Contents
What is acute flaccid myelitis
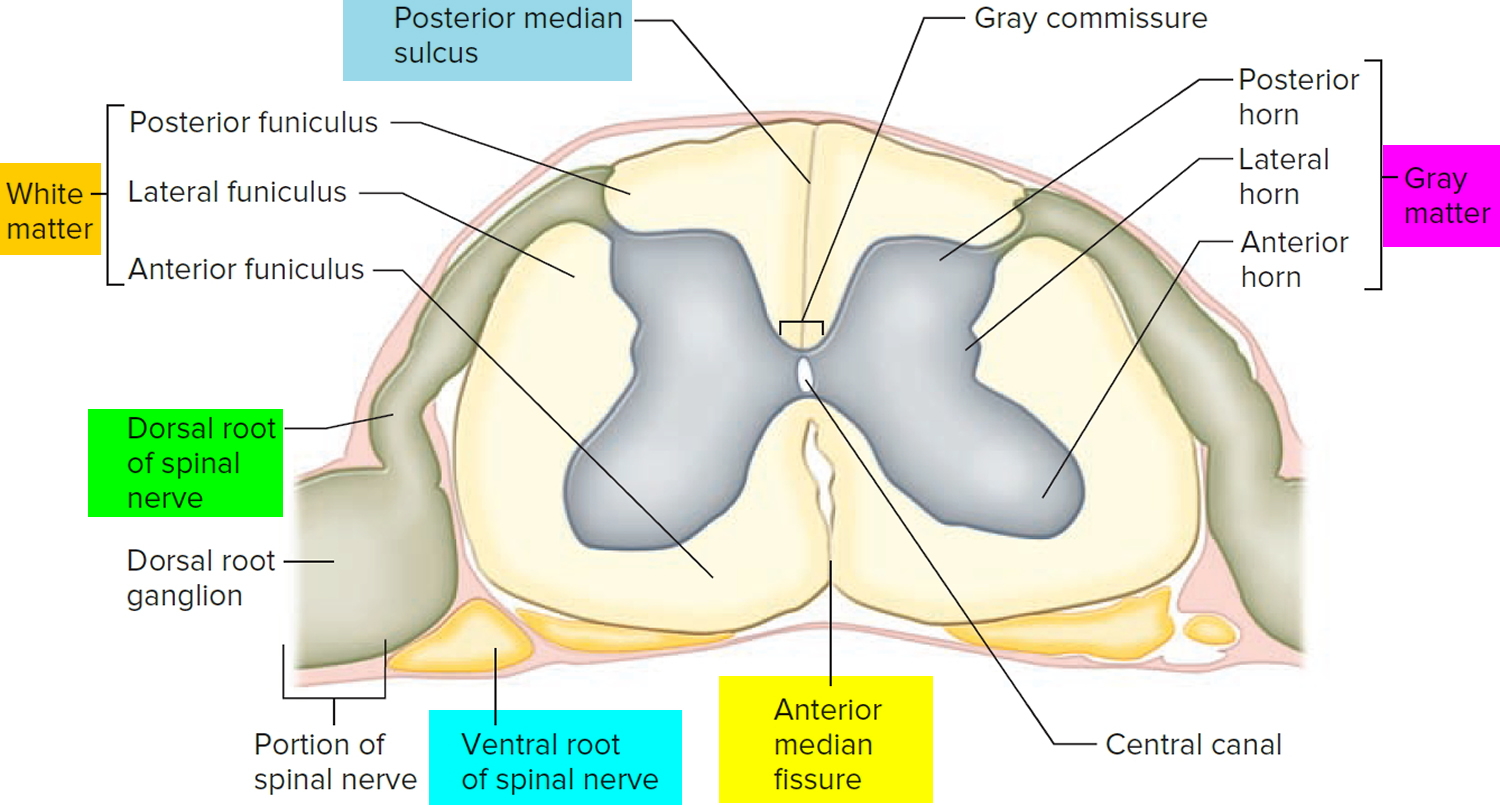
Acute flaccid myelitis is a rare but serious neurologic disease that affects an area of the spinal cord called gray matter 1. Acute flaccid myelitis can cause sudden weakness in the arms or legs and other symptoms and reflexes in the body to become weak. Some people with acute flaccid myelitis report pain 2. In some cases, acute flaccid myelitis can affect the nerves controlling the head and neck, causing facial weakness, drooping of the eyelids, and difficulty swallowing, speaking, or moving the eyes 1. The most serious complication of acute flaccid myelitis is respiratory failure if the muscles involved with breathing become weakened 3. Because of these symptoms, some people call acute flaccid myelitis a “polio-like” illness.
Acute flaccid myelitis tends to happen mainly in children, but it can develop in adults 2. Acute flaccid myelitis is still very rare (fewer than 1 in 1 million people per year in the United States).
