Contents
What is ferrous gluconate
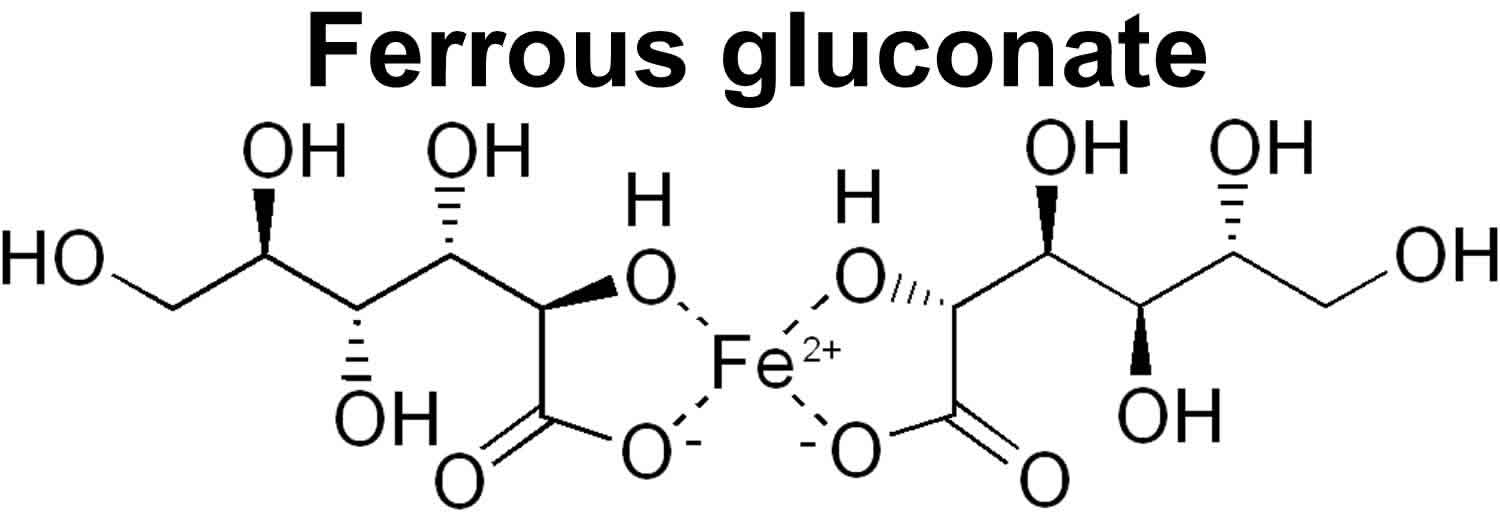
Ferrous gluconate is a form of mineral iron for oral administration, that is used to treat or prevent iron deficiency anemia (a lack of red blood cells caused by having too little iron in the body). Iron deficiency and related iron deficiency anemia are the most prevalent nutritional disorders worldwide 1. According to the World Health Organization (WHO), iron deficiency is the most common nutritional disorder affecting as much as 20% of the global population 2. Iron deficiency arises when the body’s iron requirements are not met by dietary iron. Ferrous gluconate is absorbed in the stomach and small intestine and combines with apoferritin to form ferritin, which is stored in the liver, spleen, red bone marrow, and intestinal mucosa. Iron (Fe) is important in transport of oxygen by hemoglobin to the tissues, iron is also found in myoglobin, transferrin, and ferritin, and is as a component of many enzymes such as catalase, peroxidase, and cytochromes. Hemoglobin carries oxygen through your blood to tissues and organs. Myoglobin helps your muscle cells store oxygen.
Iron is an essential mineral nutrient that has a key physiological role and is required for numerous functions such as oxygen transport, ATP production, and DNA replication. In normal healthy humans, the main source of iron loss is through shedding of skin and sloughed gastrointestinal mucosal cells 3. In males this accounts for approximately 1 mg/day, while it is higher in women due to menstruation-associated blood loss. Iron cannot be synthesized in the human body and is therefore acquired primarily from dietary sources. Assuming a normal human diet, 12–18 mg of iron is ingested daily, mostly in the ferric form (Fe3+) 4. Due to physiological as well as dietary factors, only 1–2 mg of this amount undergoes absorption through the gut enterocyte to become available to the systemic circulation 4.
Iron is found in the diet in two forms—heme iron, which is well absorbed, and nonheme iron, which is poorly absorbed. The best dietary source of absorbable (heme) iron is lean red meat. Chicken, turkey, and fish are also sources of iron, but they contain less than red meat. Cereals, beans, and some vegetables contain poorly absorbed (nonheme) iron. Foods rich in vitamin C (e.g., citrus fruits and fresh vegetables), eaten with small amounts of heme iron-containing foods, such as meat, may increase the amount of nonheme iron absorbed from cereals, beans, and other vegetables. Some foods (e.g., milk, eggs, spinach, fiber-containing, coffee, tea) may decrease the amount of nonheme iron absorbed from foods. Additional iron may be added to food from cooking in iron pots.
During the digestion of food in the stomach, bound iron is liberated from its matrix via a combination of factors that include gastric acidity, enzymatic action, and the churning action of the stomach muscles established by the specialized oblique muscle layer, which is unique to the stomach 5. The released iron is then available for absorption, which occurs predominantly in the duodenal segment of the small intestine 6.
Most dietary non-heme iron is in the insoluble ferric form which is first reduced to ferrous iron by the ferric reductase DcytB (duodenal cytochrome b) located on the brush border surface of duodenal enterocytes 7. Divalent proton-coupled metal iron transporter (DMT1) then transports ferrous iron across the apical membrane into the enterocyte, where it is either complexed within the storage protein ferritin, or transported into circulation across the basolateral membrane via the transmembrane transporter ferroportin (Ireg1) 8. Heme (haem) iron uptake occurs via an as yet unclarified mechanism which may involve the folate channel HCP1 9. The absorption process is sensitive to various factors, dietary and otherwise, that may impede this process leading to insufficient absorption and consequent iron deficiency 10.
