Contents
- What is relapsing polychondritis
What is relapsing polychondritis
Relapsing polychondritis is a rare autoimmune connective tissue disease which presents as severe, episodic, and progressive inflammation in cartilage bearing tissues like the ear, nose, larynx, trachea and bronchi, and may also involve the cardiovascular system, joints, eyes, skin, and kidneys 1, 2, 3, 4, 5, 6, 7, 8, 9. Ears, larynx and trachea may become “floppy” and the bridge of the nose can collapse into a “saddle nose” shape 10, 11. The aortic heart valve may also be affected. Relapsing polychondritis may also cause kidney inflammation and dysfunction. The inflammatory episodes are recurrent and unpredictable. A concomitant autoimmune disease also occurs in more than 30% of patients such as vasculitis 12, rheumatoid arthritis (RA) 13, and systemic lupus erythematosus (SLE) 14 or hematological diseases such as myelodysplastic syndrome (MDS) 15. Among Hungarian relapsing polychondritis patients a high prevalence (56%) of other autoimmune conditions was found, with Sjögren syndrome as the most common concomitant autoimmune disease 16, 17.
Jaksh-Wartenhorst described the first case with the name “polychondropathia” in 1923, when a 32-year-old patient presented with fever, pain, and swelling of the ears and later developed stenosis of external auditory canal and saddle nose deformity 18. A biopsy of the nasal cartilage showed the absence of cartilage. The term “relapsing polychondritis” was coined by Pearson and his coworkers in 1960 19. They recognized it as an inflammatory condition of the cartilaginous and noncartilaginous structures 19.
The cause of relapsing polychondritis is still not known 1, 20. Scientists suspect that relapsing polychondritis is an autoimmune condition 21. Autoimmune disorders also called autoimmune diseases are caused by the body’s immune system which normally helps protect your body from infection and disease begin attacking its own tissues (autoimmune) for unknown reasons 22. Some cases may be linked to abnormal reactions by blood cells (serum antibodies), to a thyroid protein (thyroglobulin), organ wall (parietal) cells, adrenal cells, or thyroid 21. Symptoms of relapsing polychondritis may arise when autoantibodies attack human cartilage.
Some researchers believe that relapsing relapsing polychondritis may be caused by an immunologic sensitivity to type II collagen, a normal substance found in skin and connective tissue.
Relapsing polychondritis is a rare autoimmune disease, being more common in Caucasians with the prevalence of 4.5 per million in a military population in the United States to 25 cases per million adults 23, 24. The annual incidence was estimated at 3.5 per million person-years in Rochester, MN, USA 25. However, a population-based cohort study conducted in the United Kingdom found a lower annual incidence, estimated at 0.71 per million person-years. The same study estimated the prevalence of relapsing polychondritis and estimated it at 9.0 cases per million population 26. The peak age at onset is between 40 years to 50 years, though it can occur at any age 27. Relapsing polychondritis occurs with equal frequency in both sexes and all racial groups. Over 30% of cases are associated with existing autoimmune condition or hematologic condition 28.
Clinical spectrum of relapsing polychondritis is variable and varies with duration of the disease and disease severity. Ear cartilage involvement is present in 90% of the cases, and inflammation is restricted to the cartilaginous portion of the ear with sparing of the ear lobes. Patients with relapsing polychondritis usually begin with the sudden onset of pain, tenderness, discoloration and swelling of the cartilage of one or both ears. The inflammation may spread to the fleshy portion of the outer ear causing it to narrow. Attacks may last several days to weeks before subsiding. Middle ear inflammation can cause obstruction of the eustachian tube. Recurrent attacks may lead to hearing loss.
Inflammation of both large and small joints is the second most common feature of relapsing polychondritis in 50% to 75% of patients. Wrist, metacarpophalangeal or the “knuckes” (the joint between the metacarpal head and the base of the proximal phalanx), proximal interphalangeal joints are commonly involved. Classic symptoms of pain and swelling are similar to those of arthritis.
Eye involvement occurs in 20% to 60% of relapsing polychondritis patients and involves episcleritis (inflammation of the episclera, the thin layer of tissue between the white of the eye [sclera] and the outer membrane [conjunctiva]), scleritis (inflammation of the sclera, the white outer layer of the eyeball, causing severe pain, redness with potential vision loss), keratitis (inflammation of the eye’s cornea, the clear tissue at the front of the eye that covers the pupil and iris), and uveitis (inflammation of the uvea, the middle layer of the eye containing blood vessels). Inflammation of the cartilage in the nose (nose chondritis) occurs in about 25% of cases. Nasal chondritis may be marked by cartilage collapse at the bridge of the nose resulting in a saddle nose deformity, nasal stuffiness or fullness and crusting.
In patients with relapsing polychondritis, up to 50% may experience airway involvement, and if unrecognized and left untreated it can lead to life threatening airway obstruction. Inflammation of the cartilage rings around trachea and bronchi results in the collapse of these airways (tracheobronchomalacia). Patient presents with a cough, speech difficulties, hoarseness of voice, wheezing and breathing difficulty. Respiratory tract involvement, specifically severe airway stenosis, can lead to acute respiratory failure, which is associated with a poor prognosis if not timely treated 29. Respiratory compromise is the most frequent cause of death in these patients.
Heart valve abnormalities, kidney inflammation and dysfunction also may occur.
The diagnosis of relapsing polychondritis is not always easy because there are no specific tests. Even when diagnosed, the treatment is not standardized. The drug treatment is tailored to each patient and the cornerstone of therapy is the use of glucocorticoids. For patients with severe relapsing polychondritis, other immunosuppressive are used including methotrexate and cyclophosphamide 30. Recently newer biological agents have also been used to manage relapsing polychondritis patients with varying results. However, prior to initiating treatment with these novel agents, the patient needs a thorough work up to ensure that he or she is fit to receive the therapy. Any patient with worsening of symptoms should be referred to the specialist 31. People who develop severe heart or respiratory complications may require surgery.
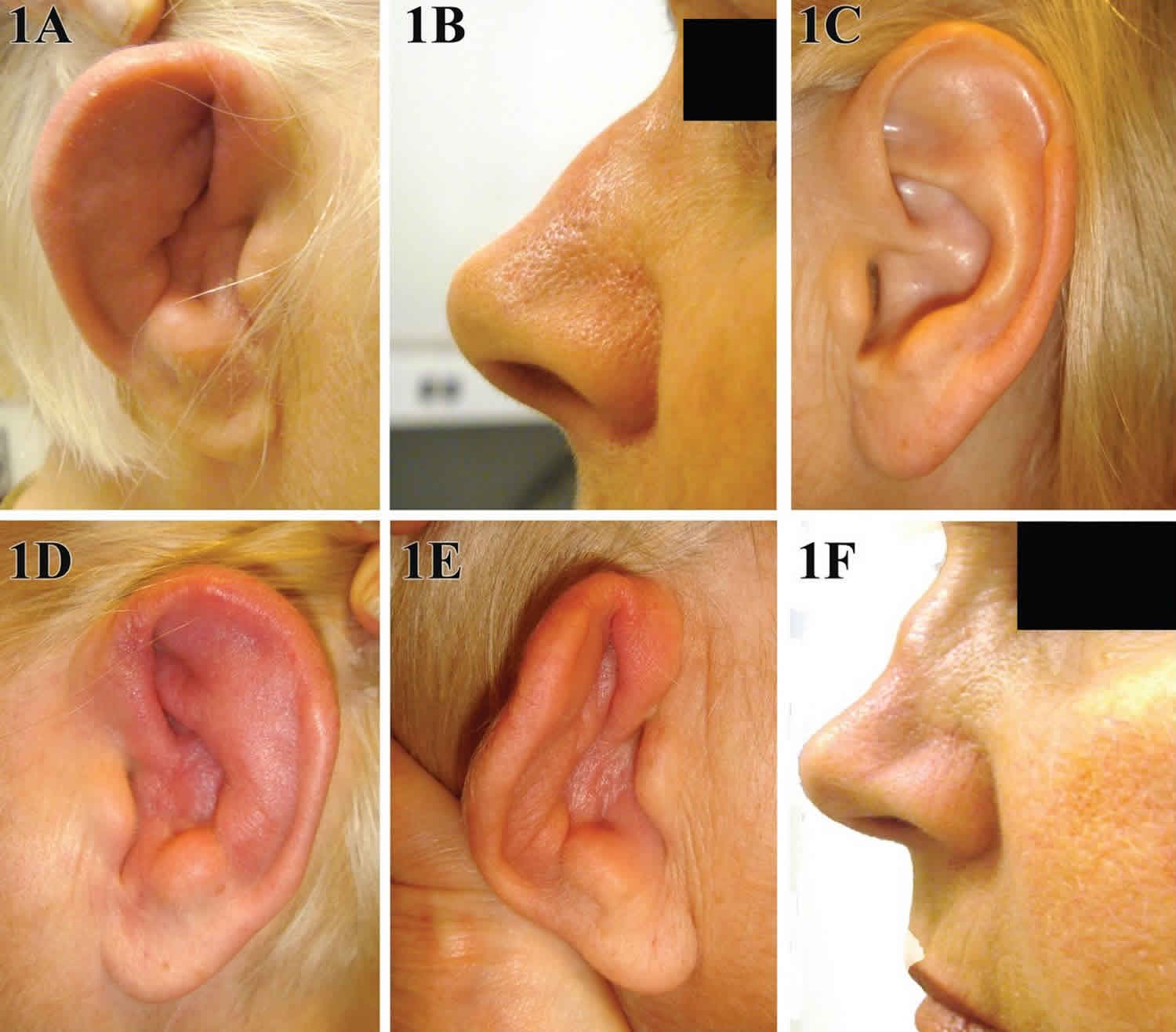
Figure 1. Relapsing polychondritis
Footnotes: A 31-year-old man presented to the emergency department with a 2-week history of swelling of the left ear and a 6-month history of weight loss, fatigue, and generalized aches. During the 2 years before presentation, he had been treated multiple times with antibiotics for recurrent episodes of pain in both ears. The physical examination revealed a tender, erythematous, and edematous left pinna, with sparing of the lobule (Panel A). The patient also had a prominent saddle-nose deformity that had developed over the previous year (Panel B). The costochondral joints were tender on palpation, and the left knee was swollen and tender. Laboratory studies showed an erythrocyte sedimentation rate of more than 120 mm per hour (reference range, 0 to 15). He received a diagnosis of relapsing polychondritis, a systemic autoimmune condition that affects cartilaginous structures, particularly of the ears, nose, joints, larynx, and large airways. Prednisone was prescribed at a dose of 40 mg daily, and the patient had some alleviation of the pain and swelling within 2 weeks. After 1 month, therapy with methotrexate was started, and the prednisone was slowly tapered over a period of 6 months.