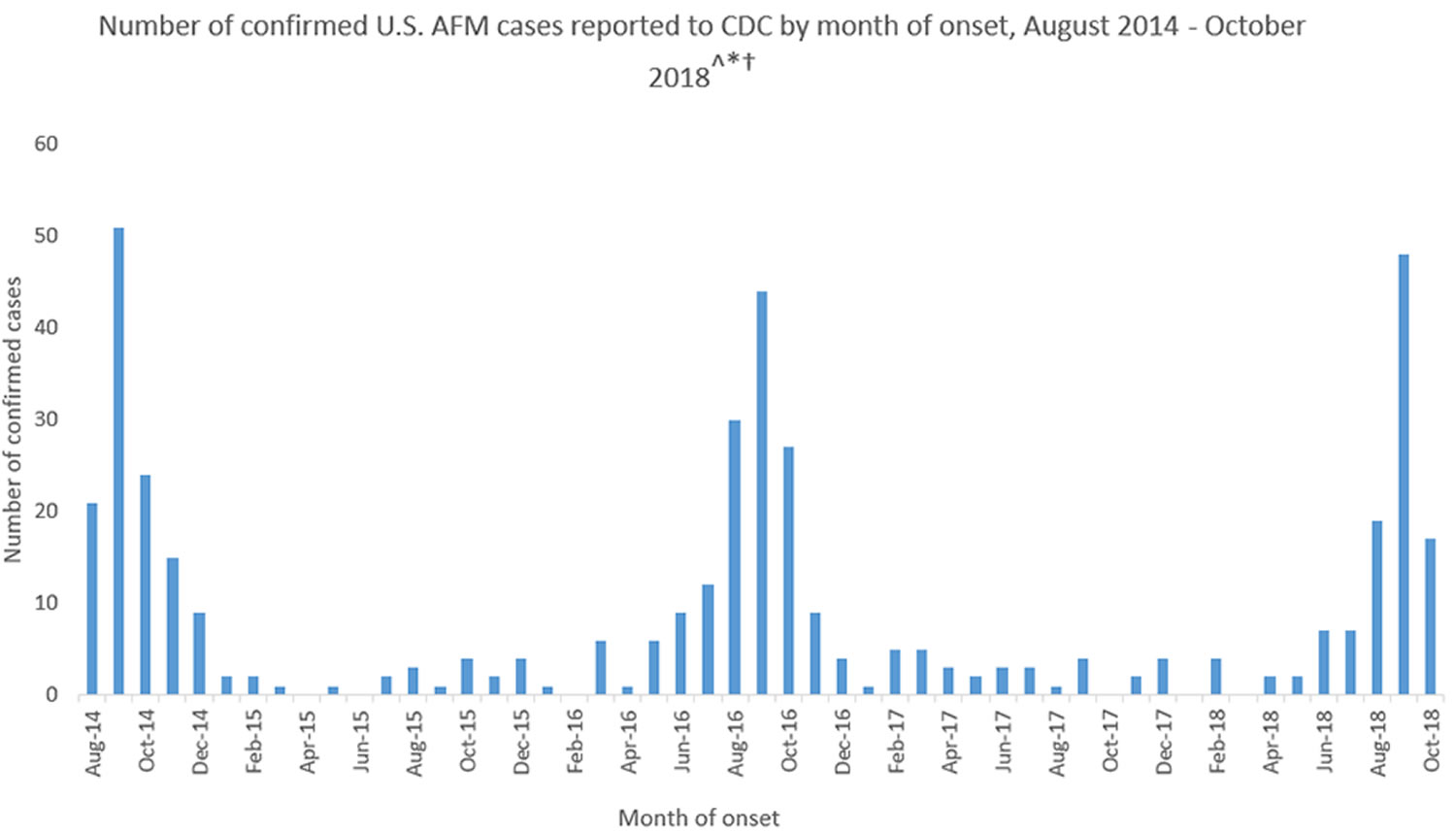
So far in 2018, there are 106 confirmed cases of acute flaccid myelitis in 29 states. These 106 confirmed cases are among the total of 273 reports that the Centers for Disease Control and Prevention (CDC) received of patients under investigation 4:
- In 2017, CDC received information for 33 confirmed cases of acute flaccid myelitis in 16 states.
- In 2016, CDC received information for 149 confirmed cases of acute flaccid myelitis in 39 states and DC.
- In 2015, CDC received information for 22 confirmed cases of acute flaccid myelitis in 17 states.
- From August to December 2014, CDC received information for 120 people confirmed cases of acute flaccid myelitis in 34 states.
- The case counts represent only those cases for which information has been sent to and confirmed by CDC.
Acute flaccid myelitis is not a new disease, but many people are learning about it now because of the recent outbreaks. Experts don’t know what’s causing the increase in cases.
Acute flaccid myelitis may have various causes. Infection with viruses such as adenovirus, poliovirus, other enteroviruses and West Nile virus may precede it 5. In some cases no clear possible cause is found 1. In addition, even when associated with a viral infection, it is not known how the infection triggers acute flaccid myelitis, and it is not clear why some people develop acute flaccid myelitis after an infection and others do not 1. West Nile virus is most commonly spread to people by mosquito bites. In North America, cases of West Nile virus occur during mosquito season, which starts in the summer and continues through fall. West Nile virus cases have been reported in all of the continental United States.
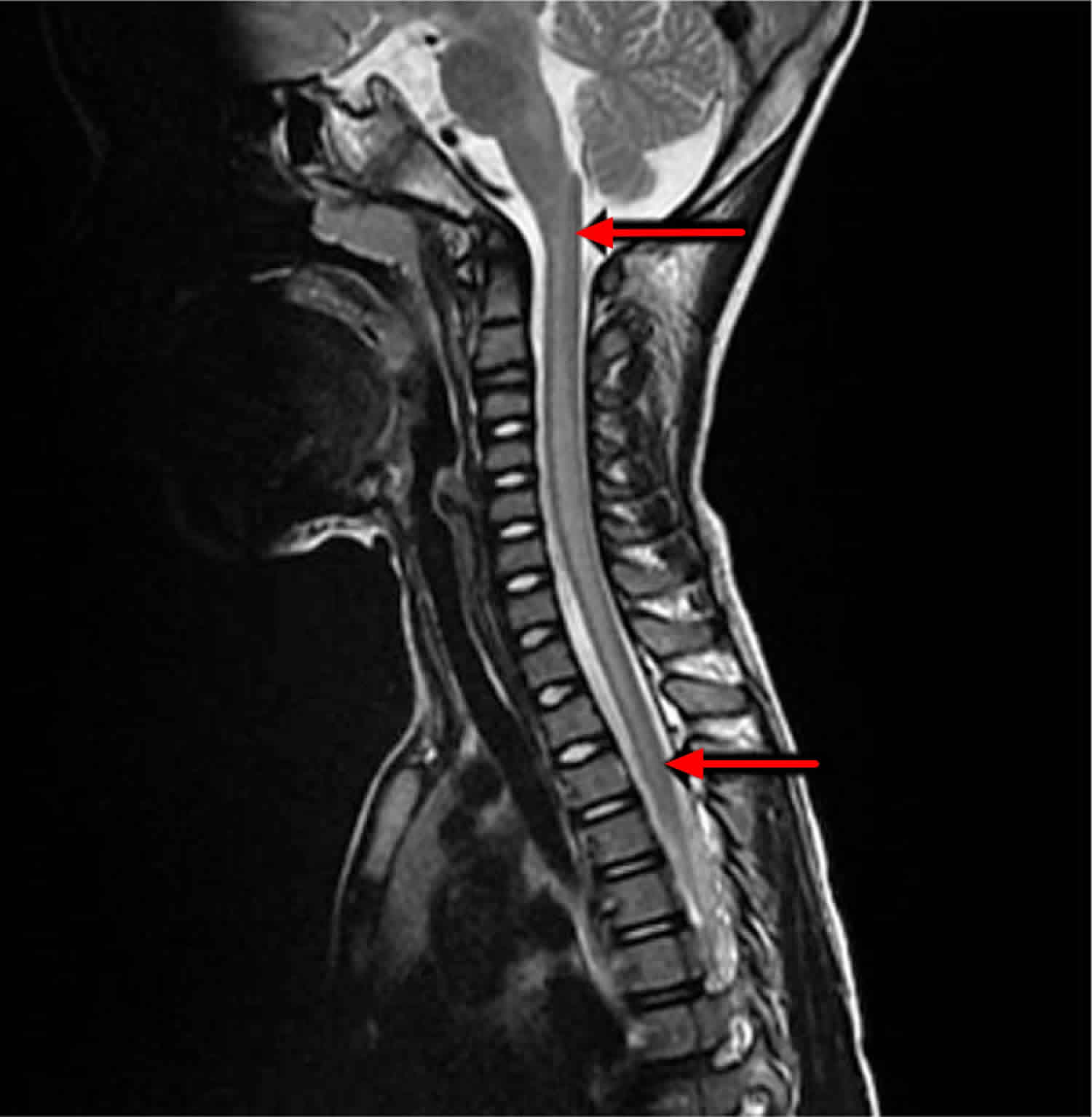
Acute flaccid myelitis can be difficult to diagnose because the symptoms are similar to other neurological diseases, such as Guillain-Barre syndrome, acute disseminated encephalomyelitis and transverse myelitis. Diagnosis may include a physical exam, an MRI of the spine, testing of the cerebral spinal fluid (CSF), and tests checking nerve speed (nerve conduction velocity) and the response of muscles to the messages from the nerves (electromyography; EMG) 5.