Reduced iron delivery to target sites such as the liver tissue, bone marrow, and muscle myoglobin results in an impairment of iron-dependent functions such as erythropoiesis (formation of red blood cells) 3. A decrease in the number of red blood cells may also be characterized by a smaller mean cell size (microcytic anemia) 11. The net outcome is decreased oxygen carrying capacity and consequent tissue hypoxia. Iron depletion and deficiency in its mildest form is not particularly detrimental, however, progression to iron deficiency anemia or sideropenic anemia can have severe physiological consequences 12. Iron deficiency anemia during pregnancy has particularly severe consequences and has been associated with preterm delivery, perinatal mortality, maternal postpartum depression, and impaired mental development and cognitive ability of the offspring 13.
Although many people in the U.S. get enough iron from their diet, some must take additional amounts to meet their needs. For example, iron is sometimes lost with slow or small amounts of bleeding in the body that you would not be aware of and which can only be detected by your doctor. Your doctor can determine if you have an iron deficiency, what is causing the deficiency, and if an iron supplement is necessary.
Lack of iron may lead to unusual tiredness, shortness of breath, a decrease in physical performance, and learning problems in children and adults, and may increase your chance of getting an infection.
Some conditions may increase your need for iron. These include:
- Bleeding problems
- Burns
- Hemodialysis
- Intestinal diseases
- Stomach problems
- Stomach removal
- Use of medicines to increase your red blood cell count
In addition, infants, especially those receiving breast milk or low-iron formulas, may need additional iron.
- Increased need for iron supplements should be determined by your health care professional.
The daily amount of iron needed is defined in several different ways.
For U.S.
- Recommended Dietary Allowances (RDAs) are the amount of vitamins and minerals needed to provide for adequate nutrition in most healthy persons. RDAs for a given nutrient may vary depending on a person’s age, sex, and physical condition (e.g., pregnancy).
- Daily Values (DVs) are used on food and dietary supplement labels to indicate the percent of the recommended daily amount of each nutrient that a serving provides. DV replaces the previous designation of United States Recommended Daily Allowances (USRDAs).
For Canada
- Recommended Nutrient Intakes (RNIs) are used to determine the amounts of vitamins, minerals, and protein needed to provide adequate nutrition and lessen the risk of chronic disease.
Normal daily recommended intakes in milligrams (mg) for iron are generally defined as follows (Note that the RDA and RNI are expressed as an actual amount of iron, which is referred to as “elemental”’ iron. The product form [e.g., ferrous fumarate, ferrous gluconate, ferrous sulfate] has a different strength):
Table 1. Daily iron requirements
| Persons | U.S. (mg) | Canada (mg) |
| Infants birth to 3 years of age | 6–10 | 0.3–6 |
| Children 4 to 6 years of age | 10 | 8 |
| Children 7 to 10 years of age | 10 | 8–10 |
| Adolescent and adult males | 10 | 8–10 |
| Adolescent and adult females | 10–15 | 8–13 |
| Pregnant females | 30 | 17–22 |
| Breast-feeding females | 15 | 8–13 |
Treatment for iron deficiency and iron deficiency anemia is generally by means of oral iron supplements. Supplementation therapy can also be prescribed prophylactically in certain cases, e.g. for pregnant women, hemodialysis patients, and low birth weight infants. Intravenous iron administration is carried out in extreme cases such as significant blood loss or advanced malnutrition 14. Ferrous sulphate (FeSO4), along with the ferrous salts, ferrous fumarate and ferrous gluconate, are the most common form of iron supplements currently in use 15.
Accidental overdose of products containing iron is a leading cause of fatal poisoning in children under the age of 6. Keep this product out of the reach of children. In case of an accidental overdose, call your doctor or a poison control center immediately.
You should not use ferrous gluconate if you have hemochromatosis, hemosiderosis, or hemolytic anemia.
Groups at Risk of Iron Inadequacy
Isolated iron deficiency is uncommon in the United States. Because iron deficiency is associated with poor diet, malabsorptive disorders, and blood loss, people with iron deficiency usually have other nutrient deficiencies 16. The World Health Organization (WHO) estimates that approximately half of the 1.62 billion cases of anemia worldwide are due to iron deficiency 17. In developing countries, iron deficiency often results from enteropathies and blood loss associated with gastrointestinal parasites 16.
Iron depletion and deficiency progresses through several stages 18:
- Mild deficiency or storage iron depletion: Serum ferritin concentrations and levels of iron in bone marrow decrease.
- Marginal deficiency, mild functional deficiency, or iron-deficient erythropoiesis (erythrocyte production): Iron stores are depleted, iron supply to erythropoietic cells and transferrin saturation decline, but hemoglobin levels are usually within the normal range. In addition, plasma iron levels decline and plasma transferrin concentrations (measured by plasma total iron-binding capacity) rise, resulting in decreased transferrin saturation. Serum transferrin receptor concentrations also increase.
- Iron deficiency anemia: Iron stores are exhausted; hematocrit and levels of hemoglobin decline; and the resulting microcytic, hypochromic anemia is characterized by small red blood cells with low hemoglobin concentrations.
Iron deficiency anemia is defined as a hemoglobin level that is lower than two standard deviations from the mean distribution in a healthy population of the same gender and age living at the same altitude 19. At sea level, hemoglobin concentrations lower than 11 to 12 g/dL in children younger than 12, 12 g/dL in adolescents and women, and 13 g/dL in men indicate the presence of iron deficiency anemia 16. In 2002, the World Health Organization (WHO) characterized iron deficiency anemia as one of the 10 leading risk factors for disease around the world 20. Although iron deficiency is the most common cause of anemia, deficiencies of other micronutrients (such as folate and vitamin B12) and other factors (such as chronic infection and inflammation) can cause different forms of anemia or contribute to their severity.
