Contents
What is Naegleria fowleri
Naegleria fowleri commonly referred to as the “brain-eating amoeba” or “brain-eating ameba”, is a free-living freshwater thermophilic ameba (single-celled living organism). Eight different types of the Naegleria fowleri pathogen show an uneven distribution throughout the world; 3 of those types have been identified within the United States 1. Naegleria fowleri ameba can cause a rare and almost always fatal infection of the brain called primary amebic meningoencephalitis (PAM) 2. Naegleria fowleri ameba is commonly found in warm freshwater (e.g. freshwater lakes, rivers, ponds and hot springs) and soil. Naegleria fowleri usually infects people when contaminated water enters the body through the nose. Once the ameba enters the nose, it travels through the nasal mucosa along the olfactory nerves, across the cribriform plate, and enters the brain where it causes PAM (primary amebic meningoencephalitis), which is usually fatal 3. Naegleria fowleri infection typically occurs when people go swimming or diving in warm freshwater places, like freshwater lakes, hot springs, ponds and rivers. In very rare instances, Naegleria infections may also occur when contaminated water from other sources (such as inadequately chlorinated swimming pool water and/or spas or heated and contaminated tap water) enters the nose 4. You cannot get infected from swallowing water contaminated with Naegleria fowleri.
Only a tiny percentage of the millions of people who are exposed to Naegleria fowleri ever get sick from it. Why some people become infected after exposure and others don’t isn’t known.
Naegleria infection causes a disease called primary amebic meningoencephalitis (PAM). This disease causes brain inflammation and destruction of brain tissue.
In the United States, millions of people are exposed to the Naegleria fowleri amoeba that causes primary amebic meningoencephalitis (PAM) infection each year, but few people get sick from it. From 2007 to 2017, 40 infections were reported.
Some factors that might increase your risk of naegleria infection include:
- Freshwater swimming. Most people who become ill have been swimming in a freshwater lake within the previous two weeks.
- Heat waves. The amoeba thrives in warm or hot water.
- Age. Children and young adults are the most likely age groups to be affected, possibly because they’re likely to stay in the water longer and are more active in the water.
Generally beginning within two to 15 days of exposure to the amoeba, signs and symptoms of Naegleria fowleri infection may include:
- A change in the sense of smell or taste
- Fever
- Sudden, severe headache
- Stiff neck
- Sensitivity to light
- Nausea and vomiting
- Confusion
- Loss of balance
- Sleepiness
- Seizures
- Hallucinations
Patients commonly experience fever, headache, nausea, vomiting, stiff neck, and, occasionally seizures. Naegleria fowleri and its associated inflammatory reaction, including the release of cytotoxic molecules, cause extensive tissue damage and necrosis 5. The sequelae include acute necrotizing meningoencephalitis and usually result in death in 7 to 10 days 2. Other flagellates found in the environment include several species of Acanthamoeba and Balamuthia mandrillaris, both of which can cause granulomatous amoebic encephalitis. It is important to consider these entities when evaluating Primary amoebic meningoencephalitis.
- These signs and symptoms can progress rapidly. They typically lead to death within a week.
Few people survive naegleria infection, even with treatment. Early diagnosis and treatment are crucial for survival.
The primary treatment for naegleria infection is an antifungal drug, amphotericin B — usually injected into a vein (intravenously) or into the space around your spinal cord to kill the amoebas.
An investigational drug called miltefosine (Impavido) is now available for emergency treatment of Naegleria fowleri infection. The medicine, when taken with other medications and along with aggressive management of brain swelling, may show promise for improved survival.
