Contents
- What is shoulder rotator cuff tear
- Shoulder rotator cuff tear types
- When should I see a doctor for a rotator cuff tear?
- Can a rotator cuff tear be healed or strengthened without surgery?
- At what point does a rotator cuff tear require surgery to fix it?
- What options are available for surgical repair?
- How important is rehabilitation in the treatment of a rotator cuff tear?
- What is the rotator cuff
- Rotator cuff strain vs rotator cuff tear
- Rotator cuff tear signs and symptoms
- Rotator cuff tear causes
- Rotator cuff tear diagnosis
- Rotator cuff tear treatment
- Shoulder rotator cuff tear types
What is shoulder rotator cuff tear
A rotator cuff tear may result from an acute injury, such as a fall, or may be caused by normal age-related wear and tear with degeneration of the rotator cuff tendon. A rotator cuff tear can extend or get larger over time. This can occur with repetitive use or a re-injury. It is common for patients with known rotator cuff problem to have acute pain and weakness following a minor injury. This likely represents extension of an existing rotator cuff tear.
A concern with rotator cuff tears is the risk of progression, which can lead to atrophy of the rotator cuff and a tear that could have been repaired becoming irreversible 1. However, it is difficult to detect which tears will progress. Full-thickness tears and lesions in older patients are more likely to enlarge.
The effectiveness and safety of surgery for chronic rotator cuff disease in older patients are unclear 2. Patients with a suspected tear should be referred to an orthopedist for a discussion about the benefits of conservative vs. operative management. It is especially important to refer young, active, healthy patients with full-thickness tears to an orthopedist as soon as possible because early operative treatment may result in better outcomes 3.
If you know you have a rotator cuff tear, then worsening pain and decreasing strength may mean the tear is getting larger. Symptomatic rotator cuff tear is a clinical diagnosis and although confirmation of diagnosis via clinicians tend to rely heavily on imaging data from MRI 4 and ultrasound to diagnose rotator cuff disorders. A clinician’s assessment becomes even more important in the diagnosis of rotator cuff syndrome (bursitis or tendinopathy without a tear), when imaging may reveal no abnormalities. Magnetic resonance imaging without contrast media is the imaging modality of choice for diagnosing tears 5. Recent studies have demonstrated that the effectiveness of ultrasonography is similar to that of MRI for the diagnosis of rotator cuff tears, and ultrasonography is more cost-effective 6. However, it should only be used if the physician is well trained in using ultrasonography and interpreting the results.
Recent reports have highlighted the importance of patient symptoms and shoulder examination results in the management of shoulder pain. However, the diagnosis of a rotator cuff tear based on patient characteristics, symptoms, and physical examination findings remains a challenge even for subspecialists 7.
In the United States, the prevalence of shoulder pain in the population ranges from 14% to 34% 8. Rotator cuff disorders are the underlying issue in 65% to 70% of patients with shoulder pain 9 and rotator cuff tears are the leading cause of shoulder pain and shoulder-related disability accounting for 4.5 million physician visits in the United States annually 10. Rotator cuff tears accounted for 272,148 surgeries in the United States in 2006 11 and the annual cost of treating shoulder pain was $7 billion in the year 2000 in the United States 12.
If you have injured your shoulder or have chronic shoulder and arm pain, it is best to see your orthopedic surgeon. He or she can then make a diagnosis and begin treatment. Your doctor may recommend a diagnostic imaging study such as a magnetic resonance imaging (MRI) scan or an ultrasound to confirm the diagnosis.
Early diagnosis and treatment of a rotator cuff tear may prevent symptoms such as loss of strength and loss of motion from setting in. If your primary physician has already made the diagnosis, an orthopaedic surgeon can review both surgical and nonsurgical options and start treatment.
Many rotator cuff tears can be treated nonsurgically. Anti-inflammatory medication, steroid injections, and physical therapy may all be of benefit in treating symptoms of a cuff tear. The goals of treatment are to relieve pain and restore strength to the involved shoulder.
Even though most tears cannot heal on their own, good function can often be achieved without surgery. If, however, you are active and use your arm for overhead work or sports, then surgery is most often recommended because many tears will not heal without surgery.
Shoulder rotator cuff tear types
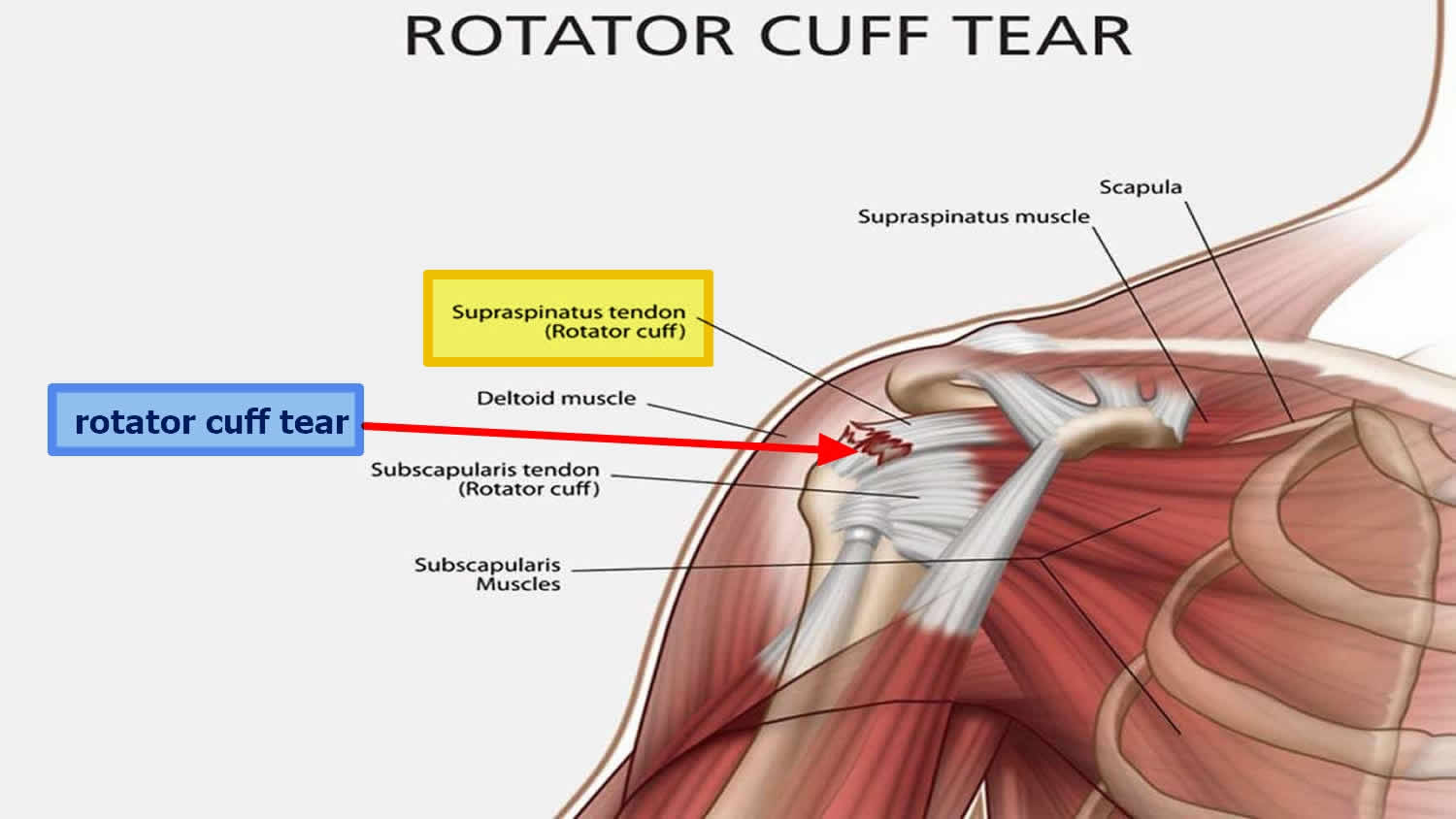
When one or more of the rotator cuff tendons is torn, the tendon no longer fully attaches to the head of the humerus.
Most tears occur in the supraspinatus tendon, but other parts of the rotator cuff may also be involved.
