Contents
What is subcutaneous injection
Subcutaneous injection is an injection into the fat layer between the skin and the underlying muscle. Subcutaneous injections are used to:
- get a rapid and systemic effect of the drug;
- give small amounts and certain kinds of medicine that cannot be administered orally due to poor absorption in gastrointestinal tract;
- when the drug is toxic and irritating to the gastrointestinal mucosa.
The onset of action for subcutaneous injections is usually slower than for intramuscular (IM) injections (heparin is absorbed as quickly when given via subcutaneous injection).
See a medical professional if:
- A fever, sneezing, or coughing develops after the injection is given.
- There is a lump, swelling, or bruising where the injection was given that does not go away.
- You have questions about how to give an injection.
Seek immediate medical care if:
- A rash or itching develops after the injection is given.
- Shortness of breath develops after the injection is given.
- The mouth, lips, or face swells after the injection is given.
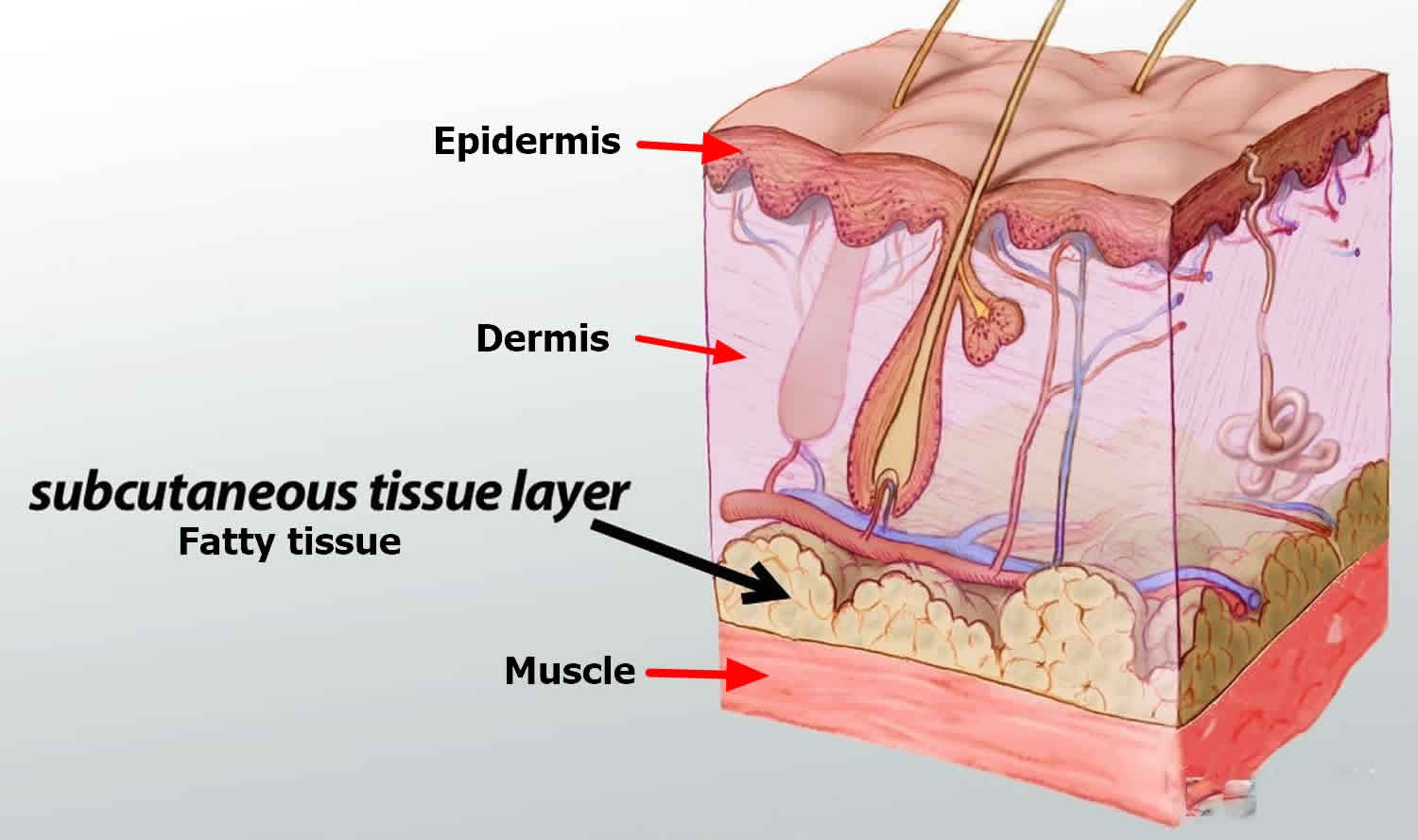
Figure 1. Subcutaneous tissue anatomy
Subcutaneous injection needle
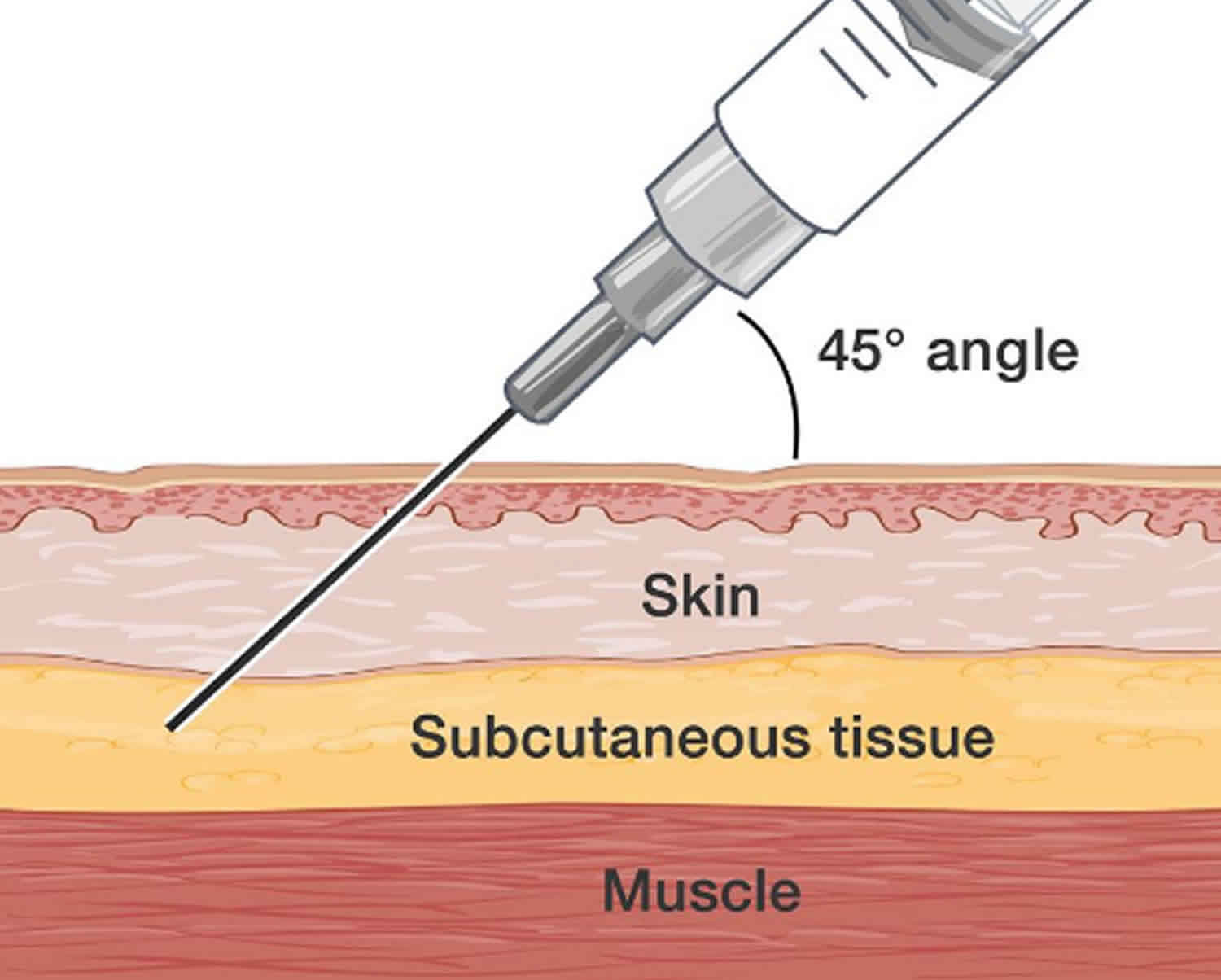
The amount of fatty tissue determines the needle length and angle of insertion. Use what is needed to deliver the medication into the subcutaneous tissue.