The functional deficits associated with anemia include gastrointestinal disturbances and impaired cognitive function, immune function, exercise or work performance, and body temperature regulation 21. In infants and children, iron deficiency anemia can result in psychomotor and cognitive abnormalities that, without treatment, can lead to learning difficulties 21. Some evidence indicates that the effects of deficiencies early in life persist through adulthood 16. Because iron deficiency is often accompanied by deficiencies of other nutrients, the signs and symptoms of iron deficiency can be difficult to isolate 16.
The following groups are among those most likely to have inadequate intakes of iron.
Pregnant women
During pregnancy, plasma volume and red cell mass expand due to dramatic increases in maternal red blood cell production 16. As a result of this expansion and to meet the needs of the fetus and placenta, the amount of iron that women need increases during pregnancy. Iron deficiency during pregnancy increases the risk of maternal and infant mortality, premature birth, and low birthweight 17.
Insufficient iron intakes during pregnancy increase a woman’s risk of iron deficiency anemia 22. Low intakes also increase her infant’s risk of low birthweight, premature birth, low iron stores, and impaired cognitive and behavioral development.
An analysis of 1999–2006 data from the National Health and Nutrition Examination Survey (NHANES) found that 18% of pregnant women in the United States had iron deficiency 23. Rates of deficiency were 6.9% among women in the first trimester,14.3% in the second trimester, and 29.7% in the third trimester.
Randomized controlled trials have shown that iron supplementation can prevent iron deficiency anemia in pregnant women and related adverse consequences in their infants 24. A Cochrane review showed that daily supplementation with 9–90 mg iron reduced the risk of anemia in pregnant women at term by 70% and of iron deficiency at term by 57% 25. In the same review, use of daily iron supplements was associated with an 8.4% risk of having a low-birthweight newborn compared to 10.2% with no supplementation. In addition, mean birthweight was 31 g higher for infants whose mothers took daily iron supplements during pregnancy compared with the infants of mothers who did not take iron.
Guidelines on iron supplementation during pregnancy vary, but many recommend some form of iron supplementation to prevent iron deficiency anemia:
- The American College of Obstetricians and Gynecologists (ACOG) states that good and consistent evidence shows that iron supplementation decreases the prevalence of maternal anemia at delivery [61]. However, it acknowledges that only limited or inconsistent evidence shows that iron deficiency anemia during pregnancy is associated with a higher risk of low birthweight, preterm birth, or perinatal mortality. The American College of Obstetricians and Gynecologists recommends screening all pregnant women for anemia and treating those with iron deficiency anemia (which it defines as hematocrit levels less than 33% in the first and third trimesters and less than 32% in the second trimester) with supplemental iron in addition to prenatal vitamins 26.
- The Centers for Disease Control and Prevention (CDC) recommends that all pregnant women, at their first prenatal visit, begin taking an oral, low dose (30 mg/day) supplement of iron and be screened for iron deficiency anemia 27. Women with iron deficiency anemia (which it defines as a hemoglobin concentration less than 9 g/dL or a hematocrit level less than 27%) should be treated with an oral dose of 60-120 mg/day of iron.
- In contrast, the U.S. Preventive Services Task Force (USPSTF) has concluded that the current evidence is insufficient to recommend for or against both screening for iron deficiency anemia in pregnant women and routinely supplementing them with iron to prevent adverse maternal health and birth outcomes 28. They note, however, that their recommendation does not apply to pregnant women who are malnourished, have symptoms of iron deficiency anemia, or those with special hematologic conditions or nutritional needs that increase iron requirements.
The Institute of Medicine notes that because the median intake of dietary iron by pregnant women is well below the Estimated Average Requirement (average daily level of intake estimated to meet the requirements of 50% of healthy individuals; usually used to assess the nutrient intakes of groups of people and to plan nutritionally adequate diets for them; can also be used to assess the nutrient intakes of individuals), pregnant women need iron supplementation 29. The Dietary Guidelines for Americans advises that women who are pregnant take an iron supplement when recommended by an obstetrician or other health-care provider 30. It adds that low intakes of iron are a public health concern for pregnant women.
Infants and young children
Infants—especially those born preterm or with low birthweight or whose mothers have iron deficiency—are at risk of iron deficiency because of their high iron requirements due to their rapid growth 31. Full-term infants usually have sufficient iron stores and need little if any iron from external sources until they are 4 to 6 months old 16. However, full-term infants have a risk of becoming iron deficient at 6 to 9 months unless they obtain adequate amounts of solid foods that are rich in bioavailable iron or iron-fortified formula.
Approximately 12% of infants aged 6 to 11 months in the United States have inadequate iron intakes, and 8% of toddlers have iron deficiency 32. The prevalence of iron deficiency anemia in U.S. toddlers aged 12 to 35 months ranges from 0.9% to 4.4% depending on race or ethnicity and socioeconomic status 33. Full-term infants typically have adequate iron stores for approximately the first 4 to 6 months, but the risk of iron deficiency in low-birthweight and preterm infants begins at birth because of their low iron stores.
Iron deficiency anemia in infancy can lead to adverse cognitive and psychological effects, including delayed attention and social withdrawal; some of these effects might be irreversible 33. In addition, iron deficiency anemia is associated with higher lead concentrations in the blood (although the cause of this is not fully understood), which can increase the risk of neurotoxicity 33.
A Cochrane review of 26 studies in 2,726 preterm and low-birthweight infants found that enteral iron supplementation (at least 1 mg/kg/day) reduces the risk of iron deficiency, but the long-term effects of supplementation on neurodevelopmental outcomes and growth is not clear 34. Another Cochrane review of 8 trials in 3,748 children younger than 2 in low-income countries showed that home fortification of semi-solid foods with micronutrient powders containing 12.5 mg to 30 mg elemental iron as ferrous fumarate and 4 to 14 other micronutrients for 2 to 12 months reduced rates of anemia by 31% and of iron deficiency by 51% compared with no intervention or placebo but had no effect on any growth measurements 35.
