Contents
Knee injuries
Each year, knee injuries is also responsible for an estimated 1.3 million visits to emergency departments in the United States 1. Your knees provide stable support for the body and allow the legs to bend and straighten. The knee is the largest joint in the body and is easily injured. The knee has 4 main types of tissues: bones, ligaments, cartilage and tendons (see Figures 1 to 3). Any of these important types of tissue can be damaged through injury. The anatomic characteristics of the knee, its exposure to external forces and the functional demands placed on the knee joint may explain the frequency of injury. Awkward movements, falls and collisions, sudden twists, excessive force or overuse can result in a range of injuries to the knee joint and the structures supporting it.
Common knee injuries include:
- sprains (an over-stretching of ligaments in the knee)
- strains (over-stretching of muscles and tendons)
- damage to the cartilage that lines the knee
- irritation to the kneecap joint
Less common injuries to the knee include:
- fractures (usually caused by sudden trauma or a direct blow, twisting, or falling on the knee)
- kneecap dislocations
- knee joint dislocations (uncommon as it requires a great force)
Knee damage can also occur from underlying disease such as osteoarthritis, rheumatoid arthritis and systemic lupus erythematosus.
Prompt medical attention for any knee injury increases the chances of a full recovery. Treatment options include physiotherapy, arthroscopic surgery and open surgery.
Knee injuries key facts to remember:
- Common knee injuries include ligament, tendon and cartilage tears, and patello-femoral pain syndrome.
- Prompt medical attention for any knee injury increases the chances of a full recovery.
- Treatment options include physiotherapy, arthroscopic surgery and open surgery.
Where to get help:
- Your doctor
- Physiotherapist
- Sports physician
Anatomy of the knee
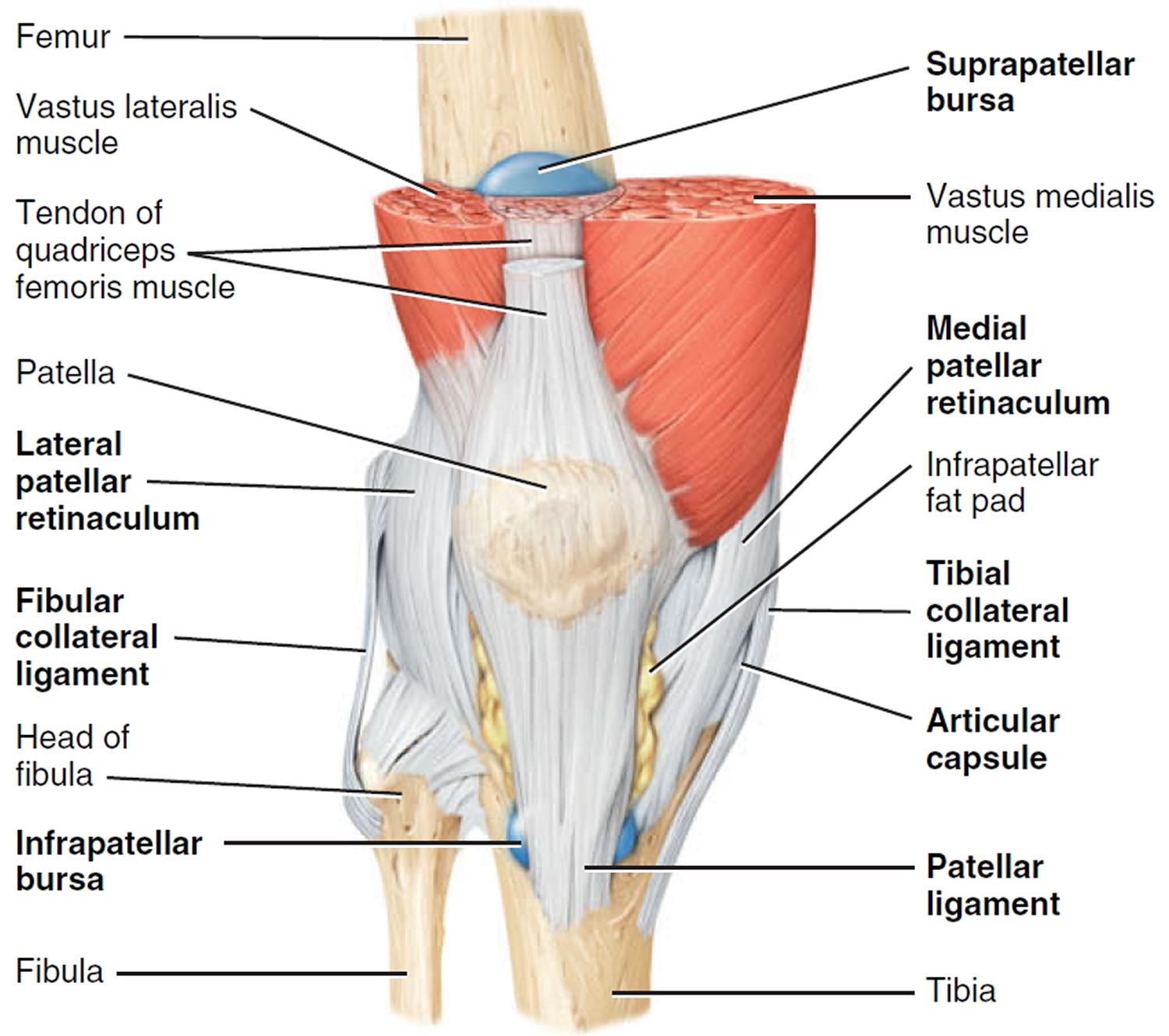
The anatomy and function of the knee are quite complex, and only the basics are described in this article. The knee is a hinge joint, situated between the thigh bone (femur) and shin bones (tibia and fibula) (Figure 1).
The knee is the largest joint in the body, and one of the most easily injured. It is made up of four main things: bones, cartilage, ligaments, and tendons.
- Bones. Three bones meet to form your knee joint: your thighbone (femur), shinbone (tibia), and kneecap (patella).
- Articular cartilage. The ends of the femur and tibia, and the back of the patella are covered with articular cartilage. This slippery substance helps your knee bones glide smoothly across each other as you bend or straighten your leg.
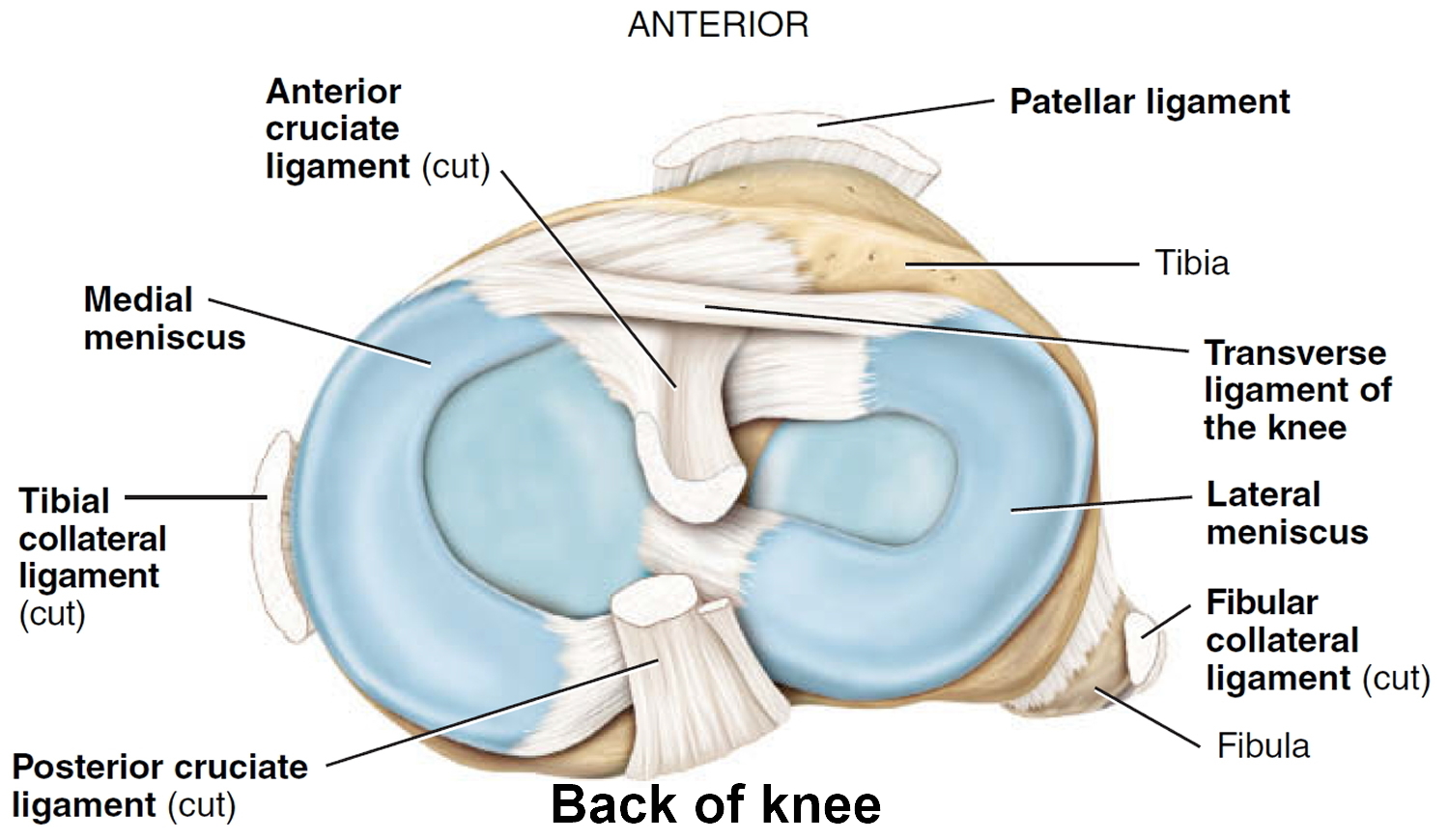
- Meniscus. Two wedge-shaped pieces of meniscal cartilage act as “shock absorbers” between your femur and tibia. Different from articular cartilage, the meniscus is tough and rubbery to help cushion and stabilize the joint. When people talk about torn cartilage in the knee, they are usually referring to torn meniscus.