Acute flaccid myelitis may be treated by doctors trained in nervous system conditions (neurologists). Therapies specifically for acute flaccid myelitis aren’t available, but doctors may suggest physical and occupational therapy to help improve weakness in the arms and legs.
To prevent acute flaccid myelitis, it may help to get your child vaccinated against poliovirus. You can also help prevent acute flaccid myelitis by limiting your child’s chances of getting West Nile virus, which is spread through mosquito bites. Using mosquito repellent, avoiding being outdoors at dusk and dawn, and eliminating standing water on your property may protect your child from getting mosquito bites.
It may also help to use commonsense precautions to avoid catching illnesses — such as having your child regularly wash his or her hands with soap and water.
In 2014, the Centers for Disease Control and Prevention (CDC) got a large number of reports of people, mostly children, with acute flaccid myelitis 6. Since then, the CDC has been working hard to better understand acute flaccid myelitis, what puts people at risk of getting it, and the possible causes. Acute flaccid myelitis remains rare (less than one to two in a million people), even with the recent increase in cases. However, acute flaccid myelitis is serious, and experts don’t yet know what causes most people to get it or how to protect people from getting acute flaccid myelitis. As scientists continue to learn about acute flaccid myelitis, the CDC urges parents to seek medical care right away if their child develops symptoms of acute flaccid myelitis.
What the Centers for Disease Control and Prevention (CDC) has learned since 2014:
- Most of the patients with acute flaccid myelitis (more than 90%) had a mild respiratory illness or fever consistent with a viral infection before they developed acute flaccid myelitis.
- Viral infections such as from enteroviruses are common, especially in children, and most people recover. Experts don’t know why a small number of people develop acute flaccid myelitis, while most others recover. The CDC are continuing to investigate this.
- These acute flaccid myelitis cases are not caused by poliovirus; all the stool specimens from acute flaccid myelitis patients that the CDC received tested negative for poliovirus.
- The CDC detected coxsackievirus A16, enterovirus A71 (EV-A71), and enterovirus D68 (EV-D68) in the spinal fluid of four of 430 confirmed cases of acute flaccid myelitis since 2014, which points to the cause of their acute flaccid myelitis. For all other patients, no pathogen (germ) has been detected in their spinal fluid to confirm a cause.
- Most patients had onset of acute flaccid myelitis between August and October, with increases in acute flaccid myelitis cases every two years since 2014. At this same time of year, many viruses commonly circulate, including enteroviruses, and will be temporally associated with acute flaccid myelitis.
- Most acute flaccid myelitis cases are children (over 90%) and have occurred in 46 states and DC.
