Contents
What is empty sella syndrome
Empty sella syndrome is a condition in which the sella turcica (also called the pituitary fossa, a bony structure at the base of the brain that protects the pituitary gland) appears to be largely empty of pituitary tissues and filled by cerebrospinal fluid 1. The pituitary gland is a small gland located just underneath the brain. It is attached to the bottom of the brain by the pituitary stalk. The pituitary sits in a saddle-like compartment in the skull called the sella turcica. In Latin, it means Turkish seat. When the pituitary gland shrinks or becomes flattened, it cannot be seen on an magnetic resonance imaging (MRI) scan. This makes the area of the pituitary gland look like an “empty sella.” But the sella is not actually empty. It is often filled with cerebrospinal fluid (CSF). CSF is fluid that surrounds the brain and spinal cord. With empty sella syndrome, CSF has leaked into the sella turcica, putting pressure on the pituitary gland. This causes the gland to shrink or flatten.
Empty sella syndrome is often discovered during radiological imaging tests for pituitary disorders. Empty sella syndrome occurs in up to 25 percent of the population. An individual with empty sella syndrome may have no symptoms or may have symptoms resulting from partial or complete loss of pituitary function (including headaches, low sex drive, and impotence).
There are two types of empty sella syndrome:
- Primary empty sella syndrome: primary empty sella syndrome occurs when a structural defect above the pituitary gland increases pressure in the sella turcica and causes the gland to flatten. Most patients with primary empty sella syndrome are female and are affected by obesity, hypertension, headaches, and/or impaired vision 2.
- Secondary empty sella syndrome: secondary empty sella syndrome occurs when the pituitary gland is damaged due to injury, a tumor, surgery or radiation therapy 3. People with secondary empty sella syndrome may have symptoms of decreased pituitary function such as absence of menstruation, infertility, fatigue, and intolerance to stress and infection.
Primary empty sella syndrome happens when a small anatomical defect above the pituitary gland allows spinal fluid to partially or completely fill the sella turcica. This causes the gland to flatten out along the interior walls of the sella turcica cavity. Individuals with primary empty sella syndrome may have high levels of the hormone prolactin, which can interfere with the normal function of the testicles and ovaries. Primary empty sella syndrome is most common in adults and women, and is often associated with obesity and high blood pressure. In some instances the pituitary gland may be smaller than usual; this may be due to a condition called pseudotumor cerebri (which means “false brain tumor” brought on by high pressure within the skull). In rare instances this high fluid pressure can be associated with drainage of spinal fluid through the nose. Secondary empty sella syndrome is the result of the pituitary gland regressing within the cavity after an injury, surgery, or radiation therapy. Individuals with secondary empty sella syndrome can sometimes have symptoms that reflect the loss of pituitary functions, such as the ceasing of menstrual periods, infertility, fatigue, and intolerance to stress and infection. In children, empty sella syndrome may be associated with early onset of puberty, growth hormone deficiency, pituitary tumors, or pituitary gland dysfunction. Magnetic resonance imaging (MRI) scans are useful in evaluating empty sella syndrome and for identifying underlying disorders that may be the cause of high fluid pressure.
The estimated prevalence of primary empty sella syndrome i.e., empty sella without any discernible cause, is not precisely known; estimates range from 6% to 20% based on unselective autopsy studies 4. Between 20% and 50% of empty sella patients have endocrinologic dysfunction 5 and hypopituitarism is one of the most common symptoms. Recurrent hyponatremia may be a presenting feature of empty sella resulting from hypopituitarism and may cause various psychiatric symptoms such as anxiety, depression, mania, and even psychosis 1.
Empty sella syndrome is not a life-threatening illness 3. In most cases, especially in people with primary empty sella syndrome, there are no symptoms and it does not affect life expectancy. Empty sella syndrome is often found incidentally on an X-ray when people are being evaluated for other reasons. Therefore, many people with empty sella syndrome are probably never diagnosed. Some researchers have estimated that less than 1% of affected people ever develop symptoms of the condition 6. It remains unclear whether, and to what extent, asymptomatic adult patients with an incidentally discovered empty sella should undergo diagnostic testing for hormonal disturbances 7.
People with normal pituitary function usually do not need any treatment. Some people (particularly those with secondary empty sella syndrome) may need hormone replacement therapy. In a few cases, surgery may be needed to repair the sella turcica. Individuals with primary empty sella syndrome who have high levels of prolactin may be given bromocriptine. In some cases, particularly when spinal fluid drainage is observed, surgery may be needed.
If a person has empty sella syndrome that is associated with an underlying condition, the long-term outlook (prognosis) may depend on that of the specific condition present.