- Ligaments. Bones are connected to other bones by ligaments. The four main ligaments in your knee act like strong ropes to hold the bones together and keep your knee stable.
- Collateral Ligaments. These are found on the sides of your knee. The medial collateral ligament is on the inside of your knee, and the lateral collateral ligament is on the outside. They control the sideways motion of your knee and brace it against unusual movement.
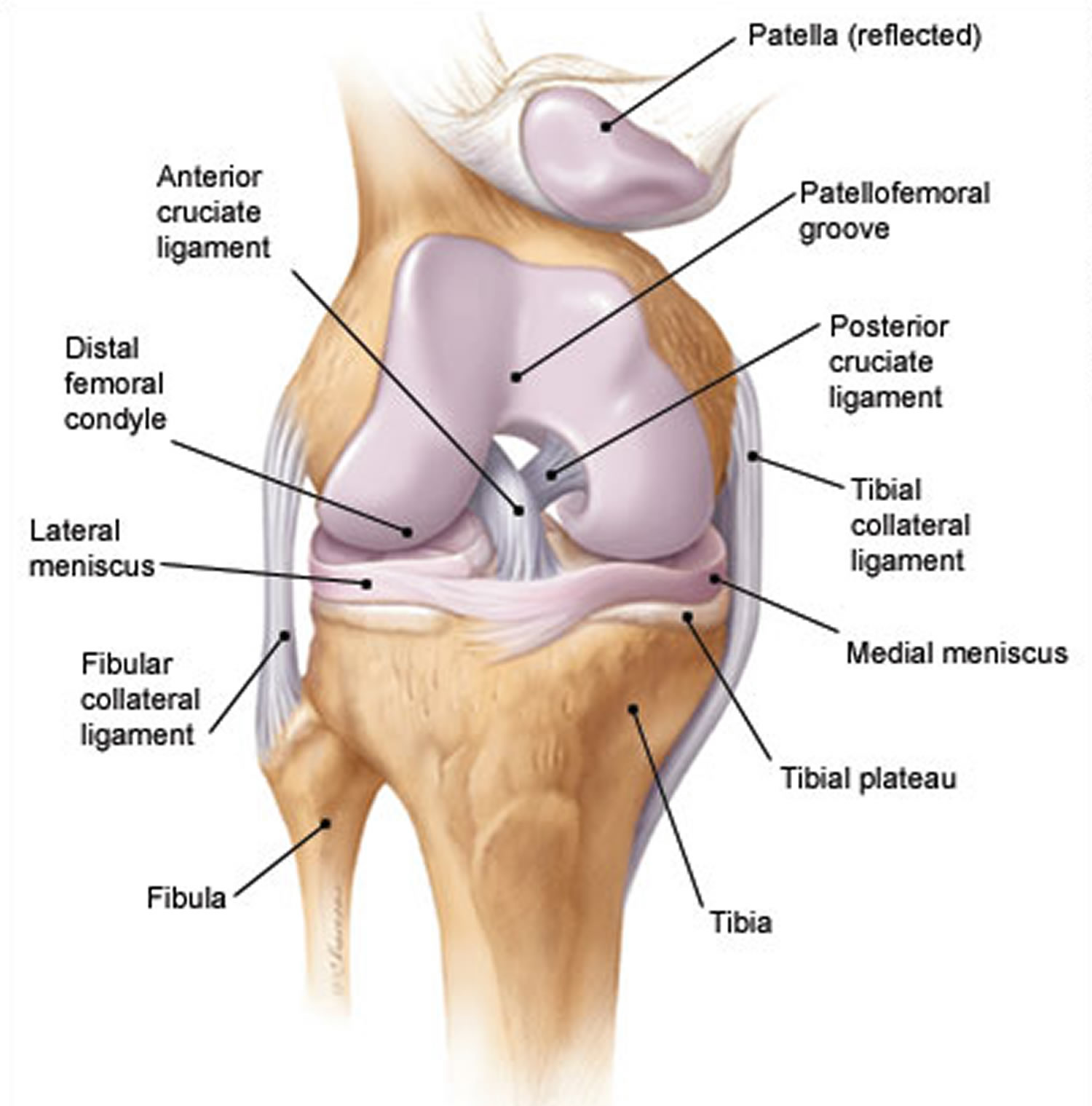
- Cruciate ligaments. These are found inside your knee joint. They cross each other to form an “X” with the anterior cruciate ligament in front and the posterior cruciate ligament in back. The cruciate ligaments control the back and forth motion of your knee.
- Tendons. Muscles are connected to bones by tendons. The quadriceps tendon connects the muscles in the front of your thigh to your patella. Stretching from your patella to your shinbone is the patellar tendon.
Contraction of the muscles on the front of the thigh (quadriceps) straightens the leg, while contraction of the muscles on the back of the thigh (the hamstrings) allows the leg to bend at the knee. The end of the femur rests in the shallow cup of the tibia (the tibial plateau), cushioned by a thick layer of cartilage (medial meniscus and lateral meniscus).
The bony structures of the knee include the distal femoral condyles, proximal tibial plateau and patella (Figure 1). The tibial plateau articulates with the femoral condyles, and the patellofemoral groove (located anteriorly between the femoral condyles) accepts the patella. At the front of the knee joint, the kneecap or patella sits in a groove at the lower end of the femur. The tibia and patella do not articulate. The gliding motion of the patella across the femur allows smooth extension at the knee and increases the mechanical advantage of the quadriceps. The bones are held in place by tough bands of connective tissue called ligaments. The entire joint is enclosed inside a tough capsule lined with a membrane and filled with lubricating synovial fluid. Extra capsules of fluid, known as bursae, offer extra cushioning.
