Contents
What is malaise
Malaise is a general feeling of discomfort, illness, or lack of well-being. Malaise is a symptom that can occur with almost any health condition. Malaise may start slowly or quickly, depending on the type of disease. See your health care provider right away if you have severe malaise.
Fatigue is a feeling of weariness, tiredness, or lack of energy. Fatigue can occur with malaise in many diseases. With fatigue you can have a feeling of not having enough energy to do your usual activities.
What is fatigue
Fatigue is a state of extreme tiredness resulting from mental or physical exertion or illness 1. Men and women differ in the way they describe fatigue: men typically say they feel tired, whereas women say they feel depressed or anxious 2. No cause can be identified in one third of cases of fatigue. Overexertion, deconditioning, viral illness, upper respiratory tract infection, anemia, lung disease, medications, cancer, and depression are common causes.
Fatigue itself is not a disease. Medical problems, treatments, and personal habits can add to fatigue. These include:
- Taking certain medicines, such as antidepressants, antihistamines, and medicines for nausea and pain
- Having medical treatments, like chemotherapy and radiation
- Recovering from major surgery
- Anxiety, stress, or depression
- Staying up too late
- Drinking too much alcohol or too many caffeinated drinks
- Pregnancy
Some lifestyle habits can make you feel tired. Here are some things that may be draining your energy:
- Staying up too late. A good night’s sleep is important to feeling refreshed and energetic. Try going to bed and waking up at the same time every day.
- Having too much caffeine. Drinking caffeinated drinks like soda, tea, or coffee late in the day can keep you from getting a good night’s sleep. Limit the amount of caffeine you have during the day, and avoid it in the evening.
- Drinking too much alcohol. Alcohol changes the way you think and act. It may also interact with your medical treatments.
- Eating junk food. Say “no thanks” to food with empty calories, like fried foods and sweets, which have few nutrients and are high in fat and sugars. Nutritious foods will give you the energy you need to do the things you enjoy.
Being bored can also make you feel tired. That may sound strange, but it’s true. If you were very busy during your working years, you may feel lost about how to spend your time when you retire. When you wake up in the morning, you may see long days stretching before you with nothing planned. It doesn’t have to be that way.
Engaging in social and productive activities that you enjoy, like volunteering in your community, may help maintain your well-being. Think about what interests you and what skills or knowledge you have to offer, and look for places to volunteer.
One disorder that causes extreme fatigue is chronic fatigue syndrome (CFS) or myalgic encephalomyelitis. Chronic fatigue syndrome (myalgic encephalomyelitis) is not the kind of tired feeling that goes away after you rest. Instead, it lasts a long time and limits your ability to do ordinary daily activities. Scientists don’t know what causes chronic fatigue syndrome (CFS). There may be more than one thing that causes it. It is possible that two or more triggers might work together to cause the illness. According to the Centers for Disease Control and Prevention 3, more than one million Americans have chronic fatigue syndrome (myalgic encephalomyelitis). At least one-quarter of individuals with chronic fatigue syndrome (myalgic encephalomyelitis) are bedbound or housebound at some point in the illness and most never regain their pre-disease level of functioning. Chronic fatigue syndrome (myalgic encephalomyelitis) strikes people of all ages and racial, ethnic, and socioeconomic groups, and is diagnosed two to four times more often in women. Chronic fatigue syndrome (myalgic encephalomyelitis) is characterized by at least six months of incapacitating fatigue experienced as profound exhaustion and extremely poor stamina, and problems with concentration and short-term memory. Chronic fatigue syndrome (myalgic encephalomyelitis) is sometimes preceded by flu-like symptoms followed by pain in the joints and muscles, unrefreshing sleep, tender lymph nodes, sore throat, and headache. A distinctive characteristic of the chronic fatigue syndrome (myalgic encephalomyelitis) is post-exertion malaise, which is a worsening of symptoms following physical or mental exertion occurring within 12-48 hours of the exertion and requiring an extended recovery period. Although the cause of chronic fatigue syndrome (myalgic encephalomyelitis) remains unknown, symptoms may be triggered by an infection.
Fatigue may be classified as secondary, physiologic, or chronic. Secondary fatigue is caused by an underlying medical condition and may last one month or longer, but it generally lasts less than six months 4. Physiologic fatigue is an imbalance in the routines of exercise, sleep, diet, or other activity that is not caused by an underlying medical condition and is relieved with rest 4. Chronic fatigue lasts longer than six months and is not relieved with rest 5.
