Contents
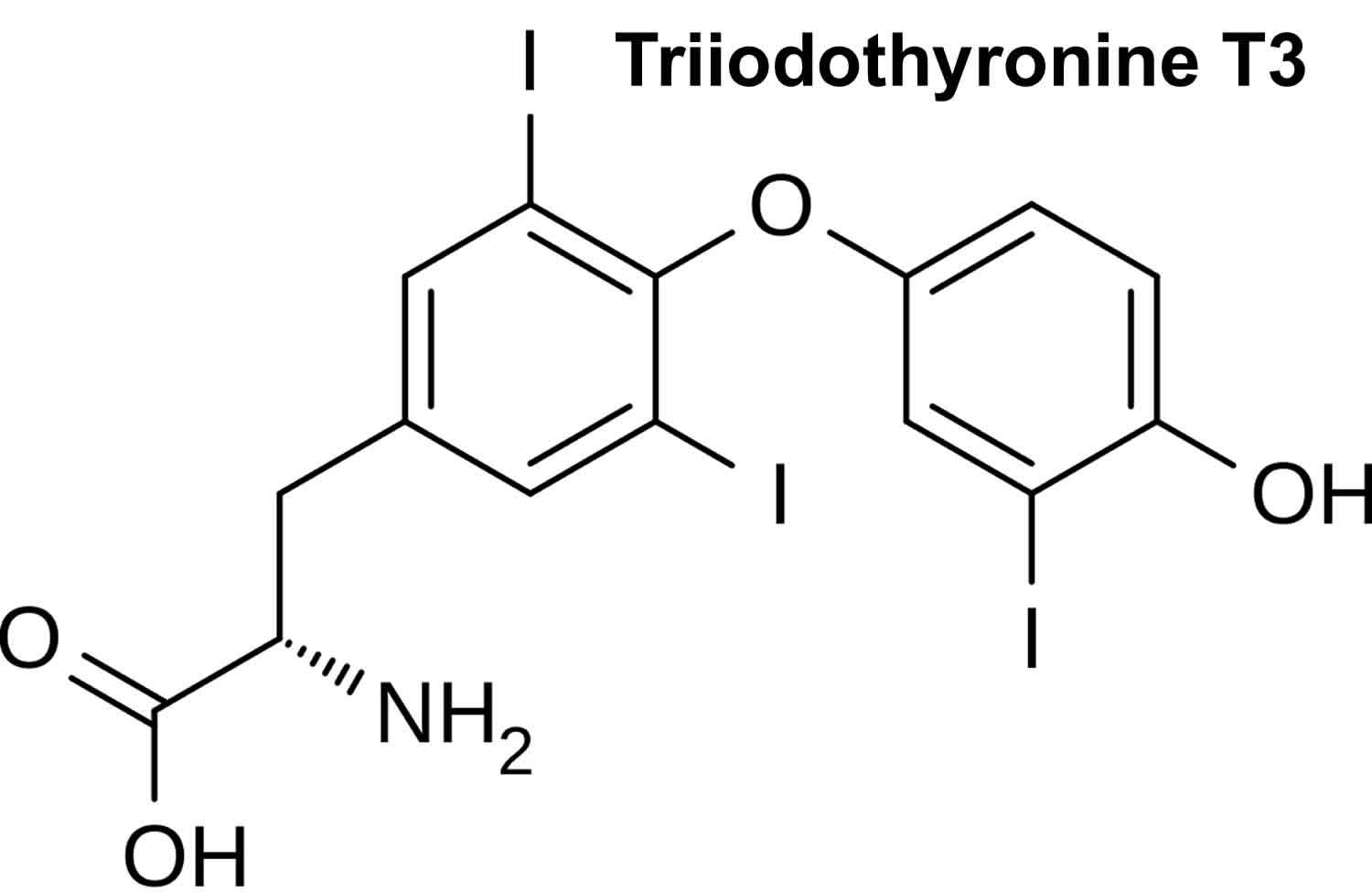
What is triiodothyronine
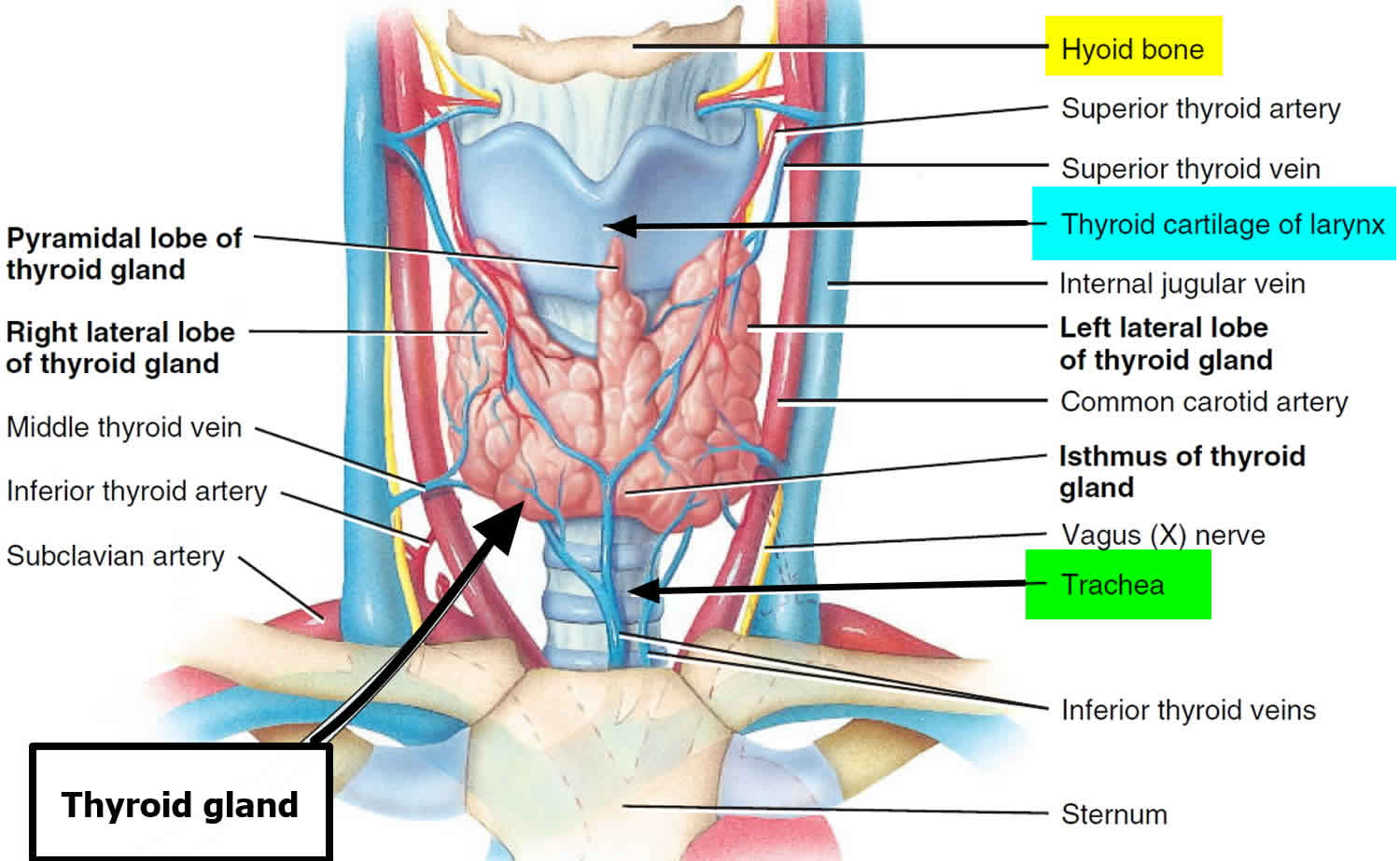
Triiodothyronine (T3) is one of two major hormones produced by the thyroid gland, a small butterfly-shaped organ that lies flat across the windpipe at the base of the throat. The other major thyroid hormone is called thyroxine (T4), which contains 4 atoms of iodine and together they help control the rate at which the body uses energy. Almost all of the triiodothyronine (T3) (and thyroxine T4) found in the blood is bound to protein. The rest is free (unbound) and is the biologically active form of the hormone. Tests can measure the amount of free triiodothyronine or the total triiodothyronine (bound plus unbound) in the blood.
The thyroid gland is responsible for the production of iodothyronines, of which there are three. The primary secretory product is inactive thyroxine (T4), which is a prohormone of triiodothyronine (T3). Thyroxine (T4) is converted to triiodothyronine (T3) peripherally by type 1 deiodinase in tissues with high blood flow, such as the liver and kidneys 1. In the brain, thyroxine (T4) is converted to active triiodothyronine (T3) by type 2 deiodinase produced by glial cells. The third iodothyronine is called reverse triiodothyronine (RT3). Reverse triiodothyronine (RT3) is inactive and forms by type 3 deiodinase activity on thyroxine (T4) 1.
