Contents
- Causes of smelly urine
- What are urinary tract infections (UTIs)
- What are the types of urinary tract infections?
- How do you get a urinary tract infection?
- Urinary tract infection women
- Urinary tract infections in children
- Urinary tract infection signs and symptoms
- Urinary tract infection prognosis
- Urinary tract infection causes
- Urinary tract infection prevention
- Urinary tract infection diagnosis
- Urinary tract infection treatment
Causes of smelly urine
Smelly urine on its own isn’t usually a cause for concern. There are often things you can do to help your urine return to normal.
Common causes of smelly urine
Urine is usually clear or pale yellow, with a mild smell.
Common things that can make your urine smell stronger include:
- certain types of food and drink, like asparagus or coffee
- being dehydrated
- some medicines
- vitamin B6 supplements
Less common causes of smelly urine
Other symptoms you have might give you an idea of what’s causing your pee to smell. But don’t self-diagnose – always see a doctor.
| Symptoms | Possible cause |
|---|---|
| Feeling very thirsty and tired, peeing more than usual, sweet-smelling pee | type 2 diabetes |
| Lower back pain, pain when peeing, blood in pee | kidney stones |
| Yellow skin and eyes (jaundice), tummy pain, nausea and vomiting | liver failure |
Things you can do yourself
Try these things to help keep your urine clear and smelling mild.
- Drink plenty of fluids, particularly water or squash – drink more in hot weather and when exercising
- DO NOT drink a lot of coffee or alcohol
- DO NOT eat garlic or asparagus – they contain strong-smelling chemicals that can pass into your pee
- DO NOT take more than 10mg of vitamin B6 a day
See a doctor if you have smelly urine and:
- you need to urine suddenly, or more often than usual
- you have pain or a burning sensation when urineing
- there’s blood in your urine
- you have lower tummy pain
- you feel tired and unwell
- you’re feeling confused or agitated
These may be symptoms of a urinary tract infection (UTI).
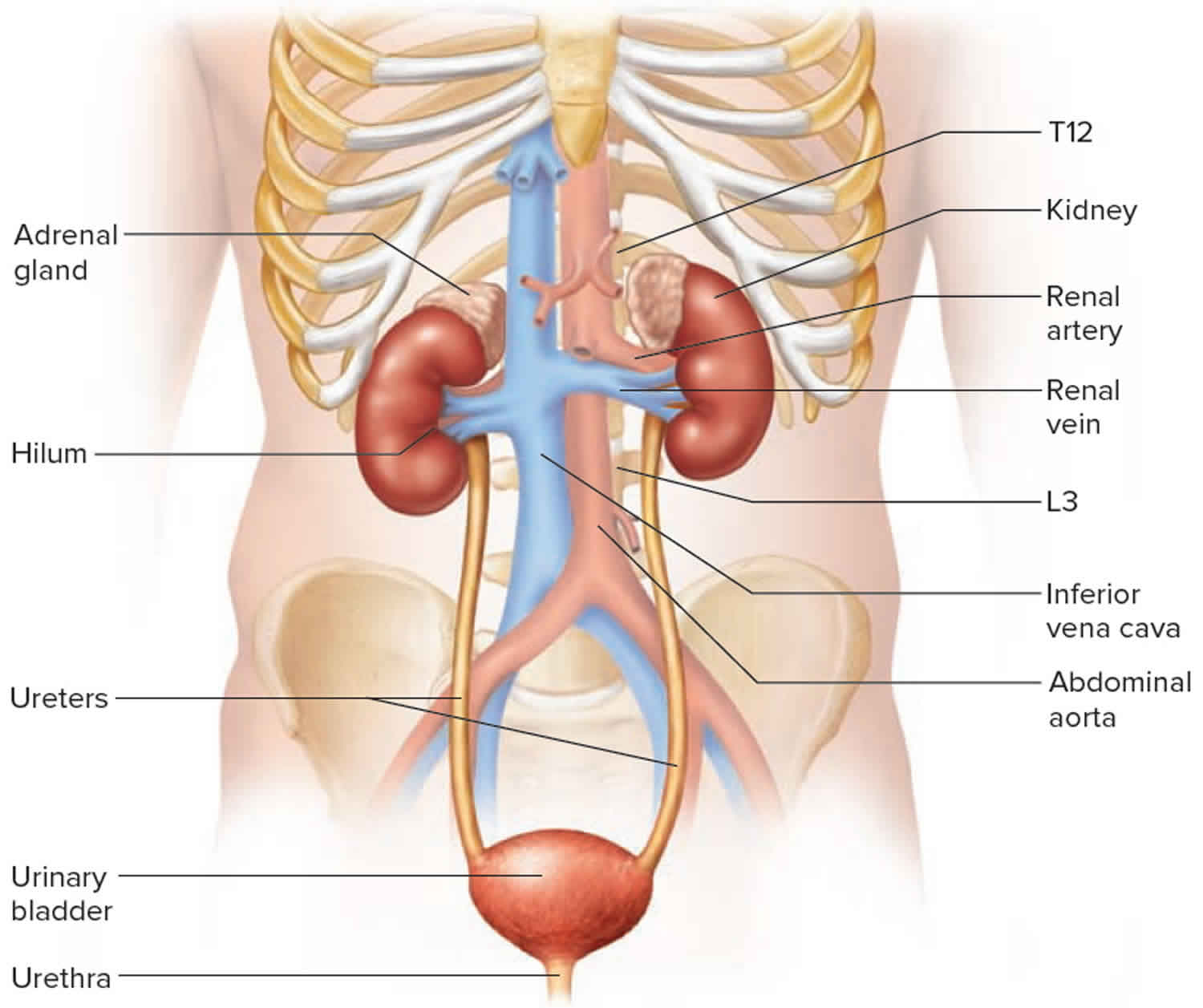
Figure 1. Urinary tract anatomy
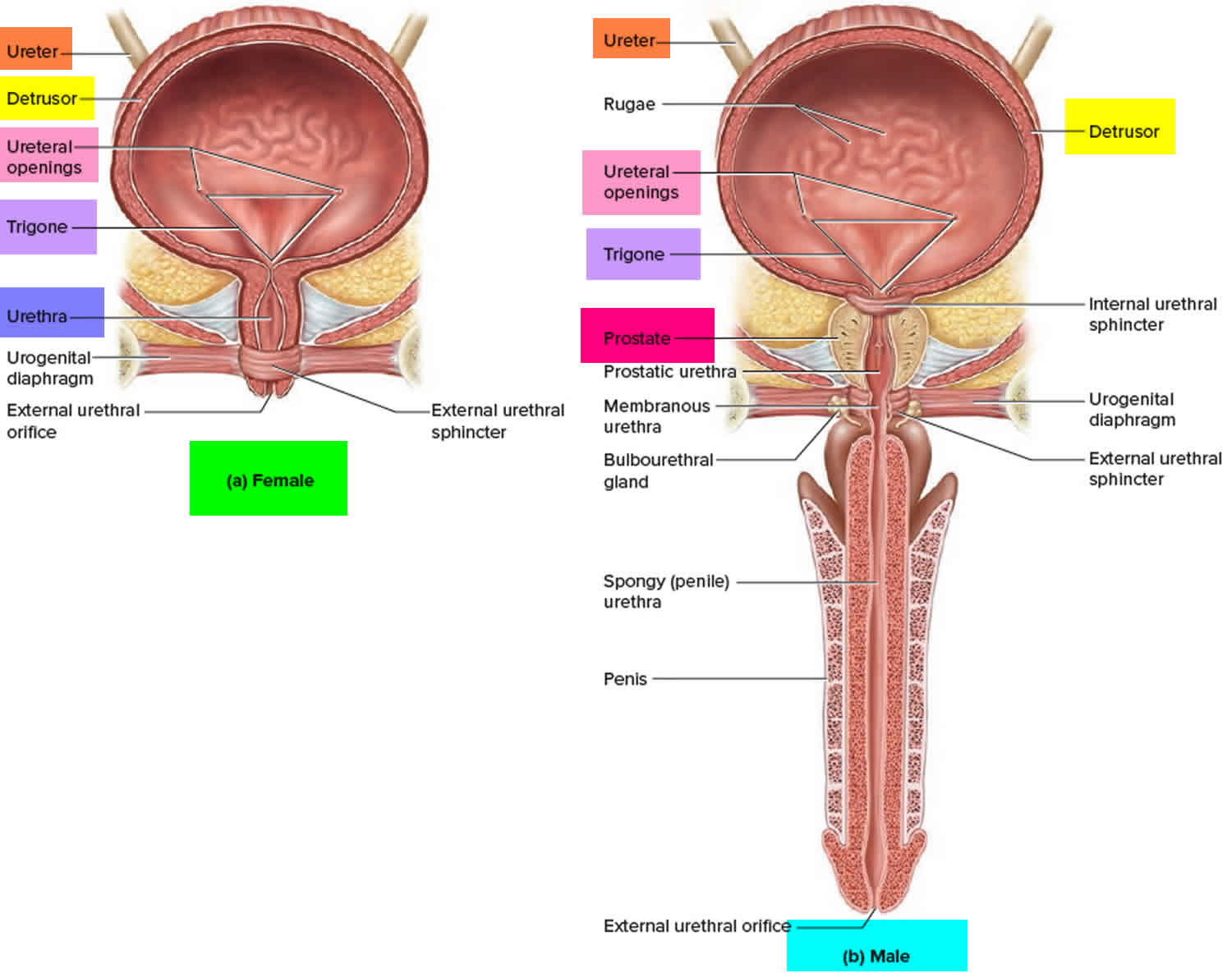
Figure 2. Urinary bladder anatomy
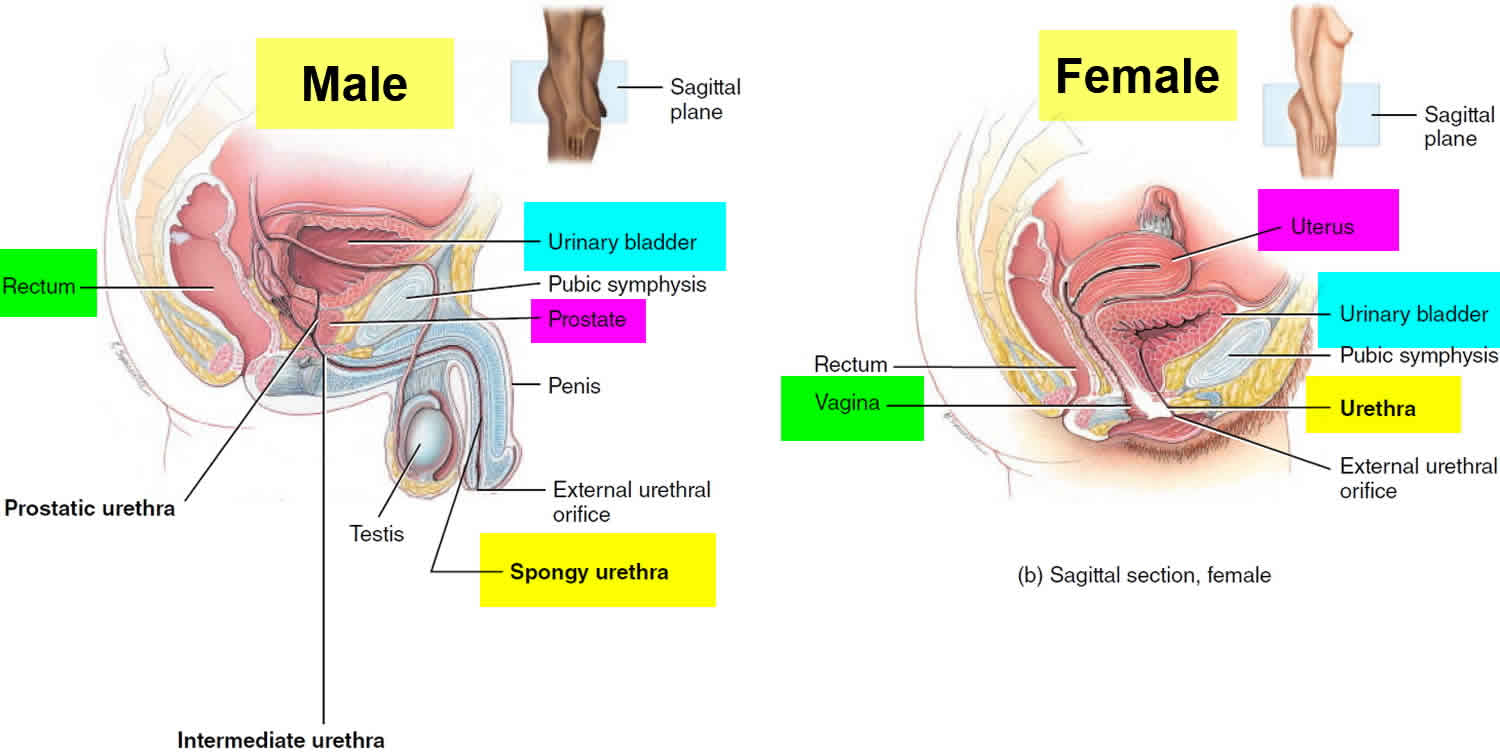
Figure 3. Urinary bladder location
What are urinary tract infections (UTIs)
Urinary tract infections can affect different parts of your urinary tract, including your bladder (cystitis), urethra (urethritis) or kidneys (kidney infection). Most urinary tract infections can be easily treated with antibiotics.
