesterone hormone levels begin falling. Very low levels of estrogen and progesterone tell your body to begin menstruation.
Periods usually start between age 11 and 14 (a girl’s first period is called menarche) and continue until menopause at about age 51 1. In the United States, most girls start menstruating shortly after 12 years of age 2. The average menstruation time in normally menstruating women is 3 to 5 days 3 but a normal menstrual period can lasts up to 8 days 4. Besides bleeding from the vagina, you may have:
- Abdominal or pelvic cramping pain
- Lower back pain
- Bloating and sore breasts
- Food cravings
- Mood swings and irritability
- Headache and fatigue
Premenstrual syndrome, or PMS, is a group of symptoms that start before the period. It can include emotional and physical symptoms.
Consult your health care provider if you have big changes in your cycle. They may be signs of other problems that should be treated.
Bleeding in any of the following situations is considered abnormal uterine bleeding:
- Bleeding or spotting between periods
- Bleeding or spotting after sex
- Heavy bleeding during your period
- Menstrual cycles that are longer than 38 days or shorter than 24 days
- “Irregular” periods in which cycle length varies by more than 7–9 days
- Bleeding after menopause
Some of the causes of abnormal bleeding include the following:
- Problems with ovulation
- Fibroids and polyps
- A condition in which the endometrium grows into the wall of the uterus
- Bleeding disorders
- Problems linked to some birth control methods, such as an intrauterine device (IUD) or birth control pills
- Miscarriage
- Ectopic pregnancy
- Certain types of cancer, such as cancer of the uterus
Your obstetrician–gynecologist (ob-gyn) or other health care professional may start by checking for problems most common in your age group. Some of them are not serious and are easy to treat. Others can be more serious. All should be checked.
Based on your symptoms and your age, other tests may be needed. Some of these tests can be done in your ob-gyn’s office. Others may be done at a hospital or surgical center:
- Ultrasound exam—Sound waves are used to make a picture of the pelvic organs.
- Hysteroscopy—A thin, lighted scope is inserted through the vagina and the opening of the cervix. It allows your ob-gyn or other health care professional to see the inside of the uterus.
- Endometrial biopsy—A sample of the endometrium is removed and looked at under a microscope.
- Sonohysterography—Fluid is placed in the uterus through a thin tube while ultrasound images are made of the inside of the uterus.
- Magnetic resonance imaging (MRI)—An MRI exam uses a strong magnetic field and sound waves to create images of the internal organs.
- Computed tomography (CT)—This X-ray procedure shows internal organs and structures in cross section.
You also may have a pregnancy test and tests for sexually transmitted infections (STIs).
Medications often are tried first to treat irregular or heavy menstrual bleeding. The medications that may be used include the following:
- Hormonal birth control methods—Birth control pills, the skin patch, and the vaginal ring contain hormones. These hormones can lighten menstrual flow. They also help make periods more regular.
- Gonadotropin-releasing hormone (GnRH) agonists—These drugs can stop the menstrual cycle and reduce the size of fibroids.
- Tranexamic acid—This medication treats heavy menstrual bleeding.
- Nonsteroidal anti-inflammatory drugs (NSAIDs)—These drugs, which include ibuprofen, may help control heavy bleeding and relieve menstrual cramps.
- Antibiotics—If you have an infection, you may be given an antibiotic.
- Special medications—If you have a bleeding disorder, your treatment may include medication to help your blood clot.
- If medication does not reduce your bleeding, a surgical procedure may be needed. There are different types of surgery depending on your condition, your age, and whether you want to have more children.
Endometrial ablation destroys the lining of the uterus. It stops or reduces the total amount of bleeding. Pregnancy is not likely after ablation, but it can happen. If it does, the risk of serious complications, including life-threatening bleeding, is greatly increased. If you have this procedure, you will need to use birth control until after menopause.
Uterine artery embolization is a procedure used to treat fibroids. This procedure blocks the blood vessels to the uterus, which in turn stops the blood flow that fibroids need to grow. Another treatment, myomectomy, removes the fibroids but not the uterus.
Hysterectomy, the surgical removal of the uterus, is used to treat some conditions or when other treatments have failed. Hysterectomy also is used to treat endometrial cancer. After the uterus is removed, a woman can no longer get pregnant and will no longer have periods.
See your doctor about your period if:
- You have gone three months without a period and are not pregnant, breastfeeding, or in perimenopause or menopause.
- You get irregular periods (your period happens more often than every 24 days or less often than every 38 days, or lasts longer than 8 days).
- You feel dizzy, lightheaded, weak, or tired, or you have chest pain or trouble breathing during or after your period.
- You bleed through one or more pads or tampons every one to two hours.
- You suddenly get a fever and feel sick after using tampons.
- You have menstrual pain that doesn’t get better with over-the-counter pain medicine, such as ibuprofen or naproxen.
- You have period pain, cramps, or heavy bleeding that makes you miss work, school, or other daily activities.
- You get a migraine around your period or your regular migraine treatment stops working.
- You have blood clots in your menstrual flow that are larger than a quarter.
- You have bleeding after sex, more than once.
- You have spotting or bleeding any time in the menstrual cycle other than during your period.
- You have bleeding after menopause.
How does my menstrual cycle affect my health?
Changing hormone levels throughout your menstrual cycle can cause health problems or make health problems worse:
- Anemia. Heavy menstrual bleeding is the most common cause of iron-deficiency anemia in women of childbearing age. Anemia is a condition that happens when your blood cannot carry enough oxygen to all of the different parts of your body because it does not have enough iron. This makes you pale or feel tired or weak.
- Asthma. Your asthma symptoms may be worse during some parts of your cycle.
- Depression. Women with a history of depression are more likely to have PMS or premenstrual dysphoric disorder (PMDD). Symptoms of depression may be worse just before their periods.
- Diabetes. Women with irregular menstrual cycles, especially those longer than 40 days, have a higher risk for type 2 diabetes.
- Irritable bowel syndrome (IBS). IBS causes cramping, bloating, and gas. Your IBS symptoms may get worse right before your period.
- Problems getting pregnant. Health problems, such as endometriosis, polycystic ovary syndrome (PCOS) or underweight or obesity, can cause irregular periods. This can make it harder to get pregnant.
When does a girl usually get her first period?
The average age for a girl in the United States to get her first period is 12 5. This does not mean that all girls start at the same age.
A girl may start her period anytime between 8 and 15. The first period normally starts about two years after breasts first start to develop and pubic hair begins to grow. The age at which a girl’s mother started her period can help predict when a girl may start her period.
A girl should see her doctor if:
- She starts her period before age 8.
- She has not had her first period by age 15.
- She has not had her first period within three years of breast growth.
What is a normal amount of bleeding during my period?
The average woman loses about two to three tablespoons of blood during her period. Your periods may be lighter or heavier than the average amount. What is normal for you may not be the same for someone else. Also, the flow may be lighter or heavier from month to month.
Your periods may also change as you get older. Some women have heavy bleeding during perimenopause, the transition to menopause. Symptoms of heavy menstrual bleeding may include:
- Bleeding through one or more pads or tampons every one to two hours
- Passing blood clots larger than the size of quarters
- Bleeding that often lasts longer than eight days
How often should I change my pad, tampon, menstrual cup, sponge, or period panties?
Follow the instructions that came with your period product. Try to change or rinse your feminine hygiene product before it becomes soaked through or full.
- Most women change their pads every few hours.
- A tampon should not be worn for more than 8 hours because of the risk of toxic shock syndrome
- Menstrual cups and sponges may only need to be rinsed once or twice a day.
- Period panties (underwear with washable menstrual pads sewn in) can usually last about a day, depending on the style and your flow.
Use a product appropriate in size and absorbency for your menstrual bleeding. The amount of menstrual blood usually changes during a period. Some women use different products on different days of their period, depending on how heavy or light the bleeding is.
What is toxic shock syndrome?
Toxic shock syndrome (TSS) is a rare but sometimes deadly condition caused by bacteria that make toxins or poisons. In 1980, 63 women died from toxic shock syndrome. A certain brand of super absorbency tampons was said to be the cause. These tampons were taken off the market.
Today, most cases of toxic shock syndrome are not caused by using tampons. But, you could be at risk for toxic shock syndrome if you use more absorbent tampons than you need for your bleeding or if you do not change your tampon often enough (at least every four to eight hours). Menstrual cups, cervical caps, sponges, or diaphragms (anything inserted into your vagina) may also increase your risk for toxic shock syndrome if they are left in place for too long (usually 24 hours). Remove sponges within 30 hours and cervical caps within 48 hours 6.
If you have any symptoms of toxic shock syndrome, take out the tampon, menstrual cup, sponge, or diaphragm, and call your local emergency services number or go to the hospital right away.
Symptoms of toxic shock syndrome include 7:
- Sudden high fever
- Muscle aches
- Vomiting
- Nausea
- Diarrhea
- Rash
- Kidney or other organ failure
How long is a typical menstrual cycle?
The typical menstrual cycle is 28 days long, but each woman is different 8. Also, a woman’s menstrual cycle length might be different from month-to-month. Your periods are still “regular” if they usually come every 24 to 38 days 9. This means that the time from the first day of your last period up to the start of your next period is at least 24 days but not more than 38 days.
Some women’s periods are so regular that they can predict the day and time that their periods will start. Other women are regular but can only predict the start of their period within a few days.
How does my menstrual cycle change as I get older?
Your cycles may change in different ways as you get older. Often, periods are heavier when you are younger (in your teens) and usually get lighter in your 20s and 30s. This is normal.
- For a few years after your first period, menstrual cycles longer than 38 days are common. Girls usually get more regular cycles within three years of starting their periods. If longer or irregular cycles last beyond that, see your doctor or nurse to rule out a health problem, such as polycystic ovary syndrome (PCOS) 10
- In your 20s and 30s, your cycles are usually regular and can last anywhere from 24 to 38 days.
- In your 40s, as your body starts the transition to menopause, your cycles might become irregular. Your menstrual periods might stop for a month or a few months and then start again. They also might be shorter or last longer than usual, or be lighter or heavier than normal.
Talk to your doctor or nurse if you have menstrual cycles that are longer than 38 days or shorter than 24 days, or if you are worried about your menstrual cycle.
How long does a woman usually have periods?
On average, women get a period for about 40 years of their life 11. Most women have regular periods until perimenopause, the time when your body begins the change to menopause. Perimenopause, or transition to menopause, may take a few years. During this time, your period may not come regularly. Menopause happens when you have not had a period for 12 months in a row. For most women, this happens between the ages of 45 and 55. The average age of menopause in the United States is 52.
Periods also stop during pregnancy and may not come back right away if you breastfeed.
But if you don’t have a period for 90 days (three months), and you are not pregnant or breastfeeding, talk to your doctor or nurse. Your doctor will check for pregnancy or a health problem that can cause periods to stop or become irregular.
Why should I keep track of my menstrual cycle?
If your periods are regular, tracking them will help you know when you ovulate, when you are most likely to get pregnant, and when to expect your next period to start.
If your periods are not regular, tracking them can help you share any problems with your doctor or nurse.