Most of the hormone produced by the thyroid is thyroxine (T4). This hormone is relatively inactive, but it is converted into the much more active triiodothyronine (T3) in the liver and other tissues.
Triiodothyronine (T3) production in the thyroid gland constitutes approximately 20% of the total triiodothyronine (T3); the rest is generated by the conversion (deiodination) of thyroxine (T4) to triiodothyronine (T3) in peripheral tissues. Circulating levels of thyroxine (T4) are much greater than triiodothyronine (T3) levels, but triiodothyronine (T3) is biologically the most metabolically active hormone (3-4 times more potent than thyroxine) although its effect is briefer due to its shorter half-life compared to thyroxine (T4).
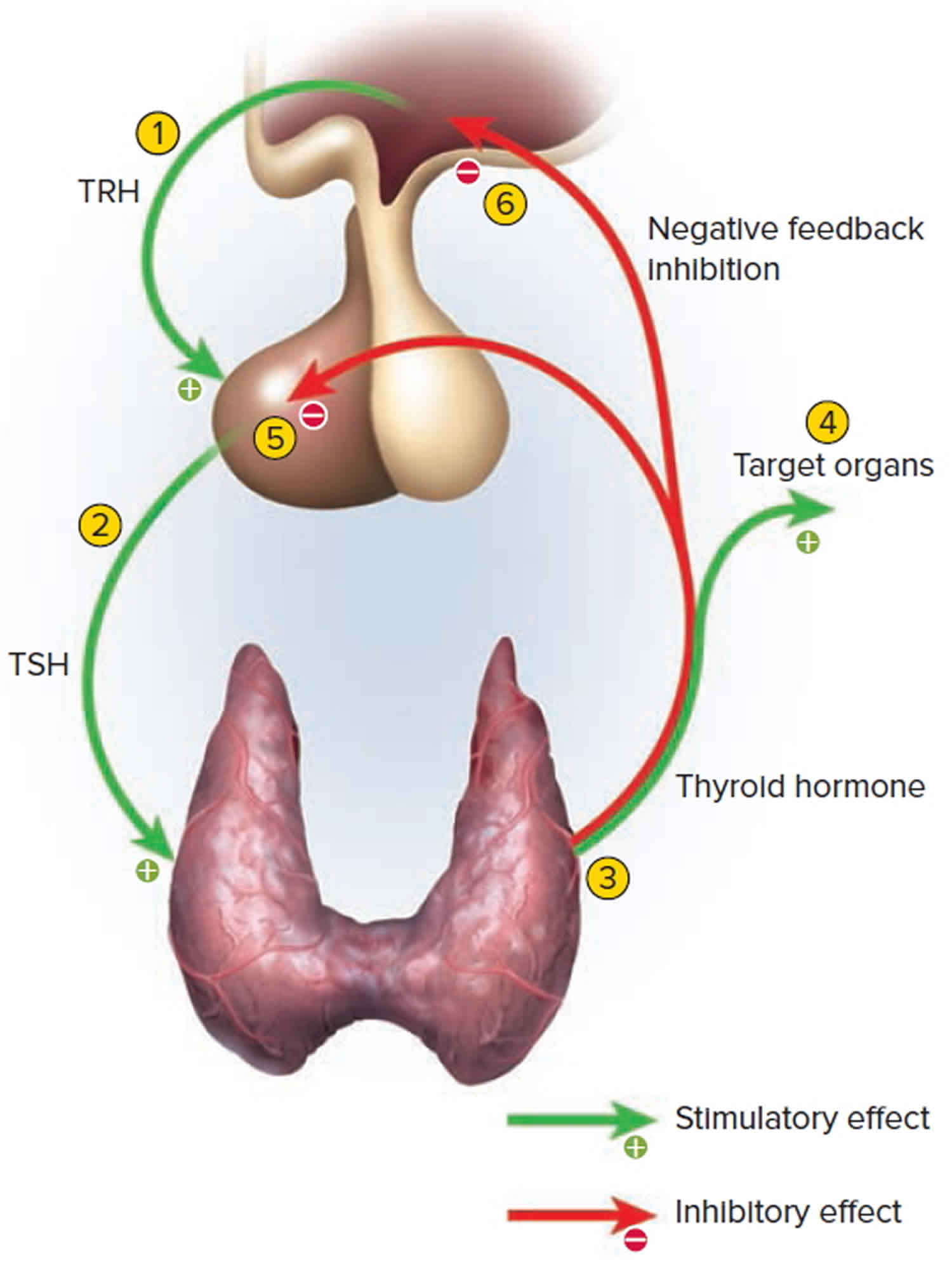
Triiodothyronine (T3) levels are regulated by the feedback system that the body uses to maintain stable amounts of thyroid hormones in the blood. Thyroxine (T4) and thyroid-stimulating hormone (TSH), along with its regulatory hormone thyrotropin releasing hormone (TRH), which comes from the hypothalamus, are also part of the feedback system.
