Contents
What is turf toe
Turf toe is a sprain of the big toe joint, the plantar metatarsophalangeal-sesamoid complex, resulting from injury during sports activities. The injury usually results from excessive upward bending of the big toe joint. The condition can be caused from either jamming the toe or from repetitive injury when pushing off repeatedly when running or jumping. Although turf toe injury is most commonly reported in football players, participants in soccer, basketball, wrestling, gymnastics and dance also are at risk.
The name “turf toe” comes from the fact that this injury is especially common among athletes who play on artificial turf. When playing sports on artificial turf, the foot can stick to the hard surface, resulting in jamming of the big toe joint. There has been some indication that less-supportive flexible shoes worn on artificial turf are also to blame.
Turf toe injury was originally described in 1976 by Bowers and Martin at the University of West Virginia, where they noted an average of 5.4 turf toe injuries per season among football players 1. Bowers and Martin described a hyperextension injury to the big toe (hallux) metatarsophalangeal (MTP) joint that injures the plantar soft tissue structures of the metatarsophalangeal (MTP) joint. The turf toe name originated following the increase in these injuries seen in American footballers after the introduction of firm artificial playing surfaces and flexible footwear 1.
The overall incidence of turf toe injuries in American national college football players is 0.062 per 1000 athlete-exposures 2. There is an average of 10.1 days lost due to turf toe injury. Rodeo et al 3 found that in a survey of 80 active professional American football players, 45% had suffered turf toe injuries in their professional careers, with 83% occurring on artificial turf. Clanton and Ford found that foot injuries were the third leading cause of missed playing time and that a large portion of these injuries involved the hallux metatarsophalangeal joint 4.
There has been an apparent increase in the occurrence of turf toe injuries, possibly due to the use of more flexible, lighter shoes or changes in surface–cleat interaction 5. A further reason for this increase may be greater awareness of the injury and earlier identification by athletic trainers and physicians. George et al 2 showed a significantly higher injury rate on third-generation artificial surfaces compared with natural grass; however, a study of high school athletes comparing injuries on modern artificial turf with injuries on natural grass showed no difference in injury patterns 6.
In rugby players, a prospective study following rugby players over four seasons showed that turf toe accounts for 11% of all foot injuries, which is equivalent to 0.4% of players affected per season. On average, these patients took 22 days to return to full fitness. The one patient in the series with a ruptured plantar plate required 89 days for recovery 7.