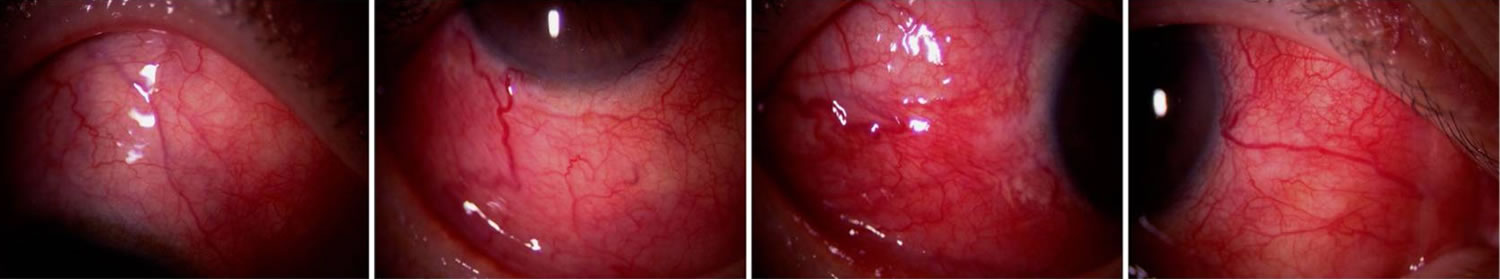
[Source 32 ]Figure 2. Relapsing polychondritis anterior acleritis (inflammation of the episcleral and scleral tissues)
Footnotes: Anterior Scleritis is inflammation of the episcleral and scleral tissues that presents with severe injection of superficial episcleral and deep scleral vessels. Depending on the severity, anterior scleritis may be associated with eye complications including loss of visual acuity, anterior uveitis, peripheral ulcerative keratitis, glaucoma, and retinal or choroidal detachment, and frequently requires work-up for associated systemic inflammatory conditions such as rheumatoid arthritis or, as in this case, relapsing polychondritis. Therefore, it is important to differentiate it from benign or self-limiting episcleritis. On slit lamp exam, visible vessels have classically demonstrate a crisscrossing pattern with conjunctival vessels oriented radially and episcleral vessels oriented in a more circumferential pattern, and yield a characteristic “violaceous hue”. Unlike conjunctival vessels, episcleral or deeper scleral vessels cannot be moved with a cotton-tipped applicator. Subconjunctival edema may be present. Instillation of phenylephrine drops will blanch the superficial conjunctival vessels but not the deeper episcleral vessels.
[Source 33 ]Figure 3. Relapsing polychondritis with diffuse anterior scleritis
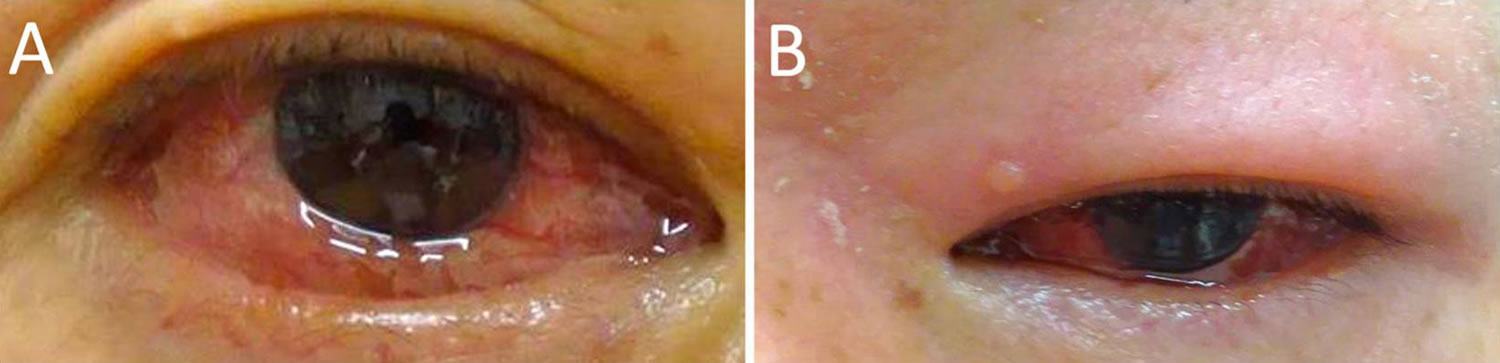
[Source 34 ]Figure 4. Relapsing polychondritis with conjunctivitis and eyelid edema
Footnotes: Relapsing polychondritis with conjunctivitis (nonspecific conjunctival redness), irritation, and itching. Subconjunctival hemorrhage and keratoconjunctivitis sicca have also been observed 35. Photographs show (A) conjunctival edema and hyperemia and (B) swelling and redness of the upper eyelid.
[Source 34 ]Relapsing polychondritis causes
The cause of relapsing polychondritis is still not known 1, 20. Scientists suspect that relapsing polychondritis is an autoimmune condition 21. Autoimmune disorders also called autoimmune diseases are caused by the body’s immune system which normally helps protect your body from infection and disease begin attacking its own tissues (autoimmune) for unknown reasons 22. Some cases may be linked to abnormal reactions by blood cells (serum antibodies), to a thyroid protein (thyroglobulin), organ wall (parietal) cells, adrenal cells, or thyroid 21. Symptoms of relapsing polychondritis may arise when autoantibodies attack human cartilage.
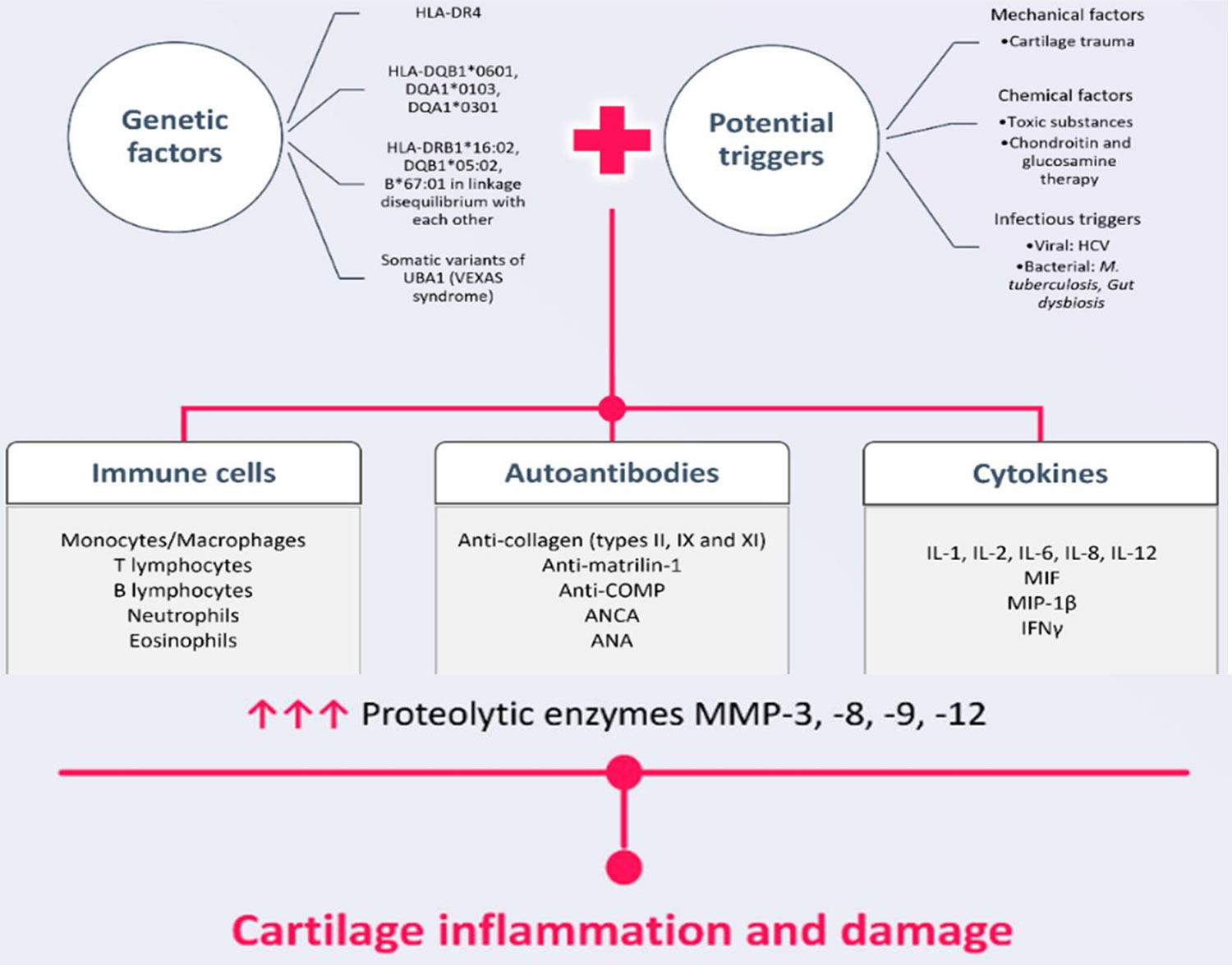
External triggers involved in the pathogenesis of relapsing polychondritis 36:
- Mechanical triggers: Mechanical factors include direct trauma to the cartilage; this leads to the exposure of cartilage matrix protein antigens, which are responsible for the occurrence of an autoimmune response 37. A published case study highlighted the appearance of inflammatory changes in the nose, ears and upper respiratory tract after an ear piercing 38.