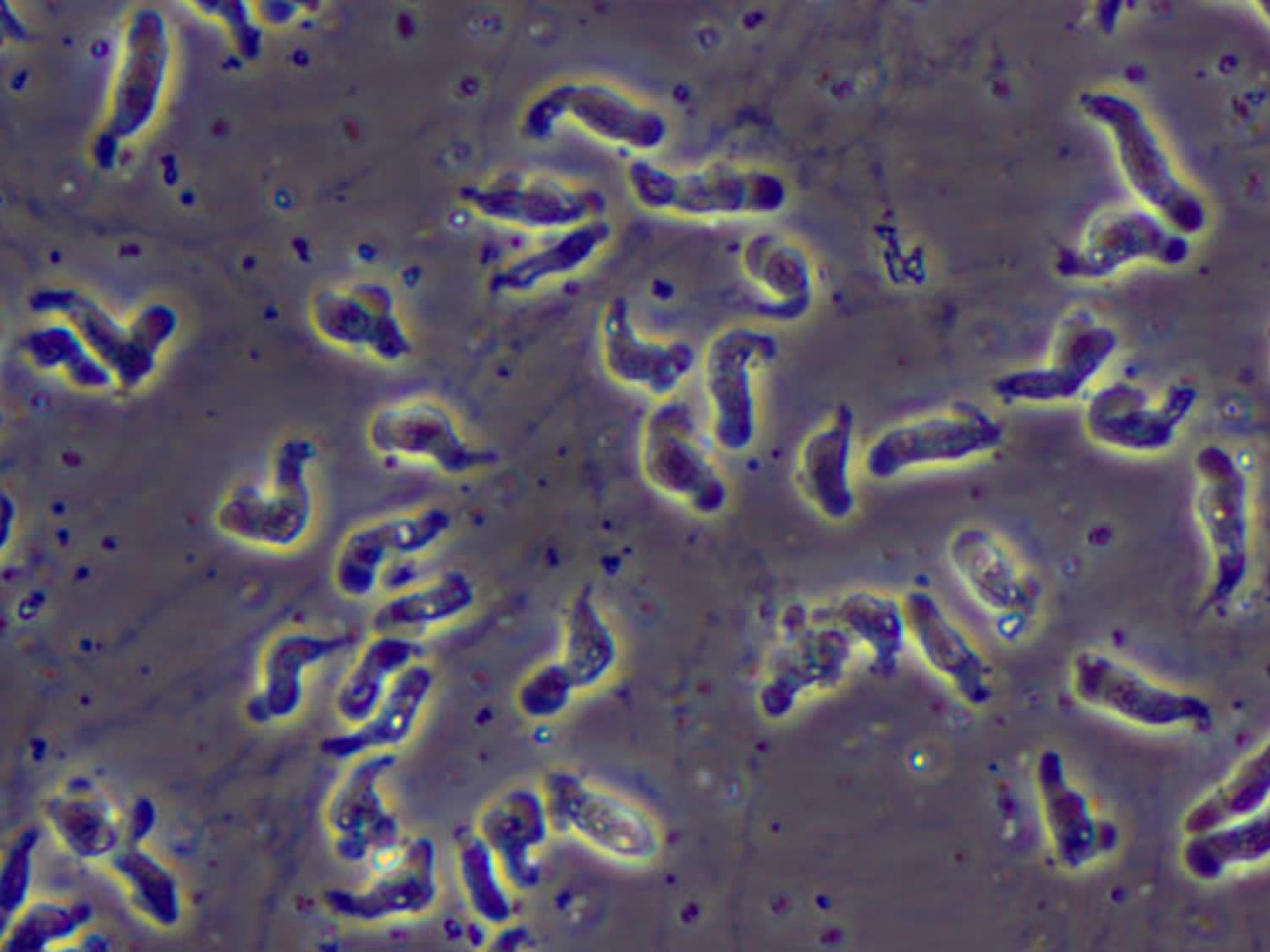
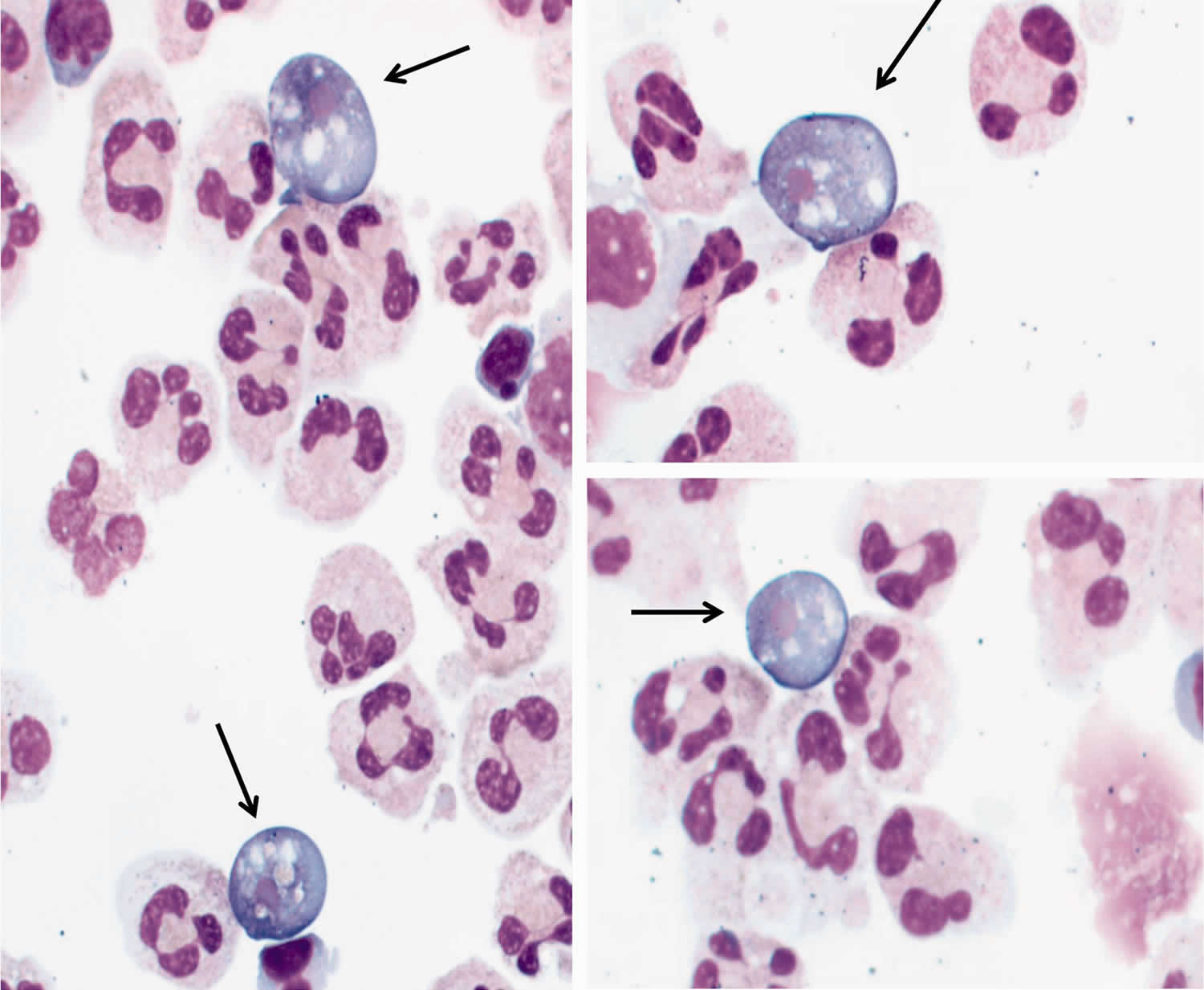
Figure 1. Naegleria fowleri ameba
Footnote: Specimen from a 12-year-old Caucasian girl. Naegleria fowleri on Wright-Giemsa stained cerebrospinal fluid (CSF) cytospin slides (original magnification, ×1000; oil immersion). Arrows indicate Naegleria organisms.
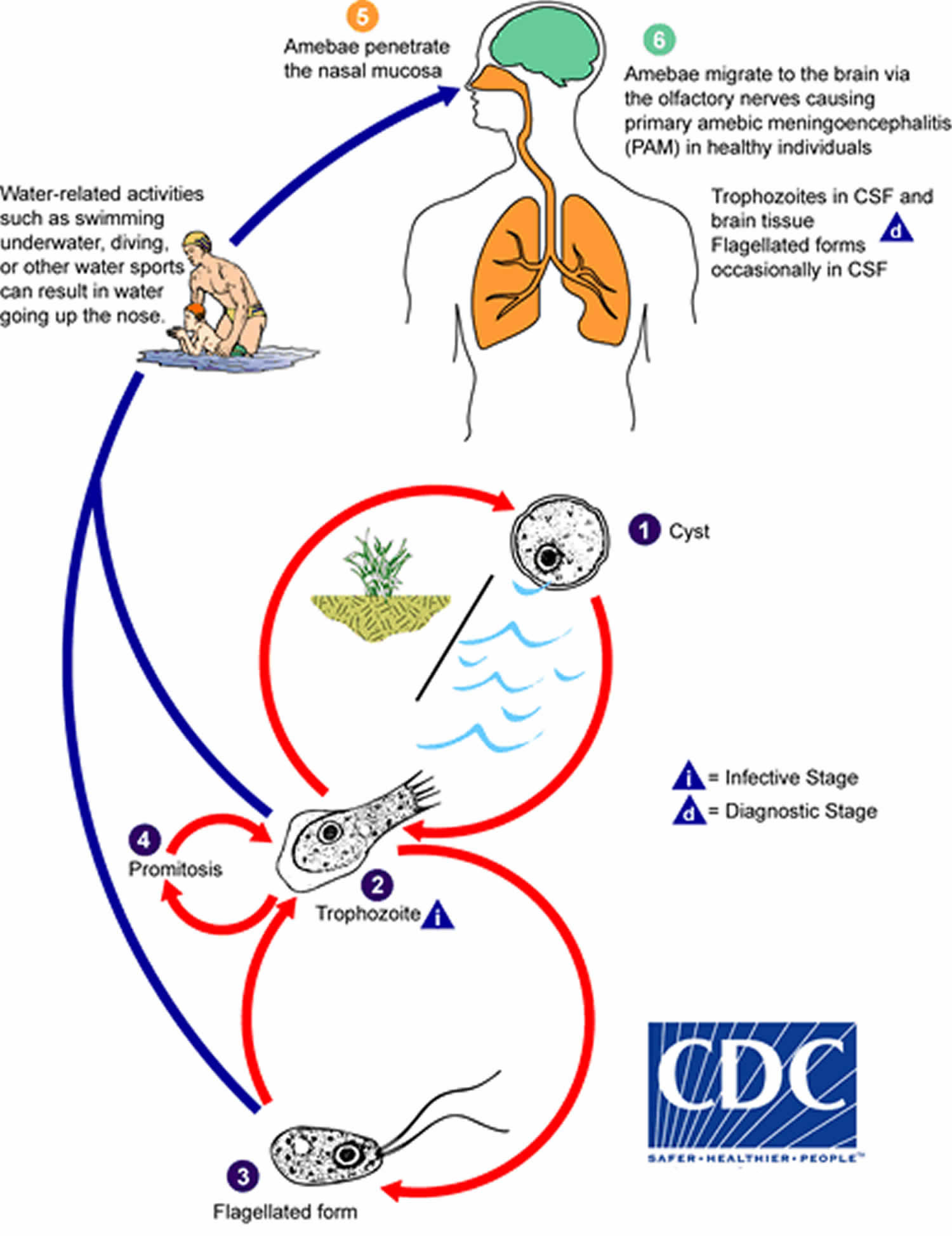
[Source 2]Naegleria fowleri life cycle
Naegleria fowleri produces an acute, and usually lethal, central nervous system (CNS) disease called primary amebic meningoencephalitis (PAM).
Naegleria fowleri has three stages in its life cycle: cysts (1), trophozoites (2), and flagellated forms (3). The trophozoites replicate by promitosis (nuclear membrane remains intact) (4). Naegleria fowleri is found in fresh