Figure 1. Spinal cord
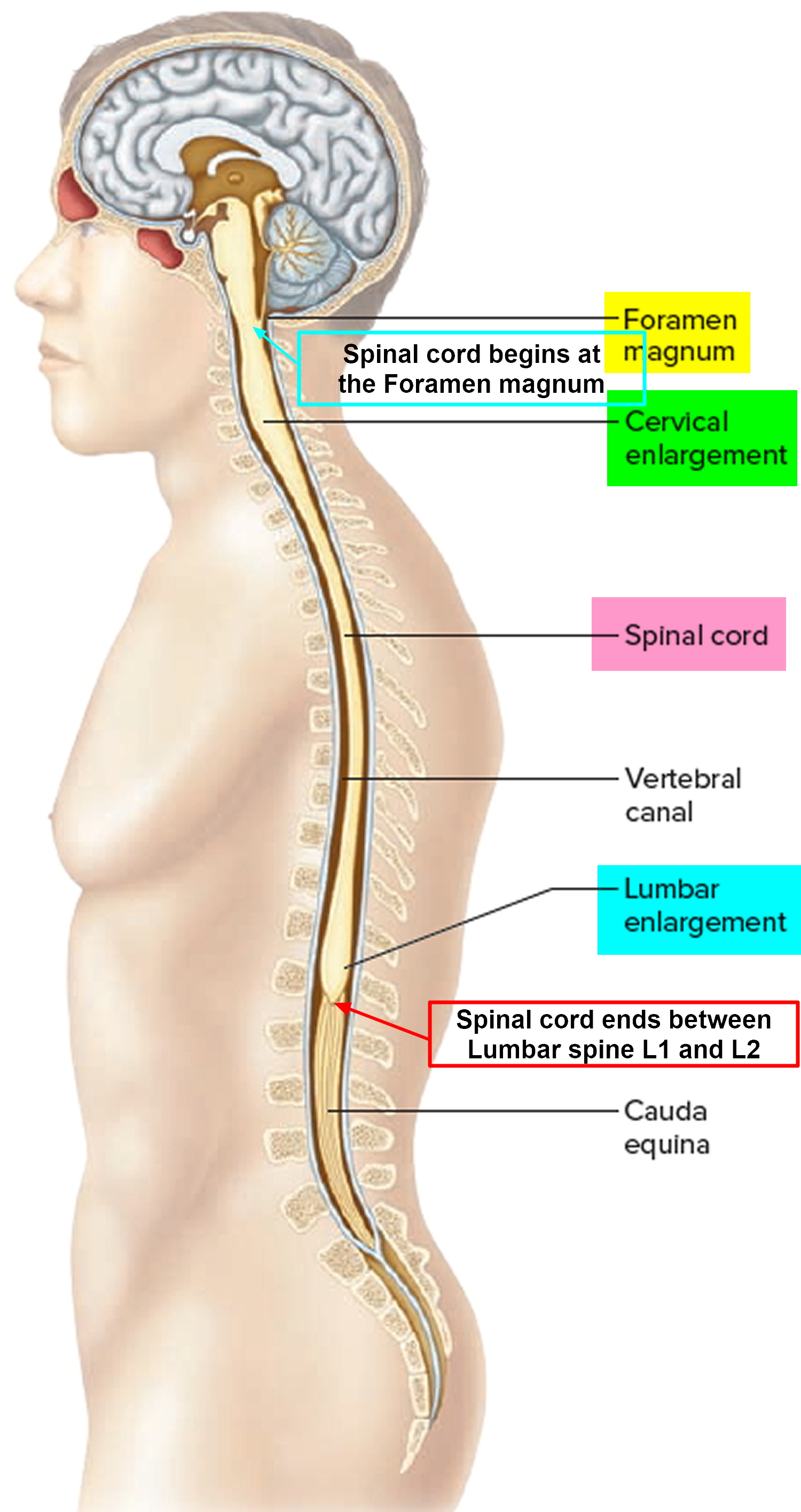
Figure 2. Spinal cord cross section
Figure 3. Acute flaccid myelitis MRI ( magnetic resonance imaging) scan – sagittal T2-weighted image MRI of the spinal cord showing enhanced signal over C1–T5 (arrows)
Is acute flaccid myelitis contagious?
Possibly. Certain viruses are known to cause acute flaccid myelitis including enteroviruses, such as poliovirus and enterovirus A71 (EV-A71), and West Nile virus 6. Since 2014, most patients with acute flaccid myelitis (more than 90%) had a mild respiratory illness or fever consistent with a viral infection before they developed acute flaccid myelitis. All the stool specimens from acute flaccid myelitis patients that the CDC received tested negative for poliovirus 6. Most patients had onset of acute flaccid myelitis between August and October, with increases in acute flaccid myelitis cases every two years since 2014 6. At this same time of year, many viruses commonly circulate, including enteroviruses, and will be temporally associated with acute flaccid myelitis.
The CDC detected coxsackievirus A16, enterovirus A71 (EV-A71), and enterovirus D68 (EV-D68) in the spinal fluid of four of 414 confirmed cases of acute flaccid myelitis since 2014, which points to the cause of their acute flaccid myelitis. For all other patients, no pathogen (germ) has been detected in their spinal fluid to confirm a cause. When a pathogen (germ) is found in the spinal fluid, it is good evidence that it was the cause of a patient’s illness. However, oftentimes, despite extensive testing of acute flaccid myelitis patients, no pathogens are found in the spinal fluid. This may be because the pathogen has been cleared by the body or it is hiding in tissues that make it difficult to detect. Another possibility is that the pathogen triggers an immune response in the body that causes damage to the spinal cord. The CDC are still searching for what triggers acute flaccid myelitis in some children who have had a fever and/or respiratory illness compared to most children who don’t get acute flaccid myelitis.
Acute flaccid myelitis causes
Experts think that viruses or toxins in the environment might cause acute flaccid myelitis.
Infections that can cause conditions like acute flaccid myelitis:
- Certain viruses, such as poliovirus, enterovirus A71 (EV-A71) and West Nile virus, can cause acute flaccid myelitis. You can protect yourself and your children from these viruses by:
- Making sure you are all up to date on polio vaccinations.
- Protecting against bites from mosquitoes, which can carry West Nile virus, by using mosquito repellent, staying indoors at dusk and dawn (when bites are more common), and removing standing or stagnant water near your home (where mosquitoes can breed).
- You can protect yourself and others from enteroviruses by washing your hands often with soap and water, avoiding close contact with people who are sick, and cleaning and disinfecting frequently touched surfaces, including toys.
Acute flaccid myelitis prevention
Because certain viruses are known to cause acute flaccid myelitis including enteroviruses, such as poliovirus and enterovirus A71 (EV-A71), and West Nile virus, you avoid spreading germs by:
- Keeping vaccinations up to date
- Keeping sick children home from school
- You can protect yourself and your children from poliovirus by getting vaccinated. Polio vaccine contains inactivated (not live) virus, and protects against poliovirus. This vaccine does not protect against other viruses that may cause acute flaccid myelitis.
- You can protect against bites from mosquitoes, which can carry West Nile virus, by using mosquito repellent, staying indoors at dusk and dawn (when bites are more common), and removing standing or stagnant water near your home (where mosquitoes can breed).
- You can protect yourself and others from enteroviruses by washing your hands often with soap and water, avoiding close contact with people who are sick, and cleaning and disinfecting frequently touched surfaces, including toys.
Acute flaccid myelitis prognosis
In a August–December 2014 Nationwide Surveillance 7 the researchers reported the following clinical findings and prognosis:
Eighty-five of 98 (87%) patients with any treatment information received some type of immunomodulating therapy for the neurologic illness, including intravenous immunoglobulin (62/85 [73%]), corticosteroids (46 [54%]), plasma exchange (13 [15%]), or other immunosuppressive medication (2 [2%]). The researchers received follow-up information from caregivers on the clinical status of 56 (47%) patients, who reported on function (effect of limb weakness on daily living activities) and limb strength (see Table 1). Median interval between limb weakness onset and report of follow-up outcome was 4.2 months (range, 0.8–7.5 months). Of the 56 respondents, 8 patients (14%) were reported as completely dependent on caregivers, 38 (68%) had some degree of functional impairment, requiring assistance for some activities, and 10 (18%) reported being fully functional. Only 3 patients (5%) reported complete recovery of strength; the remainder had some residual weakness. There were no deaths.