In many cases, torn tendons begin by fraying. As the damage progresses, the tendon can completely tear, sometimes with lifting a heavy object.
There are different types of tears:
- Partial rotator cuff tear. This type of tear is also called an incomplete tear. It damages the tendon, but does not completely sever it.
- Full-thickness rotator cuff tear. This type of tear is also called a complete tear. It separates all of the tendon from the bone. With a full-thickness tear, there is basically a hole in the tendon.
When should I see a doctor for a rotator cuff tear?
If you have injured your shoulder or have chronic shoulder and arm pain, it is best to see your orthopaedic surgeon. He or she can then make a diagnosis and begin treatment. Your doctor may recommend a diagnostic imaging study such as a magnetic resonance imaging (MRI) scan or an ultrasound to confirm the diagnosis.
Early diagnosis and treatment of a rotator cuff tear may prevent symptoms such as loss of strength and loss of motion from setting in.
If your primary physician has already made the diagnosis, an orthopaedic surgeon can review both surgical and nonsurgical options and start treatment.
Can a rotator cuff tear be healed or strengthened without surgery?
Many rotator cuff tears can be treated nonsurgically. Anti-inflammatory medication, steroid injections, and physical therapy may all be of benefit in treating symptoms of a cuff tear. The goals of treatment are to relieve pain and restore strength to the involved shoulder.
Even though most tears cannot heal on their own, good function can often be achieved without surgery.
If, however, you are active and use your arm for overhead work or sports, then surgery is most often recommended because many tears will not heal without surgery.
At what point does a rotator cuff tear require surgery to fix it?
Surgery is recommended if you have persistent pain or weakness in your shoulder that does not improve with nonsurgical treatment. Frequently, patients who require surgery will report pain at night and difficulty using the arm for lifting and reaching. Many will report ongoing symptoms despite several months of medication and limited use of the arm.
Surgery is also indicated in active individuals who use the arm for overhead work or sports. Pitchers, swimmers, and tennis players are common examples.
What options are available for surgical repair?
The type of repair performed is based on the findings at surgery. A partial tear may require only a trimming or smoothing procedure called a débridement. A full-thickness tear within the substance of the tendon can be repaired side to side. If the tendon is torn from its insertion on the humerus (the most common injury), it is repaired directly to bone.