- Trauma to the cartilage
- Ear piercing
- Chemical triggers: Chemical factors involved in the onset of chondritis refer mainly to the intravenous administration of various substances that can have a toxic effect on cartilage. The data show the rapid appearance, within 24 hour, of clinical manifestations similar to those of relapsing polychondritis, such as nasal and auricular inflammation, peripheral and axial joint damage, scleritis and vestibular disorders after an intravenous injection of some toxic substances (hydrochloric acid, carburetor fluid and the waxy internal matrix of a mentholated nasal inhaler) 39. Additionally, the rapid onset of bilateral auricular chondritis was described after the initiation of chondroitin and glucosamine therapy 40. Moreover, an intravenous injection of papain in rabbits was associated with important clinical changes, such as ear collapse or tracheal and bronchial damage, even causing acute respiratory distress 41.
- Toxic substances (hydrochloric acid, carburetor fluid, waxy internal matrix of a mentholated nasal inhaler)
- After chondroitin and glucosamine therapy initiation
- Intravenous papain injection
- Infectious triggers: Infectious triggers can determine the activation of the immune system through molecular mimicry, which is a structural similarity between one’s own heat shock proteins (HSPs) and microbial heat shock proteins 42. Therefore, the innate immune system is activated through the TLR (Toll-like receptor) and NLR (nucleotide-binding oligomerization domain-like receptor) signaling pathways 43. Cases of relapsing polychondritis associated with chronic hepatitis C virus infection have been reported in the literature 44, 45. Other data support the possible role of Mycobacterium tuberculosis in the pathogenesis of relapsing polychondritis because an antibody linked both to HSP60 from the bacterium and to cartilage structures was highlighted 46. It also seems that there is a close relationship between intestinal dysbiosis and relapsing polychondritis, as demonstrated by a metagenomic analysis. Gut dysbiosis in these patients is characterized by a numerical increase in Ruminococcus, Bacteroides, Veillonella and Eubacterium species 47.
- Chronic hepatitis C virus infection
- Mycobacterium tuberculosis
- Gut dysbiosis (increase in Ruminococcus, Bacteroides, Veillonella and Eubacterium species)
Some researchers believe that relapsing relapsing polychondritis may be caused by an immunologic sensitivity to type II collagen, a normal substance found in skin and connective tissue.
Relapsing polychondritis is suggested to occur in a genetically predisposed individual on exposure to a triggering factor. The triggering factor may be an infectious agent, chemical, toxic exposure, or direct trauma 1. Relapsing polychondritis cases have been reported after trauma occurring to the pinna (external part of the ear) 1. A possible explanation includes cryptogenic antigenic release after trauma and recognition of the antigen by the immune system. A genotyping study by Terao et al 48 found that HLA-DRB1*16:02, HLA-DQB1*05:02 and HLA-B*67:01 are associated with susceptibility to relapsing polychondritis. In Germans genetic studies, susceptibility for developing relapsing polychondritis has been found to be increased slightly in carriers of the HLA-DR4 haplotype 49, 50, 48. However, familial clustering has not been observed.
Three intriguing case reports suggest that hormonal influences may be important in relapsing polychondritis. Two men have developed relapsing polychondritis after receiving injections of luteinizing hormone–releasing hormone, and a woman with arthritis mutilans had a sudden exacerbation of her condition and new onset of atrophy of the auricular cartilage, nasal septum, weight loss, and deafness after receiving an injection of chorionic gonadotropin 51.
Relapsing polychondritis pathogenesis is not well understood. In early stages of the disease there is polymorphic inflammatory cell infiltration, later there is chondrocyte apoptosis, focal calcification, and fibrosis of the cartilage 52. The cartilage is infiltrated by neutrophils, T-lymphocytes, and natural killer T-cells. CD4+ T-cells also known as helper T cells secrete cytokines like interleukin-8, monocyte chemoattractant protein-1, and macrophage inflammatory protein 1-alpha, which recruit monocytes and macrophages 53. Macrophages release proteolytic enzymes, metalloproteinase-3 (MMP-3), cathepsin L and K which leads to cartilage destruction 52. Another hypothesis suggests that the uncontrolled production of autoantibodies against collagen type II, IX, and XI, matrilin-1, and cartilage oligomeric matrix proteins (COMPs) plays a crucial role in the pathogenesis of relapsing polychondritis 36. Molecular mimicry between different microorganisms and components of the cartilage matrix has also been observed, and this phenomenon is possibly involved in the pathogenesis 54.
Figure 5. Relapsing polychondritis pathogenesis (relapsing polychondritis pathogenic mechanisms)
[Source 36 ]Relapsing polychondritis symptoms
Relapsing polychondritis is characterized by recurrent inflammation of cartilage (the tough but flexible tissue that covers the ends of bones at a joint) and other tissues throughout the body.
Signs and symptoms of relapsing polychondritis include the following:
- Auricular chondritis. Auricular chondritis is the most common clinical feature and has been reported in approximately 60–90% of relapsing polychondritis patients 55. Auricular chondritis is characterized by painful, warm, red pressure-sensitive swelling of the helix, antihelix, tragus and antitragus with sparing of the noncartilaginous lobule. As the cartilage thins out, the underlying vasculature is more visible resulting in a bluish discoloration of the skin and is therefore called the “blue ear sign” 55, 56, 57.
- Nonerosive seronegative inflammatory polyarthritis. Joint involvements can be isolated at the onset of relapsing polychondritis. They are characterized by oligo- or polyarthritis, intermittent, migratory and asymmetric, without destruction (nonerosive). Large joints may be affected as well as small ones, such as metacarpophalangeal and interphalangeal joints, knees, ankles, or wrists 58.
- Nasal chondritis. Nasal chondritis is characterized by inflammation of the nasal cartilage. Patients typically experience pain and/or a sensation of pressure in the bridge of the nose and persistent nasal obstruction. Recurrent epistaxis, rhinorrhea and crusting may also occur. A saddle nose deformity develops due to damage of the nasal cartilage and occurs in about 20% of all patients 57, 59.
- Eye inflammation. Eye involvement is observed in 60% of cases and often precedes other signs and symptoms 60. Various eye involvement have been described, but the most common are episcleritis, scleritis, and conjunctivitis 58.
- Respiratory tract chondritis
- Tracheobronchial chondritis is found in 60% of relapsing polychondritis patients, with a time to onset of 2.5 years if absent at diagnosis 61. Tracheobronchial chondritis is characterized by cough and progressive shortness of breath (progressive dyspnea), inspiratory or expiratory stridor, depending on the severity of obstruction. Less than 50% obstruction may not be noticed by patients, leading to late diagnosis. Chest auscultation during inflammatory flare-ups may detect stridor or wheezing, indicating severe airway diseases, depending on the site of inflammation 62, 63, 64, 61. Inflammation and destruction of cartilaginous tissue results in loss of rigidity of the tracheobronchial tree, leading to either malacia, stenosis, and/or bronchiectasis, creating the conditions for infectious complications, particularly with immunosuppressive therapies 65, 66, 67. Tracheobronchial involvement leads to 25% of intensive care admission, making this sign or symptom one of the most severe in relapsing polychondritis patients, in relation to its frequency 61.
- Laryngeal chondritis is observed in 40% of cases with signs and symptoms such as dry cough, hoarseness, dysphonia/aphonia, or thyroid cartilage pain 62, 63, 64, 61. The inflammatory aspect of the larynx can be visualized by flexible nasendoscopy or bronchoscopy, with edema of the supraglottic region or the appearance of false vocal cords 65, 66. The evolution can be severe with laryngomalacia or laryngeal stenosis, responsible for inspiratory dyspnea, leading to respiratory failure, requiring tracheostomy 62, 63, 66, 67, 68.
- Audiovestibular damage. The middle and inner ear are frequently affected being described in 20% to 45% of cases and present with tinnitus, vestibular dysfunction or sensorineural hearing loss, highlighting the importance of regular audiometric examinations 58, 55, 56, 57.
- Cardiovascular disease. Cardiovascular involvement is the second common cause of death after respiratory complications and has been reported in 25% of adult relapsing polychondritis patients. The most common vascular complication is aneurysmal disease, predominantly involving the ascending aorta with ascending aortic root dilatation and aortic valve regurgitation and/or mitral regurgitation (which may be present alone) 58. Aneurysms can also occur in other vessels such as the cerebral or iliac arteries. Pericarditis, myocarditis, sinus tachycardia, atrioventricular block and peripheral vasculitis have also been described 69, 70, 71. There is also an increased risk of venous thrombosis 61, 72, 73.