When blood levels of thyroid hormones decline, the pituitary gland produces and releases thyroid-stimulating hormone (TSH) in response to TRH (thyrotropin releasing hormone) stimulation. thyroid-stimulating hormone then stimulates the thyroid gland to produce and/or release more thyroxine (T4) and triiodothyronine (T3).
- When thyroid hormone levels increase in the blood, the pituitary gland produces less TSH (thyroid-stimulating hormone) and the thyroid produces less thyroxine (T4) and triiodothyronine (T3).
- When all three organs (hypothalamus, pituitary and thyroid) are functioning normally, thyroid production is regulated to maintain relatively stable levels of thyroid hormones in the blood.
If the thyroid gland produces excessive amounts of thyroxine (T4) and triiodothyronine (T3), then the person affected may have symptoms associated with overactive thyroid (hyperthyroidism), such as nervousness, tremors of the hands, weight loss, insomnia, and puffiness around dry, irritated eyes and in some cases, bulging eyes. Graves disease is the most common cause of hyperthyroidism.
If the thyroid gland produces insufficient amounts of thyroxine (T4) and triiodothyronine (T3), then the person may have signs and symptoms associated with underactive thyroid (hypothyroidism) and a slowed metabolism, such as weight gain, dry skin, fatigue, and constipation. Hashimoto thyroiditis is the most common cause of hypothyroidism in the U.S.
Both hyperthyroidism and hypothyroidism can also be caused by thyroiditis, thyroid cancer, and excessive or deficient production of thyroid-stimulating hormone (TSH). The effect of these conditions on thyroid hormone production can be detected and monitored by measuring the free triiodothyronine (T3) or sometimes total triiodothyronine (T3).
Thyroid hormones regulate a number of developmental, metabolic, and neural activities throughout your body.
Thyroid hormones circulate primarily bound to carrier proteins (e.g., thyroid-binding globulin: TBG, prealbumin, and albumin); whereas only a small fraction circulates unbound (free). Only the free forms are metabolically active. While both triiodothyronine (T3) and thyroxine (T4) are bound to thyroid-binding globulin, triiodothyronine (T3) is bound less firmly than thyroxine (T4). Total triiodothyronine (T3) consists of both the bound and unbound fractions.
In hyperthyroidism, both thyroxine (T4) and triiodothyronine (T3) levels are usually elevated, but in a small subset of hyperthyroid patients only triiodothyronine (T3) is elevated (triiodothyronine toxicosis).
In hypothyroidism thyroxine (T4) and triiodothyronine (T3) levels are decreased. Triiodothyronine (T3) levels are frequently low in sick or hospitalized euthyroid (normal thyroid) patients.
What is reverse triiodothyronine (T3)?
Reverse triiodothyronine (RT3 or REVT3) is a biologically inactive form of triiodothyronine (T3). Normally, when the liver converts thyroxine (T4) to triiodothyronine (T3), it also produces a certain percentage of reverse triiodothyronine (RT3). When the body is under stress, such as during a serious illness, it tries to prevent many tissues that depend on triiodothyronine (T3) from being metabolically active by producing more reverse triiodothyronine (RT3) than triiodothyronine (T3). This is believed to be a way of conserving energy until the stress is relieved and it causes a syndrome called non-thyroidal illness (NTI). Reverse triiodothyronine (RT3) may also be elevated in hyperthyroidism. Use of the reverse triiodothyronine (RT3) test remains controversial and it is not widely requested.
Triiodothyronine function
Thyroid hormone induces effects on practically all nucleated cells in the human body, generally increasing their function and metabolism 1.
- Cardiac output, stroke volume, and resting heart rate increase through positive chronotropic and inotropic effects. Active thyroid hormone increases myocardial intracellular calcium to increase contraction force and speed. Concomitantly, vasculature in the skin, muscle, and heart dilate resulting in decreased peripheral vascular resistance while blood volume increases through activation of the renin-angiotensin-aldosterone system.
- Basal metabolic rate (BMR), heat production, and oxygen consumption elevate through thyroid hormone activation of mitochondrial uncoupling proteins. Glucose and fatty acid uptake, and oxidation also increase, which results in increased thermogenesis and necessitates increased heat dissipation. Heat intolerance in hyperthyroidism can be attributed to this increase in thermogenesis. Compensation for increased thermogenesis is also mediated by thyroid hormone through increases in blood flow, sweating, and ventilation.