Table 1. Demographics and Clinical Findings Among Acute Flaccid Myelitis Cases, United States, August–December 2014 (N = 120)
| Variable (No. With Information) | No. (%) |
|---|---|
| At time of acute illness | |
| Age, median (range) (n = 119) | 7.1 y (0.4–20.8 y; 4.8–12.1 y) |
| Sex (n = 120) | |
| Male | 71 (59) |
| Female | 49 (41) |
| Race (n = 95) | |
| American Indian or Alaska Native | 1 (1) |
| Asian | 8(8) |
| Black or African American | 7 (7) |
| Native Hawaiian or Pacific Islander | 0(0) |
| White | 79 (83) |
| Ethnicity (n = 88) | |
| Hispanic or Latino | 29 (33) |
| Not Hispanic or Latino | 59 (67) |
| Hospitalized (n = 119) | 118 (99) |
| Respiratory illness preceding limb weakness (n = 118) | 95 (81) |
| Febrile illness preceding limb weakness (n = 115) | 74 (64) |
| Respiratory or febrile illness preceding limb weakness (n = 117) | 105 (90) |
| Limb involvement (n = 119)a | |
| Upper extremity(ies) only | 41 (34) |
| Lower extremity(ies) only | 27 (23) |
| Upperand lowerextremities, but not all 4 extremities | 21 (18) |
| All 4 extremities involved | 30 (25) |
| Cranial nerve findings (n = 120) | |
| Any cranial nerve sign | 34 (28) |
| Facial weakness | 17 (14) |
| Dysphagia | 14 (12) |
| Diplopia/double vision | 10 (9) |
| Dysarthria | 8(7) |
| Facial numbness | 1 (1) |
| Altered mental status (n = 109) | 12 (11) |
| Seizures during illness (n = 116) | 5(4) |
| Received care in intensive care unit (n = 112) | 58 (52) |
| Required mechanical ventilation (n = 109) | 26 (20) |
| Underlying illness (n = 116) | 24 (21) |
| Asthmab | 12 (10) |
| Otherc | 12 (10) |
| At time of follow-up (median 4.2 mo after acute illness) | 56 (49) |
| Functiond | |
| Complete dependence on caretakers | 8 (14) |
| Somewhat functionally impaired | 38 (68) |
| Fully functional | 10 (18) |
| Strength (compared to initial presentation) | |
| As weak | 11 (20) |
| Some improvement | 41 (73) |
| Full recovery | 3 (5) |
| More weak | 1 (2) |
Abbreviations:
Acute flaccid myelitis symptoms
Acute flaccid myelitis is rare, but it can lead to serious neurologic problems. Acute flaccid myelitis often happens after a respiratory infection, such as a cold.
A child with acute flaccid myelitis usually has sudden weakness in the arms and legs.
You should seek medical care right away if you or your child develops any of these symptoms:
- weakness and loss of muscle tone and reflexes in the arms or legs
- facial droop or weakness
- difficulty moving the eyes
- drooping eyelids
- drooping mouth
- difficulty swallowing
- slurred speech
- trouble breathing
If you or your child have any of these symptoms, get medical care right away.
Acute flaccid myelitis treatment
There is no specific treatment for acute flaccid myelitis, but a doctor who specializes in treating brain and spinal cord illnesses (neurologist) may recommend certain interventions on a case-by-case basis 1. . For example, neurologists may recommend physical or occupational therapy to help with arm or leg weakness caused by acute flaccid myelitis. The CDC are working closely with national experts to better understand how to treat acute flaccid myelitis and update the clinical management considerations. The CDC are also working to understand the long-term outcomes (prognosis) of people with acute flaccid myelitis.
Treatments that have been tried include immunoglobulin, corticosteroids, plasma exchange, and antiviral therapy, but there is no clear evidence that any of these treatments affect recovery. Other treatment is supportive and depends on the symptoms. Physical therapy and occupation therapy are especially important during recovery 5 The extent of recovery varies. Although some people may make a full recovery, most have continued muscle weakness even after a year 5. Long term outcomes are not known 1.
Summary of Interim Considerations for Clinical Management
Based on the available evidence and input from individual experts 8:
- There is no indication and that any specific targeted therapy or intervention should be either preferred or avoided in the treatment of acute flaccid myelitis. There are currently no targeted therapies/interventions with enough evidence to endorse or discourage their use for the treatment or management of acute flaccid myelitis.
- Clinicians should expedite neurology and infectious disease consultations to discuss treatment and management considerations.
- Corticosteroids: There is no indication that corticosteroids should be either preferred or avoided in the treatment of acute flaccid myelitis. There is no clear human evidence for efficacy of steroids in the treatment of acute flaccid myelitis, and there is some evidence in a mouse model with EV-D68 that steroids may be harmful. The possible benefits of the use of corticosteroids to manage spinal cord edema or white matter involvement in acute flaccid myelitis should be balanced with the possible harm due to immunosuppression in the setting of possible viral infection.
- Intravenous immunoglobulin (IVIG): There is no indication that IVIG should be either preferred or avoided in the treatment of acute flaccid myelitis. There is no clear human evidence for efficacy of IVIG in the treatment of acute flaccid myelitis, evidence for efficacy is based on early treatment in animal models and it has not been given in a systematic manner to acute flaccid myelitis patients to allow for measurements of efficacy. There is no evidence that treatment with IVIG is likely to be harmful.
- Plasmapheresis: There is no indication that plasma exchange should be either preferred or avoided in the treatment of acute flaccid myelitis. There is no clear human evidence for efficacy of plasma exchange in the treatment of acute flaccid myelitis, and it has not been given in a systematic manner to acute flaccid myelitis patients to allow for measurements of efficacy. Although there are inherent procedure-associated risks (especially in small children), there is no evidence that using plasma exchange for patients with acute flaccid myelitis is likely to be harmful.