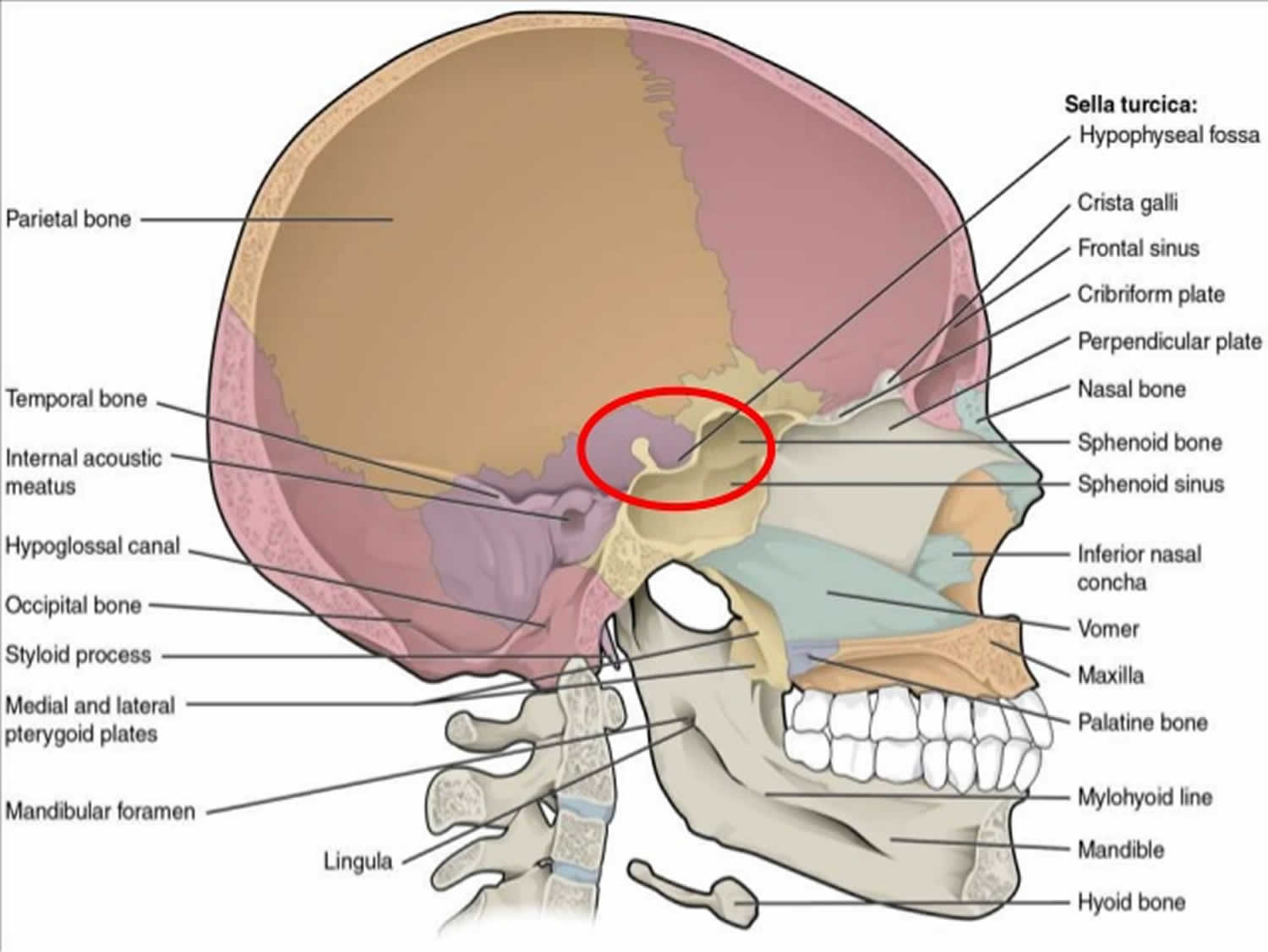
Figure 1. Sella turcica (normally the pituitary gland sits inside the sella turcica)
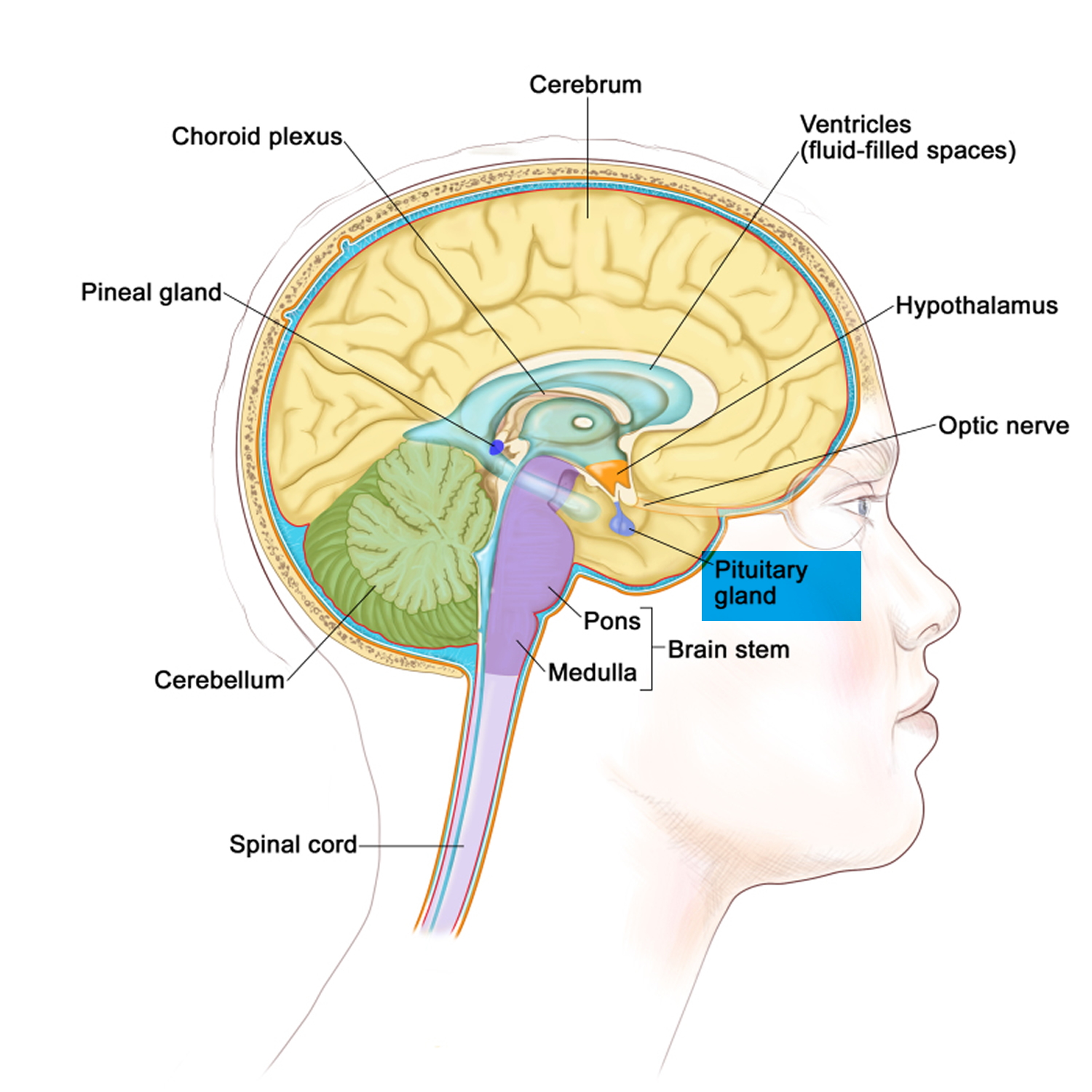
Figure 2. The pituitary gland location
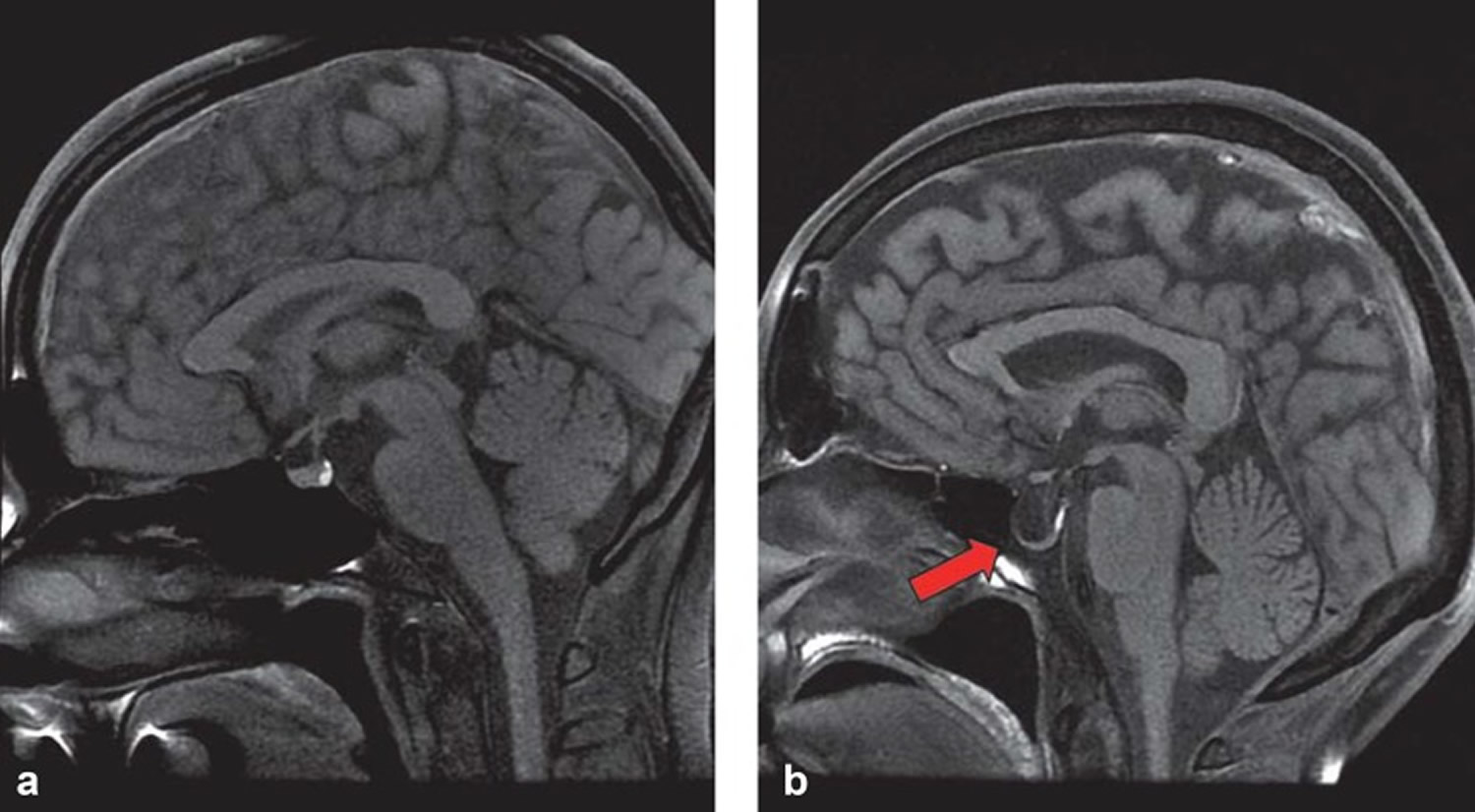
Footnote: Cerebral MRI scan of normal sella turcica with (a) regular pituitary gland and (b) empty sella.
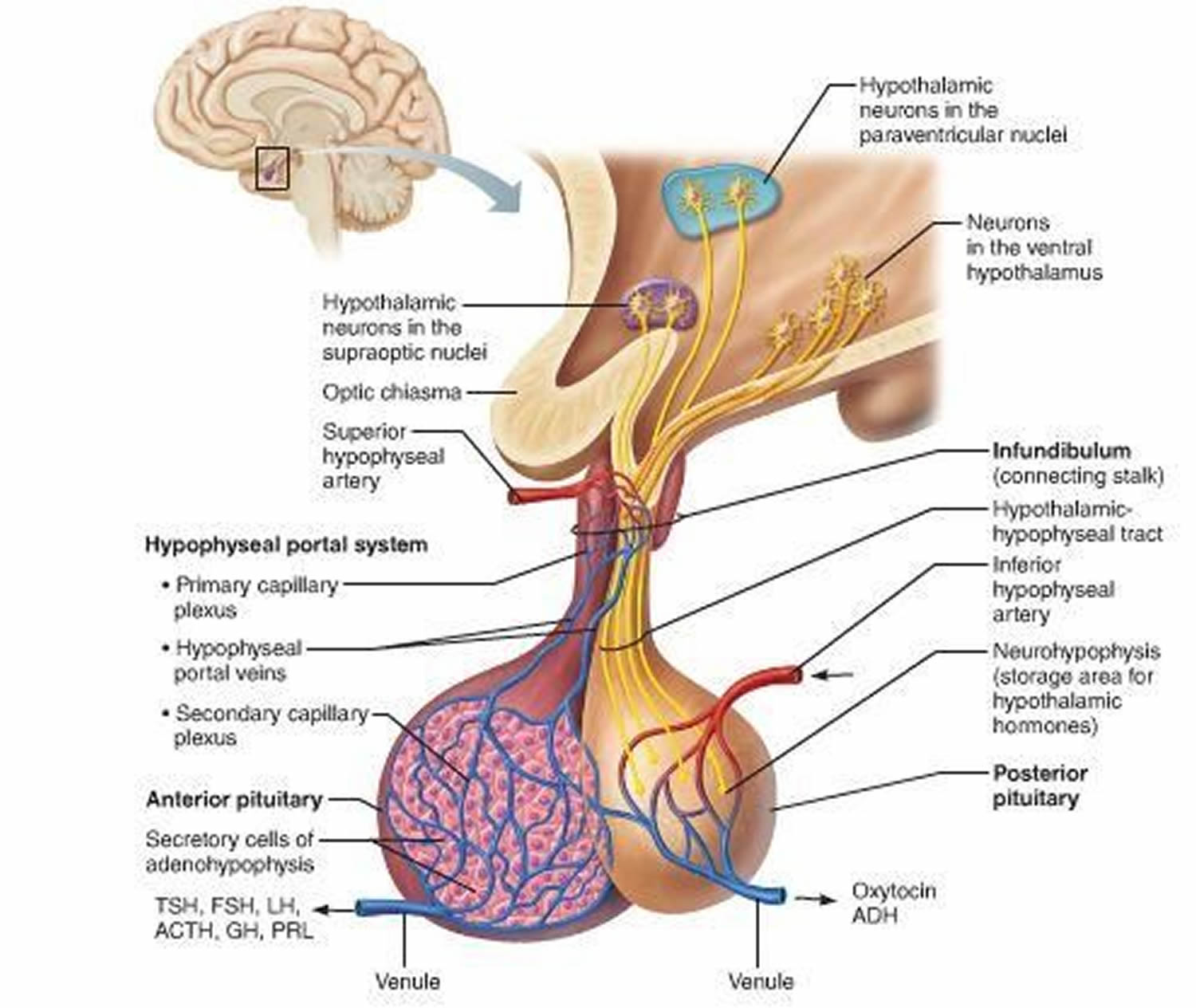
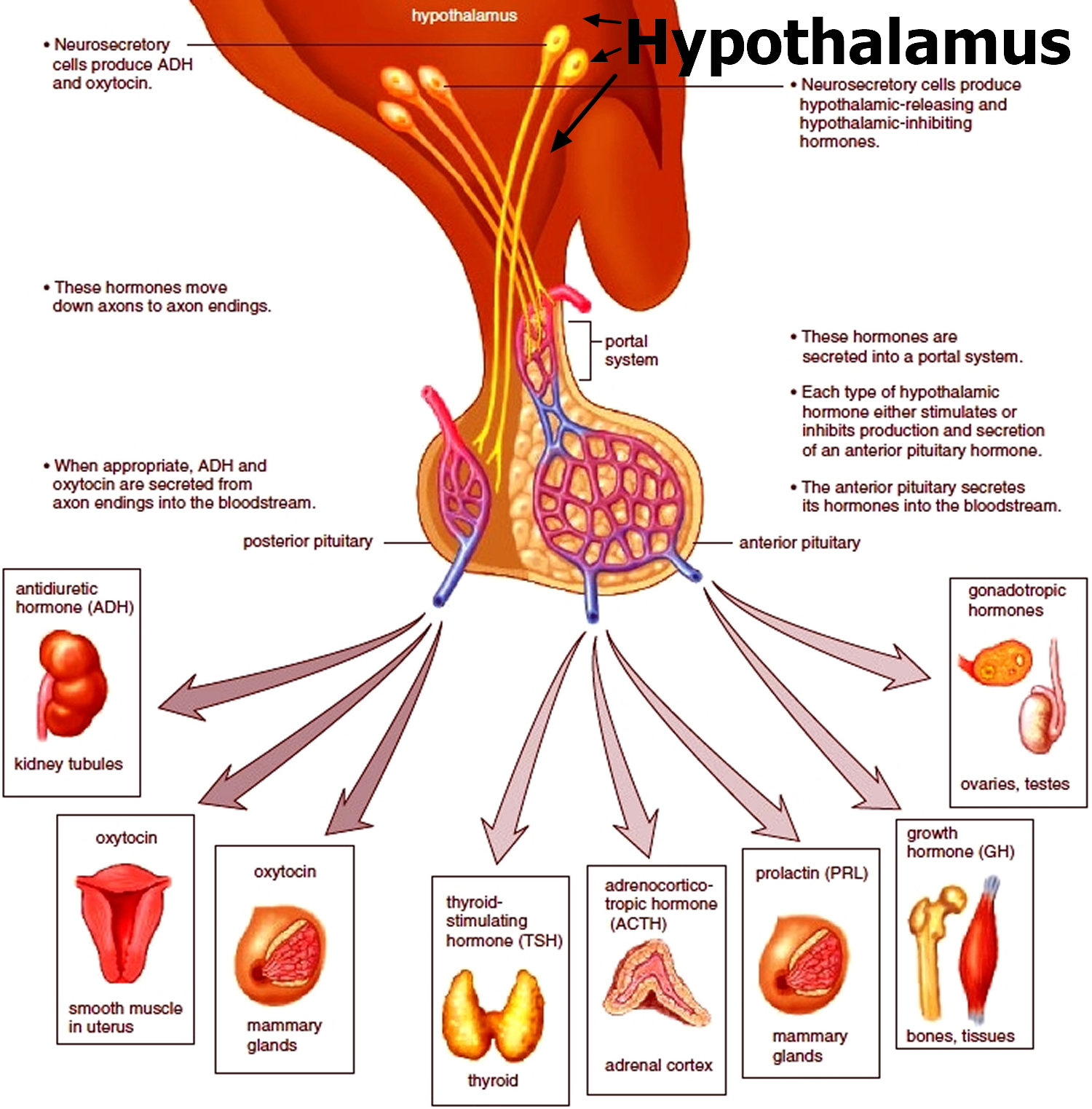
[Source 8 ]Figure 4. Pituitary gland function
Figure 5. The hypothalamus and pituitary gland (anterior and posterior) endocrine pathways and target organs
Empty sella syndrome causes
The exact, underlying cause of primary empty sella syndrome is unknown (idiopathic). Increased intracranial pressure can lead to herniation of the subarachnoid space, which