- Resting respiratory rate and minute ventilation undergo stimulation by active thyroid hormone, triiodothyronine (T3), to normalize arterial oxygen concentration in compensation for increased rates of oxidation. T3 also promotes oxygen delivery to the tissues by simulating erythropoietin and hemoglobin production as well as promoting folate and cobalamin absorption through the gastrointestinal tract.
- Triiodothyronine (T3) is responsible for the development of fetal growth centers and linear bone growth, endochondral ossification, and epiphyseal bone center maturation following birth. Additionally, T3 simulates adult bone remodeling and degradation of mucopolysaccharides and fibronectin in extracellular connective tissue.
- Triiodothyronine (T3) stimulates the nervous system resulting in increased wakefulness, alertness, and responsiveness to external stimuli. Thyroid hormone also stimulates the peripheral nervous system, resulting in increased peripheral reflexes and gastrointestinal tone and motility.
- Thyroid hormone also plays a role in reproductive health and other endocrine organ function. It allows for the regulation of normal reproductive function in both men and women by regulating both the ovulatory cycle and spermatogenesis. Thyroid hormone also regulates pituitary function; growth hormone production and release are stimulated by thyroid hormone while inhibiting prolactin production and release. Additionally, renal clearance of many substances, including some medications, can be increased due to activated thyroid hormone stimulation of renal blood flow and glomerular filtration rate (GFR) 2.
Proper thyroid function is necessary for proper development of the growing brain throughout embryologic development. Both iodine deficiency and congenital hypothyroidism, due to absence, malpositioning, underdevelopment, or failure to make thyroid hormones, can cause fetal hypothyroidism. Hypothyroidism during embryologic development may result in intellectual disability, dwarfism, deafness, and muscle hypertonia.
Figure 1. Thyroid gland
Control of Thyroid Hormone Secretion
Thyrotropin-releasing hormone (TRH) from the hypothalamus and thyroid-stimulating hormone (TSH) from the anterior pituitary stimulate secretion of thyroid hormones, as shown in Figure 2:
- Low blood levels of triiodothyronine (T3) and thyroxine (T4) or low metabolic rate stimulate the hypothalamus to secrete thyrotropin-releasing hormone (TRH).
- Thyrotropin-releasing hormone (TRH) enters the hypothalamic–hypophyseal portal system and flows to the anterior pituitary, where it stimulates thyrotrophs to secrete thyroid stimulating hormone (TSH).