- Fluoxetine: There is no indication that fluoxetine should be used for the treatment of acute flaccid myelitis. There is no clear human evidence for efficacy of fluoxetine in the treatment of acute flaccid myelitis based on a single retrospective evaluation conducted in patients with acute flaccid myelitis, and data from a mouse model also did not support efficacy.
- Antiviral medications: There is no indication that antivirals should be used for the treatment of acute flaccid myelitis, unless there is suspicion of herpesvirus infection (e.g., concomitant supra-tentorial disease or other clinical or radiologic features of herpesvirus infection). Appropriate antiviral medications (acyclovir, ganciclovir) should be empirically administered until herpesvirus infection has been excluded.
- Interferon: There is no indication that interferon should be used for the treatment of acute flaccid myelitis, and there is concern about the potential for harm from the use of interferon given the immunomodulatory effects in the setting of possible ongoing viral replication.
- Other immunosuppressive medications/biological modifiers: There is no indication that biologic modifiers and the use of other immunosuppressive agents should be used for the treatment of acute flaccid myelitis, and there is a possibility of harm in their use.
Summary of Specific Interventions/Therapies
Corticosteroids
- Steroids have been given in several published case series of acute flaccid myelitis patients, but most often in combination with other therapies such as IVIG and plasma exchange, making it difficult to assess their effects on the disease process 9.
- There is a theoretical concern about the possible adverse effects of administration of corticosteroids in the setting of acute infection, which may compromise the innate immune response to the infection, thus propagating the infectious process and leading to further neuronal damage and worse clinical outcomes.
- The use of corticosteroids has been associated with poorer outcome in observational studies of outbreaks of neuroinvasive disease due to enterovirus – 71 (EV-71) internationally and in mouse model 10. This observation following a 2012 outbreak in Cambodia led to the conclusion among a WHO-convened joint commission that corticosteroids were contraindicated in the management of EV-71 associated neuroinvasive disease (World Health Organization. Global alert and response (GAR): Severe complications of hand, foot and mouth disease (HFMD) caused by EV-71 in Cambodia — Conclusion of the joint investigation. Jul 13, 2012.). This is relevant, as an increase in EV-A71 associated neurologic disease has been reported in the US in 2018.
- In a mouse model of acute flaccid myelitis using EV-D68 as the infectious virus, mice receiving dexamethasone at either early or late time points from infection had significantly higher mortality compared to infected controls. Individual dexamethasone treated mice that died had worse paralysis associated with their motor impairment score than in infected control 11.
- There may be theoretical benefit for steroids in the setting of severe cord swelling or long tract signs suggesting white matter involvement, where steroids may salvage tissue that may be harmed due to an ongoing immune/inflammatory response. While acute flaccid myelitis is clinically and radiographically defined by the predominance of gray matter damage in the spinal cord, some patients may have some white matter involvement. It is not clear if these different patterns are important relative to therapeutic considerations.
- The differential diagnosis for acute flaccid myelitis includes conditions that would best be treated by early initiation of steroids (transverse myelitis, anti-MOG antibody related disease, acute disseminated encephalomyelitis).
Summary
There is no indication that corticosteroids should be either preferred or avoided in the treatment of acute flaccid myelitis. There is no clear human evidence for efficacy of steroids in the treatment of acute flaccid myelitis, and there is some evidence in a mouse model with EV-D68 that steroids may be harmful. The possible benefits of the use of corticosteroids to manage spinal cord edema or white matter involvement in acute flaccid myelitis should be balanced with the possible harm due to immunosuppression in the setting of possible viral infection.
Intravenous Immune Globulin (IVIG)
- IVIG has been utilized for neurologic complications in enteroviral disease associated with neurologic involvement. Enteroviruses cause chronic, severe CNS infections in agammaglobulinemic children, suggesting humoral immunity plays an important role in attenuating enteroviral infection 12. Similarly, infants who fail to acquire neutralizing antibody from their mothers have been described as having more severe disease when infected with enteroviruses 13.
- IVIG has been shown to modulate cytokine production (IFN-γ, IL-6, IL-8, IL-10, IL-13) in the CNS and systemic inflammatory response. In addition, there is a theoretical risk of IVIG interfering with naturally acquired innate immunity, due to the immunomodulatory effects of the F(ab’) region of the immunoglobulin molecule, which may impact cell-mediated immunity.
- For IVIG to modify disease in an active viral infectious process, early administration is likely required, and possibly prior to exposure. Pre-poliovirus vaccine era trials in the 1950s demonstrated potential efficacy of gamma globulin for prevention of poliomyelitis with mass gamma globulin administration to susceptible populations in an outbreak situation 14. However, a randomized, non-blinded trial of intramuscular (IM) gamma globulin treatment in 49 children (48 controls) with pre-paralytic poliomyelitis (CSF WBC>10 cells/mm without development of weakness) did not impact development or severity of paralysis during a poliovirus outbreak in New York City in 1944 15.
- There has been recent experience with the use of IVIG in the treatment of WNV and EV-D68 associated neuroinvasive disease. IVIG has been shown to have some efficacy in prevention of progression to neuroinvasive disease in rodent models 16. Paralysis in mice was prevented in a time-dependent fashion after administration of IVIG from time of infection. However, clear efficacy of IVIG has not been demonstrated in humans with WNV associated paralysis with most data limited to case reports or small case series 17.
- IVIG has been utilized for patients presenting with symptoms of acute flaccid myelitis, but to date no systematic studies of IVIG have been conducted. In a 2014 – 2015 case-series, treatment of acute flaccid myelitis using IVIG was done either alone or in combination with methylprednisolone and plasma exchange. All patients tolerated the treatment regimens well without major complications. Neurologic improvement was seen in all patients regardless of treatment, but in all except one patient, deficits persisted 18. Messacar, et al 19 reported on a review of clinical cases from 2012 – 2015. All cohorts that were reviewed received various combinations of IVIG, steroids, plasma exchange and antiviral medications. No significant improvement or deterioration was noted with these therapies, but a systematic assessment of response was not feasible with the retrospective review. Hopkins 20 noted in her review piece on acute flaccid myelitis diagnostic and management considerations that the current practice at Children’s Hospital Philadelphia is to initiate therapy with IVIG upon recognition of acute flaccid myelitis in hopes of boosting humoral immunity.
