Contents
What is balanoposthitis
Balanoposthitis is defined as inflammation of the head of the penis (glans penis) and the foreskin 1. Balanoposthitis is a common condition affecting 11% of male genitourinary clinic attendees in one study and it can be a recurrent or persistent condition. Balanoposthitis occurs only in uncircumcised males 2. There is a wide variety of causes and predisposing factors; balanitis is more common amongst uncircumcised men and boys possibly as a result of poorer hygiene and aeration or because of irritation by smegma 3.
Balanoposthitis can occur at any age. Balanoposthitis affects approximately 1 in every 25 boys and 1 in 30 uncircumcised males during their life 4. Boys under 4 years of age and uncircumcised men are the highest risk group. Balanoposthitis is more likely to occur if there is phimosis, a condition where a tight foreskin can’t retract back over the penis. When boys reach approximately the age of 5 years, the foreskin becomes easy to retract, and the risk of balanoposthitis falls. Data from meta-analyses showed that circumcised males have a 68% lower prevalence of balanoposthitis than uncircumcised males and that individuals with balanoposthitis have a 3.8-fold increase in the risk of penile cancer 5. Although data shows no direct causation, an association exists between nonspecific balanoposthitis and the uncircumcised penis. The data suggest that circumcision prevents or protects against common infective penile dermatoses.
Infectious causes of balanoposthitis include certain fungi like yeast and certain bacteria or viruses (including those that cause sexually transmitted infections (STIs) such as gonorrhea) 6. Balanoposthitis is not a sexually transmitted disease 6. The actual disease is not transferable from one person to another; however, the transfer of organisms that cause balanoposthitis is possible 6. Recurrent episodes of balanoposthitis should raise the concern for occult diabetes. Patients with recurrent episodes should undergo blood glucose screening for diabetes.
Balanoposthitis take home message:
- The most common cause of balanoposthitis is related to inadequate personal hygiene in uncircumcised males.
- Predisposing factors include poor hygiene and over washing, over-the-counter (OTC) medications, as well as non-retraction of the foreskin
- Of cases with identifiable causes, candidal infection is the most common. Various other infectious agents, dermatologic conditions, and premalignant conditions have associations with balanoposthitis.
- Retraction of the foreskin with thorough genital cleansing can be both preventive and therapeutic. The suggestion is twice-daily bathing of the affected area with a saline solution. In uncircumcised males, nonspecific balanoposthitis may respond to saline solution bathing by itself.
- Saline baths are also useful and medicated over-the-counter talcum powders are helpful in drying the area. This advice is simple, but compliance may be challenging
- HIV should be ruled out in every case not responding to therapy/having atypical presentation.
You should see your doctor if you think you’ve got balanoposthitis just to make sure it isn’t a sign of something more serious like a sexually transmitted infection (STI).
Balanoposthitis vs Balanitis
Balanitis is an inflammation of the glans penis (head of the penis); it is fairly common and affects approximately 3-11% of males during their lifetime 4. Posthitis is an inflammation of the foreskin (prepuce). Balanoposthitis involves both the glans and the foreskin and occurs in approximately 6% of uncircumcised males 4. However, in practice balanitis and balanoposthitis often occur together, and the terms are commonly used interchangeably.
Balanoposthitis causes
Balanoposthitis is common in uncircumcised men and boys as a result of poorer hygiene and aeration or because of irritation by smegma and in many cases foreskin dysfunction is a causal or contributing factor 7. Poor hygiene, a tight foreskin, and a buildup of smegma serve as a nidus for bacterial and fungal overgrowth which can lead to irritation and inflammation. Fungal infections are usually responsible, most commonly involving the yeast Candida albicans.