water, soil, thermal discharges of power plants, geothermal wells, and poorly-chlorinated swimming pools. Trophozoites can turn into temporary non-feeding flagellated forms which usually revert back to the trophozoite stage. Trophozoites infect humans or animals by penetrating the nasal mucosa (5) and migrating to the brain (6) via the olfactory nerves causing primary amebic meningoencephalitis (PAM). Naegleria fowleri trophozoites are found in cerebrospinal fluid (CSF) and tissue, while flagellated forms are occasionally found in CSF. Cysts are not seen in brain tissue.
Figure 2. Naegleria fowleri life cycle
Naegleria fowleri prevention
The Centers for Disease Control and Prevention (CDC) suggests that the following measures may reduce your risk of Naegleria fowleri infection. The only certain way to prevent a Naegleria fowleri infection due to swimming is to refrain from water-related activities in warm freshwater. Personal actions to reduce the risk of Naegleria fowleri infection should focus on limiting the amount of water going up the nose.
- Hold your nose shut, use nose clips, or keep your head above water when taking part in water-related activities in bodies of warm freshwater.
- Avoid putting your head under the water in hot springs and other untreated thermal waters.
- Avoid water-related activities in warm freshwater during periods of high water temperature.
- Avoid digging in, or stirring up, the sediment while taking part in water-related activities in shallow, warm freshwater areas.
- Don’t swim in or jump into warm freshwater lakes and rivers.