Guidelines vary on dietary iron intakes and possible supplementation to ensure adequate iron status and to prevent or treat iron deficiency anemia in infants and young children:
- The Centers for Disease Control and Prevention (CDC) recommends that infants less than 12 months of age who are not exclusively or primarily breastfed drink iron-fortified infant formula 36. Breastfed infants who were born preterm or with a low birthweight should receive 2-4 mg/kg/day of iron drops (to a maximum of 15 mg/day) from ages 1-12 months. Breastfed infants who receive insufficient iron (less than 1 mg/kg/day) from supplementary foods by age 6 months should receive 1 mg/kg/day of iron drops. The Centers for Disease Control and Prevention (CDC) also recommends that infants and preschool children at high risk for iron deficiency anemia (e.g., children from low-income families and migrant children) be screened between ages 9-12 months, 6 months later, and annually from ages 2-5 years. Treatment for iron deficiency anemia begins with 3 mg/kg/day of iron drops given between meals.
- The American Academy of Pediatrics recommends 1 mg/kg daily iron supplementation for exclusively or primarily breastfed full-term infants from age 4 months until the infants begin eating iron-containing complementary foods, such as iron-fortified cereals 33. Standard infant formulas containing 10 to 12 mg/L iron can meet the iron needs of infants for the first year of life. The American Academy of Pediatrics recommends 2 mg/kg/day iron supplementation for preterm infants aged 1 to 12 months who are fed breast milk.
- The WHO recommends universal supplementation with 2 mg/kg/day of iron in children aged 6 to 23 months whose diet does not include foods fortified with iron or who live in regions (such as developing countries) where anemia prevalence is higher than 40% 19.
- In a recommendation statement issued in 2015, the U.S. Preventive Services Task Force (USPSTF) concluded that the available evidence is insufficient to recommend for or against routine screening for iron deficiency anemia in children ages 6 to 24 months who live in the United States and who are asymptomatic for iron deficiency anemia 37. It added that this recommendation does not apply to severely malnourished children or children who were born prematurely or with low birthweight. Earlier, in 2006, the U.S. Preventive Services Task Force (USPSTF) stated that while it found insufficient evidence to recommend routine iron supplementation in asymptomatic infants at average risk of iron deficiency anemia, it did recommend routine iron supplements for children aged 6 to 12 months who are at increased risk of iron deficiency anemia (e.g., those who were premature or low birthweight) 38. The USPSTF’s 2015 statement notes that its current recommendation is limited to screening because the widespread use of iron-fortified foods in the United States (including infant formulas and cereals) would likely limit the impact of iron supplementation prescribed by physicians 39.
Some studies have suggested that iron supplementation in young children living in areas where malaria is endemic could increase their risk of malaria 40. However, a Cochrane review of 33 trials in 13,114 children showed that intermittent supplementation does not appear to have this effect 41. The WHO therefore recommends 6-month supplementation cycles as follows: children aged 24 to 59 months should receive 25 mg iron and those aged 5 to 12 years should receive 45 mg every week for 3 months, followed by 3 months of no supplementation 42. The WHO recommends providing these supplements in malaria-endemic areas in conjunction with measures to prevent, diagnose, and treat malaria.
Women with heavy menstrual bleeding
Women of reproductive age who have menorrhagia, or abnormally heavy bleeding during menstruation, are at increased risk of iron deficiency. At least 10% of menstruating women are believed to have menorrhagia, but the percentage varies widely depending on the diagnostic criteria used 43. Women with menorrhagia lose significantly more iron per menstrual cycle on average than women with normal menstrual bleeding 44. Limited evidence suggests that menorrhagia might be responsible for about 33% to 41% of cases of iron deficiency anemia in women of reproductive age 45.
Frequent blood donors
Frequent blood donors have an increased risk of iron deficiency 29. In the United States, adults may donate blood as often as every 8 weeks, which can deplete iron stores. About 25%–35% of regular blood donors develop iron deficiency 46. In a study of 2,425 blood donors, men who had given at least three and women who had given at least two whole-blood donations in the previous year were more than five times as likely to have depleted iron stores as first-time donors 47. A clinical trial of iron supplementation found that of 215 adults who had donated a unit of blood within the past 3–8 days, those randomized to take an iron supplement (37.5 mg/day elemental iron from ferrous gluconate) for 24 weeks recovered their lost hemoglobin and iron in less than half the time of those not given the supplement 46. Without iron supplementation, two-thirds of the donors had not recovered the iron they lost, even after 24 weeks.
People with cancer
Up to 60% of patients with colon cancer have iron deficiency at diagnosis, probably due to chronic blood loss 48. The prevalence of iron deficiency in patients with other types of cancer ranges from 29% to 46%. The main causes of iron deficiency in people with cancer are anemia of chronic disease (discussed in the Iron and Health section below) and chemotherapy-induced anemia. However, chronic blood loss and deficiencies of other nutrients (due, for example, to cancer-induced anorexia) can exacerbate iron deficiency in this population.
People who have gastrointestinal disorders or have had gastrointestinal surgery
People with certain gastrointestinal disorders (such as celiac disease, ulcerative colitis, and Crohn’s disease) or who have undergone certain gastrointestinal surgical procedures (such as gastrectomy or intestinal resection) have an increased risk of iron deficiency because their disorder or surgery requires dietary restrictions or results in iron malabsorption or blood loss in the gastrointestinal tract 49. The combination of low iron intake and high iron loss can lead to a negative iron balance; reduced production of hemoglobin; or microcytic, hypochromic anemia 50.
People with heart failure
Approximately 60% of patients with chronic heart failure have iron deficiency and 17% have IDA, which might be associated with a higher risk of death in this population 51. Potential causes of iron deficiency in people with heart failure include poor nutrition, malabsorption, defective mobilization of iron stores, cardiac cachexia, and use of aspirin and oral anticoagulants, which might result in the loss of some blood in the gastrointestinal tract 52.
Ferrous gluconate precautions
Before taking ferrous gluconate
You should not use ferrous gluconate if you are allergic to it, or if you have:
- iron overload disorder (hemochromatosis, hemosiderosis); or
- hemolytic anemia (caused by the breakdown of red blood cells).