can in turn lead to compression of the pituitary gland 8. This pathomechanism has been observed in cerebral tumors or idiopathic intracranial hypertension, for example. That said, the pituitary gland may be atrophied subsequent to an earlier injury. Pituitary gland necrosis can occur, among others, in a setting of pituitary adenoma, postpartum (Sheehan’s syndrome), after craniocerebral trauma, or after radiotherapy. Whenever the empty sella turcica is a consequence of another disorder, the term “secondary empty sella syndrome” is used.
Primary empty sella syndrome, the causes of the pituitary gland atrophy with a simultaneous increase in the CSF volume filling the sella turcica is not clear. Congenital anomalies are being discussed as a possible mechanism. Researchers believe that a defect in the diaphragma sellae that is present at birth (congenital defect) plays a role in the development of primary empty sella syndrome. The diaphragma sellae is a fold of dura mater (the outermost layer of the membranes that line the brain and spinal cord). The diaphragma sellae covers the sphenoid bone where the sella turcica and the pituitary are located. In some affected individuals a tear in the diaphragma sellae allows the underlying membranes to push through (herniate), which allows cerebrospinal fluid to leak out and accumulate in the sella turcica. The pressure exerted by the fluid can flatten or enlarge the sella turcica. Consequently, the pituitary becomes compressed and flattened as well. In some individuals with primary empty sella syndrome the