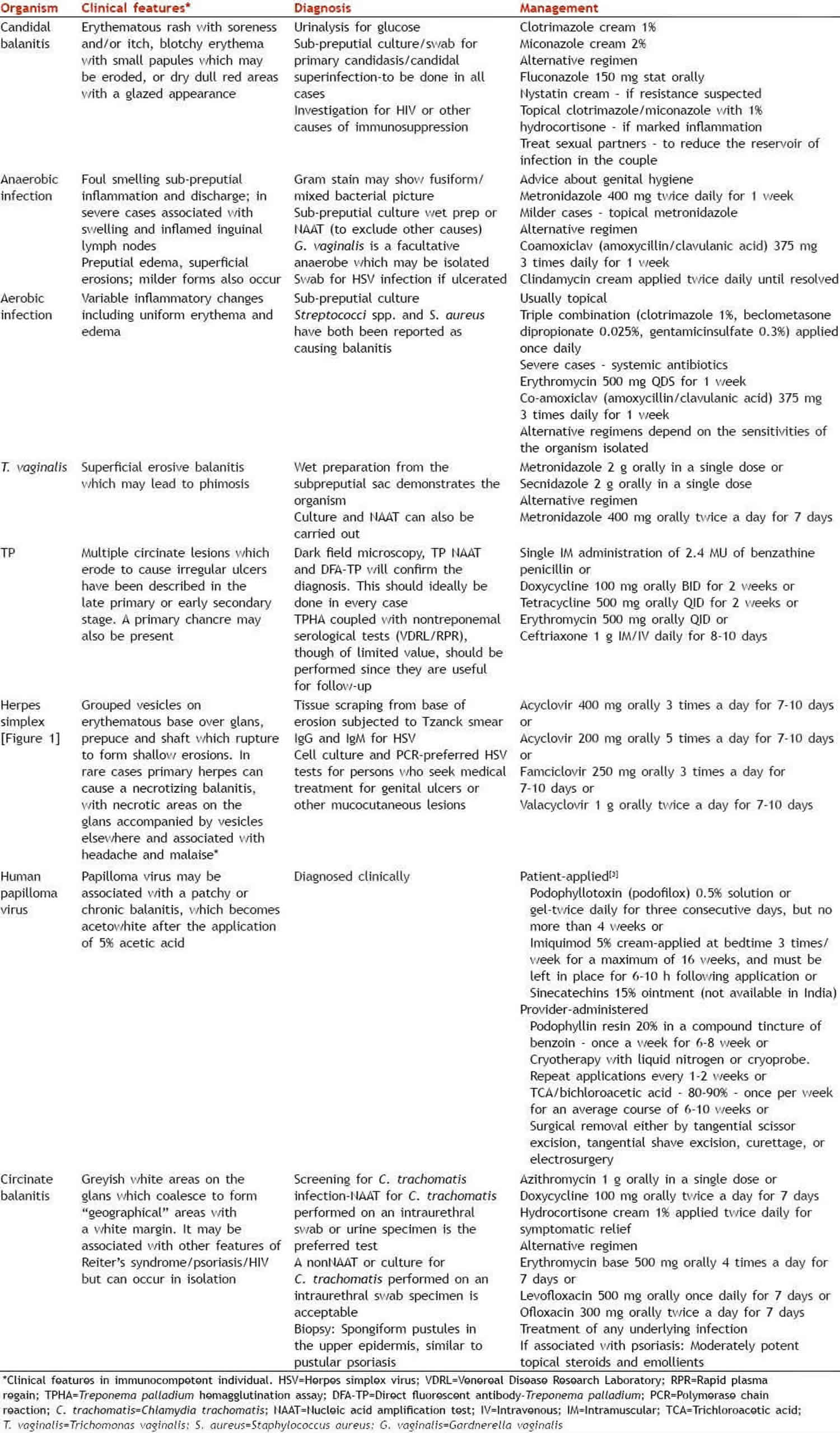
Balanoposthitis may be more severe in the presence of some underlying medical conditions 7 and has been reported as a source of fever and bacteremia in neutropenic men and candidal balanoposthitis may be especially severe in patients with diabetes mellitus 8. Descriptions of the typical appearances of infective balanoposthitis are discussed in detail (Table 2).
