What is mottled skin
Mottled skin or mottling refers to blood vessel changes in the skin that cause a patchy skin discoloration, reflecting reduced skin blood flow 1 and low tissue oxygen saturation 2 and has been suggested as a tool for clinical evaluation of tissue perfusion in patients with severe infection 3. Broadly speaking, mottled skin is divided into physiological and pathological livedo reticularis. Physiological livedo reticularis (cutis marmorata) is commonly seen on the legs of newborns and young women in cold weather and improves on rewarming. Pathological livedo reticularis is a cutaneous manifestation of a number of systemic conditions, most notably the antiphospholipid syndrome (APS), and is associated with arterial and venous thrombosis and increased pregnancy morbidity irrespective of the presence of antiphospholipid antibodies. Pathological livedo reticularis is the most common dermatologic presentation in patients with antiphospholipid syndrome (APS), presenting in 25% of patients with primary antiphospholipid syndrome and in 70% of patients with systemic lupus erythematosus (SLE)-associated antiphospholipid syndrome 4. Given this, a patient presenting with livedo reticularis should always be evaluated for antiphospholipid antibodies 5. Similarly, consideration should be given to evaluating all patients with venous leg ulceration for antiphospholipid antibodies, because there is a demonstrated association between the two 6.
More than 33% of patients with systemic lupus erythematosus (SLE) may have antiphospholipid antibodies, but not all of these patients will have clinical symptoms of the antiphospholipid syndrome. livedo reticularis is a significant preceding sign for development of neuropsychiatric lupus erythematosus 7.
Patients with antiphospholipid syndrome associated with systemic lupus erythematosus (SLE) were more likely to have arthritis, livedo reticularis, thrombocytopenia, and leukopenia than those with primary antiphospholipid syndrome, whereas patients with primary antiphospholipid syndrome were more likely to have asymptomatic avascular necrosis of the femoral head 8.
Extensive mottling extension has also been demonstrated to be predictive of mortality in patients with septic shock, independently of systemic hemodynamic parameters 9. However, the mechanism responsible for the specific regional reduction of blood flow in the mottled skin area remains unknown 10. Direct capillary obstruction by platelet aggregation and coagulation cascade activation has been suggested as a mechanism responsible for skin hypoperfusion 11 and has been documented in patients with meningococcemia 12.
Mottled skin is a manifestation of cutaneous blood flow disturbance that may occur in a variety of physiologic and pathologic states. They may be benign, as in physiologic cutis marmorata of infancy, or serious, as in the vasculitis of lupus erythematosus 13. To understand the spectrum of diseases associated with mottled skin, it is necessary to evaluate patients who present with this distinctive net-like vascular pattern in the skin.
What causes mottled skin
Broadly speaking, mottled skin is divided into physiological and pathological mottled skin. Physiological mottled skin (cutis marmorata) is commonly seen on the legs of newborns and young women in cold weather and improves on rewarming. Pathological mottled skin is a cutaneous manifestation of a number of systemic conditions, most notably the antiphospholipid syndrome (APS), and is associated with arterial and venous thrombosis and increased pregnancy morbidity irrespective of the presence of antiphospholipid antibodies.
Cutis marmorata causes temporary or physiological livedo in about 50% of normal infants and many adults, particularly young women when exposed to the cold.
Cutis marmorata telangiectatica congenita is a rare condition in which pronounced livedo is present at birth or soon after. It often improves with age. There are several congenital abnormalities associated with cutis marmorata telangiectatica.
Primary livedo reticularis is the idiopathic form in adults and can be persistent. The diagnosis is usually made once other more serious causes of livedo reticularis have been ruled out.
Secondary mottled skin (pathological livedo reticularis) or livedo racemosa, is associated with a range of systemic diseases.