diaphragma sellae is absent at birth. The exact role that defects in the diaphragma sella play is the development of primary empty sella syndrome is unknown. Whether it causes primary empty sella syndrome directly, occurs as part of a larger disease process or is only a predisposing factor to the development of the disorder is unresolved.
Primary empty sella syndrome occurs when one of the layers (arachnoid) covering the outside of the brain bulges down into the sella and presses on the pituitary.
Secondary empty sella syndrome is caused by a variety of different conditions including injury or trauma to the head, treated pituitary tumors, infection, radiation therapy, surgery on the pituitary region, or rare disorders such as Sheehan syndrome.
Possible causes of secondary empty sella syndrome:
- Increase in intracranial pressure, for example, because of a cerebral tumor or hydrocephalus
- Idiopathic intracranial hypertension
- Surgery for pituitary tumor
- Sheehan‘s syndrome (postpartum pituitary gland necrosis)
- Sequela of craniocerebral trauma
- Sequela of cerebral radiotherapy
Empty sella syndrome may be seen in a condition called pseudotumor cerebri (idiopathic intracranial hypertension), which mainly affects young, obese women and causes the CSF to be under higher pressure.
The pituitary gland makes several hormones that control other glands in the body, including the:
- Adrenal glands
- Ovaries
- Testicles
- Thyroid
A problem with the pituitary gland can lead to problems with any of the above glands and abnormal hormone levels of these glands.