If you have period pain or bleeding that causes you to miss school or work, tracking these period symptoms will help you and your doctor or nurse find treatments that work for you. Severe pain or bleeding that causes you to miss regular activities is not normal and can be treated.
How can I keep track of my menstrual cycle?
You can keep track of your menstrual cycle by marking the day you start your period on a calendar. After a few months, you can begin to see if your periods are regular or if your cycles are different each month.
You may want to track:
- Premenstrual syndrome (PMS) symptoms: Did you have cramping, headaches, moodiness, forgetfulness, bloating, or breast tenderness?
- When your bleeding begins: Was it earlier or later than expected?
- How heavy the bleeding was on your heaviest days: Was the bleeding heavier or lighter than usual? How many pads or tampons did you use?
- Period symptoms: Did you have pain or bleeding on any days that caused you to miss work or school?
- How many days your period lasted: Was your period shorter or longer than the month before?
You can also download apps (sometimes for free) for your phone to track your periods. Some include features to track your PMS symptoms, energy and activity levels, and more.
What is ovulation?
Ovulation is when the ovary releases an egg so it can be fertilized by a sperm in order to make a baby. A woman is most likely to get pregnant if she has sex without birth control in the three days before and up to the day of ovulation (since the sperm are already in place and ready to fertilize the egg as soon as it is released). A man’s sperm can live for 3 to 5 days in a woman’s reproductive organs, but a woman’s egg lives for just 12 to 24 hours after ovulation.
Each woman’s cycle length may be different, and the time between ovulation and when the next period starts can be anywhere from one week (7 days) to more than 2 weeks (19 days) 12.
At different times in a woman’s life, ovulation may or may not happen:
- Women who are pregnant do not ovulate.
- Women who are breastfeeding may or may not ovulate. Women who are breastfeeding should talk to their doctor about birth control methods if they do not
- want to get pregnant.
- During perimenopause, the transition to menopause, you may not ovulate every month.
- After menopause you do not ovulate.
How do I know if I’m ovulating?