In general, a 25 gauge, 5/8 inch needle is inserted at a 45-90 degree angle. The needle-length should be 1/2 of the depth of the skinfold. A rule of thumb is that if the skinfold depth is 2 inches, inject using a 90 degree angle; if the depth is 1 inch, inject using a 45 degree angle.
There are 3 parts to a syringe: the needle, the barrel, and the plunger. The needle goes into your skin. The barrel holds the medicine and has markings on it like a ruler. The markings are for milliliters (mL). The plunger is used to get medicine into and out of the syringe.
- Insulin syringe: This holds a maximum of 1 mL of medicine. The syringe has markings from 10 to 100. The marking at 100 is the same as 1 mL. The marking at 50 is the same as ½ mL.
- Tuberculin syringe: This syringe holds up to 1 mL of medicine. It has a needle that is slightly longer than an insulin syringe. The syringe is marked every 0.1 mL.
- Medication: Vials of liquid medication can be single-use or multiuse. Vials can also be filled with a powder to which liquid needs to be added.
- Syringes: The needles are short, at 5/8 inches long. The thickness of the needle is usually 25 or 28 gauge. There may be other options for doses more than 1 mL or for children or people with visual impairments.
- Auto-injector pen: Some medications are available in a “pen” with a short single-use needle screwed onto the end of a pen-shaped, multiuse vial. The amount of medication needed is then dialed in at the end. Emergency medications like epinephrine can also come in this form.
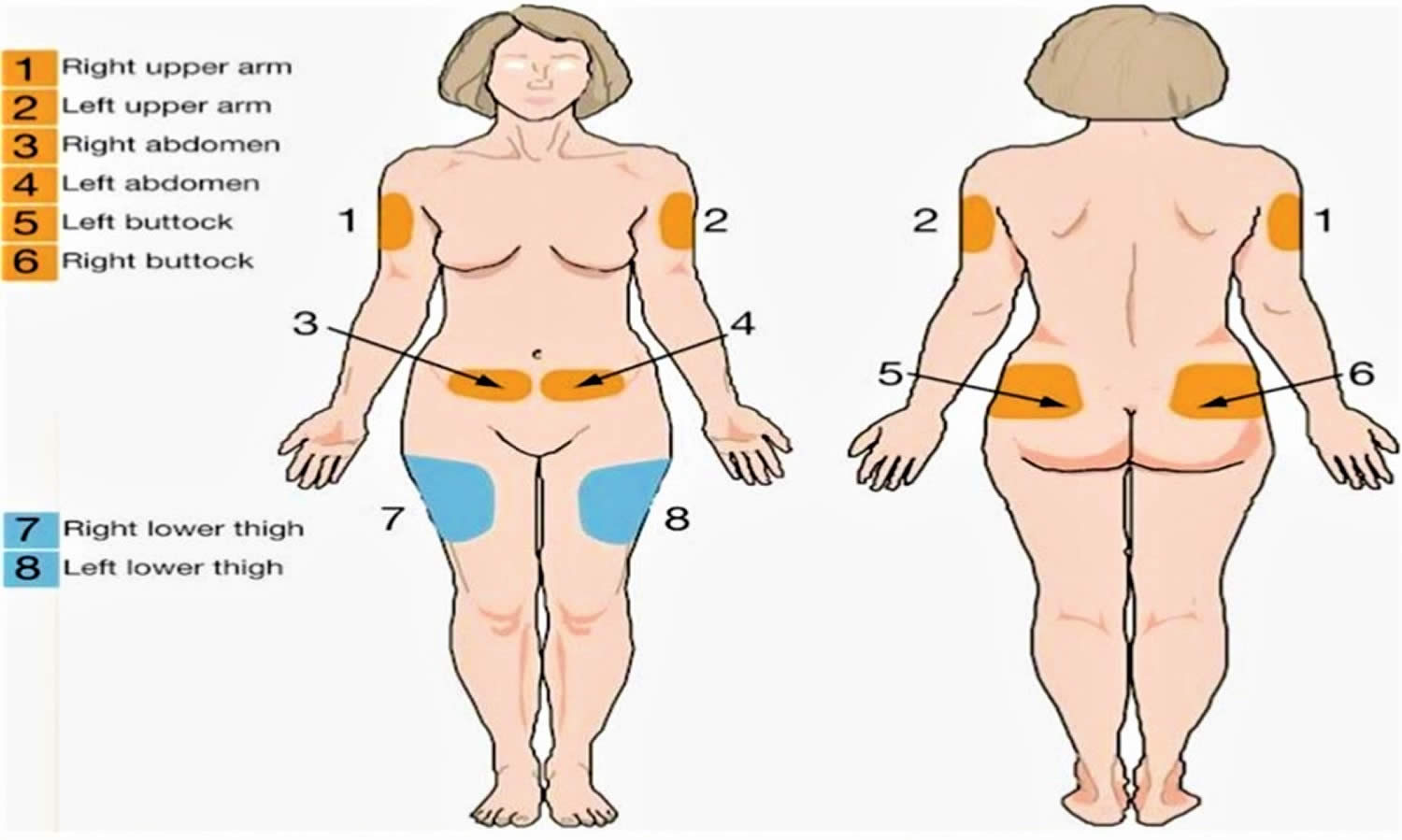
Where to give subcutaneous injection?
The following are sites where you can give a subcutaneous injection:
- The outer area of the upper arm.
