Contents
What is labyrinthitis
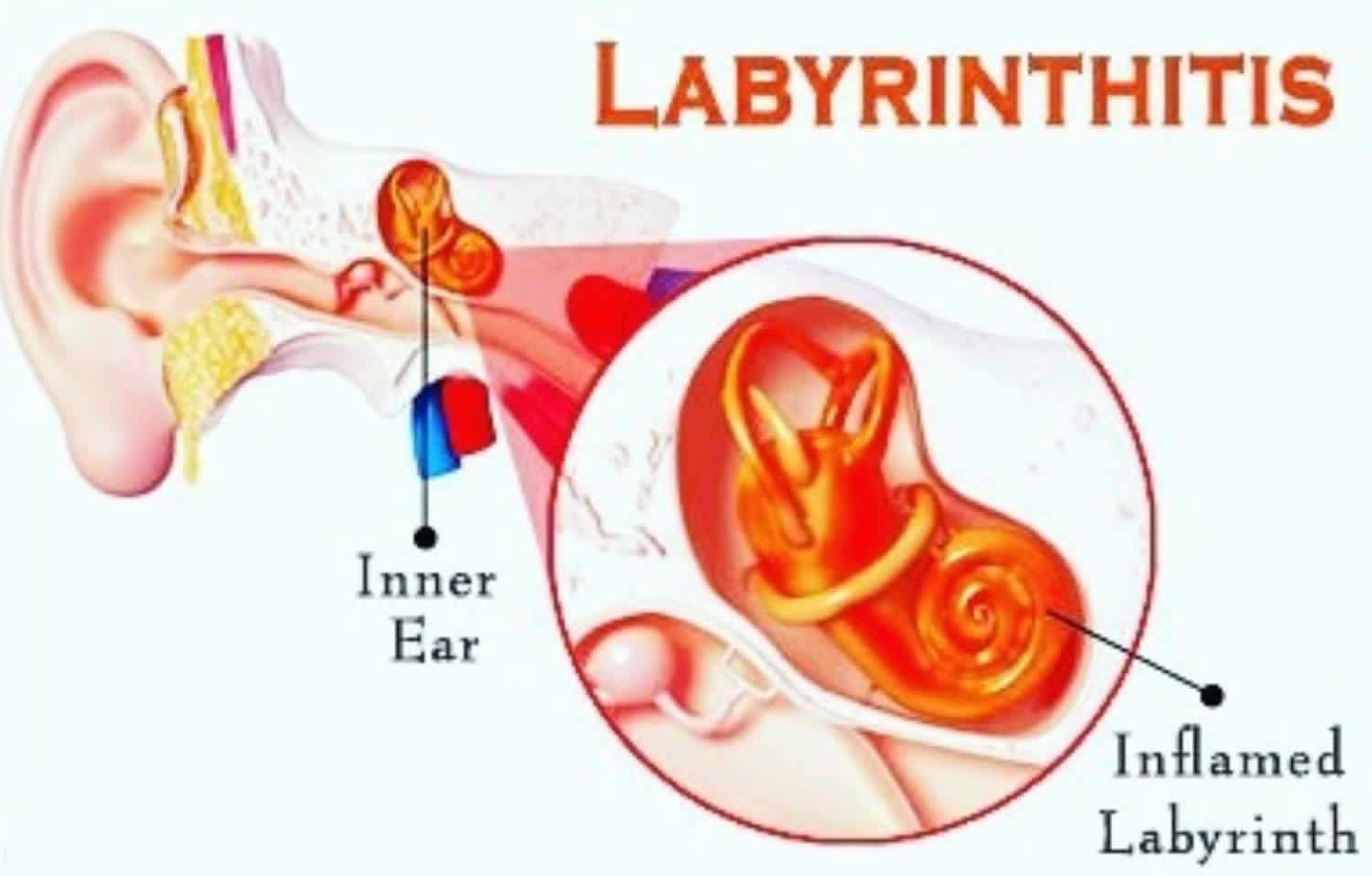
Labyrinthitis is an inflammation of the balancing center in your inner ear (or labyrinth). Labyrinthitis is usually caused by an infection that affects both branches of the vestibulo-cochlear nerve, resulting in hearing changes as well as dizziness or vertigo (see Figures 1 to 4). Symptoms include hearing loss, a spinning sensation (vertigo), and dizziness. People with severe vertigo may get dehydrated due to frequent vomiting. Most people feel better within a few weeks.
The most common cause of labyrinthitis is a viral infection, such as from a cold or the flu, or infection with a virus from the herpes group of viruses, which causes chickenpox, shingles or cold sores. Sometimes an ear infection can lead to labyrinthitis.
Less commonly, a bacterial infection, such as meningitis or a middle ear infection, can cause labyrinthitis. Some autoimmune conditions, allergies and medications can lead to labyrinthitis.
With labyrinthitis you will feel that you or your surroundings are moving or spinning, even when you are still. This dizziness is also known as vertigo. It can be mild, or it can be so bad it is hard to get out of bed.
Other symptoms of labyrinthitis may include:
- nausea, almost like sea-sickness
- a false sense of movement
- your eyes moving on their own, making it hard to focus them
- loss of balance — you may fall toward one side
- fever
- ear pain
- vomiting
- hearing loss or ringing in the ears (tinnitus)
- fluid or pus seeping out of the ear
- changes in vision, such as blurred vision or double vision.
If you have been diagnosed with labyrinthitis, you may not need any treatment.
In some cases, your doctor may prescribe medications such as:
- corticosteroids to reduce inflammation in your inner ear
- vestibular suppressants for severe vertigo
- anti-nausea medications for nausea or vomiting.
If your symptoms don’t go away, you may benefit from specialized rehabilitation and physiotherapy, which can help retrain the brain to interpret balance messages from the inner ear.