- Skin disease. Skin features include nonspecific changes such as purpura, papulonodular exanthema, maculopapular rash, annular eruptive urticaria, or ulcerative lesions of the skin or oral and genital mucosa 57, 59, 74.
- Central nervous system (CNS) involvements. Neurologic feature, although rare, is associated with high morbidity and mortality. Cranial nerve palsies of the fifth and seventh cranial nerves are most common, however sterile meningitis, encephalitis, stroke and aneurysms have also been described 75, 76, 77.
- Kidney involvements. Kidney involvement can occur as segmental necrotizing glomerulonephritis, tubulointerstitial nephritis, or IgA nephropathy. Other immune mediated diseases such as granulomatosis with polyangiitis (GPA), microscopic polyangiitis or renal involvement in systemic lupus erythematosus (SLE) should be considered as differential diagnosis.
- Myelodysplasia or myelodysplastic syndrome. Myelodysplasia is a group of bone marrow disorders where immature blood cells don’t mature into healthy, functional red blood cells, white blood cells, and platelets. This leads to a shortage of healthy blood cells, causing symptoms like anemia (fatigue, weakness), increased susceptibility to infection (from low white blood cells), and bleeding or bruising easily (from low platelets). Myelodysplasia occurs in up to 10–15% of patients with relapsing polychondritis and affects males, over the age of 50 years 75, 78, 79.
- Gastrointestinal tract involvement. Gastrointestinal tract involvement in relapsing polychondritis remains unclear. However, inflammatory bowel diseases and motility disorders have been described in patients with relapsing polychondritis 59.
- Other autoimmune diseases. Relapsing polychondritis is associated with other autoimmune diseases in up to 25–35% of patients. These include various forms of vasculitis (12%), Sjögren`s sydrome (10%), Hashimoto thyroiditis (6%), systemic lupus erythematosus (SLE) (4%), rheumatoid arthritis (3%), and less commonly antiphospholipid syndrome, Behcet disease 59, 80.
- A variety of other conditions
The features of relapsing polychondritis and the severity of symptoms vary significantly from person to person, but may include:
- Ear: The ears are the most commonly affected body part. Symptoms include a sudden onset of pain, swelling, and tenderness of the cartilage of one or both ears. The pinna usually loses firmness and becomes floppy; hearing impairment may also occur. Inflammation of the inner ear may also cause nausea, vomiting, dizziness, and/or ataxia.
- Joint: The second most common finding is joint pain with or without arthritis. Costochondritis presents with chest pain and sternal tenderness. The presence of costochondritis after remission of symptoms is a good indicator of relapse and in some cases, pain can be so severe that it impairs breathing. Intermittent, non-erosive, seronegative asymmetric oligo- or polyarthritis affecting the small and/or large joints are also common. In relapsing polychondritis, arthritis typically spares the axial skeleton 75, 81, 76, 82 .
- Eye: Affected people may experience episcleritis, uveitis and/or uni- or bilateral scleritis. Scleritis may lead to a bluish or dark discoloration of the sclera (white of the eye) and may even be associated with vision loss in severe cases. Proptosis (bulging out of one or both eye balls) may also be a symptom of relapsing polychondritis. Rarely, keratitis or uveitis have been described. Serious but rare complications include occlusion of retinal arteries or veins, optic neuritis, retinopathy, or retinal detachment 83, 84.
- Nose: Nasal cartilage inflammation may lead to stuffiness, crusting, rhinorrhea, epistaxis (nose bleeds), compromised sense of smell and/or saddle nose deformity (a condition where the nose is weakened and thus “saddled” in the middle).
- Airways: In patients with relapsing polychondritis, up to 50% may experience airway involvement, and if unrecognized and left untreated it can lead to life threatening airway obstruction. Inflammation may affect the larynx, trachea (windpipe), and bronchi (tubes that branch off the trachea and carry air to the lungs). Airway involvement may lead to a cough, wheezing, hoarseness and recurrent infections. It can become life-threatening if not properly diagnosed and managed. Laryngeal chondritis presents with a range of symptoms which include throat ache, hoarseness, cough, dyspnea and stridor. Tracheobronchial involvement can result in severe tracheobronchomalacia, where the airway collapses during expiration due to the loss of the tracheal and bronchial cartilages 81, 85, 86, 87, 88, 88. Tracheobronchial involvement is thought to be more frequent in children than in adults and accounts for approximately one third of all fatalities in relapsing polychondritis 89.
Less commonly, relapsing polychondritis may affect the heart, kidneys, nervous system, gastrointestinal tract, and/or vascular (veins) system. Nonspecific symptoms such as fever, weight loss, malaise, and fatigue may also be present.
In approximately one third of affected people, relapsing polychondritis is associated with other medical problems. Conditions reportedly associated with relapsing polychondritis include hematological disease (including Hodgkin’s lymphoma and myelodysplastic syndromes); gastrointestinal disorders (including Crohn’s disease and ulcerative colitis); endocrine diseases (including diabetes mellitus type 1 and thyroid disorders) and others.
Episodes of relapsing polychondritis may last a few days or weeks and typically resolve with or without treatment. However, it is generally progressive, and many people have persistent symptoms in between flares.
Table 1. Systemic vasculitis and connective tissue disorders associated with relapsing polychondritis (not exhaustive)
| Systemic vasculitis | Behçet’s disease (MAGIC syndrome), granulomatosis with polyangiitis, polyarthritis nodosa, Churg and Strauss’s syndrome |
| Connective tissue diseases | Sjögren’s syndrome, rheumatoid arthritis, systemic lupus erythematosus, mixed connective tissue diseases, systemic sclerosis |
| Spondyloarthritis | Ankylosing spondylitis, psoriatic arthritis, reactive arthritis, inflammatory bowels diseases |
| Other autoimmune diseases | Autoimmune thyroiditis, type 1 diabetes, familial Mediterranean fever, myasthenia gravis, primary biliary cirrhosis |
| Malignancies | Myelodysplastic syndromes, lymphomas, myeloproliferative neoplasms, thymoma |
| Dermatosis | Sweet’s syndrome, neutrophilic dermatosis, pyoderma gangrenosum, leukocytoclastic vasculitis, psoriasis |
Abbreviation: MAGIC, mouth and genital ulcers with inflamed cartilage
[Source 90 ]Relapsing polychondritis complications
Complications of relapsing polychondritis include the following:
- Vertigo
- Tinnitus
- Voice hoarseness
- Joint deformity
- Epiglottitis
- Scleritis
- Conjunctivitis
- Iritis
- Need for permanent tracheotomy (severe cases)
- Severe pulmonary infection
- Blindness
- Frail chest wall
- Respiratory failure
- Aortic regurgitation
- Mitral regurgitation
- Aortic dissection
- Glomerulonephritis-associated renal failure
Relapsing polychondritis diagnosis
Diagnosis of relapsing polychondritis is primarily based on a combination of clinical features, radiology, and biopsy of a cartilaginous site. It is guided by a set of clinical criteria suggested by McAdams et al. 79, 91, 92:
Major criteria
- Recurrent chondritis of both auricles
- Chondritis of nasal cartilages
- Laryngo-tracheal chondritis
Minor criteria
- Ocular inflammation (conjunctivitis/keratitis/scleritis/uveitis)
- Hearing loss
- Peripherical vestibular dysfunction (tinnitus/vertigo)
- Nonerosive seronegative polyarthritis
Two major criterias or one major criteria with two minor criterias are needed to diagnose relapsing polychondritis 79, 91, 92.
Any patient suspected of having relapsing polychondritis should have a dynamic exploratory CT scan to evaluate for airway involvement 78, 80. CT scans show functional airway abnormalities such as air trapping and collapse. Additional findings include thickening of the airway wall and luminal narrowing. Pulmonary function testing is done to further evaluate for airway trapping and to assess lung volumes.
PET-CT is a new diagnostic modality that aids in early disease recognition and provides a site for targeted biopsy. PET-CT may help to detect chondritis indirectly 93, 94. However, a PET-CT is not recommended as a standard diagnostic procedure 80.
Biopsy of the auricular cartilage is performed to confirm the diagnosis of polychondritis. Routine cartilage biopsy is not recommended for confirming the diagnosis of relapsing polychondritis as there are no pathognomonic histological findings. However, in the appropriate clinical setting demonstration of cartilage necrosis with variable inflammatory infiltrates can help to confirm the diagnosis and exclude differential diagnoses as bacterial infection or vasculitis 95. There are no lab markers to assess for ongoing cartilage damage.
Although anti-type II collagen antibodies have been shown to correlate well with relapsing polychondritis disease severity 96, 97, they are neither sensitive nor specific for relapsing polychondritis and can also be detected in rheumatoid arthritis and systemic lupus erythematosus (SLE) 98.
Anemia, if present, is typically normochromic and normocytic and is associated with a poor prognosis. Nonspecific indicators of inflammation (eg, elevated erythrocyte sedimentation rate [ESR], elevated levels of C-reactive protein {CRP]) are often present. Mild leukocytosis may be detected.
Radiographic findings can include a non-erosive juxta-articular osteopenia and uniform, joint space narrowing; these findings are suggestive of arthropathy in relapsing polychondritis.