Sometimes a dermatologic cause (e.g., psoriasis or lichen planus) allergic reaction, or (less likely) premalignant condition may be responsible. It may warrant specialty referral to a dermatologist for a biopsy or urologist.
Localized edema may develop if someone allows balanoposthitis to progress without treatment. The combination of inflammation and edema can cause adherence of the foreskin to the glans.
Balanoposthitis can be caused by:
- poor hygiene, leading to a build-up of smegma
- irritation under the foreskin caused by pee
- soaps, shower gels, and other skin irritants
- thrush
- a bacterial infection
- a sexually transmitted infection (STI)
- skin conditions, such as eczema, psoriasis, and lichen sclerosus
- children fiddling with their foreskin
Fungal infections are the most common identifiable infectious cause, especially the yeast Candida albicans 9. This organism is normally present on the skin of the glans. Under the right conditions (an imbalance between the normally present yeast and the baseline pH) excessive growth of bacteria or yeast occurs. However, a host of other potential causes exist. These include the following infectious and noninfectious causes.
Infectious causes of balanoposthitis:
- Candidal species (most commonly associated with diabetes)
- Group B and group A beta-hemolytic streptococci
- Neisseria gonorrhea
- Chlamydia species
- Anaerobic infection
- Human papillomavirus
- Gardnerella vaginalis
- Treponema pallidum (syphilis)
- Trichomonas species
- Borrelia vincentii and Borrelia burgdorferi
Noninfectious causes of balanoposthitis:
- Poor personal hygiene (most common)
- Chemical irritants (e.g., spermicides, detergents, perfumed soaps and shower gels, fabric conditioners)
- Edematous conditions, including congestive heart failure (right-sided), cirrhosis, and nephrosis
- Drug allergies (e.g., tetracycline, sulfonamide)
- Morbid obesity
- Allergic reaction (condom latex, contraceptive jelly)
- Fixed-drug eruption (sulfa, tetracycline)
- Plasma cell infiltration (Zoon balanitis)
- Autodigestion by activated pancreatic transplant exocrine enzymes