A urinary tract infection is caused by bacteria entering the urinary tract, leading to an infection in the bladder, ureters (tubes that connect the kidneys to the bladder), urethra (tube connecting the bladder to the outside world), or kidneys. A urinary tract infection can affect any part of the urinary system, but most commonly occurs in the bladder (cystitis) and/or urethra (urethritis). Urinary tract infections can be painful and annoying, but usually clear up with a course of antibiotics. If untreated, urinary tract infections can lead to kidney infection, so it’s important to visit your doctor for early treatment.
The urinary system is your body’s drainage system for removing wastes and extra water. The urinary system includes two kidneys, two ureters, a bladder, and a urethra. Urinary tract infections are the second most common type of infection in the body.
Urinary tract infections don’t always cause signs and symptoms, but when they do you may notice:
- Pain or burning when you urinate
- Fever, tiredness, or shakiness
- A need to urinate small amounts often, or with urgency
- Pressure or feel uncomfortable in your lower belly
- Urine that smells bad or looks cloudy or reddish (a sign of blood in the urine)
- Pain in your back or side below the ribs
- Pelvic pain, in women — especially in the center of the pelvis and around the area of the pubic bone
People of any age or sex can get urinary tract infections. But about 30 times as many women get urinary tract infections as men 1. You’re also at higher risk if you have diabetes, need a tube (catheter) to drain your bladder, or have a spinal cord injury.
The increased rate of urinary infection in the female population is explained by the difference in length of the male and female urethra. Most urinary tract infections occur when bacteria ascend from the genital region through the urethra and into the urinary bladder above. The average female urethra is approximately 4 cm long, permitting easy entry of bacteria into the bladder and cause infection. The average male urethra is 15-20 cm long, providing better protection against infection by way of its increased length. Besides the increased physical distance bacteria must travel to cause infection, the male urethra has a greater surface area to secrete antibodies to combat infection of the urinary tract.
Urinary tract infection also has special significance in children for a number of reasons. Firstly, urinary tract infection is less easily diagnosed and thus more likely to progress to a serious extent if the problem infection is not treated. Also, urinary tract infections during childhood may be the first sign of “vesico-ureteric reflux” in which urine is allowed to flow back from the bladder to the kidneys. If left untreated, these patients may develop long-term kidney problems. When managed appropriately however, these long term problems are most often avoided.
If you think you have a urinary tract infection it is important to see your doctor. Your doctor can tell if you have a urinary tract infection with a urine test. Treatment is with antibiotics. Your doctor will usually prescribe a course of antibiotics that should get rid of the symptoms in a few days.
As with any course of antibiotics, it is important to complete the entire course, even if your symptoms have settled down or disappeared.
Sometimes, people with a kidney infection or those at risk of complications may need to be treated in a hospital.
The urinary tract infection is usually an isolated event, which will never recur in 90% of patients affected. In the vast majority of cases, the simple lower urinary tract infection will be easily treated with a 3-5 day course of oral antibiotics. Upper urinary tract infections may require admission to hospital for a short course of intravenous antibiotics with an oral course to be completed on discharge. The symptoms of infection will gradually subside of the course of treatment.
Recurrent urinary tract infections therefore occur in 10% of patients following their first event. The significance of recurrent infection is determined through assessment of urinary tract function. If the urinary tracts are normal, there is little chance that infection will spread to the kidneys and cause renal impairment. If the urinary tracts are abnormal (e.g. kidney stones) and an associated disease such as diabetes is present, the infection will more likely spread to the kidneys where repeat infection will result in long-term kidney impairment.
Symptoms of a urinary tract infection
Symptoms of a urinary tract infection include:
- needing to pee suddenly or more often than usual
- pain or a burning sensation when peeing
- smelly or cloudy pee
- blood in your pee
- pain in your lower tummy
- feeling tired and unwell
- in older people, changes in behavior such as severe confusion or agitation
Children with urinary tract infections may also:
- appear generally unwell – babies may be irritable, not feed properly and have a high temperature (fever) of 99.5 °F (37.5 °C) or above
- wet the bed or wet themselves
- deliberately hold in their pee because it stings
See a doctor if:
- you’re a man with symptoms of a urinary tract infection
- you’re pregnant and have symptoms of a urinary tract infection
- your child has symptoms of a urinary tract infection
- you’re caring for someone elderly who may have a urinary tract infection
- you have not had a urinary tract infection before
- you have blood in your pee
- your symptoms do not improve within a few days
- your symptoms come back after treatment
If you have symptoms of a sexually transmitted infection (STI), you can also get treatment from a sexual health clinic.
You are at greater risk of developing complications from a urinary tract infection and should seek medical advice promptly if you:
- have existing kidney disease, diabetes, or another chronic condition
- are pregnant
- are over the age of 65
- or have one or more of the following symptoms – high temperature 100.4 °F (38°C or above), shivering, nausea and/or vomiting, diarrhea or worsening pain in your abdomen, pelvis or back.
Children and babies and urinary tract infections
See your doctor promptly if you think your child or baby has a urinary tract infection (or another infection). Although urinary tract infection in children can usually be treated quickly and effectively, serious complications can occur if left untreated. This includes scarring of the kidneys, which may cause kidney disease and high blood pressure (hypertension).
Can my eating, diet, and nutrition help prevent bladder infections?
Experts don’t think eating, diet, and nutrition play a role in preventing or treating bladder infections. Although some research shows that cranberry juice, extract, or pills may help prevent these infections, not enough evidence shows this. Research shows that cranberry products are not effective in treating a bladder infection if you already have one 2, 3, 4.
There’s mixed evidence that cranberry can help to prevent urinary tract infections:
- In a 2016 year-long study of 147 women living in nursing homes 5, taking two daily cranberry capsules decreased bacteria levels in their urine in the first 6 months of the study, but didn’t decrease their frequency of urinary tract infections over the year of the study, compared to taking a placebo. The two capsules together contained as much proanthocyanidin, a compound that is believed to protect against bacteria, as 20 ounces of cranberry juice.
- A 2012 research review of 13 clinical trials 6 suggested that cranberry may help reduce the risk of urinary tract infections in certain groups, including women with recurrent urinary tract infections, children, and people who use cranberry-containing products more than twice daily.
- A 2012 research review of 24 clinical trials 7 concluded that cranberry juice and supplements don’t prevent urinary tract infections but many of the studies were poor quality.
Cranberry hasn’t been shown to be effective as a treatment for an existing urinary tract infection.
Can drinking liquid help prevent or relieve bladder infections?