You can also help ease symptoms by:
- resting on your side during dizzy episodes
- avoiding alcohol
- drinking plenty of water
- creating a low-noise, low-stress environment
- avoiding bright lights.
To minimize any remaining feelings of dizziness and vertigo:
- lie still in a comfortable position during an attack – on your side is often best
- try to cut out noise and anything that causes stress from your surroundings
You should also avoid driving, using tools and machinery, or working at heights if you’re feeling dizzy and unbalanced.
See your doctor immediately if you have sudden hearing loss in one ear, with or without vertigo. It’s important the cause is investigated.
Call your local emergency services number if you have any of the following severe symptoms:
- Convulsions
- Double vision
- Fainting
- Vomiting a lot
- Slurred speech
- Vertigo that occurs with a fever of more than 101°F (38.3°C)
- Weakness or paralysis
If you have dizziness, vertigo, some hearing loss or any of the above symptoms and they don’t get better after a few days, or your symptoms are getting worse, see your doctor.
Symptoms of vertigo, nausea and sickness often improve gradually over a few days, although they can sometimes last for several weeks.
You may feel unsteady for a number of weeks or months. This usually improves over time and with treatment. Your hearing should return, although this may depend on the type of infection that caused the problem.
How long does labyrinthitis last?
Symptoms of vertigo, nausea and sickness often improve gradually over a few days, although they can sometimes last for several weeks.
You may feel unsteady for a number of weeks or months. This usually improves over time and with treatment. Your hearing should return, although this may depend on the type of infection that caused the problem.
- Severe symptoms usually go away within a week.
- Most people are completely better within 2 to 3 months.
- Older adults are more likely to have dizziness that lasts longer.
In very rare cases, permanent damage to the vestibular system can also occur, causing permanent hearing loss. Positional dizziness or BPPV (Benign Paroxysmal Positional Vertigo) can also be a secondary type of dizziness that develops from neuritis or labyrinthitis and may recur on its own chronically. Labyrinthitis may also cause endolymphatic hydrops (abnormal fluctuations in the inner ear fluid called endolymph) to develop several years later.