To arrive at a diagnosis, your doctor will obtain your medical history and examine your foot. X-rays are typically ordered to rule out any broken bone. Other advanced imaging studies may also be helpful for proper diagnosis.
How to treat turf toe
Initial treatments include rest, ice, compression, and elevation (RICE), as well as a change to less-flexible footwear. Surgery is reserved for individuals with severe cases and prolonged pain.
Turf toe anatomy
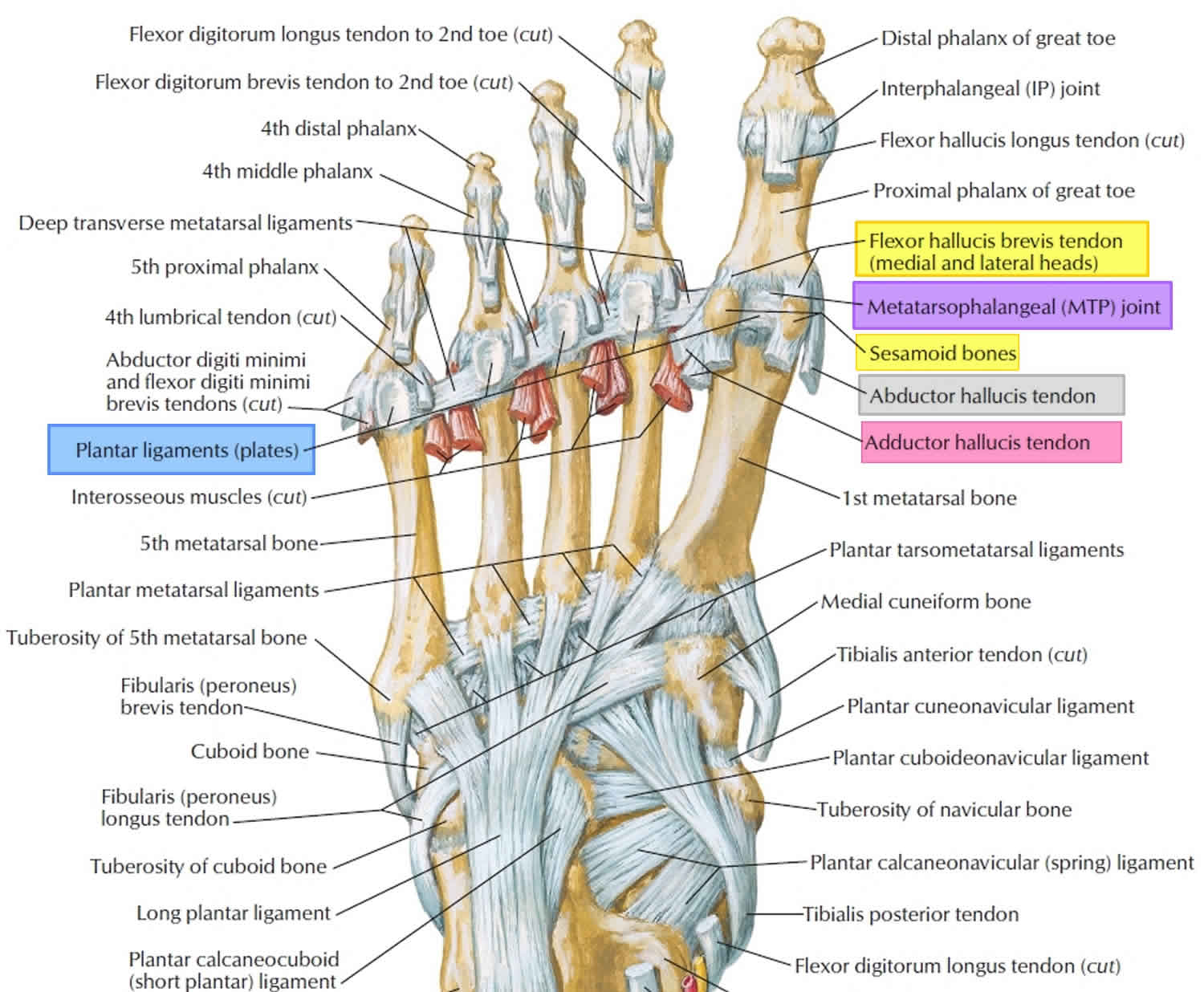
Most of the stability of the hallux metatarsophalangeal joint comes from the capsule, ligaments, and short flexor complex (Figure 3). There is little inherent stability to the metatarsophalangeal joint because the proximal phalanx has a fairly shallow cavity in which the metatarsal head articulates. Fan-shaped medial and lateral collateral ligaments provide valgus and varus stability, respectively. Each comprise a collateral component between the first metatarsal and proximal phalanx and a metatarsosesamoid slip. The plantar plate is the greatly thickened plantar capsule that courses from a weaker attachment on the metatarsal head to a more firm attachment on the proximal phalanx. In addition to the collateral ligaments and plantar plate, the hallux metatarsophalangeal joint is dynamically stabilized by the short flexor complex (the flexor hallucis brevis and the hallucal sesamoids embedded in the flexor hallucis brevis tendons), the adductor hallucis, and the abductor hallucis tendons.
The flexor hallucis brevis tendon inserts on the proximal phalanx in confluence with the plantar ligament plate (Figure 3). The muscle originates proximally on the plantar aspect of the foot, primarily from the cuboid and lateral cuneiform. As the flexor hallucis brevis moves distally toward its insertion, the tendon envelops the medial (tibial) and lateral (fibular) sesamoids. The medial sesamoid is typically larger than the lateral sesamoid and sits more distal. The first metatarsal bears plantar load through these 2 sesamoids and their respective articulations. The sesamoids also function to increase the lever arm of the flexor hallucis brevis and, indirectly, the flexor hallucis longus to mechanically augment flexion (push off) strength at the metatarsophalangeal (MTP) joint 8. The flexor hallucis longus tendon courses plantar to the metatarsal head, between the sesamoids in a separate sheath. At the level of the sesamoids, the abductor hallucis and adductor hallucis tendons conjoin with the medial and lateral heads of the flexor hallucis brevis, respectively.
In normal gait, the capsular ligamentous complex of the hallux metatarsophalangeal (MTP) joint must withstand 40% to 60% of body weight 9. This can increase to 2 to 3 times body weight in normal athletic activity and can reach as much as 8 times body weight with a running jump 10. The capsular ligamentous complex of the hallux metatarsophalangeal (MTP) joint is a stout, strong soft tissue complex that is critical to the function of an athlete.