Yes. Drink six to eight, 8-ounce glasses of liquid a day. Talk with a health care professional if you can’t drink this amount due to other health problems, such as urinary incontinence, urinary frequency, or kidney failure. The amount of liquid you need to drink depends on the weather and your activity level. If you live, work, or exercise in hot weather, you may need more liquid to replace the fluid you lose through sweat.
What are the types of urinary tract infections?
Each type of urinary tract infection may result in more-specific signs and symptoms, depending on which part of your urinary tract is infected.
The types of urinary tract infections include:
- Cystitis: urinary tract infection affecting the bladder.
- Signs and symptoms:
- Pelvic pressure
- Lower abdomen discomfort
- Frequent, painful urination
- Blood in urine
- Signs and symptoms:
- Urethritis: urinary tract infection affecting the urethra.
- Signs and symptoms:
- Burning with urination
- Discharge
- Signs and symptoms:
- Pyelonephritis: urinary tract infection affecting the kidneys.
- Signs and symptoms:
- Upper back and side (flank) pain
- High fever
- Shaking and chills
- Nausea
- Vomiting
- Signs and symptoms:
- Ureteritis: urinary tract infection affecting the ureters.
Urinary tract infection possible complications
Complications of urinary tract infections aren’t common, but they can be serious and require immediate treatment by a doctor. They usually affect people diagnosed with diabetes, a weakened immune system, men with recurrent urinary tract infections, or women who are pregnant.
Lower urinary tract infections, such as cystitis (urinary tract infection affecting the bladder) or urethritis (urinary tract infection affecting the urethra), don’t often cause complications if they are treated properly.
If a urinary tract infection is left untreated, bacteria may travel to the kidneys causing kidney infection, damage and even kidney failure. Blood poisoning can happen and occurs when the infection spreads from the kidneys to the blood-stream.
If the infection moves to the kidneys, there may be high fever, back pain, diarrhea and vomiting. If you have these symptoms, it is important to see your doctor.
Sometimes complications can occur, especially in people with weakened immune systems or upper urinary tract infections. These can include:
- Recurrent infections, especially in women who experience two or more urinary tract infections in a six-month period or four or more within a year.
- Permanent kidney damage or kidney failure from an acute or chronic kidney infection (pyelonephritis) due to an untreated urinary tract infection.
- Increased risk in pregnant women of delivering low birth weight or premature infants.
- Urethral narrowing (stricture) in men from recurrent urethritis, previously seen with gonococcal urethritis.
- Inflamed prostate in men (prostatitis)
- Sepsis (blood poisoning): a serious infection that can develop when the urinary tract infection spreads from the kidneys to the blood.
Table 1. Risk Factors for Complicated Urinary Tract Infections*
Patient characteristics |
Male sex |
Postmenopausal† |
Pregnant |
Presence of hospital-acquired urinary tract infection |
Symptoms present for seven or more days before presentation |
Medical conditions |
Diabetes mellitus† |
Immunocompromised status |
Urologic conditions |
History of childhood or recurrent urinary tract infections† |
Indwelling catheter |
Neurogenic bladder |
Polycystic kidney disease |
Recent urologic instrumentation |
Renal transplant |
Urolithiasis |
Urologic obstruction |
Urologic stents |
*—Increased chance of treatment failure.
†—Some experts consider the following groups to be uncomplicated: healthy post-menopausal women; patients with well-controlled diabetes; and patients with recurrent cystitis that responds to treatment.
How do you get a urinary tract infection?
Urinary tract infections typically occur when bacteria (e.g., Escherichia coli) that live in the digestive system enter the urinary tract through the urethra and begin to multiply in the bladder. Although the urinary system is designed to keep out such microscopic invaders, these defenses sometimes fail. When that happens, bacteria may take hold and grow into a full-blown infection in the urinary tract.
The most common urinary tract infections occur mainly in women and affect the bladder and urethra.
- Infection of the bladder (cystitis). This type of urinary tract infection is usually caused by Escherichia coli (E. coli), a type of bacteria commonly found in the gastrointestinal (GI) tract. However, sometimes other bacteria are responsible. Sexual intercourse may lead to cystitis, but you don’t have to be sexually active to develop it. All women are at risk of cystitis because of their anatomy — specifically, the short distance from the urethra to the anus and the urethral opening to the bladder.
- Infection of the urethra (urethritis). This type of urinary tract infection can occur when gastrointestinal bacteria spread from the anus to the urethra. Also, because the female urethra is close to the vagina, sexually transmitted infections, such as herpes, gonorrhea, chlamydia and mycoplasma, can cause urethritis.
Urinary tract infections are more common in women than men. This is because in women, the urethra is closer to the anus than it is in men, and is also shorter. This means the chances of bacteria entering the urinary system are greater in women.
Women have a 1-in-3 chance of developing a urinary tract infection in their lifetime. The risk of developing a urinary tract infection increases with age for both men and women.
Women are more likely to develop a urinary tract infection if they:
- Are sexually active: This is because having sex can irritate the urethra. When this happens it allows bacteria to travel more easily though the urethra and into the bladder.
- Use a diaphragm as contraception: The diaphragm can put pressure on the bladder and stop it from emptying properly.
- Develop an irritation to spermicide used on condoms: Some women develop a vaginal irritation from spermicide, making the area more vulnerable to infection.
- Are pregnant: Hormonal changes during pregnancy make women more vulnerable to urinary tract infections.
- Have gone through menopause: When levels of the hormone oestrogen decline, women may become more vulnerable to developing a urinary tract infection.
Overall, people are more likely to develop a urinary tract infection if they have:
- Kidney stones or another condition that blocks the urinary tract.
- A condition that stops the bladder from emptying fully (e.g. an enlarged prostate that presses on the bladder).
- A urinary catheter (a tube inserted into the urethra going into the bladder; often used after surgery if a person has to remain in bed for some time).
- A medical condition involving the bladder or kidneys (e.g. some babies are born with problems that stop the urine travelling properly though the urinary system).
- A medical condition that weakens the immune system (e.g. diabetes).
- Medical treatments that weaken the immune system (e.g. chemotherapy).
- A recent medical procedure on the urinary tract.
Babies and older people are also more prone to urinary tract infections.
Men with an enlarged prostate may be more prone to urinary tract infections, as this may affect the flow of urine.
Urinary tract infection women
Women get urinary tract infections up to 30 times more often than men do 1. Also, as many as 4 in 10 women who get a urinary tract infection will get at least one more within six months 9.
Urinary tract infections are caused by bacteria or, rarely, yeast getting into your urinary tract. Once there, they multiply and cause inflammation (swelling) and pain. You can help prevent urinary tract infections by wiping from front to back after using the bathroom.
Women get urinary tract infections more often because a woman’s urethra (the tube from the bladder to where the urine comes out of the body) is shorter than a man’s. This makes it easier for bacteria to get into the bladder. A woman’s urethral opening is also closer to both the vagina and the anus, the main source of germs such as Escherichia coli (E. coli) that cause urinary tract infections 10.