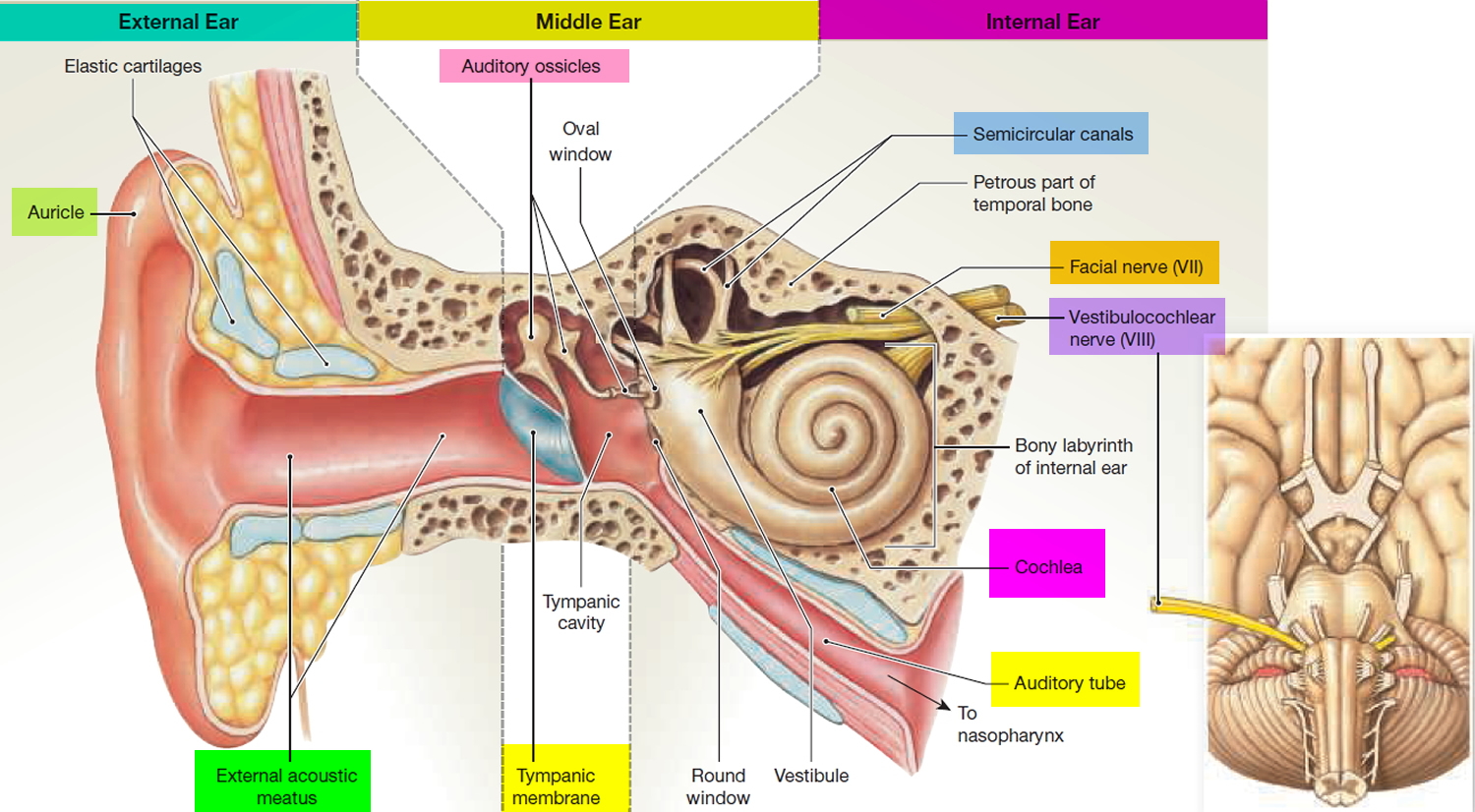
Inner ear anatomy
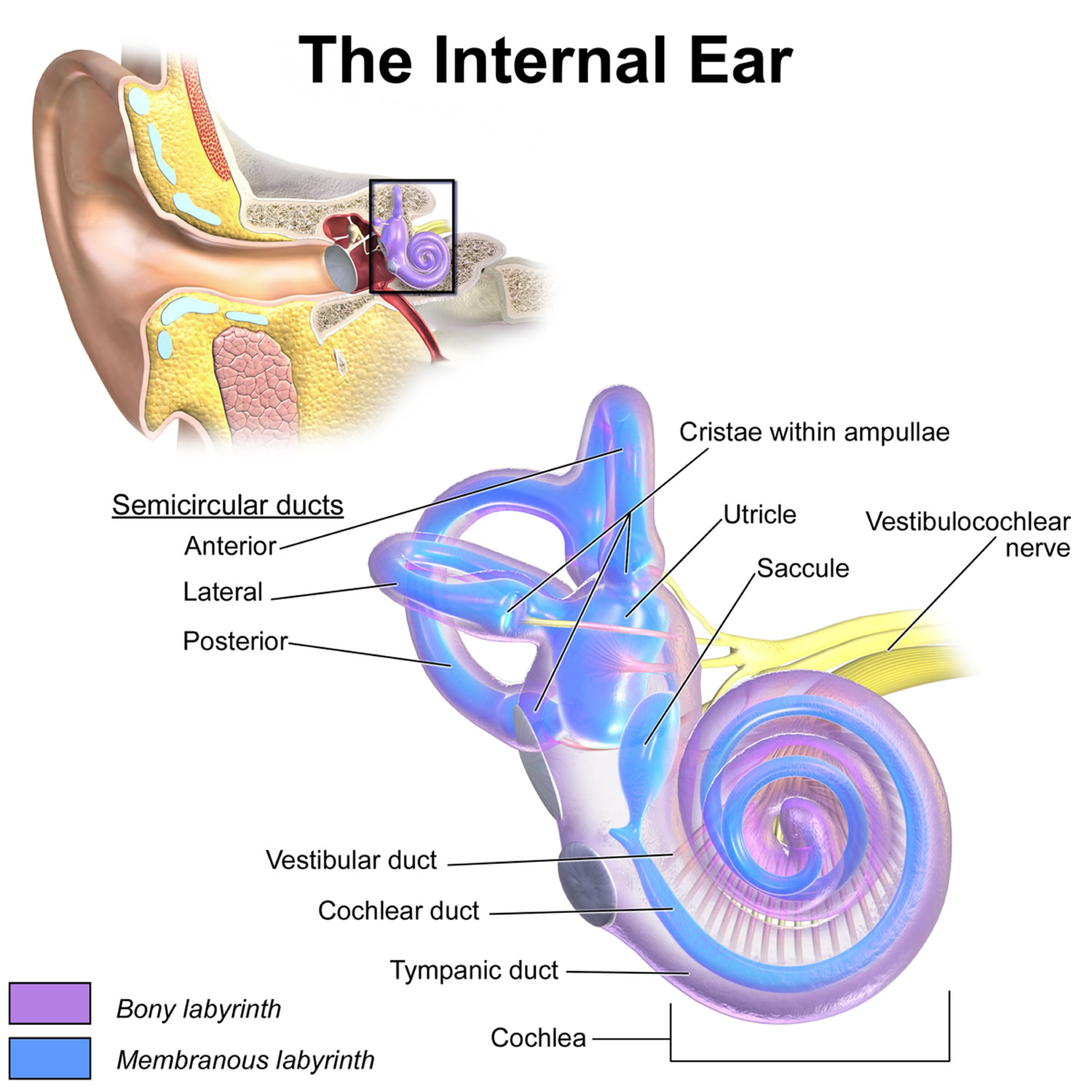
You rely on the inner ear, an intricate sensory organ, to hear and to maintain balance. The inner ear is a complex system of communicating chambers and tubes called a labyrinth. Each ear has two parts to the labyrinth—the bony (osseus) labyrinth and the membranous labyrinth (Figure 1). The bony labyrinth is a cavity within the temporal bone. The membranous labyrinth is a tube of similar shape that lies within the bony labyrinth. Between the bony and membranous labyrinths is a fluid called perilymph, which is secreted by cells in the wall of the bony labyrinth. The membranous labyrinth contains another fluid, called endolymph.
The parts of the labyrinths include three membranous semicircular ducts within three bony semicircular canals, and a cochlea. The semicircular canals and associated structures provide a sense of equilibrium (balance). The cochlea functions in hearing.
The cochlea has a bony core and a thin, bony shelf that extends out from the core and coils around it. The shelf divides the bony labyrinth of the cochlea into upper and lower compartments. The upper compartment, called the scala vestibuli, leads from the oval window to the tip of the cochlea. The lower compartment, the scala tympani, extends from the tip of the cochlea to a membrane-covered opening in the wall of the middle ear called the round window.
The part of the membranous labyrinth within the cochlea is called the cochlear duct. It lies between the two bony compartments and ends as a closed sac near the tip of the cochlea. The cochlear duct is separated from the scala vestibuli by a vestibular membrane (Reissner’s membrane) and from the scala tympani by a basilar membrane. The basilar membrane has many thousands of elastic fibers, allowing it to move in response to sound vibrations. Sound vibrations entering the perilymph at the oval window travel along the scala vestibuli and pass through the vestibular membrane and into the endolymph of the cochlear duct, where they move the basilar membrane.
After passing through the basilar membrane, the vibrations enter the perilymph of the scala tympani. Their forces are dissipated into the air in the tympanic cavity by movement of the membrane covering the round window.