- Thyroid stimulating hormone (TSH) stimulates virtually all aspects of thyroid follicular cell activity, including iodide trapping, hormone synthesis and secretion, and growth of the follicular cells.
- The thyroid follicular cells release triiodothyronine (T3) and thyroxine (T4) into the blood until the metabolic rate returns to normal.
- An elevated level of triiodothyronine (T3) inhibits release of thyrotropin-releasing hormone (TRH) and TSH (negative feedback inhibition).
Conditions that increase ATP demand—a cold environment, hypoglycemia, high altitude, and pregnancy—increase the secretion of the thyroid hormones.
Figure 2. Control of Thyroid Hormone Secretion (Negative Feedback Inhibition of the Anterior Pituitary Gland by the Thyroid Gland)
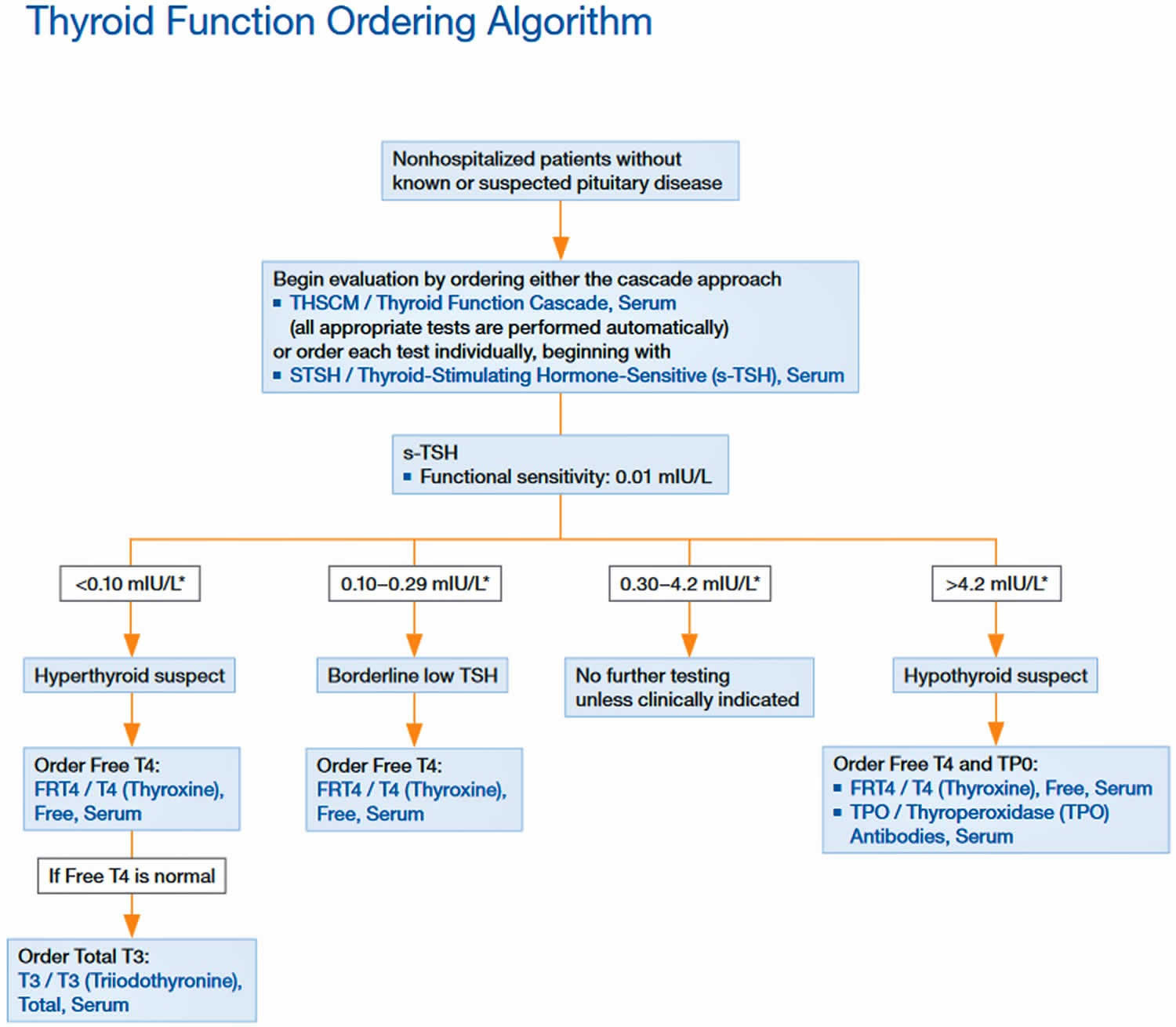
Triiodothyronine test
A free or total triiodothyronine test [free triiodothyronine (T3) or total triiodothyronine (T3)] is used to assess thyroid function. It is ordered primarily to help diagnose hyperthyroidism and may be ordered to help monitor treatment of a person with a known thyroid disorder.
Most of the thyroxine (T4) and triiodothyronine (T3) circulates in the blood bound to protein, while a small percentage is free (not bound). Blood tests can measure total T4 (unbound plus bound), free thyroxine (free T4), total triiodothyronine (T3) (bound plus unbound), or free triiodothyronine (T3).
Since most triiodothyronine (T3) is bound to protein, the total triiodothyronine (T3) can be affected by protein levels and protein binding ability, but the free triiodothyronine (T3) is not. However, some professional guidelines recommend the total triiodothyronine (T3), so either test may be used to assess thyroid function. For example, free triiodothyronine (T3) or sometimes total triiodothyronine (T3) may be ordered along with thyroid antibodies to help diagnose Graves disease, an autoimmune disorder that is the most common cause of hyperthyroidism.
The free or total triiodothyronine (T3) test is usually ordered following an abnormal TSH (thyroid-stimulating hormone), particularly if the free thyroxine (T4) test is not elevated.
Figure 3. Thyroid Function Test Diagnostic Algorithm
When is blood triiodothyronine test ordered?
A free triiodothyronine (free T3) or total triiodothyronine (total T3) test may be ordered when someone has an abnormal TSH (thyroid-stimulating hormone) test result (see Figure 1 above). Triiodothyronine (T3) test may be ordered as part of the investigative workup when a person has symptoms suggesting hyperthyroidism, especially if the free thyroxine (T4) level is not elevated.