Pathological livedo reticularis (livedo racemosa) may be a sign of vasculitis or of obstruction of the vessel by a circulating material. Causes include the following:
- Livedo can be an initial manifestation in the primary antiphospholipid syndrome, and up to 70% of patients with systemic lupus erythematosus associated with the antiphospholipid syndrome
- Polyarteritis nodosa and antineutrophil cytoplasmic antibody (ANCA)-positive vasculitis
- Cryoglobulinaemia
- Other connective tissue disorders such as dermatomyositis and rheumatoid arthritis
- Thromboangiitis obliterans
- Primary thrombocytopenia and polycythaemia vera
- Pyoderma gangrenosum
- Sneddon’s syndrome is a form of idiopathic livedo reticularis with systemic involvement that is the internal blood vessels are affected, most commonly in the brain, eye and heart
What is Livedo reticularis
Livedo reticularis refers to various conditions in which there is mottled discoloration of the skin characterized by transient or persistent, blotchy, reddish-blue to purple, net-like cyanotic pattern 13. It is described as being reticular (net-like, lace-like), as cyanotic discolouration surrounds pale central skin. Livedo reticularis itself is relatively benign. However, thromboembolic disease due to associated conditions such as antiphospholipid syndrome may lead to serious arterial events including the death of the patient.
Livedo reticularis may be differentiated into five distinct entities based on duration of the livedo pattern and its association with ambient temperature:
- Cutis marmorata: physiological, variable livedo reticularis, mainly seen in young women and newborns, occurs commonly on the legs on exposure to cold temperature, with slow resolution on rewarming. An impairment of blood flow in cutaneous vessels causes the mottling of livedo reticularis related to the vascular anatomy of normal skin.
- Cutis marmorata telangiectatica congenita: a rare congenital form of persistent livedo reticularis. The list of the abnormalities associated with cutis marmorata telangiectatica congenita are presented in Figure 5 below.
- Primary livedo reticularis: a benign form of livedo reticularis of unknown cause. Primary livedo reticularis also has a fluctuant course, but differs from cutis marmorata in that changes in skin color are unrelated to ambient temperature 14.
- Secondary livedo reticularis: association of livedo reticularis with an underlying systemic disease
- Livedo racemosa: a generalized and persistent form of livedo reticularis 14. The livid conical discoloration is symmetric, irreversible, and “broken”. The diagnosis is reached when no other pathological signs except livedo reticularis are found. It rarely represents the early stage of antiphospholipid syndrome (APS) or Sneddon’s syndrome 13.
Broadly speaking, livedo is divided into physiological and pathological livedo reticularis. Physiological livedo reticularis (cutis marmorata) is commonly seen on the legs of infants and young women in cold weather and improves on rewarming. Pathological livedo reticularis is a cutaneous manifestation of a number of systemic conditions, most notably the antiphospholipid syndrome (APS), and is associated with arterial and venous thrombosis and increased pregnancy morbidity irrespective of the presence of antiphospholipid antibodies.
Cutis marmorata causes temporary or physiological livedo in about 50% of normal infants and many adults, particularly young women when exposed to the cold.
Cutis marmorata telangiectatica congenita is a rare condition in which pronounced livedo is present at birth or soon after. It often improves with age. There are several congenital abnormalities associated with cutis marmorata telangiectatica.
Primary livedo reticularis is the idiopathic form in adults and can be persistent. The diagnosis is usually made once other more serious causes of livedo reticularis have been ruled out.
Secondary livedo (pathological livedo reticularis) or livedo racemosa, is associated with a range of systemic diseases.