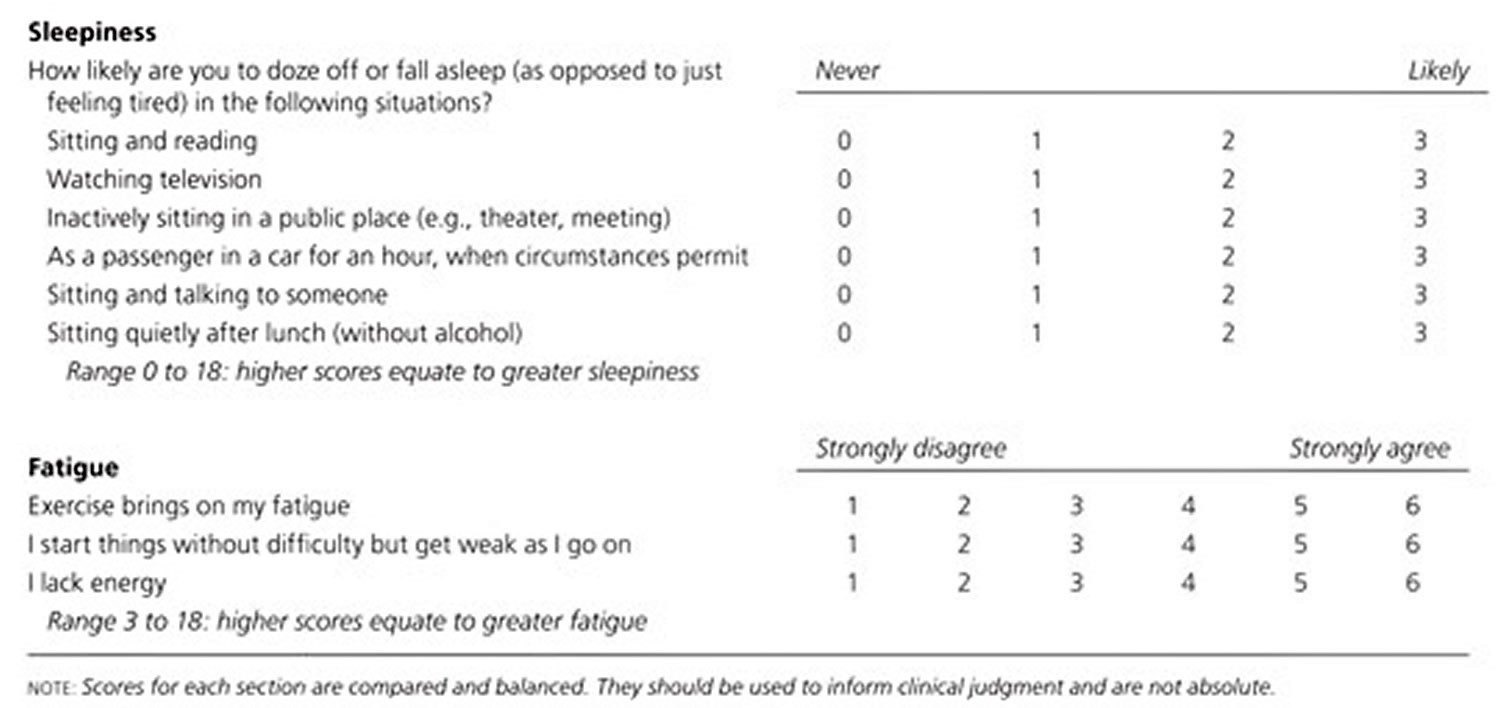
Sleepiness is the impairment of the normal arousal mechanism and is characterized by a tendency to fall asleep. Persons who are sleepy are temporarily aroused by activity, whereas fatigue is intensified by activity, at least in the short-term 6. Patients with sleepiness feel better after a nap, but patients with fatigue report a lack of energy, mental exhaustion, poor muscle endurance, delayed recovery after physical exertion, and nonrestorative sleep 4. Figure 1 provides a questionnaire to help differentiate between sleepiness and fatigue 7.
Figure 1. Fatigue questionnaire
Although it is possible for fatigue and depression to coexist, patients with fatigue report being unable to complete specific activities because of a lack of energy or stamina, whereas grief and depression are associated with a patient description that is more global, such as being unable to do “anything.”
Detailed psychiatric and sleep histories may help determine possible psychosocial contributors to fatigue.
Physical examination findings that suggest specific secondary causes of fatigue include lymphadenopathy [enlarged lymph nodes] (indicating tumor spread or recurrence), cardiac murmurs (endocarditis), goiter (thyroid hormone imbalance), edema (heart failure, liver disease, or malnutrition), poor muscle tone (advancing neurologic condition), and neurologic abnormalities (stroke or brain metastases).
Laboratory studies should be considered (Table 1), although their results affect management in only 5 percent of patients 8. Many physicians order a complete blood count, erythrocyte sedimentation rate (ESR), chemistry panel, thyroid-stimulating hormone (TSH) measurement, and urinalysis. Women of childbearing age should receive a pregnancy test. No other tests have been shown to be useful unless the history or physical examination suggests a specific medical condition 9.
Table 1. Laboratory Testing for Patients with Unexplained Fatigue
| Test* | Possible conditions | Comments |
|---|---|---|
Complete blood count Erythrocyte sedimentation rate Chemistry panel Thyroid function tests Human immunodeficiency virus antibodies Pregnancy test, if indicated | Anemia Inflammatory state Liver disease, renal failure, protein malnutrition Hypothyroidism Chronic infection, if not previously tested Pregnancy, breathlessness due to progestins | Should be performed in most patients with a two-week history of fatigue; results change management in 5 percent of patients |
Chest radiography Tuberculin skin test Electrocardiography Pulmonary function tests Toxicology screen Lyme titers Rapid plasma reagin Brain magnetic resonance imaging Echocardiography Specialized blood testing (e.g., ferritin, iron, vitamin B12, and folate levels; iron-binding capacity; direct antiglobulin test) | Adenopathy, cancer Tuberculosis, chronic infection Congestive heart failure, arrhythmia Chronic obstructive pulmonary disease, cancer Substance abuse Chronic Lyme disease Syphilis infection Multiple sclerosis Valvular heart disease, congestive heart failure Iron deficiency, Addison disease, celiac disease, myasthenia gravis, poisoning | Rarely useful; consider only if indicated by physical findings or abnormal baseline blood test results |
*— Arranged by the relative frequency that the tests produce results.
Fatigue treatment
Adequate sleep (i.e., generally seven to eight hours per night for adults) decreases tension and improves mood 10. Patients should be instructed to restructure their daily activities to get the sleep they need, and to practice good sleep hygiene. Recommendations for good sleep hygiene include the following: maintaining a regular morning rising time; increasing activity level in the afternoon; avoiding exercise in the evening or before bedtime; increasing daytime exposure to bright light; taking a hot bath within the two hours before bedtime; avoiding caffeine, nicotine, alcohol, and excessive food or fluid intake in the evening; using the bedroom only for sleep and sex; and practicing a bedtime routine that includes minimizing light and noise exposure and turning off the television 11. Naps may help, but should be limited to less than one hour in the early afternoon. One study showed that when hospitals provided patient coverage for medical intern naps (averaging 40 minutes) during overnight shifts, the interns achieved morning fatigue scores equivalent to those who were not on call 12. Time off from work also minimizes fatigue and decreases stress 13.