Three techniques are used for rotator cuff repair: traditional open repair, mini-open repair, and arthroscopic repair.
Your orthopaedic surgeon can recommend which technique is best for you.
How important is rehabilitation in the treatment of a rotator cuff tear?
Rehabilitation plays a critical role in both the nonsurgical and surgical treatment of a rotator cuff tear.
When a tear occurs, there is frequently atrophy of the muscles around the arm and loss of motion of the shoulder. An exercise or physical therapy program is necessary to regain strength and improve function in the shoulder.
Even though surgery repairs the defect in the tendon, the muscles around the arm remain weak, and a strong effort at rehabilitation is necessary for the procedure to succeed. Complete rehabilitation after surgery may take several months.
Your orthopaedic surgeon can prescribe an appropriate program based on your needs and the findings at surgery.
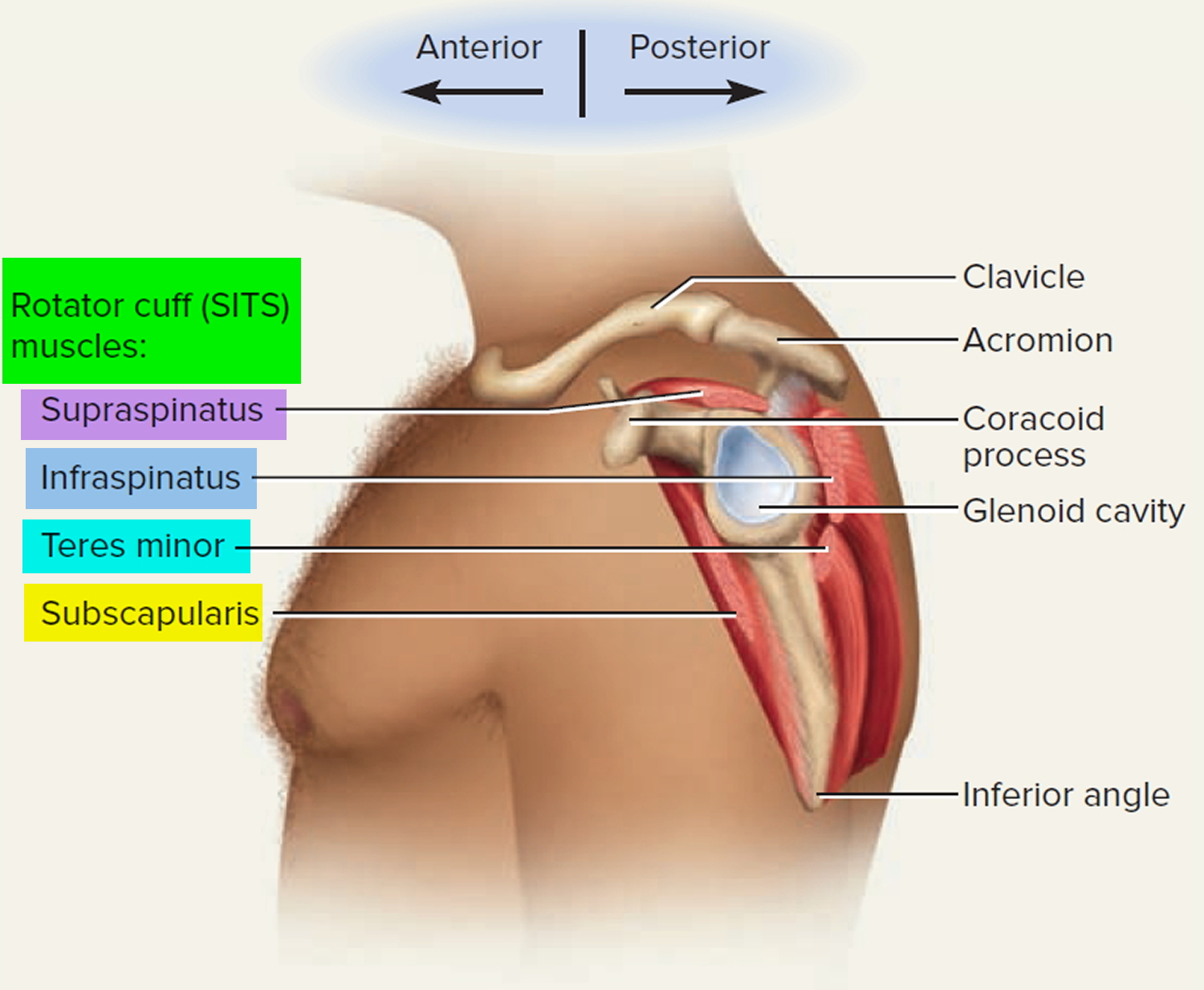
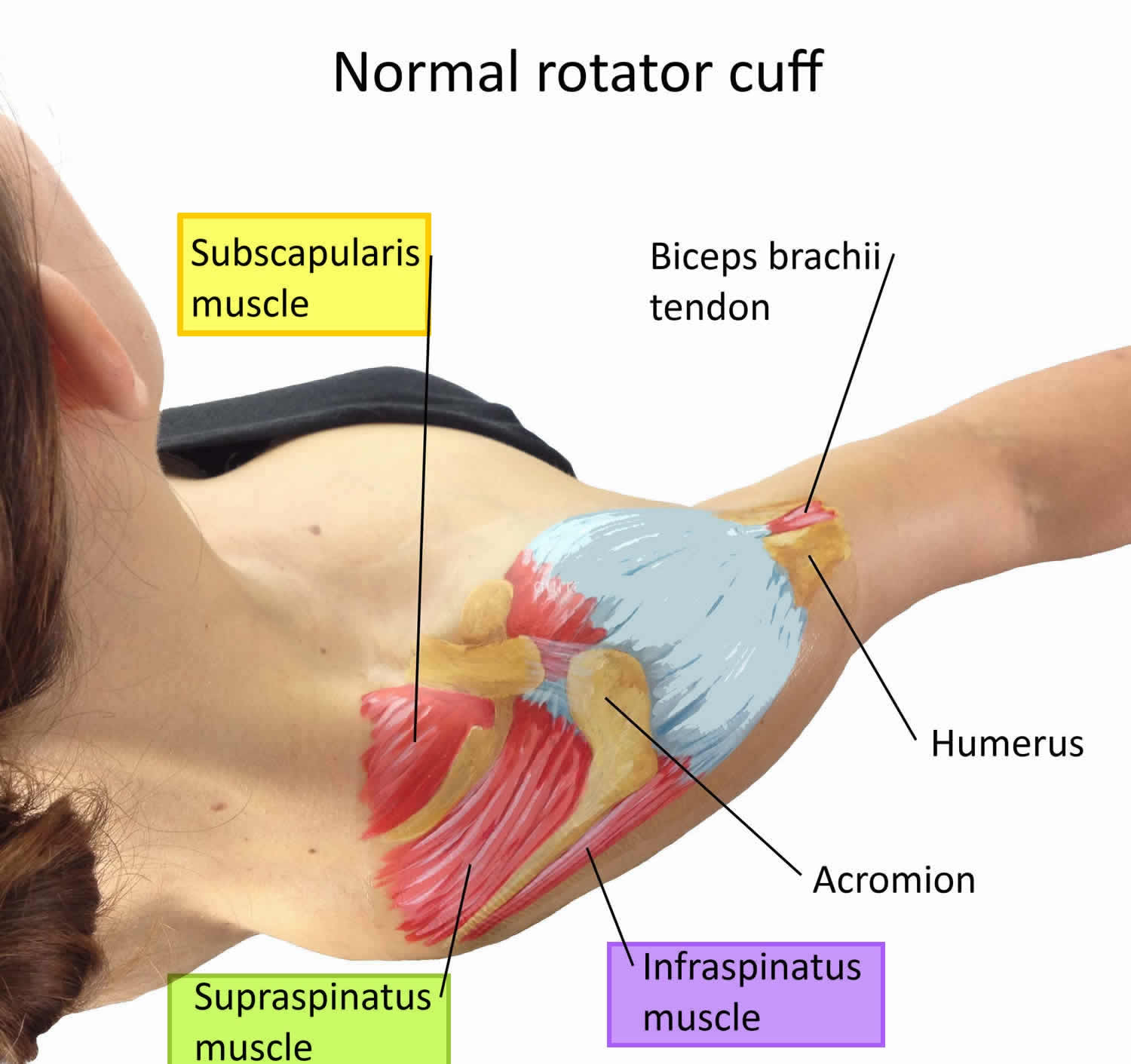
What is the rotator cuff
The rotator cuff is a group of four muscles that come together as tendons to form a “cuff” over the head of the humerus (upper arm bone). The rotator cuff is a group of muscles and their tendons that hold the shoulder joint in place by attaching the shoulder blade to the humerus (upper arm bone) and covering the head of the humerus. The rotator cuff stabilises the shoulder joint and helps move the shoulder. The 4 muscles (and their tendons) that make up the rotator cuff are:
- the supraspinatus;
- the infraspinatus;
- the subscapularis; and
- the teres minor.
The four muscles—supraspinatus, infraspinatus, subscapularis and teres minor—originate from the scapula (shoulder blade). The long head of the biceps tendon is also often included in rotator cuff pathology. The rotator cuff tendons attach to the head of the humerus in special spots referred to as the greater and lesser tuberosities.
The rotator cuff tendons cover the head of the humerus (upper arm bone), helping keep the head of the humerus in your shoulder joint and helping you to raise and rotate your arm.
There is a lubricating sac called a bursa between the rotator cuff and the bone on top of your shoulder (acromion). The bursa allows the rotator cuff tendons to glide freely when you move your arm. When the rotator cuff tendons are injured or damaged, this bursa can also become inflamed and painful.
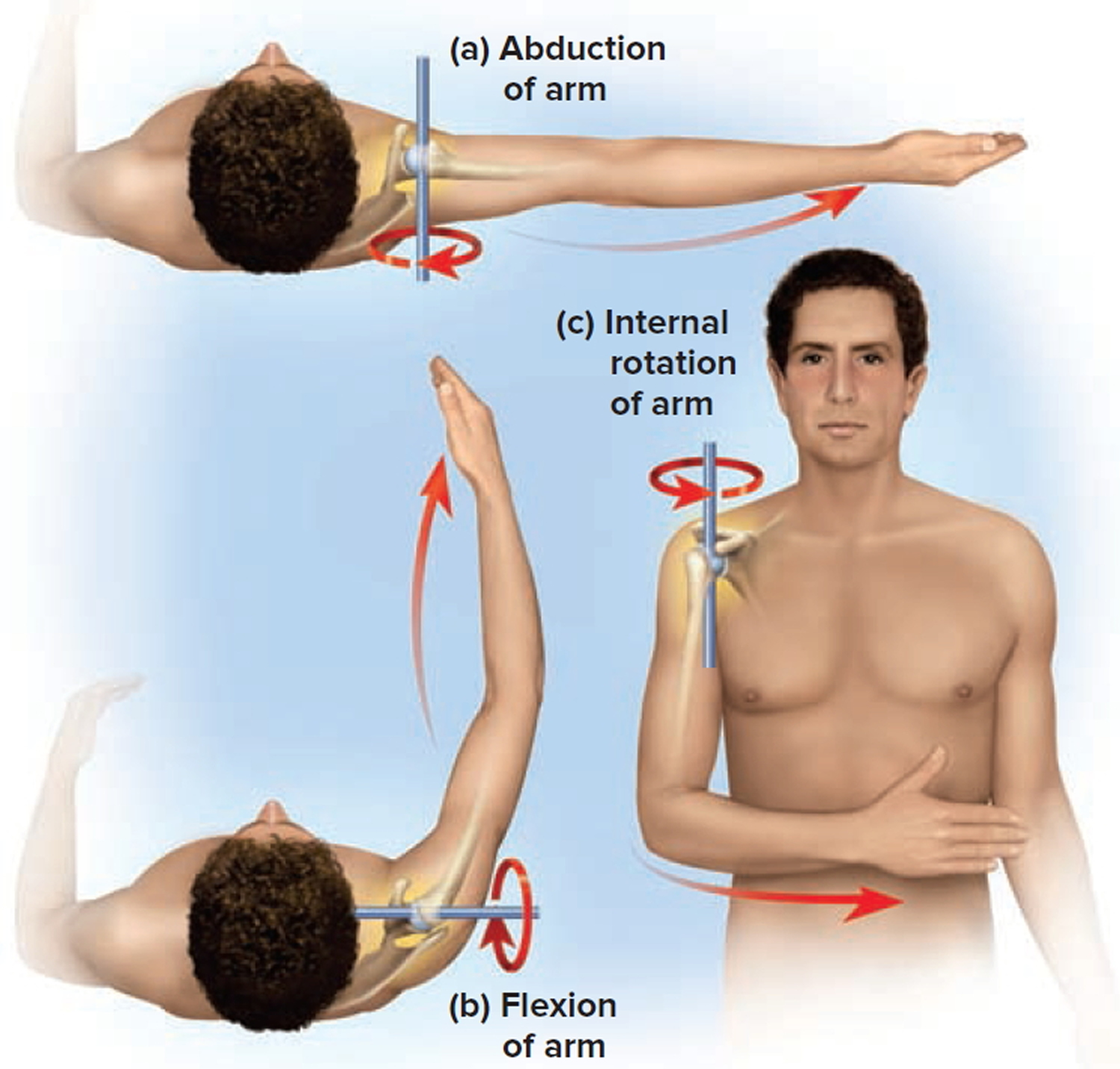
Some of the actions of the rotator cuff are to rotate the upper arm towards the body (internal rotation) and away from the body (external rotation), and to help raise the arm (abduction).
The supraspinatus assists in elevation (abduction) of the arm; infraspinatus and teres minor in external rotation, and; subscapularis in internal rotation.