Pathological livedo reticularis (livedo racemosa) may be a sign of vasculitis or of obstruction of the vessel by a circulating material. Causes include the following:
- Livedo can be an initial manifestation in the primary antiphospholipid syndrome, and up to 70% of patients with systemic lupus erythematosus associated with the antiphospholipid syndrome
- Polyarteritis nodosa and antineutrophil cytoplasmic antibody (ANCA)-positive vasculitis
- Cryoglobulinaemia
- Other connective tissue disorders such as dermatomyositis and rheumatoid arthritis
- Thromboangiitis obliterans
- Primary thrombocytopenia and polycythaemia vera
- Pyoderma gangrenosum
- Sneddon’s syndrome is a form of idiopathic livedo reticularis with systemic involvement that is the internal blood vessels are affected, most commonly in the brain, eye and heart
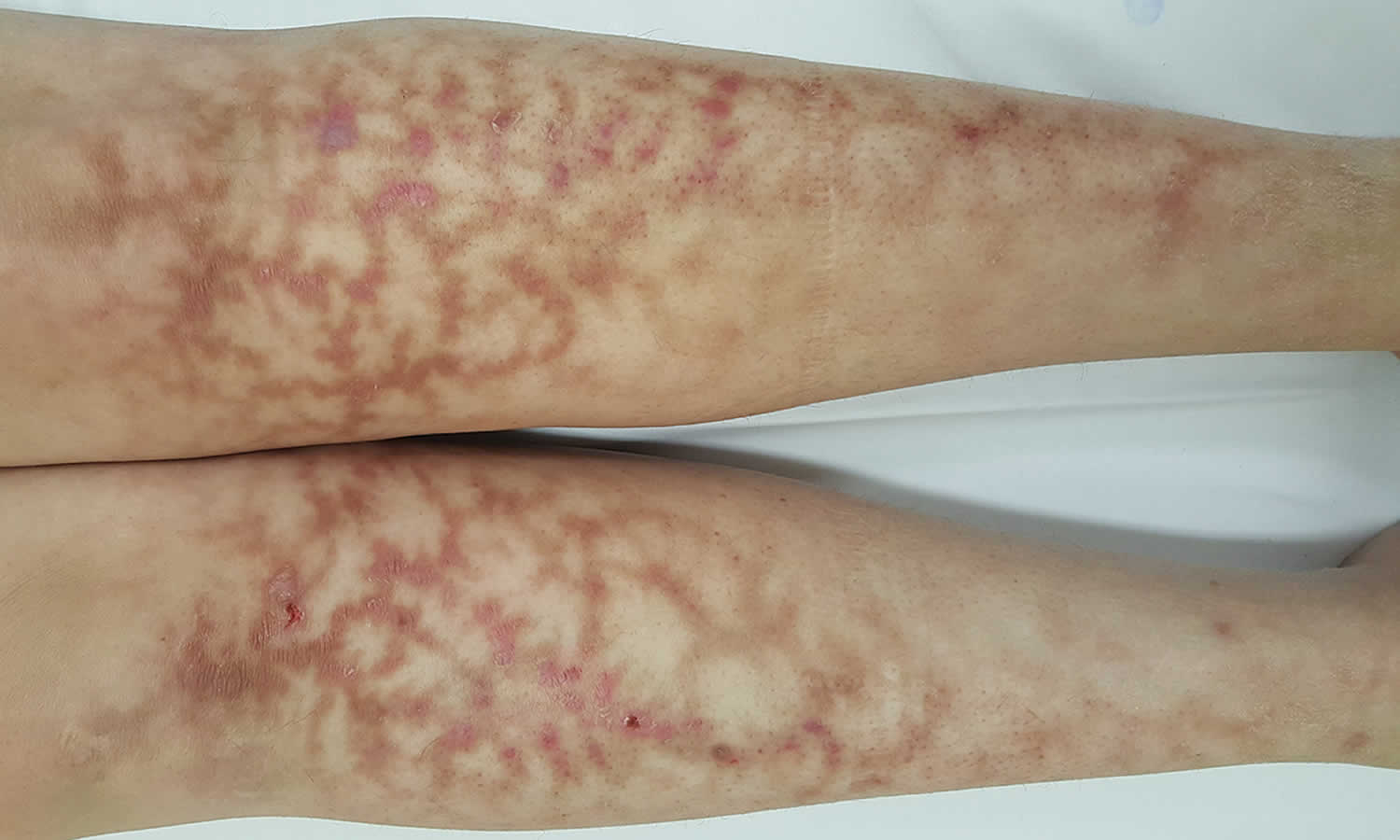
Figure 2. Livedo reticularis
Figure 3. Livedo racemosa
Footnote: 30-year-old woman presented with progressive, symmetrical, jagged and reticulate erythema and hyperpigmentation of the lower legs consistent with livedo racemosa. Her past medical history was remarkable for four embryonic miscarriages. A thrombophilia screen showed an elevated homocysteine level of 63 μmol/L (reference range, 5–15 μmol/L). She was commenced on aspirin 100 mg daily, with improvement observed at 2 weeks, after which she was lost to follow-up. Livedo racemosa may indicate a vascular insult; most commonly a medium-vessel vasculitis or hypercoagulable state. Identification and treatment of the driving pathology is needed to mitigate end-organ damage.