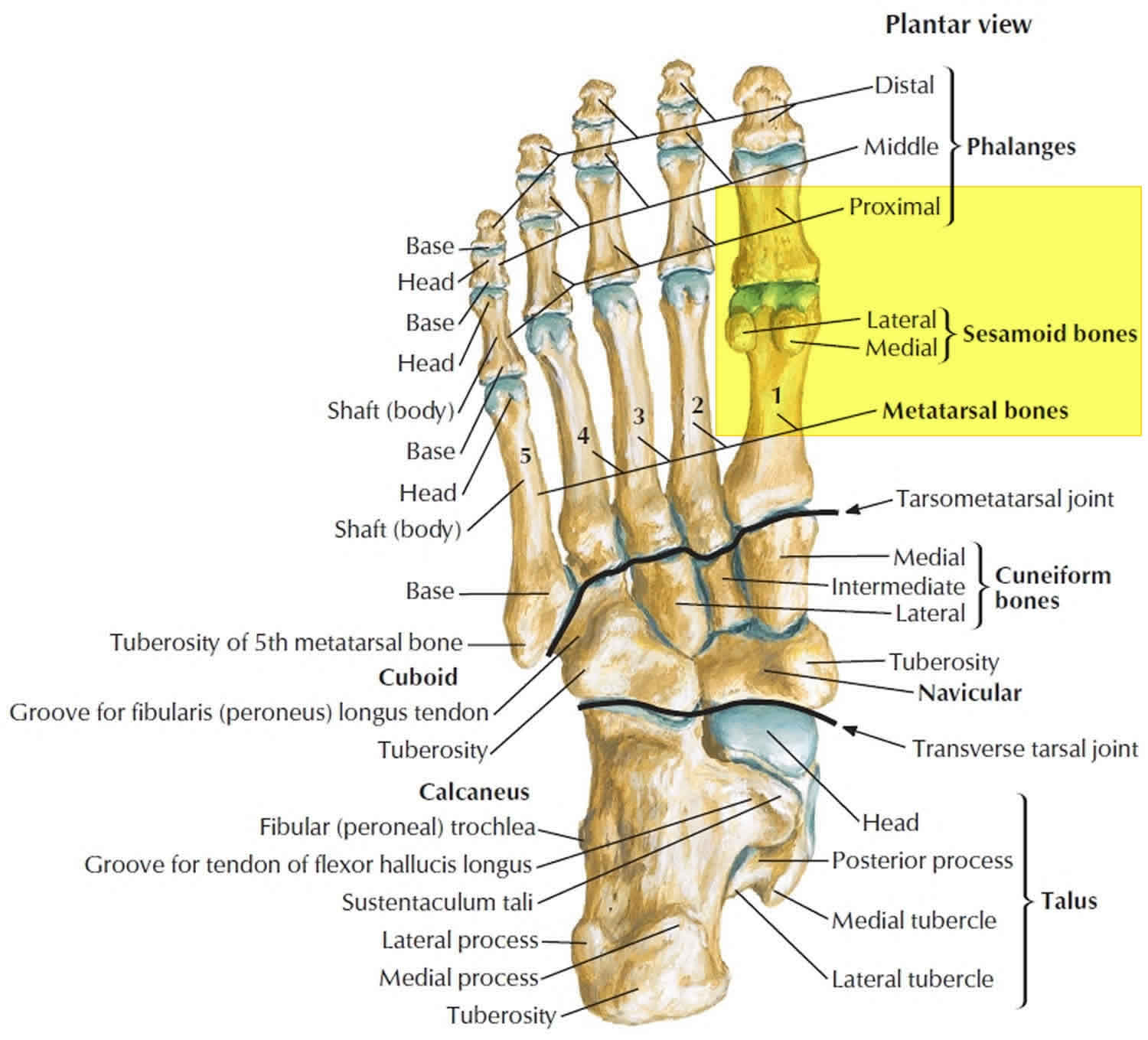
Figure 1. Big toe and foot bones (plantar view)
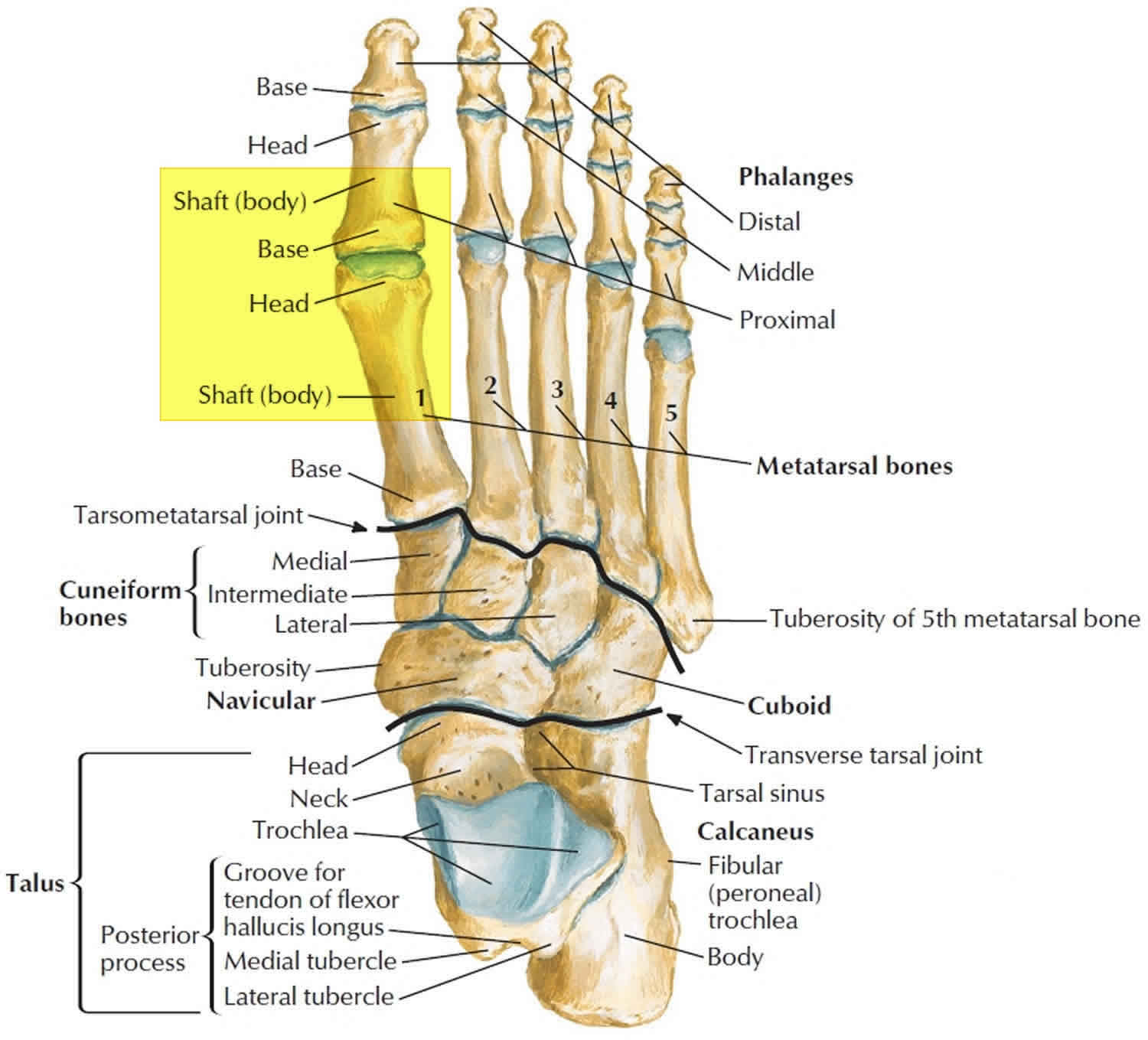
Figure 1. Big toe and foot bones (dorsal view)
Figure 3. Big toe ligaments (plantar view)
Figure 4. Turf toe – a traumatic hallux valgus deformity (left) compared to a normal hallux alignment (right)
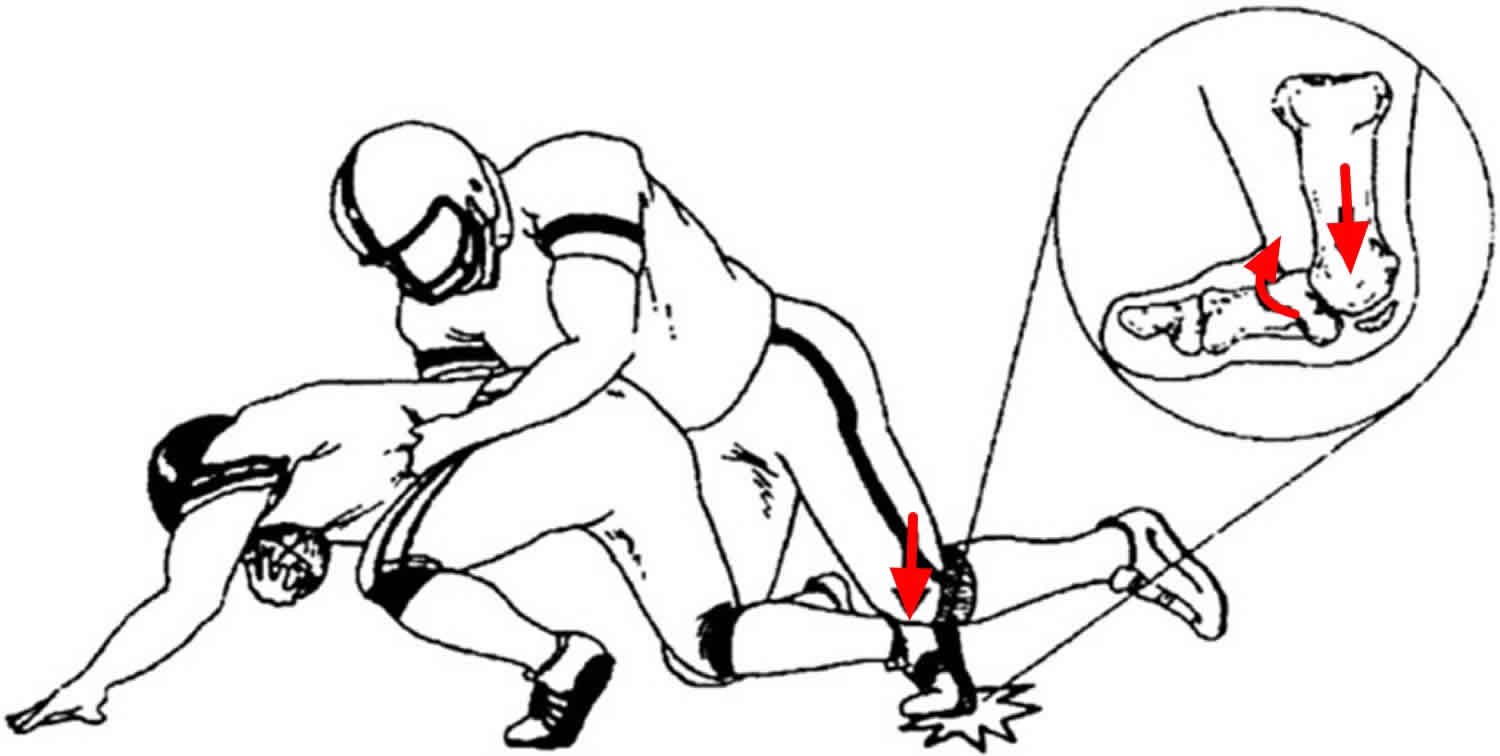
[Source 11 ]Turf toe mechanism of injury
The majority of turf toe injuries occur as a result of contact with the playing surface or contact with another player 12. This essentially causes an axial load, on a hyperextended metatarsophalangeal (MTP) joint, with fixed equinus at the ankle. The load drives the hallux metatarsophalangeal (MTP) joint into hyperextension, which leads to attenuation or disruption of the plantar capsular ligamentous complex supporting the joint 13. The plantar plate complex is designed to resist dorsiflexion of the first metatarsophalangeal (MTP) joint, but these tissues can be torn, with the degree of damage dependent on the severity of injury and forces to the joint (Figure 4).