You may be at greater risk for a urinary tract infection if you 11:
- Are sexually active. Sexual activity can move germs that cause urinary tract infections from other areas, such as the vagina, to the urethra.
- Use a diaphragm for birth control or use spermicides (creams that kill sperm) with a diaphragm or with condoms. Spermicides can kill good bacteria that protect you from urinary tract infections.
- Are pregnant. Pregnancy hormones can change the bacteria in the urinary tract, making urinary tract infections more likely. Also, many pregnant women have trouble completely emptying the bladder, because the uterus (womb) with the developing baby sits on top of the bladder during pregnancy. Leftover urine with bacteria in it can cause a urinary tract infection.
- Have gone through menopause. After menopause, loss of the hormone estrogen causes vaginal tissue to become thin and dry. This can make it easier for harmful bacteria to grow and cause a urinary tract infection.
- Have diabetes, which can lower your immune (defense) system and cause nerve damage that makes it hard to completely empty your bladder
- Have any condition, like a kidney stone, that may block the flow of urine between your kidneys and bladder
- Have or recently had a catheter in place. A catheter is a thin tube put through the urethra into the bladder. Catheters drain urine when you cannot pass urine on your own, such as during surgery.
Urinary tract infection symptoms in women
If you have a urinary tract infection, you may have some or all of these symptoms 12:
- Pain or burning when urinating
- An urge to urinate often, but not much comes out when you go
- Pressure in your lower abdomen
- Urine that smells bad or looks milky or cloudy
- Blood in the urine. This is more common in younger women. If you see blood in your urine, tell a doctor or nurse right away.
- Feeling tired, shaky, confused, or weak. This is more common in older women.
- Having a fever, which may mean the infection has reached your kidneys
How do urinary tract infections affect pregnancy?
Changes in hormone levels during pregnancy raise your risk for urinary tract infections. urinary tract infections during pregnancy are more likely to spread to the kidneys.
If you’re pregnant and have symptoms of a urinary tract infection, see your doctor or nurse right away. Your doctor will give you an antibiotic that is safe to take during pregnancy.
If left untreated, urinary tract infections could lead to kidney infections and problems during pregnancy, including:
- Premature birth (birth of the baby before 39 to 40 weeks)
- Low birth weight (smaller than 5 1/2 pounds at birth)
- High blood pressure, which can lead to a more serious condition called preeclampsia 13
What should I do if I keep getting urinary tract infections?
Women who get two urinary tract infections in six months or three in a year have recurrent urinary tract infections 14. Your doctor or nurse might do tests to find out why. If the test results are normal, you may need to take a small dose of antibiotics every day to prevent infection. Your doctor may also give you a supply of antibiotics to take after sex or at the first sign of infection 15.
How can I prevent urinary tract infections?
You can take steps to help prevent a urinary tract infection. But you may follow these steps and still get a urinary tract infection.
- Urinate when you need to. Don’t go without urinating for longer than three or four hours. The longer urine stays in the bladder, the more time bacteria have to grow.
- Try to urinate before and after sex.
- Always wipe from front to back.
- Try to drink six to eight glasses of fluid per day.
- Clean the anus and the outer lips of your genitals each day.
- Do not douche or use feminine hygiene sprays.
- If you get a lot of urinary tract infections and use creams that kill sperm (spermicides), talk to your doctor or nurse about using a different form of birth control instead.
- Wear underpants with a cotton crotch. Avoid tight-fitting pants, which trap moisture, and change out of wet bathing suits and workout clothes quickly.
- Take showers, or limit baths to 30 minutes or less.
Urinary tract infections in children
Urinary tract infections are relatively common in children, particularly young children still in nappies. Girls are more likely than boys to develop a urinary tract infection, except in the first 12 months of life, when boys seem to be more susceptible.
The most common organisms that infect the urine are bacteria that normally live in the bowel. Wiping your child’s bottom from the front to the back (rather than from back to front) can help prevent carrying bacteria from the bowel to the urinary tract.
Urinary tract infections, especially ones that recur, can also be caused by your child’s bladder not emptying properly or sometimes by structural problems of the kidneys or bladder.
Underlying kidney and bladder problems
Urine is made in the kidneys and then normally flows down from the kidneys into the bladder via the ureters. From the bladder, urine can leave the body via the urethra. In some children, urine flows back up the ureters towards the kidneys rather than being passed straight down the urethra. This abnormal flow of urine is called urinary reflux or sometimes vesico-ureteric reflux.
Urinary reflux can be harmful because it not only predisposes your child to infection (because of some urine always being left in the bladder) but it can also contribute to scarring of the kidneys if the reflux is severe.
Some children (including infants and those with severe infections) need to be tested for problems with their kidneys or bladder after having a single urinary tract infection. Most children should be tested after having recurrent urinary tract infections. These tests help show any problems with the urinary tract and whether the urine is flowing in the right direction.
The tests usually include:
- a kidney and bladder ultrasound (which can show problems with the kidneys, ureters and bladder); with or without
- a bladder X-ray, known as a micturating cystourethrogram (MCUG).
In an micturating cystourethrogram (MCUG), a catheter (thin tube) is passed into the bladder and dye is injected through it. It will show what happens when your child passes urine and whether urine is flowing in the right direction.
Occasionally, special nuclear medicine scans (DMSA and MAG3) may be recommended to help detect kidney scarring or urinary reflux.
The treatment of vesico-ureteric reflux may involve ongoing use of antibiotics in some children to prevent severe or recurrent infections. Antibiotics may be initially recommended for 6 months in these cases.
Usually with time, the reflux will improve by itself. In some severe cases, surgery may be recommended to treat the reflux.
Self-care measures for preventing urinary tract infections
In children who have had urinary tract infections, the following measures may help prevent further infections.
- Getting your child to drink plenty of fluids.
- Ensuring your child empties their bladder when they get the urge and doesn’t delay going to the toilet.
- Making sure your child properly cleans themselves and wipes from front to back after toileting.
- Avoiding bubble baths (which may irritate the urethra).
- Seeing your doctor for advice on treating constipation in children, which can contribute to problems with bladder emptying.
Signs and symptoms of urinary tract infections in children
Clinical signs and symptoms of a urinary tract infection depend on the age of the child. Newborns with urinary tract infection may present with jaundice, sepsis, failure to thrive, vomiting, or fever 16. In infants and young children, typical signs and symptoms include fever, strong-smelling urine, hematuria, abdominal or flank pain, and new-onset urinary incontinence 16. School-aged children may have symptoms similar to adults, including dysuria, frequency, or urgency 16. Boys are at increased risk of urinary tract infection if younger than six months, or if younger than 12 months and uncircumcised. Girls are generally at an increased risk of urinary tract infection, particularly if younger than one year 17. Physical examination findings can be nonspecific but may include suprapubic tenderness or costovertebral angle tenderness.