[Source 15 ]Figure 4. Cutis marmorata telangiectatica congenita
Figure 5. Abnormalities associated with cutis marmorata telangiectatica congenita
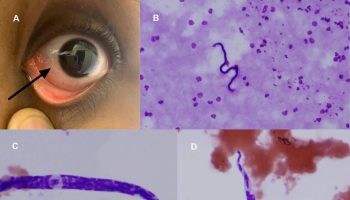
[Source 14 ]Figure 6. Cryoglobulinemia
Footnote: Physical signs include palpable purpura, livedo reticularis, ulceration and necrosis
Figure 7. Livedoid vasculopathy
Figure 8. Idiopathic livedo reticularis (Sneddon’s syndrome)
Footnote: Livedo racemosa in a female patient with a history of cerebrovascular disease
Livedo reticularis causes
Livedo reticularis results from a disturbance of blood flow to the skin causing low blood flow and reduced oxygen tension to the skin. Cutaneous vasculature is comprised of a series of 1–3 cm cones. The apex of each cone is located deep within the dermis at the site of an ascending arteriole. At the margin of each cone, the density of the arterial bed is decreased and the superficial venous plexus is more prominent. Any pathological or physiological process which impairs blood flow to the skin results in higher amounts of deoxygenated hemoglobin, leading to a livid discoloration.
Physiological arteriolar vasospasm in response to cold produces reversible skin discoloration, such as in cutis marmorata. Prolonged vasospasm, thrombosis or hyperviscosity can cause the pathological skin changes of livedo racemosa.
Other disease states have been associated with livedo reticularis, including cardiac failure and poliomyelitis 16. Vascular stasis appears to be the best explanation for livedo reticularis in these disorders.
Mechanical obstruction of blood flow can explain livedo reticularis associated with widespread deposition of oxalate crystals 17. The pathogenesis of livedo reticularis associated with B-cell lymphoma 18, cutaneous T-cell lymphoma 19, and acute pancreatitis is unknown 20.
Obstruction / vasculopathy
Occlusion of vessels may occur because of a hypercoagulable state. This may present as blue toe syndrome.
- Antiphospholipid syndrome (also known as lupus anticoagulant syndrome) is characterized by blood clots due to sticky platelets. It results in livedo racemosa in 25% of patients, and in 70% of those with systemic Lupus Erythematosus (SLE)-associated antiphospholipid syndrome.
- Sneddon syndrome is an association of livedo racemosa with stroke in young adult women.
- Livedoid vasculopathy is associated with ulceration due to fibrinolytic abnormalities and microcirculatory thrombosis.
- Cryoglobulinaemia (immune globulins that precipitate in the cold)
- Polycythaemia rubra vera (excessive number of red cells) or thrombocythaemia (platelet clumps)
- Multiple myeloma
- Cold agglutinin disease
- Protein C and S deficiency
- Antithrombin III deficiency
- Disseminated intravascular coagulation
- Hemolytic uremic syndrome (HUS)
- Deep venous thrombosis
Autoimmune / vasculitis / connective tissue disease
Small, medium and large vessel vasculitis is associated with livedo racemosa.
