Contents
What is hip pain
Hip pain involves any pain in or around the hip joint. Hip pain is a very common complaint that can affect patients of all ages and can be caused by a variety of different causes 1. Hip pain often presents a diagnostic and therapeutic challenge. The causes of hip pain (see Table 1 below) is broad, including both intra-articular and extra-articular pathology, and varies by age. A history and physical examination are essential to accurately diagnose the cause of hip pain.
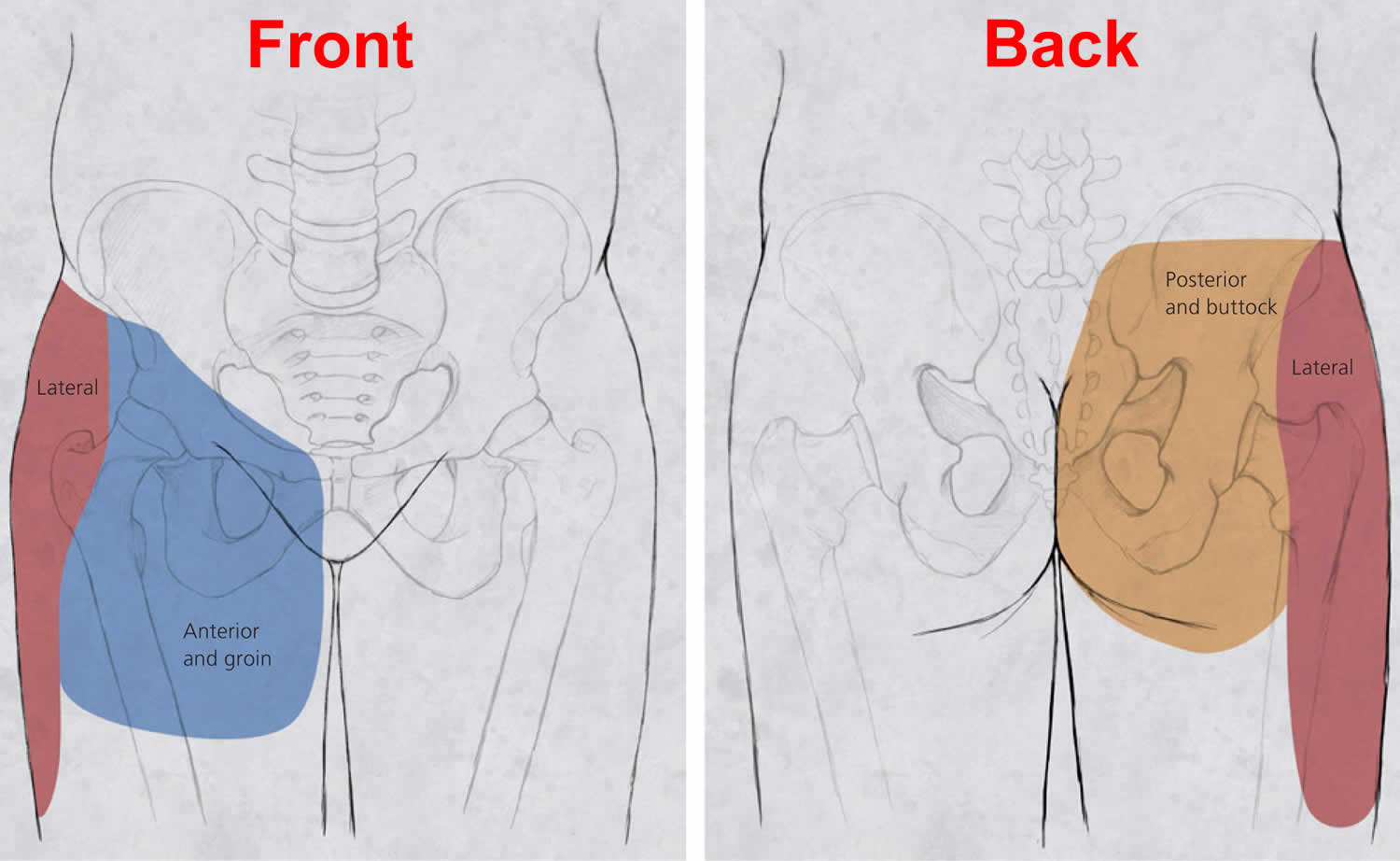
The precise location of your hip pain can provide valuable clues about the underlying cause. Problems within the hip joint itself tend to result in pain on the inside of your hip or your groin. Hip pain on the outside of your hip, upper thigh or outer buttock is usually caused by problems with muscles, ligaments, tendons and other soft tissues that surround your hip joint.
Hip pain can sometimes be caused by diseases and conditions in other areas of your body, such as your lower back. This type of pain is called referred pain.
You may not feel pain from your hip directly over the hip area. You may feel it in your groin or pain in your thigh or knee.
Patients often express that their hip pain is localized to one of three anatomic regions (see Figure 2 below):
- Front hip and groin pain: Front hip and groin pain is commonly associated with intra-articular pathology (involvement of the hip joint itself), such as osteoarthritis and hip labral tears. Patients often localize pain by cupping the anterolateral hip with the thumb and forefinger in the shape of a “C.” This is known as the C sign (see Figure 3A below).
- Back hip and buttock pain: Back hip pain is associated with piriformis syndrome, sacroiliac joint dysfunction, lumbar radiculopathy, and less commonly ischiofemoral impingement and vascular claudication.
- Outer hip pain: Outer hip pain (lateral hip pain) occurs with greater trochanteric pain syndrome.
If you have hip pain that persists, you should see a doctor or physiotherapist. Don’t try to diagnose the cause of your hip pain yourself – this should always be a matter for your doctor.
Hip pain in children is most often caused by a condition called irritable hip, which usually gets better on its own. But it should always be checked because it could be a sign of something serious.
You should talk to your doctor or physiotherapist about your hip pain immediately if:
- the pain is sudden or intense
- the result of an injury or a fall
- you can’t move your hip or leg
- you can’t put weight on the affected leg
- you notice swelling or bleeding
- you notice any sign of an infection, like a fever
If your child has pain in the hip, see your child’s doctor.
Go to a hospital or get emergency help if:
- Your hip pain is acute and caused by a serious fall or other injury.
- Your leg is deformed, badly bruised, or bleeding.
- You are unable to move your hip or bear any weight on your leg.
Ask someone to drive you to urgent care or the emergency room if your hip pain is caused by an injury and is accompanied by:
- A joint that appears deformed
- Inability to move your leg or hip
- Inability to bear weight on the affected leg
- Intense pain
- Sudden swelling
- Any signs of infection (fever, chills, redness)
See your doctor if:
- Your hip is still painful after 1 week of home treatment.
- You also have a fever or rash.
- You have sudden hip pain, plus sickle cell anemia or long-term steroid use.
- You have pain in both hips and other joints as well.
Ask for an urgent doctor appointment or go to emergency room if your child:
- gets sudden pain in their hip, thigh or knee (hip problems can sometimes be felt in the thigh or knee)
- is limping or can’t put any weight on one leg
Your child probably just have irritable hip (inflammation of the hip joint). This isn’t serious and gets better by itself.
But your child should be checked to rule out anything like a broken bone or infected joint (septic arthritis).
The treatment for hip pain might include:
- physiotherapy or occupational therapy
- anti-inflammatory, pain-killing medicines or creams
- antibiotics
- steroid injections
- acupuncture
- advice about weight loss and exercise
- stretching, strengthening exercises or resistance training
- water exercise including swimming
Your doctor may suggest you consult an orthopedic surgeon if surgery or other specialist treatment is needed. You might find pain relief with home treatments such as rest, heat or ice, massage or gentle exercises for hip pain.
Steps you can do to lessen hip pain include:
- Try to avoid activities that make pain worse.
- Take over-the-counter pain medication, such as ibuprofen or acetaminophen.
- Sleep on the side of your body that does not have pain. Put a pillow between your legs.
- Lose weight if you are overweight. Ask your health care provider for help.
- Try not to stand for long periods of time. If you must stand, do so on a soft, cushioned surface. Stand with an equal amount of weight on each leg.
- Wear flat shoes that are cushioned and comfortable.
Things you can do to avoid hip pain related to overuse or physical activity include:
- Always warm up before exercising and cool down afterward. Stretch your quadriceps and hamstrings.
- Avoid running straight down hills. Walk down instead.
- Swim instead of run or bicycle.
- Run on a smooth, soft surface, such as a track. Avoid running on cement.
- If you have flat feet, try special shoe inserts and arch supports (orthotics).
- Make sure your running shoes are made well, fit well, and have good cushioning.
- Cut down the amount of exercise you do.
See your doctor or physiotherapist before exercising your hip if you think you may have arthritis or have injured your hip.