Hyperthyroidism
Hyperthyroidism is an endocrine disorder with excess thyroid hormone production. In contrast to hypothyroidism (under active thyroid), hyperthyroidism often causes heat intolerance, weight gain, anxiety, hyperreflexia, and diarrhea, as well as palpitations. Increased stimulation of basal metabolic rate, thermogenesis, resting heart rate, and cardiac output, and central and peripheral nervous systems result in the most common symptoms. However, a multitude of symptoms can present, including brittle hair, dry skin, and pretibial myxedema 3. In Graves disease, an autoimmune condition where the TSH-receptor is activated by an auto-antibody, additional pathophysiology of orbitopathy can be present. The TSH-receptor antibody also activates T cells and causes fibroblast proliferation and accumulation of glycosaminoglycans in the extraocular muscles and retroocular connective tissue leading to proptosis.
Signs and symptoms of hyperthyroidism may include:
- Increased heart rate
- Anxiety
- Weight loss
- Difficulty sleeping
- Tremors in the hands
- Weakness
- Diarrhea (sometimes)
- Light sensitivity, visual disturbances
- The eyes may be affected: puffiness around the eyes, dryness, irritation, and, in some cases, bulging of the eyes.
Free or total triiodothyronine (T3) may sometimes be ordered at intervals to monitor a known thyroid condition and to help monitor the effectiveness of treatment for hyperthyroidism.
Hypothyroidism
Hypothyroidism is an endocrine disorder with resultant under-production of thyroid hormone. Common symptoms of hypothyroidism include cold intolerance and weight gain, due to decreased basal metabolic rate and thermogenesis, depression, fatigue, decreased peripheral reflexes, and constipation, due to decreased stimulation of the central and peripheral nervous system. Many other consequences of hypothyroidism can manifest secondary to the lack of activated thyroid hormone on various tissues and organs of the body 4.
Triiodothyronine normal range
Pediatric patients triiodothyronine (T3) normal levels:
- 0-5 days of age: 73-288 ng/dL
- 6 days-2 months of age: 80-275 ng/dL
- 3-11 months of age: 86-265 ng/dL
- 1-5 years of age: 92-248 ng/dL
- 6-10 years of age: 93-231 ng/dL
- 11-19 years of age: 91-218 ng/dL
Adult (> or =20 years): 80-200 ng/dL
What does the triiodothyronine (T3) test result mean?
Total triiodothyronine (total T3) or free triiodothyronine (free T3) results are typically evaluated with other thyroid testing results (i.e., TSH and T4).
In general, high total or free triiodothyronine (T3) results may indicate an overactive thyroid gland (hyperthyroidism) and low total or free triiodothyronine (T3) results may indicate an underactive thyroid gland (hypothyroidism). The test results alone are not diagnostic but will prompt the healthcare practitioner to perform additional testing to investigate the cause of the excess or deficiency.
When used for monitoring treatment for thyroid or pituitary disorders, results of thyroid tests will inform the healthcare practitioner whether treatment is effective and/or whether an adjustment to dose is necessary. For example, in people with hyperthyroidism, free T4, free triiodothyronine (T3), and TSH are regularly checked while they are on anti-thyroid drugs to assure that the drugs are working and to decrease doses if thyroid hormone levels get too low. In people with hypothyroidism, TSH and free T4 are regularly checked to assure that the right dose of thyroid hormone is being given to make TSH normal.
It is important to note that thyroid tests are a “snapshot” of what is occurring within a dynamic system. An individual person’s total T3, free T3, total T4, free T4, and/or TSH results may vary and may be affected by:
- Increases, decreases, and changes (inherited or acquired) in the proteins that bind T4 and T3 (This is important for tests that measure total T3, but it is not likely important for free T4 and free T3 tests, which measure the thyroid hormones that are not bound to protein.)
- Pregnancy
- Liver disease
- Systemic illness
- Rarely, resistance to thyroid hormones
The following table summarizes some examples of typical test results and their potential meaning.