Depending on the position of the hallux at the time of injury, variations from the classic hyperextension injury can occur. If the force vector on the great toe at the time of impact has a medial component to it, greater injury occurs to the medial and plantar-medial ligamentous structures, as well as the tibial sesamoid complex. As a result, there is a relative contracture of the lateral structures (lateral sesamoid complex and adductor hallucis), leading to a traumatic hallux valgus and bunion deformity 14.
Figure 5. Mechanism of injury to cause a turf toe – an axial load, on a hyperextended metatarsophalangeal joint, with fixed equinus at the ankle.
[Source 15 ]Turf toe injury classification
A classification system has been modified over several years but was initially proposed by Clanton and Ford 4.
- Grade 1: Ligamentous complex sprain. Attenuation of plantar structures with localized swelling and minimal ecchymosis. It represents a micro-tear of the ligament. The first metatarsophalangeal (MTP) joint is still competent and can resist dorsiflexion. Treatment for this is symptomatic and return to sport is expected within a week.
- Grade 2: Partial ligamentous tear. Injuries include partial tear of the plantar structures with moderate swelling and restricted motion.
- Grade 3: Complete ligamentous tear. Injuries are of complete disruption to the plantar structures with hallux flexion weakness and instability. This may occur with a dorsal dislocation. There may also be concomitant injury to the articular surface of the metatarsophalangeal (MTP) joint as the proximal phalanx impacts or shears across the articular surface of the metatarsal head 16. Surgery is often indicated in this group, especially with higher-level athletes. Recovery can take up to six months 17.
Table 1. Summary of turf toe grading and treatment
| Grade | Description/Findings | Treatment | Return to Play |
|---|---|---|---|
| 1 | Attenuation of plantar structures Localized swelling Minimal ecchymosis | Symptomatic | Return as tolerated |
| 2 | Partial tear of plantar structures Moderate swelling Restricted motion due to pain | Walking boot Crutches as needed | Up to 2 weeks May need taping on return to play |
| 3 | Complete disruption of plantar structures Significant swelling/ecchymosis Hallux flexion weakness Frank instability of hallux metatarsophalangeal | Long-term immobilization in boot or cast OR Surgical reconstruction | 10 to 16 weeks depending on sport and position Likely to need taping on return to play |
Turf toe symptoms
Turf toe injury can be subtle. The injury can range from a mild sprain of the plantar ligamentous complex to complete disruption of these soft tissue structures. The signs and symptoms of turf toe can include pain, stiffness, swelling of the first metatarsophalangeal (MTP) joint with limited joint movement. Patient may describe weakness in push-off.
If turf toe is caused by repetitive actions that cause injury, the signs and symptoms will usually begin slowly and can gradually worsen. Turf toe can also be caused by a direct injury leading to damage of the bone beneath the cartilage. If direct injury is the cause, the signs and symptoms may begin suddenly and get worse over a 24-hour period.
Turf toe diagnosis
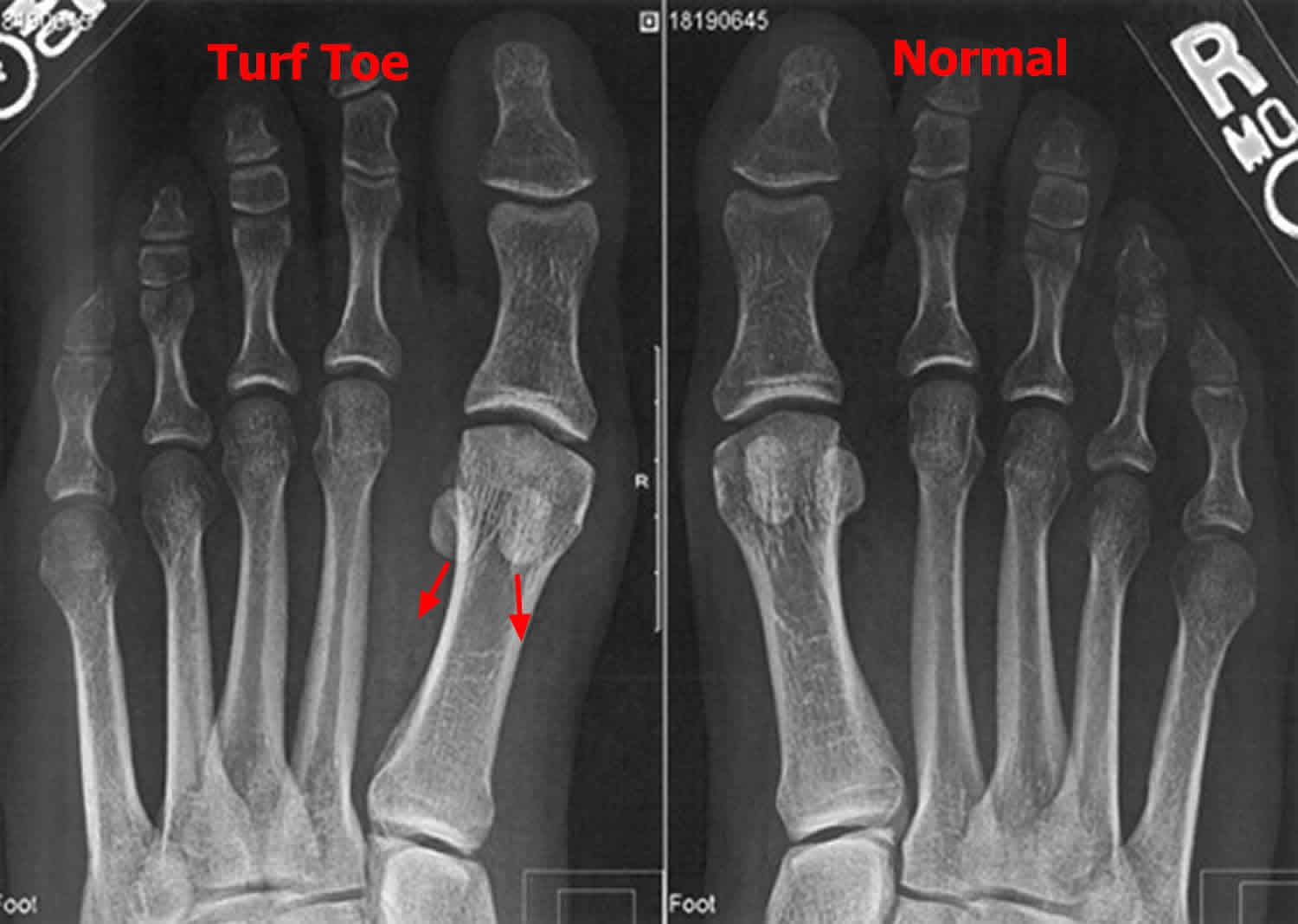