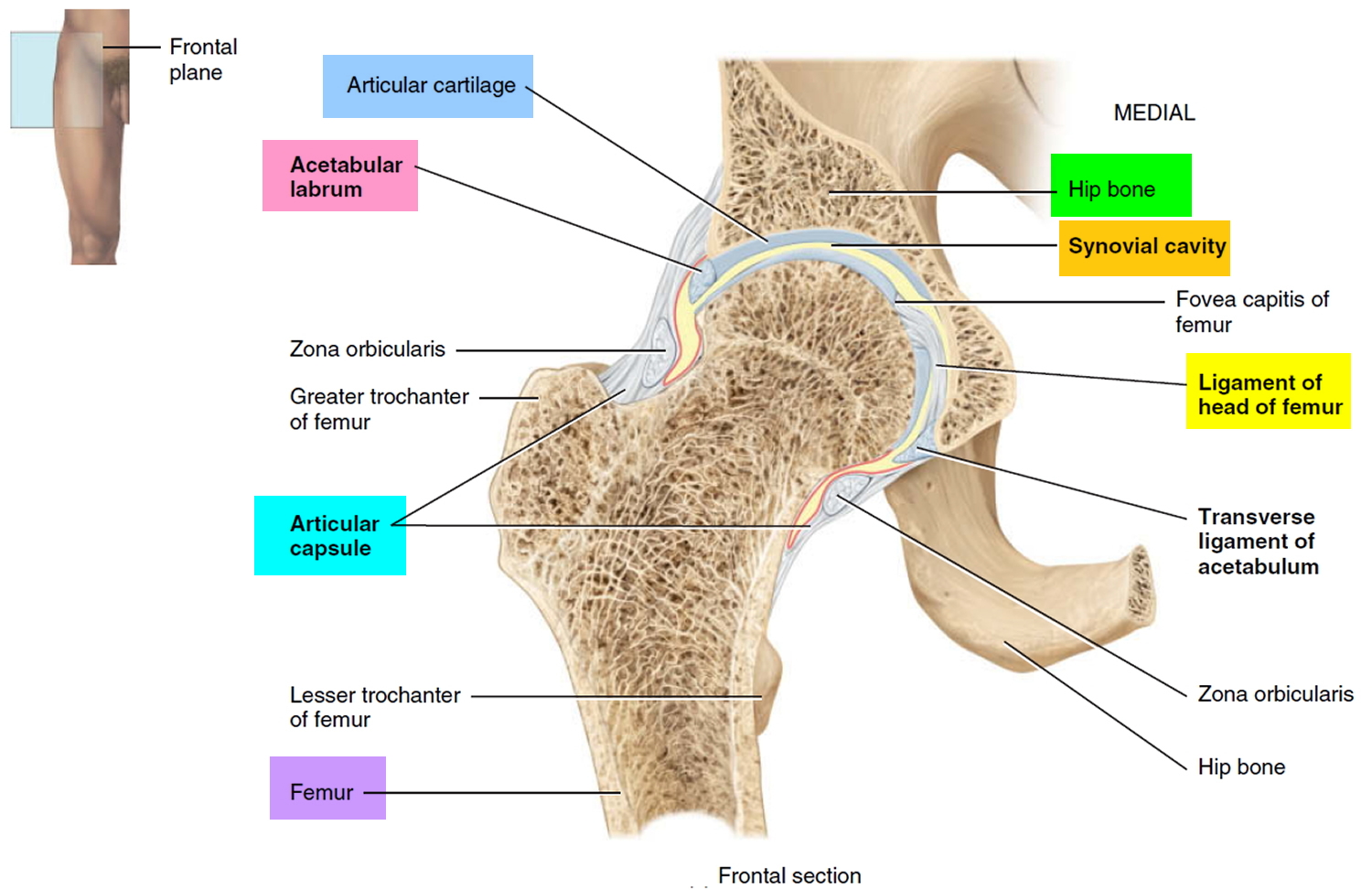
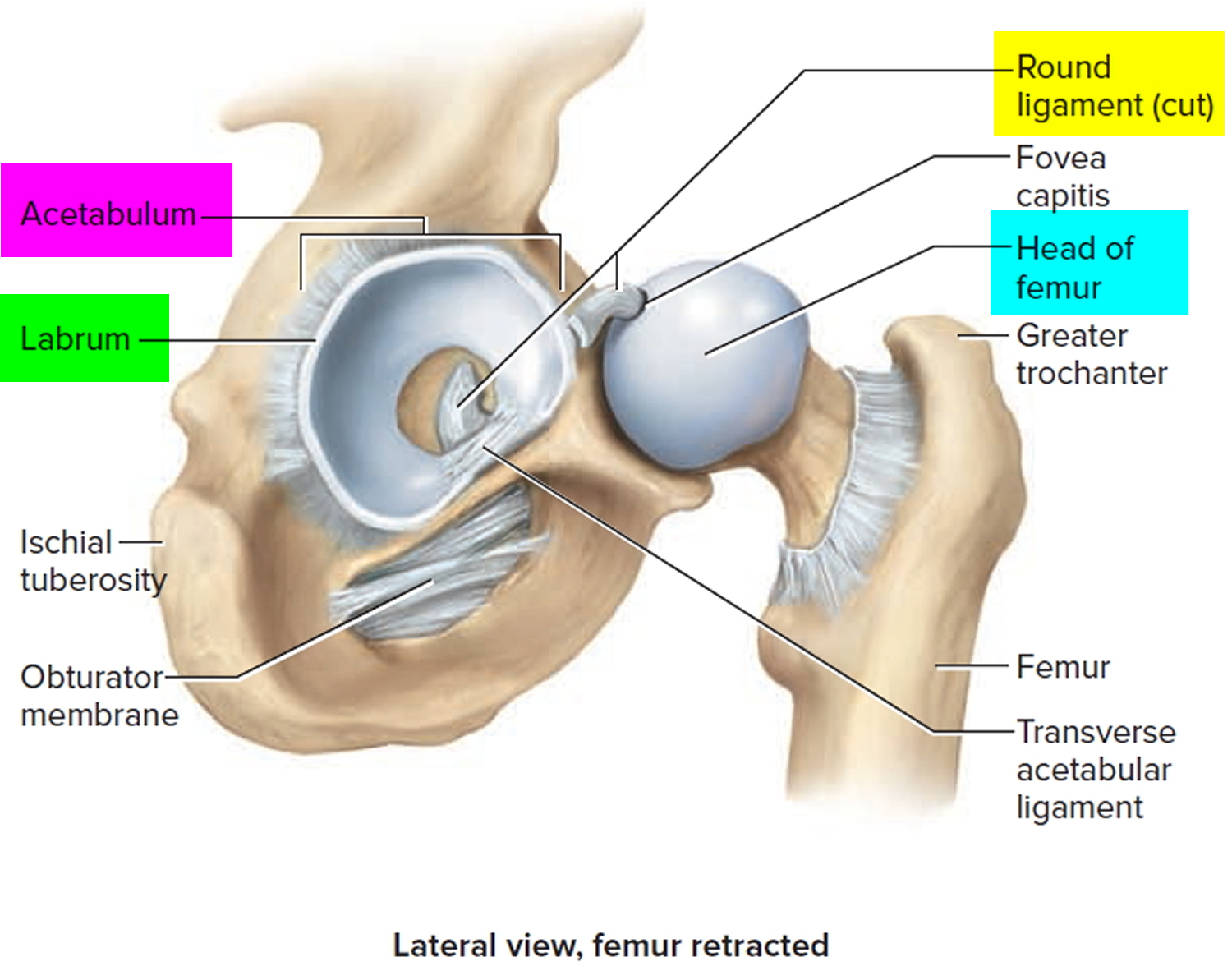
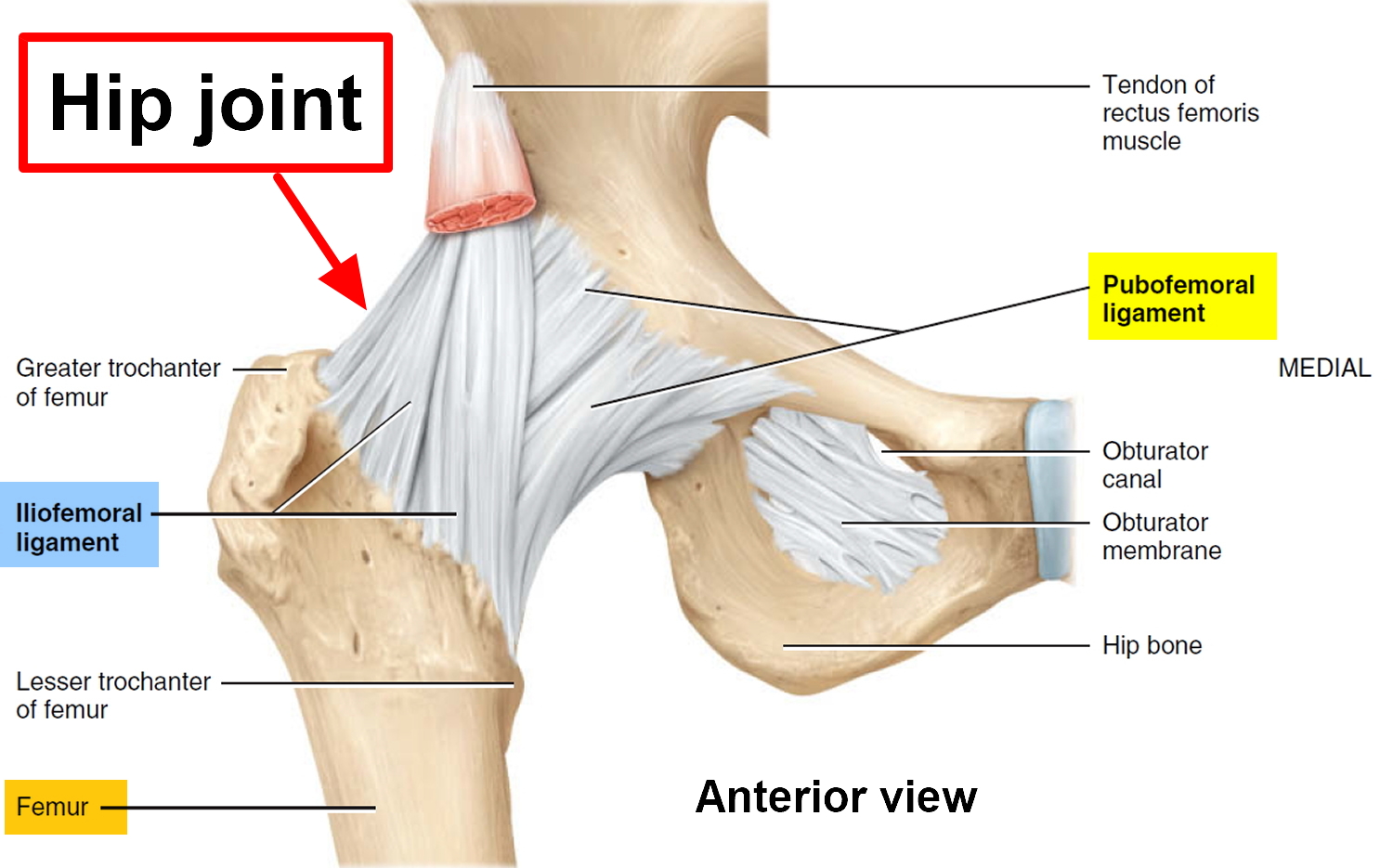
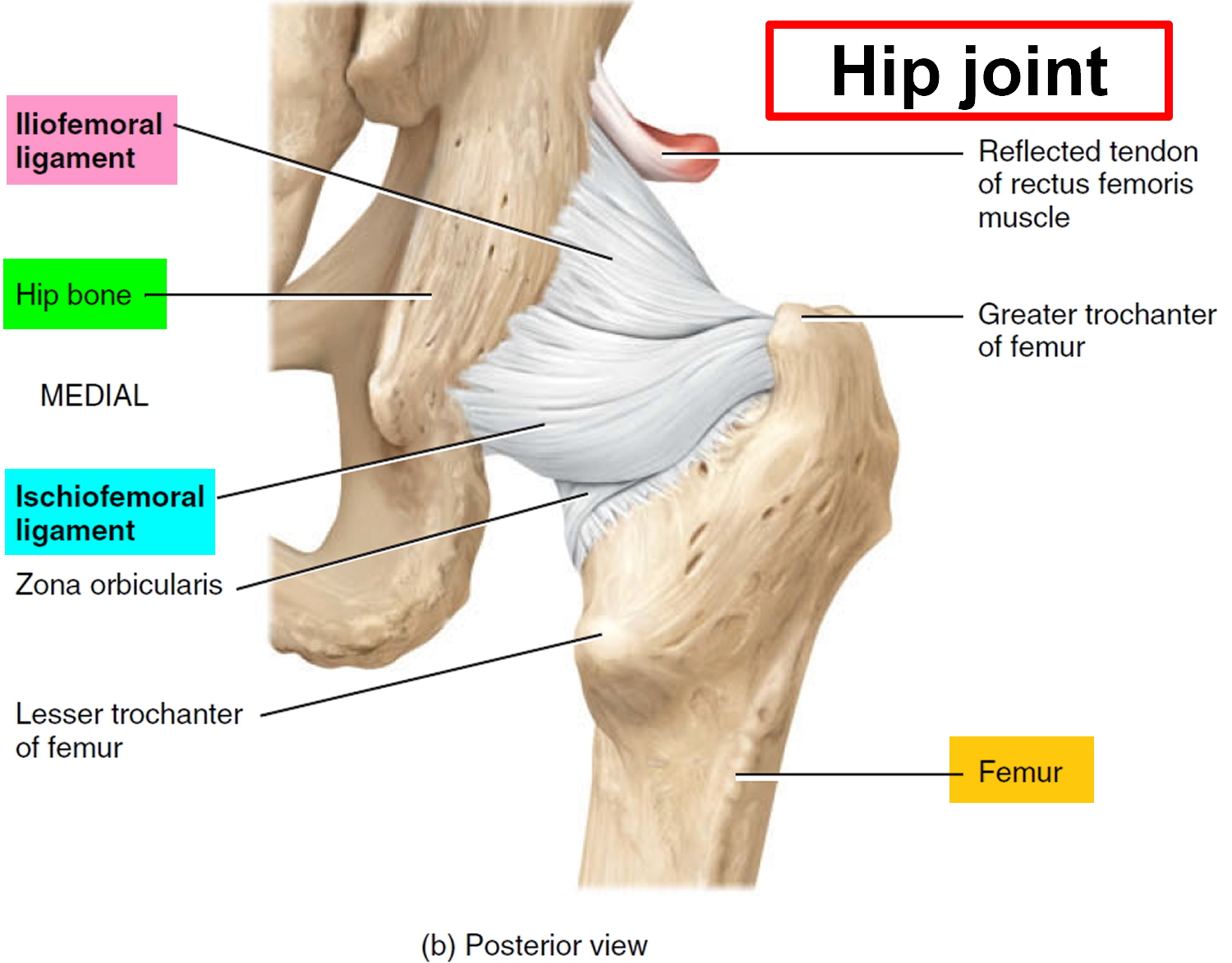
The hip joint anatomy
The hip joint is a ball-and-socket synovial joint designed to allow multiaxial motion while transferring loads between the upper and lower body. The acetabular rim is lined by fibrocartilage (labrum), which adds depth and stability to the femoroacetabular joint. The articular surfaces are covered by hyaline cartilage that dissipates shear and compressive forces during load bearing and hip motion. The hip’s major innervating nerves originate in the lumbosacral region, which can make it difficult to distinguish between primary hip pain and radicular lumbar pain.