To make sure ferrous gluconate is safe for you, tell your doctor if you have ever had:
- ulcerative colitis;
- stomach ulcers or similar stomach problems;
- thalassemia (a genetic disorder of red blood cells); or
- if you receive regular blood transfusions.
Ask a doctor before using ferrous gluconateif you are pregnant or breast-feeding. Your dose needs may be different during pregnancy or while you are nursing.
Ferrous gluconate is not approved for use by anyone younger than 18 years old.
How should I take ferrous gluconate?
Use ferrous gluconate exactly as directed on the label, or as prescribed by your doctor. Do not use it in larger amounts or for longer than recommended.
Take ferrous gluconate on an empty stomach, at least 1 hour before or 2 hours after a meal.
Ferrous gluconate may be taken with food if it upsets your stomach.
Take ferrous gluconate with a full glass of water or juice.
Measure liquid medicine with the dosing syringe provided, or with a special dose-measuring spoon or medicine cup. If you do not have a dose-measuring device, ask your pharmacist for one.
Do not crush, chew, or break an extended-release tablet. Swallow the pill whole.
Ferrous gluconate can stain your teeth, but this effect is temporary. To prevent tooth staining, mix the liquid form of ferrous gluconate with water or fruit juice (not with milk) and drink the mixture through a straw. You may also clean your teeth with baking soda once per week to treat any tooth staining.
Ferrous gluconate may be only part of a complete program of treatment that also includes a special diet. Follow the diet plan created for you by your doctor or nutrition counselor. Get familiar with the list of foods you should eat to make sure you get enough iron in your diet.
Store at room temperature, away from moisture and heat.
How should iron ferrous gluconate be used?
Iron ferrous gluconate come as regular tablets; capsules, and an oral liquid (drops and elixir) to take by mouth. Iron ferrous gluconate is usually taken with food or immediately after a meal once daily or as directed by your doctor. Take iron ferrous gluconate at around the same time(s) every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take iron ferrous gluconate exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Ferrous gluconate supplements are available alone and in fixed-combination with vitamins (e.g. folic acid or ascorbic acid) and certain medications. If your doctor has prescribed ferrous gluconate that contains iron, you should be careful not to take any other supplements or medications that also contain iron.
Swallow the tablets, film-coated tablets, and extended release tablets whole; do not split, chew, or crush them.
Mix the syrup with water or fruit juice to avoid possible teeth staining; do not mix with milk or a wine-based solutions.
Iron drops come with a special dropper for measuring the dose. Ask your pharmacist or doctor to show you how to use it. The drops may be placed directly in the mouth or mixed with water, breastmilk, cereal, formula, or fruit juice. Dispense gently into mouth towards inner cheek; a small amount will remain in the tip. If you are giving iron drops to a child, read the package label carefully to be sure that it is the right product for a child of that age. Do not give iron products that are made for adults to children.
What should I avoid while taking ferrous gluconate?
Ask your doctor before using any vitamin or mineral supplement, or an antacid. Use only the type of antacid or supplements that your doctor recommends. Some minerals or antacids can make it harder for your body to absorb ferrous gluconate.
Avoid taking antacids or antibiotics within 2 hours before or 2 hours after taking ferrous gluconate. This is especially important if you take:
- ciprofloxacin, levofloxacin, lomefloxacin, norfloxacin, ofloxacin; or
- demeclocycline, doxycycline, minocycline, or tetracycline.
Certain foods can also make it harder for your body to absorb ferrous gluconate. Avoid taking this medicine within 1 hour before or 2 hours after eating fish, meat, liver, and whole grain or “fortified” breads or cereals.
Ferrous gluconate uses
Ferrous gluconate is used to treat or prevent iron deficiency anemia (a lower than normal number of red blood cells) when the amount of iron taken in from the diet is not enough. Iron is a mineral that is available as a dietary supplement. It works by helping the body to produce red blood cells.
Ferrous gluconate Pregnancy Warnings
Maternal anemia increases the risk of low birthweight, premature delivery, and impaired cognitive and behavioral development. Randomized trials show that supplementation can prevent iron deficiency anemia and related adverse consequences to the infant. Recent studies 53, 54 have linked high serum iron with an increased risk of gestational diabetes.
US FDA pregnancy category: Not Assigned
Ferrous gluconate and breastfeeding
Use is considered acceptable.
Excreted into human milk: Yes
Comments:
- Iron in breast milk is very bioavailable, but amounts are generally not sufficient for infants older than 4 months; iron supplementation of the mother does not change this situation.
- Iron content of breast milk is not affected by the mother’s nutritional status.
Ferrous gluconate dosage
Dosage for ferrous gluconate (oral tablet, oral capsule, oral tablet, extended release, compounding powder, oral liquid).
Administration advice:
- Coffee, tea, milk, cereal, dietary fiber, and phosphate containing carbonated drinks decrease iron absorption.
- Supplements containing calcium, zinc, manganese, or copper decrease iron absorption.
- Antacids, H2 blockers, and proton pump inhibitors decrease iron absorption; do not use within 1 to 2 hours of iron administration.
- Vitamin C and acidic foods increase iron absorption.
- Delayed release and enteric coated formulations are better tolerated, but are not as well absorbed.
Adult Dose for Iron Deficiency Anemia
- Initial dose: 960 mg/day ferrous gluconate (120 mg/day elemental iron) for 3 months
- Give in divided doses (1 to 3 times daily)
Adult Dose for Vitamin/Mineral Supplementation
- Initial dose: 1 tablet orally three to four times a day
or
- Initial dose: 48 to 144 mg/day ferrous gluconate (6 to 18 mg/day elemental iron) orally, in divided doses (1 to 3 times daily)
- 51 and over: 40 to 64 mg/day ferrous gluconate (5 to 8 mg/day elemental) orally, in divided doses (1 to 3 times daily)
Adult Dose for Anemia Associated with Chronic Renal Failure
- Initial dose: 1600 mg/day ferrous gluconate (200 mg/day elemental iron) orally in divided doses (1 to 3 times daily)
Comments:
- If goals are not met with oral iron after 1 to 3 months, consider IV iron supplementation.