These recommendations make common sense but are not based on any scientific testing since the low numbers of infections make it difficult to ever show that they are effective.
Naegleria fowleri infects people when water containing the ameba enters the body through the nose. Infection is rare and typically occurs when people go swimming or diving in warm freshwater places, like lakes and rivers. Very rarely, infections have been reported when people submerge their heads, cleanse their noses during religious practices, or irrigate their sinuses (nose) using contaminated tap or faucet water. Naegleria fowleri can grow in pipes, hot water heaters, and water systems, including treated public drinking water systems. You cannot get infected from drinking water contaminated with Naegleria. You can only be infected when contaminated water goes up into your nose.
Risk of Infection
Naegleria fowleri is found naturally in freshwater lakes, rivers, and hot springs in the United States 6, particularly in southern-tier states 7, but has recently caused infections as far north as Minnesota 8. No data exist to accurately estimate the true risk of primary amoebic meningoencephalitis (PAM). Hundreds of millions of visits to swimming venues occur each year in the U.S. 9 that result in 0-8 infections per year 10. It is unknown why certain persons become infected with the Naegleria fowleri amebae while millions of others exposed to warm recreational fresh waters do not, including those who were swimming with people who became infected. Attempts have been made to determine what concentration of Naegleria fowleri in the environment poses an unacceptable risk 11. However, no method currently exists that accurately and reproducibly measures the numbers of amebae in the water. This makes it unclear how a standard might be set to protect human health and how public health officials would measure and enforce such a standard. However, the risk of Naegleria fowleri infection is very low. There have been 34 reported infections in the U.S. in the 10 years from 2008 to 2017, despite hundreds of millions of recreational water exposures each year 9. By comparison, in the ten years from 2001 to 2010, there were more than 34,000 drowning deaths in the United States.
Naegleria fowleri symptoms
Primary amebic meningoencephalitis (PAM), is a disease of the central nervous system 6. Primary amebic meningoencephalitis (PAM) is caused by Naegleria fowleri, a free-living ameba. It is a rare disease that is almost always fatal 10; only 4 people in the U.S. out of 143 have survived infection from 1962 to 2017 12.
Signs and symptoms of Naegleria fowleri infection are clinically similar to bacterial meningitis, which lowers the chances of initially diagnosing primary amoebic meningoencephalitis (PAM) 12. Humans become infected when water containing Naegleria fowleri enters the nose and the ameba migrates to the brain along the olfactory nerve 10. People do not become infected from drinking contaminated water. Symptoms start 1-9 days (median 5 days) after swimming or other nasal exposure to Naegleria-containing water. People die 1-18 days (median 5 days) after symptoms begin 12. Primary amebic meningoencephalitis (PAM) is difficult to detect because the disease progresses rapidly so that diagnosis is usually made after death 6. Signs and symptoms of the infection include:
Stage 1
- Severe frontal headache
- Fever
- Nausea
- Vomiting
Stage 2
- Stiff neck
- Seizures
- Altered mental status
- Hallucinations
- Coma
The disease is generally fatal 10; among well-documented cases, there are only five known survivors in North America: one from the U.S. in 1978 13, one from Mexico in 2003 14, two from the U.S. in 2013 15, 16, and one from the U.S. in 2016 2. The original U.S. survivor’s condition gradually improved during a one-month hospitalization. The only reported side effect to treatment was a reduction in leg sensation for two months after discharge, which gradually improved. There was also no detection of Naegleria fowleri 3 days post-treatment 13. It has been suggested that the original survivor’s strain of Naegleria fowleri may have been less virulent, which contributed to the patient’s recovery. In laboratory experiments, the California survivor’s strain did not cause damage to cells as quickly as other strains, suggesting that it is less virulent than strains recovered from other fatal cases 17.
The Mexico survivor’s condition did not begin to improve until 40 hours after hospital admission. On day 22 of admission, there was no abnormality shown in the brain scan and the patient was discharged the next day. The patient was followed up for the next 12 months without any recurrence of disease 14.
After 35 years without a Naegleria fowleri survivor in the United States, during the summer of 2013, two children with Naegleria fowleri infection survived. The first, a 12-year-old girl, was diagnosed with primary amoebic meningoencephalitis (PAM) approximately 30 hours after becoming ill and was started on the recommended treatment within 36 hours. She also received the investigational drug miltefosine 2 and her brain swelling was aggressively managed with treatments that included cooling the body below normal body temperature (therapeutic hypothermia). This patient made a full neurologic recovery and returned to school. Her recovery has been attributed to early diagnosis and treatment and novel therapeutics including miltefosine and hypothermia 15.