The hip joint’s wide range of motion is second only to that of the glenohumeral joint and is enabled by the large number of muscle groups that surround the hip. The flexor muscles include the iliopsoas, rectus femoris, pectineus, and sartorius muscles. The gluteus maximus and hamstring muscle groups allow for hip extension. Smaller muscles, such as gluteus medius and minimus, piriformis, obturator externus and internus, and quadratus femoris muscles, insert around the greater trochanter, allowing for abduction, adduction, and internal and external rotation.
In persons who are skeletally immature, there are several growth centers of the pelvis and femur where injuries can occur. Potential sites of apophyseal injury in the hip region include the ischium, anterior superior iliac spine, anterior inferior iliac spine, iliac crest, lesser trochanter, and greater trochanter. The apophysis of the superior iliac spine matures last and is susceptible to injury up to 25 years of age 2.
Figure 1. Hip joint anatomy
Hip pain causes
The cause of your hip pain will affect when and where you feel the soreness. Usually if the problem is with the hip itself you will feel pain inside your hip or your groin. If the pain is outside your hip, on the upper thigh or outer buttock, the cause will usually be problems with muscles, ligaments or tendons around the hip joint. Hip pain may be caused by arthritis, injuries or other problems.
Conditions that cause hip pain include:
- Arthritis of the hip from a variety of causes – osteoarthritis (disease causing the breakdown of joints) is the most common, especially in people older than 50
- Juvenile idiopathic arthritis (formerly known as juvenile rheumatoid arthritis)
- Psoriatic arthritis
- Rheumatoid arthritis (inflammatory joint disease)
- Injuries
- Dislocation
- Hip fracture
- Hip labral tear
- Lower back problems
- A fracture of the neck (top) of the femur (thigh bone)
- A strained muscle
- An inflamed tendon or other inflammatory conditions
- Bursitis (joint inflammation)
- An infection or septic arthritis
- Pinched nerves
- Meralgia paresthetica
- Sacroiliitis
- Sciatica
- Inguinal hernia
- Sprains and strains
- Tendinitis
- Cancer
- Advanced (metastatic) cancer that has spread to the bones
- Bone cancer
- Leukemia
- Other problems
- Avascular necrosis (death of bone tissue due to limited blood flow)
- Legg-Calve-Perthes disease (in children)
- Osteomyelitis (a bone infection)
- Osteoporosis
- Synovitis
Hip pain may be caused by problems in the bones or cartilage of your hip, including:
- Hip fractures — can cause sudden and acute hip pain. These injuries can be serious and lead to major problems.
- Hip fractures are more common as people get older because falls are more likely and your bones become weaker.
- Infection in the bones or joints.
- Osteonecrosis of the hip (necrosis from loss of blood supply to the bone).
- Arthritis — often felt in the front part of the thigh or groin.
- Labral tear of the hip.
Pain in or around the hip may also be caused by problems such as:
- Bursitis — pain when getting up from a chair, walking, climbing stairs, and driving
- Hamstring strain
- Iliotibial band syndrome — an inflamed ligament in the thigh, often caused by too much running. This is treated with rest.
- Hip flexor strain
- Hip impingement syndrome
- Groin strain
- Snapping hip syndrome
Pain you feel in the hip may reflect a problem in your back, rather than in the hip itself.
Table 1. Causes of Hip Pain
| Diagnosis | Pain characteristics | History/risk factors | Examination findings | Additional testing |
|---|---|---|---|---|
Front thigh pain | ||||
Meralgia paresthetica | Paresthesia, hypesthesia | Obesity, pregnancy, tight pants or belt, conditions with increased intra-abdominal pressure | Anterior thigh hypesthesia, dysesthesia | None |
Front groin pain | ||||
Athletic pubalgia (sports hernia) | Dull, diffuse pain radiating to inner thigh; pain with direct pressure, sneezing, sit-ups, kicking, Valsalva maneuver | Soccer, rugby, football, hockey players | No hernia, tenderness of the inguinal canal or pubic tubercle, adductor origin, pain with resisted sit-up or hip flexion | Radiography: No bony involvement |
MRI: Can show tear or detachment of the rectus abdominis or adductor longus | ||||
Anterolateral hip and groin pain (C sign) — Patients often localize pain by cupping the front and outer hip with the thumb and forefinger in the shape of a “C.” | ||||
Femoral neck fracture/stress fracture | Deep, referred pain; pain with weight bearing | Females (especially with female athlete triad), endurance athletes, low aerobic fitness, steroid use, smokers | Painful ROM, pain on palpation of greater trochanter | Radiography: Cortical disruption |
MRI: Early bony edema | ||||
Femoroacetabular impingement | Deep, referred pain; pain with standing after prolonged sitting | Pain with getting in and out of a car | FADIR and FABER tests are sensitive | Radiography: Cam or pincer deformity, acetabular retroversion, coxa profunda |
Hip labral tear | Dull or sharp, referred pain; pain with weight bearing | Mechanical symptoms, such as catching or painful clicking; history of hip dislocation | Trendelenburg or antalgic gait, loss of internal rotation, positive FADIR and FABER tests | MRI: Can show a labral tear |
Magnetic resonance arthrography: offers added sensitivity and specificity | ||||
Iliopsoas bursitis (internal snapping hip) | Deep, referred pain; intermittent catching, snapping, or popping | Ballet dancers, runners | Snap with FABER to extension, adduction, and internal rotation; reproduction of snapping with extension of hip from flexed position | Radiography: No bony involvement |
MRI: Bursitis and edema of the iliotibial band | ||||
Ultrasonography: Tendinopathy, bursitis, fluid around tendon | ||||
Dynamic ultrasonography: Snapping of iliopsoas or iliotibial band over greater trochanter | ||||
Legg-Calvé-Perthes disease | Deep, referred pain; pain with weight bearing | 2 to 12 years of age, male predominance | Antalgic gait, limited ROM or stiffness | Radiography: Early small femoral epiphysis, sclerosis and flattening of the femoral head |
Loose bodies and chondral lesions | Deep, referred pain; painful clicking | Mechanical symptoms, history of hip dislocation or low-energy trauma, history of Legg-Calvé-Perthes disease | Limited ROM, catching and grinding with provocative maneuvers, positive FADIR and FABER tests | Radiography: Can show ossified or osteochondral loose bodies |
MRI: Can detect chondral and fibrous loose bodies | ||||
Osteoarthritis of the hip | Deep, aching pain and stiffness; pain with weight bearing | Older than 50 years, pain with activity that is relieved with rest | Internal rotation < 15 degrees, flexion < 115 degrees | Radiography: Presence of osteophytes at the acetabular joint margin, asymmetrical joint-space narrowing, subchondral sclerosis and cyst formation |
Osteonecrosis of the hip | Deep, referred pain; pain with weight bearing | Adults: Lupus, sickle cell disease, human immunodeficiency virus infection, corticosteroid use, smoking, and alcohol use; insidious onset, but can be acute with history of trauma | Pain on ambulation, positive log roll test, gradual limitation of ROM | Radiography: Femoral head lucency and subchondral sclerosis, subchondral collapse (i.e., crescent sign), flattening of the femoral head |
MRI: Bony edema, subchondral collapse | ||||
Slipped capital femoral epiphysis | Deep, referred pain; pain with weight bearing | 11 to 14 years of age, overweight (80th to 100th percentile) | Antalgic gait with foot externally rotated on occasion, positive log roll and straight leg raise against resistance tests, pain with hip internal rotation relieved with external rotation | Radiography: Widened epiphysis early, slippage of femur under epiphysis later |
Septic arthritis | Refusal to bear weight, pain with leg movement | Children: 3 to 8 years of age, fever, ill appearance Adults: Older than 80 years, diabetes mellitus, rheumatoid arthritis, recent joint surgery, hip or knee prostheses | Guarding against any ROM; pain with passive ROM | Hip aspiration guided by fluoroscopy, computed tomography, or ultrasonography; Gram stain and culture of joint aspirate |
MRI: Useful for differentiating septic arthritis from transient synovitis | ||||
Transient synovitis | Refusal to bear weight | Children: 3 to 8 years of age, sometimes fever and ill appearance | Pain with extremes of ROM | |
Outer hip pain | ||||
External snapping hip* | Pain with direct pressure, radiation down lateral thigh, snapping or popping | All age groups, audible snap with ambulation | Positive Ober test, snap with Ober test, pain over greater trochanter | Radiography: No bony involvement |
MRI: Bursitis and edema of the iliotibial band | ||||
Ultrasonography: Tendinopathy, bursitis, fluid around tendon | ||||
Greater trochanteric bursitis* | Pain with direct pressure, radiation down lateral thigh | Runners, middle-aged women | Pain over greater trochanter | Dynamic ultrasonography: Snapping of iliopsoas or iliotibial band over greater trochanter |
Greater trochanteric pain syndrome | Pain with direct pressure, radiation down lateral thigh | Associated with knee osteoarthritis, increased body mass index, low back pain; female predominance | Proximal iliotibial band tenderness, Trendelenburg gait is sensitive and specific | |
Posterolateral hip pain (back and outer hip pain) | ||||
Gluteal muscle tear or avulsion* | Pain with direct pressure, radiation down lateral thigh and buttock | Middle-aged women | Weak hip abduction, pain with resisted external rotation, Trendelenburg gait is sensitive and specific | MRI: Gluteal muscle edema or tears |
Iliac crest apophysis avulsion | Tenderness to direct palpation | History of direct trauma, skeletal immaturity (younger than 25 years) | Iliac crest tenderness and/or ecchymosis | Radiography: Apophysis widening, soft tissue swelling around iliac crest |
Back of hip pain | ||||
Hamstring muscle strain or avulsion | Buttock pain, pain with direct pressure | Eccentric muscle contraction while hip flexed and leg extended Skeletal immaturity, eccentric muscle contraction (cutting, kicking, jumping) | Ischial tuberosity tenderness, ecchymosis, weakness to leg flexion, palpable gap in hamstring | Radiography: Avulsion or strain of hamstring attachment to ischium |
Ischial apophysis avulsion | Buttock pain, pain with direct pressure | MRI: Hamstring edema and retraction | ||
Ischiofemoral impingement | Buttock or back pain with posterior thigh radiation, sciatica symptoms | Groin and/or buttock pain that may radiate distally | None established | MRI: Soft tissue edema around quadratus femoris muscle |
Piriformis syndrome | Buttock pain with posterior thigh radiation, sciatica symptoms | History of direct trauma to buttock or pain with sitting, weakness and numbness are rare compared with lumbar radicular symptoms | Positive log roll test, tenderness over the sciatic notch | MRI: Lumbar spine has no disk herniation, piriformis muscle atrophy or hypertrophy, edema surrounding the sciatic nerve |
Sacroiliac joint dysfunction | Pain radiates to lumbar back, buttock, and groin | Female predominance, common in pregnancy, history of minor trauma | FABER test elicits posterior pain localized to the sacroiliac joint, sacroiliac joint line tenderness | Radiography: Possibly no findings, narrowing and sclerotic changes of the sacroiliac joint space |
Footnote: *—Conditions associated with greater trochanteric pain syndrome.
