Contents
What is prickly heat
Prickly heat is also known as sweat rash or miliaria. Prickly heat is a group of skin conditions that arise from blockage of eccrine sweat ducts. Prickly heat is frequently seen in hot, humid or tropical climates, in patients in hospital, and in the neonatal period. There are three types of prickly heat (miliaria) classified by the level of blockage of the sweat duct. These include miliaria crystallina, miliaria rubra and miliaria profunda.
Miliaria (prickly heat) appears in about 15% of newborns. Babies are more commonly affected than children or adults as their sweat ducts are not yet fully developed.
Adults may also be affected, particularly those who work in humid and hot conditions.
Prickly heat rash is uncomfortable but usually harmless. It should clear up on its own after a few days.
The complications of miliaria include:
- Secondary bacterial infection, most commonly caused by staphylococci
- Impaired thermoregulation
- Hyperhidrosis in non-affected areas. In rare cases where a person suffers from chronic and recurrent miliaria rubra or miliaria profunda, a large number of sweat glands may end up not functioning properly. This can lead to compensatory facial sweating.
Miliaria spots can become infected and form abscesses (pus-filled lumps). In addition, when a large surface area of the body is affected, affected individuals can develop a high temperature and suffer from heat stress syndrome.
However, most cases of miliaria resolve within a day or two after changing to a cooler environment without any treatment or complications.
Prickly heat treatment
Miliaria usually disappears after the body is cooled down. It is best prevented by avoiding overheating and over swaddling.
More severe cases (e.g. miliaria profunda) can take several weeks to resolve as time is required for the plugs that block the opening of sweat ducts to be pushed outward by new sweat duct cells.
General measures recommended to improve symptoms:
- Avoid further sweating and irritation/friction of the skin.
- Good ventilation is important.
- Wear loose cotton clothing.
- Avoid plastic covered mattresses.
Soothing lotions (e.g. calamine lotion) or topical steroids may help to relieve symptoms.
Antiseptics and antibiotics may be recommended if a secondary infection is suspected.
What are sweat glands?
Sweating prevents overheating of your body, because sweat cools your skin as it evaporates. Only mammals have sweat glands (sudoriferous glands). Humans have more than 2.5 million sweat glands distributed over the entire skin surface, except on the nipples and parts of the external genitalia. Humans normally produce about 500 ml of sweat per day, but this amount can increase to 12 liters (over 3 gallons) on hot days during vigorous exercise. Hair interferes with the evaporation of sweat and the ability to cool the body, so the need for increased temperature regulation through sweating led to a reduction of hairiness in humans.
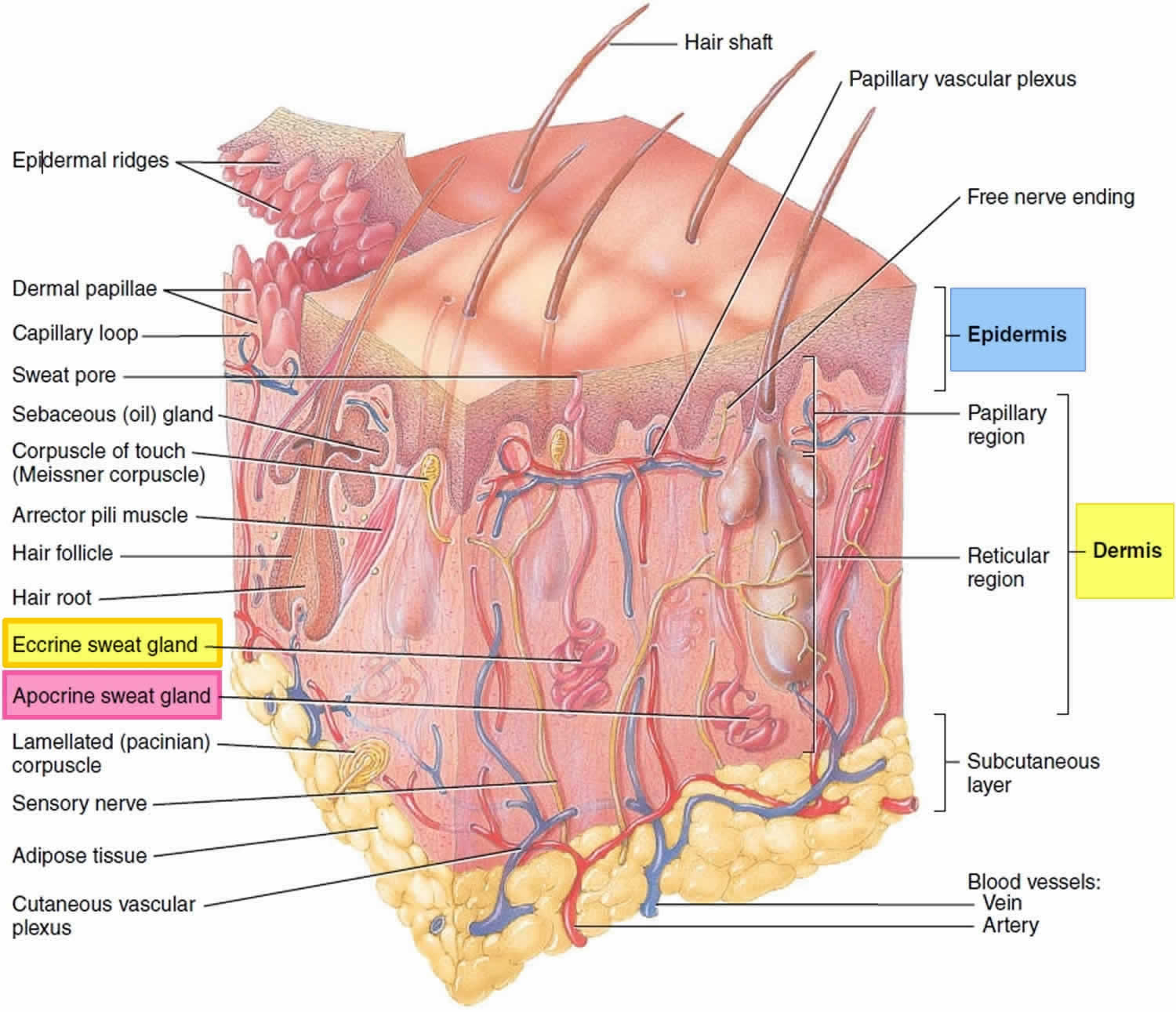
There are two types of sweat glands, both of which increase their secretion in response to stress as well as to heat: eccrine and apocrine glands.