Use antinuclear antibody reflexive panel, rheumatoid factor, and antiphospholipid antibodies (if history of thrombosis is found) to evaluate for other autoimmune connective-tissue diseases 99. Positive serologic testing for rheumatoid factor and anti-nuclear antibody may be seen in patients with other associated rheumatologic diseases. Complement levels are usually normal in patients with relapsing polychondritis.
For a vasculitis workup, perform the following studies 99:
- Complete blood cell count (CBC) with differential
- Metabolic panel
- Serum creatinine
- Liver transaminase and serum alkaline phosphatase studies
- Urinalysis dipstick and microscopic evaluation of sediment
- Cryoglobulins
- Viral hepatitis panel
- Antinuclear antibody (ANA)
- Antineutrophil cytoplasmic antibody (ANCA)
Use the purified protein derivative test to evaluate for exposure to tuberculosis. Tuberculosis is often overlooked as an infectious cause of perichondritis 99.
Use serologic tests for syphilis if it is suspected, including rapid plasma reagent or VDRL testing 99. Saddle-nose deformity is a clinical manifestation of congenital syphilis and can go undiagnosed into adulthood; however, it can also be a consequence of gumma formation in adulthood.
Cultures may be indicated, depending on the clinical presentation, as follows 99:
- Sputum cultures for bacteria and acid-fast bacilli may be needed in patients with respiratory symptoms.
- Bacterial, acid-fast bacilli, and fungal cultures may be appropriate for cartilage biopsy samples, especially from the respiratory tree.
- Blood cultures may be useful in the assessment of febrile episodes that are combined with nausea, vertigo, and/or muscle weakness.
- Bacterial and viral cultures of the cerebrospinal fluid may be indicated to exclude meningitis or to help exclude aseptic meningitis or CNS vasculitis.
Table 2. Relapsing Polychondritis diagnostic criteria
| McAdam’s criteria | Damiani’s criteria | Michet’s criteria |
|---|---|---|
| Clinical features | ||
|
| Major criteria |
| ||
| Minor criteria | ||
| ||
| Diagnosis | ||
|
|
|
| ||
| ||
Relapsing polychondritis differential diagnosis
The differential diagnosis of relapsing polychondritis includes the following 102, 24:
- VEXAS (vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic) syndrome
- Autoinflammatory diseases
- Immune checkpoint inhibitor-related adverse events
Other conditions to consider in the differential diagnosis of polychondritis include 102:
- Rheumatoid arthritis
- Polyarteritis nodosa
- Cogan syndrome
- Infectious perichondritis
- MAGIC syndrome (relapsing polychondritis [RP] plus Behçet disease)
- Trauma (especially in boxers and wrestlers)
- Congenital syphilis
- Chronic external otitis
- Auricular calcification (secondary to other conditions, eg, trauma, Addison disease, diabetes, hyperthyroidism)
- Addison Disease
- Behcet Disease
- Cellulitis
- Granulomatosis with Polyangiitis (GPA) also called Wegener Granulomatosis
- Hyperthyroidism and Thyrotoxicosis
- Polyarteritis Nodosa
- Syphilis
- Systemic Lupus Erythematosus (SLE)
Auricular chondritis causes include 102:
- Infectious perichondritis (commonly due to Pseudomonas aeruginosa infection); also, fungal infection, tuberculosis, syphilis, and leprosy
- Chronic external otitis
- Trauma
- Frostbite
- Calcification of the pinna resulting from Addison disease, ochronosis, acromegaly, essential hypertension, diabetes mellitus, and familial cold hypersensitivity
- Complication of mastoid surgery
- Benign nodular deformity (ie, chondrodermatitis nodularis chronica helicis)
Inflammatory arthritis causes include 102::
- Rheumatoid arthritis (adult or juvenile)
- Reactive arthritis
- Acute gonococcal arthropathy
- Rheumatic fever
- Granulomatosis with polyangiitis (formerly known as Wegener granulomatosis)
- Polyarteritis nodosa
- Systemic lupus erythematosus and other collagen-vascular disorders
Nasal chondritis or saddle-nose deformity causes include 102:
- Infectious perichondritis
- Granulomatosis with polyangiitis (formerly known as Wegener granulomatosis)
- Congenital syphilis
- Syphilis
- Nasal NK/peripheral T-cell lymphoma (formerly known as angiocentric lymphoma)
- Drug abuse (cocaine)
Eye inflammation causes include 102:
- Reactive arthritis (ie, conjunctivitis plus arthritis plus urethritis)
- Rheumatoid arthritis, Behçet disease, enteropathic arthritis, or Still disease (ie, iritis or chorioretinitis plus arthritis)
- Polyarteritis nodosa or granulomatosis with polyangiitis (ie, scleritis or episcleritis plus arthritis)
- Sjögren syndrome (ie, keratoconjunctivitis sicca plus arthritis)
- Cogan syndrome (ie, intersitial keratitis plus cochlear and vestibular damage)
- Arteriosclerosis, syphilis, collagen vascular disease, herpes zoster, sickle cell disease, migraine, coagulation disorders (ie, ischemic optic neuropathy)
Tracheal obstruction causes include the following 102:
- Trauma (eg, strangulation)
- Prolonged intubation
- Sarcoidosis
- Granulomatosis with polyangiitis
- Endoluminal malignancy
- Tuberculosis/sarcoidosis webs
Respiratory tree chondritis or perichondritis of the larynx resulting from any of the following 102:
- Herpes
- Syphilis
- Erysipelas
- Tonsillitis
- Peritonsillar abscess
- Tuberculosis
- Measles
- Diphtheria
- Scarlet fever
- Avitaminosis
- Blastomycosis
- Actinomycosis
- Granulomatosis with polyangiitis
- Xanthoma
- Typhus
- Vincent infection
- Anthrax
CNS alterations causes include the following 102::
- Septic meningitis (fungal, bacterial, mycobacterial)
- Aseptic meningitis unrelated to relapsing polychondritis, ie, viral
- Ménière disease
- Temporal arteritis
- Malignancy
- Drug toxicity
- Encephalitis or meningoencephalitis
- Other causes of cerebral vasculitis
- Other causes of seizure disorder
- Leprosy
Aortitis causes include the following 102::
- Erdheim cystic medial necrosis
- Marfan syndrome
- Syphilitic aortitis
- Giant cell arteritis
Relapsing polychondritis treatment
Due to the rarity of relapsing polychondritis, there are no there is no standardized treatment approach, and the treatment is guided by the clinical presentation and the severity of the disease 7, 53.
Relapsing polychondritis is a complex condition that requires a team approach for patient care:
- Dermatologists or specialists in infectious diseases are often involved early in the course of the disease to evaluate the patient for infectious causes of cellulitis or perichondritis.
- Rheumatologists usually become the primary care provider and should be involved early in patient care.
- Ophthalmologists should also be involved early to diagnose, monitor, and treat the potentially devastating ocular complications.
- Cardiologists, neurologists, nephrologists, and otolaryngologists may be asked to manage other aspects of relapsing polychondritis.
- Plastic surgeons can aid in nasal reconstruction if saddle-nose deformity is present.
For patients presenting with ear, nose or joint involvement but no systemic involvement, anti-inflammatory medications, colchicine or dapsone is recommended. Low-dose glucocorticoid therapy is often required.
For patients with more severe presentation such as large airway involvement such as laryngeal or tracheobronchial chondritis, abrupt onset of sensorineural hearing loss, or eye involvement, glucocorticoid therapy with IV methylprednisolone 1 gram for three days followed by oral prednisone 1 mg/kg along with immunosuppressive therapy is indicated 1. The most commonly used immunosuppressive agents include cyclophosphamide, methotrexate, azathioprine, and cyclosporine. Cyclophosphamide is commonly used as the initial medication (1-2 mg/kg); after remission is achieved, cyclophosphamide is switched to other less toxic immunosuppressive agents like azathioprine or methotrexate 1.
Biologics have been used in the treatment of relapsing polychondritis 1. The most commonly used biologic is the TNF-alpha inhibitor infliximab 1. Other biologics which have been tried with variable results include adalimumab, etanercept, abatacept, tocilizumab. Data on rituximab has not shown success, and this agent is not recommended as the first-line biologic agent 1.
Surgical interventions such as stenting, airway dilation, tracheostomy, and laryngotracheal reconstruction are needed in cases of airway collapse 1.
Surgical treatment
Surgeries encountered in the care of patients with relapsing polychondritis may include the following:
- Tracheostomy
- Permanent tracheotomy placement
- Tracheal stent placement
- Aortic aneurysm repair
- Cardiac valve replacement
- Saddle-nose deformity repair
Subglottic stenosis can be treated with submucosal corticosteroid injection followed by serial dilation. Wierzbicka et al reported good airway patency for more than 24 months in eight of 12 patients with relapsing polychondritis or other autoimmune disorders treated with this approach. [58]
The benefits of any proposed surgery must be weighed adequately against the patient’s risk for infection, especially in the event of acute relapse, since patients are at an increased risk of infection whether or not they are using corticosteroids.
Additionally, patients with relapsing polychondritis and tracheal disease may be at particular risk regarding complications resulting from tracheal intubation and extubation.
Relapsing polychondritis prognosis
The prognosis or long-term outlook for people with relapsing polychondritis varies from person to person. In general, relapsing polychondritis is a chronic and progressive (worsening overtime) condition. Some form of disability is common in the later stages of relapsing polychondritis; these may include visual impairment, hearing loss, vestibular dysfunction, and/or cardiopulmonary (heart and lung) disease 103.