Abbreviations: FABER = flexion, abduction, external rotation; FADIR = flexion, adduction, internal rotation; MRI = magnetic resonance imaging; ROM = range of motion.
[Source 1 ]Front Hip Pain
Anterior hip or groin pain suggests involvement of the hip joint itself. Patients often localize pain by cupping the anterolateral hip with the thumb and forefinger in the shape of a “C.” This is known as the C sign (Figure 3A).
Osteoarthritis
Osteoarthritis is the most likely diagnosis in older adults with limited motion and gradual onset of symptoms. Patients have a constant, deep, aching pain and stiffness that are worse with prolonged standing and weight bearing, which can make it difficult to move the affected joints and do certain activities. Osteoarthritis in your hips often causes difficulty moving your hip joints. For example, you may find it difficult to put your shoes and socks on or to get in and out of a car.
The symptoms of osteoarthritis can vary greatly from person to person, but if it affects the hip, it will typically cause:
- mild inflammation of the tissues in and around the hip joint
- damage to cartilage – the strong, flexible tissue that lines the bones
- bony growths (osteophytes) that develop around the edge of the hip joint
This can lead to pain, stiffness and difficulty doing certain activities.
Examination reveals decreased range of motion, and extremes of hip motion often cause pain. Plain radiographs demonstrate the presence of asymmetrical joint-space narrowing, osteophytosis, and subchondral sclerosis and cyst formation 3.
There’s no cure for osteoarthritis, but the symptoms can be eased using a number of different treatments. Surgery isn’t usually necessary.
Femoroacetabular impingement
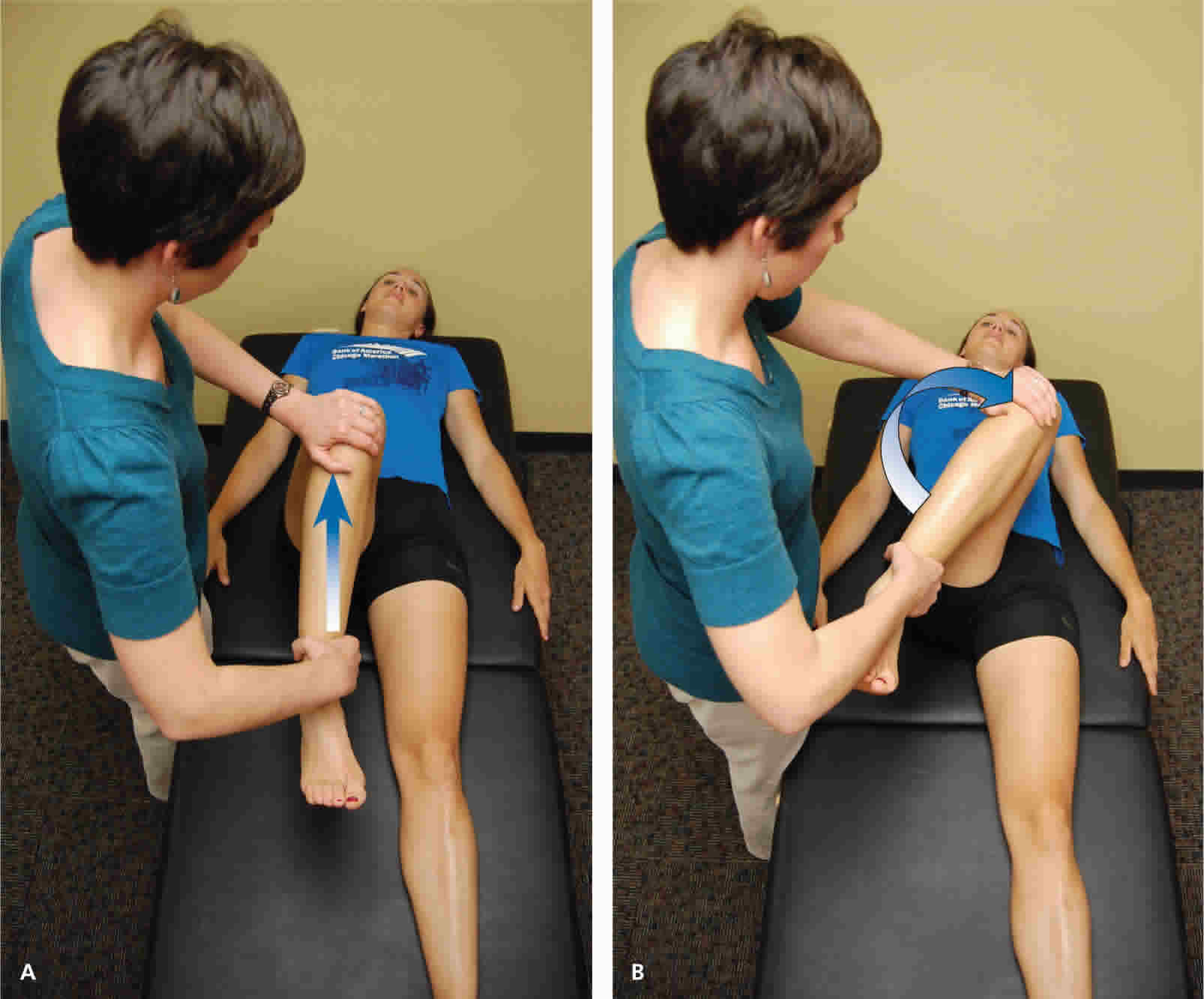
In femoroacetabular impingement, the hip pain is caused by the bones of the hip rubbing together because they’re abnormally shaped. Patients with femoroacetabular impingement are often young and physically active. They describe insidious onset of pain that is worse with sitting, rising from a seat, getting in or out of a car, or leaning forward 4. The pain is located primarily in the groin with occasional radiation to the lateral hip and anterior thigh 5. The FABER test (flexion, abduction, external rotation; Figure 5) has a sensitivity of 96% to 99%. The FADIR test (flexion, adduction, internal rotation; Figure 6), log roll test (Figure 7), and straight leg raise against resistance test (Figure 8) are also effective, with sensitivities of 88%, 56%, and 30%, respectively 5. In addition to the anteroposterior and lateral radiograph views, a Dunn view should be obtained to help detect subtle lesions 6.
Hip labral tear
Hip labral tear is a tear in the ring of cartilage surrounding the socket of the hip joint. Hip labral tears cause dull or sharp groin pain, and one-half of patients with a labral tear have pain that radiates to the lateral hip, anterior thigh, and buttock. The pain usually has an insidious onset, but occasionally begins acutely after a traumatic event. About one-half of patients with this injury also have mechanical symptoms, such as catching or painful clicking with activity 7. The FADIR and FABER tests are effective for detecting intra-articular pathology (the sensitivity is 96% to 75% for the FADIR test and is 88% for the FABER test), although neither test has high specificity 5. Magnetic resonance arthrography is considered the diagnostic test of choice for labral tears 8. However, if a labral tear is not suspected, other less invasive imaging modalities, such as plain radiography and conventional MRI, should be used first to rule out other causes of hip and groin pain.
Iliopsoas bursitis (Internal snapping hip)
Iliopsoas bursitis is an inflammation and swelling of the fluid-filled sac (bursa) over your hip joint. Patients with this condition have anterior hip pain when extending the hip from a flexed position, often associated with intermittent catching, snapping, or popping of the hip 9. Dynamic real-time ultrasonography is particularly useful in evaluating the various forms of snapping hip 10.
You can use the following three steps to help bring down swelling and pain:
- Rest – try not to move the joint too much, and avoid activities that will put pressure on it.
- Ice – gently hold an ice pack (or a bag of frozen peas) wrapped in a tea towel on the area for around 10 minutes at a time and repeat every few hours during the day.
- Elevate – keep the area raised to the level of your heart as much as possible.
Take painkillers, such as paracetamol or ibuprofen, to ease any pain. You may also want to put extra cushions around the affected joint while you sleep to help protect and support it.
If your symptoms don’t get better after basic home treatment your doctor may refer you for further tests, such as:
- blood tests to look for other conditions, like rheumatoid arthritis or gout
- scans to look for other causes, such as damage to the muscles
Occult or stress fracture of the hip
Occult or stress fracture of the hip should be considered if trauma or repetitive weight-bearing exercise is involved, even if plain radiograph results are negative 11. A hip fracture will cause sudden hip pain and is more common in older people with weaker bones. Falls are very common in older people, who may have reduced vision or mobility and balance problems. Hip fractures are also more common in women, who are more susceptible to osteoporosis (weak and fragile bones). Clinically, these injuries cause anterior hip or groin pain that is worse with activity.
Symptoms of a hip fracture after a fall may include:
- hip pain
- not being able to lift, move or rotate (turn) your leg
- being unable to stand or put weight on your leg
- bruising and swelling around the hip area
- a shorter leg on the injured side
- your leg turning outwards more on the injured side
A hip fracture won’t necessarily cause bruising or prevent you from standing or walking.
Pain may be present with extremes of motion, active straight leg raise, the log roll test, or hopping 12. MRI is useful for the detection of occult traumatic fractures and stress fractures not seen on plain radiographs 13.
Transient synovitis and septic arthritis
Acute onset of atraumatic anterior hip pain that results in impaired weight bearing should raise suspicion for transient synovitis and septic arthritis (infection in the hip joint). Risk factors for septic arthritis in adults include age older than 80 years, diabetes mellitus, rheumatoid arthritis, recent joint surgery, and hip or knee prostheses 14. Septic arthritis is inflammation of a joint caused by a bacterial infection. It’s also known as infectious or bacterial arthritis. Any joint can be affected by septic arthritis, but it’s most common in the knees and hips. More than one joint can be affected at the same time.
Symptoms of septic arthritis:
- Septic arthritis typically causes severe pain, swelling, redness and heat in affected joints. These symptoms tend to develop quickly over a few hours or days.
- You may also have difficulty moving the affected joint, and some people have a high temperature (fever).