A few days before you ovulate, your vaginal mucus or discharge changes and becomes more slippery and clear. This type of mucus helps sperm move up into your uterus and into the fallopian tubes where it can fertilize an egg. Some women feel minor cramping on one side of their pelvic area when they ovulate. Some women have other signs of ovulation.
Luteinizing hormone (LH) is a hormone released by your brain that tells the ovary to release an egg (called ovulation). LH levels begin to surge upward about 36 hours before ovulation, so some women and their doctors test for LH levels. LH levels peak about 12 hours before ovulation 13. Women who are tracking ovulation to become pregnant will notice a slight rise in their basal temperature (your temperature after sleeping before you get out of bed) around ovulation.
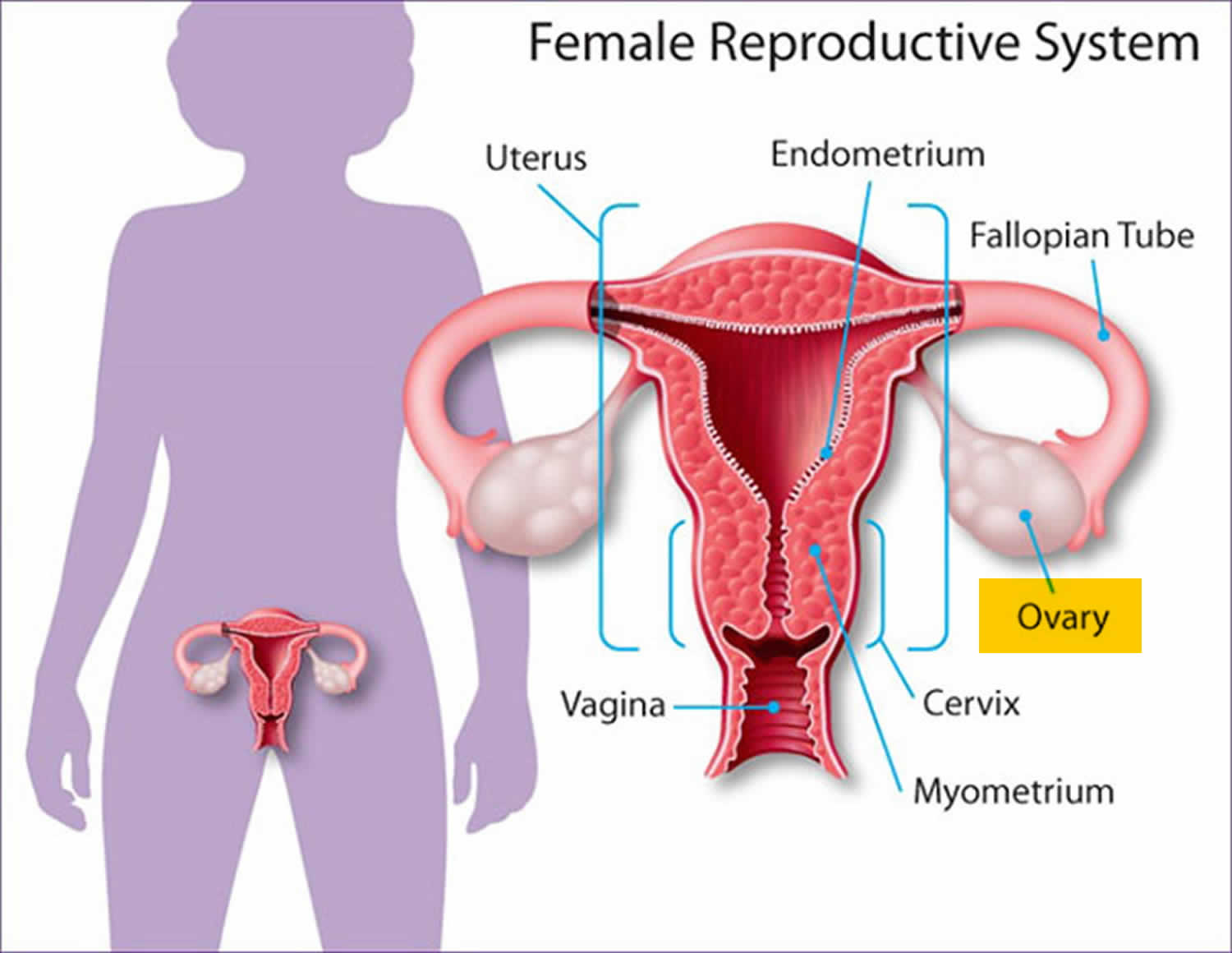
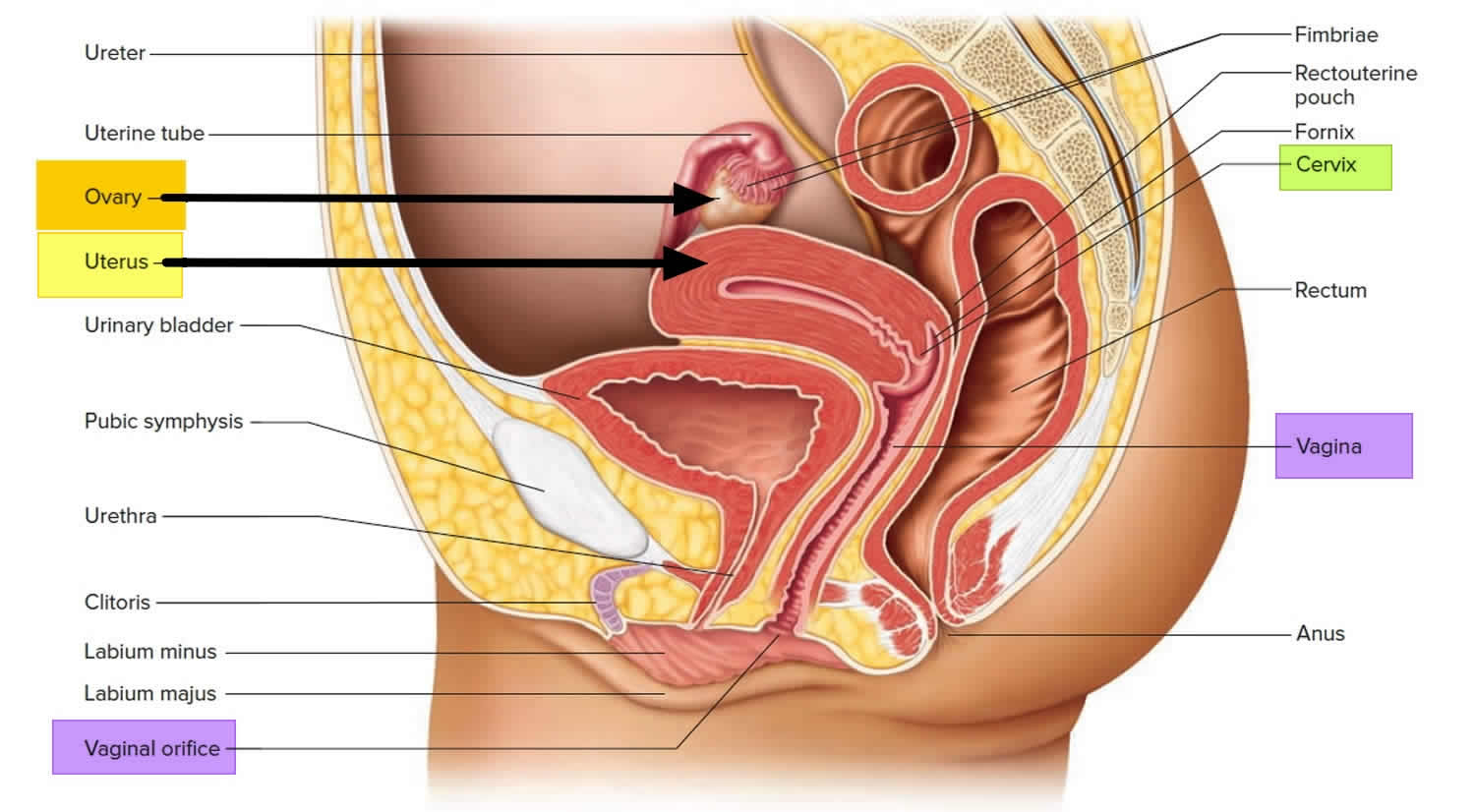
Figure 1. Female reproductive organs
Menstruation cycle
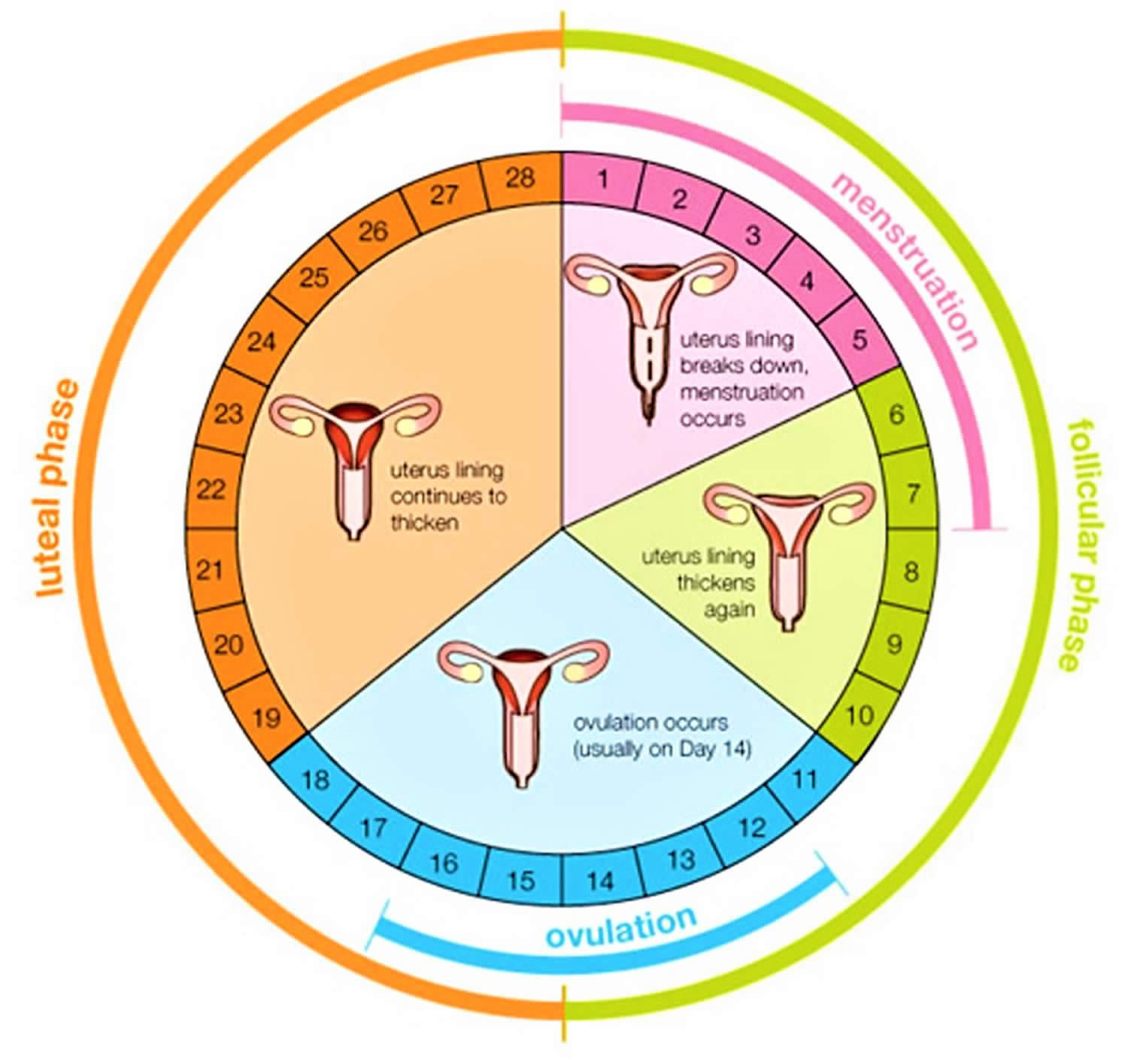
The menstrual cycle is the monthly process in which female hormones stimulate an ovary to release an egg, thicken the lining of the uterus to support a pregnancy, and then cause the uterus to shed this lining (through menstruation) if there is no pregnancy. The average menstrual cycle is 28 days, but this varies between women and from month to month. In teens, the menstrual cycle can range from 21 to 45 days, but for most women, it is 21 to 35 days 2.
The menstrual cycle is characterized by regular, recurring changes in the endometrium, which culminate in menstrual bleeding (menses). Such cycles usually begin around age thirteen and continue into the early fifties, then cease.
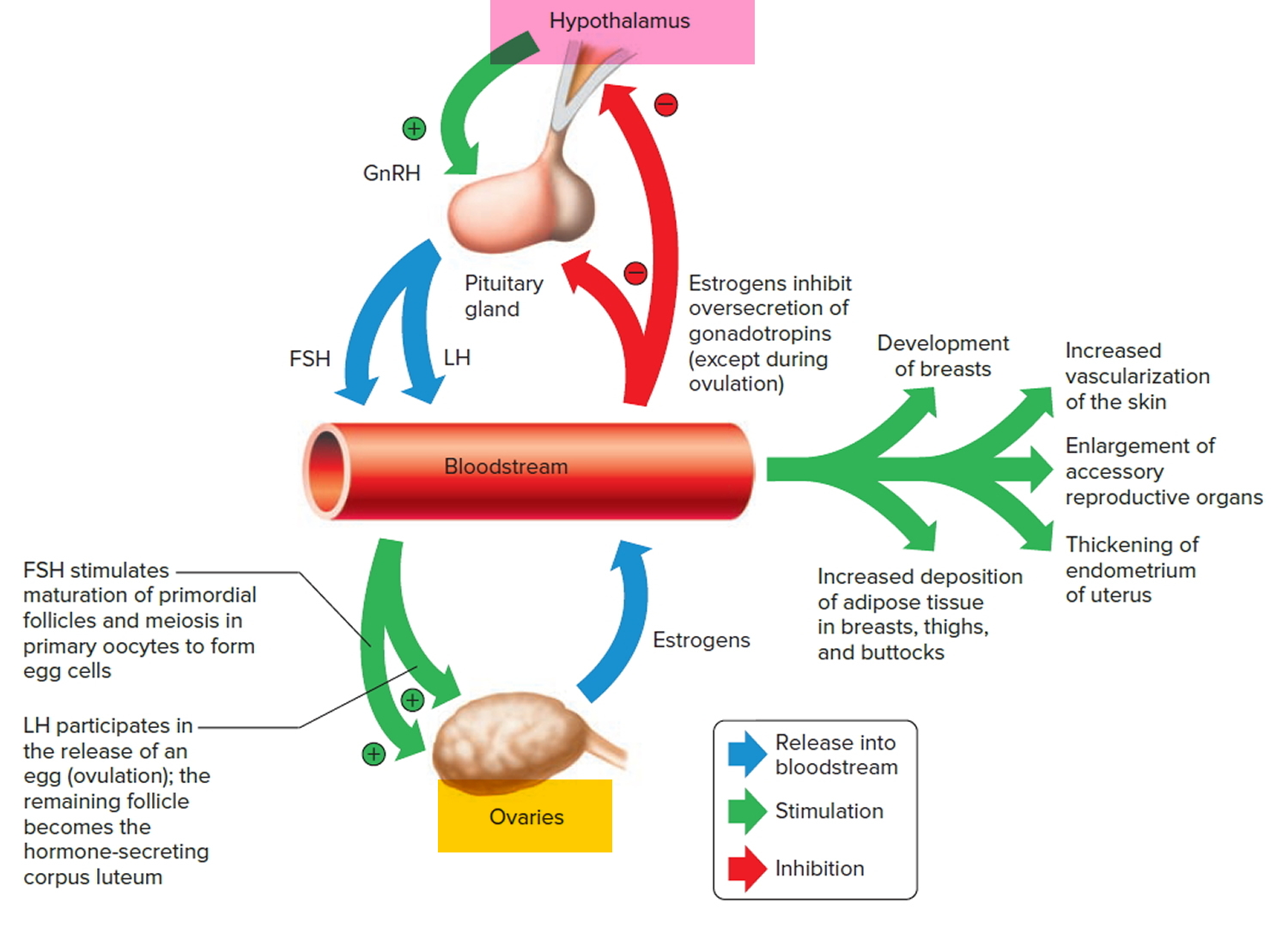
A female’s first menstrual cycle, called menarche, occurs after the ovaries and other organs of the reproductive control system mature and begin responding
to certain hormones. Then, the hypothalamic secretion of gonadotropin-releasing hormone (GnRH) stimulates the anterior pituitary to release threshold levels of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Follicle-stimulating hormone (FSH) stimulates the final maturation of an ovarian follicle. The follicular cells produce increasing amounts of estrogens and some progesterone. Luteinizing hormone (LH) stimulates certain ovarian cells to secrete precursor molecules (such as testosterone), also used to produce estrogens.
In a young female, estrogens stimulate the development of secondary sex characteristics. Estrogens secreted during subsequent menstrual cycles continue the development and maintenance of these characteristics.