- Smaller daily doses may be better tolerated
- Dialysis: Iron supplementation is routinely provided to peritoneal dialysis and hemodialysis patients for prevention or treatment of anemia associated with chronic renal failure.
Pediatric Dose for Iron Deficiency Anemia
Give in divided doses (1 to 3 times daily):
- 0 to 5 years: 24 to 48 mg/kg/day ferrous gluconate (3 to 6 mg/kg/day elemental iron)
- 5 to 12 years: 480 mg ferrous gluconate (60 mg/day elemental)
- 12 to 18 years male: 480 mg ferrous gluconate (60 mg elemental) orally daily
- 12 to 18 years female: 480 to 960 mg/day ferrous gluconate (60 to 120 mg/day elemental)
Pediatric Dose for Vitamin/Mineral Supplementation
Give in divided doses (1 to 3 times daily):
- Preterm infant (less than 37 weeks gestation), 0 to 12 months: 16 mg/kg/day ferrous gluconate (2 mg/kg/day elemental iron)
- 0 to 6 months: 1.6 to 2.16 mg/day ferrous gluconate (0.2 to 0.27 mg/day elemental)
- 7 to 12 months: 56 to 88 mg/day ferrous gluconate (7 to 11 mg/day elemental)
- 1 to 3 years: 32 to 72 mg/day ferrous gluconate (4 to 9 mg/day elemental)
- 4 to 8 years: 32 to 80 mg/day ferrous gluconate (4 to 10 mg/day elemental)
- 9 to 13 years: 48 to 64 mg/day ferrous gluconate (6 to 8 mg/day elemental)
- 14 to 18 years: 64 to 120 mg/day ferrous gluconate (8 to 15 mg/day elemental)
Dose Adjustments
Vitamin supplementation/Prevention of anemia:
- 14 to 18 years: Pregnancy: 184 to 216 mg/day ferrous gluconate (23 to 27 mg/day elemental iron)
- 14 to 18 years: Lactation: 56 to 80 mg/day ferrous gluconate (7 to 10 mg/day elemental)
- 19 to 50 years: Pregnancy: 176 to 216 mg/day ferrous gluconate (22 to 27 mg/day elemental)
- 19 to 50 years: Lactation: 52 to 72 mg/day ferrous gluconate (6.5 to 9 mg/day elemental)
- Maximum dose: 360 mg ferrous gluconate (45 mg/day elemental)
Treatment of anemia:
- Pregnancy: 480 to 960 mg ferrous gluconate (60 to 120 mg/day elemental)
Renal Dose Adjustments
- No adjustments recommended
Liver Dose Adjustments
- No adjustments recommended
What happens if I miss a dose?
Take the missed dose as soon as you remember. Skip the missed dose if it is almost time for your next scheduled dose. Do not take extra medicine to make up the missed dose.
Ferrous gluconate side effects
Common side effects may include:
- constipation, diarrhea;
- nausea, vomiting, stomach pain;
- loss of appetite;
- green-colored stools; or
- temporary staining of the teeth.
Get emergency medical help if you have signs of an allergic reaction: hives, blistering or peeling skin; fever; difficulty breathing; swelling of your face, lips, tongue, or throat.
Call your doctor at once if you have:
- bright red blood in your stools;
- black or tarry stools;
- a fever;
- stomach pain;
- coughing up blood or vomit that looks like coffee grounds; or
- pain in your chest or throat when swallowing a ferrous gluconate tablet.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects.
Iron overdose
In case of overdose, call the poison control helpline at 1-800-222-1222. Information is also available online at https://www.poisonhelp.org/help. If the victim has collapsed, had a seizure, has trouble breathing, or can’t be awakened, immediately call your local emergency services number.
Symptoms of overdose may include the following:
- drowsiness,
- severe nausea or stomach pain,
- vomiting,
- bloody diarrhea,
- coughing up blood or vomit that looks like coffee grounds,
- shallow breathing,
- weak and rapid pulse,
- cold or clammy skin,
- blue lips, and
- seizure (convulsions).
Note: Symptoms may go away in a few hours, then return again after 1 day or later.
Below are symptoms of an iron overdose in different parts of the body.
AIRWAYS AND LUNGS
- Buildup of fluids in the lungs
STOMACH AND INTESTINES
- Black, and possibly bloody stools
- Diarrhea
- Liver damage
- Metallic taste in mouth
- Nausea
- Vomiting blood
HEART AND BLOOD
- Dehydration
- Low blood pressure
- Fast and weak pulse
- Shock
NERVOUS SYSTEM
- Chills
- Coma (decreased level of consciousness and lack of responsiveness, may occur within 1/2 hour to 1 hour after overdose)
- Convulsions
- Dizziness
- Drowsiness
- Fever
- Headache
- Lack of desire to do anything
SKIN
- Bluish-colored lips and fingernails
- Flushing
- Loss of color from the skin (pallor)
What to expect at the Emergency Room
Take the container to the hospital with you, if possible.
The health care provider will measure and monitor the person’s vital signs, including temperature, pulse, breathing rate, and blood pressure. Symptoms will be treated.
Tests that may done include:
- Blood and urine tests, including tests to check iron levels
- ECG (electrocardiogram, or heart tracing)
- X-ray to detect and track iron tablets through the stomach and intestines
Treatment may include:
- Fluids through a vein (by IV)
- Medicine to help remove iron from the body and treat symptoms
- Endoscopy — camera and tube placed down the throat to view the esophagus and the stomach and to remove pills or stop internal bleeding
- Whole bowel irrigation with a special solution to quickly flush the iron through the stomach and intestines (taken by mouth or through a tube through the nose into the stomach)
- Breathing support, including tube through the mouth into the lungs and connected to a breathing machine (ventilator)
Outlook (Prognosis)
There is a good chance of recovery if the person’s symptoms are gone 48 hours after the iron overdose. But, severe liver damage can occur 2 to 5 days after the overdose. Some people have died up to a week after an iron overdose. The more quickly the person receives treatment, the better the chance for survival.