Standard weight-bearing anterior-posterior, lateral and sesamoid axial radiographs should be obtained 15. The bony structures in the radiographs are frequently normal. A small fleck of bone from the proximal phalanx or distal sesamoid may indicate a capsular disruption or avulsion. Comparison radiographs of the contralateral foot are useful to compare sesamoid location beneath the first metatarsal head. Patients with a plantar plate rupture will have proximal migration of one or both sesamoids (see Figure 6) 18. Sesamoid retraction of 3 mm or greater (compared with the intact side) has a high likelihood of having sustained a significant injury to the ligaments of the plantar plate complex 19.
A forced dorsiflexion lateral view of the hallux metatarsophalangeal (MTP) joint should be obtained if there is clinical suspicion of plantar plate injury. With complete disruption of the plantar plate the sesamoids will not track distally with great toe extension, remaining beneath the metatarsal head. Fluoroscopy can demonstrate the inability of the sesamoids to track distally with extension at the metatarsophalangeal (MTP) joint. Sesamoid motion can be compared with the contralateral side 20.
MRI is a useful and accurate tool for evaluating plantar plate injuries (Figure 7). The normal plantar plate appears as a dense band of low signal connecting the hallux sesamoids (or the metatarsal head in the case of the lesser metatarsals) to the plantar base of the proximal phalanx and is seen best on sagittal and short-axis images. MRI findings in plantar plate injury vary with the severity and acuity of the injury. Full-thickness plantar plate tears will appear as focal discontinuity of the plantar plate with retraction and a fluid gap (Figure 7), whereas sprains and partial thickness tears may show either thinning or thickening with indistinctness of the plantar plate 18.
Figure 6. Turf toe X-ray — anteroposterior radiograph of the feet demonstrating sesamoid retraction (left), compared with normal sesamoid position (right).
[Source 11 ]Figure 7. Grade 3 turf toe injury – MRI scan
[Source 15 ]Turf toe recovery time
In American national college football players, there is an average of 10.1 days lost due to injury 15. In rugby players, on average, these patients took 22 days to return to full fitness. The one patient in the series with a ruptured plantar plate required 89 days for recovery 7. However, in a grade 3 complete ligamentous tear, surgery is often indicated in this group, especially with higher-level athletes and recovery can take up to six months 17.
Turf toe prognosis
Clanton and Ford reported on surgical and non-surgical patients with a five-year follow-up: 50% described persistent symptoms of pain and stiffness at the first metatarsophalangeal joint 4. Brophy et al measured first metatarsophalangeal 21 range of motion after recovery from turf toe injury, reporting a statistically significant decrease in dorsiflexion compared with uninjured toes.
Anderson described 19 high-level competitive athletes with disabling turf toe injuries 22. Nine required operative repair and seven of these returned to full athletic participation with restoration of plantar stability. No complications from surgery were reported.
One case report in an elite footballer showed that early surgical intervention and attentive rehabilitation ensured return to first team playing after only 5.5 months. At the two-years eight-month follow-up, the patient was still playing competitive elite-level first team football 23.