- Systemic lupus erythematosus
- Dermatomyositis
- Rheumatoid arthritis
- Polyarteritis nodosa
- Granulomatosis with polyangiitis
- Temporal arteritis
- Sjogren syndrome
Neurological disease
- Reflex sympathetic dystrophy
- Multiple sclerosis
- Parkinson disease
Infection
- Tuberculosis
- Syphilis
- Mycoplasma pneumonia
- Viral infection, eg parvovirus, hepatitis C
- Bacterial sepsis, eg meningococcal disease, streptococcal disease
- Rheumatic fever (erythema marginatum)
Cancer
- Renal cell carcinoma
- Inflammatory breast cancer (carcinoma erysipeloides)
- B-cell lymphoma
- Lymphoma (mycosis fungoides) 21
- Acute lymphocytic leukemia
Drugs
Amantadine (dopamine agonist used to treat Parkinson disease, multiple sclerosis and attention deficit hyperactivity disorder) causes livedo through arteriolar vasospasm associated with depletion of catecholamines. Other drug-associated livedo has been reported with:
- Minocycline
- Gemcitabine
- Catecholamines
- Non-steroidal anti-inflammatories (NSAIDs).
Endocrine and nutritional causes
Hormonal and dietary factors may produce livedo reticularis. Hypothyroidism can be associated with livedo reticularis that may resolve with appropriate replacement therapy 22. Pseudohypoparathyroidism with associated hypercalcemia is reported to cause widespread calcification and, in turn, ischemic skin signs such as skin infarction and livedo reticularis. The mechanism of livedo in hypoparathyroidism appears to be similar 16. Cushing’s disease is also reported to be associated with livedo reticularis 16. Pellagra is the only nutritional disorder associated with livedo reticularis 22.
Other causes
- Cardiac failure
- Poliomyelitis 23
- Cholesterol emboli and homocystinuria
- Septic emboli
- Hypercalcemia (calcium deposits)
- Thromboangiitis obliterans (Buerger disease)
- Intra-arterial injection (especially in drug addicts)
- Acute pancreatitis
- Primary fibromyalgia
- Congenital hypogammaglobulinemia
Livedo reticularis symptoms
Classical cutaneous features of livedo reticularis is characterized by:
- Net or lace-like cyanotic pattern. The network may comprise regular unbroken circles or an irregular broken pattern
- A red-blue, reticular (net-like) discoloration surrounding pale central areas
- Blotchy, reddish-blue to purple (livid color)
- Transient or persistent
- It occurs mostly on the legs, arms and trunk
- It may be more pronounced in cold conditions
- May or may not improve with warming
- Cold exposure may result in tingling and numbness of affected skin
- In physiological livedo the signs improve as the skin warms, and the patient is otherwise well
- In pathological livedo the rash is persistent, non-reversible with rewarming, and the patient may be unwell
- The term livedo racemosa is sometimes used when the livedo is more generalized, and has an irregular-broken shape with an annular pattern. While this pattern is recognized in Sneddon’s syndrome, it can also be found in other causes of pathological livedo such as the antiphospholipid syndrome (APS) and the ANCA-positive vasculitides. Livedo racemosa often affects the trunk and buttocks as well as legs.
In cutis marmorata, mottling is diffuse, mild and usually symptomless. The livedo commonly occurs on the legs and gradually resolves on rewarming. Cutis marmorata telangiectatica congenita is more pronounced than cutis marmorata. Primary livedo reticularis in adults is intermittent, and the changes in skin color are less influenced by ambient temperature.
Livedoid vasculopathy
- Livedo may present as a cutaneous ulcer (livedoid vasculopathy), and atrophie blanche may be a consequence
- It usually affects the lower legs bilaterally and is more common in summer
- It may affect all age groups but is more common in young females
- Initially there is a painful papular rash that develops into an ulcer. The ulcer subsequently heals leaving a porcelain white scar (atrophie blanche) that is often star-shaped
- Livedoid vasculopathy was originally described as a clinical manifestation of vasculitis; however the present concept is that it is a vaso-occlusive phenomenon with thrombosis of intradermal venules. It may be primary, or secondary, for example to a coagulopathy such as the antiphospholipid syndrome (APS) or cryoglobulinemia
Systemic associations with pathological livedo reticularis
- Arterial and venous thrombosis has been observed in patients with livedo irrespective of the presence of antiphospholipid antibodies
- Pregnancy morbidity also appears to be higher in patients with SLE and livedo, even when negative for antiphospholipid antibodies
- Accelerated atherosclerosis may be a feature
Livedo reticularis diagnosis
Livedo reticularis is diagnosed by its clinical appearance. Investigations are undertaken to seek for an underlying cause (see above) based on careful history and examination, as extensive screening studies are unlikely to be helpful. The lupus anticoagulant panel should be ordered in acquired livedo that is not clearly induced by the cold.