Figure 3. Pituitary gland hormones under the influence of the hypothalamus controlling the ovaries production of egg cell, ovulation and development of the female secondary sex characteristics
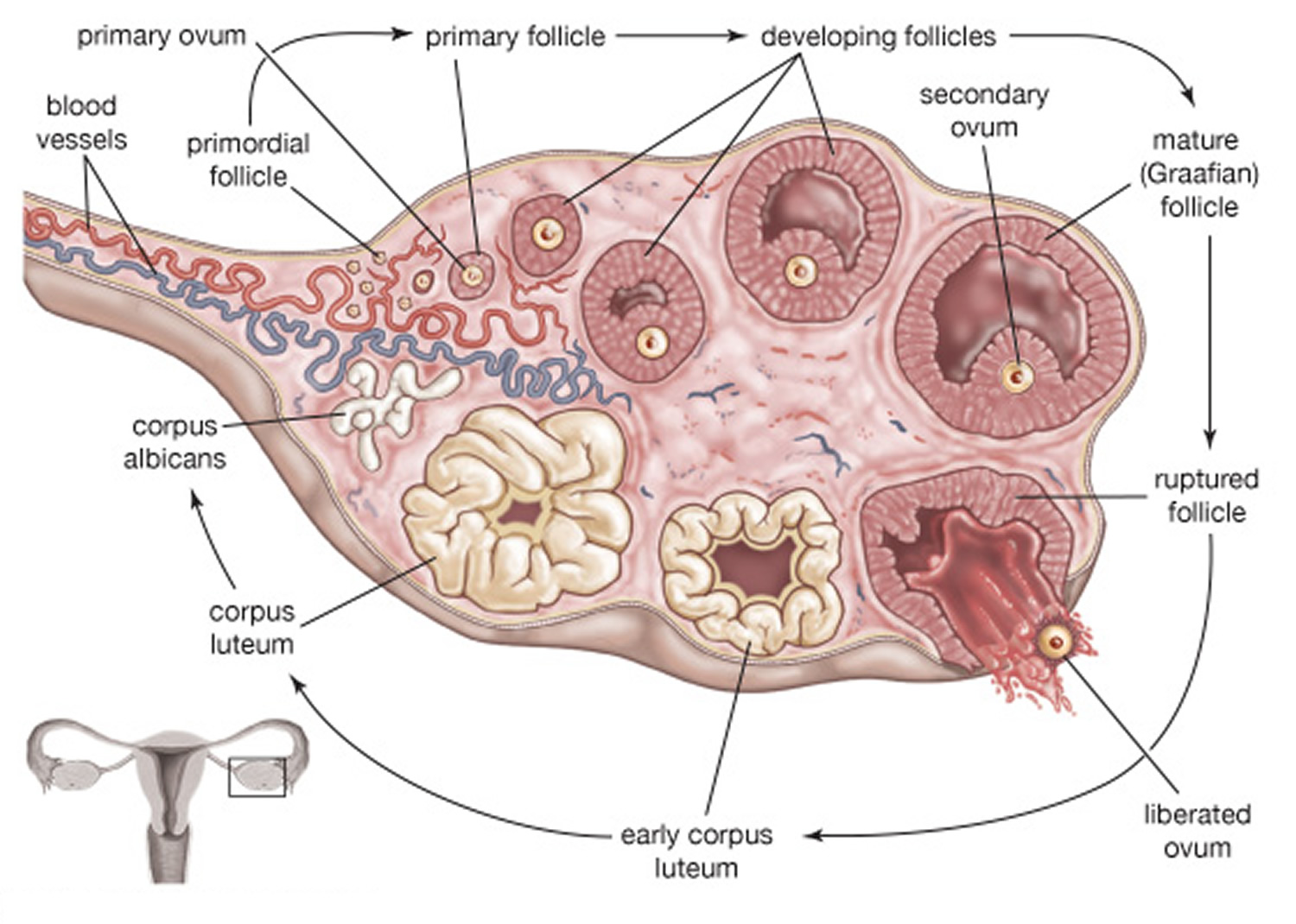
Figure 4. Ovarian Follicle Maturation
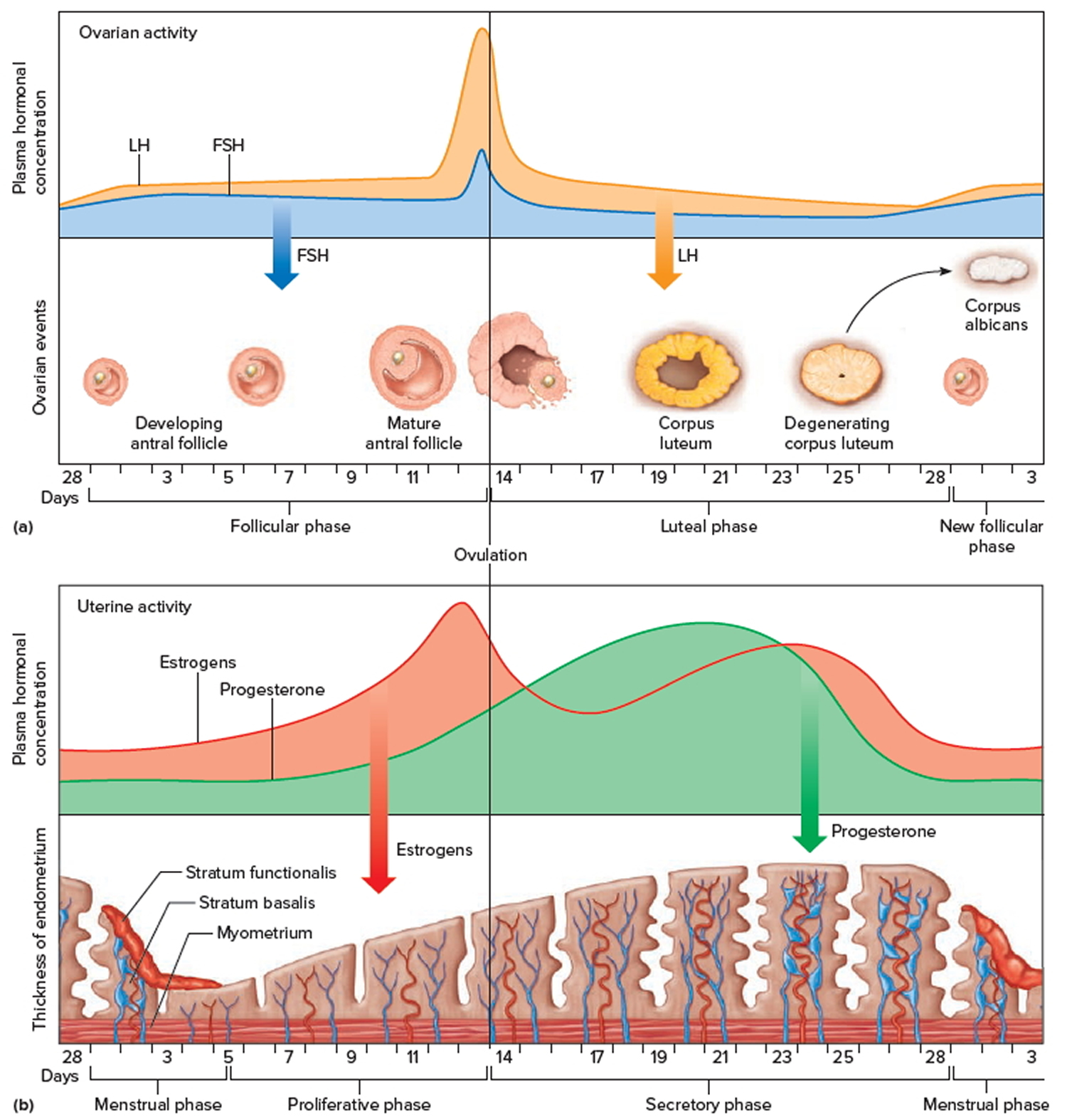
Figure 5. Ovarian activity during the Menstrual cycle
Note: Major events in the female menstrual cycle. (a) Plasma hormonal concentrations of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) affect follicle maturation in the ovaries. (b) Plasma hormonal concentrations of estrogen and progesterone influence changes in the uterine lining.
Increasing concentration of estrogens during the first week or so of a menstrual cycle changes the uterine lining, thickening the glandular endometrium (proliferative phase). Meanwhile, the follicle fully matures, and by around the fourteenth day of the cycle, the antral follicle appears on the ovary surface as a blisterlike bulge. Within the follicle, the follicular cells, which surround and connect the secondary oocyte to the inner wall, loosen. Follicular fluid accumulates.
While the follicle matures, it secretes estrogens that inhibit the release of luteinizing hormone (LH) from the anterior pituitary gland but allow luteinizing hormone (LH) to be stored in the gland. Estrogens also make anterior pituitary cells more sensitive to the action of gonadotropin-releasing hormone (GnRH), which is released from the hypothalamus in rhythmic pulses about ninety minutes apart.
Near the fourteenth day of follicular development, the anterior pituitary cells finally respond to the pulses of GnRH (gonadotropin-releasing hormone) and release the stored LH (luteinizing hormone). The resulting surge in LH concentration lasts about thirty-six hours. In response to the LH, the primary oocyte completes meiosis I. The LH (luteinizing hormone) also acts with FSH (follicle-stimulating hormone) inducing complex interactions with prostaglandins, progesterone, plasmin, and proteolytic enzymes, leading to the weakening and rupturing of the bulging follicular wall. This event sends the secondary oocyte and follicular fluid out of the ovary (ovulation).
Following ovulation, the space containing the follicular fluid fills with blood, which soon clots. Under the influence of LH (luteinizing hormone), the remnants of the follicle within the ovary form a temporary glandular structure in the ovary called a corpus luteum (“yellow body”).
Follicular cells secrete some progesterone during the first part of the menstrual cycle. During the second half of the cycle, cells of the corpus luteum secrete abundant progesterone and estrogens. Consequently, as a corpus luteum forms, the blood progesterone concentration sharply increases.
Progesterone causes the endometrium to become more vascular and glandular. It also stimulates the uterine glands to secrete more glycogen and lipids (secretory phase). The endometrial tissues fill with fluids containing nutrients and electrolytes, which provide a favorable environment for an embryo to develop.
High levels of estrogens and progesterone inhibit the anterior pituitary gland’s release of LH (luteinizing hormone) and FSH (follicle-stimulating hormone). Consequently, no other follicles are stimulated to complete development when the corpus luteum is active. However, if the secondary oocyte released at ovulation is not fertilized, the corpus luteum begins to degenerate (regress) on about the twenty-fourth day of the cycle. Eventually, connective tissue replaces it. The remnant of such a corpus luteum is called a corpus albicans, and is eventually absorbed.
When the corpus luteum ceases to function, concentrations of estrogens and progesterone rapidly decline, and in response, blood vessels in the endometrium constrict. This reduces the supply of oxygen and nutrients to the thickened endometrium (stratum functionalis and stratum basalis), and these lining tissues soon disintegrate and slough off. At the same time, blood leaves damaged capillaries, creating a flow of blood and cellular debris that passes through the vagina as the menstrual flow (menses). This flow usually begins about the twenty-eighth day of the cycle and continues for three to five days, while the concentrations of estrogens are relatively low. The beginning of the menstrual flow marks the end of a menstrual cycle and the beginning of the next cycle as a new developing antral follicle becomes available.
Low blood concentrations of estrogens and progesterone at the beginning of the menstrual cycle mean that the hypothalamus and anterior pituitary gland are no longer inhibited. Consequently, FSH (follicle-stimulating hormone) and LH (luteinizing hormone) concentrations soon increase, stimulating a new antral follicle to mature. As this follicle secretes estrogens, the uterine lining undergoes repair, and the endometrium begins to thicken again.
Day 1
The first day of bleeding is considered the first day of the menstrual cycle. After bleeding ends, usually around day 5, levels of the hormone estrogen begin to rise. The rise in estrogen causes the lining of the uterus to thicken as it prepares to hold a fertilized egg. At the same time, the changes in hormone levels cause follicles (the sacs in the ovary that contain eggs) to grow and mature, in preparation for one follicle to go through ovulation.
Ovulation
Around day 12 to 14 in an average 28-day cycle, the egg is released from a follicle on the ovary in a process called ovulation. Ovulation can occur anywhere between 10 and 21 days after the first day of a woman’s menstrual cycle. Ovulation is when the ovary releases an egg so it can be fertilized by a sperm to make a baby. A woman is most likely to get pregnant if she has sex without birth control in the three days before and up to the day of ovulation.
It may be difficult to know when you ovulate, but you can watch for signs. A few days before you ovulate, your vaginal mucus or discharge changes and becomes
more slippery and clear. A woman can also tell when she has begun ovulating using several methods, including at-home tests that measure levels of luteinizing hormone (LH) in the urine and keeping track of her body temperature, which typically rises slightly at ovulation. At mid-cycle, some women experience pain on one side of their pelvic area; this pain is called “Mittelschmerz” (meaning “middle pain,” because it occurs in the middle of the cycle) and may be a signal of ovulation 14.
More than 90 percent of women say they get symptoms of premenstrual syndrome (PMS) in the time after ovulation and before their period starts.
If a pregnancy does not occur, decreasing hormone levels signal for the lining of the uterus, called the endometrium, to be shed during menstruation.
The endometrium builds up and breaks down during the menstrual cycle. The endometrium is thickest halfway through the 28-day cycle. Then, if there is no pregnancy, it breaks down. This breakdown causes the bleeding of the menstrual phase. Figure 5 above illustrates an average 28-day cycle.
What happens if a pregnancy occurs?
Fertilization
After ovulation, the egg (ovum) moves down the fallopian tube (also called uterine tube). The sperm can fertilize the egg at this point. After the sperm is ejaculated into the vagina, it moves into the cervix and through the uterus into the fallopian tube (uterine tube). Sperm can live up to 5 days in a woman’s body.