Table 1. Thyroid Function Test Results
| TSH | Free T4 | Total or Free T3 | Most likely diagnosis |
|---|---|---|---|
| Normal | Normal | Normal | Normal thyroid function (e.g., “euthyroid”) |
| Normal or decreased | Normal or decreased | Decreased | Normal adjustment in thyroid function due to illness (nonthyroidal illness or sick euthyroid syndrome) |
| Increased | Normal | Normal | Subclinical hypothyroidism1; in a person with hypothyroidism on treatment, not enough thyroid hormone is being given |
| Increased | Decreased | Normal of decreased | Hypothyroidism resulting from a problem with the thyroid gland itself (primary hypothyroidism) |
| Normal or increased | Increased | Increased | Hyperthyroidism resulting from a problem with the pituitary gland signals (central hyperthyroidism) or from a problem with the thyroid hormone receptor (thyroid hormone resistance) |
| Decreased | Normal | Normal | Subclinical hyperthyroidism2; in a person with hypothyroidism, too much thyroid hormone is being given |
| Decreased | Normal | Increased | Hyperthyroidism resulting from the thyroid gland making too much active thyroid hormone T3 (uncommon, also known as T3 toxicosis) |
| Decreased | Increased | Increased | Hyperthyroidism resulting from the gland making too much thyroid hormones (primary hyperthyroidism) |
| Decreased | Decreased | Decreased | Hypothyroidism resulting from a problem with the hypothalamus or pituitary signals that govern the thyroid gland (central hypothyroidism) |
1. In affected adults, the diagnosis of subclinical hypothyroidism is applied when the TSH level is elevated and the free T4 level is normal on repeat testing over a number of weeks or months. Adults with subclinical hypothyroidism may have few or no overt symptoms of hypothyroidism. However, subclinical hypothyroidism places affected adults at somewhat increased risk for an elevated LDL “bad” cholesterol level, increased risk for cardiovascular disease, and reduced mental acuity.
2. In affected adults, the diagnosis of subclinical hyperthyroidism is applied when the TSH level is decreased and the free T4 level and T3 levels are normal on repeat testing over a number of weeks or months. Adults with subclinical hyperthyroidism may have few or no overt symptoms of hyperthyroidism. However, subclinical hyperthyroidism places affected persons at somewhat increased risk for atrial fibrillation and osteoporosis.
Footnote: Laboratory results must always be correlated with the clinical findings of the patient.
What medications can affect thyroid testing?
Many multivitamins, supplements (especially hair, skin, and nail) and over-the-counter and prescription medications may affect thyroid test results, and their use should be discussed with the healthcare practitioner prior to testing. For example, biotin (vitamin B7) can interfere with some lab tests, so your healthcare practitioner may advise you to refrain from taking biotin or supplements that contain biotin for a few days before having blood drawn for thyroid hormone testing. If you have a procedure done in which fluorescein dyes are injected into your blood (e.g., angiography), you may need to wait a few days before having thyroid testing done.
Triiodothyronine high
Triiodothyronine (T3) values >200 ng/dL in adults or > age related cutoffs in children are consistent with hyperthyroidism or increased thyroid hormone-binding proteins.
Abnormal levels (high or low) of thyroid hormone-binding proteins (primarily albumin and thyroid-binding globulin) may cause abnormal T3 concentrations in euthyroid (normal thyroid) patients.
Triiodothyronine (T3) is not useful for general screening of the population without a clinical suspicion of hyperthyroidism.
Triiodothyronine low
Triiodothyronine (T3) is not a reliable marker for hypothyroidism.
Therapy with amiodarone can lead to depressed triiodothyronine (T3) values.
Phenytoin, phenylbutazone, and salicylates cause release of triiodothyronine (T3) from the binding proteins, thus leading to a reduction in the total triiodothyronine (T3) hormone level at normal free triiodothyronine (T3) levels.
Autoantibodies to thyroid hormones can interfere with the triiodothyronine (T3) assay.
Binding protein anomalies may cause values that deviate from the expected results. Pathological concentrations of binding proteins can lead to results outside the reference range, although the patient may be in a euthyroid (normal thyroid) state. Free triiodothyronine (T3) or free thyroxine (free T4) testing is indicated in these cases.
Some patients who have been exposed to animal antigens, either in the environment or as part of treatment or imaging procedures, may have circulating antianimal antibodies present. These antibodies may interfere with the assay reagents to produce unreliable results.
- Armstrong M, Fingeret A. Physiology, Thyroid Function. [Updated 2018 Dec 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537039[↩][↩][↩]
- Choi JH, Cho JH, Kim JH, Yoo EG, Kim GH, Yoo HW. Variable Clinical Characteristics and Molecular Spectrum of Patients with Syndromes of Reduced Sensitivity to Thyroid Hormone: Genetic Defects in the THRB and SLC16A2 Genes. Horm Res Paediatr. 2018 Nov 29;:1-8[↩]
- Davis JR, Dackiw AP, Holt SA, Nwariaku FE, Oltmann SC. Rapid Relief: Thyroidectomy is a Quicker Cure than Radioactive Iodine Ablation (RAI) in Patients with Hyperthyroidism. World J Surg. 2019 Mar;43(3):812-817.[↩]
- Merson J. Hypothyroidism. JAAPA. 2018 Dec;31(12):43-44.[↩]