Symptoms of a urinary tract infection can vary. In infants and young children, symptoms are often non-specific and can include:
- fever;
- irritability;
- vomiting;
- diarrhea;
- tiredness;
- smelly urine;
- poor feeding; or
- failure to put on weight.
As children get older, the symptoms often become more specific, such as:
- pain or stinging on passing urine;
- accidentally wetting themselves when they’ve been toilet trained previously;
- abdominal or back pain; and
- going to the toilet more frequently than usual.
Fever may or may not be present.
Urinary tract infection tests and diagnosis in children
Your doctor will ask about your child’s symptoms and perform a physical examination, looking for signs of a urinary tract infection.
To diagnose a urinary tract infection, your doctor will need to send a urine specimen to the laboratory for testing. In older children, this can easily be done by collecting a sample in a specimen jar as your child passes urine into the toilet.
In younger children, urine samples can be more difficult to collect. The most common collection method used in infants and toddlers who wear nappies is removing the nappy, waiting for the child to urinate and trying to catch some urine in a specimen jar.
Very occasionally, your doctor may need to insert a tube (catheter) through the urethra into your child’s bladder, or pass a fine needle into the bladder through the wall of the abdomen to collect a sample.
So called ‘bag urines’, where an adhesive plastic collecting bag is used to collect urine, frequently yield contaminated samples which cannot provide a diagnosis; if this method is used, it’s best that a nurse or doctor performs the collection rather than trying to do it yourself at home.
Treatment of urinary tract infections in children
If your child is unwell and a urinary tract infection is strongly suspected, your doctor may prescribe antibiotics as soon as the urine specimen is collected. Otherwise your doctor may wait until the result of the urine test is known.
Commonly, antibiotics are given by mouth. However, in some cases, such as in children who are extremely unwell or in very young infants, antibiotics will be given via a drip into a vein (intravenous antibiotics). Intravenous (IV) antibiotics need to be given in hospital.
Some children with urinary tract infections may be referred to a pediatrician (specialist in children’s health) for further assessment and treatment.
Table 2. Antibiotics Commonly Used to Treat Urinary Tract Infections in Children
| Antibiotic | Dosing | Common adverse effects |
|---|---|---|
Amoxicillin/clavulanate (Augmentin) | 25 to 45 mg per kg per day, divided every 12 hours | Diarrhea, nausea/vomiting, rash |
Cefixime (Suprax) | 8 mg per kg every 24 hours or divided every 12 hours | Abdominal pain, diarrhea, flatulence, rash |
Cefpodoxime | 10 mg per kg per day, divided every 12 hours | Abdominal pain, diarrhea, nausea, rash |
Cefprozil (Cefzil) | 30 mg per kg per day, divided every 12 hours | Abdominal pain, diarrhea, elevated results on liver function tests, nausea |
Cephalexin (Keflex) | 25 to 50 mg per kg per day, divided every 6 to 12 hours | Diarrhea, headache, nausea/vomiting, rash |
Trimethoprim/sulfamethoxazole (Bactrim, Septra) | 8 to 10 mg per kg per day, divided every 12 hours | Diarrhea, nausea/vomiting, photosensitivity, rash |
Urinary tract infection signs and symptoms
Common symptoms of a urinary tract infection include:
- A burning sensation when passing urine.
- The need to urinate urgently.
- Passing urine more frequently than usual.
- Feeling the urge to urinate, but being unable to or only passing a few drops.
- Dull pain in the pelvis.
- Unpleasant smelling urine.
- Urine that is cloudy, bloody, pink or dark.
- Back pain.
- Generally feeling unwell.
- Fever.
Symptoms that may indicate that the infection involves the kidney(s) (pyelonephritis) include:
- Fever and rigors (shivering).
- Nausea or vomiting.
- Diarrhea.
- Back pain.
Urinary tract infection prognosis
Lower urinary tract infections are seldom complicated and complete recovery is expected with a short course of antibiotics. Those patients with an uncomplicated lower urinary tract infection are at no risk of developing renal failure in later life.
Upper urinary tract infections will require admission to hospital for intravenous antibiotics followed by an extended oral course of antibiotics at home following discharge from hospital. Recovery is expected with a variable but commonly small reduction in kidney function.
Urinary tract infection causes
The urinary system’s job is to excrete wastes from the body in the form of urine. The kidneys act as filtration units to remove some of the body’s waste products from the blood, such as urea and ammonia. These are then converted to urine and passed through the ureters, into the bladder and then through the urethra to leave the body.
A urinary tract infection occurs when part of the urinary tract becomes infected, usually with bacteria (e.g., Escherichia coli) that live in the digestive system — where they usually live and do not cause a problem. The bacteria often enter the urinary tract through the urethra, for example from the anus. This can happen if bacteria in feces is transmitted to the urethra by toilet paper, such as when a woman wipes from back to front rather than from front to back. Once inside the urinary tract, these bacteria can multiply and cause an infection resulting in local irritation and inflammation.
For most people, a urinary tract infection is a one-off illness that resolves quickly and responds to treatment with antibiotics when necessary. However, for some people, urinary tract infections are a recurrent (recurring) problem.
You are considered to have recurrent urinary tract infections if you have either:
- 2 or more urinary tract infections within 6 months, or
- 3 or more urinary tract infections within 1 year.
Risk factors for urinary tract infection
Urinary tract infections are common in women, and many women experience more than one infection during their lifetimes. Risk factors specific to women for urinary tract infections include:
- Female anatomy. A woman has a shorter urethra than a man does, which shortens the distance that bacteria must travel to reach the bladder.
- Sexual activity. Sexually active women tend to have more urinary tract infections than do women who aren’t sexually active. Having a new sexual partner also increases your risk.
- Certain types of birth control. Women who use diaphragms for birth control may be at higher risk, as well as women who use spermicidal agents.
- Menopause. After menopause, a decline in circulating estrogen causes changes in the urinary tract that make you more vulnerable to infection.
Other risk factors for urinary tract infections include:
- Urinary tract abnormalities. Babies born with urinary tract abnormalities that don’t allow urine to leave the body normally or cause urine to back up in the urethra have an increased risk of urinary tract infections.
- Blockages in the urinary tract. Kidney stones or an enlarged prostate can trap urine in the bladder and increase the risk of urinary tract infections.
- A suppressed immune system. Diabetes and other diseases that impair the immune system — the body’s defense against germs — can increase the risk of urinary tract infections.
- Catheter use. People who can’t urinate on their own and use a tube (catheter) to urinate have an increased risk of urinary tract infections. This may include people who are hospitalized, people with neurological problems that make it difficult to control their ability to urinate and people who are paralyzed.