If fertilization occurs, the newly formed embryo travels through the fallopian tube into the uterus, where it implants in the wall of the uterus. If fertilization does not occur, the egg naturally breaks down, and the uterine wall is lost in the form of menstrual bleeding.
Implantation
The embryo must successfully implant into the thickened wall of the uterus for the pregnancy to occur. The embryo first attaches to the wall of the uterus around 5 or 6 days after ovulation. It becomes more firmly implanted between 6 and 12 days after ovulation. Implantation causes a release of human chorionic gonadotropin (hCG)—a hormone that signals the body to change to support the pregnancy. This hormone is what a pregnancy test detects.
What are symptoms of menstruation
The primary sign of menstruation is bleeding from the vagina. Additional symptoms include:
- Abdominal or pelvic cramping
- Lower back pain
- Bloating and sore breasts
- Food cravings
- Mood swings and irritability
- Headache
- Fatigue
When is menstrual bleeding abnormal?
Bleeding in any of the following situations is considered abnormal uterine bleeding:
- Bleeding or spotting between periods
- Bleeding or spotting after sex
- Heavy bleeding during your period
- Menstrual cycles that are longer than 38 days or shorter than 24 days
- “Irregular” periods in which cycle length varies by more than 7–9 days
- Bleeding after menopause
Menstruation problems
For most women, a normal menstrual cycle ranges from 21 to 35 days 15. However, 14% to 25% of women of childbearing age have irregular menstrual cycles, meaning the cycles are shorter or longer than normal; are heavier or lighter than normal; or are experienced with other problems, like abdominal cramps 16. Irregular cycles can be ovulatory, meaning that ovulation occurs, or anovulatory, meaning ovulation does not occur.
The most common menstrual irregularities include:
- Amenorrhea or absent menstrual periods: When a woman does not get her period by age 16, or when she stops getting her period for at least 3 months and is not pregnant 1.
- Oligomenorrhea or infrequent menstrual periods: Periods that occur more than 35 days apart 17
- Menorrhagia or heavy menstrual periods: Also called excessive bleeding. Although anovulatory bleeding and menorrhagia are sometimes grouped together, they do not have the same cause and require different diagnostic testing 18
- Prolonged menstrual bleeding: Bleeding that exceeds 8 days in duration on a regular basis 17
- Dysmenorrhea: Painful periods that may include severe menstrual cramps 19
Additional menstrual irregularities include:
- Polymenorrhea: Frequent menstrual periods occurring less than 21 days apart 17
- Irregular menstrual periods with a cycle-to-cycle variation of more than 20 days 17
- Shortened menstrual bleeding of less than 2 days in duration 17
- Intermenstrual bleeding: Episodes of bleeding that occur between periods, also known as spotting 17
What causes menstruation problems
Menstrual irregularities can have a variety of causes, including pregnancy, hormonal imbalances, infections, diseases, trauma, and certain medications 15, 1, 20.
Causes of irregular periods (generally light) include 1:
- Perimenopause (generally in the late 40s and early 50s)
- Primary ovarian insufficiency
- Eating disorders (anorexia nervosa or bulimia)
- Excessive exercise
- Thyroid dysfunction (too much or too little thyroid hormone)
- Elevated levels of the hormone prolactin, which is made by the pituitary gland to help the body produce milk
- Uncontrolled diabetes
- Cushing’s syndrome (elevated levels of the hormone cortisol, used in the body’s response to stress)
- Late-onset congenital adrenal hyperplasia (problem with the adrenal gland)
- Hormonal birth control (birth control pills, injections, or implants)
- Hormone-containing intrauterine devices (IUDs)
- Scarring within the uterine cavity (Asherman’s syndrome)
- Medications, such as those to treat epilepsy or mental health problems
Common causes of heavy or prolonged menstrual bleeding include 1, 20:
- Adolescence (during which cycles may not be associated with ovulation)
- Polycystic ovary syndrome (PCOS) (bleeding irregular but heavy)
- Uterine fibroids (benign growths of uterine muscle)
- Endometrial polyps (benign overgrowth of the lining of the uterus)
- Adenomyosis (the presence of uterine lining in the wall of the uterus)
- Nonhormonal IUDs
- Bleeding disorders, such as leukemia, platelet disorders, clotting factor deficiencies, or (less common) von Willebrand disease
- Pregnancy complications (miscarriage)
Common causes of dysmenorrhea (menstrual pain) include 21, 19:
- Endometriosis (uterine lining grows outside the uterus)
- Uterine abnormalities (fibroids or adenomyosis)
- IUDs (intrauterine devices)
- Pelvic scarring due to sexually transmitted infections, such as chlamydia or gonorrhea
- Heavy menstrual flow
Menstruation problems diagnosis
Your health care provider can diagnose menstrual problems using a combination of the following 1:
- Medical history
- Physical examination
- Blood tests
- Ultrasound examination
- Endometrial biopsy—a small sample of the uterus’s endometrial lining is taken to be examined under a microscope
- Hysteroscopy—a diagnostic scope that allows a health care provider to examine the inside of the uterus, typically done as an outpatient procedure
- Saline infusion sonohysterography—ultrasound imaging of the uterine cavity while it is filled with sterile saline solution
- Transvaginal ultrasonography—ultrasound imaging of the pelvic organs, including the ovaries and uterus, using an ultrasound transducer that is inserted into the vagina
Table 1. Evaluation of Abnormal Uterine Bleeding and Differential Diagnosis
| Category | Characteristics | Differential diagnosis | Evaluation | |||
|---|---|---|---|---|---|---|
| Anovulatory |
|
|
| |||
| Ovulatory |
|
|
| |||
TSH = thyroid-stimulating hormone.
*—Not usually needed in adolescents.
Anovulatory Bleeding
At extremes of the reproductive years, irregular cycles resulting from anovulation can occur. Following menarche, the immature hypothalamic-pituitary-ovarian axis may result in anovulatory cycles for two to three years 23. Up to eight years before menopause, women may again have intermittent anovulatory cycles 24. During the rest of the reproductive years, however, recurrent irregular cycles may be caused by anovulation and are considered abnormal 25.
When ovulation does not occur, no corpus luteum forms to produce progesterone, leading to prolonged estrogenic stimulation of the endometrium, excessive proliferation, endometrial instability, and erratic bleeding 25. Approximately 6 to 10 percent of women with anovulation have underlying polycystic ovary syndrome 25. Uncontrolled diabetes mellitus 23, hypo- or hyperthyroidism 26 and hyperprolactinemia4 also may cause anovulation by interfering with the hypothalamic-pituitary-ovarian axis 23. Antiepileptics (especially valproic acid [Depakene]) may cause weight gain, hyperandrogenism, and anovulation 27. Use of typical antipsychotics (e.g., haloperidol, chlorpromazine, thiothixene [Navane]) and some atypical antipsychotics (e.g., clozapine [Clozaril], risperidone [Risperdal]) may contribute to anovulation by raising prolactin levels 28.
Recurrent anovulation causes an increased risk of endometrial cancer 25. Endometrial cancer in adolescents is rare, but has been reported and should be considered if recurrent anovulation for two to three years or morbid obesity is present 29. About 14 percent of premenopausal women with recurrent anovulatory cycles develop endometrial cancer or its precursor, hyperplasia with atypia 30. Ten to 20 percent of endometrial cancers are diagnosed in premenopausal women 31. Women at highest risk of cancer have advanced age, obesity, nulliparity, infertility, diabetes, family history of colon cancer, long-term unopposed estrogen therapy, or a history of tamoxifen use 32. One study demonstrated the highest incidence of endometrial abnormality, ranging from hyperplasia without atypia to cancer, in premenopausal women 45 years or older with abnormal uterine bleeding (number needed to screen [NNS] = 13), women weighing 198 lb (90 kg) or greater (NNS = 8), or both (NNS = 5) 31. Hyperplasia without atypia is generally considered benign, with less than 5 percent of cases progressing to cancer 33. In contrast, 30 percent of cases of hyperplasia with atypia progress to cancer 33 and 42.6 percent of women with this pathology have undiagnosed, concurrent endometrial adenocarcinoma 34.
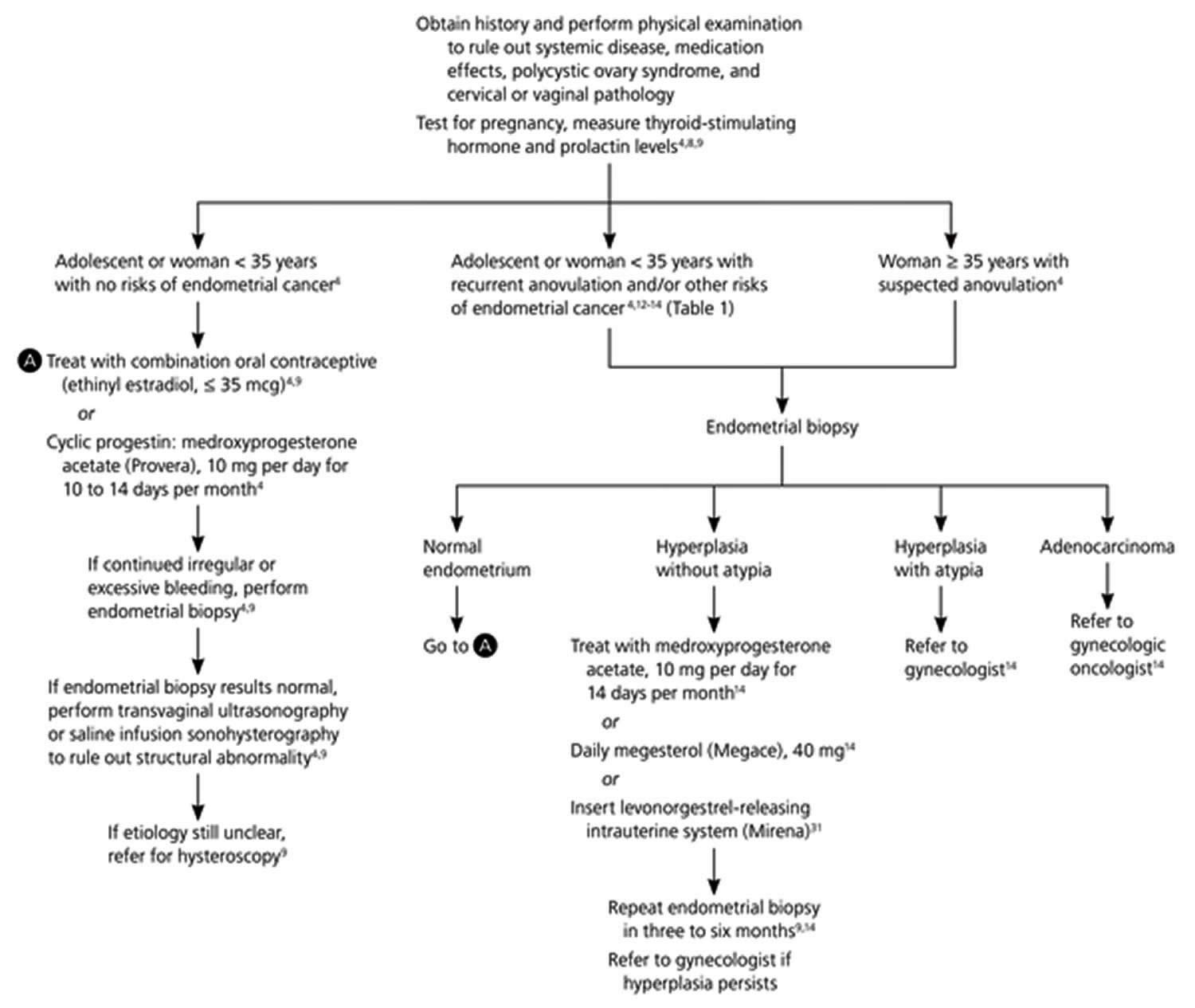
Evaluation of anovulatory uterine bleeding
Patients with irregular cycles who should be evaluated include adolescents with consistently more than three months between cycles6 or those with irregular cycles for more than three years4; women with suspected recurrent anovulatory cycles 25; and women who are likely perimenopausal and have increased volume or duration of bleeding over baseline, periods more often than every 21 days, intermenstrual spotting, or postcoital bleeding 35.