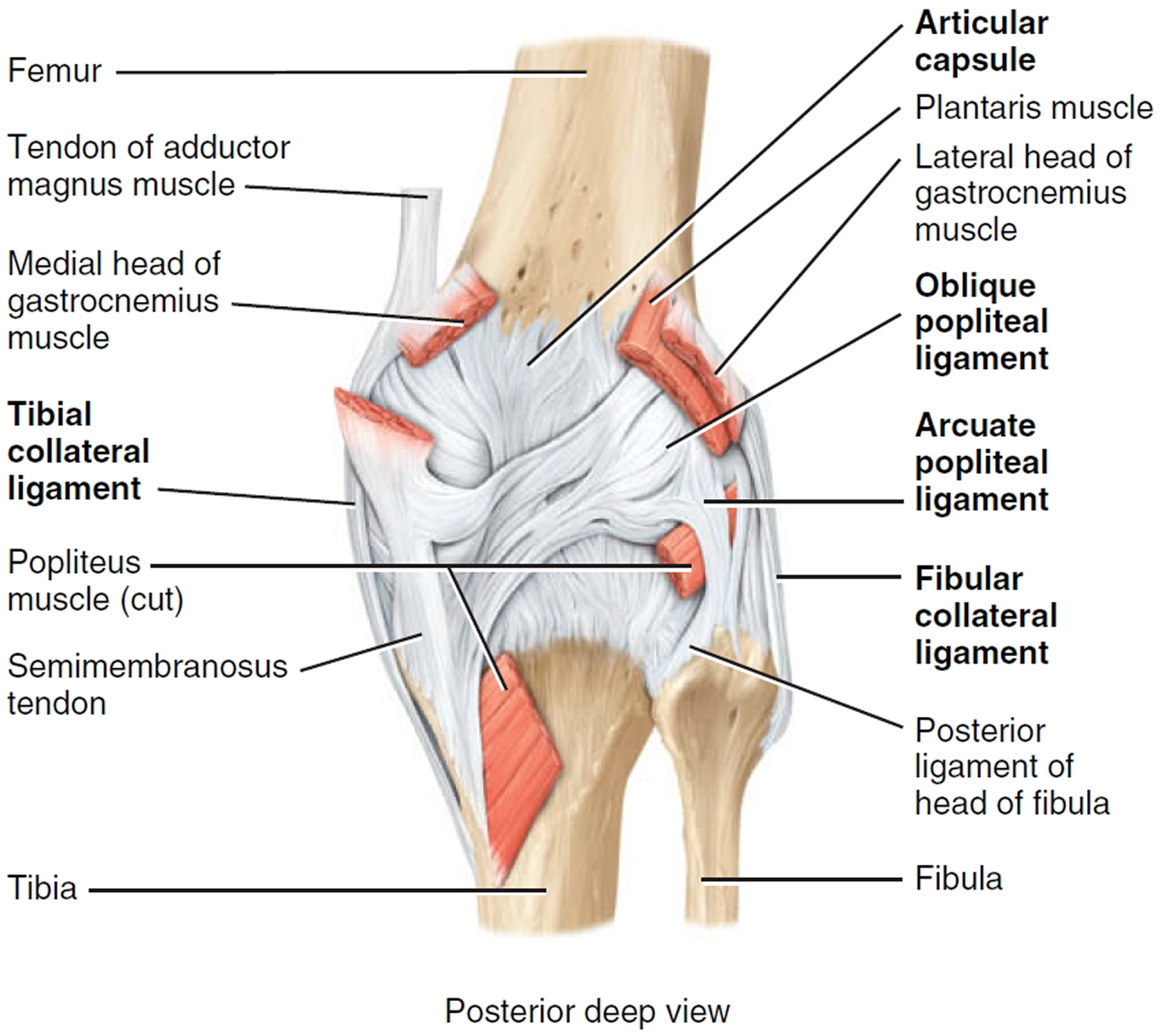
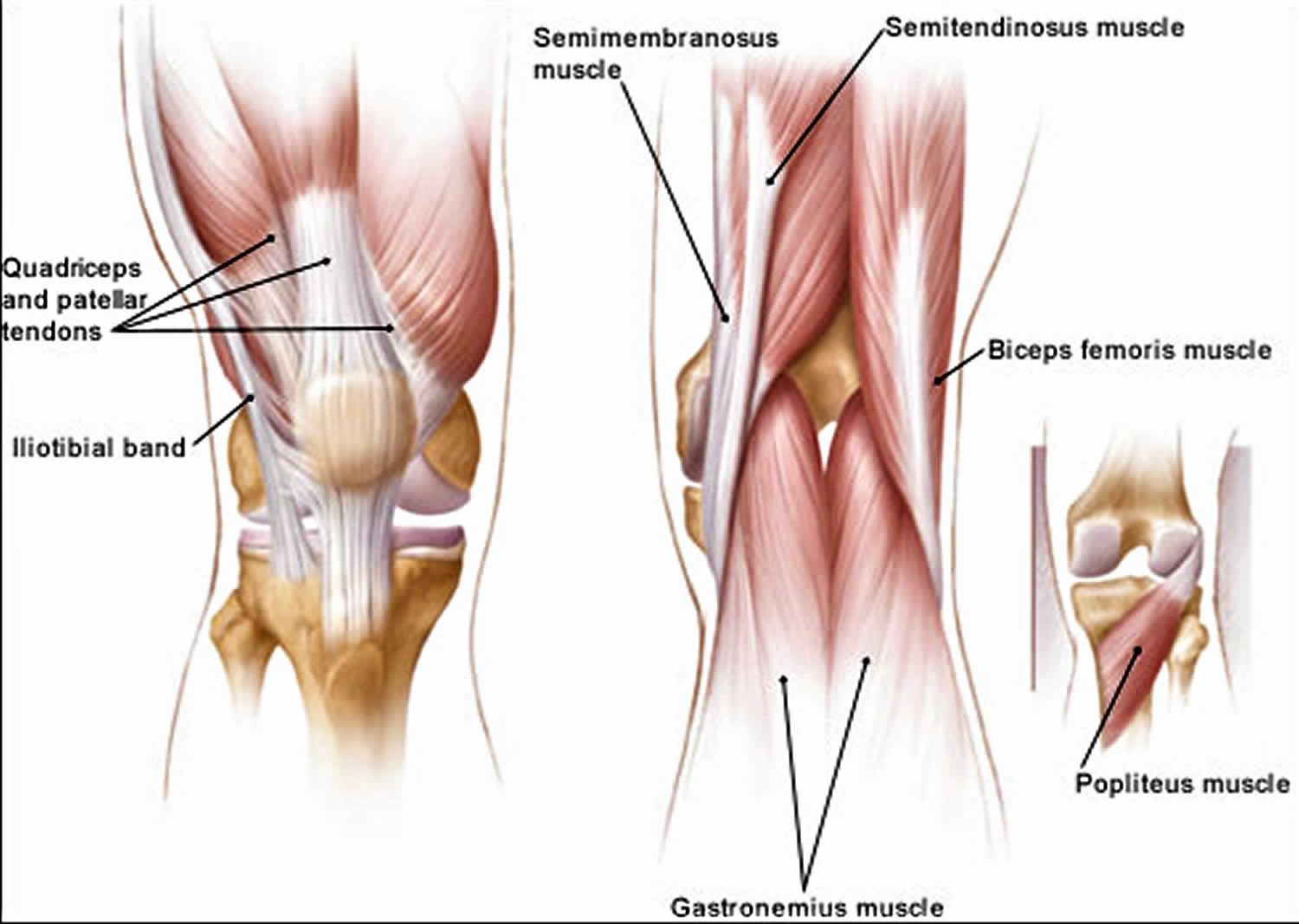
The extra-articular muscle-tendon units include the quadriceps and patellar tendons (responsible for knee extension), medial and lateral hamstrings (chiefly responsible for knee flexion), gastrocnemius muscle, popliteal ligament and iliotibial band (Figure 3).
The extra-articular ligamentous structures include the tibial and fibular collateral ligaments (Figure 1). These ligaments act as the principal extra-articular static stabilizing structures (i.e., they provide stability for the medial and lateral aspects of the knee).
The intra-articular structures include the medial and lateral menisci and the anterior and posterior cruciate ligaments (Figure 1). The menisci are fibrocartilaginous wedges that rim and cushion each tibiofemoral articulation. The anterior and posterior cruciate ligaments provide stability for the knee joint.
Figure 1. Anatomy of the knee
Figure 2. Knee joint anatomy posterior view
Mechanism of the knee injury
It is important to know if the patient sustained a direct blow to the knee, if the foot was planted at the time of injury, if the patient was decelerating or stopping suddenly, if the patient was landing from a jump, if there was a twisting component to the injury, and if hyperextension occurred.
A direct blow to the knee can cause serious injury. Anterior force applied to the proximal tibia with the knee in flexion (e.g., when the knee hits the dashboard in an automobile accident) can cause injury to the posterior cruciate ligament. The medial collateral ligament is most commonly injured as a result of direct lateral force to the knee (e.g., clipping in football); this force creates a valgus load on the knee joint and can result in rupture of the medial collateral ligament. Conversely, a medial blow that creates a varus load can injure the lateral collateral ligament.
Noncontact forces also are an important cause of knee injury. Quick stops and sharp cuts or turns create significant deceleration forces that can sprain or rupture the anterior cruciate ligament. Hyperextension can result in injury to the anterior cruciate ligament or posterior cruciate ligament. Sudden twisting or pivoting motions create shear forces that can injure the meniscus. A combination of forces can occur simultaneously, causing injury to multiple structures.
Types of knee injuries
Possible Causes of Knee Pain by Anatomic Site
- Anterior knee pain
- Patellar subluxation or dislocation
- Tibial apophysitis (Osgood-Schlatter lesion)
- Jumper’s knee (patellar tendonitis)
- Patellofemoral pain syndrome (chondromalacia patellae)
- Medial knee pain
- Medial collateral ligament sprain
- Medial meniscal tear
- Pes anserine bursitis
- Medial plica syndrome
- Lateral knee pain
- Lateral collateral ligament sprain
- Lateral meniscal tear
- Iliotibial band tendonitis
- Posterior knee pain
- Popliteal cyst (Baker’s cyst)
- Posterior cruciate ligament injury
Table 1. Common Causes of Knee Pain by Age Group
Children and adolescents
| Adults
| Older adults
|
Knee Ligament Injuries
The knee joint is held together by tough bands of connective tissue called ligaments. Sudden twists or excessive force on the knee joint, commonly caused by repeated jumping or coming to a rapid halt while running, can stretch ligaments beyond their capacity. Torn ligaments can bleed into the knee and typically cause swelling, pain and joint laxity. The anterior cruciate ligament (ACL) situated in the center of the knee joint is the knee ligament commonly injured. A ruptured ACL (anterior cruciate ligament) does not heal by itself and may require reconstructive surgery.
Anterior cruciate ligament injury
Rupture of the anterior cruciate ligament (ACL) is a serious injury, and the diagnosis may be missed 3. Injury to the anterior cruciate ligament usually occurs because of noncontact deceleration forces, as when a runner plants one foot and sharply turns in the opposite direction. Resultant valgus stress on the knee leads to anterior displacement of the tibia and sprain or rupture of the ligament 4. The patient usually reports hearing or feeling a “pop” at the time of the injury, and must cease activity or competition immediately. Swelling of the knee within two hours after the injury indicates rupture of the ligament and consequent hemarthrosis (bleeding inside the knee joint).