Eccrine glands (“secreting”) are by far the more numerous type (Figure 1). They are most abundant on the palms, soles, and forehead. Each is a coiled version of a simple tubular gland. The coiled, secretory base lies in the deep dermis and hypodermis, and the duct runs superficially to open at the skin surface through a funnel-shaped pore. (Although most pores on the skin surface are sweat pores, the “pores” seen on the face are openings of hair follicles.)
Apocrine glands are mostly confined to the armpits, anal, and genital areas. They are larger than eccrine glands, and their ducts open into hair follicles. Apocrine glands produce a special kind of sweat consisting of fatty substances and proteins, in addition to the components of true sweat. For this reason, apocrine sweat is viscous and sometimes has a milky or yellow color. This product is odorless when first secreted, but as its organic molecules are decomposed by bacteria on the skin, it takes on a musky smell. This is the source of body odor.
Apocrine glands start to function at puberty under the influence of androgens. Their activity is increased by sexual foreplay, and they enlarge and recede with the phases of a woman’s menstrual cycle. The secretions from the apocrine glands were identified as true human pheromones (chemical signals that convey information to a member of the same species) in the late 1990s when it was shown that they are responsible for the synchrony of the menstrual cycle that occurs in females who live together.
Apocrine glands are involved with sexual signaling and appear to function in attractiveness and mate selection. The genes that encode for the immune system, the major histocompatibility complex (MHC), also influence secretions from apocrine glands. Each person has a unique set of these genes. In experiments, the body odor scents that women selected as “sexy” or “attractive” came from men who had immune system genes most different from their own. Mates with complementary immune system genes provide their offspring with greater disease protection and decreased likelihood of recessive disorders.
Figure 1. Sweat glands
What causes prickly heat?
Miliaria is caused by obstruction of sweat ducts, often from heat and excess sweating.
Miliaria results from sweating. The main contributing causes are:
- Immature sweat ducts in a newborn child. A newborn’s sweat ducts aren’t fully developed. They can rupture more easily, trapping perspiration beneath the skin. Heat rash can develop in the first week of life, especially if the infant is being warmed in an incubator, is dressed too warmly or has a fever.
- A hot and humid environment.
- Intense physical activity. Intense exercise, hard work or any activity that causes you to sweat heavily can lead to heat rash.
- Fever
- Occlusion of the skin with non-porous dressings or synthetic clothing against the skin
- Prolonged bed rest. Heat rash can also occur in people who are confined to bed for long periods, especially if they have a fever.
Common situations in which blockage of the sweat ducts occurs include:
- excessive sweating under synthetic clothing
- swaddling newborns in multiple garments
- lying in bed for long periods (e.g. because of medical illness or immobility), particularly with a fever.