Complications of relapsing polychondritis such as saddle-nose deformity, systemic vasculitis, laryngotracheobronchial stricture, arthritis, and anemia in patients younger than 51 years portend a poorer prognosis than in age-matched patients with relapsing polychondritis without complications. In patients older than 51 years, only anemia is associated with a poorer prognosis. Renal involvement is a poor prognostic factor at all ages.
Severe cases of relapsing polychondritis can be life-threatening. Respiratory complications (windpipe collapse and infections) are the most common cause of death followed by cardiovascular (heart and blood vessel) involvement 104.
In recent years, improvements have been made in the outcomes of patients with relapsing polychondritis. Survival rates have increased from 70% after 5 years, to 94% after 8 years and even 91% after 10 years in a recent study 105.
Relapsing polychondritis life expectancy
Patients with relapsing polychondritis have frequent relapses and the quality of life is poor. The mortality rate of relapsing polychondritis patients is twice that of the general population. The outcome of patients with relapsing polychondritis has improved in the recent years; survival has increased from 70% at five years to 91% at ten years 106. However, those data may represent relapsing polychondritis in patients with less severe disease than patients studied in earlier reports. Another study reported a 5-year survival rate associated with relapsing polychondritis has been reported to be 66-74% (45% if relapsing polychondritis occurs with systemic vasculitis), with a 10-year survival rate of 55% 107.
The more common clinical presentation is a relatively benign disease with respiratory failure due to airway collapse being the most common cause of death.
The most frequent causes of death associated with relapsing polychondritis include infection secondary to corticosteroid treatment or respiratory compromise (10%-50% of deaths result from airway complications), systemic vasculitis, and malignancy unrelated to relapsing polychondritis.
Although the life expectancy in all patients with relapsing polychondritis is decreased compared with age- and sex-matched healthy individuals, patients with renal involvement have a significantly lower age-adjusted life expectancy. In those with renal disease, uremia is the third most frequent cause of death.
Until randomized controlled studies are available, the treatment of relapsing polychondritis will remain empirical and based on personal experience. For healthcare workers who have never treated such a patient, referral to a tertiary care center is recommended 108.
- Chauhan K, Surmachevska N, Hanna A. Relapsing Polychondritis. [Updated 2023 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK436007[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Liu Y, Li X, Cheng L, Zhan H, Huang Y, Li H, Li Y. Progress and challenges in the use of blood biomarkers in relapsing polychondritis. Clin Exp Immunol. 2023 Jun 5;212(3):199-211. doi: 10.1093/cei/uxad014[↩]
- Sharma A, Gnanapandithan K, Sharma K, Sharma S. Relapsing polychondritis: a review. Clin Rheumatol. 2013 Nov;32(11):1575-83. doi: 10.1007/s10067-013-2328-x[↩]
- Butterton JR, Collier DS, Romero JM, Zembowicz A. Case records of the Massachusetts General Hospital. Case 14-2007. A 59-year-old man with fever and pain and swelling of both eyes and the right ear. N Engl J Med. 2007 May 10;356(19):1980-8. doi: 10.1056/NEJMcpc079009[↩]
- Borgia F, Giuffrida R, Guarneri F, Cannavò SP. Relapsing Polychondritis: An Updated Review. Biomedicines. 2018 Aug 2;6(3):84. doi: 10.3390/biomedicines6030084[↩]
- Masuda N, Nishikawa R, Ueda T, Ogata N. Severe panuveitis with relapsing polychondritis. Am J Ophthalmol Case Rep. 2018 Apr 20;11:3-5. doi: 10.1016/j.ajoc.2018.04.024[↩]
- Zheutlin A, Schiopu E. Relapsing Polychondritis following Treatment with Secukinumab for Ankylosing Spondylitis: Case Report and Review of the Literature. Case Rep Rheumatol. 2018 Jul 2;2018:6760806. doi: 10.1155/2018/6760806[↩][↩]
- Neycheva S, Kamburova A. IL-17 Inhibitor Secukinumab Achieves Remission in Relapsing Polychondritis: A Case Report. Am J Case Rep. 2025 Mar 20;26:e946916. doi: 10.12659/AJCR.946916[↩]
- Winter G, Löffelmann T, Chaya S, Kaiser H, Prenzler NK, Warnecke A, Wetzke M, Derlin T, Renz D, Stueber T, Länger F, Schütz K, Schwerk N. Relapsing Polychondritis with Tracheobronchial Involvement: A Detailed Description of Two Pediatric Cases and Review of the Literature. Klin Padiatr. 2024 Feb;236(2):97-105. doi: 10.1055/a-2230-1521[↩]
- Arnaud L, Mathian A, Haroche J, et al. Pathogenesis of relapsing polychondritis: A 2013 update. Autoimmun Rev. 2014;13:90–95. doi: 10.1016/j.autrev.2013.07.005[↩]
- Trentham DE, Le CH. Relapsing polychondritis. Ann Intern Med. 1998;129:114–22. doi: 10.7326/0003-4819-129-2-199807150-00011[↩]
- D’Cruz DP, Ferrada MA. Relapsing Polychondritis and Large-vessel Vasculitis. J Rheumatol. 2020 Dec 1;47(12):1732-1733. doi: 10.3899/jrheum.200083[↩]
- Ostrowski RA, Takagishi T, Robinson J. Rheumatoid arthritis, spondyloarthropathies, and relapsing polychondritis. Handb Clin Neurol. 2014;119:449-61. doi: 10.1016/B978-0-7020-4086-3.00029-1[↩]
- Zeuner M, Straub RH, Rauh G, Albert ED, Schölmerich J, Lang B. Relapsing polychondritis: clinical and immunogenetic analysis of 62 patients. J Rheumatol. 1997 Jan;24(1):96-101.[↩]
- Dion J, Costedoat-Chalumeau N, Sène D, Cohen-Bittan J, Leroux G, Dion C, Francès C, Piette JC. Relapsing Polychondritis Can Be Characterized by Three Different Clinical Phenotypes: Analysis of a Recent Series of 142 Patients. Arthritis Rheumatol. 2016 Dec;68(12):2992-3001. doi: 10.1002/art.39790[↩]
- Horváth A, Páll N, Molnár K, et al. A nationwide study of the epidemiology of relapsing polychondritis. Clin Epidemiol. 2016;8:211–230. doi: 10.2147/CLEP.S91439[↩]
- Kent PD, Michet CJ, Luthra HS. Relapsing polychondritis. Curr Opin Rheumatol. 2004;16:56–61. doi: 10.1097/00002281-200401000-00011[↩]
- Jaksch-Wartenhorst R. Polychondropathia. Wien. Arch. Inn. Med. 1923;6:93–100.[↩]
- Pearson C.M., Kline H.M., Newcomer V.D. Relapsing polychondritis. N. Engl. J. Med. 1960 Jul 14;263:51-8. doi: 10.1056/NEJM196007142630201[↩][↩]
- Relapsing Polychondritis. https://emedicine.medscape.com/article/331475-overview#a7[↩][↩]
- Relapsing Polychondritis. https://rarediseases.org/rare-diseases/relapsing-polychondritis/[↩][↩][↩][↩]
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Selected Heritable Disorders of Connective Tissue and Disability; Wedge RA, Cartaxo T, Spicer CM, et al., editors. Selected Heritable Disorders of Connective Tissue and Disability. Washington (DC): National Academies Press (US); 2022 Jul 8. Available from: https://www.ncbi.nlm.nih.gov/books/NBK584971[↩][↩]
- Relapsing polychondritis in the Department of Defense population and review of the literature. Mathew SD, Battafarano DF, Morris MJ. Semin Arthritis Rheum. 2012 Aug; 42(1):70-83.[↩]
- Mertz, P., Costedoat-Chalumeau, N., Ferrada, M.A. et al. Relapsing polychondritis: clinical updates and new differential diagnoses. Nat Rev Rheumatol 20, 347–360 (2024). https://doi.org/10.1038/s41584-024-01113-9[↩][↩]
- Relapsing polychondritis. Kent PD, Michet CJ Jr, Luthra HS. Curr Opin Rheumatol. 2004 Jan; 16(1):56-61.[↩]
- Incidence and mortality of relapsing polychondritis in the UK: a population-based cohort study. Hazra N, Dregan A, Charlton J, Gulliford MC, D’Cruz DP. Rheumatology (Oxford). 2015 Dec; 54(12):2181-7.[↩]
- Lekpa FK, Chevalier X. Refractory relapsing polychondritis: Challenges and solutions. Open Access Rheumatol. 2018;10:1–11. doi: 10.2147/OARRR.S142892[↩]
- Leung KK, Edani S. Red-eared zebra diagnosis: Case of relapsing polychondritis. Can Fam Physician. 2018 May;64(5):363-367. https://pmc.ncbi.nlm.nih.gov/articles/PMC5951651[↩]