Initial evaluation of anovulatory uterine bleeding should include history, physical examination to look for obesity and hirsutism (manifestations of polycystic ovary syndrome), a pregnancy test, and measurement of thyroid-stimulating hormone and prolactin levels 25. The American College of Obstetricians and Gynecologists recommends endometrial tissue assessment to rule out cancer in adolescents and in women younger than 35 years with prolonged unopposed estrogen stimulation, women 35 years or older with suspected anovulatory bleeding, and women unresponsive to medical therapy 25. Office endometrial biopsy is relatively inexpensive, convenient, and has a low risk of complications 36. Findings may include benign endometrium, simple or complex hyperplasia without atypia, hyperplasia with atypia, or endometrial adenocarcinoma 32. In premenopausal women, endometrial biopsy is 82.3 percent sensitive for detecting hyperplasia with atypia and 91 percent sensitive for detecting endometrial cancer; specificity is 98 percent for both (Table 2) 37.
Women at low risk of endometrial cancer and women with benign endometrial histology who have continued irregular or excessive uterine bleeding despite treatment should undergo imaging to rule out concomitant structural changes 25. If no abnormalities are found, hysteroscopy should be considered 25. Figure 5 is an algorithm for the evaluation and treatment of anovulatory abnormal uterine bleeding 25.
Table 2. Imaging and Tissue Sampling for Detection of Endometrial Pathology in Premenopausal Women
| Test | Utility | Limitations or contraindications | Effectiveness |
|---|---|---|---|
Endometrial biopsy |
|
| 91 percent sensitive and 98 percent specific for detecting cancer |
82.3 percent sensitive and 98 percent specific for detecting hyperplasia with atypia | |||
Office hysteroscopy |
|
| 94 percent sensitive and 89 percent specific for detecting intracavitary abnormality (data pooled from pre- and postmenopausal women) |
Saline infusion sonohysterography |
|
| 88 to 99 percent sensitive and 72 to 95 percent specific for detecting intracavitary abnormality in premenopausal women |
Transvaginal ultrasonography |
|
| 60 to 92 percent sensitive and 62 to 93 percent specific for diagnosing intracavitary abnormality in premenopausal women |
[Source 22]
Figure 5. Algorithm for the evaluation and treatment of anovulatory abnormal uterine bleeding
[Source 22]Ovulatory Bleeding
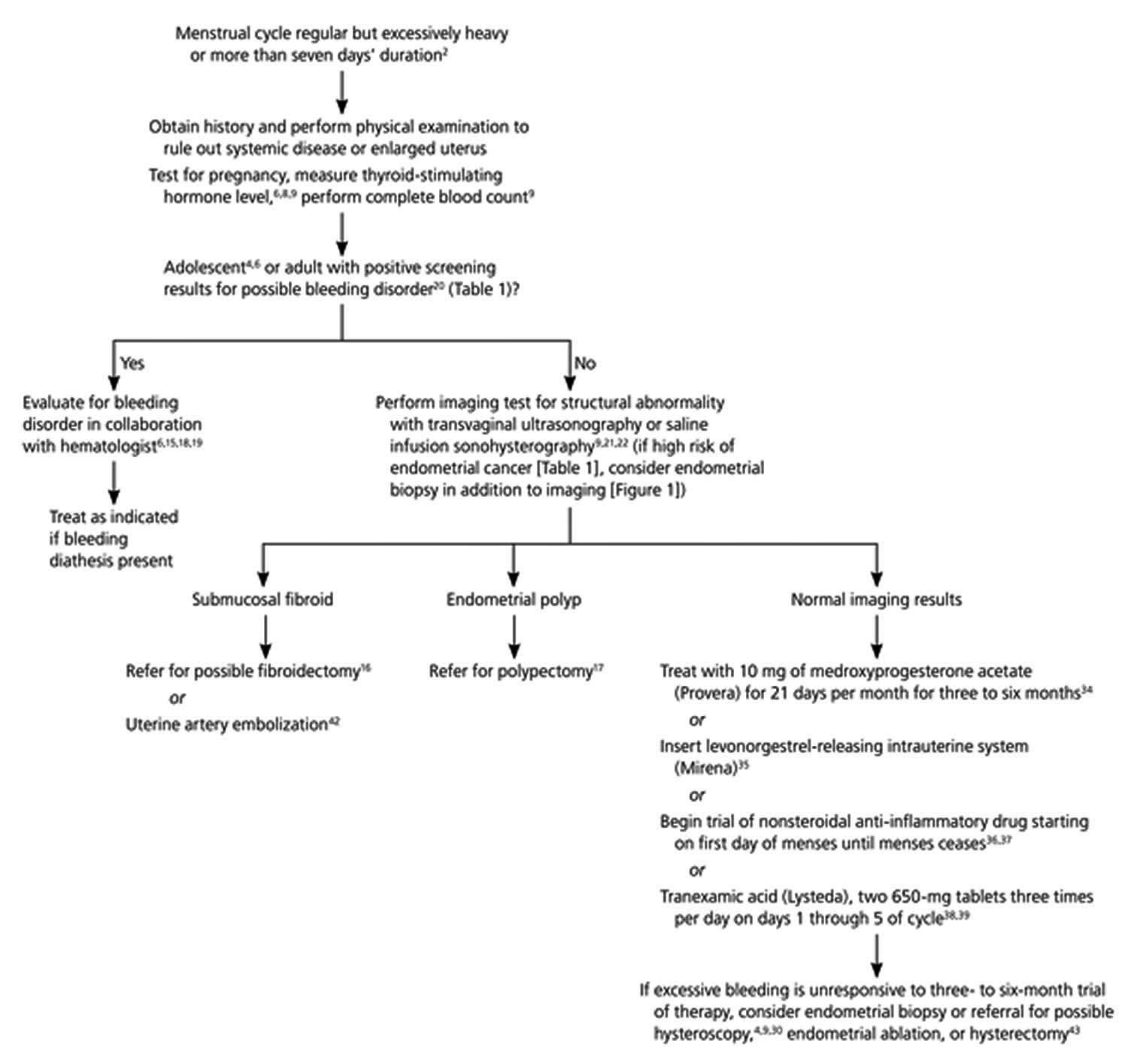
Ovulatory abnormal uterine bleeding or menorrhagia (heavy or prolonged menstrual bleeding), presents as bleeding that occurs at normal, regular intervals but that is excessive in volume or duration 24. Hypothyroidism, late-stage liver disease or bleeding disorders may cause menorrhagia, as may structural changes, such as submucosal fibroids or endometrial polyps 38. Von Willebrand disease (vWD), the most common heritable bleeding disorder, is present in approximately 13 percent of women with menorrhagia 39. The prevalence is likely higher in adolescents presenting with excessive uterine bleeding 23. In contrast to women with anovulatory bleeding, women with ovulatory bleeding produce progesterone, slough the endometrium regularly, and have minimal risk of developing cancer 30. Approximately one-half of women with menorrhagia have no discernable cause 40.
Evaluation of ovulatory abnormal uterine bleeding or menorrhagia
Initial evaluation of menorrhagia (heavy or prolonged menstrual bleeding) should include a pregnancy test, complete blood count and measurement of thyroid-stimulating hormone level 26. The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists recommend evaluating adolescents with menorrhagia for possible bleeding disorders, specifically von Willebrand disease 23. A woman with menorrhagia should be evaluated for a possible bleeding disorder if she has one or more of the following: a family history of bleeding disorder; menses lasting seven days or more with flooding or impairment of activities with most periods; a history of treatment for anemia; or a history of excessive bleeding with tooth extraction, delivery or miscarriage, or surgery 41. Initial testing for bleeding disorders includes complete blood count (to assess for anemia, leukemia, and thrombocytopenia), and prothrombin and activated partial thromboplastin time (to assess for factor deficiencies) 23. The approach to further testing for bleeding disorders, specifically von Willebrand disease, is varied, and collaboration with a hematologist is recommended 23.
Although uncommon in adolescents, uterine polyps and fibroids may underlie menorrhagia in women 38. Transvaginal ultrasonography is used to evaluate the ovaries, uterus, and endometrium 42. Saline infusion sonohysterography is the intrauterine infusion of saline during transvaginal ultrasonography that provides enhanced views of the endometrium 43. In two small studies of premenopausal women, transvaginal ultrasonography had 60 to 92 percent sensitivity and 62 to 93 percent specificity for diagnosing intracavitary lesions. In both studies, saline infusion sonohysterography improved sensitivity to 88 to 99 percent and specificity to 72 to 95 percent 43.
If no etiology is found on ultrasonography, if bleeding is unresponsive to medical therapy, or if there are considerable risks of endometrial cancer, additional evaluation with endometrial biopsy 25 or direct visualization of the endometrium with hysteroscopy is recommended 44. Hysteroscopy has a 94 percent sensitivity and 89 percent specificity for detecting intracavitary abnormalities 44.
Figure 6. Algorithm for the evaluation and treatment of ovulatory abnormal uterine bleeding
 [Source 22]
[Source 22]
Common treatments for menstrual problems
Treatments for menstrual irregularities often vary based on the type of menstrual problem and certain lifestyle factors, such as whether a woman is planning to get pregnant.