- Young children with septic arthritis will generally be irritable and may cry whenever the infected joint is moved – for example, during nappy changing. They may also try to avoid using or putting any weight on affected joints.
Fever, complete blood count, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level should be used to evaluate the risk of septic arthritis 15. MRI is useful for differentiating septic arthritis from transient synovitis 16. However, hip aspiration using guided imaging such as fluoroscopy, computed tomography, or ultrasonography is recommended if a septic joint is suspected 17.
Osteonecrosis
Osteonecrosis of the hip is death of the hip bone tissue due to a lack of blood supply to the hip joint. Legg-Calvé-Perthes disease is an idiopathic osteonecrosis of the femoral head in children two to 12 years of age, with a male-to-female ratio of 4:1 18. In adults, risk factors for osteonecrosis include systemic lupus erythematosus, sickle cell disease, human immunodeficiency virus infection, smoking, alcoholism, and corticosteroid use 19. Pain is the presenting symptom and is usually insidious. Range of motion is initially preserved but can become limited and painful as the disease progresses 20. MRI is valuable in the diagnosis and prognostication of osteonecrosis of the femoral head 21.
Back of Hip and Buttock Pain
Piriformis syndrome and Ischiofemoral impingement
Piriformis syndrome causes buttock pain that is aggravated by sitting or walking, with or without ipsilateral radiation down the posterior thigh from sciatic nerve compression 22. Pain with the log roll test is the most sensitive test, but tenderness with palpation of the sciatic notch can help with the diagnosis 23.
Ischiofemoral impingement is a less well-understood condition that can lead to nonspecific buttock pain with radiation to the posterior thigh 24. This condition is thought to be a result of impingement of the quadratus femoris muscle between the lesser trochanter and the ischium.
Unlike sciatica from disc herniation, piriformis syndrome and ischiofemoral impingement are exacerbated by active external hip rotation. MRI is useful for diagnosing these conditions 25.
Other causes of posterior hip pain
Other causes of posterior hip pain include sacroiliac joint dysfunction 26, lumbar radiculopathy 27 and vascular claudication 28. The presence of a limp, groin pain, and limited internal rotation of the hip is more predictive of hip disorders than disorders originating from the low back 29.
Outer Hip Pain
Greater trochanteric pain syndrome
Lateral hip pain affects 10% to 25% of the general population 30. Greater trochanteric pain syndrome refers to pain over the greater trochanter. Several disorders of the lateral hip can lead to this type of pain, including iliotibial band thickening, bursitis, and tears of the gluteus medius and minimus muscle attachment 31. Patients may have mild morning stiffness and may be unable to sleep on the affected side. Gluteus minimus and medius injuries present with pain in the posterior lateral aspect of the hip as a result of partial or full-thickness tearing at the gluteal insertion. Most patients have an atraumatic, insidious onset of symptoms from repetitive use 32.
Hip pain symptoms
You might have soreness inside the hip joint but you may also feel pain in your:
- buttock
- lower back
- thigh
- groin
- knee
Sometimes pain from other areas can be felt in your hip – this is called ‘referred pain’. Pain in the hip can affect you when you:
- walk up or down stairs
- sit or stand for some time
- exercise or play sport
Hip pain diagnosis
A doctor or physiotherapist can work out what is causing the pain in your hip. They might talk to you and examine you, checking how you stand, how you walk and what movements cause pain. They may suggest blood tests or X-rays.
Medical history
Age alone can narrow the differential diagnosis of hip pain. In prepubescent and adolescent patients, congenital malformations of the femoroacetabular joint, avulsion fractures, and apophyseal or epiphyseal injuries should be considered. In those who are skeletally mature, hip pain is often a result of musculotendinous strain, ligamentous sprain, contusion, or bursitis. In older adults, degenerative osteoarthritis and fractures should be considered first.
Patients with hip pain should be asked about antecedent trauma or inciting activity, factors that increase or decrease the pain, mechanism of injury, and time of onset. Questions related to hip function, such as the ease of getting in and out of a car, putting on shoes, running, walking, and going up and down stairs, can be helpful 33. Location of the pain is informative because hip pain often localizes to one of three basic anatomic regions: the anterior hip and groin, posterior hip and buttock, and lateral hip (see Figure 2).
Physical examination
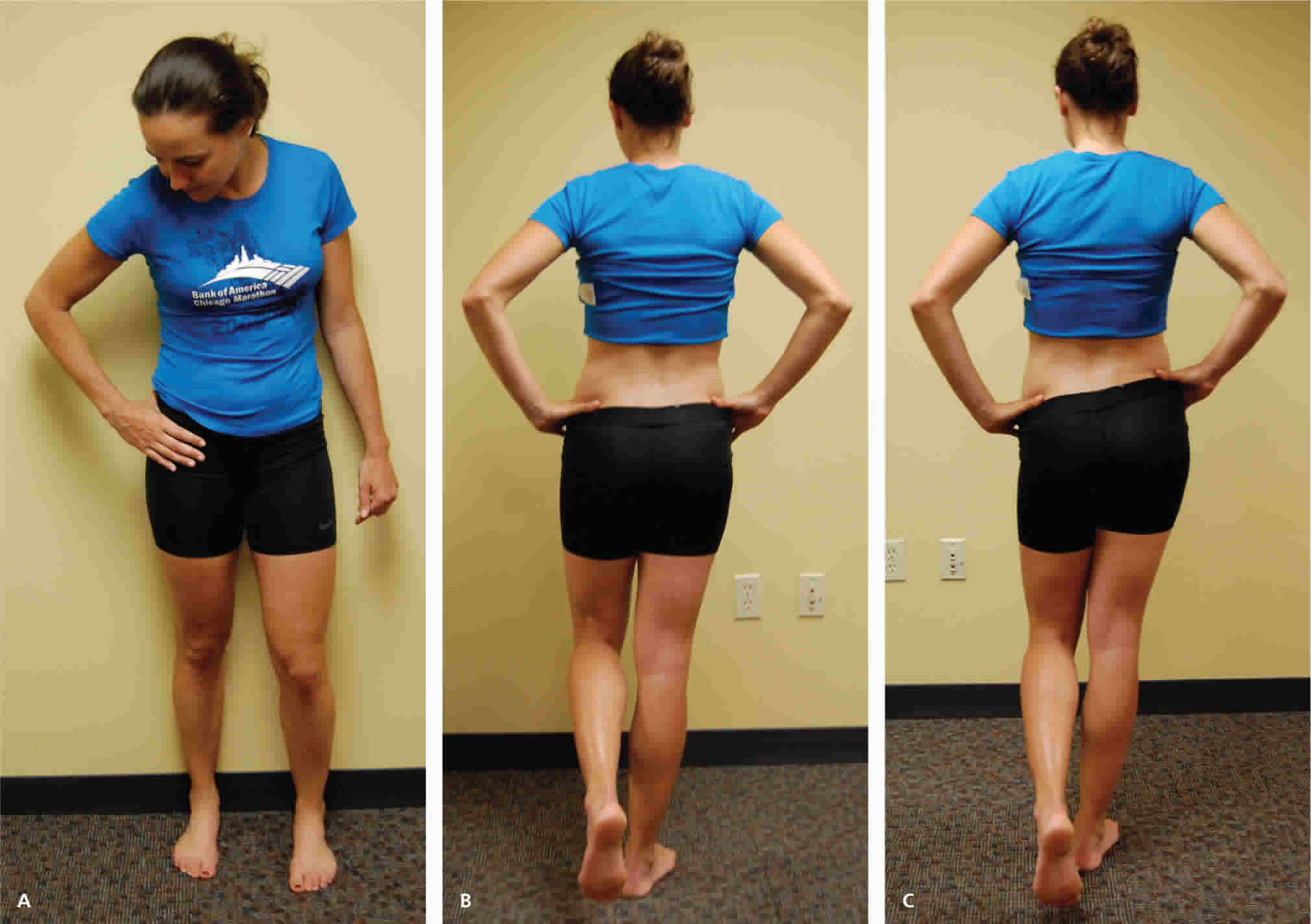
The hip examination should evaluate the hip, back, abdomen, and vascular and neurologic systems. It should start with a gait analysis and stance assessment, followed by evaluation of the patient in seated, supine, lateral, and prone positions. Physical examination tests for the evaluation of hip pain are summarized in Table 2.