The second child, an 8-year-old male, is also considered a primary amoebic meningoencephalitis (PAM) survivor, although he has suffered what is likely to be permanent brain damage 16. He was also treated with miltefosine but was diagnosed and treated several days after his symptoms began. Cooling of the body below normal body temperature was not used 16.
In the summer of 2016, a 16-year-old boy was reported as the 4th U.S. PAM survivor. This patient was diagnosed within hours of presentation to the hospital and was treated with the same protocol used for the 12-year-old 2013 survivor. This patient also made a full neurologic recovery and returned to school.
Overall, the outlook for people who get this disease is poor, although early diagnosis and new treatments might increase the chances for survival.
Naegleria fowleri diagnosis
Imaging tests
Computerized tomography (CT) or magnetic resonance imaging (MRI) can reveal swelling and bleeding within the brain.
- CT scan. This procedure combines X-ray views taken from many different directions into detailed cross-sectional images.
- MRI. An MRI machine uses radio waves and a strong magnetic field to produce extremely detailed images of soft tissues, such as the brain.
Spinal tap (lumbar puncture)
Naegleria amoeba can be seen under a microscope in the fluid that surrounds your brain and spinal cord. The spinal fluid is obtained by inserting a needle between two vertebrae in your lower back. This test also can measure the cerebral spinal fluid pressure and look for inflammatory cells.
Laboratory Diagnosis
The diagnosis of Naegleria fowleri infection can be made most quickly by microscopic examination of fresh, unfrozen, unrefrigerated cerebrospinal fluid (CSF) (NOTE: samples cannot be frozen or refrigerated because cold temperatures kill the Naegleria fowleri amebae).
A wet mount may detect motile trophozoites, and a Giemsa-stained smear will show trophozoites with typical morphology. In Acanthamoeba infections, the diagnosis can be made from microscopic examination of stained smears of biopsy specimens (brain tissue, skin, cornea) or of corneal scrapings, which may detect trophozoites and cysts. Confocal microscopy or cultivation of the causal organism, and its identification by direct immunofluorescent antibody, may also prove useful. An increasing number of PCR-based techniques (conventional and real-time PCR) have been described for detection and identification of free-living amebic infections in the clinical samples listed above. Such techniques may be available in selected reference diagnostic laboratories.
Real-Time PCR
A real-time PCR was developed at the Centers for Disease Control and Prevention (CDC) for identification of Acanthamoeba spp., Naegleria fowleri, and Balamuthia mandrillaris in clinical samples 18. This assay uses distinct primers and TaqMan probes for the simultaneous identification of these three parasites.
Naegleria fowleri treatment
Although most cases of primary amebic meningoencephalitis (PAM) caused by Naegleria fowleri infection in the United States have been fatal (139/143 in the U.S.) 10, there have been five well-documented survivors in North America: one in the U.S. in 1978 19, one in Mexico in 2003 14, two additional survivors from the U.S. in 2013 15, 16 and one from the U.S. in 2016 2. It has been suggested that the original U.S. survivor’s strain of Naegleria fowleri was less virulent, which contributed to the patient’s recovery. In laboratory experiments, the original U.S. survivor’s strain did not cause damage to cells as rapidly as other strains, suggesting that it is less virulent than strains recovered from other fatal infections 17.
Recently an investigational breast cancer and anti-leishmania drug, miltefosine 20, has shown some promise in combination with some of these other drugs. Miltefosine has shown ameba-killing activity against free-living amebae, including Naegleria fowleri, in the laboratory 21. Miltefosine has also been used to successfully treat patients infected with Balamuthia 22 and disseminated Acanthamoeba infection 23. If you are a clinician and have a patient with suspected Naegleria fowleri or other free-living ameba infection, please contact the CDC Emergency Operations Center at 770-488-7100 to consult with a CDC expert regarding the use of this drug. Miltefosine is now commercially available. Please visit impavido.com (http://www.impavido.com/) for more information on obtaining miltefosine in the United States. If you have a patient with suspected free-living ameba infection, please contact the CDC Emergency Operations Center at 770-488-7100 to consult with a CDC expert regarding the use of this drug.