Stimulants improve short-term performance. A randomized, double-blind, crossover study of persons driving in nighttime conditions showed that participants had fewer errors after consuming regular coffee (i.e., 200 mg of caffeine) or taking a 30-minute nap 14. Modafinil, which is approved to manage fatigue that is induced by shift work, has the same effect on performance as 600 mg of caffeine. Modafinil and caffeine do not have most of the adverse cardiovascular effects and abuse potential that are associated with amphetamines 14. Although modafinil and caffeine temporarily improve performance, they are not a substitute for adequate rest, and long-term use of modafinil has been associated with depression.
Physical fitness also improves energy levels. One study showed that truck drivers who engaged in 30-minute exercise sessions more than once a week had fewer traffic incidents 15. Another study showed that 10 weeks of supervised exercise increased energy levels among persons with fatigue, regardless of the underlying cause 16.
Physiologic Fatigue
Physiologic fatigue is initiated by inadequate rest, physical effort, or mental strain unrelated to an underlying medical condition. Diminished motivation and boredom also play a role. Physiologic fatigue is most common in adolescents and older persons. In the United States, 24 percent of adults report having fatigue lasting two weeks or longer, and two thirds of these persons cannot identify the cause of their fatigue 17.
During intense training, well-conditioned athletes occasionally misinterpret fatigue as illness or depression 18. Conversely, fatigue and depression can emerge in a physically fit athlete after as little as one week with no exercise. Submaximal exercise mitigates these symptoms when training is limited because of injury 19.
Managing Secondary Fatigue
Medications that may be causing fatigue should be replaced or discontinued, if possible, and physiologic parameters should be corrected. With cancer, renal disease, or other chronic diseases associated with anemia, patients are likely to be less fatigued if their hemoglobin level is maintained at 10 g per dL (100 g per L), using erythropoietin agents if needed 20. Nonanemic, menstruating women who have low normal ferritin levels report modest increased energy after four weeks of iron supplementation 21.
Performing some form of daily exercise, sustaining interpersonal relationships, and returning to work are consistently associated with improvement in fatigue of any cause 22. Regular moderate aerobic activity (i.e., 30 minutes of walking or an equivalent activity on most days of the week) reduces disease-related fatigue more effectively than rest. Yoga, group therapy, and stress management diminish fatigue in patients with cancer 23. Patients who have features suggestive of depression may be offered a six-week trial of a selective serotonin reuptake inhibitor (SSRI) 24. Psychostimulants (e.g., methylphenidate [Ritalin], modafinil [Provigil]) improve fatigue in the short-term in patients with human immunodeficiency virus, multiple sclerosis, or cancer 25. Stimulants seldom return patients to predisease performance, and the drugs are associated with headaches, restlessness, insomnia, and dry mouth 26. If used, stimulants are best used as needed for episodic situations requiring alertness.
What is chronic fatigue
Chronic fatigue is defined as fatigue that lasts longer than six months. Chronic fatigue syndrome (CFS) is a common, enigmatic medical condition comprising mental and physical fatigue, diagnosed after exclusion of possible medical causes 1. Medical conditions that may cause or contribute to chronic fatigue are listed below. The prevalence of idiopathic chronic fatigue ranges from five to 40 per 100,000, depending on the population studied 27.
Chronic fatigue occurs in all age groups, including children. Women, minorities, and persons with lower educational and occupational statuses have a higher prevalence of chronic fatigue. No clinical test can confirm the presence of chronic fatigue syndrome (CFS). Treatment is supportive with no specific therapy shown to be reproducibly effective 1. Only 2 percent of patients who are chronically fatigued report complete long-term resolution of symptoms, but 64 percent have limited improvement. Patients whose symptoms worsen for longer than 24 hours after physical exertion have a poor prognosis 28.
On average, a typical family physician has in his or her practice two patients with fatigue of longer than six months for which no explanation can be determined 27. The diagnostic criteria for chronic fatigue syndrome (Table 2) are useful for defining disability or for research purposes, but may not be clinically helpful in all circumstances. Two thirds of patients with chronic fatigue do not meet these criteria, but they share many similarities to those with the syndrome and have only a slightly better prognosis 29.
Laboratory tests for chronic fatigue demonstrate some abnormality in 12 percent of patients and lead to alternate diagnoses in up to 8 percent of patients 30. However, when initial test results are normal, referral to an occupational sub-specialist, psychiatrist, or another physician is more helpful than repeating the tests 31.
Table 2. Diagnostic Criteria for Chronic Fatigue Syndrome
Major criteria: |
At least six months’ duration; does not resolve with bed rest; reduces daily activity to less than 50 percent; other conditions have been excluded |
Physical criteria: |
Low-grade fever; nonexudative pharyngitis; lymphadenopathy |
Minor criteria: |
Sore throat; mild fever or chills; lymph node pain; generalized muscle weakness; myalgia; prolonged fatigue after exercise; new-onset headaches; migratory noninflammatory arthralgia; sleep disturbance; neuropsychological symptoms (e.g., photophobia, scotomata, forgetfulness, irritability, confusion, inability to concentrate, depression, difficulty thinking); description of initial onset as acute or subacute |
Footnote: A diagnosis of chronic fatigue syndrome includes all major criteria plus: eight minor criteria, or six minor criteria and two physical criteria.