- The abdomen from the rib margin to the iliac crest avoiding a 2 inch circle around the navel, this has the fastest rate of absorption among the sites.
- The front of the thigh, midway to the outer side, 4 inches below the top of the thigh to 4 inches above the knee, this has a slower rate of of absorption.
- The upper back.
- Lower back in the upper area of the buttock, just behind the hip bone, this has the slowest rate of absorption among sites.
Birth to 12 months
For newborns and infants, inject medicine into the middle of the thigh where there is a lot of fatty tissue. This is called the anterolateral thigh muscle. Use the front, outer top of the thigh. Do not use the inner thigh or back of the thigh.
12 months and older
For children older than 12 months, medicines can be injected into two sites.
Middle of the thigh. Inject medicine into the middle of the thigh where there is a lot of fatty tissue. This is called the anterolateral thigh muscle. Use the front, outer top of the thigh. Do not use the inner thigh or back of the thigh.
Figure 2. Subcutaneous injection sites
Figure 3. Subcutaneous injection site for infants
Abdomen
The abdomen from the rib margin to the iliac crest avoiding a 2 inch circle around the navel, this has the fastest rate of absorption among the sites.
Uncover your abdomen. You may give an injection within the following area: below the waist to just above the hip bone and from the side to about 2 inches from the belly button. Avoid the belly button.
Front of the thigh
Uncover the entire leg. Find the area halfway between the knee and hip and slightly to the side. The front of the thigh, midway to the outer side, 4 inches below the top of the thigh to 4 inches above the knee, this has a slower rate of of absorption.