Iron overdose can be very severe in children. Children may sometimes eat large amounts of iron pills because they look like candy. Many manufacturers have changed their pills so they no longer look like candy.
- Zariwala MG, Somavarapu S, Farnaud S, Renshaw D. Comparison study of oral iron preparations using a human intestinal model. Sci Pharm. 2013;81(4):1123-39. Published 2013 Jun 21. doi:10.3797/scipharm.1304-03 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3867244/[↩]
- Zimmermann MB, Hurrell RF. Nutritional iron deficiency. Lancet. 2007;370:511–520 https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(07)61235-5/fulltext[↩]
- Andrews NC. Disorders of Iron Metabolism. New Eng J Med. 1999;341:1986–1995. http://dx.doi.org/10.1056/NEJM199912233412607[↩][↩]
- Crichton RR, Wilmet S, Legssyer R, Ward RJ. Molecular and cellular mechanisms of iron homeostasis and toxicity in mammalian cells. J Inorg Biochem. 2002;91:9–18. http://dx.doi.org/10.1016/S0162-0134(02)00461-0[↩][↩]
- Miret S, Simpson RJ, McKie AT. Physiology and molecular biology of dietary iron absorption. Annu Rev Nutri. 2003;23:283–301. http://www.ncbi.nlm.nih.gov/pubmed/12626689[↩]
- Muir A, Hopfer U. Regional specificity of iron uptake by small intestinal brush-border membranes from normal and iron-deficient mice. Am J Physiol. 1985;248:G376–G379. http://www.ncbi.nlm.nih.gov/pubmed/3976894[↩]
- Riedel HD, Remus AJ, Fitscher BA, Stremmel W. Characterization and partial purification of a ferrireductase from human duodenal microvillus membranes. Biochem J. 1995;309:745–748. http://www.ncbi.nlm.nih.gov/pubmed/7639688[↩]
- Garrick MD, Garrick LM. Cellular iron transport. Biochim Biophys Acta. 2009;1790:309–325. http://dx.doi.org/10.1016/j.bbagen.2009.03.018[↩]
- Laftah AH, Latunde-Dada GO, Fakih S, Hider RC, Simpson RJ, McKie AT. Haem and folate transport by proton-coupled folate transporter/haem carrier protein 1 (SLC46A1) Br J Nutr. 2009;101:1150–1156. http://dx.doi.org/10.1017/S0007114508066762[↩]
- Conrad ME, Umbreit JN. A concise review: Iron absorption-the mucin-mobilferrin-integrin pathway. A competitive pathway for metal absorption. Am J Hematol. 1993;42:67–73. http://dx.doi.org/10.1002/ajh.2830420114[↩]
- Iolascon A, De Falco L, Beaumont C. Molecular basis of inherited microcytic anemia due to defects in iron acquisition or heme synthesis. Haematologica. 2009;94:395–408. http://dx.doi.org/10.3324/haematol.13619[↩]
- Hercberg S, Preziosi P, Galan P. Iron deficiency in Europe. Public Health Nutr. 2001;4:537–545. http://dx.doi.org/10.1079/PHN2001139[↩]
- Usha R, editor. Nutritional Anemias. CRC Press, Taylor & Francis Group; 2000. Functional Consequences of Nutritional Anemia during Pregnancy and Early Childhood; pp. 43–68.[↩]
- Intravenous iron dextran in clinical medicine. Hamstra RD, Block MH, Schocket AL. JAMA. 1980 May 2; 243(17):1726-31.[↩]
- Guidelines for the management of iron deficiency anaemia. Goddard AF, James MW, McIntyre AS, Scott BB, British Society of Gastroenterology. Gut. 2011 Oct; 60(10):1309-16.[↩]
- Aggett PJ. Iron. In: Erdman JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed. Washington, DC: Wiley-Blackwell; 2012:506-20.[↩][↩][↩][↩][↩][↩][↩]
- World Health Organization. Worldwide Prevalence of Anaemia 1993–2005: WHO Global Database on Anaemia. World Health Organization, 2008. http://apps.who.int/iris/bitstream/handle/10665/43894/9789241596657_eng.pdf[↩][↩]
- World Health Organization. Report: Priorities in the Assessment of Vitamin A and Iron Status in Populations, Panama City, Panama, 15-17 September 2010. Geneva; 2012. http://apps.who.int/iris/bitstream/handle/10665/75334/9789241504225_eng.pdf[↩]
- World Health Organization. Iron Deficiency Anaemia: Assessment, Prevention, and Control. World Health Organization, 2001. http://www.who.int/nutrition/publications/en/ida_assessment_prevention_control.pdf[↩][↩]
- World Health Organization. The World Health Report. Geneva: World Health Organization; 2002.[↩]
- Clark SF. Iron Deficiency Anemia. Nutr Clin Pract 2008;23:128-41.[↩][↩]
- Pena-Rosas JP, De-Regil LM, Dowswell T, Viteri FE. Daily oral iron supplementation during pregnancy. Cochrane Database Syst Rev 2012;12:CD004736[↩]
- Mei Z, Cogswell ME, Looker AC, Pfeiffer CM, Cusick SE, Lacher DA, et al. Assessment of iron status in US pregnant women from the National Health and Nutrition Examination Survey (NHANES), 1999-2006. Am J Clin Nutr 2011;93:1312-20.[↩]
- Makrides M, Crowther CA, Gibson RA, Gibson RS, Skeaff CM. Efficacy and tolerability of low-dose iron supplements during pregnancy: a randomized controlled trial. Am J Clin Nutr 2003;78:145-53.[↩]
- Pena-Rosas JP, De-Regil LM, Dowswell T, Viteri FE. Daily oral iron supplementation during pregnancy. Cochrane Database Syst Rev 2012;12:CD004736.[↩]
- American Congress of Obstetrics and Gynecology. ACOG Practice Bulletin No. 95: anemia in pregnancy. Obstet Gynecol 2008;112:201-7.[↩]
- Centers for Disease Control and Prevention (CDC). Recommendations to prevent and control iron deficiency in the United States. MMWR Recomm Rep 1998;47:1-29.[↩]