Anterior cruciate ligament injury symptoms
When you injure your anterior cruciate ligament, you might hear a “popping” noise and you may feel your knee give out from under you. Other typical symptoms include:
- Pain with swelling. Within 24 hours, your knee will swell. If ignored, the swelling and pain may resolve on its own. However, if you attempt to return to sports, your knee will probably be unstable and you risk causing further damage to the cushioning cartilage (meniscus) of your knee.
- Loss of full range of motion
- Tenderness along the joint line
- Discomfort while walking
On physical examination, the patient has a moderate to severe joint effusion that limits range of motion. The anterior drawer test may be positive, but can be negative because of hemarthrosis and guarding by the hamstring muscles. The Lachman test should be positive and is more reliable than the anterior drawer test (watch the Lachman test video below).
The immediate development of a hemorrhagic effusion is an important point in the history of anterior cruciate ligament (ACL) injury. The stability of the ACL may be clinically assessed with the use of the Lachman test (modified anterior drawer test). More than 90 percent of ACL injuries can be detected based on the history and physical examination 5. However, even the best specialists may fail to recognize the joint laxity of an ACL injury. Therefore, radiographic signs are useful in making the diagnosis.
ACL injury has three main radiographic signs: (1) avulsion of the intercondylar tubercle, (2) anterior displacement of the tibia with respect to the femur, termed the “radiographic drawer sign,” and (3) Segond fracture (a thin sliver of bone avulsed from the proximal lateral tibia with the lateral capsular ligament), termed the “lateral capsular sign” 6. Note, however, that these radiographic signs are frequently absent in patients with ACL injuries 7. MRI of the knee is indicated as part of a presurgical evaluation.
The gold standard for the diagnosis of ruptured ACL is arthroscopy. Compared with this procedure, MRI has a diagnostic accuracy of more than 90 percent. In addition, ultrasound examination has been shown to be a useful and inexpensive mode of detecting a ruptured ACL in the clinical setting of a traumatic hemarthrosis 8.
Anterior cruciate ligament injury treatment
Treatment for an ACL tear will vary depending upon the patient’s individual needs. For example, the young athlete involved in agility sports will most likely require surgery to safely return to sports. The less active, usually older, individual may be able to return to a quieter lifestyle without surgery.
Nonsurgical Treatment
A torn ACL will not heal without surgery. But nonsurgical treatment may be effective for patients who are elderly or have a very low activity level. If the overall stability of the knee is intact, your doctor may recommend simple, nonsurgical options.
- Bracing. Your doctor may recommend a brace to protect your knee from instability. To further protect your knee, you may be given crutches to keep you from putting weight on your leg.
- Physical therapy. As the swelling goes down, a careful rehabilitation program is started. Specific exercises will restore function to your knee and strengthen the leg muscles that support it.
What happens naturally with an ACL injury without surgical intervention varies from patient to patient and depends on the patient’s activity level, degree of injury and instability symptoms.
The prognosis for a partially torn ACL is often favorable, with the recovery and rehabilitation period usually at least 3 months. However, some patients with partial ACL tears may still have instability symptoms. Close clinical follow-up and a complete course of physical therapy helps identify those patients with unstable knees due to partial ACL tears.
Complete ACL ruptures have a much less favorable outcome without surgical intervention. After a complete ACL tear, some patients are unable to participate in cutting or pivoting-type sports, while others have instability during even normal activities, such as walking. There are some rare individuals who can participate in sports without any symptoms of instability. This variability is related to the severity of the original knee injury, as well as the physical demands of the patient.
About half of ACL injuries occur in combination with damage to the meniscus, articular cartilage or other ligaments. Secondary damage may occur in patients who have repeated episodes of instability due to ACL injury. With chronic instability, a large majority of patients will have meniscus damage when reassessed 10 or more years after the initial injury. Similarly, the prevalence of articular cartilage lesions increases in patients who have a 10-year-old ACL deficiency.
Surgical Treatment
Rebuilding the ligament. Most ACL tears cannot be sutured (stitched) back together. To surgically repair the ACL and restore knee stability, the ligament must be reconstructed. Your doctor will replace your torn ligament with a tissue graft. This graft acts as a scaffolding for a new ligament to grow on.
Grafts can be obtained from several sources. Often they are taken from the patellar tendon, which runs between the kneecap and the shinbone. Hamstring tendons at the back of the thigh are a common source of grafts. Sometimes a quadriceps tendon, which runs from the kneecap into the thigh, is used. Finally, cadaver graft (allograft) can be used.
There are advantages and disadvantages to all graft sources. You should discuss graft choices with your own orthopaedic surgeon to help determine which is best for you.
Because the regrowth takes time, it may be six months or more before an athlete can return to sports after surgery.
Procedure. Surgery to rebuild an anterior cruciate ligament is done with an arthroscope using small incisions. Arthroscopic surgery is less invasive. The benefits of less invasive techniques include less pain from surgery, less time spent in the hospital, and quicker recovery times.
Rehabilitation
Whether your treatment involves surgery or not, rehabilitation plays a vital role in getting you back to your daily activities. A physical therapy program will help you regain knee strength and motion.
If you have surgery, physical therapy first focuses on returning motion to the joint and surrounding muscles. This is followed by a strengthening program designed to protect the new ligament. This strengthening gradually increases the stress across the ligament. The final phase of rehabilitation is aimed at a functional return tailored for the athlete’s sport.
Posterior cruciate ligament injury
Injuries of the posterior cruciate ligament (PCL) are relatively uncommon, apparently because this is the strongest major knee ligament. The mechanism of isolated PCL (posterior cruciate ligament) injury is blunt trauma to the anterior proximal tibia (“dashboard injury”).
Posterior cruciate ligament injury symptoms
The typical symptoms of a posterior cruciate ligament injury are:
- Pain with swelling that occurs steadily and quickly after the injury
- Swelling that makes the knee stiff and may cause a limp
- Difficulty walking
- The knee feels unstable, like it may “give out”
Several maneuvers can be helpful in diagnosing PCL injuries. In one study 9, the gravity sign near extension correctly diagnosed PCL injury in 20 of 24 patients, and active reduction of posterior tibial subluxation correctly identified PCL injury in 18 of 24 patients. The gravity test is performed at 20 degrees of knee flexion. Neither maneuver requires anesthesia.
Nonetheless, clinical diagnosis may be difficult, and radiographic signs are important. The most common radiographic sign of PCL injury is avulsion at the site of the ligament’s origin on the posterior tibia. Less commonly, avulsion can be seen at the site of PCL insertion at the medial femoral condyle. When the PCL fails, posterior sagging of the tibia relative to the femur may be seen on the lateral radiograph.
MRI is accurate in diagnosing PCL injuries. It can also show associated injuries of the ACL and medial collateral ligament (MCL), as well as bone contusions.
Posterior cruciate ligament treatment
Nonsurgical Treatment
If you have injured just your posterior cruciate ligament, your injury may heal quite well without surgery Your doctor may recommend simple, nonsurgical options.
- RICE. When you are first injured, the RICE method – rest, ice, gentle compression and elevation — can help speed your recovery.
- Immobilization. Your doctor may recommend a brace to prevent your knee from moving. To further protect your knee, you may be given crutches to keep you from putting weight on your leg.
- Physical therapy. As the swelling goes down, a careful rehabilitation program is started. Specific exercises will restore function to your knee and strengthen the leg muscles that support it. Strengthening the muscles in the front of your thigh (quadriceps) has been shown to be a key factor in a successful recovery.
Surgical Treatment
Your doctor may recommend surgery if you have combined injuries. For example, if you have dislocated your knee and torn multiple ligaments including the posterior cruciate ligament, surgery is almost always necessary.
Rebuilding the ligament. Because sewing the ligament ends back together does not usually heal, a torn posterior cruciate ligament must be rebuilt. Your doctor will replace your torn ligament with a tissue graft. This graft is taken from another part of your body, or from another human donor (cadaver). It can take several months for the graft to heal into your bone.
Procedure. Surgery to rebuild a posterior cruciate ligament is done with an arthroscope using small incisions. Arthroscopic surgery is less invasive. The benefits of less invasive techniques include less pain from surgery, less time spent in the hospital, and quicker recovery times.
Surgical procedures to repair posterior cruciate ligaments continue to improve. More advanced techniques help patients resume a wider range of activities after rehabilitation.
Rehabilitation
Whether your treatment involves surgery or not, rehabilitation plays a vital role in getting you back to your daily activities. A physical therapy program will help you regain knee strength and motion. If you had surgery, physical therapy will begin 1 to 4 weeks after your procedure.
How long it takes you to recover from a posterior cruciate ligament injury will depend on the severity of your injury. Combined injuries often have a slow recovery, but most patients do well over time.
If your injury requires surgery, it may be several weeks before you return to a desk job – perhaps months if your job requires a lot of activity. Full recovery typically requires 6 to 12 months.