Gently grasp the area to make sure you can pinch 1 to 2 inches of skin.
Lower back
Uncover the back from the waist to the top of the buttocks. Imagine a line that runs across the back just above the crack between the buttocks. An injection may be given below the waist and above this line. Give the injection halfway between the spine and the side.
Upper Arm
Uncover the arm to the shoulder. Have the person getting the injection stand with his hand on his hip. Stand next to and a little behind the person. Find the area halfway between the elbow and shoulder. Gently grasp the skin at the back of the arm between your thumb and first 2 fingers. You should be able to grasp 1 to 2 inches of skin.
How do I choose the best place for a subcutaneous injection?
- Keep track of where the injections are given: Make a list of the sites you can use. Write down the date, time, and the site each time you give an injection.
- Change sites for the injections: It is important to use a different site each time you give an injection. This prevents scars and skin changes. The sites where injections are given should be at least 1 inch away from each other. Ask your healthcare provider if you need to inject the medicine in a certain site.
How to give subcutaneous injection
Subcutaneous injections can be given straight in at a 90 degree angle or at a 45 degree angle. Give the injection at a 90 degree angle if you can grasp 2 inches of skin between your thumb and first finger. If you can grasp only 1 inch of skin, give the injection at a 45 degree angle.
- Open the alcohol wipe: Wipe the area where you plan to give the injection. Let the area dry. Do not touch this area until you give the injection.
- Prepare the needle: Hold the syringe with your writing hand and pull the cover off with your other hand. Place the syringe between your thumb and first finger. Let the barrel of the syringe rest on your second finger.
- Pinch up on the fatty (subcutaneous) tissue to prevent injection into muscle: With your other hand, grasp the skin.
- Insert the needle into the skin: Hold the syringe barrel tightly and use your wrist to inject the needle into the skin. Once the needle is all the way in, push the plunger down to inject the medicine.
- Aspirate if recommended by pulling back gently on the plunger to determine whether needle is in a blood vessel. If blood appears, withdraws needle and discard.
- Do not aspirate for heparin/insulin.
- Give the drug rapidly to reduce pain. Firmly push the plunger down as far as it will go.
- Pull out the needle: Remove the needle at the same angle you put it in. Gently wipe the area with the gauze pad.
- Apply firm pressure with a cotton ball to the injection site for 30 seconds following each injection to reduce the chance of bruising. Do not rub the area as it may irritate the skin.
- Put the needle and syringe in a thick, plastic bottle or sharps container with a lid. Do not try to put the cap back on the needle. This is for safety. When the container is full, bring it to your local pharmacy. They can safely dispose of it for you. Do not put it in your regular garbage.
It is important to dispose of the needles and syringes correctly. Do not throw needles into the trash. You may receive a hard plastic container made especially for used syringes and needles. You can also use a soda bottle or other plastic bottle with a screw lid. Make sure that both the syringe and needle fit into the container easily and cannot break through the sides. Ask your healthcare provider or a pharmacist what your state or local requirements are for getting rid of used syringes and needles.