Figure 1. Shoulder joint rotator cuff muscles
Figure 2. Shoulder joint (lateral view)
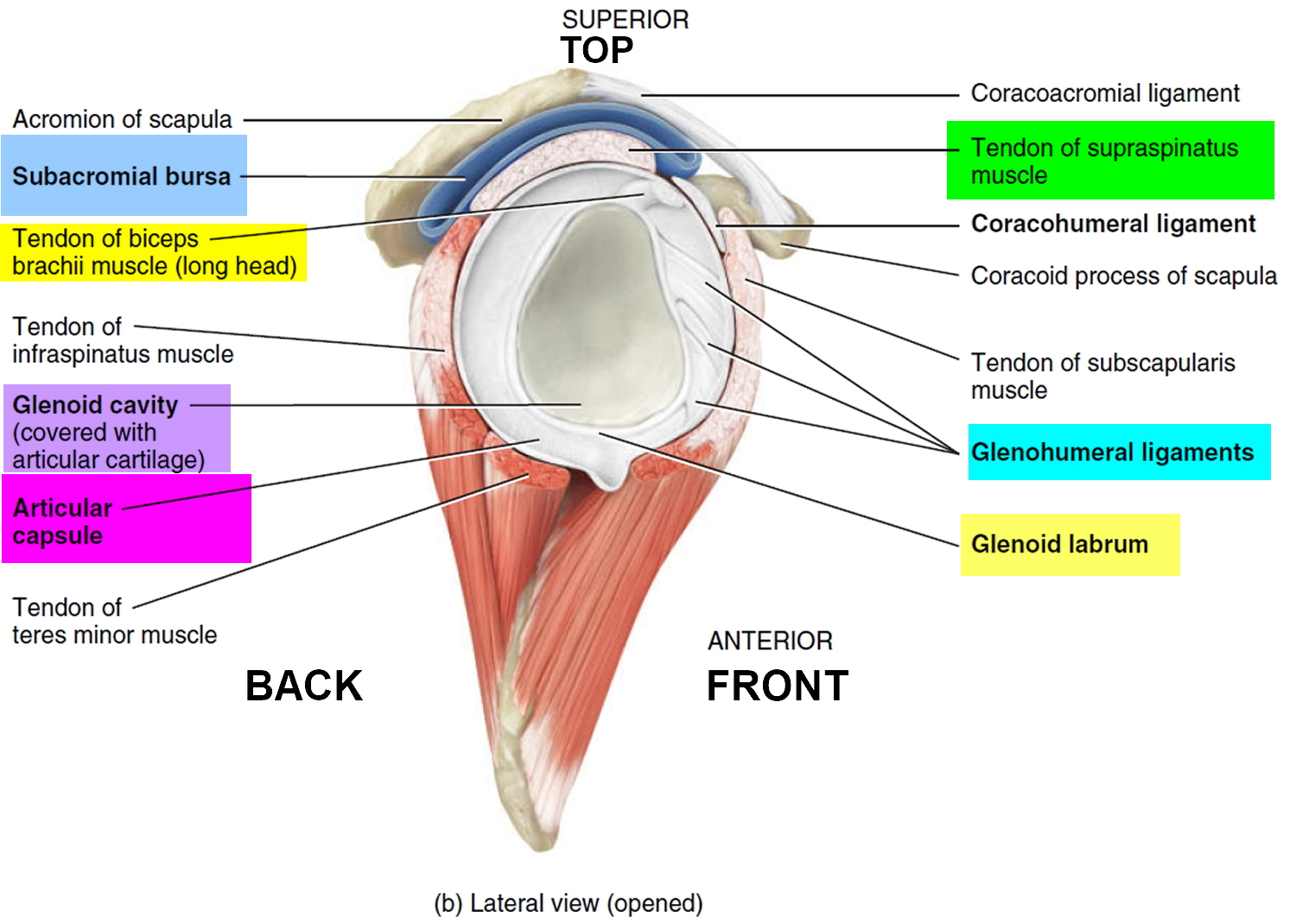 Figure 3. Full thickness rotator cuff tear – the red arrow indicate a full-thickness tear in the supraspinatus tendon, the most common location for rotator cuff tears.
Figure 3. Full thickness rotator cuff tear – the red arrow indicate a full-thickness tear in the supraspinatus tendon, the most common location for rotator cuff tears.Rotator cuff strain vs rotator cuff tear
The rotator cuff is a common source of pain in the shoulder. Pain can be the result of:
- Tendinitis. The rotator cuff tendons can be irritated or damaged.
- Bursitis. The bursa can become inflamed and swell with more fluid causing pain.
- Impingement. When you raise your arm to shoulder height, the space between the acromion and rotator cuff narrows. The acromion can rub against (or “impinge” on) the tendon and the bursa, causing irritation and pain.
Rotator cuff strain is common in both young athletes and middle-aged people. Young athletes who use their arms overhead for swimming, baseball, and tennis are particularly vulnerable. Those who do repetitive lifting or overhead activities using the arm, such as paper hanging, construction, or painting are also susceptible.
Rotator cuff pain may develop as the result of a minor injury. Sometimes, it occurs with no apparent cause.
Rotator cuff strain commonly causes local swelling and tenderness in the front of the shoulder. You may have pain and stiffness when you lift your arm. There may also be pain when the arm is lowered from an elevated position.
Beginning rotator cuff strain symptoms may be mild. Patients frequently do not seek treatment at an early stage. These symptoms may include:
- Minor pain that is present both with activity and at rest
- Pain radiating from the front of the shoulder to the side of the arm
- Sudden pain with lifting and reaching movements
- Athletes in overhead sports may have pain when throwing or serving a tennis ball
As the problem progresses, the symptoms increase:
- Pain at night
- Loss of strength and motion
- Difficulty doing activities that place the arm behind the back, such as buttoning or zippering
If the pain comes on suddenly, the shoulder may be severely tender. All movement may be limited and painful.
Rotator cuff strain imaging tests
Imaging tests which may help your doctor confirm your diagnosis include:
- X-rays. Becauses x-rays do not show the soft tissues of your shoulder like the rotator cuff, plain x-rays of a shoulder with rotator cuff pain are usually normal or may show a small bone spur. A special x-ray view, called an “outlet view,” sometimes will show a small bone spur on the front edge of the acromion.
- Magnetic resonance imaging (MRI) and ultrasound. These studies can create better images of soft tissues like the rotator cuff tendons. They can show fluid or inflammation in the bursa and rotator cuff. In some cases, partial tearing of the rotator cuff will be seen.
Rotator cuff strain treatment
The goal of treatment is to reduce pain and restore function. In planning your treatment, your doctor will consider your age, activity level, and general health.
Nonsurgical Treatment
In most cases, initial treatment is nonsurgical. Although nonsurgical treatment may take several weeks to months, many patients experience a gradual improvement and return to function.
- Rest. Your doctor may suggest rest and activity modification, such as avoiding overhead activities.
- Non-steroidal anti-inflammatory medicines (NSAIDs). Drugs like ibuprofen and naproxen reduce pain and swelling.
- Physical therapy. A physical therapist will initially focus on restoring normal motion to your shoulder. Stretching exercises to improve range of motion are very helpful. If you have difficulty reaching behind your back, you may have developed tightness of the posterior capsule of the shoulder (capsule refers to the inner lining of the shoulder and posterior refers to the back of the shoulder). Specific stretching of the posterior capsule can be very effective in relieving pain in the shoulder. Once your pain is improving, your therapist can start you on a strengthening program for the rotator cuff muscles.
- Steroid injection. If rest, medications, and physical therapy do not relieve your pain, an injection of a local anesthetic and a cortisone preparation may be helpful. Cortisone is a very effective anti-inflammatory medicine. Injecting it into the bursa beneath the acromion can relieve pain.
Surgical Treatment
When nonsurgical treatment does not relieve pain, your doctor may recommend surgery.
The goal of surgery is to create more space for the rotator cuff. To do this, your doctor will remove the inflamed portion of the bursa. He or she may also perform an anterior acromioplasty, in which part of the acromion is removed. This is also known as a subacromial decompression. These procedures can be performed using either an arthroscopic or open technique.
Arthroscopic technique. In arthroscopy, thin surgical instruments are inserted into two or three small puncture wounds around your shoulder. Your doctor examines your shoulder through a fiberoptic scope connected to a television camera. He or she guides the small instruments using a video monitor, and removes bone and soft tissue. In most cases, the front edge of the acromion is removed along with some of the bursal tissue.