Treatment for menstrual problems that are due to anovulatory bleeding (absent periods, infrequent periods, and irregular periods) include 45:
- Oral contraceptives
- Cyclic progestin
- Treatments for an underlying disorder that is causing the menstrual problem, such as counseling and nutritional therapy for an eating disorder
Treatment for menstrual irregularities that are due to ovulatory bleeding (heavy or prolonged menstrual bleeding) include 18:
- Insertion of a hormone-releasing intrauterine device
- Use of various medications (such as those containing progestin or tranexamic acid) or nonsteroidal anti-inflammatory medications
If the cause is structural or if medical management is ineffective, then the following may be considered:
- Surgical removal of polyps or uterine fibroids
- Uterine artery embolization, a procedure to block blood flow to the uterus
- Endometrial ablation, a procedure to cauterize (remove or close off by burning) blood vessels in the endometrial lining of the uterus
- Hysterectomy
Treatment for dysmenorrhea (painful periods) include 46:
- Applying a heating pad to the abdomen
- Taking nonsteroidal anti-inflammatory medications
- Taking contraceptives, including injectable hormone therapy or birth control pills, using varied or less common treatment regimens
Table 3. Pharmacologic Treatment of Abnormal Uterine Bleeding
| Medication | Dosage | Comments | |
| Anovulatory bleeding | |||
| Combination oral contraceptives | ≤ 35 mcg of ethinyl estradiol monophasic or triphasic pills | Provides contraception | |
| Contraindications include smokers older than 35 years, personal history or high risk of deep venous thrombosis or pulmonary embolism, multiple risk factors for arterial cardiovascular disease, history of breast cancer, and severe cirrhosis or liver cancer | |||
| Medroxyprogesterone acetate (Provera) | 10 mg per day for 10 to 14 days per month | Does not provide contraception | |
| Caution in patients with severe hepatic dysfunction | |||
| Endometrial hyperplasia without atypia | |||
| Medroxyprogesterone acetate | 10 mg per day for 14 days per month | Does not provide contraception | |
| Caution in patients with severe hepatic dysfunction | |||
| Megestrol (Megace) | 40 mg per day | Does not provide contraception | |
| Caution in patients with severe hepatic dysfunction | |||
| Levonorgestrel-releasing intrauterine system (Mirena) | Releases 20 mcg per 24 hours | 96 percent regression rate for hyperplasia without atypia | |
| Provides contraception for five years | |||
| May cause irregular bleeding or amenorrhea | |||
| Contraindications include breast cancer; uterine anomaly that distorts the cavity; acute pelvic or cervical infection; and severe cirrhosis or liver cancer | |||
| More expensive initially, but similar to other therapies when averaged over five years | |||
| Ovulatory bleeding or heavy or prolonged menstrual bleeding | |||
| Levonorgestrel-releasing intrauterine system | Releases 20 mcg per 24 hours | FDA-approved for menorrhagia in 2009; see additional comments above | |
| Medroxyprogesterone acetate | 10 mg per day for 21 days per month | Does not provide contraception | |
| Effective short-term therapy for decreasing heavy flow | |||
| Not tolerated as well long term as levonorgestrel-releasing intrauterine system | |||
| Caution in patients with severe hepatic dysfunction | |||
| NSAIDs | |||
| Ibuprofen | 600 to 1,200 mg per day, five days per month | Begin first day of menses and continue for five days or until menses ceases | |
| Treats dysmenorrhea | |||
| Caution in patients with gastrointestinal risks | |||
| Naproxen sodium (Anaprox) | 550 to 1,100 mg per day, five days per month | Begin first day of menses and continue for five days or until menses ceases | |
| Treats dysmenorrhea | |||
| Caution in patients with gastrointestinal risks | |||
| Mefenamic acid (Ponstel) | 1,500 mg per day, five days per month | Begin first day of menses and continue for five days or until menses ceases | |
| Treats dysmenorrhea | |||
| Caution in patients with gastrointestinal risks | |||
| Tranexamic acid (Lysteda) | 650 mg; two tablets three times per day, five days per month | FDA-approved for menorrhagia in 2009 | |
| Begin first day of menses and continue for five days | |||
| Caution in patients with history or risk of thromboembolic or renal disease | |||
| Contraindicated if patient has active intravascular clotting or subarachnoid hemorrhage | |||
| Considerably more expensive than other available therapies | |||
FDA = U.S. Food and Drug Administration; NA = not available; NSAIDs = nonsteroidal anti-inflammatory drugs.
[Source 22]Anovulatory uterine bleeding
There is little consensus on specific treatment regimens for anovulatory uterine bleeding 47. Pharmacologic treatment options are listed in Table 3. The American College of Obstetricians and Gynecologists recommends treatment with combination oral contraceptives or cyclic progestin 25. Progestin therapy and oral contraceptives induce routine withdrawal bleeding, decrease the risk of hyperplasia or cancer, and correct any related excessive menstrual bleeding 25. Oral contraceptives containing 35 mcg or less of ethinyl estradiol are preferred 25. Cyclic oral medroxyprogesterone acetate (Provera) at a dosage of 10 mg per day for 10 to 14 days per month also is effective 26.
Treatment options for women who have hyperplasia without atypia include cyclic medroxyprogesterone acetate at 10 mg per day for 14 days per month, continuous megestrol (Megace) at 40 mg per day 32 or the levonorgestrel-releasing intrauterine system (Mirena) 48. After the initiation of treatment, endometrial biopsy should be repeated in three to six months to assure resolution of the hyperplasia 49. Because of the high rate of progression to cancer, women found to have hyperplasia with atypia should be referred to a gynecologist to review treatment options 49. Hysterectomy is the recommended treatment, but women desiring continued fertility may be candidates for progestin therapy and close follow-up 49. Women found to have adenocarcinoma should be referred to a gynecologic oncologist for hysterectomy and staging 49.
Menorrhagia (heavy or prolonged menstrual bleeding)
The goals of treatment for menorrhagia are to reduce flow volume and to correct anemia. Hormonal and non-hormonal therapeutic options are available to patients (Table 3). Figure 6 is an algorithm for the evaluation and treatment of ovulatory abnormal uterine bleeding.
Hormonal Therapies
Progestins effectively decrease excessive menstrual bleeding. In contrast to the shorter course of oral progestin therapy used for anovulatory uterine bleeding, progestin therapy for menorrhagia needs to be given for 21 days per month to be effective 50. The continuous progesterone release provided by the levonorgestrel-releasing intrauterine system reduces menorrhagia more effectively than oral progestins 51. It is better tolerated than the 21-day oral regimen and has patient satisfaction scores similar to endometrial ablation and hysterectomy at a significantly lower cost 51. The levonorgestrel-releasing intrauterine system is the only contraceptive approved by the U.S. Food and Drug Administration (FDA) for the treatment of menorrhagia.
Oral contraceptives have been shown to reduce menstrual flow volume, especially when used continuously, but they have not been studied specifically in women with menorrhagia 52. Consequently, there are few data to support their effectiveness 53. Oral contraceptives are, however, the treatment of choice in women with known von Willebrand disease who also desire contraception 54.
Nonhormonal Therapies
At scheduled pharmacologic doses, nonsteroidal anti-inflammatory drugs (NSAIDs) decrease prostaglandin levels, reducing menstrual bleeding 55. In one small study, naproxen sodium (Anaprox) and mefenamic acid (Ponstel) decreased flow volume by 46 and 47 percent, respectively 56. There is no evidence that one NSAID is more effective than another, but cost varies considerably 55.
Tranexamic acid (Lysteda), an antifibrinolytic that prevents activation of plasminogen, is FDA-approved for the treatment of menorrhagia. Two 650-mg tablets taken three times per day for the first five days of the cycle decreased bleeding significantly more than NSAIDs did 57. Although increased rates of thrombosis were initially a concern, long-term studies have not demonstrated this 57. Cost remains a limiting factor of tranexamic acid. It is likely most appropriate in women with bleeding disorders who desire fertility or have contraindications to oral contraceptives.
Surgery
Uterine polyps and leiomyomas, specifically submucosal fibroids, may cause menorrhagia. Available evidence suggests that hysteroscopic polypectomy reduces 75 to 100 percent of abnormal uterine bleeding symptoms in women with endometrial polyps 58. For menorrhagia associated with submucosal fibroids, surgical resection may allow women to maintain child-bearing capacity.16 Resection may normalize menses, but the clear long-term impact on reproduction is unknown 38. Alternatively, fibroids may be treated with uterine artery embolization, the percutaneous embolization of perifibroid vessels causing infarction of the fibroid 59. The effect of uterine artery embolization on future pregnancies also needs further study 59. Whether abnormal uterine bleeding caused by fibroids is treated with surgical resection or uterine artery embolization, approximately 20 percent of women subsequently undergo a hysterectomy for recurrent abnormal uterine bleeding 38
If excessive uterine bleeding is unresponsive to medical intervention, endometrial ablation (the surgical destruction of the endometrium) may be considered 60. This intervention is considered permanent and not advised in women who desire continued fertility. By five years postablation, approximately one-third of women require a second operation 60.
Hysterectomy is the definitive treatment for excessive uterine bleeding in women who no longer wish to conceive. Disadvantages include increased number of adverse effects, longer recovery time, and higher initial health care costs compared with uterine-sparing procedures 59. Hysterectomy also may be associated with ovarian failure nearly four years earlier than expected 61.