- Kothari T, Valsamakis T, Sridhar A V et al. Case of paediatric relapsing polychondritis with severe airway involvement: the challenges of long-term airway and respiratory management. BMJ Case Rep. 2021;14:e239774. doi: 10.1136/bcr-239774[↩]
- Meshkov AD, Novikov PI, Zhilyaev EV, Ilevsky IDJ, Moiseev SV. Tofacitinib in steroid-dependent relapsing polychondritis. Ann. Rheum. Dis. 2018 May 03[↩]
- Moulis G, Pugnet G, Costedoat-Chalumeau N, Mathian A, Leroux G, Boutémy J, Espitia O, Bouillet L, Berthier S, Gaultier JB, Jeandel PY, Konaté A, Mékinian A, Solau-Gervais E, Terrier B, Wendling D, Andry F, Garnier C, Cathébras P, Arnaud L, Palmaro A, Cacoub P, Amoura Z, Piette JC, Arlet P, Lapeyre-Mestre M, Sailler L. Efficacy and safety of biologics in relapsing polychondritis: a French national multicentre study. Ann. Rheum. Dis. 2018 Aug;77(8):1172-1178[↩]
- Relapsing Polychondritis. N Engl J Med 2018; 378:1715 DOI: 10.1056/NEJMicm1713302 https://www.nejm.org/doi/full/10.1056/NEJMicm1713302[↩]
- Scleritis. https://eyerounds.org/atlas/pages/Scleritis13.htm#gsc.tab=0[↩]
- Fukuda K, Mizobuchi T, Nakajima I, Kishimoto T, Miura Y, Taniguchi Y. Ocular Involvement in Relapsing Polychondritis. J Clin Med. 2021 Oct 26;10(21):4970. doi: 10.3390/jcm10214970[↩][↩]
- Isaak B.L., Liesegang T., Michet C.J. Ocular and Systemic Findings in Relapsing Polychondritis. Ophthalmology. 1986;93:681–689. doi: 10.1016/S0161-6420(86)33695-9[↩]
- Cardoneanu A, Rezus II, Burlui AM, Richter P, Bratoiu I, Mihai IR, Macovei LA, Rezus E. Autoimmunity and Autoinflammation: Relapsing Polychondritis and VEXAS Syndrome Challenge. Int J Mol Sci. 2024 Feb 13;25(4):2261. doi: 10.3390/ijms25042261[↩][↩][↩]
- Canas C.A., Abadía F.B. Local cartilage trauma as a pathogenic factor in autoimmunity (one hypothesis based on patients with relapsing polychondritis triggered by cartilage trauma) Autoimmune Dis. 2012;2012:453698. doi: 10.1155/2012/453698[↩]
- Alissa H., Kadanoff R., Adams E. Does mechanical insult to cartilage trigger relapsing polychondritis? Scand. J. Rheumatol. 2001;30:311. doi: 10.1080/030097401753180426[↩]
- Berger R. Polychondritis resulting from intravenous substance abuse. Am. J. Med. 1988;85:415–417. doi: 10.1016/0002-9343(88)90597-9[↩]
- Furer V., Wieczorek R.L., Pillinger M.H. Bilateral pinna chondritis preceded by glucosamine chondroitin supplement initiation. Scand. J. Rheumatol. 2010;40:241–243. doi: 10.3109/03009742.2010.507551[↩]
- Mccluskey R.T., Thomas L. The removal of cartilage matrix, in vivo, by papain: Identification of crystalline papain protease as the cause of the phenomenon. J. Exp. Med. 1958;108:371. doi: 10.1084/jem.108.3.371[↩]
- Zugel U., Kaufmann S.H. Role of heat shock proteins in protection from and pathogenesis of infectious diseases. Clin. Microbiol. Rev. 1999;12:19–39. doi: 10.1128/CMR.12.1.19[↩]
- Yang C.L., Brinckmann J., Rui H.F., Vehring K.H., Lehmann H., Kekow J., Wolff H.H., Gross W.L., Müller P.K. Autoantibodies to cartilage collagens in relapsing polychondritis. Arch. Dermatol. Res. 1993;285:245–249. doi: 10.1007/BF00371591[↩]
- Hemmati I., Yoshida E., Shojania K. Relapsing polychondritis associated with hepatitis C virus infection. Clin. Rheumatol. 2012;31:391–394. doi: 10.1007/s10067-011-1881-4[↩]
- Herrera I., Concha R., Molina E.G., Schiff E.R., Altman R.D. Relapsing polychondritis, chronic hepatitis C virus infection, and mixed cryoglobulemia. Semin. Arthritis Rheum. 2004;33:388–403. doi: 10.1016/j.semarthrit.2003.11.001[↩]
- Menge T., Rzepka R., Melchers I. Monoclonal autoantibodies from patients with autoimmune diseases: Specificity, affinity and crossreactivity of MAbs binding to cytoskeletal and nucleolar epitopes, cartilage antigens and mycobacterial heat-shock protein 60. Immunobiology. 2002;205:1–16. doi: 10.1078/0171-2985-00107[↩]
- Shimizu J., Takai K., Takada E., Fujiwara N., Arimitsu N., Ueda Y., Wakisaka S., Suzuki T., Suzuki N. Possible association of proinflammatory cytokines including IL1beta and TNFalpha with enhanced Th17 cell differentiation in patients with Behcet’s disease. Clin. Rheumatol. 2016;35:1857–1863. doi: 10.1007/s10067-015-2966-2[↩]
- Terao C, Yoshifuji H, Yamano Y, Kojima H, Yurugi K, Miura Y, Maekawa T, Handa H, Ohmura K, Saji H, Mimori T, Matsuda F. Genotyping of relapsing polychondritis identified novel susceptibility HLA alleles and distinct genetic characteristics from other rheumatic diseases. Rheumatology (Oxford). 2016 Sep;55(9):1686-92. doi: 10.1093/rheumatology/kew233[↩][↩]
- Paravar T. Less common rheumatologic disorders: Current concepts of skin and systemic manifestations. Clin Dermatol. 2018 Jul-Aug;36(4):525-532. doi: 10.1016/j.clindermatol.2018.04.009[↩]
- Krishnan Y, Grodzinsky AJ. Cartilage diseases. Matrix Biol. 2018 Oct;71-72:51-69. doi: 10.1016/j.matbio.2018.05.005[↩]
- Labarthe MP, Bayle-Lebey P, Bazex J. Cutaneous manifestations of relapsing polychondritis in a patient receiving goserelin for carcinoma of the prostate. Dermatology. 1997;195(4):391-4. doi: 10.1159/000245996[↩]
- Zampeli E, Moutsopoulos HM. Relapsing polychondritis: a diagnosis not to be missed. Rheumatology (Oxford). 2018 Oct 1;57(10):1768. doi: 10.1093/rheumatology/key124[↩][↩]
- Lekpa FK, Chevalier X. Refractory relapsing polychondritis: challenges and solutions. Open Access Rheumatol. 2018 Jan 9;10:1-11. doi: 10.2147/OARRR.S142892[↩][↩]
- Menge T, Rzepka R, Melchers I. Monoclonal autoantibodies from patients with autoimmune diseases: Specificity, affinity and crossreactivity of MAbs binding to cytoskeletal and nucleolar epitopes, cartilage antigens and mycobacterial heat-shock protein 60. Immunobiology. 2002;205(1):1–16. doi: 10.1078/0171-2985-00107[↩]
- Bachor E, Blevins N H, Karmody C et al. Otologic manifestations of relapsing polychondritis. Review of literature and report of nine cases. Auris Nasus Larynx. 2006;33:135–141. doi: 10.1016/j.anl.2005.11.020[↩][↩][↩]
- Yang H, Peng L, Jian M et al. Clinical analysis of 15 patients with relapsing auricular polychondritis. Eur Arch Otorhinolaryngol. 2014;271:473–476. doi: 10.1007/s00405-013-2422-3[↩][↩]
- Smylie A, Malhotra N, Brassard A. Relapsing Polychondritis: A Review and Guide for the Dermatologist. Am J Clin Dermatol. 2017;18:77–86. doi: 10.1007/s40257-016-0226-0[↩][↩][↩][↩]
- Grandière L, Vicaire H, Pop G, Didier M, Freynet O, Alexandre M, Clero D, Mathian A, Martinod E, Brillet PY, Gille T, Uzunhan Y. Relapsing polychondritis: tracheobronchial involvement and differential diagnoses. J Thorac Dis. 2025 Jan 24;17(1):461-475. doi: 10.21037/jtd-24-1603[↩][↩][↩][↩]
- Lahmer T, Treiber M, von Werder A et al. Relapsing polychondritis: An autoimmune disease with many faces. Autoimmun Rev. 2010;9:540–546. doi: 10.1016/j.autrev.2010.02.016[↩][↩][↩][↩]
- Hazra N, Dregan A, Charlton J, et al. Incidence and mortality of relapsing polychondritis in the UK: a population-based cohort study. Rheumatology (Oxford) 2015;54:2181-7. 10.1093/rheumatology/kev240[↩]
- Dion J, Costedoat-Chalumeau N, Sène D, et al. Relapsing Polychondritis Can Be Characterized by Three Different Clinical Phenotypes: Analysis of a Recent Series of 142 Patients. Arthritis Rheumatol 2016;68:2992-3001. 10.1002/art.39790[↩][↩][↩][↩][↩]
- Longo L, Greco A, Rea A, et al. Relapsing polychondritis: A clinical update. Autoimmun Rev 2016;15:539-43. 10.1016/j.autrev.2016.02.013[↩][↩][↩]
- Puéchal X, Terrier B, Mouthon L, et al. Relapsing polychondritis. Joint Bone Spine 2014;81:118-24. 10.1016/j.jbspin.2014.01.001[↩][↩][↩]
- Mathian A, Miyara M, Cohen-Aubart F, et al. Relapsing polychondritis: A 2016 update on clinical features, diagnostic tools, treatment and biological drug use. Best Pract Res Clin Rheumatol 2016;30:316-33. 10.1016/j.berh.2016.08.001[↩][↩]