After 35 years without a Naegleria fowleri survivor in the United States, during the summer of 2013, two children with Naegleria fowleri infection survived. The first, a 12-year-old girl, was diagnosed with primary amoebic meningoencephalitis (PAM) approximately 30 hours after becoming ill and was started on the recommended treatment within 36 hours. She also received the investigational drug miltefosine 2 and her brain swelling was aggressively managed with treatments that included cooling the body below normal body temperature (therapeutic hypothermia). This patient made a full neurologic recovery and returned to school. Her recovery has been attributed to early diagnosis and treatment and novel therapeutics including miltefosine and hypothermia 15.
The second child, an 8-year-old male, is also considered a primary amoebic meningoencephalitis (PAM) survivor, although he has suffered what is likely to be permanent brain damage 16. He was also treated with miltefosine but was diagnosed and treated several days after his symptoms began. Cooling of the body below normal body temperature was not used 16.
In the summer of 2016, a 16-year-old boy was reported as the 4th U.S. PAM survivor. This patient was diagnosed within hours of presentation to the hospital and was treated with the same protocol used for the 12-year-old 2013 survivor. This patient also made a full neurologic recovery and returned to school.
- De Jonckheere JF.What do we know by now about the genus Naegleria? Exp Parasitol . 2014;145(Suppl):S2–S9.[↩]
- Andrew L. Dunn, Tameika Reed, Charlotte Stewart, Rebecca A. Levy; Naegleria fowleri That Induces Primary Amoebic Meningoencephalitis: Rapid Diagnosis and Rare Case of Survival in a 12-Year-Old Caucasian Girl, Laboratory Medicine, Volume 47, Issue 2, 1 May 2016, Pages 149–154, https://doi.org/10.1093/labmed/lmw008[↩][↩][↩][↩][↩][↩][↩]
- Marciano-Cabral F, Cabral GA. The immune response to Naegleria fowleri amebae and pathogenesis of infection. FEMS Immunol Med Microbiol. 2007;51:243–259.[↩]
- Yoder JS, Eddy BA, Visvesvara GS, Capewell L, Beach MJ. The epidemiology of primary amoebic meningoencephalitis in the USA, 1962-2008. Epidemiol Infect. 2010;138(7):968-75. https://www.ncbi.nlm.nih.gov/pubmed/19845995[↩]
- Grace E, Asbill S, Virga K. Naegleria fowleri: pathogenesis, diagnosis, and treatment options. Antimicrob Agents Chemother . 2015;59(11):6677–6681.[↩]
- Visvesvara GS. Free-living amebae as opportunistic agents of human disease. J Neuroparasitol. 2010;1. https://www.researchgate.net/profile/Govinda_Visvesvara/publication/47554562_Free-Living_Amebae_as_Opportunistic_Agents_of_Human_Disease/links/0deec515c2fe23e45b000000/Free-Living-Amebae-as-Opportunistic-Agents-of-Human-Disease.pdf?origin=publication_detail[↩][↩][↩]
- Maclean RC, Richardson DJ, LePardo R, Marciano-Cabral F. The identification of Naegleria fowleri from water and soil samples by nested PCR. Parasitol Res. 2004;93: 211–17. https://link.springer.com/article/10.1007%2Fs00436-004-1104-x[↩]
- Kemble SK, Lynfield R, DeVries AS, Drehner DM, Pomputius WF 3rd, Beach MJ, Visvesvara GS, da Silva AJ, Hill VR, Yoder JS, Xiao L, Smith KE, Danila R. Fatal Naegleria fowleri infection acquired in Minnesota: possible expanded range of a deadly thermophilic organism. Clin Infect Dis. 2012;54:805-9. cid.oxfordjournals.org/content/54/6/805.full.pdf+html[↩]
- US Census Bureau. Statistical Abstract of the United States: 2012. Arts, Recreation, and Travel: Participation in Selected Sports Activities 2009-2012. www2.census.gov/library/publications/2011/compendia/statab/131ed/tables/12s1249.xls[↩][↩]