Faltus et al 24 described five cases: two were grade 2 injuries and three were grade 3 injuries which required surgical repair. Recovery from the conservatively managed grade 2 athletes showed a return to elite-level sport in two to three months. In those who underwent surgical repair, return to sport was in four to five months.
Drakos et al 25 reported two cases managed surgically with repair of the plantar plate and flexor hallucis brevis and soft-tissue repair to the sesamoids. Both of these patients had a return to sport in six months. One patient had a grade 2 tear which was conservatively managed; he returned to sport in five months.
Turf toe treatment
Non-operative treatment
The early stages of treatment are similar in all grades of injury. Rest, ice, compression and elevation (R.I.C.E.) can be applied to help reduce pain and swelling. Anti-inflammatory medications can also be used to help relieve acute symptoms.
Grade 1 injury usually allows return to athletic competition as tolerated, with little or no loss of playing time. After the acute phase of injury, the great toe will benefit from taping in a slightly plantar-flexed position to limit motion and provide compression. The athlete should use a stiff-soled shoe with a turf toe plate insert or a custom orthotic with a Morton’s extension to limit hallux motion 25. If the injury is more medially based and there is concern of a traumatic hallux valgus, a toe separator between the hallux and second toes can provide further support.
For Grade 2 injuries, symptomatic treatment is warranted and may include a walking boot and protected weight-bearing. If the capsule has a substantial injury as seen on MRI but no instability on provocative testing, then casting for four to six weeks with the metatarsophalangeal joint in plantar flexion may be prudent. At three to five days post-injury, gentle range of motion can begin, with passive plantar flexion to prevent sesamoid adhesions while protecting the injured and healing plantar soft tissues 20. The patient should be carefully followed in these early stages of recovery because deformity can progress with athletic activity. Low-impact exercise, such as bicycling, elliptical training and hydrotherapy, can be attempted with toe protection. Cortisone or anaesthetic agents are not advised 24. There is some evidence to support biological therapies (such as platelet-rich plasma and autologous conditioned plasma injections) 26. Once the toe can tolerate low-impact exercise, the athlete can progress to higher impact activities, followed by explosive or push-off activities. Footwear should be adjusted to include the use of a turf toe plate or Morton’s extension 24.
Grade 3 injury may require eight weeks or longer of recovery and immobilization. The hallux metatarsophalangeal joint should have 50° to 60° of painless passive dorsiflexion before running or explosive activities are attempted 27. It may take up to six months for complete resolution of symptoms.
Turf toe surgery
Fewer than 2% of turf toe injuries require surgical intervention 2.
In complete plantar plate ruptures, a dual-incision technique allows access to the medial and lateral aspects of the plantar capsular ligamentous complex 28. Other techniques have described stabilizing the first metatarsophalangeal joint by anchoring the plantar plate to the extensor hallucis longus tendon 29. Other approaches include a medial ‘J’ incision together with plantar incisions 30.
The capsular disruption typically occurs distal to the sesamoid bones. If this is the only injury, the plantar soft-tissue structures can be primarily repaired end-to-end with non-absorbable sutures. Bone tunnels can also be used to directly attach the plantar plate to the base of the proximal phalanx 31. If a traumatic hallux valgus occurs with a primarily medial soft-tissue injury, a lateral release can be performed either percutaneously, or via the dorsal approach, to balance the hallux metatarsophalangeal joint.
If the sesamoid is fractured or fragmented, one pole of the sesamoid should be preserved, if possible. A smaller distal pole is amenable to excision. A drill hole in the larger proximal pole may allow soft-tissue repair to the sesamoid bone. If complete sesamoidectomy is necessary, then the abductor hallucis tendon should be transferred into the soft-tissue defect of the excised sesamoid to provide collagen to the site of injury and allow the abductor to function as a plantar restraint to dorsiflexion while augmenting flexion at the metatarsophalangeal joint 22.
Chronic presentation
Missed diagnoses can lead to unrestrained dorsiflexion of the injured toe. This can lead to longitudinal tears of the flexor hallucis longus tendon, hallux rigidus from repetitive joint impaction, progressive hallux valgus or varus deformity, or a cock-up toe with a hallux interphalangeal joint flexion contracture.
Surgical intervention includes fasciotomy or tendon lengthening. A Girdlestone-Taylor transfer can be performed for cock-up deformities; flexor hallucis longus can be transferred to the proximal phalanx (via drill hole and biotenodesis screw) or flexor hallucis longus can be split and re-approximated to the dorsal extensor complex. An interphalangeal fusion can be performed if the contracture is fixed. Surgical options for hallux rigidus include cheilectomy and more definitive options such as arthroplasty or fusion 28.