- Trauma
- Neoplastic conditions
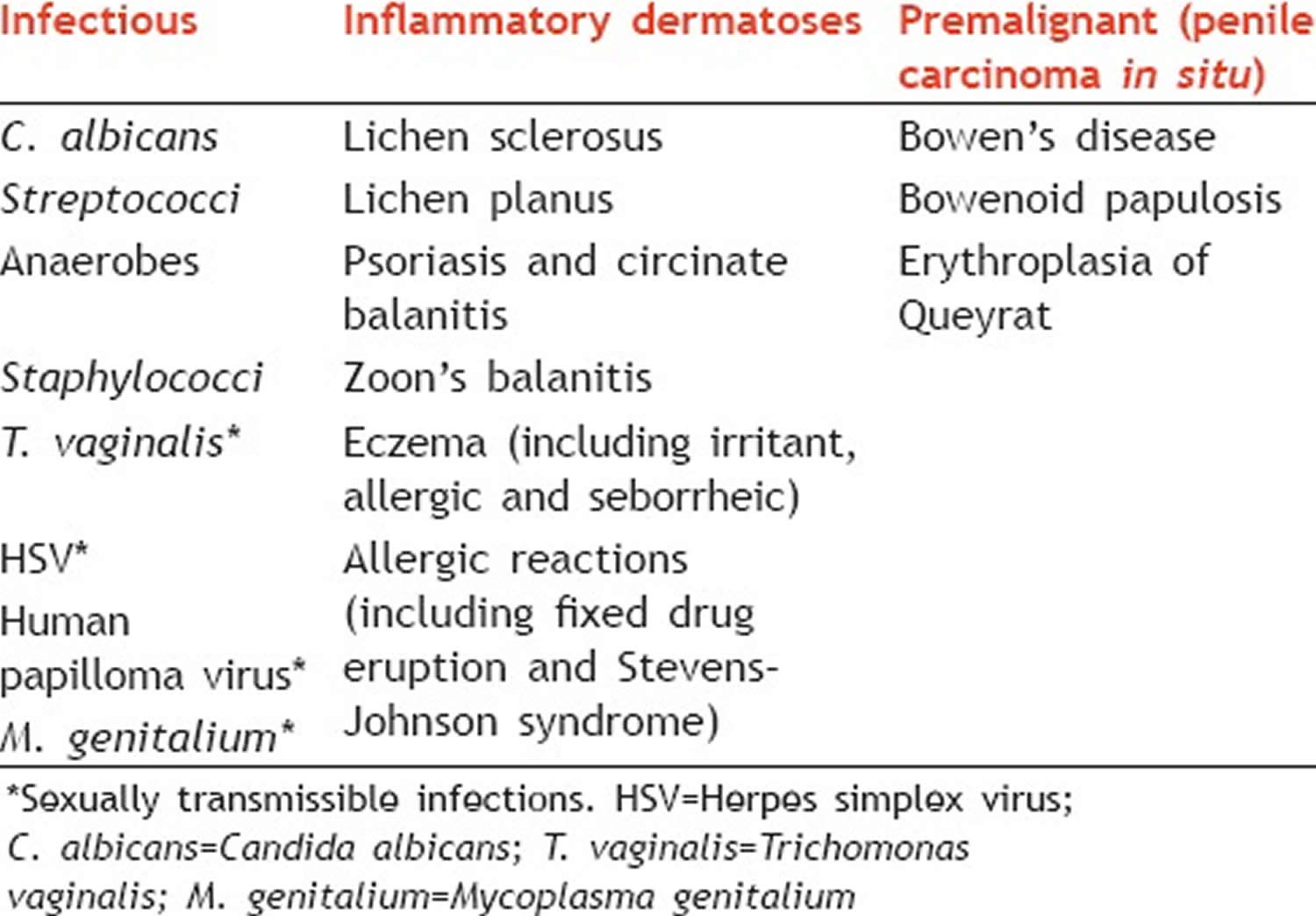
Table 1. Conditions affecting head of the penis (glans penis) and foreskin (prepuce)
[Source 7 ]Table 2. Balanoposthitis infectious causes
[Source 10 ]Risk factors for balanoposthitis
Risk factors for balanoposthitis include:
- Presence of foreskin
- Morbid obesity
- Poor hygiene
- Diabetes (particularly males with uncontrolled diabetes), probably due to Glucose on the skin, encouraging bacterial and fungal growth
- Nursing home environment
- Condom catheters
- Sensitivity to chemical irritants (i.e., soaps and lubricants)
- Edematous conditions: congestive heart failure, nephrosis
- Reactive arthritis
- Sexually transmitted diseases
Balanoposthitis prevention
You can reduce your chances of getting balanoposthitis by:
- keeping your penis clean
- avoiding harsh soaps and other skin irritants
- using soap substitutes, such as an emollient
- practising safe sex to avoid an STI (sexually transmitted infection)
- using latex-free condoms if you have a latex allergy
Young boys may not yet be able to clean under their foreskin because it may not fully pull back yet.
Don’t attempt to pull back a child’s foreskin to clean under it if it’s still fixed, as this can cause damage.
Balanoposthitis symptoms
Balanoposthitis symptoms and signs vary according to cause (see Table 2 above). Men with suspected balanoposthitis often complain of penile pain and redness.
Balanoposthitis symptoms include:
- a sore, itchy and smelly penis
- redness and swelling
- build-up of thick fluid
- pain when peeing
- redness and swelling
- discharge or oozing
- a pink or red rash, smooth or scaly, spotty or patchy
- problems pulling back the foreskin (phimosis)
Some adults may also have a tight foreskin that won’t pull back. This is a condition called phimosis.
Balanoposthitis complications
Complications associated with balanoposthitis include the development of pain, ulcerative lesions of the glans/foreskin, phimosis, paraphimosis, meatal/urethral stricture, and malignant transformation of premalignant lesions.