Other diseases and treatments that have been associated with miliaria are:
- Adverse reaction to medication (isotretinoin, doxorubicin)
- Stevens-Johnson syndrome / toxic epidermal necrolysis
- Genetic disease (Morvan syndrome and pseudohypoaldosteronism type I)
- Radiotherapy
Prickly heat rash prevention
To help protect yourself or your child from heat rash:
- Avoid overdressing. In summer, wear soft, lightweight, cotton clothing. In winter, children should dress only as warmly as an adult.
- Avoid tightfitting clothes that can irritate skin.
- When it’s hot, stay in the shade or in an air-conditioned building or use a fan to circulate the air.
- Keep your sleeping area cool and well-ventilated.
What does prickly heat rash look like?
Miliaria commonly appears in areas of skin that have been blocked particularly around the neck and upper trunk in both children and adults. Other areas that can be affected include the groin, waistline, under the breasts, skin folds and armpits.
Unlike acne, miliaria does not arise around hair follicles.
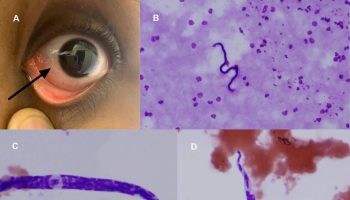
- Miliaria crystallina (miliaria sudamina) appears as small ~ 1–2 mm, superficial and clear blisters. These break easily from mild friction or bathing. There is no inflammation. The blisters are usually seen widely spread on the head, neck, and upper trunk. There is no inflammation. The blisters are usually seen widely spread on the head, neck, and upper trunk. Miliaria crystallina is most commonly seen in neonates with the mean age of 1 week, affecting up to 9% of all neonates (see Figure 2). It can also occur in adults with fever (Figure 3).
- Miliaria rubra appears as small, red flat or bumpy spots that are usually very itchy. Miliaria rubra is the most common form of miliaria. It is seen in children and in up to 30% of adults who move to a tropical environment or are unexpectedly exposed to heat and humidity. In children, miliaria affects the skin folds of the neck, axilla or groin. In adults, miliaria often affects the upper trunk, scalp, neck and flexures, particularly areas of friction with clothing. In chronic and recurrent cases, the lesions can turn into pus-filled spots.
- Miliaria pustulosa is a variant of milia rubra in which there are pustules.
- Miliaria profunda the result of sweat leaking into the middle layer of skin (dermis), appears as deep red or flesh–colored, 1–3 mm diameter papules usually arise on the trunk and extremities. These lesions are generally not itchy as they appear below the itch receptors. Miliaria profunda is rare and presents in adult males. It is a complication of repeated episodes of miliaria rubra.
Figure 2. Miliaria crystallina in an infant – note that the lesions are confluent
Figure 3. Miliaria crystallina
Figure 4. Miliaria rubra
Figure 5. Miliaria pustulosa – is a variant of miliaria rubra in which there are pustules (the pustules are not the result of secondary infection and are self-limiting but can get secondarily infected and can be associated with severe itch)
Prickly heat rash symptoms
The symptoms of prickly heat rash are:
- small red spots
- an itchy, prickly feeling
- redness and mild swelling
The symptoms are often the same in adults and children.
It can appear anywhere on the body and spread, but it’s not infectious to other people.
How is miliaria diagnosed?
Miliaria is most often diagnosed based on the typical appearance of the lesions. The doctor may perform a simple diagnostic test where a fine needle is used to rupture the blister so that the clear fluid/sweat can be assessed.
A biopsy of the skin may be needed to confirm the diagnosis and distinguish it from other conditions that look similar (e.g. erythema toxicum neonatorum, neonatal cephalic pustulosis, candidiasis, Grover’s disease).
The doctor may also request a skin swab to rule out secondary infection.
Individuals who develop heat stress syndrome may need to have blood tests.
Prickly heat rash treatment
Management of prickly heat requires heat and humidity to be controlled to reduce sweating and the avoidance of irritation to the skin. Strategies to avoid sweating and reduce irritation follow.
- Work in an air-conditioned office for at least a few hours a day.
- Sleep in a ventilated, cool bedroom.
- Move away from a tropical climate.
- Avoid excessive clothing and tight clothing.
- Avoid excessive soap and irritants.
- Wear shirts and blouses made of breathable synthetic fabrics or cotton.
- Remove wet clothing.
Treatment of miliaria may include:
- Cool water compresses
- Calamine lotion to relieve discomfort; because of its drying effect, an emollient may be required.
- Treatment of fever with antipyretic such as acetoaminophen/paracetamol
- Mild topical steroids
- Antiseptics and anti-staphylococcal antibiotics for secondary infection.
- Avoid using creams and ointments that contain petroleum or mineral oil, which can block pores further.