- Sweet, M. G., Schmidt-Dalton, T. A., Weiss, P. M., & Madsen, K. P. (2012). Evaluation and management of abnormal uterine bleeding in premenopausal women. American Family Physician, 85, 35–43.[↩][↩][↩][↩][↩][↩]
- McDowell, M. A., Brody, D. J., & Hughes, J.P. (2007). Has age at menarche changed? Results from the National Health and Nutrition Examination Survey (NHANES) 1999-2004. Journal of Adolescent Health, 40, 227–231.[↩][↩]
- Dasharathy, S. S., Mumford, S. L., Pollack, A. Z., Perkins, N. J., Mattison, D. R., Wactawski-Wende, J., & Schisterman, E. F. (2012). Menstrual bleeding patterns among regularly menstruating women. American Journal of Epidemiology, 175, 536–545.[↩]
- Abnormal Uterine Bleeding. https://www.acog.org/Patients/FAQs/Abnormal-Uterine-Bleeding[↩]
- McDowell, M.A., Brody, D.J., Hughes, J.P. (2007). Has Age at Menarche Changed? Results from the National Health and Nutrition Examination Survey (NHANES) 1999–2004 (link is external). Journal of Adolescent Health; 40(3): 227–231.[↩]
- American College of Obstetricians and Gynecologists. (2016). Barrier Methods of Birth Control: Spermicide, Condom, Sponge, Diaphragm, and Cervical Cap.[↩]
- Matsuda, Y., Kato, H., Ono, E., Kikuchi, K., Muraoka, M., Takagi, K. (2008). Diagnosis of toxic shock syndrome by two different systems; clinical criteria and monitoring of TSST-1-reactive T cells. Microbiol Immunol; 52(11):513-21.[↩]
- Chiazze, L., Brayer, F.T., Macisco, J.J., Parker, M.P., Duffy, B.J. (1968). The Length and Variability of the Human Menstrual Cycle (link is external). JAMA; 203(6): 377–380.[↩]
- Fraser, I.S., Critchley, H., Broder, M., Munro, M.G. (2011). The FIGO Recommendations on Terminologies and Definitions for Normal and Abnormal Uterine Bleeding. (link is external)The Seminars in Reproductive Medicine; 29(5): 383-390.[↩]
- American College of Obstetricians and Gynecologists. (2015). Menstruation in Girls and Adolescents: Using the Menstrual Cycle as a Vital Sign.[↩]
- Shifren, J.L., Gass, M.L.S., for the NAMS Recommendations for Clinical Care of Midlife Women Working Group. (2014). The North American Menopause Society Recommendations for Clinical Care of Midlife Women (link is external). Menopause; 21(10): 1038–1062.[↩]
- Wilcox, A. J., Dunson, D., Baird, D. D. (2000). The timing of the “fertile window” in the menstrual cycle: day specific estimates from a prospective study. British Medical Journal, 321(7271):1259-1262.[↩]
- Reed, B.G., Carr, B.R. (2015). The Normal Menstrual Cycle and the Control of Ovulation. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.[↩]
- Krohn, P. L. (1949). Intermenstrual pain (the “Mittelschmerz”) and the time of ovulation. British Medical Journal, 1(4609), 803–805. Retrieved September 27, 2016[↩]
- American College of Obstetricians and Gynecologists (ACOG). (2017). FAQ: Abnormal uterine bleeding. https://www.acog.org/Patients/FAQs/Abnormal-Uterine-Bleeding[↩][↩]
- Whitaker, L., & Critchley, H. O. D. (2016). Abnormal uterine bleeding. Best Practice & Research Clinical Obstetrics & Gynaecology, 34, 54–65. https://doi.org/10.1016/j.bpobgyn.2015.11.012[↩]
- Munro, M. G., Critchley, H. O., & Fraser, I. S. (2012). The FIGO systems for nomenclature and classification of causes of abnormal uterine bleeding in the reproductive years: Who needs them? American Journal of Obstetrics and Gynecology, 207(4), 259–265.[↩][↩][↩][↩][↩][↩]
- Apgar, B. S., Kaufman, A. H., George-Nwogu, U., & Kittendorf, A. (2007). Treatment of menorrhagia. American Family Physician, 75, 1813–1819.[↩][↩]
- French, L. (2005). Dysmenorrhea. American Family Physician, 71, 285–291.[↩][↩]
- Godfrey, E. M., Folger, S. G., Jeng, G., Jamieson, D. J., & Curtis, K. M. (2013). Treatment of bleeding irregularities in women with copper-containing IUDs: A systematic review. Contraception, 87(5), 549–566. https://doi.org/10.1016/j.contraception.2012.09.006[↩][↩]
- American College of Obstetricians and Gynecologists. (2016). FAQ: Gonorrhea, chlamydia, and syphilis. https://www.acog.org/Patients/FAQs/Chlamydia-Gonorrhea-and-Syphilis[↩]
- Evaluation and Management of Abnormal Uterine Bleeding in Premenopausal Women. Am Fam Physician. 2012 Jan 1;85(1):35-43.[↩][↩][↩][↩][↩]
- Diaz A, Laufer MR, Breech LL; American Academy of Pediatrics Committee on Adolescence, American College of Obstetricians and Gynecologists Committee on Adolescent Health Care. Menstruation in girls and adolescents: using the menstrual cycle as a vital sign. Pediatrics. 2006;118(5):2245–2250.[↩][↩][↩][↩][↩][↩][↩]
- Speroff L, Fritz MA. Clinical Gynecologic Endocrinology and Infertility. 7th ed. Philadelphia, Pa.: Lippincott Williams & Wilkins; 2005:402, 547, 549, 553–556, 560–561, 566, 569, 628–629, 808, 811.[↩][↩]
- ACOG Committee on Practice Bulletins—Gynecology. American College of Obstetricians and Gynecologists. ACOG practice bulletin: management of anovulatory bleeding. Int J Gynaecol Obstet. 2001;72(3):263–271.[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Ely JW, Kennedy CM, Clark EC, Bowdler NC. Abnormal uterine bleeding: a management algorithm. J Am Board Fam Med. 2006;19(6):590–602.[↩][↩][↩]
- Morrell MJ, Hayes FJ, Sluss PM, et al. Hyperandrogenism, ovulatory dysfunction, and polycystic ovary syndrome with valproate versus lamotrigine. Ann Neurol. 2008;64(2):200–211.[↩]
- Madhusoodanan S, Parida S, Jimenez C. Hyperprolactinemia associated with psychotropics—a review. Hum Psychopharmacol. 2010;25(4):281–297.[↩]
- Stovall DW, Anderson RJ, DeLeon FD. Endometrial adenocarcinoma in teenagers. Adolesc Pediatr Gynecol. 1989;2:157–159.[↩]
- Ash SJ, Farrell SA, Flowerdew G. Endometrial biopsy in DUB. J Reprod Med. 1996;41(12):892–896.[↩][↩]
- Farquhar CM, Lethaby A, Sowter M, Verry J, Baranyai J. An evaluation of risk factors for endometrial hyperplasia in premenopausal women with abnormal menstrual bleeding. Am J Obstet Gynecol. 1999; 181(3):525–529.[↩][↩]
- Sorosky JI. Endometrial cancer. Obstet Gynecol. 2008;111(2 pt 1):436–447.[↩][↩][↩]
- Lacey JV Jr, Chia VM. Endometrial hyperplasia and the risk of progression to carcinoma. Maturitas. 2009;63(1):39–44.[↩][↩]
- Trimble CL, Kauderer J, Zaino R, et al. Concurrent endometrial carcinoma in women with a biopsy diagnosis of atypical endometrial hyperplasia: a Gynecologic Oncology Group study. Cancer. 2006;106(4):812–819.[↩]
- Clinical challenges of perimenopause: consensus opinion of The North American Menopause Society. Menopause. 2000;7(1):5–13.[↩]
- Gordon P. Videos in clinical medicine. Endometrial biopsy. N Engl J Med. 2009;361(26):e61.[↩]
- Dijkhuizen FP, Mol BW, Brölmann HA, Heintz AP. The accuracy of endometrial sampling in the diagnosis of patients with endometrial carcinoma and hyperplasia: a meta-analysis. Cancer. 2000;89(8):1765–1772.[↩]
- American College of Obstetricians and Gynecologists. ACOG practice bulletin. Alternatives to hysterectomy in the management of leiomyomas. Obstet Gynecol. 2008;112(2 pt 1):387–400.[↩][↩][↩][↩]
- Shankar M, Lee CA, Sabin CA, Economides DL, Kadir RA. von Willebrand disease in women with menorrhagia: a systematic review. BJOG. 2004;111(7):734–740.[↩]
- Rees M. Menorrhagia. Br Med J (Clin Res Ed). 1987;294(6574):759–762.[↩]
- Philipp CS, Faiz A, Dowling NF, et al. Development of a screening tool for identifying women with menorrhagia for hemostatic evaluation. Am J Obstet Gynecol. 2008;198(2):163.e1–e8.[↩]
- Dueholm M, Forman A, Jensen ML, Laursen H, Kracht P. Transvaginal sonography combined with saline contrast sonohysterography in evaluating the uterine cavity in premenopausal patients with abnormal uterine bleeding. Ultrasound Obstet Gynecol. 2001;18(1):54–61.[↩]
- de Vries LD, Dijkhuizen FP, Mol BW, Brölmann HA, Moret E, Heintz AP. Comparison of transvaginal sonography, saline infusion sonography, and hysteroscopy in premenopausal women with abnormal uterine bleeding. J Clin Ultrasound. 2000;28(5):217–223.[↩][↩]
- van Dongen H, de Kroon CD, Jacobi CE, Trimbos JB, Jansen FW. Diagnostic hysteroscopy in abnormal uterine bleeding: a systematic review and meta-analysis. BJOG. 2007;114(6):664–675.[↩][↩]
- ACOG Committee on Practice Bulletins—Gynecology, American College of Obstetricians and Gynecologists. (2013). Practice bulletin no. 136: Management of abnormal uterine bleeding associated with ovulatory dysfunction. Obstetrics and Gynecology, 122(1), 176–185. https://journals.lww.com/greenjournal/Citation/2013/07000/Practice_Bulletin_No__136___Management_of_Abnormal.38.aspx[↩]
- Proctor, M. L., & Farquhar, C. M. (2007). Dysmenorrhoea. Clinical Evidence, pii, 0813.[↩]
- Hickey M, Higham J, Fraser IS. Progestogens versus oestrogens and progestogens for irregular uterine bleeding associated with anovulation. Cochrane Database Syst Rev. 2007;(4):CD001895.[↩]
- Buttini MJ, Jordan SJ, Webb PM. The effect of the levonorgestrel releasing intrauterine system on endometrial hyperplasia: an Australian study and systematic review. Aust N Z J Obstet Gynaecol. 2009;49(3):316–322.[↩]
- Sorosky JI. Endometrial cancer. Obstet Gynecol. 2008;111(2 pt 1):436–447[↩][↩][↩][↩]
- Lethaby A, Irvine GA, Cameron I. Cyclical progestogens for heavy menstrual bleeding. Cochrane Database Syst Rev. 2008;(1):CD001016.[↩]
- Lethaby AE, Cooke I, Rees M. Progesterone or progestogen-releasing intrauterine systems for heavy menstrual bleeding. Cochrane Database Syst Rev. 2005;(4):CD002126.[↩][↩]
- Larsson G, Milsom I, Lindstedt G, Rybo G. The influence of a low-dose combined oral contraceptive on menstrual blood loss and iron status. Contraception. 1992;46(4):327–334.[↩]
- Farquhar C, Brown J. Oral contraceptive pill for heavy menstrual bleeding. Cochrane Database Syst Rev. 2009;(4):CD000154.[↩]
- James AH, Manco-Johnson MJ, Yawn BP, Dietrich JE, Nichols WL. von Willebrand disease: key points from the 2008 National Heart, Lung, and Blood Institute guidelines. Obstet Gynecol. 2009;114(3):674–678.[↩]
- Lethaby A, Augood C, Duckitt K, Farquhar C. Nonsteroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database Syst Rev. 2007;(4):CD000400.[↩][↩]
- Hall P, Maclachlan N, Thorn N, Nudd MW, Taylor CG, Garrioch DB. Control of menorrhagia by the cyclooxygenase inhibitors naproxen sodium and mefenamic acid. Br J Obstet Gynaecol. 1987;94(6):554–558.[↩]
- Lethaby A, Farquhar C, Cooke I. Antifibrinolytics for heavy menstrual bleeding. Cochrane Database Syst Rev. 2000;(4):CD000249.[↩][↩]
- Nathani F, Clark TJ. Uterine polypectomy in the management of abnormal uterine bleeding: a systematic review. J Minim Invasive Gynecol. 2006;13(4):260–268.[↩]
- Edwards RD, Moss JG, Lumsden MA, et al.; Committee of the Randomized Trial of Embolization versus Surgical Treatment for Fibroids. Uterine-artery embolization versus surgery for symptomatic uterine fibroids. N Engl J Med. 2007;356(4):360–370.[↩][↩][↩]
- Dickersin K, Munro MG, Clark M, et al.; Surgical Treatments Outcomes Project for Dysfunctional Uterine Bleeding (STOP-DUB) Research Group. Hysterectomy compared with endometrial ablation for dysfunctional uterine bleeding: a randomized controlled trial. Obstet Gynecol. 2007;110(6):1279–1289.[↩][↩]
- Farquhar CM, Sadler L, Harvey SA, Stewart AW. The association of hysterectomy and menopause: a prospective cohort study. BJOG. 2005;112(7):956–962.[↩]