The spiral organ (organ of Corti) contains the hearing receptors. It is located on the upper surface of the basilar membrane and stretches from the apex to the base of the cochlea. The receptor cells, called hair cells, are organized in rows and have many hairlike processes that project into the endolymph of the cochlear duct. Above these hair cells is a tectorial membrane attached to the bony shelf of the cochlea, passing over the receptor cells and contacting the tips of their hairs.
As sound vibrations move the basilar membrane, the hairs move back and forth against the tectorial membrane and the resulting mechanical deformation of the hairs stimulates the hair cells (Figure 4. The Cochlea). Hair cells at different locations along the length of the cochlear duct respond to different frequencies (pitch) of sound vibrations. This enables us to hear sounds of different pitch simultaneously.
Hair cells are epithelial but function somewhat like neurons. For example, when a hair cell is at rest, its membrane is polarized. When it is stimulated, selective ion channels open, depolarizing the membrane and making it more permeable to calcium ions. The hair cell has no axon or dendrites, but it has neurotransmitter-containing vesicles near its base. As calcium ions diffuse into the cell, some of these vesicles fuse with the cell membrane and release a neurotransmitter by exocytosis. The neurotransmitter stimulates the dendrites of nearby sensory neurons. In response these neurons send action potentials along the cochlear branch of the vestibulocochlear nerve to the auditory cortex of the temporal lobe of the brain.
The ear of a young person with normal hearing can detect sound waves with frequencies ranging from 20 to more than 20,000 vibrations per second. The range of greatest sensitivity is 2,000 to 3,000 vibrations per second. More-intense stimulation of the hair cells causes more action potentials per second to reach the auditory cortex, and we sense a louder sound.
Figure 1. Inner ear anatomy
Figure 2. Parts of the inner ear
Sense of Equilibrium
The sense of equilibrium (balance) is really two senses:
- Static equilibrium and
- Dynamic equilibrium—that come from different sensory organs.
The organs of static equilibrium sense the position of the head, maintaining balance, stability and posture when the head and body are still. When the head and body suddenly move or rotate, the organs of dynamic equilibrium detect such motion and aid in maintaining balance.
Static Equilibrium
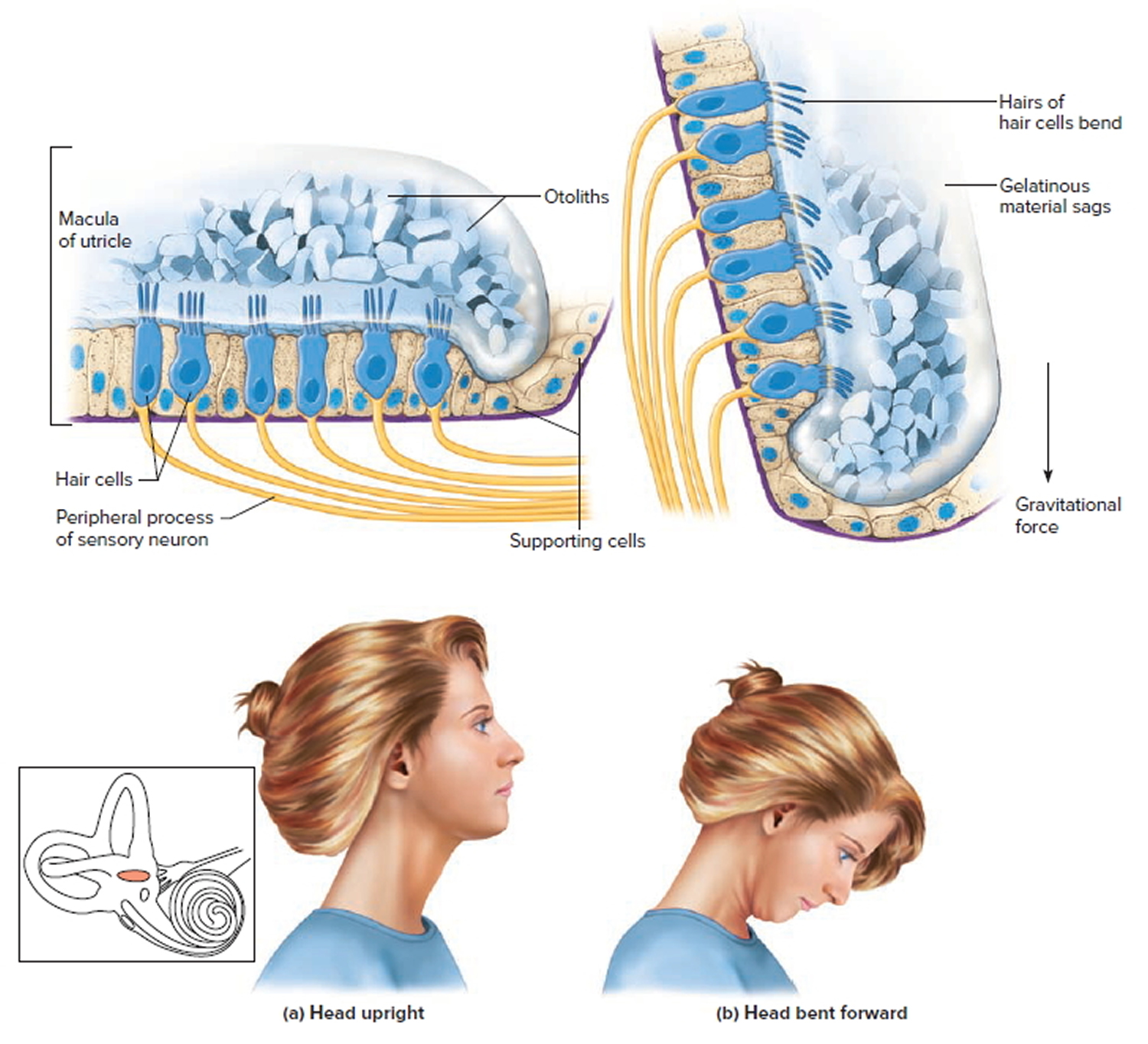
The organs of static equilibrium are in the vestibule, a bony chamber between the semicircular canals and the cochlea. The membranous labyrinth inside the vestibule consists of two expanded chambers—a utricle and a saccule (see Figure 2).