[Source 32 ]Recently an international panel of researchers, clinicians, and patient advocates have proposed returning to the diagnostic label of myalgic encephalomyelitis 33.
A patient with Chronic Fatigue Syndrome or Myalgic Encephalomyelitis will meet the criteria for fatigue, post-exertional malaise and/or fatigue, sleep dysfunction, and pain; have two or more neurological/cognitive manifestations and one or more symptoms from two of the categories of autonomic, neuroendocrine and immune manifestations; and adhere to item 34, 33.
- Fatigue: The patient must have a significant degree of new onset, unexplained, persistent, or recurrent physical and mental fatigue that substantially reduces activity level.
- Post-Exertional Malaise and/or Fatigue: There is an inappropriate loss of physical and mental stamina, rapid muscular and cognitive fatigability, post exertional malaise and/or fatigue and/or pain and a tendency for other associated symptoms within the patient’s cluster of symptoms to worsen. There is a pathologically slow recovery period – usually 24 hours or longer.
- Sleep Dysfunction:* There is unrefreshed sleep or sleep quantity or rhythm disturbances such as reversed or chaotic diurnal sleep rhythms.
- Pain:* There is a significant degree of myalgia. Pain can be experienced in the muscles and/or joints, and is often widespread and migratory in nature. Often there are significant headaches of new type, pattern or severity.
- Neurological/Cognitive Manifestations: Two or more of the following difficulties should be present: confusion, impairment of concentration and short-term memory consolidation, disorientation, difficulty with information processing, categorizing and word retrieval, and perceptual and sensory disturbances – e.g., spatial instability and disorientation and inability to focus vision. Ataxia, muscle weakness and fasciculations are common. There may be overload phenomena: cognitive, sensory – e.g., photophobia and hypersensitivity to noise – and/or emotional overload, which may lead to “crash” periods and/or anxiety.
- At least one symptom from two of the following categories:
- (i) Autonomic Manifestations: orthostatic intolerance – neurally mediated hypotension (NMH), postural orthostatic tachycardia syndrome (POTS), delayed postural hypotension; lightheadedness; extreme pallor; nausea and irritable bowel syndrome; urinary frequency and bladder dysfunction; palpitations with or without cardiac arrhythmias; exertional dyspnoea.
- (ii) Neuroendocrine Manifestations: loss of thermostatic stability – subnormal body temperature and marked diurnal fluctuation, sweating episodes, recurrent feelings of feverishness and cold extremities; intolerance of extremes of heat and cold; marked weight change – anorexia or abnormal appetite; loss of adaptability and worsening of symptoms with stress.
- (iii) Immune Manifestations: tender lymph nodes, recurrent sore throat, recurrent flu-like symptoms, general malaise, new sensitivities to food, medications and/or chemicals.
- The illness persists for at least six months. It usually has a distinct onset,** although it may be gradual. Preliminary diagnosis may be possible earlier. Three months is appropriate for children.
- To be included, the symptoms must have begun or have been significantly altered after the onset of this illness. It is unlikely that a patient will suffer from all symptoms in criteria 5 and 6. The disturbances tend to form symptom clusters that may fluctuate and change over time. Children often have numerous prominent symptoms but their order of severity tends to vary from day to day. *There is a small number of patients who have no pain or sleep dysfunction, but no other diagnosis fits except myalgic encephalomyelitis/Chronic Fatigue Syndrome. A diagnosis of myalgic encephalomyelitis/Chronic Fatigue Syndrome can be entertained when this group has an infectious illness type onset. **Some patients have been unhealthy for other reasons prior to the onset of myalgic encephalomyelitis/Chronic Fatigue Syndrome and lack detectable triggers at onset and/or have more gradual or insidious onset.
- Exclusions: Exclude active disease processes that explain most of the major symptoms of fatigue, sleep disturbance, pain, and cognitive dysfunction. It is essential to exclude certain diseases, which would be tragic to miss: Addison’s disease, Cushing’s syndrome, hypothyroidism, hyperthyroidism, iron deficiency, other treatable forms of anaemia, iron overload syndrome, diabetes mellitus, and cancer. It is also essential to exclude treatable sleep disorders such as upper airway resistance syndrome and obstructive or central sleep apnoea; rheumatological disorders such as rheumatoid arthritis, lupus, polymyositis and polymyalgia rheumatica; immune disorders such as AIDS; neurological disorders such as multiple sclerosis (MS), Parkinsonism, myasthenia gravis and B12 deficiency; infectious diseases such as tuberculosis, chronic hepatitis, Lyme disease, etc.; primary psychiatric disorders and substance abuse. Exclusion of other diagnoses, which cannot be reasonably excluded by the patient’s history and physical examination, is achieved by laboratory testing and imaging. if a potentially confounding medical condition is under control, then the diagnosis of cfs can be entertained if patients meet the criteria otherwise.
- Co-Morbid Entities:
- Fibromyalgia Syndrome (FMS), Myofascial Pain Syndrome (MPS), Temporo- mandibular Joint Syndrome (TMJ), Irritable Bowel Syndrome (IBS), Interstitial Cystitis, Irritable Bladder Syndrome, Raynaud’s Phenomenon, Prolapsed Mitral Valve, Depression, Migraine, Allergies, Multiple Chemical Sensitivities (MCS), Hashimoto’s thyroiditis, Sicca Syndrome, etc. Such comorbid entities may occur in the setting of Chronic Fatigue Syndrome. Others such as IBS may precede the development of Chronic Fatigue Syndrome by many years, but then become associated with it. The same holds true for migraines and depression. Their association is thus looser than between the symptoms within the syndrome. Chronic Fatigue Syndrome and Fibromyalgia Syndrome often closely connect and should be considered to be “overlap syndromes.”