If required, it is best to take at least 2 biopsies from red/blue and white areas of the livedo and to ask for serial sections to be performed. Even a large skin biopsy of the center of livedo racemosa ring may be reported as normal. Multiple biopsies may increase the diagnostic yield. The goal of a biopsy is to obtain samples of the medium vessel found in the deep reticular dermis and subcutaneous fat, which may require a wedge or large punch biopsy for increased yield.
Early signs of vasculopathy are lymphocytes and histiocytes attaching to endothelial cells (lining cells of the blood vessels). The cells join with fibrin to occlude the lumen of capillaries. Other capillaries may be dilated, or replaced by scar tissue (fibrosis).
Livedo reticularis treatment
There is no specific treatment for physiological livedo reticularis, except for cold avoidance. Conservative measures such as limb elevation and compression stocking may be helpful in symptomatic patients of livedo reticularis. When underlying disorders are identified, treatment should be directed at treating the underlying disorder causing the pathological livedo reticularis.
In some patients, the symptoms may improve spontaneously with age. Rewarming the area in idiopathic cases or treatment of the underlying cause of secondary livedo may reverse the discoloration.
Smoking cessation is essential to reduce the risk of associated arterial events such as stroke.
Therapy for pathological livedo reticularis (livedo recemosa) should be directed toward the underlying disorder. Patients with pathological livedo reticularis (livedo recemosa) and the antiphospholipid antibody syndrome with thrombosis require anticoagulation therapy. Treatment of livedoid vasculopathy is not promising but potentially beneficial medications include anticoagulants, antiplatelet agents, immunosuppressants, pentoxifylline, danazol, and tissue plasminogen activator. Hyperbaric oxygen and psoralen and ultraviolet A light therapy have also been successfully utilized in some cases to treat livedoid vasculopathy 24.
Livedo reticularis prognosis
Livedo reticularis itself is relatively benign. However, thromboembolic disease due to associated conditions such as antiphospholipid syndrome may lead to serious arterial events including the death of the patient.
Cutis marmorata is usually less obvious with age. Over time, in primary livedo reticularis and livedo racemosa, the vessels become permanently dilated and livedo reticularis becomes permanent regardless of the surrounding temperature.
- Ait-Oufella H, Bourcier S, Alves M, Galbois A, Baudel JL, Margetis D, Bige N, et al. Alteration of skin perfusion in mottling area during septic shock. Ann Intensive Care. 2013;1:31. doi: 10.1186/2110-5820-3-31.[↩]
- Ait-Oufella H, Joffre J, Boelle PY, Galbois A, Bourcier S, Baudel JL, Margetis D, et al. Knee area tissue oxygen saturation is predictive of 14-day mortality in septic shock. Intensive Care Med. 2012;6:976–83. doi: 10.1007/s00134-012-2555-7.[↩]
- Ait-Oufella H, Bakker J. Understanding clinical signs of poor tissue perfusion during septic shock. Intensive Care Med. 2016;12:2070–2. doi: 10.1007/s00134-016-4250-6.[↩]
- Livedo racemosa: a striking dermatological sign for the antiphospholipid syndrome. Uthman IW, Khamashta MA. J Rheumatol. 2006 Dec; 33(12):2379-82.[↩]
- The antiphospholipid antibody syndrome in the emergency department setting–livedo reticularis and recurrent venous thrombosis. Kester S, McCarty DL, McCarty GA. Ann Emerg Med. 1992 Feb; 21(2):207-11.[↩]