The saccule and utricle each have a tiny structure called a macula. Maculae have many hair cells, which serve as sensory receptors. The hairs of the hair cells project into a mass of gelatinous material, which has grains of calcium carbonate (otoliths) embedded in it. These particles add weight to the gelatinous structure.
Bending the head forward, backward, or to either side tilts the gelatinous masses of the maculae, and as they sag in response to gravity, the hairs projecting into them bend. This action causes the hair cells to signal the sensory neurons associated with them in a manner similar to that of hair cells associated with hearing. The resulting action potentials are conducted into the central nervous system on the vestibular branch of the vestibulocochlear nerve, informing the brain of the head’s new position. The brain responds by adjusting the pattern of motor impulses to skeletal muscles, which contract or relax to maintain balance (Figure 5).
Figure 3. Inner ear maculae respond to changes in head position
Note: (a) Macula of the utricle with the head in an upright position. (b) Macula of the utricle with the head bent forward.
Dynamic Equilibrium
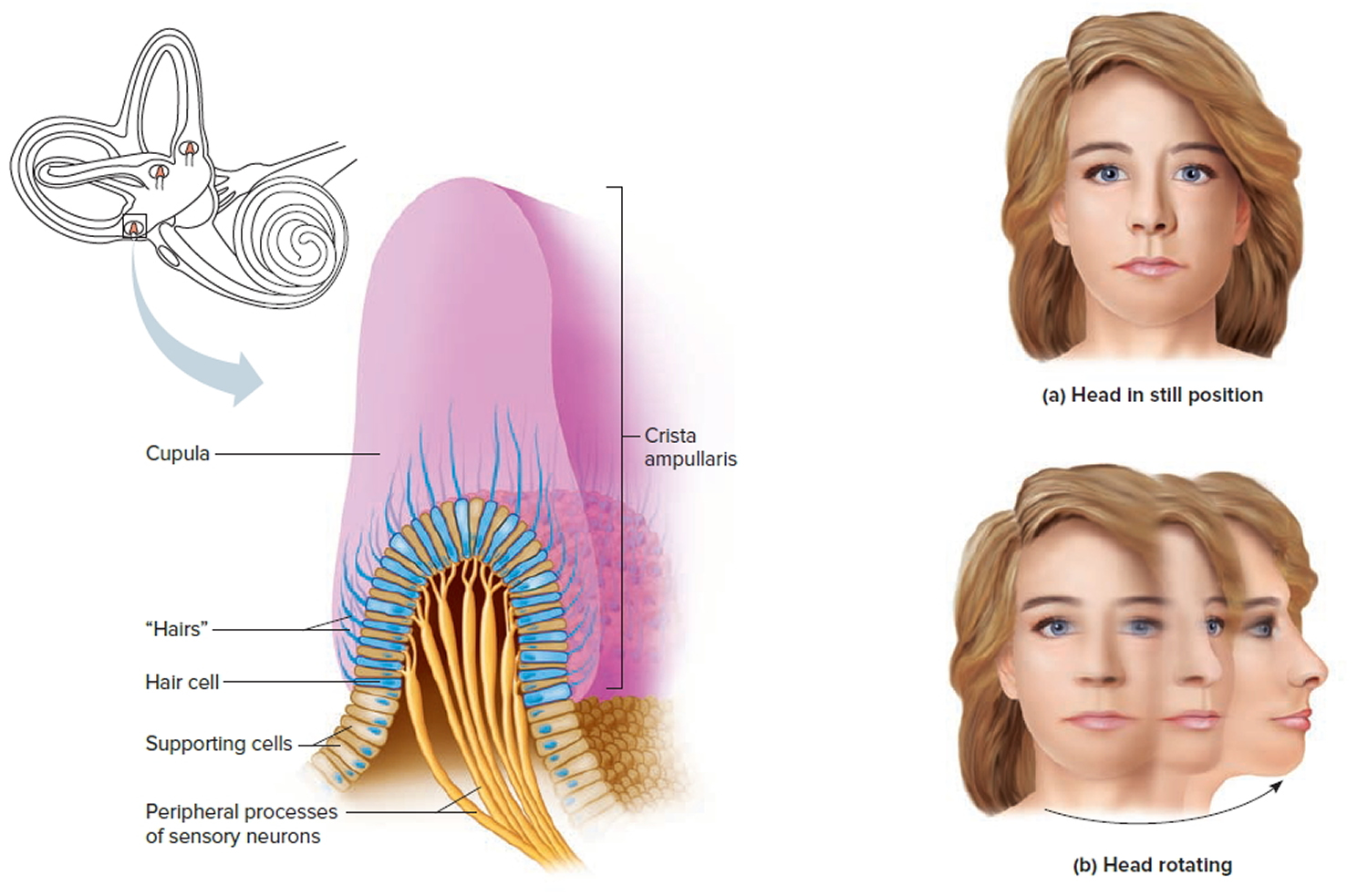
The organs of dynamic equilibrium are the three semicircular canals in the labyrinth. They detect motion of the head and aid in balancing the head and body during sudden movement. These canals lie at right angles to each other (see Figure 2).
Suspended in the perilymph of the bony portion of each semicircular canal is a membranous semicircular duct that ends in a swelling called an ampulla, which
houses the sensory organs of the semicircular canals. Each of these sensory organs, called a crista ampullaris, contains a number of sensory hair cells and supporting cells. Like the hairs of the maculae, the hair cells of the crista ampullaris extend upward into a dome-shaped, gelatinous mass called the cupula (Figure 6). When the head is stationary, the cupula of the crista ampullaris remains upright. When the head is moving rapidly, the cupula bends opposite the motion of the head, stimulating sensory receptors.