Your surgeon may also treat other conditions present in the shoulder at the time of surgery. These can include arthritis between the clavicle (collarbone) and the acromion (acromioclavicular arthritis), inflammation of the biceps tendon (biceps tendonitis), or a partial rotator cuff tear.
Open surgical technique. In open surgery, your doctor will make a small incision in the front of your shoulder. This allows your doctor to see the acromion and rotator cuff directly.
Rehabilitation
After surgery, your arm may be placed in a sling for a short period of time. This allows for early healing. As soon as your comfort allows, your doctor will remove the sling to begin exercise and use of the arm.
Your doctor will provide a rehabilitation program based on your needs and the findings at surgery. This will include exercises to regain range of motion of the shoulder and strength of the arm. It typically takes 2 to 4 months to achieve complete relief of pain, but it may take up to a year.
Rotator cuff tear signs and symptoms
Typically, you will feel pain in the front of your shoulder that radiates down the side of your arm. It may be present with overhead activities such as lifting or reaching. You may feel pain when you try to sleep on the affected side. You may note weakness of your arm and difficulty with routine activities such as combing your hair or reaching behind your back.
If the rotator cuff tear occurs with injury, such as from a fall, you may experience intense pain, a snapping sensation, and immediate weakness in your upper arm.
The most common symptoms of a rotator cuff tear include:
- Pain at rest and at night, particularly if lying on the affected shoulder
- Pain when lifting and lowering your arm or with specific movements
- Weakness when lifting or rotating your arm
- Crepitus or crackling sensation when moving your shoulder in certain positions
Rotator cuff tear that develop slowly due to overuse also cause pain and arm weakness. You may have pain in the shoulder when you lift your arm, or pain that moves down your arm. At first, the pain may be mild and only present when lifting your arm over your head, such as reaching into a cupboard. Over-the-counter medication, such as aspirin or ibuprofen, may relieve the pain at first.
Over time, the pain may become more noticeable at rest, and no longer goes away with medications. You may have pain when you lie on the painful side at night. The pain and weakness in the shoulder may make routine activities such as combing your hair or reaching behind your back more difficult.
It should be noted that some rotator cuff tears are not painful. These tears, however, may still result in arm weakness and other symptoms.
Rotator cuff tear causes
There are two main causes of rotator cuff tears: injury and degeneration.
Acute rotator cuff tear
If you fall down on your outstretched arm or lift something too heavy with a jerking motion, you can tear your rotator cuff. This type of tear can occur with other shoulder injuries, such as a broken collarbone or dislocated shoulder.
Degenerative rotator cuff tear
Most tears are the result of a wearing down of the tendon that occurs slowly over time. This degeneration naturally occurs as we age. Rotator cuff tears are more common in the dominant arm. If you have a degenerative tear in one shoulder, there is a greater likelihood of a rotator cuff tear in the opposite shoulder — even if you have no pain in that shoulder.
Several factors contribute to degenerative or chronic rotator cuff tears:
- Repetitive stress. Repeating the same shoulder motions again and again can stress your rotator cuff muscles and tendons. Baseball, tennis, rowing, and weightlifting are examples of sports activities that can put you at risk for overuse tears. Many jobs and routine chores can cause overuse tears, as well.
- Lack of blood supply. As we get older, the blood supply in our rotator cuff tendons lessens. Without a good blood supply, the body’s natural ability to repair tendon damage is impaired. This can ultimately lead to a tendon tear.
- Bone spurs. As we age, bone spurs (bone overgrowth) often develop on the underside of the acromion bone. When we lift our arms, the spurs rub on the rotator cuff tendon. This condition is called shoulder impingement, and over time will weaken the tendon and make it more likely to tear.
Risk factors for rotator cuff tear
Because most rotator cuff tears are largely caused by the normal wear and tear that goes along with aging, people over 40 are at greater risk.
People who do repetitive lifting or overhead activities are also at risk for rotator cuff tears. Athletes are especially vulnerable to overuse tears, particularly tennis players and baseball pitchers. Painters, carpenters, and others who do overhead work also have a greater chance for tears.
Although overuse tears caused by sports activity or overhead work also occur in younger people, most tears in young adults are caused by a traumatic injury, like a fall.
Rotator cuff tear diagnosis
Medical history and physical examination
After discussing your symptoms and medical history, your doctor will examine your shoulder. He or she will check to see whether it is tender in any area or whether there is a deformity. To measure the range of motion of your shoulder, your doctor will have you move your arm in several different directions. He or she will also test your arm strength.
Your doctor will check for other problems with your shoulder joint. He or she may also examine your neck to make sure that the pain is not coming from a “pinched nerve,” and to rule out other conditions, such as arthritis.
Imaging Tests
Other tests which may help your doctor confirm your diagnosis include:
- X-rays. The first imaging tests performed are usually x-rays. Because x-rays do not show the soft tissues of your shoulder like the rotator cuff, plain x-rays of a shoulder with rotator cuff pain are usually normal or may show a small bone spur.
- Magnetic resonance imaging (MRI) or ultrasound. These studies can better show soft tissues like the rotator cuff tendons. They can show the rotator cuff tear, as well as where the tear is located within the tendon and the size of the tear. An MRI can also give your doctor a better idea of how “old” or “new” a tear is because it can show the quality of the rotator cuff muscles.
How to test for rotator cuff tear
There are no historical features that reliably identify full-thickness rotator cuff tears. The physical examination maneuvers that best identify the presence of a full-thickness rotator cuff tear are the internal rotation lag test, the external rotation lag test, and a positive “belly-off” sign 13. The best maneuver to help confirm the absence of a full-thickness rotator cuff tear of the subscapularis is a negative internal rotation lag test 13.
Internal rotation lag test (Lag Sign)
The examiner passively brings the patient’s arm behind the body into maximal internal rotation (around the lower back region) and pull it backwards away from the back 14. The result of this test is considered normal if the patient maintains maximum internal rotation after the examiner releases the patient’s hand. The test is positive if the patient cannot maintain this position due to weakness of the subscapularis.
External rotation lag test – test for Supraspinatus and Infraspinatus
- External Rotation Lag Sign at 0 Degrees: The patient is seated with his or her back to the physician. The elbow is passively flexed to 90°, and the shoulder is held at 20° elevation (in the scapular plane) and near maximum external rotation (i.e., maximum external rotation minus 5° to avoid elastic recoil in the shoulder) by the physician 15. The patient is then asked to actively maintain the position of external rotation as the physician releases the wrist while maintaining support of the limb at the elbow. The sign is positive when a lag, or angular drop, occurs. The magnitude of the lag is recorded to the nearest 5°. A positive test indicates postero-superior cuff (supraspinatus and infraspinatus) deficiency 16.
- External Rotation Lag Sign at 90 Degrees (Drop Sign): The patient is seated with his or her back to the physician, who holds the affected arm at 90° of elevation (in the scapular plane) and at almost full external rotation, with the elbow flexed at 90° 15. In this position the maintenance of the position of external rotation of the shoulder is a function mainly of the infraspinatus. The patient is asked to actively maintain this position as the physician releases the wrist while supporting the elbow. The sign is positive if a lag or ‘drop’ occurs. The magnitude of the lag is recorded to the nearest 5°. A positive test indicates postero-inferior cuff deficiency 16.
Belly-Off Sign
The examiner assesses the subscapularis in this test by passively bringing the shoulder of the patient into flexion and maximum internal rotation with the elbow 90° flexed. The elbow of the patient is supported by one hand of the examiner while the other hand brings the arm into maximum internal rotation placing the palm of the hand on the abdomen. The patient is then asked to keep the wrist straight and actively maintain the position of internal rotation as the examiner releases the wrist 17. If the patient cannot maintain the above position, lag occurs and the hand lifts off the abdomen resulting in a positive belly-off sign. Otherwise, the test is negative.
Bear Hug Test
The examiner instructs the patient to place the palm of the involved side on the opposite shoulder, extend the fingers (so that the patient could not resist by grabbing the shoulder), and position the elbow anterior to the body 18. The examiner then asks the patient to hold that position (resisted internal rotation) as the examiner tries to pull the patient’s hand from the shoulder with an external rotation force applied perpendicular to the forearm. The test is considered positive indicating subscapularis weakness if the patient cannot hold the hand against the shoulder or if he or she shows weakness of resisted internal rotation of greater than 20% compared with the opposite side. If the strength is comparable to that of the opposite side, without any pain, the test is negative.