- IVIG is generally safe and well tolerated, though expensive. Common intra-infusion adverse effects of IVIG include fever, headache, myalgia, chills, nausea, and vomiting which are typically infusion rate-dependent 21. Less commonly, hypersensitivity and anaphylactoid symptoms of flushing, tachycardia, hypotension can be seen. Post-infusion adverse events include headaches and aseptic meningitis, fatigue, and arthralgias 22. IVIG is occasionally associated with severe adverse events such as acute renal failure, thromboembolic events, hemolytic anemia and neutropenia.
- IVIG preparations have been shown to contain antibody to circulating enteroviruses, including EV-D68 23.
Summary
There is no indication that IVIG should be either preferred or avoided in the treatment of acute flaccid myelitis. There is no clear human evidence for efficacy of IVIG in the treatment of acute flaccid myelitis, evidence for efficacy is based on early treatment in animal models and it has not been given in a systematic manner to acute flaccid myelitis patients to allow for measurements of efficacy. There is no evidence that treatment with IVIG is likely to be harmful.
Plasma Exchange (PLEX)
- It is presumed that there are beneficial effects from the innate humoral immune response to an acute viral infection, in which the body produces neutralizing antibodies to the infectious pathogen 24. Removal of these antibodies induced in response to acute infection could cause potential harm. Additionally, plasmapheresis requires placement of invasive intravenous access and procedure-associated risks.
- Plasmapheresis has been used in published case-series of acute flaccid myelitis patients. From a case-series in Argentina, 4 children were given PLEX in combination with IVIG and steroids. Treatment did not lead to clinical improvement 25. Nelson et al 18 referenced above also used PLEX in combination with steroids and IVIG. In a single acute flaccid myelitis case published in 2017, Esposito et al 26 treated a 4 y/o child with plasmapheresis in addition to corticosteroids and IVIG for 3 days. After 4 weeks of oral steroids and a 2-week taper, significant improvement was noted. No data was available to evaluate plasmapheresis in the absence of other therapies. No adverse events were noted for PLEX in the above publications.
Summary
There is no indication that plasma exchange should be either preferred or avoided in the treatment of acute flaccid myelitis. There is no clear human evidence for efficacy of plasma exchange in the treatment of acute flaccid myelitis, and it has not been given in a systematic manner to acute flaccid myelitis patients to allow for measurements of efficacy. Although there are inherent procedure-associated risks (especially in small children), there is no evidence that using plasma exchange for patients with acute flaccid myelitis is likely to be harmful.
Fluoxetine
- Fluoxetine is a selective serotonin reuptake inhibitor that demonstrates activity in vitro against enteroviruses including EV-D68. Its concentration in the brain far exceeds that of the serum, which suggested a possible option for treating CNS infection due to enteroviruses.
- In a mouse model of EV-D68 induced paralysis, fluoxetine injections had no effect on paralysis compared to infected controls, regardless of dose. In addition, mortality was higher in mice who received fluoxetine compared to controls 11.
- In a comparison of patients who received treatment with fluoxetine, and those who did not, using a summative limb strength score between their initial examination and most recent follow-up as an outcome, fluoxetine was not associated with improved neurologic outcomes 9. The patients treated with fluoxetine were more likely to have severe paralysis and to have EV-D68 isolated from respiratory specimens.
Summary
There is no indication that fluoxetine should be used for the treatment of acute flaccid myelitis. There is no clear human evidence for efficacy of fluoxetine in the treatment of acute flaccid myelitis based on a single retrospective evaluation conducted in patients with acute flaccid myelitis, and data from a mouse model also did not support efficacy.
Antiviral medications
- It is important to point out that, while symptoms of a viral illness precede limb weakness onset, and clinical data supporting pathogenesis point to an acute infectious process, a specific pathogen isolated from a sterile site in the majority of acute flaccid myelitis patients has yet to be identified.
- Any guidance regarding antiviral medications should be interpreted with great caution, given the unknowns about the pathogenesis of this illness at present. Heath departments, CDC, and other academic entities are working to try to identify all causative agents for acute flaccid myelitis, which will help provide further guidance regarding the use of anti-microbial therapies for this illness.
- Testing has been conducted at CDC for antiviral activity of compounds pleconaril, pocapavir, and vapendavir and none have significant activity against currently circulating strains of EV-D68 at clinically relevant concentrations 27.
Summary
There is no indication that antivirals should be used for the treatment of acute flaccid myelitis, unless there is suspicion of herpesvirus infection (e.g., concomitant supra-tentorial disease or other clinical or radiologic features of herpesvirus infection). Appropriate antiviral medications (acyclovir, ganciclovir) should be empirically administered until herpesvirus infection has been excluded.
Interferon
- Anecdotal accounts of improvement with interferon α-2b in the treatment of West Nile poliomyelitis-like illness were reviewed in 2014. In addition, a case series assessing the efficacy of IFN-α in the treatment of Saint Louis encephalitis, including AFP presentations, suggested some improvement in a non-randomized pilot trial 28; however, subsequent non-controlled assessments failed to replicate this improvement in cases of SLE and WNV.
- A randomized trial performed in Vietnam from 1996–1999 evaluated 117 children with Japanese encephalitis randomized to receive interferon (10 million units/m2 daily for 7 days) or placebo. Outcome at discharge and 3 months did not differ between the two treatment groups; 20 (33%) of 61 children in the interferon group had a poor outcome (death or severe sequelae), compared with 18 (32%) of 56 in the placebo group 29.
- Although there are limited in vitro, animal, and anecdotal human data suggesting activity of some interferons against viral infections, sufficient data are lacking in the setting of acute flaccid myelitis.
Summary
There is no indication that interferon should be used for the treatment of acute flaccid myelitis, and there is concern about the potential for harm from the use of interferon given the immunomodulatory effects in the setting of possible ongoing viral replication.
Other immunosuppressive medications / biological modifiers
- In the setting of acute flaccid myelitis, biologic modifiers may have an adverse impact on patients, presuming infectious etiology. The combination of immunosuppressive agents directly impairing T-cell function (and B-cell function indirectly), or therapy directed against primary humoral immunity (e.g., rituximab) may further worsen the ability to clear infection.
Summary
There is no indication that biologic modifiers and the use of other immunosuppressive agents should be used for the treatment of acute flaccid myelitis, and there is a possibility of harm in their use.