Rapid movement of the head or body stimulates the hair cells of the crista ampullaris (Figure 4). At such times, the semicircular canals move with the head or body, but the fluid inside the membranous ducts remains stationary. Imagine turning rapidly while holding a full glass of water. This action bends the cupula in one or more of the canals in a direction opposite that of the head or body movement, and the hairs embedded in it also bend. The stimulated hair cells signal their associated neurons, which conduct impulses to the brain. The brain interprets these impulses as a movement in a particular direction.
Parts of the cerebellum are particularly important in interpreting impulses from the semicircular canals. Analysis of such information allows the brain to predict the consequences of rapid body movements. By modifying signals to appropriate skeletal muscles, the cerebellum can maintain balance.
Other sensory structures aid in maintaining equilibrium. For example, certain mechanoreceptors (proprioceptors), particularly those associated with the joints of the neck, inform the brain about the position of body parts. In addition, the eyes detect changes in position that result from body movements. Such visual information is so important that even if the organs of equilibrium are damaged, a person may be able to maintain normal balance by keeping the eyes open and moving slowly.
The nausea, vomiting, dizziness, and headache of motion sickness arise from sensations that don’t make sense. The eyes of a person reading in a moving car, for example, signal the brain that the person is stationary, because the print doesn’t move. However, receptors in the skin detect bouncing, swaying, starting, and stopping as the inner ear detects movement. The contradiction triggers the symptoms. Similarly, in a passenger of an airplane flying through heavy turbulence, receptors in the skin and inner ear register the chaos outside, but the eyes focus on the immobile seats and surroundings.
To prevent or lessen the misery of motion sickness, focus on the horizon or an object in the distance ahead. Medications are available by pill (diphenhydramine and dimenhydrinate) and, for longer excursions, in a skin patch (scopolamine).
Figure 4. Dynamic inner ear balance organs (crista ampullaris) within the Semicricular ducts
Labyrinthitis symptoms
The most common symptoms of labyrinthitis are:
- feeling that you or your surroundings are moving or spinning, even when you are still (vertigo).
- feeling or being sick
- some hearing loss
These symptoms can vary in severity, it can be mild, or it can be so bad it is hard to get out of bed, with some people feeling that they can’t stand upright.
Other symptoms of labyrinthitis may include:
- nausea, almost like sea-sickness
- a false sense of movement
- your eyes moving on their own, making it hard to focus them
- loss of balance — you may fall toward one side
- fever
- ear pain
- vomiting
- hearing loss or ringing in the ears (tinnitus)
- fluid or pus seeping out of the ear
- changes in vision, such as blurred vision or double vision.
The symptoms of labyrinthitis can be quite severe during the first week, but usually get better after a few weeks.
In some cases the symptoms can last longer and have a significant impact on your quality of life and ability to carry out everyday tasks.
Acute phase
Onset of symptoms is usually very sudden, with severe dizziness developing abruptly during routine daily activities. In other cases, the symptoms are present upon awakening in the morning. The sudden onset of such symptoms can be very frightening; many people go to the emergency room or visit their physician on the same day.
Chronic phase
After a period of gradual recovery that may last several weeks, some people are completely free of symptoms. Others have chronic dizziness if the virus has damaged the vestibular nerve.
Many people with chronic neuritis or labyrinthitis have difficulty describing their symptoms, and often become frustrated because although they may look healthy, they don’t feel well. Without necessarily understanding the reason, they may observe that everyday activities are fatiguing or uncomfortable, such as walking around in a store, using a computer, being in a crowd, standing in the shower with their eyes closed, or turning their head to converse with another person at the dinner table.
Some people find it difficult to work because of a persistent feeling of disorientation or “haziness,” as well as difficulty with concentration and thinking.
Labyrinthitis causes
Labyrinthitis is usually caused by a virus and sometimes by bacteria. Having a cold or flu can trigger the condition. Less often, an ear infection may lead to labyrinthitis. Other causes include allergies or certain drugs that are bad for the inner ear.
The labyrinth is the innermost part of the ear. The labyrinth contains the:
- cochlea – a small spiral-shaped cavity that relays sounds to the brain and is responsible for hearing
- vestibular system – a set of fluid-filled channels that contributes to your sense of balance
Your inner ear is important for both hearing and balance. When you have labyrinthitis, the parts of your inner ear become irritated and swollen. This can make you lose your balance and cause hearing loss.
Labyrinthitis usually follows a viral infection, such as a cold or the flu. The infection can spread from the chest, nose, mouth and airways to the inner ear.
Infections that affect the rest of the body, such as measles, mumps or glandular fever, are a less common cause of viral labyrinthitis.
In rare cases, labyrinthitis can be caused by a bacterial infection. Bacterial labyrinthitis is more likely to affect young children and can be serious.
Bacteria can enter the labyrinth if the thin membranes separating your middle ear from your inner ear are broken. This can happen if you have a middle ear infection or an infection of the brain lining (meningitis).
Labyrinthitis can also develop in people who have an underlying autoimmune condition, where the immune system mistakenly attacks healthy tissue rather than fighting off infections.
These factors raise your risk for labyrinthitis:
- Drinking large amounts of alcohol
- Fatigue
- History of allergies
- Recent viral illness, respiratory infection, or ear infection
- Smoking
- Stress
- Using certain prescription or nonprescription drugs (such as aspirin)
Complications of labyrinthitis
Bacterial labyrinthitis carries a higher risk of causing permanent hearing loss, particularly in children who’ve developed it as a complication of meningitis.
As a result of this increased risk, a hearing test is recommended after having bacterial labyrinthitis.