Phimosis is an abnormal constriction of the opening in the foreskin that precludes retraction over the glans penis, results from chronic inflammation and edema of the foreskin. Development of phimosis often complicates sexual function, voiding, and hygiene. If the patient or medical staff forcibly retract the foreskin, paraphimosis (trapping of the foreskin) can occur.
Phimosis is treatable in the emergent setting by dilation using a surgical clamp and pain medication. In the event this is not successful, a dorsal slit circumcision can be performed by a urologist to temporize the problem. Definitive treatment, under elective circumstances, is complete circumcision.
Paraphimosis refers to the trapping of the foreskin behind the glans penis and is a urologic emergency. The constricting foreskin has become located proximal to the glans penis. Under these circumstances, the constricting band will limit the venous and lymphatic outflow while allowing continued arterial inflow. Over the course of minutes to hours, the glans will increase in size and become exquisitely painful and must undergo treatment by a urologist with reduction of the paraphimosis.
Genital yeast infection (termed “candidiasis” or “thrush”) is uncommon in healthy individuals, but in immunocompromised individuals, such as those with HIV infection, in diabetic and cancer patients C. albicans can also cause bloodstream infection with serious consequences.
Balanoposthitis diagnosis
Your doctor should be able to tell if you have balanoposthitis by looking at your penis and asking a few questions. However, balanoposthitis is a descriptive term covering a variety of unrelated conditions (see Tables 1 and 2 above), the appearances of which maybe suggestive, but should never be thought to be characteristic or indicative of a particular disease or condition, and biopsy is sometimes needed to exclude premalignant disease.
If treatment doesn’t start to work within seven days, your doctor may suggest some tests to see if there’s an infection or something more serious.
If your doctor isn’t sure what’s causing your balanoposthitis, they may refer you to:
- a skin specialist called a dermatologist
- a urologist, who treats penis problems
- a sexual health clinic
Additional evaluation may be warranted based upon the history and physical findings. This might include bacterial culture (in the presence of purulent exudate), herpes simplex virus (HSV) testing (in the presence of vesicular or ulcerative lesions), syphilis testing (in the present of an ulcer), testing for scabies, and testing for trichomonas and Mycoplasma genitalium (in the presence of urethritis).
Balanoposthitis treatment
Most cases of balanoposthitis are easily treated with good hygiene and creams and ointments recommended by your doctor.
The objectives of management are:
- To minimize sexual dysfunction
- To minimize urinary dysfunction
- To exclude penile cancer
- To treat premalignant disease
- To diagnose and treat sexually transmitted disease.
*All persistent/undiagnosed genital lesions regardless of appearance must be evaluated for herpes.
Experts recommend circumcision for recurrent and intractable episodes especially in immunocompromised and diabetic patients, consult urology. Data from meta-analyses showed that circumcised males have a 68% lower prevalence of balanoposthitis than uncircumcised males and that balanoposthitis is accompanied by a 3.8-fold increase in the risk of penile cancer 11.
Female sexual partners of men with balanoposthitis should be offered testing for candida or empiric treatment to reduce the reservoir of infection in the couple 12.
Hygiene
If you have balanoposthitis, you should clean your penis daily with lukewarm water and gently dry it.
- Don’t use soap, bubble bath, shampoo or any other potential irritant.
- Dry gently under the foreskin after peeing.
- Try a soap substitute like an emollient, available from a pharmacy.
Cleaning a child’s penis
- Don’t pull back their foreskin to clean under it if it’s still fixed.
- If the child is still in nappies, change them frequently.
- Don’t use baby wipes to clean their penis.
- Creams and ointments
Depending on what’s causing the balanoposthitis, your doctor may recommend creams or ointments, such as:
- steroid cream or ointment for a simple skin irritation
- antifungal cream or tablets for a yeast infection
- antibiotics for a bacterial infection
See your doctor if the treatment doesn’t start to work within seven days. You may need another treatment or be advised to see a specialist.