- A recent urinary procedure. Urinary surgery or an exam of your urinary tract that involves medical instruments can both increase your risk of developing a urinary tract infection.
Urinary tract infection prevention
Besides prescription antibiotic treatment, if you have repeated urinary tract infections there are some self-help measures that may help prevent further infections:
- Drink more fluids to help flush out bacteria to at least 2L/day.
- Drink cranberry juice. Although studies are not conclusive that cranberry juice prevents urinary tract infections, it is likely not harmful.
- Urinate immediately after intercourse. Also, drink a full glass of water to help flush bacteria.
- Gently wipe from front to back after urinating and after a bowel movement helps prevent bacteria in the anal region from spreading to the vagina and urethra.
- Wear cotton underwear and loose fitting pants.
- Avoid potentially irritating feminine products. Using deodorant sprays or other feminine products, such as douches and powders, in the genital area can irritate the urethra.
- Eat natural yogurt to restore normal vaginal environment
- Find an alternative method of birth control if you use spermicides or diaphragm
Cranberry products are not effective and should not be recommended for the prevention of urinary tract infections 2, 3, 4. If you want to try cranberry products ask your doctor for advice.
Urinary tract infection diagnosis
Your doctor will ask about your symptoms and perform a physical examination.
If the doctor suspects a urinary tract infection, you will be asked to provide a mid-stream urine (MSU) sample. A urine sample that is collected ‘mid-stream’ is important in order to stop bacteria present around the urethra, the vagina, the anus, the groin area and on your hands from contaminating the urine test.
The urine sample can be tested for features that suggest a possible urinary tract infection, such as white blood cells, red blood cells and nitrites.
The urine sample may also be tested at a laboratory called a urine M/C/S (microscopy, culture and sensitivity/susceptibility) to determine what sort of bacteria are present and what antibiotic will work best.
The microscopy urine test, called a microurine or urine microscopy, checks for the presence of any blood or pus. This is generally followed by a urine culture test to detect the type and number of bacteria in the urine. How sensitive the bacteria is to certain antibiotics may also be tested at this stage, and these results help your healthcare professional to decide on the most appropriate antibiotic treatment.
Additional tests aren’t generally needed. However, additional tests may be recommended if the symptoms don’t get better with treatment or you have recurrent urinary tract infections.
Additional tests may also be recommended if:
- A man gets a urinary tract infection: These are uncommon so it’s important to check if there is an underlying cause of the urinary tract infections.
- There is blood in the urine.
- There is a greater risk of developing complications: For example, if the infection occurs in a pregnant woman or a person with a weakened immune system.
Further testing may involve repeat testing of urine samples or imaging tests of the urinary tract.
- Imaging tests of your urinary tract. If you are having frequent infections that your doctor thinks may be caused by an abnormality in your urinary tract, you may have an ultrasound, a computerized tomography (CT) scan or magnetic resonance imaging (MRI). Your doctor may also use a contrast dye to highlight structures in your urinary tract.
- Ultrasonography is the preferred initial test for patients with obstruction, abscess, recurrent infection, or suspected kidney stones, because it avoids radiation exposure 18
- Helical computed tomography urography is used to view the kidneys and adjacent structures, and may be considered to further evaluate patients with possible abscess, obstruction, or suspected anomalies when ultrasonography is not diagnostic 19
- Using a scope to see inside your bladder. If you have recurrent UTIs, your doctor may perform a cystoscopy, using a long, thin tube with a lens (cystoscope) to see inside your urethra and bladder. The cystoscope is inserted in your urethra and passed through to your bladder.
- Urodynamic studies can be performed for persistent voiding symptoms with otherwise unrevealing workup 20
Urinary tract infection treatment
Urinary tract infection home remedies
Urinary tract infections can be painful and annoying, but you can help to manage the infection by:
- Drinking plenty of water to at least 2L/day to help dilute the urine and flush out the bacteria
- Avoiding drinks that can irritate the bladder: Avoid coffee, alcohol, and soft drinks containing citrus juices or caffeine until your infection has cleared. They can irritate your bladder and tend to aggravate your frequent or urgent need to urinate.
- Use a heating pad. Apply a warm, but not hot, heating pad to your abdomen to minimize bladder pressure or discomfort.
Studies 2, 3, 4 have found that drinking cranberry juice is not effective in treating urinary tract infections, but it may have an effect in preventing recurrent urinary tract infections.
If you enjoy drinking cranberry juice and feel it helps you prevent urinary tract infections, there’s little harm in it, but watch the calories. For most people, drinking cranberry juice is safe, but some people report an upset stomach or diarrhea. However, don’t drink cranberry juice if you’re taking blood-thinning medication, such as warfarin.
While you are taking antibiotics to treat a urinary tract infection, it is recommended that you drink plenty of water and make sure you completely empty your bladder each time you go to the toilet.
Depending on the kind of antibiotic treatment prescribed, your healthcare professional may recommend the use of urinary alkalylinizers which make the urine less acidic and can ease the pain and burning sensation during urination that sometimes occurs with urinary tract infections.
Any abdominal, pelvic, or back pain due to an upper urinary tract infection can usually be managed with over-the-counter (OTC) pain relief, such as paracetamol, ibuprofen or naproxen.
You can minimize your risk of developing a urinary tract infection by:
- Drinking lots of water each day
- Urinating as soon as the need arises
- Wiping the bottom from front to back to prevent bacteria from around the anus entering the urethra
- Using adequate lubrication during sex
- Urinating after having sex: this can help to flush out any bacteria that may have entered the urethra during intercourse
- Avoiding feminine hygiene products such as sprays or douches
- Talking to the doctor about other forms of contraception if using a diaphragm
- Treating constipation or diarrhea promptly: constipation can cause feces in the rectum to press on the bladder and prevent it from emptying fully, while diarrhea can make it easier for bacteria to enter the urinary tract.
Urinary tract infection antibiotics
There are several different types of antibiotics that can be used, if needed, to treat urinary tract infections. Your doctor will decide on the most appropriate antibiotic for you, depending on what infection you have (e.g., cystitis, pyelonephritis) and the type of bacteria found in your urine.
Simple urinary tract infection
Drugs commonly recommended for simple urinary tract infections include:
- Trimethoprim/sulfamethoxazole (Bactrim, Septra, others)
- Fosfomycin (Monurol)
- Nitrofurantoin (Macrodantin, Macrobid)
- Cephalexin (Keflex)
- Ceftriaxone
| Antibiotics may be prescribed for: | Active ingredient |
| Women (who are not pregnant) |
|
| Pregnant women |
|
| Men |
|
| Children | Mild UTI
Severe UTI
|
The group of antibiotic medicines known as fluoroquinolones — such as ciprofloxacin (Cipro), levofloxacin (Levaquin) and others — isn’t commonly recommended for simple urinary tract infections, as the risks of these medicines generally outweigh the benefits for treating uncomplicated urinary tract infections. In some cases, such as a complicated urinary tract infection or kidney infection, your doctor might prescribe a fluoroquinolone medicine if no other treatment options exist.