Severe hearing loss after bacterial labyrinthitis can sometimes be treated with a cochlear implant. This is a small hearing device fitted under the skin behind your ear during surgery.
Vestibular neuronitis
Neuritis (inflammation of the nerve) affects the branch associated with balance, resulting in dizziness or vertigo but no change in hearing. The term neuronitis (damage to the sensory neurons of the vestibular ganglion) is also used.
Many people diagnosed with labyrinthitis only experience the balance symptoms without hearing loss.
This is known as vestibular neuronitis rather than labyrinthitis. However, both terms are often used to describe the same diagnosis.
Symptoms of viral neuritis can be mild or severe, ranging from subtle dizziness to a violent spinning sensation (vertigo). They can also include nausea, vomiting, unsteadiness and imbalance, difficulty with vision, and impaired concentration.
Sometimes the symptoms can be so severe that they affect the ability to stand up or walk.
Viral labyrinthitis may produce the same symptoms, along with tinnitus (ringing or noises in the ear) and/or hearing loss.
Viral labyrinthitis
Viral infections of the inner ear are more common than bacterial infections, but less is known about them. An inner ear viral infection may be the result of a systemic viral illness (one affecting the rest of the body, such as infectious mononucleosis or measles); or, the infection may be confined to the labyrinth or the vestibulo-cochlear nerve. Usually, only one ear is affected.
Some of the viruses that have been associated with vestibular neuritis or labyrinthitis include herpes viruses (such as the ones that cause cold sores or chicken pox and shingles), influenza, measles, rubella, mumps, polio, hepatitis, and Epstein-Barr. Other viruses may be involved that are as yet unidentified because of difficulties in sampling the labyrinth without destroying it. Because the inner ear infection is usually caused by a virus, it can run its course and then go dormant in the nerve only to flare up again at any time. There is currently no way to predict whether or not it will come back.
Bacterial labyrinthitis
In serous labyrinthitis, bacteria that have infected the middle ear or the bone surrounding the inner ear produce toxins that invade the inner ear via the oval or round windows and inflame the cochlea, the vestibular system, or both. Serous labyrinthitis is most frequently a result of chronic, untreated middle ear infections (chronic otitis media) and is characterized by subtle or mild symptoms.
Less common is suppurative labyrinthitis, in which bacterial organisms themselves invade the labyrinth. The infection originates either in the middle ear or in the cerebrospinal fluid, as a result of bacterial meningitis. Bacteria can enter the inner ear through the cochlear aqueduct or internal auditory canal, or through a fistula (abnormal opening) in the horizontal semicircular canal.
Labyrinthitis diagnosis
If you have symptoms indicative of labyrinthitis, you may need to visit your doctor for diagnosis and treatment.
Labyrinthitis is diagnosed based on your symptoms, medical history and a physical examination.
Your doctor will talk to you and examine you. The examination may include:
- Asking you to move your head rapidly
- Your ears will be checked for signs of inflammation and infection
- Eye tests. If they’re flickering uncontrollably, it’s usually a sign that your vestibular system, the body’s balancing system, isn’t working properly.
- Checking your blood pressure
- Checking your balance.
Your doctor may also organize tests such as:
- Hearing tests, as labyrinthitis is more likely if you have hearing loss
- Electroencephalogram (EEG) is a test to measure the electrical activity of your brain.
- Electronystagmography a test that looks at eye movements to see how well two nerves in the brain are working:
- Vestibular nerve (eighth cranial nerve), which runs from the brain to the ears
- Occulomotor nerve, which runs from the brain to the eyes
- Warming and cooling the inner ear with air or water to test eye reflexes (caloric stimulation). Caloric stimulation is a test that uses differences in temperature to diagnose damage to the acoustic nerve. This is the nerve that is involved in hearing and balance. The test also checks for damage to the brain stem.
- Head CT scan or an MRI scan.
Labyrinthitis treatment
The symptoms of labyrinthitis usually pass within a few weeks.
Labyrinthitis is usually treated using a combination of self-help techniques and medication.
Treatment involves drinking plenty of fluid to avoid becoming dehydrated, bed rest, and medication to help you cope better with the symptoms.
Most cases of labyrinthitis are caused by a viral infection, in which case antibiotics won’t help. But you’ll be offered antibiotics if your doctor thinks your infection is bacterial.
Contact your doctor if your symptoms don’t improve after three weeks. You may need to be referred to an ear, nose and throat (ENT) specialist.
A small number of people have symptoms that persist for several months or, in some cases, years. This requires a more intensive type of treatment called vestibular rehabilitation therapy. Vestibular rehabilitation therapy is a specialized form of physiotherapy may be recommended to treat long-term (chronic) labyrinthitis.
Self-help
In the early stages of labyrinthitis you may feel constantly dizzy and have severe vertigo. Drink plenty of liquid, particularly water, little and often to avoid becoming dehydrated.
You should rest in bed to avoid falling and injuring yourself. Your symptoms should improve after a few days and you shouldn’t feel dizzy all the time.
Follow your health care provider instructions about taking care of yourself at home. Doing these things can help you manage vertigo:
- Stay still and rest.
- Avoid sudden movements or position changes.
- Rest during severe episodes. Slowly resume activity. You may need help walking when you lose your balance during attacks.
- Avoid bright lights, TV, and reading during attacks.
- Ask your doctor about balance therapy. This may help once nausea and vomiting have passed.
You should avoid the following for 1 week after symptoms disappear:
- Driving
- Operating heavy machinery
- Climbing
A sudden dizzy spell during these activities can be dangerous.
Being dizzy can cause you to lose your balance, fall, and hurt yourself. These tips can help keep symptoms from getting worse and keep you safe:
- When you feel dizzy, sit down right away.
- To get up from a lying position, slowly sit up and stay seated for a few moments before standing.
- When standing, make sure you have something to hold on to.