Circumcision may be advised in rare cases where a child keeps getting balanoposthitis.
Sex and balanoposthitis
You can have sex during treatment if your balanoposthitis isn’t caused by an infection.
But if it’s caused by an infection, like an sexually transmitted infection (STI) or thrush (candidal balanoposthitis), there’s a risk of passing this on.
Candidal balanoposthitis
Candida infections in men are common because the fungus that causes yeast infections (candida) is normally present on skin, especially moist skin. When some contributing factor — such as having sex with a female partner who has a vaginal yeast infection — causes an overgrowth of candida, infection can result.
Balanoposthitis is more common in uncircumcised men. Signs and symptoms of balanoposthitis may include:
- Moist skin on the penis, possibly with areas of a thick, white substance collecting in skin folds
- Areas of shiny, white skin on the penis
- Redness, itching or a burning sensation on the penis
You may be more likely to develop balanoposthitis from a candida infection if you:
- Aren’t circumcised
- Use antibiotics for prolonged periods
- Have diabetes
- Have an impaired immune system, such as with HIV
- Are overweight
- Practice poor hygiene
Most male yeast infections are easily treated with over-the-counter antifungal medications.
If you and your partner both have symptoms of a yeast infection, it’s important that you both be treated to avoid reinfecting each other.
Candidal balanoposthitis treatment
Topical antifungals usually for one to three weeks is the treatment of choice for most patients with candidal balanoposthitis. Imidazoles such as clotrimazole 1% twice daily and miconazole 1% twice daily are the first line therapy choice. Nystatin cream is an alternative in patients allergic to imidazoles.
In cases of more severe inflammation, the addition of fluconazole 150 mg stat orally or the combination of a topical imidazole and a low potency topical steroids such as hydrocortisone 0.5% bid often lead to the resolution.
- Edwards S. Balanitis and balanoposthitis: a review. Genitourin Med. 1996;72(3):155-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1195642/pdf/genitmed00009-0009.pdf[↩]
- Edwards S. Balanitis and balanoposthitis: a review. Genitourin Med. 1996 Jun;72(3):155-9.[↩]
- Vohra S, Badlani G. Balanitis and balanoposthitis. Urol ClinNorthAm 1992;19:143-7.[↩]
- Wray AA, Khetarpal S. Balanitis. [Updated 2019 Jan 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537143[↩][↩][↩]
- Vohra S, Badlani G. Balanitis and balanoposthitis. Urol. Clin. North Am. 1992 Feb;19(1):143-7.[↩]
- Wray AA, Khetarpal S. Balanitis. [Updated 2019 Jan 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537143[↩][↩][↩]
- Pandya I, Shinojia M, Vadukul D, Marfatia YS. Approach to balanitis/balanoposthitis: Current guidelines. Indian J Sex Transm Dis AIDS. 2014;35(2):155-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4553848/[↩][↩][↩]
- Edwards S. balanoposthitis and balanoposthitis: a review. Genitourin Med. 1996;72(3):155-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1195642/pdf/genitmed00009-0009.pdf[↩]
- Lisboa C, Ferreira A, Resende C, Rodrigues AG. Infectious balanoposthitis: management, clinical and laboratory features. Int. J. Dermatol. 2009 Feb;48(2):121-4.[↩]
- 2013 European guideline for the management of balanoposthitis. Edwards SK, Bunker CB, Ziller F, van der Meijden WI. Int J STD AIDS. 2014 Aug; 25(9):615-26.[↩]
- Morris BJ, Krieger JN, Klausner JD. CDC’s Male Circumcision Recommendations Represent a Key Public Health Measure. Glob Health Sci Pract. 2017 Mar 24;5(1):15-27.[↩]
- Edwards SK, Bunker CB, Ziller F, van der Meijden WI. 2013 European guideline for the management of balanoposthitis. Int J STD AIDS. 2014 Aug;25(9):615-26.[↩]