Although it is a slow process, your commitment to therapy is the most important factor in returning to all the activities you enjoy.
Medial collateral ligament injury
Injury to the medial collateral ligament is fairly common and is usually the result of acute trauma. Knee injuries involving valgus force, with or without a rotational element, are suggestive of medial collateral ligament (MCL) injury. The patient reports a misstep or collision that places valgus stress on the knee, followed by immediate onset of pain and swelling at the medial aspect of the knee 4. The physical examination may demonstrate effusion or local soft tissue swelling and ecchymosis 3. Injuries to the MCL (Medial collateral ligament) usually occur at the ligament’s proximal origin. Therefore, tenderness is usually localized along the distal femur and extends to the joint line 10.
On physical examination, the patient with medial collateral ligament injury has point tenderness at the medial joint line. Valgus stress testing of the knee flexed to 30 degrees reproduces the pain (watch the valgus stress test video below). A clearly defined end point on valgus stress testing indicates a grade 1 or grade 2 sprain, whereas complete medial instability indicates full rupture of the ligament (grade 3 sprain).
The major secondary radiographic sign of medial collateral ligament (MCL) injury is widening of the medial joint space. A lateral tibial plateau fracture may also suggest MCL injury.
MRI demonstrates medial collateral ligament (MCL) injury as well as associated injuries of the medial meniscus, capsule and ACL.
Injuries to the MCL rarely require surgery.
Nonsurgical treatment
- Ice. Icing your injury is important in the healing process. The proper way to ice an injury is to use crushed ice directly to the injured area for 15 to 20 minutes at a time, with at least 1 hour between icing sessions. Chemical cold products (“blue” ice) should not be placed directly on the skin and are not as effective.
- Bracing. Your knee must be protected from the same sideways force that caused the injury. You may need to change your daily activities to avoid risky movements. Your doctor may recommend a brace to protect the injured ligament from stress. To further protect your knee, you may be given crutches to keep you from putting weight on your leg.
- Physical therapy. Your doctor may suggest strengthening exercises. Specific exercises will restore function to your knee and strengthen the leg muscles that support it.
Surgical treatment
Most isolated collateral ligament injuries can be successfully treated without surgery. If the collateral ligament is torn in such a way that it cannot heal or is associated with other ligament injuries, your doctor may suggest surgery to repair it.
Return to sports
Once your range of motion returns and you can walk without a limp, your doctor may allow functional progression. This is a gradual, progressive return to sports activities.
For example, if you play soccer, your functional progression may start as a light jog. Then you progress to a sprint, and eventually to full running and kicking the ball.
Your doctor may suggest a knee brace during sports activities, depending on the severity of your sprain.
Lateral collateral ligament injury
Injuries of the lateral collateral ligamentous complex (LCL) are estimated to account for only 5 percent of all knee ligament injuries 3. Injury of the lateral collateral ligament is much less common than injury of the medial collateral ligament (MCL). Lateral collateral ligament sprain usually results from varus stress to the knee, as occurs when a runner plants one foot and then turns toward the ipsilateral knee 11. The patient reports acute onset of lateral knee pain that requires prompt cessation of activity.
On physical examination, point tenderness is present at the lateral joint line. Instability or pain occurs with varus stress testing of the knee flexed to 30 degrees (watch the varus stress test video below). Radiographs are not usually indicated. Radiographic signs suggesting LCL (lateral collateral ligament) injury include lateral joint space widening and medial tibial plateau fracture 3.
If you have injured just your LCL, treatment is similar to an MCL sprain (see above). But if your LCL injury involves other structures in your knee, your treatment will address those, as well.
Knee cartilage tears
The knee joint is bolstered on both sides by additional strips of cartilage, called ‘meniscus’ or semilunar cartilages. One of the most common knee injuries is a torn or split meniscus. Severe impact or sudden twisting injury, especially during weight bearing exercise such as may occur when a runner suddenly changes direction, can tear the meniscus 12. Meniscal tear also may occur in association with a prolonged degenerative process, particularly in a patient with an anterior cruciate ligament–deficient knee. Tears of the meniscus can also occur in older people due to wear and tear. Symptoms include swelling, pain and the inability to straighten the leg. The damaged cartilage can be surgically trimmed or even removed without causing any joint instability.
Symptoms of meniscus tear
You might feel a “pop” when you tear a meniscus. Most people can still walk on their injured knee. Many athletes keep playing with a tear. Over 2 to 3 days, your knee will gradually become more stiff and swollen.
The most common symptoms of meniscus tear are:
- Pain
- Stiffness and swelling
- Catching or locking of your knee
- The sensation of your knee “giving way”
- You are not able to move your knee through its full range of motion
Without treatment, a piece of meniscus may come loose and drift into the joint. This can cause your knee to slip, pop, or lock.
Patient usually reports recurrent knee pain and episodes of catching or locking of the knee joint, especially with squatting or twisting of the knee.
On physical examination, a mild effusion is usually present, and there is tenderness at the medial or lateral joint line. Atrophy of the vastus medialis obliquus portion of the quadriceps muscle also may be noticeable. The McMurray test may be positive (watch McMurray test video below), but a negative test does not eliminate the possibility of a meniscal tear.
Plain-film radiographs usually are negative and seldom are indicated. MRI is the radiologic test of choice because it demonstrates most significant meniscal tears.
Knee cartilage tear treatment
How your orthopaedic surgeon treats your tear will depend on the type of tear you have, its size, and location.
The outside one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a blood supply. Without nutrients from blood, tears in this “white” zone cannot heal. These complex tears are often in thin, worn cartilage. Because the pieces cannot grow back together, tears in this zone are usually surgically trimmed away.
Along with the type of tear you have, your age, activity level, and any related injuries will factor into your treatment plan.
Nonsurgical Treatment
If your tear is small and on the outer edge of the meniscus, it may not require surgical repair. As long as your symptoms do not persist and your knee is stable, nonsurgical treatment may be all you need.
The R.I.C.E. protocol is effective for most sports-related injuries. RICE stands for Rest, Ice, Compression, and Elevation.
- Rest. Take a break from the activity that caused the injury. Your doctor may recommend that you use crutches to avoid putting weight on your leg.
- Ice. Use cold packs for 20 minutes at a time, several times a day. Do not apply ice directly to the skin.
- Compression. To prevent additional swelling and blood loss, wear an elastic compression bandage.
- Elevation. To reduce swelling, recline when you rest, and put your leg up higher than your heart.
Non-steroidal anti-inflammatory medicines. Drugs like aspirin and ibuprofen reduce pain and swelling.
Surgical Treatment
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Knee arthroscopy is one of the most commonly performed surgical procedures. In it, a miniature camera is inserted through a small incision (portal). This provides a clear view of the inside of the knee. Your orthopaedic surgeon inserts miniature surgical instruments through other portals to trim or repair the tear.
- Partial meniscectomy. In this procedure, the damaged meniscus tissue is trimmed away.
- Meniscus repair. Some meniscus tears can be repaired by suturing (stitching) the torn pieces together. Whether a tear can be successfully treated with repair depends upon the type of tear, as well as the overall condition of the injured meniscus. Because the meniscus must heal back together, recovery time for a repair is much longer than from a meniscectomy.
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
For the most part, rehabilitation can be carried out at home, although your doctor may recommend physical therapy. Rehabilitation time for a meniscus repair is about 3 months. A meniscectomy requires less time for healing — approximately 3 to 4 weeks.
Knee tendon tears
The muscles are anchored to the knee joints with tendons. Overstretched tendons can tear and bleed, but these injuries tend to heal by themselves without the need for surgery.
The quadriceps and patellar tendons can be stretched and torn. Although anyone can injure these tendons, tears are more common among middle-aged people who play running or jumping sports. Falls, direct force to the front of the knee, and landing awkwardly from a jump are common causes of knee tendon injuries.
Patellar tendon tear
Tendons are strong cords of fibrous tissue that attach muscles to bones. The patellar tendon attaches the bottom of the kneecap (patella) to the top of the shinbone (tibia). It is actually a ligament that connects to two different bones, the patella and the tibia. The patella is attached to the quadriceps muscles by the quadriceps tendon. The patellar tendon works with the quadriceps muscles to straighten your leg.
Patellar tendon tears can be either partial or complete.
- Partial tears. Many tears do not completely disrupt the soft tissue. This is similar to a rope stretched so far that some of the fibers are frayed, but the rope is still in one piece.
- Complete tears. A complete tear will disrupt the soft tissue into two pieces. When the patellar tendon is completely torn, the tendon is separated from the kneecap. Without this attachment, you cannot straighten your knee.
Small tears of the patellar tendon can make it difficult to walk and participate in other daily activities. A large tear of the patellar tendon is a disabling injury. It usually requires surgery and physical therapy to regain full knee function.
Most people require surgery to regain knee function. Surgical repair reattaches the torn tendon to the kneecap. People who require surgery do better if the repair is performed soon after the injury. Early repair may prevent the tendon from scarring and tightening into a shortened position.