Risk factors for empty sella syndrome
Primary empty sella syndrome affects approximately 4 times more women than men. Most cases occur in middle-aged women who are obese and have high blood pressure (hypertension). Across all studies, a higher prevalence of hormonal disturbances was seen in women. In addition to female sex, a higher body mass index (BMI) and hypertension were named as risk factors. Lupi et al. 9 investigated the association between overweight (BMI 25 to <30kg/m²) and obesity (BMI = 30 kg/m²) and pituitary insufficiency in primary empty sella syndrome. Hypopituitarism had been diagnosed in 24 of 39 (62%) overweight patients and in 15 of 33 (45%) obese patients, but in only 2 of 13 (15%) patients with a normal weight. In the study reported by Colao et al. 10, patients with primary empty sella syndrome had a higher cardiovascular risk profile, independently of their BMI, especially a higher Framingham score and poorer glucose and lipid profiles than the control cohort.
Empty sella syndrome symptoms
The symptoms of empty sella syndrome may vary from one person to another and depends on the underlying cause. In most cases, especially in individuals with primary empty sella syndrome, there are no associated symptoms (asymptomatic). Often, empty sella syndrome is discovered incidentally on CT or MRI examination when individuals are being evaluated for other reasons.
If there are symptoms, they may include any of the following:
- Erection problems
- Headaches
- Irregular or absent menstruation
- Decreased or no desire for sex (low libido)
- Fatigue, low energy
- Nipple discharge
The most common symptom potentially associated with empty sella syndrome is chronic headaches. However, it is unknown whether headaches develop because of empty sella syndrome or are simply a coincidental finding. Many individuals with empty sella syndrome have high blood pressure (hypertension), which can itself cause headaches if severe.
In rare cases, individuals with empty sella syndrome have developed increased pressure within the skull (benign intracranial pressure), leakage of cerebrospinal fluid from the nose (cerebrospinal rhinnorhea), swelling of the optic disc due to increased cranial pressure (papilledema), and abnormalities affecting vision such as loss of clarity of vision (visual acuity).
In the empty sella syndrome, the function of the pituitary gland is usually not affected. It is often not well seen on imaging, but is otherwise perfectly functional. The pituitary is a small gland located near the base of the skull that stores several critical hormones and releases them into the bloodstream as needed by the body. These hormones regulate many different bodily functions. Although a rare occurrence, some abnormal or decreased pituitary function can occur (hypopituitarism) in the setting of empty sella. A specific finding in some individuals with empty sella, including children, has been isolated growth hormone deficiency.
Individuals with secondary empty sella syndrome are more likely to develop abnormalities affecting vision and decreased function of the pituitary because the underlying cause of their empty sella (e.g.treated pituitary tumor or trauma) result in these other associated problems.
Empty sella syndrome possible complications
Complications of primary empty sella syndrome include a slightly higher than normal level of prolactin. This is a hormone made by the pituitary gland. Prolactin stimulates breast development and milk production in women.
Complications of secondary empty sella syndrome are related to the cause of pituitary gland disease or to the effects of too little pituitary hormone.
Empty sella syndrome diagnosis
Primary empty sella syndrome is most often discovered during an MRI or CT scan of the head and brain. Pituitary function is usually normal.
Your health care provider may order tests to make sure the pituitary gland is working normally.
Sometimes, tests for high pressure in the brain will be done, such as:
- Examination of the retina by an ophthalmologist
- Lumbar puncture (spinal tap)
According to some experts opinion 8, for pragmatic reasons, a basic diagnostic evaluation should be undertaken even in asymptomatic patients. This screening should comprise several measurements: morning cortisol concentrations, free thyroxine (free T4), estradiol in women (who do not have a regular cycle) and testosterone in men, insulin-like growth factor-1 (IFG-1) and prolactin. This approach is consistent with the general recommendations for conducting pituitary tests 11 and seems to have the best cost-benefit effect. If abnormalities are found, the following measurements should be taken additionally: thyrotropin releasing hormone (TSH) for the thyrotropic axis, and follicle stimulating hormone (FSH) and luteinizing hormone (LH) for the gonadotropic axis. For a detailed assessment of the somatotropic axis, a stimulation test is required (for example, the insulin-induced hypoglycemia test or growth hormone releasing hormone [GHRH]-L-arginine test). A stimulation test is also recommended for the corticotropic axis—for example, the insulin-induced hypoglycemia test or the adrenocorticotropic hormone [ACTH] test, although, strictly speaking, the latter tests only adrenal function. These recommendations are supported by a recently published review article 12, which refers to incidental and symptomatic primary empty sella syndrome; they are also confirmed by further review article 13. In the basic diagnostic evaluation, potential factors that influence hormone concentrations have to be considered. For example, the use of oral contraceptives can lower the IGF-1 value below the sex and age specific normal value. With regard to rational weighing-up of costs and benefits, it should be mentioned that isolated growth hormone deficiency has to be confirmed by using at least two stimulation tests before health insurers will cover hormone substitution treatment at this point in time. Furthermore, in a setting of isolated growth hormone deficiency, substitution treatment with growth hormone does not have license approval. The reason is that the phase III (registration) trials to date did not study isolated deficiency states. In principle, growth hormone therapy can be assumed to be beneficial even in isolated growth hormone deficiency 14, even though at the moment this constitutes off-label treatment.