- Avoid sudden movements or position changes.
- You may need a cane or other help walking when symptoms are severe.
- Avoid bright lights, TV, and reading during a vertigo attack. They may make symptoms worse.
- Avoid activities such as driving, operating heavy machinery, and climbing while you are having symptoms.
If symptoms continue, ask your provider about balance therapy. Balance therapy includes head, eye, and body exercises you can do at home to help train your brain to overcome dizziness.
Symptoms of labyrinthitis can cause stress. Make healthy lifestyle choices to help you cope, such as:
- Eat a well-balanced, healthy diet. DO NOT overeat.
- Exercise regularly, if possible.
- Get enough sleep.
- Limit caffeine and alcohol.
Help ease stress by using relaxation techniques, such as:
- Deep breathing
- Guided imagery
- Meditation
- Progressive muscle relaxation
- Tai chi
- Yoga
Medication
If your symptoms are severe, your doctor may prescribe medication.
Medications could include:
- Antihistamines – Benadryl (diphenhydramine), Phenergen (promethazine hydrochloride) and Antivert (meclizine)
- Medicines to control nausea and vomiting, such as prochlorperazine
- Medicines to relieve dizziness, such as meclizine or scopolamine
- Benzodiazepine Sedatives, such as Ativan (lorazepam) and Valium (diazepam) – reduces activity inside your central nervous system, making your brain less likely to be affected by the abnormal signals coming from your vestibular system, the part of the labyrinth that affects balance
- An antiemetic (vestibular sedative) – can help relieve the symptoms of nausea and vomiting
- Corticosteroids (e.g. prednisone) – to reduce inflammation
- Antibiotics (e.g., amoxicillin)– may be prescribed if labyrinthitis is thought to be caused by a bacterial infection
- Antiviral medicines (e.g., Acyclovir) – may be prescribed if labyrinthitis is thought to be caused by a viral infection
Check the patient information leaflet that comes with your medication for a full list of possible side effects.
If you have severe vomiting, you may be admitted to the hospital.
Chronic labyrinthitis
A small number of people experience dizziness and vertigo for months or even years. This is sometimes known as chronic labyrinthitis.
The symptoms aren’t usually as severe as when you first get the condition, but even mild dizziness can have an impact on your quality of life and daily activities.
Vestibular rehabilitation therapy
Vestibular rehabilitation therapy can help people with chronic labyrinthitis.
Vestibular rehabilitation therapy uses exercises to help retrain your brain and nervous system to compensate for the abnormal signals coming from the vestibular system.
It’s usually carried out under the supervision of a specially trained physiotherapist, who will use a range of exercises to:
- co-ordinate your hand and eye movements
- stimulate sensations of dizziness so your brain gets used to the disruptive signals sent by your vestibular system and starts to ignore them
- improve your balance and walking ability
- improve your strength and fitness
Labyrinthitis exercises
Please note that you should not attempt any of these exercises without first seeing an ENT specialist or physiotherapist for a comprehensive assessment, advice and guidance. Your doctor can refer you. Some of these exercises will not be suitable for everyone, and some are only suitable for certain conditions.
Make sure that you are in a safe environment before you start any of the exercises to reduce the risk of injury. Do not complete any exercises if you feel that you are risk of falling without safety measures in place to stop this. It is also important to note that you may experience mild dizziness whilst doing these exercises. This is completely normal.
The aims of the labyrinthitis exercises include relaxing the neck and shoulder muscles, training the eyes to move independently of the head, practising good balance in everyday situations, practising the head movements that cause dizziness (to help the development of vestibular compensation), improving general co-ordination, and encouraging natural unprompted movement.
Vestibular compensation is a process that allows the brain to regain balance control and minimize dizziness symptoms when there is damage to, or an imbalance between, the right and left vestibular organs (balance organs) in the inner ear. Essentially, the brain copes with the disorientating signals coming from the inner ears by learning to rely more on alternative signals coming from the eyes, ankles, legs and neck to maintain balance.
Labyrinthitis exercises (Cawthorne-Cooksey Exercises) might include the following:
- In bed or sitting:
- A. Eye movements
- Up and down
- From side to side
- Focusing on finger moving from three feet to one foot away from face
- B. Head movements
- Bending forwards and backwards
- Turning from side to side
- A. Eye movements
- Sitting:
- A. Eye and head movements, as 1)
- B. Shrug and circle shoulders
- C. Bend forward and pick up objects from the ground
- D. Bend side to side and pick up objects from the ground
- Standing:
- A. Eye, head and shoulder movements, as 1) and 2)
- B. Change from a sitting to a standing position with eyes open, then closed (please note this is not advised for the elderly with postural hypertension)
- C. Throw a ball from hand to hand above eye level
- D. Throw a ball from hand to hand under the knee
- E. Change from a sitting to a standing position, turning around in between
- Moving about:
- A. Walk up and down a slope
- B. Walk up and down steps
- C. Throw and catch a ball
- D. Any game involving stooping, stretching and aiming (for example, bowling)
Gaze stabilization exercises
The aim of gaze stabilization exercises is to improve vision and the ability to focus on a stationary object while the head is moving.
Your therapist should assess you and say which exercises are suitable for you.
- Look straight ahead and focus on a letter (for example, an ‘E’) held at eye level in front of you.
- Turn your head from side to side, keeping your eyes focused on the target letter. Build up the speed of your head movement. It is crucial that the letter stays in focus. If you get too dizzy, slow down.
- Start doing the exercise for a length of time that brings on mild to moderate symptoms (you could use the number rating scale). This might only be for 10 seconds. Over time, you can build up to one minute (the brain needs this time in order to adapt). Build up gradually to repeat three to five times a day. You can also do this exercise with an up and down (nodding) movement.
Progressions with this exercise can include placing the target letter on a busy background. You should start the exercise whilst seated and then move on to standing.