Table 2. Physical Examination Tests for the Evaluation of Hip Pain
| Test | Other names | Positioning | Positive findings | Differential diagnosis |
|---|---|---|---|---|
Gait testing (C sign, Figure 3A; gait analysis, Figure 3B) | — | Standing | Antalgic gait, Trendelenburg gait, pelvic wink (rotation of more than 40 degrees in the axial plane toward the affected hip when terminally extending the hip), excessive pronation or supination of the ankles, and limps caused by differing leg lengths | Hip labral tear, transient synovitis, Legg-Calvé-Perthes disease, SCFE |
Modified Trendelenburg test (Figure 3C) | Single leg stance phase | Standing | 2-cm drop in the level of the iliac crest, indicating weakness on the contralateral side | Hip labral tear, transient synovitis, Legg-Calvé-Perthes disease, SCFE |
ROM testing (Figure 4) | — | Supine, lateral, or sitting | Pain with passive ROM, limited ROM | Pain with passive ROM: Transient synovitis, septic arthritis |
Limited ROM: Loose bodies, chondral lesions, osteoarthritis, Legg-Calvé-Perthes disease, osteonecrosis | ||||
FABER test (Figure 5) | Patrick test | Supine | Posterior pain localized to the sacroiliac joint, lumbar spine, or posterior hip; groin pain with the test is sensitive for intra-articular pathology | Hip labral tear, loose bodies, chondral lesions, femoral acetabular impingement, osteoarthritis, sacroiliac joint dysfunction, iliopsoas bursitis |
FADIR test (Figure 6) | Impingement test | Supine | Pain | Hip labral tear, loose bodies, chondral lesions, femoral acetabular impingement |
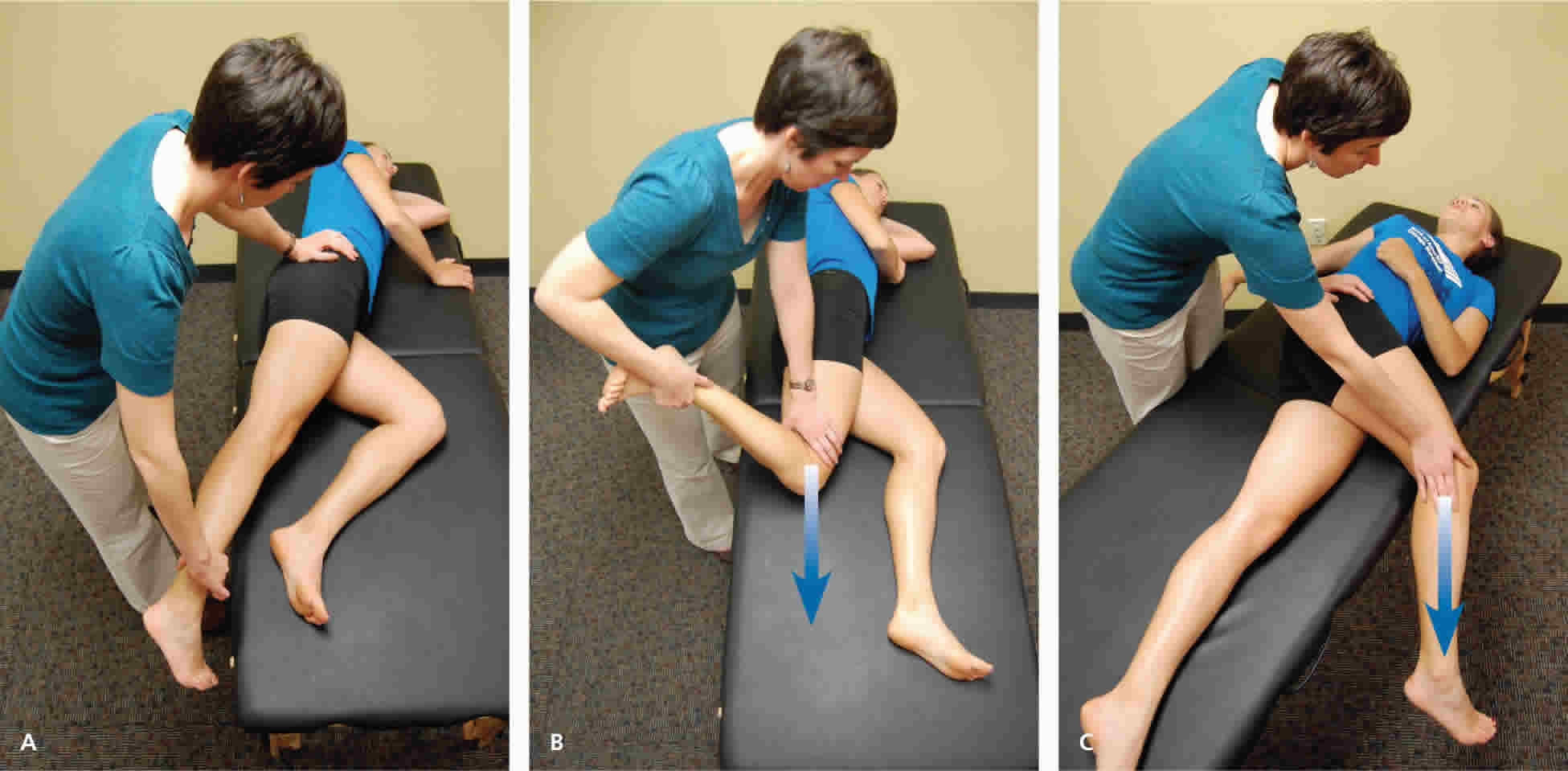
Log roll test (Figure 7) | Passive supine rotation, Freiberg test | Supine | Restricted movement, pain | Piriformis syndrome, SCFE |
Straight leg raise against resistance test (Figure 8) | Stinchfield test | Supine | Weakness to resistance, pain | Athletic pubalgia (sports hernia), SCFE, femoral acetabular impingement |
Ober test (Figure 9) | Passive adduction | Lateral | Passive adduction past midline cannot be achieved | External snapping hip, greater trochanteric pain syndrome |
Abbreviations: FABER = flexion, abduction, external rotation; FADIR = flexion, adduction, internal rotation; ROM = range of motion; SCFE = slipped capital femoral epiphysis.
[Source 1 ]Figure 3. Hip pain – gait testing
Footnote: Gait testing. (A) C sign. Patients often localize pain by cupping the anterolateral hip with the thumb and forefinger in the shape of a “C.” (B) Gait analysis. The patient is observed while walking to evaluate for limp or antalgic gait characteristics. (C) Modified Trendelenburg test (single leg stance phase). The patient stands with feet shoulder width apart and lifts one leg. The examiner observes for a drop in the level of the iliac crest on the side of the lifted leg.
[Source 1 ]Figure 4. Hip range-of-motion testing
Footnote: (A) Abduction. (B) Adduction. (C) Extension. (D) Internal and external rotation.
[Source 1 ]Figure 5. FABER (flexion, abduction, external rotation) test or Patrick test
Footnote: The examiner moves the leg into 45 degrees of flexion, then (A) externally rotates and (B) abducts the leg so that the ankle rests proximal to the knee of the contralateral leg.
[Source 1 ]Figure 6. FADIR test (flexion, adduction, internal rotation; impingement test)
Footnote: The examiner passively moves the leg into (A) full flexion, then into (B) adduction and internal rotation.
[Source 1 ]Figure 7. Log roll test (passive supine rotation) or Freiberg test
Footnote: Patient’s leg is extended and relaxed on examination table as the examiner internally and externally rotates the leg (log roll).
[Source 1 ]Figure 8. Straight leg raise against resistance test or Stinchfield test
Footnote: The patient lifts the straight leg to 45 degrees while the examiner applies downward force on the thigh.
[Source 1 ]Figure 9. Ober test or passive adduction test
Footnote: The patient is positioned on his or her side, with the unaffected hip on the examination table. The examiner stands behind the patient with one hand on the patient’s hip, and the other hand supporting the lower leg. (A) To evaluate the tensor fasciae latae: The hip and knee are held at 0 degrees of extension and allowed to passively adduct with gravity. (B) The gluteus medius: The hip is held at 0 degrees of extension and 45 to 90 degrees of knee flexion. (C) The gluteus maximus: The shoulders are rotated back toward the table, with the hip in flexion and knee in extension.
[Source 1 ]Imaging tests
Radiography
Radiography of the hip should be performed if there is any suspicion of acute fracture, dislocation, or stress fracture. Initial plain radiography of the hip should include an anteroposterior view of the pelvis and a frog-leg lateral view of the symptomatic hip 18.
Magnetic Resonance Imaging and Arthrography
Conventional magnetic resonance imaging (MRI) of the hip can detect many soft tissue abnormalities, and is the preferred imaging modality if plain radiography does not identify specific pathology in a patient with persistent pain 34. Conventional MRI has a sensitivity of 30% and an accuracy of 36% for diagnosing hip labral tears, whereas magnetic resonance arthrography provides added sensitivity of 90% and accuracy of 91% for the detection of labral tears 35.
Ultrasonography
Ultrasonography is a useful technique for evaluating individual tendons, confirming suspected bursitis, and identifying joint effusions and functional causes of hip pain 10. Ultrasonography is especially useful for safely and accurately performing imaging-guided injections and aspirations around the hip 36. It is ideal for an experienced ultrasonographer to perform the diagnostic study; however, emerging evidence suggests that less experienced clinicians with appropriate training can make diagnoses with reliability similar to that of an experienced musculoskeletal ultrasonographer 37.
Hip pain treatment
You may not need to see a doctor if your hip pain is minor. Try these self-care tips:
- Rest. Avoid repeated bending at the hip and direct pressure on the hip. Try not to sleep on the affected side and avoid prolonged sitting.
- Pain relievers. Over-the-counter pain relievers such as acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve) may help ease your hip pain.
- Ice or heat. Use ice cubes or a bag of frozen vegetables wrapped in a towel to apply cold treatments to your hip. Conversely, a warm bath or shower may help prepare your muscles for stretching exercises that can reduce pain.
If self-care treatments don’t help, make an appointment with your doctor.
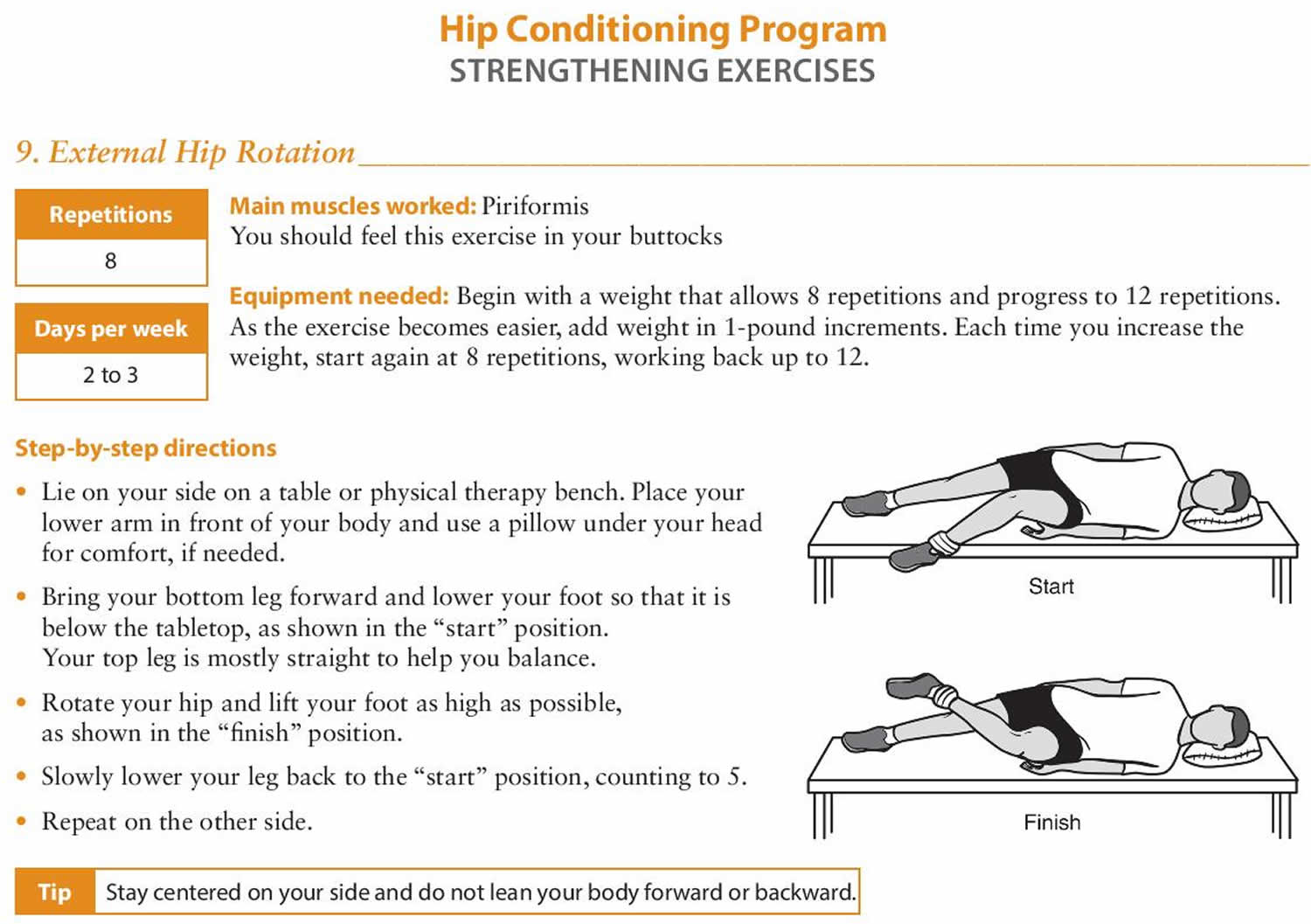
Hip conditioning exercises
This is a general conditioning program that provides a wide range of hip exercises. To ensure that the hip exercise is safe and effective for you, it should be performed under your doctor’s supervision. Talk to your doctor or physical therapist about which exercises will best help you meet your rehabilitation goals.
- Strength exercise: Strengthening the muscles that support your hip will help keep your hip joint stable. Keeping these muscles strong can relieve pain and prevent further injury.
- Flexibility exercise: Stretching the muscles that you strengthen is important for restoring range of motion and preventing injury.