Range of Motion
Active and passive range of motion is assessed. If time is a constraint, experts recommend limiting the assessment to active range of motion only since rotator cuff tears lead to loss of active range of motion and passive range of motion is often preserved. Passive motion is typically limited in glenohumeral articular disorders.
Range of motion is measured in degrees and best assessed with a goniometer. Goniometers are commercially available via numerous vendors. If range of motion cannot be assessed with a goniometer due to time constraints, subjective assessment of range of motion and comparison with the contralateral shoulder is recommended.
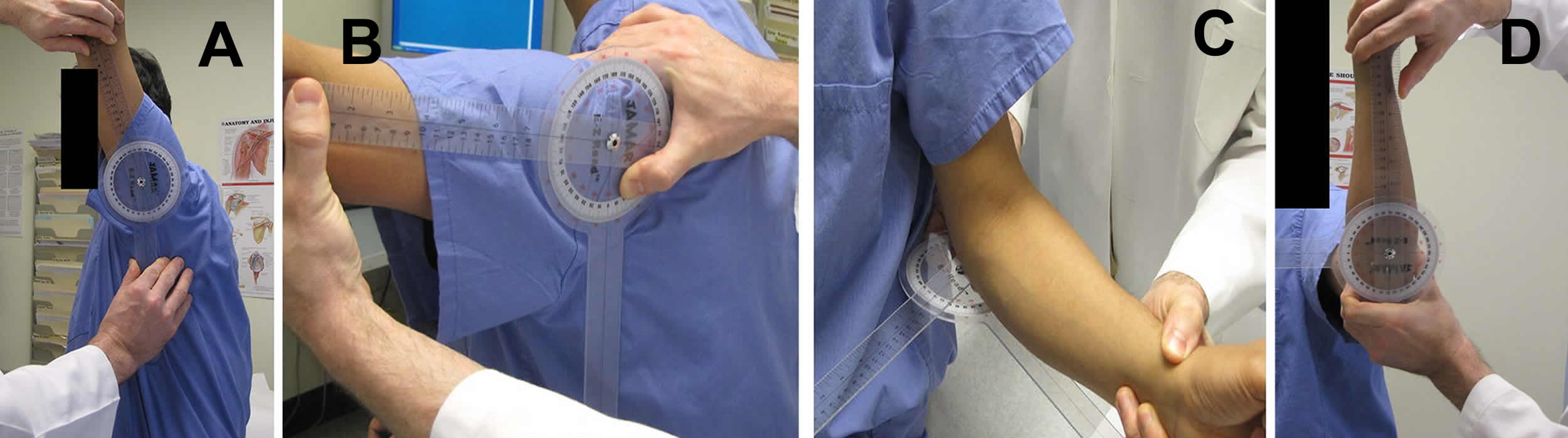
Figure 4. Shoulder joint movement
Forward Flexion
Flexion is performed by asking the patient to raise the arm straight up in front of them as high as the patient can with the thumb pointing upwards. The flexion angle is formed by aligning the goniometer with the lateral epicondyle of the humerus, the middle of the glenoid fossa, and a vertical line in the coronal plane (Figure 5A).
Isolated Abduction
Abduction is performed by asking the patient to raise the arm at the side as high as they can with the examiner stabilizing the scapula by holding it down. The abduction angle is formed by aligning the goniometer with the lateral epicondyle of the humerus, the middle of the posterior glenohumeral joint line, and a vertical line in the sagittal plane (Figure 5B).
External Rotation at 0 Degrees (in neutral)
This is performed with the patient in 0 degrees of glenohumeral joint abduction, 90 degrees of elbow flexion, and neutral supination/pronation forearm position. The patient is then asked to keep his elbow to his/ her waist and rotate the arm outwards. The external rotation angle is formed by aligning the goniometer with the ulna styloid process, the olecranon process of the ulna, and a horizontal line in the transverse plane (Figure 5C).
External/ Internal Rotation at 90 Degrees (in abduction)
The patient is in 90 degrees of glenohumeral abduction, 90 degrees of elbow flexion, and neutral supination/pronation of forearm. The patient is then asked to keep the elbow at 90 degrees and move the forearm upwards as high as they can and then downwards as low as they can. The external rotation and internal rotation angles in 90 degrees of abduction are formed by aligning the goniometer with the ulnar styloid process, the olecranon process of the ulna, and a horizontal line in the horizontal plane (Figure 5D).
Highest Posterior Anatomy Reached with Thumb
The patient is asked to reach his back with the dorsum (back) of his/ her thumb. The patient is then asked to reach as high as they can along the spine. The highest level that the patient can reach is marked. The bony landmarks adapted from Malanga et al. 19 are the inferior border of the scapula that corresponds to the T7 level and the top of the iliac crests that corresponds to the L4 level. Follow up the spinous processes from L4 to mark the L1 level. The highest point is noted as follows: above T7; between T7 and above L1; between L1 and above L4; L4 and below; and to the body (if the patient cannot reach their back).
Figure 5. Range of motion testing for rotator cuff tear
Footnote: A) Forward flexion; B) Isolated abduction; C) External rotation in neutral; D) External rotation in abduction
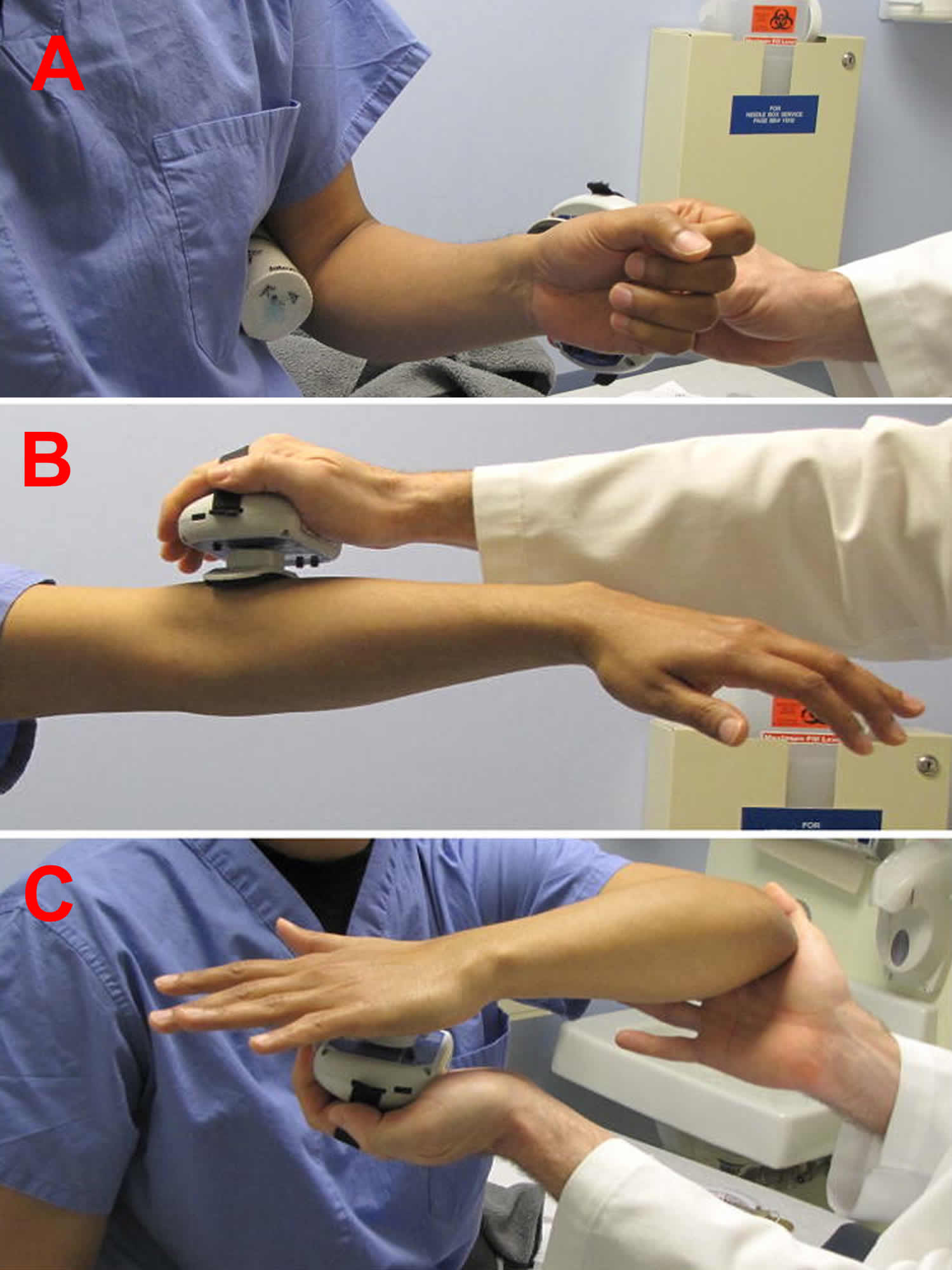
[Source 20]Strength Testing
Strength testing is performed using a portable hand-held dynamometer. Numerous devices are commercially available for this purpose and measure strength in kilograms or pounds. After positioning the shoulder for each of the maneuvers (described below), the patient is told, “This part of the test requires me to match your resistance. Now, please to push into the dynamometer as hard as you can.” Once the examiner feels that they have matched the subject’s resistance so that the muscle contraction is truly isometric the patient is asked to continue pushing into the dynamometer, while the tester resists the force exerted by the subject, maintaining positional equilibrium throughout the 5 second period of exertion. The examiner lets them know when the 5 seconds time is up. The examiner disregards the muscle performance measurement if it is determined that the patient in appropriately used other musculature to complete the desired task. All maneuvers are performed twice on each arm with a 10 second rest between repetitions. The scores are then averaged for each arm and evaluated for symmetry. The protocol below is modified from prior studies9 and our experience.