- Overload phenomena affect sensory modalities where the patient may be hypersensitive to light, sound, vibration, speed, odours, and/or mixed sensory modalities.
Chronic fatigue causes
- Cardiopulmonary: congestive heart failure, chronic obstructive pulmonary disease, peripheral vascular disease, atypical angina
- Disturbed sleep: sleep apnea, gastroesophageal reflux disease, allergic or vasomotor rhinitis
- Endocrine: diabetes mellitus, hypothyroidism, pituitary insufficiency, hypercalcemia, adrenal insufficiency, chronic kidney disease, hepatic failure
- Infectious: endocarditis, tuberculosis, mononucleosis, hepatitis, parasitic disease, human immunodeficiency virus, cytomegalovirus
- Inflammatory: rheumatoid arthritis, systemic lupus erythematosus
- Medication use (e.g., sedative-hypnotics, analgesics, antihypertensives, antidepressants, muscle relaxants, opioids, antibiotics) or substance abuse
- Psychological: depression, anxiety, somatization disorder, dysthymic disorder
Chronic fatigue treatment
There is no cure or approved treatment for myalgic encephalomyelitis/chronic fatigue syndrome, but you may be able to treat or manage some of your symptoms. You, your family, and your health care provider should work together to decide on a plan. You should figure out which symptom causes the most problems, and try to treat that first. For example, if sleep problems affect you the most, you might first try using good sleep habits. If those do not help, you may need to take medicines or see a sleep specialist.
Strategies such as learning new ways to manage activity can also be helpful. You need to make sure that you do not “push and crash.” This can happen when you feel better, do too much, and then get worse again.
Since the process of developing a treatment plan and attending to self-care can be hard if you have Chronic Fatigue Syndrome, it is important to have support from family members and friends.
Don’t try any new treatments without talking to your health care provider. Some treatments that are promoted as cures for Chronic Fatigue Syndrome are unproven, often costly, and could be dangerous.
Symptoms that healthcare providers might try to address are:
Post-exertional Malaise
Post-exertional malaise is the worsening of symptoms after even minor physical, mental or emotional exertion. The symptoms typically get worse 12 to 48 hours after the activity and can last for days or even weeks.
Post-exertional malaise can be addressed by activity management, also called pacing. The goal of pacing is to learn to balance rest and activity to avoid post-exertional malaise flare-ups, which can be caused by exertion that patients with chronic fatigue syndrome (myalgic encephalomyelitis) cannot tolerate. To do this, patients need to find their individual limits for mental and physical activity. Then they need to plan activity and rest to stay within these limits. Some patients and doctors refer to staying within these limits as staying within the “energy envelope.” The limits may be different for each patient. Keeping activity and symptom diaries may help patients find their personal limits, especially early on in the illness.
For some patients with chronic fatigue syndrome (myalgic encephalomyelitis), even daily chores and activities such as cleaning, preparing a meal, or taking a shower can be difficult and may need to be broken down into shorter, less strenuous pieces. Rehabilitation specialists or exercise physiologists who know chronic fatigue syndrome (myalgic encephalomyelitis) may help patients with adjusting to life with chronic fatigue syndrome (myalgic encephalomyelitis). Patients who have learned to listen to their bodies might benefit from carefully increasing exercise to improve fitness and avoid deconditioning. However, exercise is not a cure for chronic fatigue syndrome (myalgic encephalomyelitis).
Patients with chronic fatigue syndrome (myalgic encephalomyelitis) need to avoid ‘push-and-crash’ cycles through carefully managing activity. “Push-and-crash” cycles are when someone with chronic fatigue syndrome (myalgic encephalomyelitis) is having a good day and tries to push to do more than they would normally attempt (do too much, crash, rest, start to feel a little better, do too much once again). This can then lead to a “crash” (worsening of chronic fatigue syndrome (myalgic encephalomyelitis) symptoms). Finding ways to make activities easier may be helpful, like sitting while doing the laundry or showering, taking frequent breaks, and dividing large tasks into smaller steps.
Any activity or exercise plan for people with chronic fatigue syndrome (myalgic encephalomyelitis) needs to be carefully designed with input from each patient. While vigorous aerobic exercise can be beneficial for many chronic illnesses, patients with chronic fatigue syndrome (myalgic encephalomyelitis) do not tolerate such exercise routines. Standard exercise recommendations for healthy people can be harmful for patients with chronic fatigue syndrome (myalgic encephalomyelitis). However, it is important that patients with chronic fatigue syndrome (myalgic encephalomyelitis) undertake activities that they can tolerate, as described above.
Sleep Problems
Patients with chronic fatigue syndrome (myalgic encephalomyelitis) often feel less refreshed and restored after sleep than they did before they became ill. Common sleep complaints include difficulty falling or staying asleep, extreme sleepiness, intense and vivid dreaming, restless legs, and nighttime muscle spasms.
Good sleep habits are important for all people, including those with chronic fatigue syndrome (myalgic encephalomyelitis). When people try these tips but are still unable to sleep, their doctor might recommend taking medicine to help with sleep. First, people should try over-the-counter sleep products. If this does not help, doctors can offer a prescription sleep medicine, starting at the smallest dose and using for the shortest possible time.
People might continue to feel unrefreshed even after the medications help them to get a full night of sleep. If so, they should consider seeing a sleep specialist. Most people with sleep disorders, like sleep apnea (symptoms include brief pausing in breathing during sleep) and narcolepsy (symptoms include excessive daytime sleepiness), respond to therapy. However, for people with chronic fatigue syndrome (myalgic encephalomyelitis), not all symptoms may go away.
Pain
People with chronic fatigue syndrome (myalgic encephalomyelitis) often have deep pain in their muscles and joints. They might also have headaches (typically pressure-like) and soreness of their skin when touched.