Gently stretching after strengthening exercises can help reduce muscle soreness and keep your muscles long and flexible.
Target Muscles
The muscle groups targeted in this hip conditioning program include:
- Gluteus maximus (buttocks)
- Gluteus medius (buttocks)
- Hamstrings (back of thigh)
- Piriformis (buttocks)
- Adductors (inner thigh)
- Abductors (outer thigh)
- Tensor Fascia (outer thigh)
Performing the exercises two to three days a week will maintain strength and range of motion in your hips and thighs.
- If you are not sure how to do an exercise, or how often to do it, contact your doctor or physical therapist.
Getting Started
- Warm up: Before doing the following exercises, warm up with 5 to 10 minutes of low impact activity, like walking or riding a stationary bicycle.
- Stretch: After the warm-up, do the stretching exercises shown on Page 1 before moving on to the strengthening exercises. When you have completed the strengthening exercises, repeat the stretching exercises to end the program.
- Do not ignore pain: You should not feel pain during an exercise. Talk to your doctor or physical therapist if you have any pain while exercising.
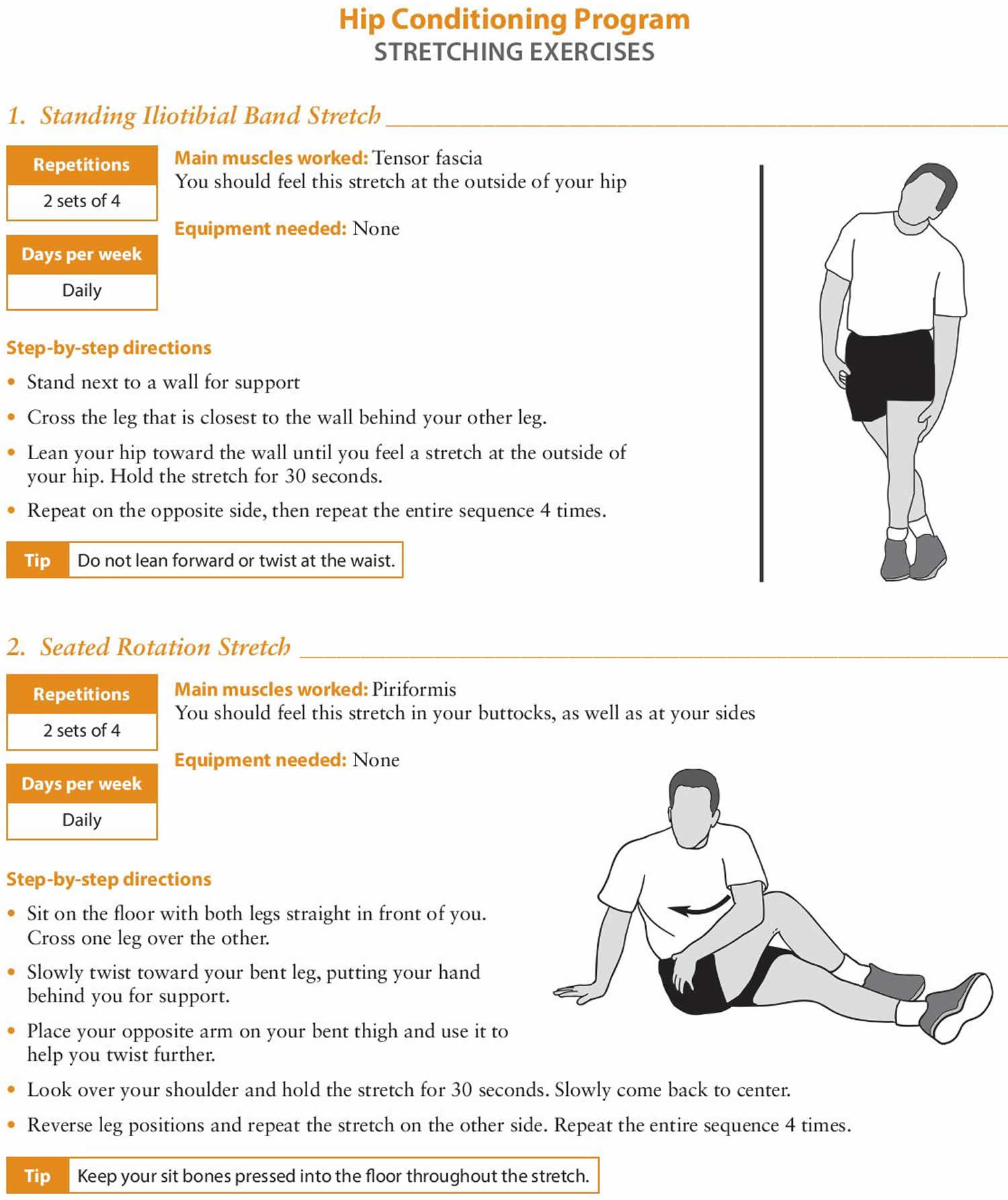
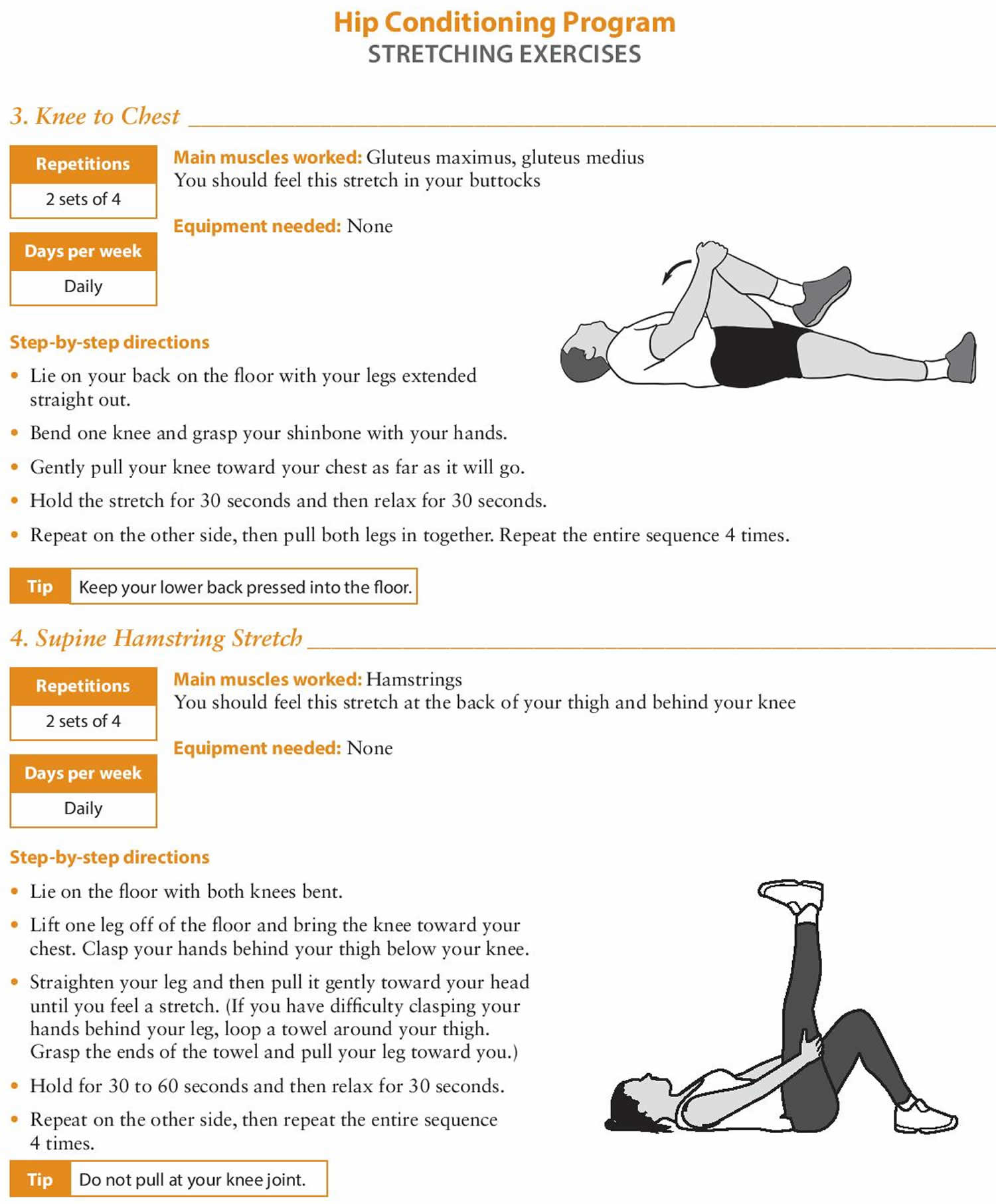
Figure 10. Hip stretching exercises
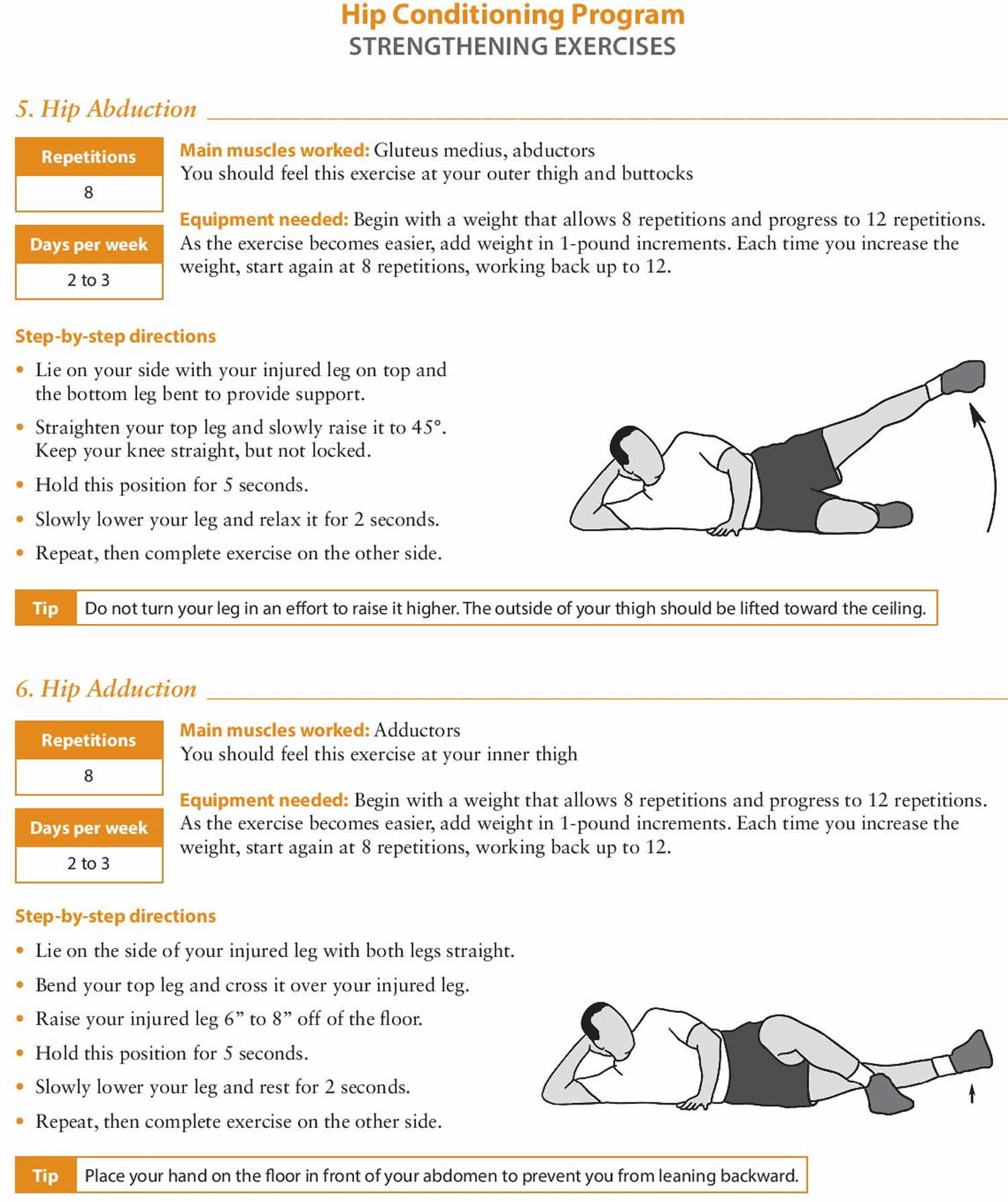
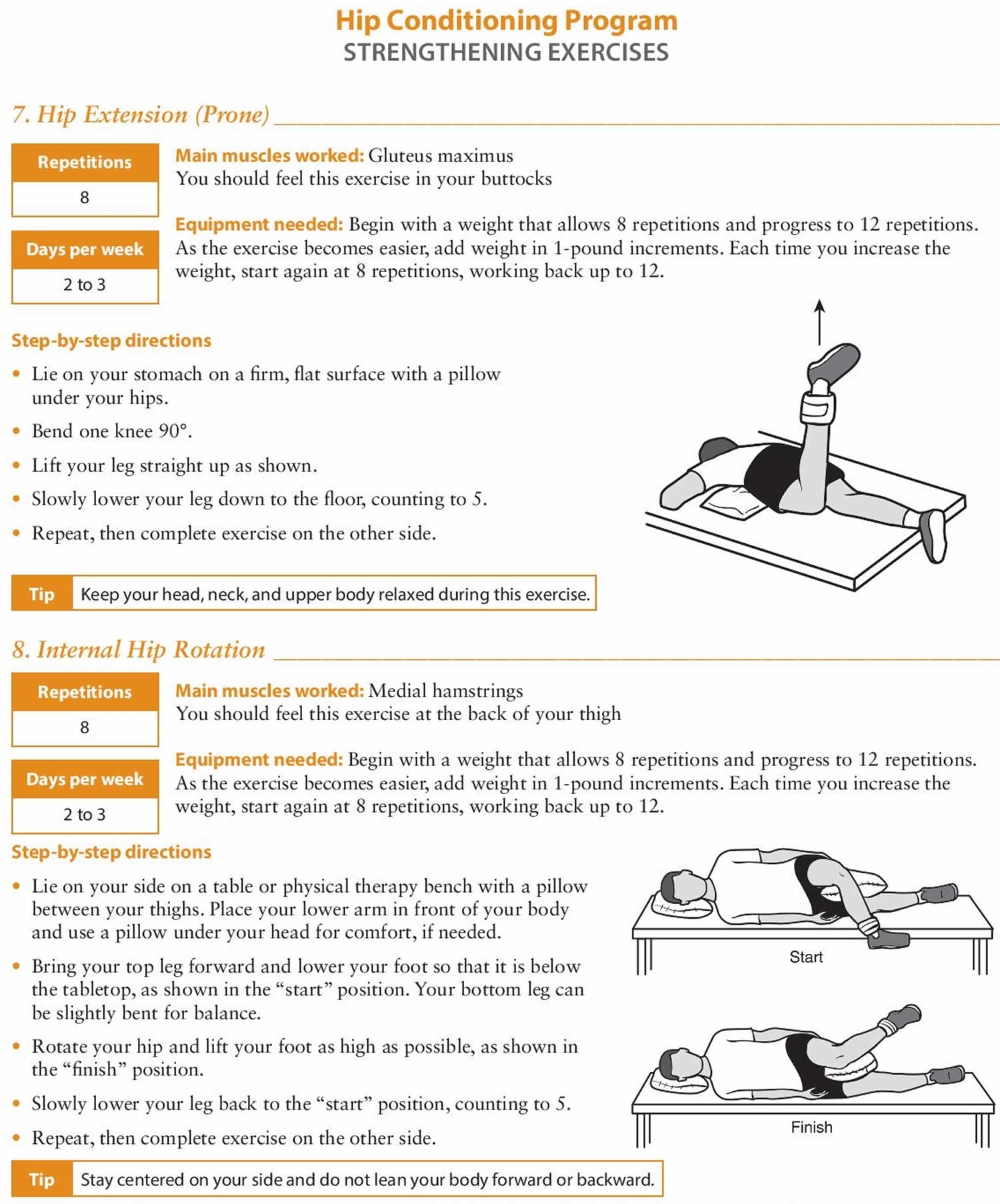
Figure 11. Hip strengthening exercises
- Evaluation of the Patient with Hip Pain. Am Fam Physician. 2014 Jan 1;89(1):27-34. https://www.aafp.org/afp/2014/0101/p27.html[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Rossi F, Dragoni S. Acute avulsion fractures of the pelvis in adolescent competitive athletes. Skeletal Radiol. 2001;30(3):127–131.[↩]
- Altman R, Alarcón G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34(5):505–514.[↩]
- Banerjee P, McLean CR. Femoroacetabular impingement. Curr Rev Musculoskelet Med. 2011;4(1):23–32.[↩]
- Clohisy JC, Knaus ER, Hunt DM, et al. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467(3):638–644.[↩][↩][↩]
- Beall DP, Sweet CF, Martin HD, et al. Imaging findings of femoroacetabular impingement syndrome. Skeletal Radiol. 2005;34(11):691–701.[↩]
- Burnett RS, Della Rocca GJ, Prather H, et al. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006;88(7):1448–1457.[↩]
- Groh MM, Herrera J. A comprehensive review of hip labral tears. Curr Rev Musculoskelet Med. 2009;2(2):105–117.[↩]
- Blankenbaker DG, De Smet AA, Keene JS. Sonography of the iliopsoas tendon and injection of the iliopsoas bursa for diagnosis and management of the painful snapping hip. Skeletal Radiol. 2006;35(8):565–571.[↩]
- Deslandes M, Guillin R, Cardinal E, et al. The snapping iliopsoas tendon: new mechanisms using dynamic sonography. AJR Am J Roentgenol. 2008;190(3):576–581.[↩][↩]
- Egol KA, Koval KJ, Kummer F, et al. Stress fractures of the femoral neck. Clin Orthop Relat Res. 1998;(348):72–78.[↩]
- Fullerton LR Jr, Snowdy HA. Femoral neck stress fractures. Am J Sports Med. 1988;16(4):365–377.[↩]
- Newberg AH, Newman JS. Imaging the painful hip. Clin Orthop Relat Res. 2003;(406):19–28.[↩]
- Margaretten ME, Kohlwes J, Moore D, et al. Does this adult patient have septic arthritis? JAMA. 2007;297(13):1478–1488.[↩]