- About Acute Flaccid Myelitis. https://www.cdc.gov/acute-flaccid-myelitis/about-afm.html[↩][↩][↩][↩][↩][↩]
- Messacar K, Schreiner TL, Van Haren K, et al. Acute flaccid myelitis: A clinical review of US cases 2012-2015. Ann Neurol. September, 2016; 80(3):326-338. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5098271[↩][↩]
- Nelson GR, Bonkowsky JL, Doll E, Green M, Hedlund GL, Moore KR, Bale JF Jr. Recognition and Management of Acute Flaccid Myelitis in Children. Pediatr Neurol. February, 2016; 55:17-21. https://www.ncbi.nlm.nih.gov/pubmed/26621554[↩]
- AFM Confirmed U.S. Cases. https://www.cdc.gov/acute-flaccid-myelitis/afm-cases.html[↩]
- Hopkins SE. Acute Flaccid Myelitis: Etiologic Challenges, Diagnostic and Management Considerations. Curr Treat Options Neurol. November 28, 2017; 19(12):48. https://www.ncbi.nlm.nih.gov/pubmed/29181601[↩][↩][↩][↩]
- Acute Flaccid Myelitis in U.S. Children. https://www.cdc.gov/features/acute-flaccid-myelitis/index.html[↩][↩][↩][↩]
- Sejvar JJ, Lopez AS, Cortese MM, et al. Acute Flaccid Myelitis in the United States, August-December 2014: Results of Nationwide Surveillance. Clin Infect Dis. 2016;63(6):737-745. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5709818/[↩][↩]
- Acute Flaccid Myelitis: Interim Considerations for Clinical Management. https://www.cdc.gov/acute-flaccid-myelitis/hcp/clinical-management.html[↩]
- Messacar K SS, Hopkins S, et al. Safety, Tolerability, and Efficacy of Fluoxetine as an Anti-viral for Acute Flaccid Myelitis. Neurology. 2018; Nov 9.[↩][↩]
- He Y, Yang J, Zeng G, et al. Risk factors for critical disease and death from hand, foot and mouth disease. The Pediatric infectious disease journal. 2014;33:966-970.[↩]
- Hixon AM, Clarke P, Tyler KL. Evaluating Treatment Efficacy in a Mouse Model of Enterovirus D68-Associated Paralytic Myelitis. The Journal of infectious diseases. 2017;216:1245-1253.[↩][↩]
- Wilfert CM, Buckley RH, Mohanakumar T, et al. Persistent and fatal central-nervous-system ECHOvirus infections in patients with agammaglobulinemia. The New England journal of medicine. 1977;296:1485-1489.[↩]
- Modlin JF, Kinney JS. Perinatal enterovirus infections. Advances in pediatric infectious diseases. 1987;2:57-78.[↩]
- Ward R, Logrippo GA, Graef I, Earle DP, Jr. Quantitative studies on excretion of poliomyelitis virus: a comparison of virus concentration in the stools of paralytic and non-paralytic patients. The Journal of clinical investigation. 1954;33:354-357.[↩]
- Bahlke AM, Perkins JE. Treatment of preparalytic poliomyelitis with gamma globulin. Journal of the American Medical Association. 1945;129:1146-1150.[↩]
- Hurst BL, Evans WJ, Smee DF, et al. Evaluation of antiviral therapies in respiratory and neurological disease models of Enterovirus D68 infection in mice. Virology. 2018; Oct 31; 526:146-154.[↩]
- Hebert J, Armstrong D, Daneman, N. et al. Adult-onset opsoclonus-myoclonus syndrome due to West Nile virus treated with IVIG. J Neurovirol. 2017; Feb; 23(1):158-159.[↩]
- Nelson GR, Bonkowsky JL, Doll E, et al. Recognition and Management of Acute Flaccid Myelitis in Children. Pediatric neurology. 2016;55:17-21.[↩][↩]
- Messacar K, Schreiner TL, Van Haren K, et al. Acute flaccid myelitis: A clinical review of US cases 2012-2015. Annals of neurology. 2016;80:326-338.[↩]
- Hopkins SE. Acute Flaccid Myelitis: Etiologic Challenges, Diagnostic and Management Considerations. Current treatment options in neurology. 2017;19:48.[↩]
- Pediatrics AAo. Passive Immunization. In: Pickering LK B, CJ, Kimberlin DW, Long SS, eds., ed. Red Book: 2012 Report of the Committee on Infectious Diseases Elk Grove Village, IL: American Academy of Pediatrics; 2012:59-62.[↩]
- Singh-Grewal D, Kemp A, Wong M. A prospective study of the immediate and delayed adverse events following intravenous immunoglobulin infusions. Archives of disease in childhood. 2006;91:651-654.[↩]
- Zhang Y, Moore DD, Nix WA, Oberste MS, Weldon WC. Neutralization of Enterovirus D68 isolated from the 2014 US outbreak by commercial intravenous immune globulin products. Journal of clinical virology : the official publication of the Pan American Society for Clinical Virology. 2015;69:172-175.[↩]
- Schwartz J. Evidence-based guideline update: plasmapheresis in neurologic disorders. Neurology. 2011;77:e105-106; author reply e106.[↩]
- Ruggieri V, Paz MI, Peretti MG, et al. Enterovirus D68 infection in a cluster of children with acute flaccid myelitis, Buenos Aires, Argentina, 2016. European journal of paediatric neurology : EJPN : official journal of the European Paediatric Neurology Society. 2017;21:884-890.[↩]
- Esposito S, Chidini G, Cinnante C, et al. Acute flaccid myelitis associated with enterovirus-D68 infection in an otherwise healthy child. Virology journal. 2017;14:4.[↩]
- Rhoden E, Zhang M, Nix WA, Oberste MS. In Vitro Efficacy of Antiviral Compounds against Enterovirus D68. Antimicrobial agents and chemotherapy. 2015;59:7779-7781.[↩]
- Rahal JJ, Anderson j, Rosenberg C. et al. Effect of interferon-alpha2b therapy on St. Louis viral meningoencephalitis: clinical and laboratory results of a pilot study. JID. 2004; Sept 15; 190 (6):1084-7.[↩]
- Solomon T, Dung NM, Wills B, et al. Interferon alfa-2a in Japanese encephalitis: a randomised double-blind placebo-controlled trial. Lancet (London, England). 2003;361:821-826.[↩]