Empty sella syndrome treatment
Most individuals with empty sella syndrome do not have any symptoms and do not require treatment. When symptoms do occur, treatment is directed toward the specific symptoms that are apparent in each individual. If the pituitary is affected, then replacement therapy for specific hormones should be administered as needed. Surgery may be necessary when cerebrospinal fluid leaks from the nose (CSF rhinnorhea).
For primary empty sella syndrome:
- There is no treatment if pituitary function is normal.
- Medicines may be prescribed to treat any abnormal hormone levels.
For secondary empty sella syndrome, treatment involves replacing the hormones that are missing.
In some cases, surgery is needed to repair the sella turcica.
Empty sella syndrome prognosis
Primary empty sella syndrome does not cause health problems, and it does not affect life expectancy.
- A Case Report of Late Onset Mania Caused by Hyponatremia in a Patient With Empty Sella Syndrome. Medicine (Baltimore). 2016 Feb; 95(6): e2629. doi: 10.1097/MD.0000000000002629 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4753879/[↩][↩]
- Primary empty sella (PES): a review of 175 cases. Guitelman M, Garcia Basavilbaso N, Vitale M, Chervin A, Katz D, Miragaya K, Herrera J, Cornalo D, Servidio M, Boero L, Manavela M, Danilowicz K, Alfieri A, Stalldecker G, Glerean M, Fainstein Day P, Ballarino C, Mallea Gil MS, Rogozinski A. Pituitary. 2013 Jun; 16(2):270-4.[↩]
- Empty Sella Syndrome Information Page. https://www.ninds.nih.gov/Disorders/All-Disorders/Empty-Sella-Syndrome-Information-Page[↩][↩]
- Primary empty sella with isolated ACTH deficiency and microprolactinoma. Agrawal NK, Jain P, Garg S. Gynecol Endocrinol. 2012 Jul; 28(7):568-9.[↩]
- Primary “empty sella” in adults: endocrine findings. Del Monte P, Foppiani L, Cafferata C, Marugo A, Bernasconi D. Endocr J. 2006 Dec; 53(6):803-9.[↩]
- Empty Sella Syndrome. https://rarediseases.org/rare-diseases/empty-sella-syndrome[↩]
- Primary Empty Sella Syndrome and the Prevalence of Hormonal Dysregulation. Dtsch Arztebl Int. 2018 Feb; 115(7): 99–105. doi: 10.3238/arztebl.2018.0099 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5842341/[↩]
- Auer MK, Stieg MR, Crispin A, Sievers C, Stalla GK, Kopczak A. Primary Empty Sella Syndrome and the Prevalence of Hormonal Dysregulation. Dtsch Arztebl Int. 2018;115(7):99-105. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5842341/[↩][↩][↩]
- Pituitary autoimmunity is associated with hypopituitarism in patients with primary empty sella. Lupi I, Manetti L, Raffaelli V, Grasso L, Sardella C, Cosottini M, Iannelli A, Gasperi M, Bogazzi F, Caturegli P, Martino E. J Endocrinol Invest. 2011 Sep; 34(8):e240-4.[↩]
- Role of pituitary dysfunction on cardiovascular risk in primary empty sella patients. Colao A, Cotta OR, Ferone D, Torre ML, Ferraù F, Di Somma C, Boschetti M, Teti C, Savanelli MC, Alibrandi A, Trimarchi F, Cannavò S. Clin Endocrinol (Oxf). 2013 Aug; 79(2):211-6.[↩]
- Petersenn S, Quabbe HJ, Schöfl C, Stalla GK, von Werder K, Buchfelder M. The rational use of pituitary stimulation tests. Dtsch Arztebl Int. 2010;107:437–443[↩]
- Chiloiro S, Giampietro A, Bianchi A, et al. Diagnosis of endocrine disease: primary empty sella: a comprehensive review. Eur J Endocrinol. 2017;177:R275–R285.[↩]
- Guitelman M, Garcia Basavilbaso N, Vitale M, et al. Primary empty sella (PES): a review of 175 cases. Pituitary. 2013;16:270–274.[↩]
- Gardner CJ, Mattsson AF, Daousi C, Korbonits M, Koltowska-Haggstrom M, Cuthbertson DJ. GH deficiency after traumatic brain injury: improvement in quality of life with GH therapy: analysis of the KIMS database. Eur J Endocrinol. 2015;172:371–381[↩]