- Turf-toe: a shoe-surface related football injury. Bowers KD Jr, Martin RB. Med Sci Sports. 1976 Summer; 8(2):81-3.[↩][↩]
- George E, Harris HS, Dragoo JL, Hunt KJ. Incidence and risk factors for turf toe injuries in intercollegiate football: data from the National Collegiate Athletic Association Injury Surveillance System. Foot Ankle Int 2013;35:108-115[↩][↩][↩]
- Rodeo SA, O’Brien SJ, Warren RF, Barnes R, Wickiewicz TL. Turf toe: diagnosis and treatment. Phys Sportsmed 1989;17:132-147.[↩]
- Clanton TO, Ford JJ. Turf toe injury. Clin Sports Med 1994;13:731-741.[↩][↩][↩]
- McCormick JJ, Anderson RB. The great toe: failed turf toe, chronic turf toe, and complicated sesamoid injuries. Foot Ankle Clin 2009;14:135-150[↩]
- Meyers MCBB. Incidence, causes, and severity of high school football injuries on FieldTurf versus natural grass: a 5-year prospective study. Am J Sports Med 2004;32:1626-1638.[↩]
- Pearce CJ, Brooks JHM, Kemp SPT, Calder JDF. The epidemiology of foot injuries in professional rugby union players. Foot Ankle Surg 2011;17:113-118.[↩][↩]
- Aper RL, Saltzman CL, Brown TD. The effect of hallux sesamoid excision on the flexor hallucis longus moment arm. Clin Orthop Relat Res. 1996;325:209-217[↩]
- Stokes IA, Hutton WC, Stott JR, et al. Forces under the hallux valgus foot before and after surgery. Clin Orthop Relat Res. 1979;142:64-72[↩]
- Nigg BM. Biomechanical aspects of running. In: Nigg BM, editor. , ed. Biomechanics of Running Shoes. Champaign, IL: Human Kinetics; 1986:1-25[↩]
- McCormick JJ, Anderson RB. Turf toe: anatomy, diagnosis, and treatment. Sports Health. 2010;2(6):487-94. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3438874/[↩][↩][↩]
- George E, Harris HS, Dragoo JL, Hunt KJ. Incidence and risk factors for turf toe injuries in intercollegiate football: data from the National Collegiate Athletic Association Injury Surveillance System. Foot Ankle Int 2013;35:108-115.[↩]
- Mullen JE, O’Malley MJ. Sprains – Residual instability of subtalar, Lisfranc joints, and turf toe. Clin Sports Med 2004;23:97-121.[↩]
- Fabeck LG, Zekhnini C, Farrokh D, et al. Traumatic hallux valgus following rupture of the medial collateral ligament of the first metatarsophalangeal joint: a case report. J Foot Ankle Surg 2002;41:125-128.[↩]
- Najefi AA, Jeyaseelan L, Welck M. Turf toe: A clinical update. EFORT Open Rev. 2018;3(9):501-506. Published 2018 Sep 24. doi:10.1302/2058-5241.3.180012 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6174855/[↩][↩][↩][↩]
- Nihal A, Trepman E, Nag D. First ray disorders in athletes. Sports Med Arthrosc Rev 2009;17:160-166.[↩]
- Coughlin MJ, Kemp TJ, Hirose CB. Turf toe: soft tissue and osteocartilaginous injury to the first metatarsophalangeal joint. Phys Sportsmed 2010;38:91-100.[↩][↩]
- Schein AJ, Skalski MR, Patel DB, et al. Turf toe and sesamoiditis: what the radiologist needs to know. Clin Imaging 2015;39:380-389.[↩][↩]
- Waldrop NE, 3rd, Zirker CA, Wijdicks CA, Laprade RF, Clanton TO. Radiographic evaluation of plantar plate injury: an in vitro biomechanical study. Foot Ankle Int 2013;34:403-408.[↩]
- McCormick JJ, Anderson RB. Turf toe: anatomy, diagnosis, and treatment. Sports Health 2010;2:487-494.[↩][↩]
- Brophy RH, Gamradt SC, Ellis SJ, et al. Effect of turf toe on foot contact pressures in professional American football players. Foot Ankle Int 2009;30:405-409.[↩]
- Anderson R. Turf toe injuries of the hallux metatarsophalangeal joint. Tech Foot Ankle Surg 2002;1:102-111.[↩][↩]
- Roche AJ, Calder JD. An atraumatic turf toe in an elite soccer player – A stress related phenomenon? Foot Ankle Surg 2014;20:71-73.[↩]
- Faltus J, Mullenix K, Moorman CT, Beatty K, Easley ME. Case series of first metatarsophalangeal joint injuries in division 1 college athletes. Sports Health 2014;6:519-526.[↩][↩][↩]
- Drakos MC, Fiore R, Murphy C, DiGiovanni CW. Plantar-plate disruptions: “the severe turf-toe injury.” Three cases in contact athletes. J Athl Train 2015;50:553-560[↩][↩]
- Mares AV, Schreiter R, van Eck CF, Blanc R, Musahl V. Management of athletic turf toe using biologics. Oper Tech Orthop 2016;26:117-121.[↩]
- McCormick JJ, Anderson RB. Rehabilitation following turf toe injury and plantar plate repair. Clin Sports Med 2010;29:313-323.[↩]
- McCormick JJ, Anderson RB. The great toe: failed turf toe, chronic turf toe, and complicated sesamoid injuries. Foot Ankle Clin 2009;14:135-150.[↩][↩]
- Lui TH. Stabilization of first metatarsophalangeal instability with plantar plate tenodesis. Foot Ankle Surg 2008;14:211-214.[↩]
- McCormick JJ, Anderson RB. Turf toe: anatomy, diagnosis, and treatment. Sports Health 2010;2:487-494[↩]
- Doty JF, C MJ. Turf toe repair: a technical note. Foot Ankle Spec 2013;6:452-456[↩]