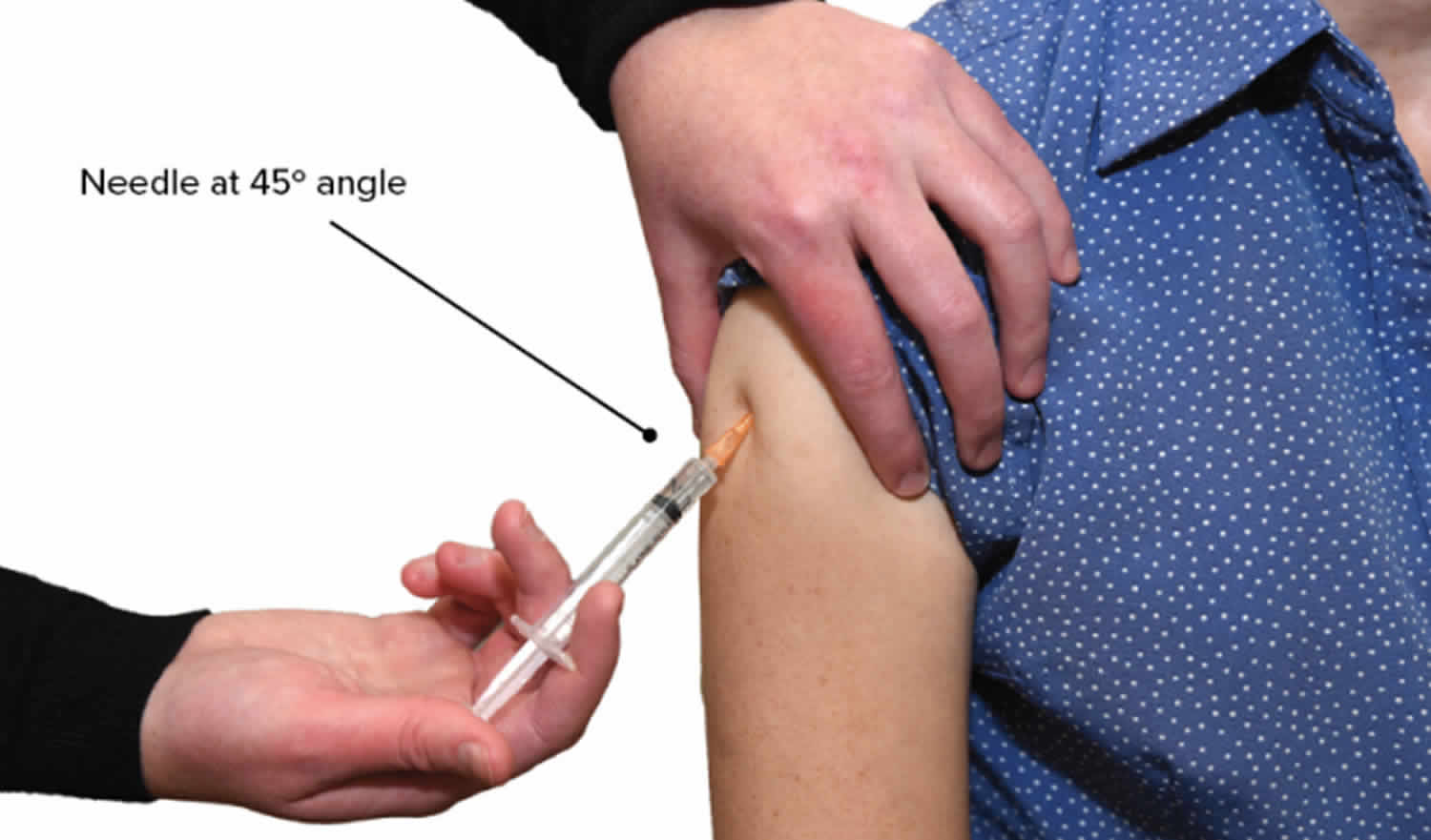
Figure 4. Subcutaneous injection technique
Footnote: An adult is having a subcutaneous injection in the deltoid. The person giving the injection is holding the person’s shoulder with their left hand, and inserting the needle upwards into the deltoid, at a 45 degree angle to the arm.
Subcutaneous insulin injection
To perform your insulin injection:
- Wherever possible, wash your hands with soap and water before injecting.
- Put a new needle onto your pen.
- Remove the caps of the pen needle.
- Hold the pen upright and perform an ‘air shot’. This requires dialling up at least 2 units and pressing the plunger to expel a test shot of insulin. This helps to clear any bubbles out of the needle. If you do not get a steady stream, repeat the air shot until you do get a steady stream of insulin coming out.
- Dial up your dose.
- Pick a soft fatty area to inject. Tops of thighs, belly, bum and triceps (triceps; the top and back of the upper arm, are not always recommended for children or thinner people).