Patients should always talk to their healthcare provider before trying any medication. Doctors may first recommend trying over-the-counter pain-relievers, like acetaminophen, aspirin, or ibuprofen. If these do not provide enough pain relief, patients may need to see a pain specialist. People with chronic pain, including those with chronic fatigue syndrome (myalgic encephalomyelitis), can benefit from counseling to learn new ways to deal with pain.
Other pain management methods include stretching and movement therapies, gentle massage, heat, toning exercises, and water therapy for healing. Acupuncture, when done by a licensed practitioner, might help with pain for some patients.
Depression, Stress, and Anxiety
Adjusting to a chronic, debilitating illness sometimes leads to other problems, including depression, stress, and anxiety. Many patients with chronic fatigue syndrome (myalgic encephalomyelitis) develop depression during their illness. When present, depression or anxiety should be treated. Although treating depression or anxiety can be helpful, it is not a cure for chronic fatigue syndrome (myalgic encephalomyelitis).
Some people with chronic fatigue syndrome (myalgic encephalomyelitis) might benefit from antidepressants and anti-anxiety medications. However, doctors should use caution in prescribing these medications. Some drugs used to treat depression have other effects that might worsen other chronic fatigue syndrome (myalgic encephalomyelitis) symptoms and cause side effects. When healthcare providers are concerned about patient’s psychological condition, they may recommend seeing a mental health professional.
Some people with chronic fatigue syndrome (myalgic encephalomyelitis) might benefit from trying techniques like deep breathing and muscle relaxation, massage, and movement therapies (such as stretching, yoga, and tai chi). These can reduce stress and anxiety, and promote a sense of well-being.
Dizziness and Lightheadedness (Orthostatic Intolerance)
Some people with chronic fatigue syndrome (myalgic encephalomyelitis) might also have symptoms of orthostatic intolerance that are triggered when-or made worse by-standing or sitting upright. These symptoms can include:
- Frequent dizziness and lightheadedness
- Changes in vision (blurred vision, seeing white or black spots)
- Weakness
- Feeling like your heart is beating too fast or too hard, fluttering, or skipping a beat
For patients with these symptoms, their doctor will check their heart rate and blood pressure, and may recommend they see a specialist, like a cardiologist or neurologist.
For people with chronic fatigue syndrome (myalgic encephalomyelitis) who do not have heart or blood vessel disease, doctor might suggest patients increase daily fluid and salt intake and use support stockings. If symptoms do not improve, prescription medication can be considered.
Memory and Concentration Problems
Memory aids, like organizers and calendars, can help with memory problems. For people with chronic fatigue syndrome (myalgic encephalomyelitis) who have concentration problems, some doctors have prescribed stimulant medications, like those typically used to treat Attention-Deficit / Hyperactivity Disorder (ADHD). While stimulants might help improve concentration for some patients with chronic fatigue syndrome (myalgic encephalomyelitis), they might lead to the ‘push-and-crash’ cycle and worsen symptoms. “Push-and-crash” cycles are when someone with chronic fatigue syndrome (myalgic encephalomyelitis) is having a good day and tries to push to do more than they would normally attempt (do too much, crash, rest, start to feel a little better, do too much once again).
Living with chronic fatigue syndrome
Strategies that do not involve use of medications and might be helpful to some patients are:
- Professional counseling: Talking with a therapist to help find strategies to cope with the illness and its impact on daily life and relationships.
- Balanced diet. A balanced diet is important for everyone’s good health and would benefit a person with or without any chronic illness.
- Nutritional supplements. Doctors might run tests to see if patients lack any important nutrients and might suggest supplements to try. Doctors and patients should talk about any risks and benefits of supplements, and consider any possible interactions that may occur with prescription medications. Follow-up tests to see if nutrient levels improve can help with treatment planning.
- Complementary therapies. Therapies, like meditation, gentle massage, deep breathing, or relaxation therapy, might be helpful.
Important note: Patients should talk with their doctors about all potential therapies because many treatments that are promoted as cures for chronic fatigue syndrome (myalgic encephalomyelitis) are unproven, often costly, and could be dangerous.
Malaise causes
The following lists give examples of the diseases, conditions, and medicines that can cause malaise.
Short-term (acute) infectious disease
- Acute bronchitis or pneumonia
- Acute viral syndrome
- Infectious mononucleosis (EBV)
- Influenza
- Lyme disease
Long-term (chronic) infectious disease
- AIDS
- Chronic active hepatitis
- Disease caused by parasites
- Tuberculosis
Heart and lung (cardiopulmonary) disease
- Congestive heart failure
- Chronic obstructive pulmonary disease (COPD)
Organ failure
- Acute or chronic kidney disease
- Acute or chronic liver disease
Connective tissue disease
- Rheumatoid arthritis
- Sarcoidosis
- Systemic lupus erythematosus
Endocrine or metabolic disease
- Adrenal gland dysfunction
- Diabetes
- Pituitary gland dysfunction (rare)
- Thyroid disease
Cancer
- Leukemia
- Lymphoma (cancer that starts in the lymph system)
- Solid tumor cancers, such as colon cancer
Blood disorders
- Severe anemia
Psychiatric
- Depression
- Dysthymia
Medicines
- Anticonvulsant (antiseizure) medicines
- Antihistamines
- Beta blockers (medicines used to treat heart disease or high blood pressure)
- Psychiatric medicines
- Treatments involving several medicines
Malaise diagnosis
Your doctor will perform a physical exam and ask questions such as:
- How long has this feeling lasted (weeks or months)?
- What other symptoms do you have?
- Is the malaise constant or episodic (comes and goes)?
- Can you complete your daily activities? If not, what limits you?
- Have you traveled recently?
- What medicines are you on?