- Yoder JS, Eddy BA, Visvesvara GS, Capewell L, Beach MJ. The epidemiology of primary amoebic meningoencephalitis in the USA, 1962-2008. Epidemiol Infect. 2010;138:968-75. https://www.ncbi.nlm.nih.gov/pubmed/19845995[↩][↩][↩][↩][↩]
- Cabanes PA, Wallet F, Pringuez E, Pernin P. Assessing the risk of primary amoebic meningoencephalitis from swimming in the presence of environmental Naegleria fowleri. Appl Environ Microbiol. 2001;67:2927-31. https://aem.asm.org/content/67/7/2927.long[↩]
- Capewell LG, Harris AM, Yoder JS, Cope JR, Eddy BA, Roy SL, Visvesvara GS, Fox LM, Beach MJ. Diagnosis, clinical course, and treatment of primary amoebic meningoencephalitis in the United States, 1937–2013. J Pediatric Infect Dis Soc. 2014;Epub: 1–8. https://academic.oup.com/jpids/article/4/4/e68/2580118[↩][↩][↩]
- Seidel J, Harmatz P, Visvesvara GS, Cohen A, Edwards J, Turner J. Successful treatment of primary amebic meningoencephalitis. New Engl J Med. 1982;306:346-8. https://www.nejm.org/doi/full/10.1056/NEJM198202113060607[↩][↩]
- Vargas-Zepeda J, Gomez-Alcala AV, Vasquez-Morales JA, Licea-Amaya L, De Jonckheere JF, Lores-Villa F. Successful treatment of Naegleria PAM using IV amphotericin B, fluconazole, and rifampin. Arch Med Res. 2005;36:83-6. https://www.ncbi.nlm.nih.gov/pubmed/15900627[↩][↩][↩]
- Linam WM, Ahmed M, Cope JR, Chu C, Visvesvara GS, da Silva AJ, Qvarnstrom Y, Green J. Successful treatment of an adolescent with Naegleria fowleri primary amebic meningoencephalitis. Pediatrics. 2015;135:e744. http://pediatrics.aappublications.org/content/early/2015/02/04/peds.2014-2292[↩][↩][↩][↩]
- Cope JR, Conrad DA, Cohen N, Cotilla M, DaSilva A, Jackson J, Visvesvara GS. Use of the novel therapeutic agent miltefosine for the treatment of primary amebic meningoencephalitis: report of 1 fatal and 1 surviving case. Clin Infect Dis 2016;62(6):774-6. https://academic.oup.com/cid/article/62/6/774/2462791[↩][↩][↩][↩][↩][↩]
- John DT, John RA. Cytopathogenicity of Naegleria fowleri in mammalian cell cultures. Parasitol Res. 1989;76:20-5. https://www.ncbi.nlm.nih.gov/pubmed/2622894[↩][↩]
- Qvarnstrom Y, Visvesvara GS, Sriram R, da Silva AJ. Multiplex real-time PCR assay for simultaneous detection of Acanthamoeba spp., Balamuthia mandrillaris, and Naegleria fowleri. J Clin Microbiol 2006;44(10):3589-3595.[↩]
- Seidel JS, Harmatz P, Visvesvara GS, Cohen A, Edwards J, Turner J. Successful treatment of primary amebic meningoencephalitis. N Engl J Med. 1982;306:346-8. https://www.nejm.org/doi/full/10.1056/NEJM198202113060607[↩]
- Kaminsky R. Miltefosine Zentaris. Curr Opin Investig Drugs. 2002;3(4):550-4. https://www.ncbi.nlm.nih.gov/pubmed/12090722[↩]
- Kim JH, Jung SY, Lee YJ, Song KJ, Kwon D, Kim K, Park S, Im KI, Shin HJ. Effect of therapeutic chemical agents in vitro and on experimental meningoencephalitis due to Naegleria fowleri.[PDF – 7 pages] Antimicrob Agents Chemother. 2008;52:4010-16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2573150/pdf/0197-08.pdf[↩]
- Martínez DY, Seas C, Bravo F, Legua P, Ramos C, Cabello AM, Gotuzzo E. Successful treatment of Balamuthia mandrillaris amoebic infection with extensive neurological and cutaneous involvement. Clin Infect Dis. 2010;51:e7-11.[↩]
- Aichelburg AC, Walochnik J, Assadian O, Prosch H, Steuer A, Perneczky G, Visvesvara GS, Aspöck H, Vetter N. Successful treatment of disseminated Acanthamoeba sp. infection with miltefosine.[PDF – 4 pages] Emerg Infect Dis. 2008;14(11):1743-6.[↩]