- Ernst A, Rafeq S, Boiselle P, et al. Relapsing polychondritis and airway involvement. Chest 2009;135:1024-30. 10.1378/chest.08-1180[↩][↩]
- de Montmollin N, Dusser D, Lorut C, et al. Tracheobronchial involvement of relapsing polychondritis. Autoimmun Rev 2019;18:102353. 10.1016/j.autrev.2019.102353[↩][↩][↩]
- Chen N, Zheng Y. Characteristics and Clinical Outcomes of 295 Patients With Relapsing Polychondritis. J Rheumatol 2021;48:1876-82. 10.3899/jrheum.210062[↩][↩]
- Xie C, Shah N, Shah PL, et al. Laryngotracheal reconstruction for relapsing polychondritis: case report and review of the literature. J Laryngol Otol 2013;127:932-5. 10.1017/S0022215113001746[↩]
- Tomelleri A, Campochiaro C, Sartorelli S et al. Large-vessel Vasculitis Affecting the Aorta and its Branches in Relapsing Polychondritis: Case Series and Systematic Review of the Literature. J Rheumatol. 2020;47:1780–1784. doi: 10.3899/jrheum.190862[↩]
- Bahena-Lopez E, Loya-Centurion J. Relapsing polychondritis, a rare cause of valvulopathy: A review of the medical literature. Arch Cardiol Mex. 2020;90:173–176. doi: 10.24875/ACME.M20000112[↩]
- Erdogan M, Esatoglu S N, Hatemi G et al. Aortic involvement in relapsing polychondritis: case-based review. Rheumatol Int. 2021;41:827–837. doi: 10.1007/s00296-019-04468-5[↩]
- Chen N, Zheng Y. Characteristics and Clinical Outcomes of 295 Patients With Relapsing Polychondritis. J Rheumatol 2021;48:1876-82. 10.3899/jrheum.21006[↩]
- Le Besnerais M, Arnaud L, Boutémy J, et al. Aortic involvement in relapsing polychondritis. Joint Bone Spine 2018;85:345-51. 10.1016/j.jbspin.2017.05.009[↩]
- Firestein G S, Gruber H E, Weisman M H et al. Mouth and genital ulcers with inflamed cartilage: MAGIC syndrome. Five patients with features of relapsing polychondritis and Behcet’s disease. Am J Med. 1985;79:65–72. doi: 10.1016/0002-9343(85)90547-9[↩]
- Trentham D E, Le C H. Relapsing polychondritis. Ann Intern Med. 1998;129:114–122. doi: 10.7326/0003-4819-129-2-199807150-00011[↩][↩][↩]
- Puechal X, Terrier B, Mouthon L et al. Relapsing polychondritis. Joint Bone Spine. 2014;81:118–124. doi: 10.1016/j.jbspin.2014.01.001[↩][↩]
- Jeon C H. Relapsing Polychondritis with Central Nervous System Involvement: Experience of Three Different Cases in a Single Center. J Korean Med Sci. 2016;31:1846–1850. doi: 10.3346/jkms.2016.31.11.1846[↩]
- Lee K S, Ernst A, Trentham D E et al. Relapsing polychondritis: prevalence of expiratory CT airway abnormalities. Radiology. 2006;240:565–573. doi: 10.1148/radiol.2401050562[↩][↩]
- McAdam LP, O’Hanlan MA, Bluestone R, Pearson CM. Relapsing polychondritis: prospective study of 23 patients and a review of the literature. Medicine (Baltimore). 1976 May;55(3):193-215.[↩][↩][↩][↩]
- Arnaud L, Costedoat-Chalumeau N, Mathian A et al. French practical guidelines for the diagnosis and management of relapsing polychondritis. Rev Med Interne. 2023;44:282–294. doi: 10.1016/j.revmed.2023.05.005[↩][↩][↩]
- Alqanatish J T, Alshanwani J R. Relapsing polychondritis in children: A review. Mod Rheumatol. 2020;30:788–798. doi: 10.1080/14397595.2019.1707995[↩][↩]
- Kingdon J, Roscamp J, Sangle S et al. Relapsing polychondritis: a clinical review for rheumatologists. Rheumatology (Oxford) 2018;57:1525–1532. doi: 10.1093/rheumatology/kex406[↩]
- Yu E N, Jurkunas U, Rubin PA D et al. Obliterative microangiopathy presenting as chronic conjunctivitis in a patient with relapsing polychondritis. Cornea. 2006;25:621–622. doi: 10.1097/01.ico.0000227886.26747.a9[↩]
- Isaak B L, Liesegang T J, Michet CJ J. Ocular and systemic findings in relapsing polychondritis. Ophthalmology. 1986;93:681–689. doi: 10.1016/s0161-6420(86)33695-9[↩]
- Rafeq S, Trentham D, Ernst A. Pulmonary manifestations of relapsing polychondritis. Clin Chest Med. 2010;31:513–518. doi: 10.1016/j.ccm.2010.04.004[↩]
- Ernst A, Rafeq S, Boiselle P et al. Relapsing polychondritis and airway involvement. Chest. 2009;135:1024–1030. doi: 10.1378/chest.08-1180[↩]
- Letko E, Zafirakis P, Baltatzis S et al. Relapsing polychondritis: a clinical review. Semin Arthritis Rheum. 2002;31:384–395. doi: 10.1053/sarh.2002.32586[↩]
- Molina J F, Espinoza L R. Relapsing polychondritis. Baillieres Best Pract Res Clin Rheumatol. 2000;14:97–109. doi: 10.1053/berh.1999.0079[↩][↩]
- Lin D, Yang W, Zhang P et al. Clinical and prognostic characteristics of 158 cases of relapsing polychondritis in China and review of the literature. Rheumatol Int. 2016;36:1003–1009. doi: 10.1007/s00296-016-3449-8[↩]
- Lekpa FK, Chevalier X. Refractory relapsing polychondritis: challenges and solutions. Open Access Rheumatol. 2018;10:1-11. Published 2018 Jan 9. doi:10.2147/OARRR.S142892 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5768290/[↩]
- Michet CJ, Jr, McKenna CH, Luthra HS, et al. Relapsing polychondritis. Survival and predictive role of early disease manifestations. Ann Intern Med 1986;104:74-8. 10.7326/0003-4819-104-1-74[↩][↩]
- Rose T, Schneider U, Bertolo M, Klotsche J, Casteleyn V, Biesen R, Burmester GR, Hiepe F. Observational study and brief analysis of diagnostic criteria in relapsing polychondritis. Rheumatol Int. 2018 Nov;38(11):2095-2101. doi: 10.1007/s00296-018-4121-2[↩][↩]
- Deng H, Chen P, Wang L et al. Relapsing polychondritis on PET/CT. Clin Nucl Med. 2012;37:712–715. doi: 10.1097/rlu.0b013e31823eae56[↩]
- Yamashita H, Takahashi H, Kubota K et al. Utility of fluorodeoxyglucose positron emission tomography/computed tomography for early diagnosis and evaluation of disease activity of relapsing polychondritis: a case series and literature review. Rheumatology (Oxford) 2014;53:1482–1490. doi: 10.1093/rheumatology/keu147[↩]
- Gergely P J, Poor G. Relapsing polychondritis. Best Pract Res Clin Rheumatol. 2004;18:723–738. doi: 10.1016/j.berh.2004.05.012[↩]
- Giroux L, Paquin F, Guerard-Desjardins M J et al. Relapsing polychondritis: an autoimmune disease. Semin Arthritis Rheum. 1983;13:182–187. doi: 10.1016/0049-0172(83)90005-7[↩]
- Foidart J M, Abe S, Martin G R et al. Antibodies to type II collagen in relapsing polychondritis. N Engl J Med. 1978;299:1203–1207. doi: 10.1056/NEJM197811302992202[↩]
- Terato K, Shimozuru Y, Katayama K et al. Specificity of antibodies to type II collagen in rheumatoid arthritis. Arthritis Rheum. 1990;33:1493–1500. doi: 10.1002/art.1780331006[↩]
- Relapsing Polychondritis Workup. https://emedicine.medscape.com/article/331475-workup[↩][↩][↩][↩][↩]
- Michet CJ J, McKenna C H, Luthra H S et al. Relapsing polychondritis. Survival and predictive role of early disease manifestations. Ann Intern Med. 1986;104:74–78. doi: 10.7326/0003-4819-104-1-74[↩]
- Damiani JM, Levine HL. Relapsing polychondritis–report of ten cases. Laryngoscope. 1979 Jun;89(6 Pt 1):929-46.[↩]
- Relapsing Polychondritis Differential Diagnoses. https://emedicine.medscape.com/article/331475-differential[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Relapsing Polychondritis. https://emedicine.medscape.com/article/331475-overview[↩]
- Relapsing polychondritis. https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=en&Expert=728 [↩]
- Puéchal X, Terrier B, Mouthon L, Costedoat-Chalumeau N, Guillevin L, Le Jeunne C. Relapsing polychondritis. Joint Bone Spine. 2014 Mar;81(2):118-24. doi: 10.1016/j.jbspin.2014.01.001[↩]
- Chauhan K, Hanna A. Relapsing Polychondritis. [Updated 2019 Jan 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK436007[↩]
- Michet CJ Jr, McKenna CH, Luthra HS, O’Fallon WM. Relapsing polychondritis. Survival and predictive role of early disease manifestations. Ann Intern Med. 1986 Jan. 104(1):74-8.[↩]
- Sharma A, Law AD, Bambery P, Sagar V, Wanchu A, Dhir V, Vijayvergiya R, Sharma K, Gupta A, Panda NK, Singh S. Relapsing polychondritis: clinical presentations, disease activity and outcomes. Orphanet J Rare Dis. 2014 Dec 20;9:198.[↩]