When a patellar tendon tears there is often a tearing or popping sensation. Pain and swelling typically follow, and you may not be able to straighten your knee. Additional symptoms include:
- An indentation at the bottom of your kneecap where the patellar tendon tore
- Bruising
- Tenderness
- Cramping
- Your kneecap may move up into the thigh because it is no longer anchored to your shinbone
- Difficulty walking due to the knee buckling or giving way
To confirm the diagnosis, your doctor may order some imaging tests, such as an x-ray or magnetic resonance imaging (MRI) scan.
X-rays. The kneecap moves out of place when the patellar tendon tears. This is often very obvious on a “sideways” x-ray view of the knee. Complete tears can often be identified with these x-rays alone.
MRI. This scan creates better images of soft tissues like the patellar tendon. The MRI can show the amount of tendon torn and the location of the tear. Sometimes, an MRI is required to rule out a different injury that has similar symptoms.
Quadriceps tendon tear
The quadriceps tendon works with the muscles in the front of your thigh to straighten your leg. Quadriceps tendon tears are not common. They most often occur among middle-aged people who play running or jumping sports.
A quadriceps tear often occurs when there is a heavy load on the leg with the foot planted and the knee partially bent. Think of an awkward landing from a jump while playing basketball. The force of the landing is too much for the tendon and it tears.
Tears can also be caused by falls, direct force to the front of the knee, and lacerations (cuts).
Quadriceps tendon tears can be either partial or complete:
- Partial tears. Many tears do not completely disrupt the soft tissue. This is similar to a rope stretched so far that some of the fibers are frayed, but the rope is still in one piece.
- Complete tears. A complete tear will split the soft tissue into two pieces.
When the quadriceps tendon completely tears, the muscle is no longer anchored to the kneecap. Without this attachment, the knee cannot straighten when the quadriceps muscles contract.
Small tears of the quadriceps tendon can make it difficult to walk and participate in other daily activities. A large tear of the quadriceps tendon is a disabling injury. It usually requires surgery and physical therapy to regain full knee function.
Symptoms
When a quadriceps tendon tears, there is often a tearing or popping sensation. Pain and swelling typically follow, and you may not be able to straighten your knee. Additional symptoms include:
- An indentation at the top of your kneecap where the tendon tore
- Bruising
- Tenderness
- Cramping
- Your kneecap may sag or droop because the tendon is torn
- Difficulty walking due to the knee buckling or giving way
To confirm the diagnosis, your doctor may order some imaging tests, such as an x-ray or magnetic resonance imaging (MRI) scan.
X-rays. The kneecap moves out of place when the quadriceps tendon tears. This is often very obvious on a “sideways” x-ray view of the knee. Complete tears can often be identified with these x-rays alone.
MRI. This scan creates better images of soft tissues like the quadriceps tendon. The MRI can show the amount of tendon torn and the location of the tear. Sometimes, an MRI is required to rule out a different injury that has similar symptoms.
Treatment
Your doctor will consider several things when planning your treatment, including:
- The type and size of your tear
- Your activity level
- Your age
Nonsurgical Treatment
Most small, partial tears respond well to nonsurgical treatment.
Immobilization. Your doctor may recommend you wear a knee immobilizer or brace. This will keep your knee straight to help it heal. You will most likely need crutches to help you avoid putting all of your weight on your leg. You can expect to be in a knee immobilizer or brace for 3 to 6 weeks.
Physical therapy. Once the initial pain and swelling has settled down, physical therapy can begin. Specific exercises can restore strength and range of motion.
Exercises will gradually be added to your program. Straight leg raises to strengthen your quadriceps are often central to a physical therapy plan. As time goes on, your doctor or therapist will unlock your brace. This will allow you to move more freely with a greater range of motion. You will be prescribed more strengthening exercises as you heal.
Your doctor will discuss with you when it is safe to return to sports activity.
Surgical Treatment
Most people with complete tears will require surgery to repair the torn tendon. If you have a large partial tear or a partial tear associated with tendon degeneration, your doctor may also recommend surgery. This will likely depend upon your age, your activities, and your previous level of function.
Surgical repair reattaches the torn tendon to the top of the kneecap. People who require surgery do better if the repair is performed soon after the injury. Early repair may prevent the tendon from scarring and tightening into a shortened position.
Patello-femoral pain syndrome
Patients with patello-femoral pain syndrome (chondromalacia patellae) typically present with a vague history of mild to moderate anterior knee pain that usually occurs after prolonged periods of sitting (the so-called “theater sign”) 13. Patello-femoral pain syndrome is characterised by pain felt behind the kneecap. Squatting, walking up and down hills or stairs, or sitting still for extended periods of time can exacerbate the pain. The usual cause is abnormal movement of the kneecap as the knee is bent and straightened. This can lead to wear and tear of the cartilage on the back of the kneecap. Imbalances in muscle strength, tight muscles and structural abnormalities of the lower limb can contribute to the problem. The pain usually comes on gradually over time.
Patello-femoral pain syndrome is a common cause of anterior knee pain in women.
On physical examination, a slight effusion may be present, along with patellar crepitus on range of motion. The patient’s pain may be reproduced by applying direct pressure at the anterior aspect of the patella. Patellar tenderness may be elicited by subluxing the patella medially or laterally and palpating the superior and inferior facets of the patella. Radiographs usually are not indicated.
Knee Fractures
Fractures may occur in the patella, femoral condyles or tibial plateau 6. Patellar fractures are divided into transverse, vertical, upper pole, lower pole, comminuted and osteochondral fractures. Each type can be undisplaced or displaced 14. The two main mechanisms of patellar fracture are direct trauma to the anterior aspect of the knee or a powerful contraction of the quadriceps muscle (transverse, upper pole and lower pole fractures).
Radiographs are essential to assess traumatic patellar injury 14. In addition to antero-posterior, notch and lateral views, Merchant and infrapatellar views with the knee in 45 degrees of flexion may be necessary to identify an osteochondral fragment.
Fractures of the femoral condyles involve the distal 9 to 15 cm of the femur 14. Both the diaphyseal and metaphyseal regions may be involved. Fractures may also show intra-articular extension. Most condylar fractures occur as a result of motor vehicle accidents. Other causes include falling on a flexed knee or falling from a height. In young people, higher energy is necessary for a fracture to occur; consequently, more soft tissue damage is also present. In older patients with osteoporosis, less energy is needed to produce a fracture; therefore, less associated soft tissue damage is present.
Fractures of the tibial plateau are of special importance because they occur in one of the most important weight-bearing areas 14. These fractures may involve the metaphysis, epiphysis and/or articular cartilage. The forces that produce fractures in this area are compression, valgus force (outward twisting [away from the midline]) or a combination of both. The fractures primarily involve the lateral plateau, the medial plateau or both structures (bicondylar fractures).
Knee injuries evaluation
Medical history
A history of knee injury or surgery is important. The patient should be asked about previous attempts to treat knee pain, including the use of medications, supporting devices, and physical therapy. The physician also should ask if the patient has a history of gout, pseudogout, rheumatoid arthritis, or other degenerative joint disease.
Pain characteristics
The patient’s description of knee pain is helpful in focusing the differential diagnosis 15. It is important to clarify the characteristics of the pain, including its onset (rapid or insidious), location (anterior, medial, lateral, or posterior knee), duration, severity, and quality (e.g., dull, sharp, achy). Aggravating and alleviating factors also need to be identified. If knee pain is caused by an acute injury, the physician needs to know whether the patient was able to continue activity or bear weight after the injury or was forced to cease activities immediately.
Mechanical symptoms
The patient should be asked about mechanical symptoms, such as locking, popping, or giving way of the knee. A history of locking episodes suggests a meniscal tear. A sensation of popping at the time of injury suggests ligamentous injury, probably complete rupture of a ligament (third-degree tear). Episodes of giving way are consistent with some degree of knee instability and may indicate patellar subluxation or ligamentous rupture.
Knee joint effusion
The timing and amount of joint effusion are important clues to the diagnosis. Rapid onset (within two hours) of a large, tense effusion suggests rupture of the anterior cruciate ligament or fracture of the tibial plateau with resultant hemarthrosis, whereas slower onset (24 to 36 hours) of a mild to moderate knee joint effusion is consistent with meniscal injury or ligamentous sprain. Recurrent knee effusion after activity is consistent with meniscal injury.
Physical Examination
Inspection and palpation
The physician begins by comparing the painful knee with the asymptomatic knee and inspecting the injured knee for erythema, swelling, bruising, and discoloration. The musculature should be symmetric bilaterally. In particular, the vastus medialis obliquus of the quadriceps should be evaluated to determine if it appears normal or shows signs of atrophy.
The knee is then palpated and checked for pain, warmth, and effusion. Point tenderness should be sought, particularly at the patella, tibial tubercle, patellar tendon, quadriceps tendon, anterolateral and anteromedial joint line, medial joint line, and lateral joint line. Moving the patient’s knee through a short arc of motion helps identify the joint lines. Range of motion should be assessed by extending and flexing the knee as far as possible (normal range of motion: extension, zero degrees; flexion, 135 degrees) 16.