- What are your other medical problems?
- Do you use alcohol or other drugs?
You may have tests to confirm the diagnosis if your provider thinks the problem may be due to an illness. These may include blood tests, x-rays, or other diagnostic tests.
Malaise treatment
Your doctor will recommend treatment if needed based on your exam and tests.
Some changes to your lifestyle can make you feel less tired. Here are some suggestions:
- Keep a fatigue diary to help you find patterns throughout the day when you feel more or less tired.
- Exercise regularly. Almost anyone, at any age, can do some type of physical activity. If you have concerns about starting an exercise program, ask your doctor if there are any activities you should avoid. Moderate exercise may improve your appetite, energy, and outlook. Some people find that exercises combining balance and breathing (for example, tai chi or yoga) improve their energy.
- Try to avoid long naps (over 30 minutes) late in the day. Long naps can leave you feeling groggy and may make it harder to fall asleep at night.
- Stop smoking. Smoking is linked to many diseases and disorders, such as cancer, heart disease, and breathing problems, which can drain your energy.
- Ask for help if you feel swamped. Some people have so much to do that just thinking about their schedules can make them feel tired. Working with others may help a job go faster and be more fun.
Patients who believe that their symptoms are related to modifiable factors (e.g., workload, stress, coping strategies, depression, over-commitment) are much more likely to recover than those who believe that their symptoms are due to external factors, such as a viral infection 35. In a British study, 90 percent of patients who saw their family physicians for chronic fatigue received medication, diagnostic testing, or referral 36. The patients, however, were seeking to engage the physician, convey their suffering, and receive reassurance; the patients reported greatest satisfaction with physician explanations linking physical and psychological factors to psychosocial management.
Four weeks of aerobic, strength, or flexibility training is associated with improved energy and decreased fatigue 37 and moderate aerobic exercise (e.g., a daily 30-minute walk) has a more consistently positive impact on fatigue than any other intervention studied 38. Meta-analyses confirm the effectiveness of regular structured exercise. With the exception of patients with depression, pharmacologic therapy (including stimulants) only has a short-term impact 39. Cognitive behavior therapy is effective 40.
A six-week trial of an SSRI (e.g., fluoxetine [Prozac], paroxetine [Paxil], sertraline [Zoloft]) may be considered in patients with chronic fatigue if depression is possible 41. If the patient has difficulty getting restful sleep, trazodone (Desyrel, brand no longer available in the United States), doxepin, or imipramine (Tofranil) may be effective 42. If pain is present, the patient may respond to venlafaxine (Effexor), desipramine (Norpramin), nortriptyline (Pamelor), duloxetine (Cymbalta), or a nonsteroidal anti-inflammatory drug.
Fatigue, even when linked with a disease process, is associated with an imbalance of sleep, stress, or psychological coping skills. Balancing these factors reduces reliance on and is more effective than medication 36. Regular visits (i.e., every two weeks to two months) allow physicians to focus on fatigue as a central problem and circumvent the tendency for these patients to present at urgent care appointments 43.
- ABDULLA J, Torpy BDJ. Chronic Fatigue Syndrome. [Updated 2017 Apr 20]. In: De Groot LJ, Chrousos G, Dungan K, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279099[↩][↩][↩]
- Fahlén G, Knutsson A, Peter R, et al. Effort-reward imbalance, sleep disturbances and fatigue. Int Arch Occup Environ Health. 2006;79(5):371–378.[↩]
- Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. https://www.cdc.gov/me-cfs/[↩]
- Fatigue: An Overview. Am Fam Physician. 2008 Nov 15;78(10):1173-1179. https://www.aafp.org/afp/2008/1115/p1173.html[↩][↩][↩][↩]
- Brown RF, Schutte NS. Direct and indirect relationships between emotional intelligence and subjective fatigue in university students. J Psychosom Res. 2006;60(6):585–593.[↩]
- Shen J, Botly LC, Chung SA, Gibbs AL, Sabanadzovic S, Shapiro CM. Fatigue and shift work. J Sleep Res. 2006;15(1):1–5.[↩]
- Bailes S, Libman E, Baltzan M, Amsel R, Schondorf R, Fichten CS. Brief and distinct empirical sleepiness and fatigue scales. J Psychosom Res. 2006;60(6):605–613.[↩]
- Lane TJ, Matthews DA, Manu P. The low yield of physical examinations and laboratory investigations of patients with chronic fatigue. Am J Med Sci. 1990;299(5):313–318.[↩]
- Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann Intern Med. 1994;121(12):953–959.[↩]
- Pilcher JJ, Ginter DR, Sadowsky B. Sleep quality versus sleep quantity: relationships between sleep and measures of health, well-being and sleepiness in college students. J Psychosom Res. 1997;42(6):583–596.[↩]
- Alam T, Alessi CA. Sleep disorders. In: Rosenthal TC, Williams ME, Naughton BJ, eds. Office Care Geriatrics. Philadelphia, Pa.: Lippincott Williams & Wilkins; 2006:254–265.[↩]