- Eich GF, Superti-Furga A, Umbricht FS, et al. The painful hip: evaluation of criteria for clinical decision-making. Eur J Pediatr. 1999;158(11):923–928.[↩]
- Learch TJ, Farooki S. Magnetic resonance imaging of septic arthritis. Clin Imaging. 2000;24(4):236–242.[↩]
- Leopold SS, Battista V, Oliverio JA. Safety and efficacy of intraarticular hip injection using anatomic landmarks. Clin Orthop Relat Res. 2001; (391):192–197.[↩]
- Gough-Palmer A, McHugh K. Investigating hip pain in a well child. BMJ. 2007;334(7605):1216–1217.[↩][↩]
- Mont MA, Zywiel MG, Marker DR, et al. The natural history of untreated asymptomatic osteonecrosis of the femoral head. J Bone Joint Surg Am. 2010;92(12):2165–2170.[↩]
- Assouline-Dayan Y, Chang C, Greenspan A, et al. Pathogenesis and natural history of osteonecrosis. Semin Arthritis Rheum. 2002;32(2):94–124.[↩]
- Mitchell DG, Rao VM, Dalinka MK, et al. Femoral head avascular necrosis: correlation of MR imaging, radiographic staging, radionuclide imaging, and clinical findings. Radiology. 1987;162(3):709–715.[↩]
- Kirschner JS, Foye PM, Cole JL. Piriformis syndrome, diagnosis and treatment. Muscle Nerve. 2009;40(1):10–18.[↩]
- Hopayian K, Song F, Riera R, et al. The clinical features of the piriformis syndrome. Eur Spine J. 2010;19(12):2095–2109.[↩]
- Ali AM, Whitwell D, Ostlere SJ. Case report: imaging and surgical treatment of a snapping hip due to ischiofemoral impingement. Skeletal Radiol. 2011;40(5):653–656.[↩]
- Lee EY, Margherita AJ, Gierada DS, et al. MRI of piriformis syndrome. AJR Am J Roentgenol. 2004;183(1):63–64.[↩]
- Slipman CW, Jackson HB, Lipetz JS, et al. Sacroiliac joint pain referral zones. Arch Phys Med Rehabil. 2000;81(3):334–338.[↩]
- Moore KL, Dalley AF, Agur AM. Clinically Oriented Anatomy. 6th ed. Philadelphia, Pa.: Lippincott Williams & Wilkins; 2010.[↩]
- Adlakha S, Burket M, Cooper C. Percutaneous intervention for chronic total occlusion of the internal iliac artery for unrelenting buttock claudication. Catheter Cardiovasc Interv. 2009;74(2):257–259.[↩]
- Brown MD, Gomez-Marin O, Brookfield KF, et al. Differential diagnosis of hip disease versus spine disease. Clin Orthop Relat Res. 2004; (419):280–284.[↩]
- Segal NA, Felson DT, Torner JC, et al.; Multicenter Osteoarthritis Study Group. Greater trochanteric pain syndrome. Arch Phys Med Rehabil. 2007;88(8):988–992.[↩]
- Strauss EJ, Nho SJ, Kelly BT. Greater trochanteric pain syndrome. Sports Med Arthrosc. 2010;18(2):113–119.[↩]
- Williams BS, Cohen SP. Greater trochanteric pain syndrome. Anesth Analg. 2009;108(5):1662–1670.[↩]
- Martin HD, Shears SA, Palmer IJ. Evaluation of the hip. Sports Med Arthrosc. 2010;18(2):63–75.[↩]
- Bencardino JT, Palmer WE. Imaging of hip disorders in athletes. Radiol Clin North Am. 2002;40(2):267–287.[↩]
- Czerny C, Hofmann S, Urban M, et al. MR arthrography of the adult acetabular capsular-labral complex. AJR Am J Roentgenol. 1999;173(2):345–349.[↩]
- Blankenbaker DG, De Smet AA. Hip injuries in athletes. Radiol Clin North Am. 2010;48(6):1155–1178.[↩]
- Ramwadhdoebe S, Sakkers RJ, Uiterwaal CS, et al. Evaluation of a training program for general ultrasound screening for developmental dysplasia of the hip in preventive child health care. Pediatr Radiol. 2010;40(10):1634–1639.[↩]