- Some people may need to raise a fold of fatty flesh slightly between your thumb and fingers. If you are unsure about whether you need to do this, ask your healthcare team.
- Put the needle in and keep the pen steady.
- Push the plunger relatively slowly to inject the dose.
- After the dose has been injected, hold the needle in for a good 10 seconds to help insulin get delivered and prevent any of the dose escaping out.
- Ensure that the used needle bin is deposited into a sharps bin.
How to avoid pain when injecting insulin
Most injections are not painful. The chance of pain is greatly minimized by using a new needle.
Some tips to help avoid or minimize pain when injecting, include:
- Always use a new needle.
- Use a needle that is the right length. Your health team can advise you on whether you’re using the right needle length.
- Use insulin and a needle which is at room temperature.
- Push the needle in quickly when injecting.
- Try not to wiggle the needle as you’re injecting or withdrawing the needle.
Injections and bruising
You may notice a little blood leaks out after injecting.
This is not to worry about, it just means the needle has gone through a small blood vessel.
If this happens, you may notice a raised area of your skin from the blood underneath but this should ease down over the next few hours and you’ll be left with a bit of a bruise for a few days.
Rotate your injection sites to avoid ‘lumpy’ skin
If you tend to inject in the same places you may find that your flesh becomes less flexible than usual. This is called lumpy skin and means the insulin won’t be absorbed as well.
Avoid having a ‘favorite part’ of that area to inject into as this greatly increases the risk of lumpy skin. If this is the case, try injecting into surrounding areas, picking a new spot each time.
Each of the main four areas (abdomen, buttocks, outer thighs and upper arms) should give a give a good area of flesh to inject into. Using different areas of the body to inject into is insulin injection site rotation.
However, you may find you have a ‘favorite part’ of that area to inject into. If this is the case, try injecting into surrounding areas, picking a new spot each time.
One way to pick a non-lumpy area is to feel or squeeze the skin before injecting insulin. If it doesn’t feel as supple as it could be, pick a different spot to inject into.
Subcutaneous injection medications
The medications given via subcutaneous injection are isotonic, nonirritating, and water-soluble; examples are epinephrine, insulin, heparin. Medications administered by subcutaneous injection include drugs that can be given in small volumes (usually less than 1 mL but up to 2 mL is safe). Insulin, heparin and some hormones are commonly administered as subcutaneous injections.
Other drugs that need to be given very quickly can also be administered via subcutaneous injection. Epinephrine comes in an automated injector form, called an EpiPen, that’s used to quickly treat severe allergic reactions. While it’s intended to be given intramuscularly, epinephrine will also work if given subcutaneously.
Some pain medications like morphine and hydromorphone (Dilaudid) can be given this way as well. Drugs that prevent nausea and vomiting like metoclopramide (Reglan) or dexamethasone (DexPak) can also be given via subcutaneous injection.
Some vaccines and allergy shots are administered as a subcutaneous injection. Many other vaccines are administered as an intramuscular injection — into muscle tissue rather than under the skin.
What is subcutaneous injection maximum volume?
The dosage that can be given subcutaneous injection is usually less than 1 ml, but up to 2 ml is safe.
Subcutaneous injection complications
You may get an infection, have the needle break in your skin, or hit a nerve. You may have scarring, lumps, or dimpling of the skin from a subcutaneous injection.
What does it mean if there is bruising at the injection site?
This can happen from time to time. It is not harmful. It usually means the needle has nicked a tiny blood vessel. To reduce the chance of bruising, apply gentle pressure to the site with a dry piece of cotton or a clean finger after injecting. Also, be careful not to pinch the skin too tightly or insert the needle too slowly. If you have too much bruising, consult your health-care team.
What would happen if an air bubble was accidentally injected into subcutaneous tissue?
It is not harmful to inject an air bubble under the skin. However, if you are injecting air rather than medicine, you may not be getting the full dose, which may mean you are not being properly treated.