- Siu AL, on behalf of the U.S. Preventive Services Task Force. Screening for iron deficiency anemia and iron supplementation in pregnant women to improve maternal health and birth outcomes: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. doi:10.7326/M15-1707.[↩]
- Institute of Medicine. Food and Nutrition Board. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc : a Report of the Panel on Micronutrients. Washington, DC: National Academy Press; 2001. https://www.nap.edu/read/10026/chapter/1[↩][↩]
- Dietary Guidelines. https://health.gov/dietaryguidelines/[↩]
- Black MM, Quigg AM, Hurley KM, Pepper MR. Iron deficiency and iron-deficiency anemia in the first two years of life: strategies to prevent loss of developmental potential. Nutr Rev 2011;69 Suppl 1:S64-70[↩]
- Butte NF, Fox MK, Briefel RR, Siega-Riz AM, Dwyer JT, Deming DM, et al. Nutrient intakes of US infants, toddlers, and preschoolers meet or exceed dietary reference intakes. J Am Diet Assoc 2010;110:S27-37[↩]
- Baker RD, Greer FR. Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0-3 years of age). Pediatrics 2010;126:1040-50.[↩][↩][↩][↩]
- Mills RJ, Davies MW. Enteral iron supplementation in preterm and low birth weight infants. Cochrane Database Syst Rev 2012;3:CD005095[↩]
- De-Regil LM, Suchdev PS, Vist GE, Walleser S, Pena-Rosas JP. Home fortification of foods with multiple micronutrient powders for health and nutrition in children under two years of age (review). Cochrane Database Syst Rev 2011:CD008959[↩]
- Centers for Disease Control and Prevention (CDC). Recommendations to prevent and control iron deficiency in the United States. MMWR Recomm Rep 1998;47:1-29[↩]
- Siu AL, on behalf of the US Preventive Services Task Force. Screening for iron deficiency anemia in young children: USPSTF recommendation statement. Pediatrics 2015;136:746-52[↩]
- U.S. Preventive Services Task Force. Screening for Iron Deficiency Anemia—Including Iron Supplementation for Children and Pregnant Women: Recommendation Statementexternal. Publication No. AHRQ 06-058., 2006. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/iron-deficiency-anemia-screening[↩]
- Siu AL, on behalf of the US Preventive Services Task Force. Screening for iron deficiency anemia in young children: USPSTF recommendation statement. Pediatrics 2015;136:746-52.[↩]
- Sazawal S, Black RE, Ramsan M, Chwaya HM, Stoltzfus RJ, Dutta A, et al. Effects of routine prophylactic supplementation with iron and folic acid on admission to hospital and mortality in preschool children in a high malaria transmission setting: community-based, randomised, placebo-controlled trial. Lancet 2006;367:133-43[↩]
- De-Regil LM, Jefferds ME, Sylvetsky AC, Dowswell T. Intermittent iron supplementation for improving nutrition and development in children under 12 years of age. Cochrane Database Syst Rev 2011:CD009085[↩]
- World Health Organization. Guideline: Intermittent Iron Supplementation in Preschool and School-age Children. Geneva; 2011[↩]
- Matthews ML. Abnormal uterine bleeding in reproductive-aged women. Obstet Gynecol Clin North Am 2015;42:103-15.[↩]
- Napolitano M, Dolce A, Celenza G, Grandone E, Perilli MG, Siragusa S, et al. Iron-dependent erythropoiesis in women with excessive menstrual blood losses and women with normal menses. Ann Hematol 2014;93:557-63[↩]
- Vannella L, Aloe Spiriti MA, Cozza G, Tardella L, Monarca B, Cuteri A, et al. Benefit of concomitant gastrointestinal and gynaecological evaluation in premenopausal women with iron deficiency anaemia. Aliment Pharmacol Ther 2008;28:422-30[↩]
- Kiss JE, Brambilla D, Glynn SA, Mast AE, Spencer BR, Stone M, et al. Oral iron supplementation after blood donation: a randomized clinical trial. JAMA 2015;313:575-83[↩][↩]
- Cable RG, Glynn SA, Kiss JE, Mast AE, Steele WR, Murphy EL, et al. Iron deficiency in blood donors: analysis of enrollment data from the REDS-II Donor Iron Status Evaluation (RISE) study. Transfusion 2011;51:511-22[↩]
- Aapro M, Osterborg A, Gascon P, Ludwig H, Beguin Y. Prevalence and management of cancer-related anaemia, iron deficiency and the specific role of i.v. iron. Ann Oncol 2012;23:1954-62.[↩]
- Bayraktar UD, Bayraktar S. Treatment of iron deficiency anemia associated with gastrointestinal tract diseases. World J Gastroenterol 2010;16:2720-5.[↩]
- Kulnigg S, Gasche C. Systematic review: managing anaemia in Crohn’s disease. Aliment Pharmacol Ther 2006;24:1507-23[↩]
- Parikh A, Natarajan S, Lipsitz SR, Katz SD. Iron deficiency in community-dwelling US adults with self-reported heart failure in the National Health and Nutrition Examination Survey III: prevalence and associations with anemia and inflammation. Circ Heart Fail 2011;4:599-606.[↩]
- Lipsic E, van der Meer P. Erythropoietin, iron, or both in heart failure: FAIR-HF in perspective. Eur J Heart Fail 2010;12:104-5.[↩]
- Rawal S, Hinkle SN, Bao W, et.al “A longitudinal study of iron status during pregnancy and the risk of gestational diabetes: findings from a prospective, multiracial cohort.” Diabetologia 60 (2017): 249-57[↩]
- Bao W, Chavarro JE, Tobias DK, et.al “Long-term risk of type 2 diabetes in relation to habitual iron intake in women with a history of gestational diabetes: a prospective cohort study.” Am J Clin Nutr 103 (2016): 375-81[↩]