External Rotation (measures force predominately exerted by infraspinatus muscle)
The patient is instructed to sit with their arm in neutral rotation while holding their elbow and forearm at 90 degrees of flexion. The forearm is in midrange of motion between supinatation and pronation with the thumb directed upward. The tester places the dynamometer on the lateral surface of the distal forearm just proximal to the ulnar styloid process (Figure 6A).
Abduction (measures force predominately exerted by supraspinatus muscles)
The patient sits with both shoulders in approximately 90 degrees abduction and approximately 45 degrees of horizontal abduction (elbows are fully extended with palms facing down). The tester places dynamometers on each distal arm at the lateral humeral epicondyle (Figure 6B).
Internal Rotation (measures force predominately exerted by subscapularis muscle)
The subject sits with their arm at approximately 90 degrees of forward flexion and their elbow at 90 degrees of flexion. The tester places the dynamometer under the subject’s hand. The tester places one finger tip of the hand not holding the dynamometer on the subject’s olecranon process to ensure the patient is producing an internal rotation moment and not an adduction moment (Figure 6C).
Figure 6. Strength testing for rotator cuff tear
Footnote: Strength testing using a dynamometer. A) External rotation; B) Abduction; C) Internal rotation
[Source 20]Rotator cuff tear treatment
If you have a rotator cuff tear and you keep using it despite increasing pain, you may cause further damage. A rotator cuff tear can get larger over time.
Chronic shoulder and arm pain are good reasons to see your doctor. Early treatment can prevent your symptoms from getting worse. It will also get you back to your normal routine that much quicker.
The goal of any treatment is to reduce pain and restore function. There are several treatment options for a rotator cuff tear, and the best option is different for every person. In planning your treatment, your doctor will consider your age, activity level, general health, and the type of tear you have.
There is no evidence of better results from surgery performed near the time of injury versus later on. For this reason, many doctors first recommend management of rotator cuff tears with physical therapy and other nonsurgical treatments.
Nonsurgical Treatment
In about 80% of patients, nonsurgical treatment relieves pain and improves function in the shoulder.
Nonsurgical treatment options may include:
- Rest. Your doctor may suggest rest and limiting overhead activities. He or she may also prescribe a sling to help protect your shoulder and keep it still.
- Activity modification. Avoid activities that cause shoulder pain.
- Nonsteroidal anti-inflammatory medication. Drugs like ibuprofen and naproxen reduce pain and swelling.
- Strengthening exercises and physical therapy. Specific exercises will restore movement and strengthen your shoulder. Your exercise program will include stretches to improve flexibility and range of motion. Strengthening the muscles that support your shoulder can relieve pain and prevent further injury.
- Steroid injection. If rest, medications, and physical therapy do not relieve your pain, an injection of a local anesthetic and a cortisone preparation may be helpful. Cortisone is a very effective anti-inflammatory medicine; however, it is not effective for all patients.
The chief advantage of nonsurgical treatment is that it avoids the major risks of surgery, such as:
- Infection
- Permanent stiffness
- Anesthesia complications
- Sometimes lengthy recovery time
The disadvantages of nonsurgical treatment are:
- Size of tear may increase over time
- Activities may need to be limited
Rotator cuff tear exercises
Rehabilitation plays a critical role in both the nonsurgical and surgical treatment of a rotator cuff tear.
When a tear occurs, there is frequently atrophy of the muscles around the arm and loss of motion of the shoulder. An exercise or physical therapy program is necessary to regain strength and improve function in the shoulder.
Even though surgery repairs the defect in the tendon, the muscles around the arm remain weak, and a strong effort at rehabilitation is necessary for the procedure to succeed. Complete rehabilitation after surgery may take several months.
Your orthopaedic surgeon can prescribe an appropriate program based on your needs and the findings at surgery.
Rotator cuff tear surgery
Rotator cuff surgery is recommended if you have persistent pain or weakness in your shoulder that does not improve with nonsurgical treatment. Frequently, patients who require surgery will report pain at night and difficulty using the arm for lifting and reaching. Many will report ongoing symptoms despite several months of medication and limited use of the arm.
Other signs that surgery may be a good option for you include:
- Your symptoms have lasted 6 to 12 months
- You have a large tear (more than 3 cm) and the quality of the surrounding tissue is good
- You have significant weakness and loss of function in your shoulder
- Your tear was caused by a recent, acute injury
Surgery is also indicated in active individuals who use the arm for overhead work or sports. Pitchers, swimmers, and tennis players are common examples.
The type of rotator cuff tear surgical repair performed is based on the findings at surgery. A partial tear may require only a trimming or smoothing procedure called a débridement. A full-thickness tear within the substance of the tendon can be repaired side to side. If the tendon is torn from its insertion on the humerus (the most common injury), it is repaired directly to bone.
Surgery to repair a torn rotator cuff most often involves re-attaching the tendon to the head of humerus (upper arm bone). Three techniques are used for rotator cuff repair: traditional open repair, mini-open repair, and arthroscopic repair.
Your orthopaedic surgeon can recommend which technique is best to meet your individual health needs.
Rotator Cuff Tears: Surgical Treatment Options
Surgery to repair a torn rotator cuff most often involves re-attaching the tendon to the head of humerus (upper arm bone). A partial tear, however, may need only a trimming or smoothing procedure called a debridement. A complete tear is repaired by stitching the tendon back to its original site on the humerus.
The type of repair performed depends on several factors, including your surgeon’s experience and familiarity with a particular procedure, the size of your tear, your anatomy, and the quality of the tendon tissue and bone.
Many surgical repairs can be done on an outpatient basis and do not require you to stay overnight in the hospital. Your orthopaedic surgeon will discuss with you the best procedure to meet your individual health needs.
You may have other shoulder problems in addition to a rotator cuff tear, such as biceps tendon tears, osteoarthritis, bone spurs, or other soft tissue tears. During the operation, your surgeon may be able to take care of these problems, as well.
The three techniques most commonly used for rotator cuff repair include traditional open repair, arthroscopic repair, and mini-open repair. In the end, patients rate all three repair methods the same for pain relief, strength improvement, and overall satisfaction.
Open Repair
A traditional open surgical incision (several centimeters long) is often required if the tear is large or complex. The surgeon makes the incision over the shoulder and detaches one of the shoulder muscles (deltoid) to better see and gain access to the torn tendon.