Patellofemoral assessment
An evaluation for effusion should be conducted with the patient supine and the injured knee in extension. The suprapatellar pouch should be milked to determine whether an effusion is present.
Patellofemoral tracking is assessed by observing the patella for smooth motion while the patient contracts the quadriceps muscle. The presence of crepitus should be noted during palpation of the patella.
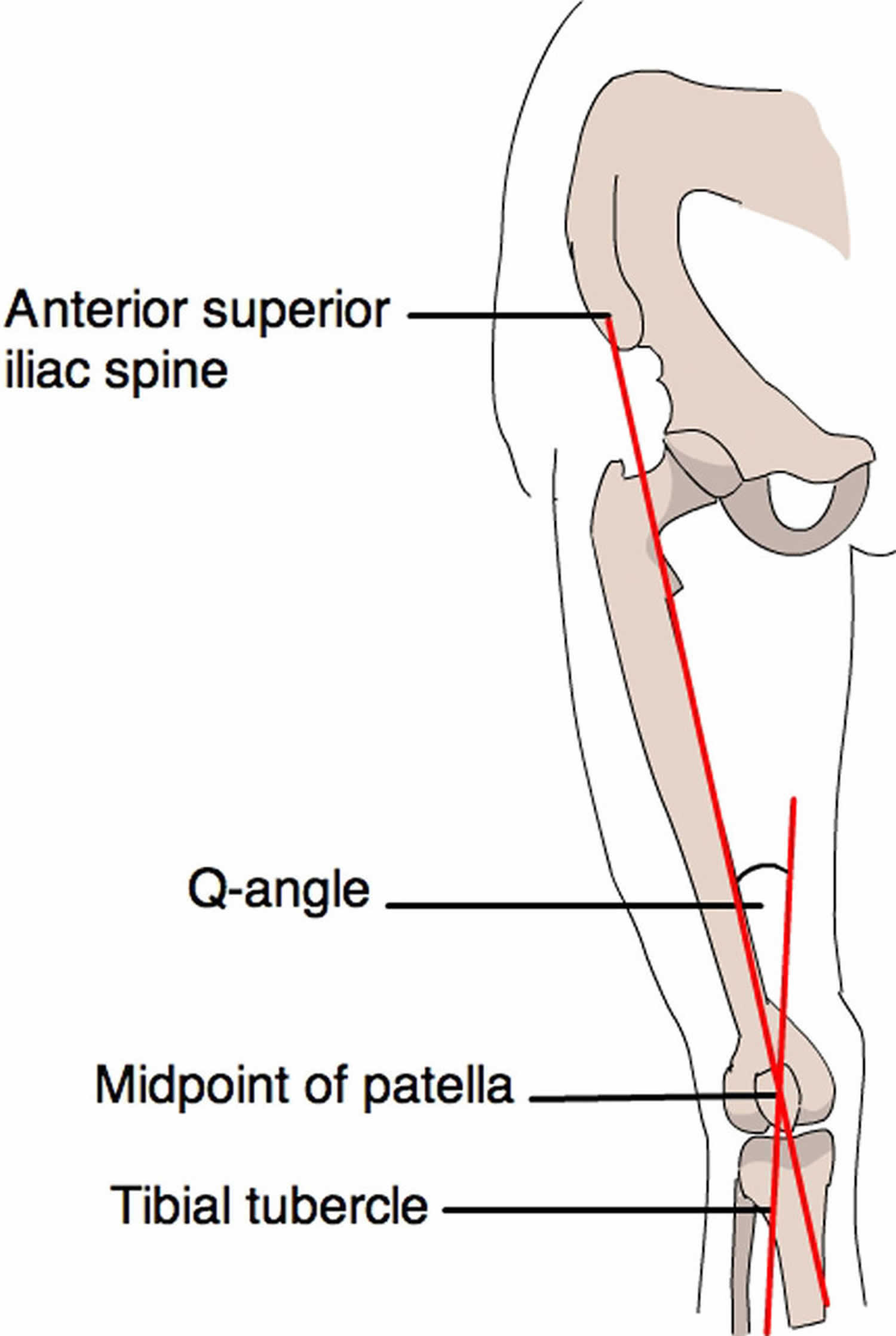
The quadriceps angle (Q angle) is determined by drawing one line from the anterior superior iliac spine through the center of the patella and a second line from the center of the patella through the tibial tuberosity (Figure 4) 17. A Q angle greater than 15 degrees is a predisposing factor for patellar subluxation (i.e., if the Q angle is increased, forceful contraction of the quadriceps muscle can cause the patella to sublux laterally).
A patellar apprehension test is then performed. With fingers placed at the medial aspect of the patella, the physician attempts to sublux the patella laterally. If this maneuver reproduces the patient’s pain or a giving-way sensation, patellar subluxation is the likely cause of the patient’s symptoms 18. Both the superior and inferior patellar facets should be palpated, with the patella subluxed first medially and then laterally.
Figure 4. The quadriceps angle (Q angle)
Cruciate Ligaments
Anterior Cruciate Ligament
For the anterior drawer test, the patient assumes a supine position with the injured knee flexed to 90 degrees. The physician fixes the patient’s foot in slight external rotation (by sitting on the foot) and then places thumbs at the tibial tubercle and fingers at the posterior calf. With the patient’s hamstring muscles relaxed, the physician pulls anteriorly and assesses anterior displacement of the tibia (anterior drawer sign).
The Lachman test is another means of assessing the integrity of the anterior cruciate ligament 18. The test is performed with the patient in a supine position and the injured knee flexed to 30 degrees. The physician stabilizes the distal femur with one hand, grasps the proximal tibia in the other hand, and then attempts to sublux the tibia anteriorly. Lack of a clear end point indicates a positive Lachman test.
Posterior Cruciate Ligament
For the posterior drawer test, the patient assumes a supine position with knees flexed to 90 degrees. While standing at the side of the examination table, the physician looks for posterior displacement of the tibia (posterior sag sign) 18. Next, the physician fixes the patient’s foot in neutral rotation (by sitting on the foot), positions thumbs at the tibial tubercle, and places fingers at the posterior calf. The physician then pushes posteriorly and assesses for posterior displacement of the tibia.
Collateral Ligaments
Medial Collateral Ligament
The valgus stress test is performed with the patient’s leg slightly abducted. The physician places one hand at the lateral aspect of the knee joint and the other hand at the medial aspect of the distal tibia. Next, valgus stress is applied to the knee at both zero degrees (full extension) and 30 degrees of flexion 18. With the knee at zero degrees (i.e., in full extension), the posterior cruciate ligament and the articulation of the femoral condyles with the tibial plateau should stabilize the knee; with the knee at 30 degrees of flexion, application of valgus stress assesses the laxity or integrity of the medial collateral ligament.
Lateral Collateral Ligament
To perform the varus stress test, the physician places one hand at the medial aspect of the patient’s knee and the other hand at the lateral aspect of the distal fibula. Next, varus stress is applied to the knee, first at full extension (i.e., zero degrees), then with the knee flexed to 30 degrees 18. A firm end point indicates that the collateral ligament is intact, whereas a soft or absent end point indicates complete rupture (third-degree tear) of the ligament.
Medial and lateral menisci
Patients with injury to the menisci usually demonstrate tenderness at the joint line. The McMurray test is performed with the patient lying supine 19. The test has been described variously in the literature, but the author suggests the following technique.
The physician grasps the patient’s heel with one hand and the knee with the other hand. The physician’s thumb is at the lateral joint line, and fingers are at the medial joint line. The physician then flexes the patient’s knee maximally. To test the lateral meniscus, the tibia is rotated internally, and the knee is extended from maximal flexion to about 90 degrees; added compression to the lateral meniscus can be produced by applying valgus stress across the knee joint while the knee is being extended. To test the medial meniscus, the tibia is rotated externally, and the knee is extended from maximal flexion to about 90 degrees; added compression to the medial meniscus can be produced by placing varus stress across the knee joint while the knee is being extended. A positive test produces a thud or a click, or causes pain in a reproducible portion of the range of motion.
Because most patients with knee pain have soft tissue injuries, plain-film radiographs generally are not indicated. The Ottawa knee rules are a useful guide for ordering radiographs of the knee (Table 2).
Table 2. The Ottawa knee rules
Knee X-ray indications after acute knee injury:
- aged 55 years or over
- tenderness at the head of the fibula
- isolated tenderness of the patella
- inability to flex knee to 90 degrees
- inability to bear weight (defined as an inability to take four steps, ie. two steps on each leg, regardless of limping) immediately and at presentation
If radiographs are required, three views are usually sufficient: anteroposterior view, lateral view, and Merchant’s view (for the patellofemoral joint) 21. Teenage patients who report chronic knee pain and recurrent knee effusion require a notch or tunnel view (posteroanterior view with the knee flexed to 40 to 50 degrees). This view is necessary to detect radiolucencies of the femoral condyles (most commonly the medial femoral condyle), which indicate the presence of osteochondritis dissecans 22.
Radiographs should be closely inspected for signs of fracture, particularly involving the patella, tibial plateau, tibial spines, proximal fibula, and femoral condyles. If osteoarthritis is suspected, standing weight-bearing radiographs should be obtained.