For some high-risk individuals (e.g., a person who has a urinary catheter or someone who has undergone urological surgery), a urinary tract infection may be caused by a fungus called Candida, rather than by bacteria. In this instance, a health care professional may prescribe an antifungal medicine to treat the infection, and not antibiotics.
Often, symptoms clear up within a few days of treatment. But you may need to continue antibiotics for a week or more. Take the entire course of antibiotics as prescribed.
For an uncomplicated urinary tract infection that occurs when you’re otherwise healthy, your doctor may recommend a shorter course of treatment, such as taking an antibiotic for one to three days. But whether this short course of treatment is enough to treat your infection depends on your particular symptoms and medical history.
Your doctor may also prescribe a pain medication (analgesic) that numbs your bladder and urethra to relieve burning while urinating, but pain usually is relieved soon after starting an antibiotic.
Frequent urinary tract infections
If you have frequent urinary tract infections, your doctor may make certain treatment recommendations, such as:
- Low-dose antibiotics, initially for six months but sometimes longer
- Self-diagnosis and treatment, if you stay in touch with your doctor
- A single dose of antibiotic after sexual intercourse if your infections are related to sexual activity
- Vaginal estrogen therapy if you’re postmenopausal
If you have recurrent urinary tract infections and your prescriber has ruled out any underlying disease or abnormality of the urinary tract as a cause, you may be prescribed preventive antibiotics. This is not a recommended course of action in everyone and your prescriber will need to consider your particular circumstances.
Use of other treatments such as intravaginal estrogen therapy for postmenopausal women has been examined in trials. Research has reported that intravaginal estrogen therapy (pessaries or creams) relieves urinary tract infection symptoms and reduces the number of recurrent infections.
There is some evidence that taking methamine hippurate tablets may be helpful in preventing recurrent urinary tract infections in some people. This medicine works by changing the chemical composition of your urine, making it ’less attractive’ to bacteria, and can be used as an alternative for preventing recurrent urinary tract infections in people who can’t take antibiotics. Because it isn’t an antibiotic, it may be a helpful tool for preventing antibiotic resistance. However, methenamine hippurate is not as effective as antibiotics for preventing recurrent urinary tract infection, and more research is required to show the true protective benefit of this medicine.
Severe urinary tract infection
For a severe urinary tract infection, you may need treatment with intravenous antibiotics in a hospital.
- Foxman, B. (2002). Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. American Journal of Medicine; 113(Suppl. 1A): 5S-13S.[↩][↩]
- Jepson RG, Craig JC. Cranberries for preventing urinary tract infections. Cochrane Database Syst Rev. 2008;(1):CD001321.[↩][↩][↩]
- Wang CH, Fang CC, Chen NC, et al. Cranberry-containing products for prevention of urinary tract infections in susceptible populations: a systematic review and meta-analysis of randomized controlled trials. Arch Intern Med. 2012;172;(13):988–996.[↩][↩][↩]
- Epp A, Larochelle A, Lovatsis D, et al.; Society of Obstetricians and Gynaecologists of Canada. Recurrent urinary tract infection [published correction appears in J Obstet Gynaecol Can. 2011;33(1):12]. J Obstet Gynaecol Can. 2010;32(11):1082–1090.[↩][↩][↩]
- Juthani-Mehta M, Van Ness PH, Bianco L, et al. Effect of Cranberry Capsules on Bacteriuria Plus Pyuria among Older Women in Nursing Homes: A Randomized Clinical Trial. JAMA. 2016;316(18):1879-1887. doi:10.1001/jama.2016.16141. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5300771/[↩]
- Wang CH, Fang CC, Chen NC, et al. Cranberry-containing products for prevention of urinary tract infections in susceptible populations: a systematic review and meta-analysis of randomized controlled trials. Archives of Internal Medicine. 2012;172(13):988-996. https://www.ncbi.nlm.nih.gov/pubmed/22777630[↩]
- Jepson RG, Williams G, Craig JC. Cranberries for preventing urinary tract infections. Cochrane Database of Systematic Reviews. 2012;(10):CD001321[↩]
- Dysuria: Evaluation and Differential Diagnosis in Adults. Am Fam Physician. 2015 Nov 1;92(9):778-788. https://www.aafp.org/afp/2015/1101/p778.html[↩]
- Arnold, J.J., Hehn, L.E., Klein, D.A. (2016). Common questions about recurrent urinary tract infections in women. (link is external) American Family Physician; 93(7): 560-569.[↩]
- Najar, M.S., Saldanha, C.L., Banday, K.A. (2009). Approach to urinary tract infections. Indian Journal of Nephrology; 19(4): 129-139.[↩]
- Bergamin, P.A., Kiosoglous, A.J. (2017). Non-surgical management of recurrent urinary tract infections in women. Translational Andrology and Urology; 6(Suppl 2): S142-S152.[↩]
- What are the symptoms of a bladder infection? https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-infection-uti-in-adults/symptoms-causes[↩]
- Karmon, A., Sheiner, E. (2008). The relationship between urinary tract infection during pregnancy and preeclampsia: causal, confounded or spurious? Archives of Gynecology and Obstetrics; 277(6): 479-481.[↩]
- Arnold, J.J., Hehn, L.E., Klein, D.A. (2016). Common questions about recurrent urinary tract infections in women. American Family Physician; 93(7): 560-569.[↩]
- Dason, S., Dason, J.T., Kapoor, A. (2011). Guidelines for the diagnosis and management of recurrent urinary tract infection in women. Canadian Urological Association Journal; 5(5): 316-322.[↩]
- Diagnosis and Treatment of Urinary Tract Infections in Children. Am Fam Physician. 2011 Feb 15;83(4):409-415. https://www.aafp.org/afp/2011/0215/p409.html[↩][↩][↩][↩]
- UTI Guideline Team, Cincinnati Children’s Hospital Medical Center. Evidence-based care guideline for medical management of first urinary tract infection in children 12 years of age or less. https://www.cincinnatichildrens.org/[↩]
- Smith-Bindman R, Aubin C, Bailitz J, et al. Ultrasonography versus computed tomography for suspected nephrolithiasis. N Engl J Med. 2014; 371(12):1100–1110.[↩]
- Gupta K, Trautner B. In the clinic. Urinary tract infection. Ann Intern Med. 2012;156(5):ITC3-1–ITC3-15.[↩]
- Hanno PM, Erickson D, Moldwin R, Faraday MM. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol. 2015;193(5):1545–1553.[↩]