- Lupus anticoagulant and venous leg ulceration. Fink AM, Kottas-Heldenberg A, Mayer W, Partsch H, Bayer PM, Bednar R, Steiner A. Br J Dermatol. 2002 Feb; 146(2):308-10.[↩]
- Karassa FB, Loannidis JP, Touloumi G, Boki KA, Moutsopoulos HM. Risk factors for central nervous system involvement in systemic lupus erythematosus. QJM. 2000;93:169–74.[↩]
- Tektonidou MG, Malagari K, Vlachoyiannopoulos PG, Kelekis DA, Moutsopoulos HM. Asymptomatic avascular necrosis in patients with primary antiphospholipid syndrome in the absence of corticosteroid use: A prospective study by magnetic resonance imaging. Arthritis Rheum. 2003;48:732–6.[↩]
- de Moura EB, Amorim FF, da Cruz Santana AN, Kanhouche G, de Souza Godoy LG, de Jesus Almeida L, Rodrigues TA, et al. Skin mottling score as a predictor of 28-day mortality in patients with septic shock. Intensive Care Med. 2016;3:479–80. doi: 10.1007/s00134-015-4184-4.[↩]
- Bourcier S, Joffre J, Dubée V, et al. Marked regional endothelial dysfunction in mottled skin area in patients with severe infections. Crit Care. 2017;21(1):155. Published 2017 Jun 23. doi:10.1186/s13054-017-1742-x https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5481873/[↩]
- Ait-Oufella H, Maury E, Lehoux S, Guidet B, Offenstadt G. The endothelium: physiological functions and role in microcirculatory failure during severe sepsis. Intensive Care Med. 2010;8:1286–98. doi: 10.1007/s00134-010-1893-6.[↩]
- Faust SN, Levin M, Harrison OB, Goldin RD, Lockhart MS, Kondaveeti S, Laszik Z, et al. Dysfunction of endothelial protein C activation in severe meningococcal sepsis. N Engl J Med. 2001;6:408–16. doi: 10.1056/NEJM200108093450603[↩]
- Sajjan VV, Lunge S, Swamy MB, Pandit AM. Livedo reticularis: A review of the literature. Indian Dermatol Online J. 2015;6(5):315-21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4594389/[↩][↩][↩]
- Livedo reticularis: an update. Gibbs MB, English JC 3rd, Zirwas MJ. J Am Acad Dermatol. 2005 Jun; 52(6):1009-19.[↩][↩][↩]
- Livedo racemosa. Med J Aust 2017; 207 (8): 327. doi: 10.5694/mja16.01355 https://www.mja.com.au/journal/2017/207/8/livedo-racemosa[↩]
- Copeman PW. Livedo reticularis. Signs in the skin of disturbance of blood viscosity and of blood flow. Br J Dermatol. 1975;93:519–29.[↩][↩][↩]
- Baethge BA, Sanusi ID, Landreneau MD, Rohr MS, McDonald JC. Livedo reticularis and peripheral gangrene associated with primary hyperoxaluria. Arthritis Rheum. 1988;31:1199–203.[↩]
- Fishel B, Brenner S, Weiss S, Yaron M. POEMS syndrome associated with cryoglobulinemia, lymphoma, multiple seborrheic keratosis, and ichthyosis. J Am Acad Dermatol. 1988;19:979–82.[↩]
- Champion RH. Livedo reticularis: A review. Br J Dermatol. 1965;77:167–79.[↩]
- Sigmund WJ, Shelley WB. Cutaneous manifestation of acute pancreatitis, with special reference to Livedo reticularis. N Engl J Med. 1954;251:851–3.[↩]
- LIVEDO RETICULARIS. A REVIEW. CHAMPION RH. Br J Dermatol. 1965 Apr; 77():167-79.[↩]
- Picasa DD, Pellegrini JR. Livedo reticularis. Cutis. 1987;38:429–32.[↩][↩]
- Champion RH. Cutaneous reaction to cold. In: Rooks A, Wilkinson DS, Ebling FJ, editors. Textbook of Dermatology. 4th ed. Oxford: Blackwell; 1986. pp. 627–31.[↩]
- Chadachan V, Dean SM, Eberhardt RT. Cutaneous changes in peripheral arterial vascular disease. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Wolff K, editors. Fitzpatrick’s Dermatology in General Medicine. 8th ed. USA: McGraw-Hill; 2012. pp. 2106–8.[↩]