- Arora V, Dunphy C, Chang VY, Ahmad F, Humphrey HJ, Meltzer D. The effects of on-duty napping on intern sleep time and fatigue. Ann Intern Med. 2006;144(11):792–798.[↩]
- Sonnentag S, Zijlstra FR. Job characteristics and off-job activities as predictors of need for recovery, well-being, and fatigue. J Appl Psychol. 2006;91(2):330–350.[↩]
- Guilleminault C, Ramar K. Naps and drugs to combat fatigue and sleepiness. Ann Intern Med. 2006;144(11):856–857.[↩][↩]
- Taylor AH, Dorn L. Stress, fatigue, health, and risk of road traffic accidents among professional drivers: the contribution of physical inactivity. Annu Rev Public Health. 2006;27:371–391.[↩]
- O’Connor PJ, Puetz TW. Chronic physical activity and feelings of energy and fatigue. Med Sci Sports Exerc. 2005;37(2):299–305.[↩]
- Smith L, Tanigawa T, Takahashi M, et al. Shiftwork locus of control, situational and behavioural effects on sleepiness and fatigue in shiftworkers. Ind Health. 2005;43(1):151–170.[↩]
- Rietjens GJ, Kuipers H, Adam JJ, et al. Physiological, biochemical and psychological markers of strenuous training-induced fatigue. Int J Sports Med. 2005;26(1):16–26.[↩]
- Berlin AA, Kop WJ, Deuster PA. Depressive mood symptoms and fatigue after exercise withdrawal: the potential role of decreased fitness. Psychosom Med. 2006;68(2):224–230.[↩]
- Munch TN, Zhang T, Willey J, Palmer JL, Bruera E. The association between anemia and fatigue in patients with advanced cancer receiving palliative care. J Palliat Med. 2005;8(6):1144–1149.[↩]
- Verdon F, Burnand B, Stubi CL, et al. Iron supplementation for unexplained fatigue in non-anaemic women: double blind randomised placebo controlled trial. BMJ. 2003;326(7399):1124.[↩]
- van Weert E, Hoekstra-Weebers J, Otter R, Postema K, Sanderman R, van der Schans C. Cancer-related fatigue: predictors and effects of rehabilitation. Oncologist. 2006;11(2):184–196.[↩]
- Mock V. Evidence-based treatment for cancer-related fatigue. J Natl Cancer Inst Monogr. 2004;(32):112–118.[↩]
- Greco T, Eckert G, Kroenke K. The outcome of physical symptoms with treatment of depression. J Gen Intern Med. 2004;19(8):813–818.[↩]
- Bruera E, Valero V, Driver L, et al. Patient-controlled methylphenidate for cancer fatigue: a double-blind, randomized, placebo-controlled trial. J Clin Oncol. 2006;24(13):2073–2078.[↩]
- Reineke-Bracke H, Radbruch L, Elsner F. Treatment of fatigue: modafinil, methylphenidate, and goals of care. J Palliat Med. 2006;9(5):1210–1214.[↩]
- Fitzgibbon EJ, Murphy D, O’Shea K, Kelleher C. Chronic debilitating fatigue in Irish general practice: a survey of general practitioners’ experience. Br J Gen Pract. 1997;47(423):618–622.[↩][↩]
- Taylor RR, Jason LA, Curie CJ. Prognosis of chronic fatigue in a community-based sample. Psychosom Med. 2002;64(2):319–327.[↩]
- Darbishire L, Ridsdale L, Seed PT. Distinguishing patients with chronic fatigue from those with chronic fatigue syndrome: a diagnostic study in UK primary care. Br J Gen Pract. 2003;53(491):441–445.[↩]
- Sugarman JR, Berg AO. Evaluation of fatigue in a family practice. J Fam Pract. 1984;19(5):643–647.[↩]
- Raine R, Carter S, Sensky T, Black N. General practitioners’ perceptions of chronic fatigue syndrome and beliefs about its management, compared with irritable bowel syndrome: qualitative study. BMJ. 2004;328(7452):1354–1357.[↩]
- Holmes GP, Kaplan JE, Gantz NM, et al. Chronic fatigue syndrome: a working case definition. Ann Intern Med. 1988;108(3):387–389.[↩]
- Carruthers BM, Jain AK, De Meirleir KL, et al. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols. J Chronic Fatigue Syndr 2003;11(1):7-115.[↩][↩]
- Sharpe MC, Archard LC, Banatvala JE, et al. A report – chronic fatigue syndrome: guidelines for research. J Roy Soc of Med 1991;84: 118-21.[↩]
- Sharpe M. Psychiatric management of PVFS. Br Med Bull. 1991;47(4):989–1005.[↩]
- Dowrick CF, Ring A, Humphris GM, Salmon P. Normalisation of unexplained symptoms by general practitioners: a functional typology. Br J Gen Pract. 2004;54(500):165–170.[↩][↩]
- Puetz TW, O’Connor PJ, Dishman RK. Effects of chronic exercise on feelings of energy and fatigue: a quantitative synthesis. Psychol Bull. 2006;132(6):866–876.[↩]
- Powell P, Bentall RP, Nye FJ, Edwards RH. Randomised controlled trial of patient education to encourage graded exercise in chronic fatigue syndrome. BMJ. 2001;322(7283):387–390.[↩]
- Blockmans D, Persoons P, Van Houdenhove B, Bobbaers H. Does methylphenidate reduce the symptoms of chronic fatigue syndrome? Am J Med. 2006;119(2):167.e23–30.[↩]
- Whiting P, Bagnall AM, Sowden AJ, Cornell JE, Mulrow CD, Ramírez G. Interventions for the treatment and management of chronic fatigue syndrome: a systematic review [published correction appears in JAMA. 2002;287(11):1401]. JAMA. 2001;286(11):1360–1368.[↩]
- Stulemeijer M, de Jong LW, Fiselier TJ, Hoogveld SW, Bleijenberg G. Cognitive behaviour therapy for adolescents with chronic fatigue syndrome: randomised controlled trial [published correction appears in BMJ. 2005;330(7495):820]. BMJ. 2005;330(7481):14.[↩]
- Smith RC, Lein C, Collins C, et al. Treating patients with medically unexplained symptoms in primary care. J Gen Intern Med. 2003;18(6):478–489.[↩]
- Rosenthal TC, Griswold KS, Danzo A. Puzzling physical conditions. AAFP home study essentials, 334. Leawood, Kan.: American Academy of Family Physicians; 2007.[↩]