No validated rules have been formulated for the use of radiography in patients with suspected knee ligament injuries 10. Although plain radiographs may be useful in the initial diagnosis of these knee injuries, magnetic resonance imaging (MRI) is becoming the preferred diagnostic method 3 and is rapidly replacing other techniques as the study of choice for the evaluation of knee injuries 23. However, the routine use of MRI has been questioned because of its significant cost ($600 to $1,200) and the high accuracy of clinical examination in diagnosing some injuries 24.
Laboratory Studies
The presence of warmth, exquisite tenderness, painful effusion, and marked pain with even slight range of motion of the knee joint is consistent with septic arthritis or acute inflammatory arthropathy. In addition to obtaining a complete blood count with differential and an erythrocyte sedimentation rate (ESR), arthrocentesis should be performed. The joint fluid should be sent to a laboratory for a cell count with differential, glucose and protein measurements, bacterial culture and sensitivity, and polarized light microscopy for crystals.
Because a tense, painful, swollen knee may present an unclear clinical picture, arthrocentesis may be required to differentiate simple effusion from hemarthrosis or occult osteochondral fracture 15. A simple joint effusion produces clear, straw-colored transudative fluid, as in a knee sprain or chronic meniscal injury. Hemarthrosis is caused by a tear of the anterior cruciate ligament, a fracture or, less commonly, an acute tear of the outer portion of the meniscus. An osteochondral fracture causes hemarthrosis, with fat globules noted in the aspirate.
Rheumatoid arthritis may involve the knee joint. Hence, serum ESR and rheumatoid factor testing are indicated in selected patients.
How to prevent knee injuries
You may be able to help to prevent injuries if you:
- Warm up joints and muscles by gently going through the motions of your sport or activity and stretching muscles.
- Wear appropriate footwear.
- Avoid sudden jarring motions.
- Try to turn on the balls of your feet when you’re changing direction, rather than twisting through your knees.
- Cool down after exercise by performing light, easy and sustained stretches
- Build up an exercise program slowly over time.
Knee injuries first aid
When you are first injured, the RICE method — rest, ice, gentle compression and elevation – can help speed your recovery. Use the first aid for knee injuries in the first 48 to 72 hours.
Suggestions for first aid treatment of an injured knee include:
- Stop your activity immediately. Don’t ‘work through’ the pain.
- Rest the joint at first.
- Reduce pain, swelling and internal bleeding with icepacks, applied for 15 minutes every couple of hours.
- Bandage the knee firmly and extend the wrapping down the lower leg.
- Elevate the injured leg.
- Don’t apply heat to the joint.
- Avoid alcohol, as this encourages bleeding and swelling.
- Don’t massage the joint, as this encourages bleeding and swelling.
Be sure to seek treatment as soon as possible, especially if you:
- Hear a popping noise and feel your knee give out at the time of injury
- Have severe pain
- Cannot move the knee
- Begin limping
- Have swelling at the injury site
Knee injuries treatment
Mild knee injuries may heal by themselves, but all injuries should be checked and diagnosed by a doctor or physiotherapist. Persistent knee pain needs professional help. Prompt medical attention for any knee injury increases the chances of a full recovery.
Treatment options include:
- Aspiration – if the knee joint is grossly swollen, the doctor may release the pressure by drawing off some of the fluid with a fine needle.
- Physiotherapy – including techniques to reduce pain, kneecap taping, exercises for increased mobility and strength, and associated rehabilitation techniques.
- Arthroscopic surgery – or ‘keyhole’ surgery, where the knee operation is performed by inserting slender instruments through small incisions (cuts). Cartilage tears are often treated with arthroscopic surgery.
- Open surgery – required when the injuries are more severe and the entire joint needs to be laid open for repair.
Nonsurgical Treatment
Many knee injuries can be treated with simple measures, such as:
- Immobilization. Your doctor may recommend a brace to prevent your knee from moving. If you have fractured a bone, a cast or brace may hold the bones in place while they heal. To further protect your knee, you may be given crutches to keep you from putting weight on your leg.
- Physical therapy. Specific exercises will restore function to your knee and strengthen the leg muscles that support it.
- Non-steroidal anti-inflammatory medicines. Drugs like aspirin and ibuprofen reduce pain and swelling.
Surgical Treatment
Many fractures and injuries around the knee require surgery to fully restore function to your leg. In some cases – such as many ACL tears — surgery can be done arthroscopically using miniature instruments and small incisions. Many injuries require open surgery with a larger incision that provides your surgeon with a more direct view and easier access to the injured structures.
- Stiell IG, Greenberg GH, Wells GA, McDowell I, Cwinn AA, Smith NA, et al. Prospective validation of a decision rule for the use of radiography in acute knee injuries. JAMA. 1996;275:611–5.[↩]
- Evaluation of Patients Presenting with Knee Pain: Part II. Differential Diagnosis. Am Fam Physician. 2003 Sep 1;68(5):917-922. https://www.aafp.org/afp/2003/0901/p917.html[↩]
- Manaster BJ, Ensign MF. Imaging the ligaments of the knee. Crit Rev Diagn Imaging. 1991;32:323–66.[↩][↩][↩][↩][↩]
- Micheli LJ, Foster TE. Acute knee injuries in the immature athlete. Instr Course Lect. 1993;42:473–80.[↩][↩]
- Reginato AJ, Reginato AM. Diseases associated with deposition of calcium pyrophosphate or hydroxyapatite. In: Kelley WN, ed. Textbook of rheumatology. 5th ed. Philadelphia: Saunders, 1997:1352–67.[↩]
- Weinstein SL, Buckwalter JA, eds. Turek’s Orthopaedics, principles and their application. 5th ed. Philadelphia: Lippincott, 1994.[↩][↩]
- Acute Knee Injuries: Use of Decision Rules for Selective Radiograph Ordering. https://www.aafp.org/afp/1999/1201/p2599.html[↩]
- Ptasznik R, Feller J, Bartlett J, Fitt G, Mitchell A, Hennessy O. The value of sonography in the diagnosis of traumatic rupture of the anterior cruciate ligament of the knee. AJR Am J Roentgenol. 1995;164:1461–3.[↩]
- Stäubli HU, Jakob RP. Posterior instability of the knee near extension. A clinical and stress radiographic analysis of acute injuries of the posterior cruciate ligament. J Bone Joint Surg. [Br] 1990;72:225–30.[↩]
- Smith BW, Green GA. Acute knee injuries: Part II. Diagnosis and management. Am Fam Physician. 1995;51:799–806.[↩][↩]
- Walsh WM. Knee injuries. In: Mellion MB, Walsh WM, Shelton GL, eds. The team physician’s handbook. 2d ed. St. Louis: Mosby, 1990:554–78.[↩]
- Smith BW, Green GA. Acute knee injuries: part II. Diagnosis and management. Am Fam Physician. 1995;51:799–806.[↩]
- Ruffin MT 5th, Kiningham RB. Anterior knee pain: the challenge of patellofemoral syndrome. Am Fam Physician. 1993;47:185–94.[↩]
- Acute Knee Injuries: Use of Decision Rules for Selective Radiograph Ordering. Am Fam Physician. 1999 Dec 1;60(9):2599-2608. https://www.aafp.org/afp/1999/1201/p2599.html[↩][↩][↩][↩]
- Bergfeld J, Ireland ML, Wojtys EM, Glaser V. Pinpointing the cause of acute knee pain. Patient Care. 1997;31(18):100–7.[↩][↩]
- Magee DJ. Knee. In: Orthopedic physical assessment. 4th ed. Philadelphia: Saunders, 2002:661–763.[↩]
- Juhn MS. Patellofemoral pain syndrome: a review and guidelines for treatment. Am Fam Physician. 1999;60:2012–22.[↩]
- Smith BW, Green GA. Acute knee injuries: part I. History and physical examination. Am Fam Physician. 1995;51:615–21.[↩][↩][↩][↩][↩]
- McMurray TP. The semilunar cartilage. Br J Surg. 1942;29:407–14.[↩]
- Stiell IG, Wells GA, Hoag RH, et al. Implementation of the Ottawa Knee Rule for the Use of Radiography in Acute Knee Injuries. JAMA. 1997;278(23):2075–2079. doi:10.1001/jama.1997.03550230051036[↩]
- Sartoris DJ, Resnick D. Plain film radiography: routine and specialized techniques and projections. In: Resnick D, ed. Diagnosis of bone and joint disorders. 3d ed. Philadelphia: Saunders:1–40.[↩]
- Schenck RC Jr, Goodnight JM. Osteochondritis dissecans. J Bone Joint Surg [Am]. 1996;78:439–56.[↩]
- Stull MA, Nelson MC. The role of MRI in diagnostic imaging of the injured knee. Am Fam Physician. 1990;41:489–500.[↩]
- O’Shea KJ, Murphy KP, Heekin RD, Herzwurm PJ. The diagnostic accuracy of history, physical examination, and radiographs in the evaluation of traumatic knee disorders. Am J Sports Med. 1996;24:164–7.[↩]