During an open repair, the surgeon typically removes bone spurs from the underside of the acromion (this procedure is called an acromioplasty). An open repair may be a good option if the tear is large or complex or if additional reconstruction, such as a tendon transfer, is indicated.
Open repair was the first technique used for torn rotator cuffs. Over the years, new technology and improved surgeon experience has led to less invasive procedures.
All-Arthroscopic Repair
During arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your shoulder joint. The camera displays pictures on a television screen, and your surgeon uses these images to guide miniature surgical instruments.
Because the arthroscope and surgical instruments are thin, your surgeon can use very small incisions (cuts), rather than the larger incision needed for standard, open surgery.
All-arthroscopic repair is usually an outpatient procedure and is the least invasive method to repair a torn rotator cuff.
Mini-Open Repair
The mini-open repair uses newer technology and instruments to perform a repair through a small incision. The incision is typically 3 to 5 cm long.
This technique uses arthroscopy to assess and treat damage to other structures within the joint. Bone spurs, for example, are often removed arthroscopically. This avoids the need to detach the deltoid muscle.
Once the arthroscopic portion of the procedure is completed, the surgeon repairs the rotator cuff through the mini-open incision. During the tendon repair, the surgeon views the shoulder structures directly, rather than through the video monitor.
Rotator cuff tear surgery complications
After rotator cuff surgery, a small percentage of patients experience complications. In addition to the risks of surgery in general, such as blood loss or problems related to anesthesia, complications of rotator cuff surgery may include:
- Nerve injury. This typically involves the nerve that activates your shoulder muscle (deltoid).
- Infection. Patients are given antibiotics during the procedure to lessen the risk for infection. If an infection develops, an additional surgery or prolonged antibiotic treatment may be needed.
- Deltoid detachment. During an open repair, this shoulder muscle is detached to provide better access to the rotator cuff. It is stitched back into place at the end of the procedure. It is very important to protect this area after surgery and during rehabilitation to allow it to heal.
- Stiffness. Early rehabilitation lessens the likelihood of permanent stiffness or loss of motion. Most of the time, stiffness will improve with more aggressive therapy and exercise.
- Tendon re-tear. There is a chance for re-tear following all types of repairs. The larger the tear, the higher the risk of re-tear. Patients who re-tear their tendons usually do not have greater pain or decreased shoulder function. Repeat surgery is needed only if there is severe pain or loss of function.
Post rotator cuff tear surgery recovery
Pain Management
After surgery, you will feel pain. This is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery faster.
Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery, they are a narcotic and can be addictive. Opioid dependency and overdose has become a critical public health issue. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids. Talk to your doctor if your pain has not begun to improve within a few weeks after your surgery.
Rehabilitation
Rehabilitation plays a vital role in getting you back to your daily activities. A physical therapy program will help you regain shoulder strength and motion.
- Immobilization. After surgery, therapy progresses in stages. At first, the repair needs to be protected while the tendon heals. To keep your arm from moving, you will most likely use a sling and avoid using your arm for the first 4 to 6 weeks. How long you require a sling depends upon the severity of your injury.
- Passive exercise. Even though your tear has been repaired, the muscles around your arm remain weak. Once your surgeon decides it is safe for you to move your arm and shoulder, a therapist will help you with passive exercises to improve range of motion in your shoulder. With passive exercise, your therapist supports your arm and moves it in different positions. In most cases, passive exercise is begun within the first 4 to 6 weeks after surgery.
- Active exercise. After 4 to 6 weeks, you will progress to doing active exercises without the help of your therapist. Moving your muscles on your own will gradually increase your strength and improve your arm control. At 8 to 12 weeks, your therapist will start you on a strengthening exercise program.
Expect a complete recovery to take several months. Most patients have a functional range of motion and adequate strength by 4 to 6 months after surgery. Although it is a slow process, your commitment to rehabilitation is key to a successful outcome.
Post rotator cuff tear surgery outcome
The majority of patients report improved shoulder strength and less pain after surgery for a torn rotator cuff.
Each surgical repair technique (open, mini-open, and arthroscopic) has similar results in terms of pain relief, improvement in strength and function, and patient satisfaction. Surgeon expertise is more important in achieving satisfactory results than the choice of technique.
Factors that can decrease the likelihood of a satisfactory result include:
- Poor tendon/tissue quality
- Large or massive tears
- Poor patient compliance with rehabilitation and restrictions after surgery
- Patient age (older than 65 years)
- Smoking and use of other nicotine products
- Workers’ compensation claims
- American Academy of Orthopaedic Surgeons. Optimizing the management of rotator cuff problems: guideline and evidence report. https://www.aaos.org/research/guidelines/RCP_guideline.pdf[↩]
- Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Am. 2010;92(3):542–549.[↩]
- Petersen SA, Murphy TP. The timing of rotator cuff repair for the restoration of function. J Shoulder Elbow Surg. 2011;20(1):62–68.[↩]
- Imaging of shoulder injuries in sports medicine: current protocols and concepts. Parker BJ, Zlatkin MB, Newman JS, Rathur SK. Clin Sports Med. 2008 Oct; 27(4):579-606.[↩]
- Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77(1):10–15.[↩]
- Roy JS, Braën C, Leblond J, et al. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. Br J Sports Med. 2015;49(20):1316–1328.[↩]
- Jain NB, Yamaguchi K. History and physical examination provide little guidance on diagnosis of rotator cuff tears. Evidence-based medicine. 2014;19(3):108. doi:10.1136/eb-2013-101593. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4709248/[↩]
- Shoulder pain: diagnosis and management in primary care. Mitchell C, Adebajo A, Hay E, Carr A. BMJ. 2005 Nov 12; 331(7525):1124-8.[↩]
- Shoulder disorders in the elderly: a community survey. Chard MD, Hazleman R, Hazleman BL, King RH, Reiss BB. Arthritis Rheum. 1991 Jun; 34(6):766-9.[↩]
- Indications for rotator cuff repair: a systematic review. Oh LS, Wolf BR, Hall MP, Levy BA, Marx RG. Clin Orthop Relat Res. 2007 Feb; 455():52-63.[↩]
- National trends in rotator cuff repair. Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. J Bone Joint Surg Am. 2012 Feb 1; 94(3):227-33. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3262185/[↩]
- Persistent shoulder pain: epidemiology, pathophysiology, and diagnosis. Meislin RJ, Sperling JW, Stitik TP. Am J Orthop (Belle Mead NJ). 2005 Dec; 34(12 Suppl):5-9.[↩]
- History and Physical Examination for Identifying Rotator Cuff Tears. Am Fam Physician. 2017 Nov 1;96(9):online. https://www.aafp.org/afp/2017/1101/od2.html[↩][↩]
- Gerber C, Hersche O, Farron A. Isolated rupture of the subscapularis tendon. J Bone Joint Surg Am. 1996 Jul;78(7):1015–1023.[↩]
- Lag signs in the diagnosis of rotator cuff rupture. Hertel R, Ballmer FT, Lombert SM, Gerber C. J Shoulder Elbow Surg. 1996 Jul-Aug; 5(4):307-13.[↩][↩]
- Cameron BD, Williams GR, Jr, Iannotti JP. Disorders of the shoulder: diagnosis and management. 2. Vol. 1. Philadelphia: Lippincott Williams & Wilkins; 2007.[↩][↩]
- The belly-off sign: a new clinical diagnostic sign for subscapularis lesions. Scheibel M, Magosch P, Pritsch M, Lichtenberg S, Habermeyer P. Arthroscopy. 2005 Oct; 21(10):1229-35.[↩]
- The bear-hug test: a new and sensitive test for diagnosing a subscapularis tear. Barth JR, Burkhart SS, De Beer JF. Arthroscopy. 2006 Oct; 22(10):1076-84.[↩]
- Malanga GA, Nadler SF. Musculoskeletal physical examination: An evidence-based approach. Philadelphia: Elsevier Inc; 2006[↩]
- Jain NB, Wilcox R, Katz JN, Higgins LD. Clinical Examination of the Rotator Cuff. PM & R : the journal of injury, function, and rehabilitation. 2013;5(1):10.1016/j.pmrj.2012.08.019. doi:10.1016/j.pmrj.2012.08.019. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3826176/[↩][↩]