Contents
What is toxic megacolon
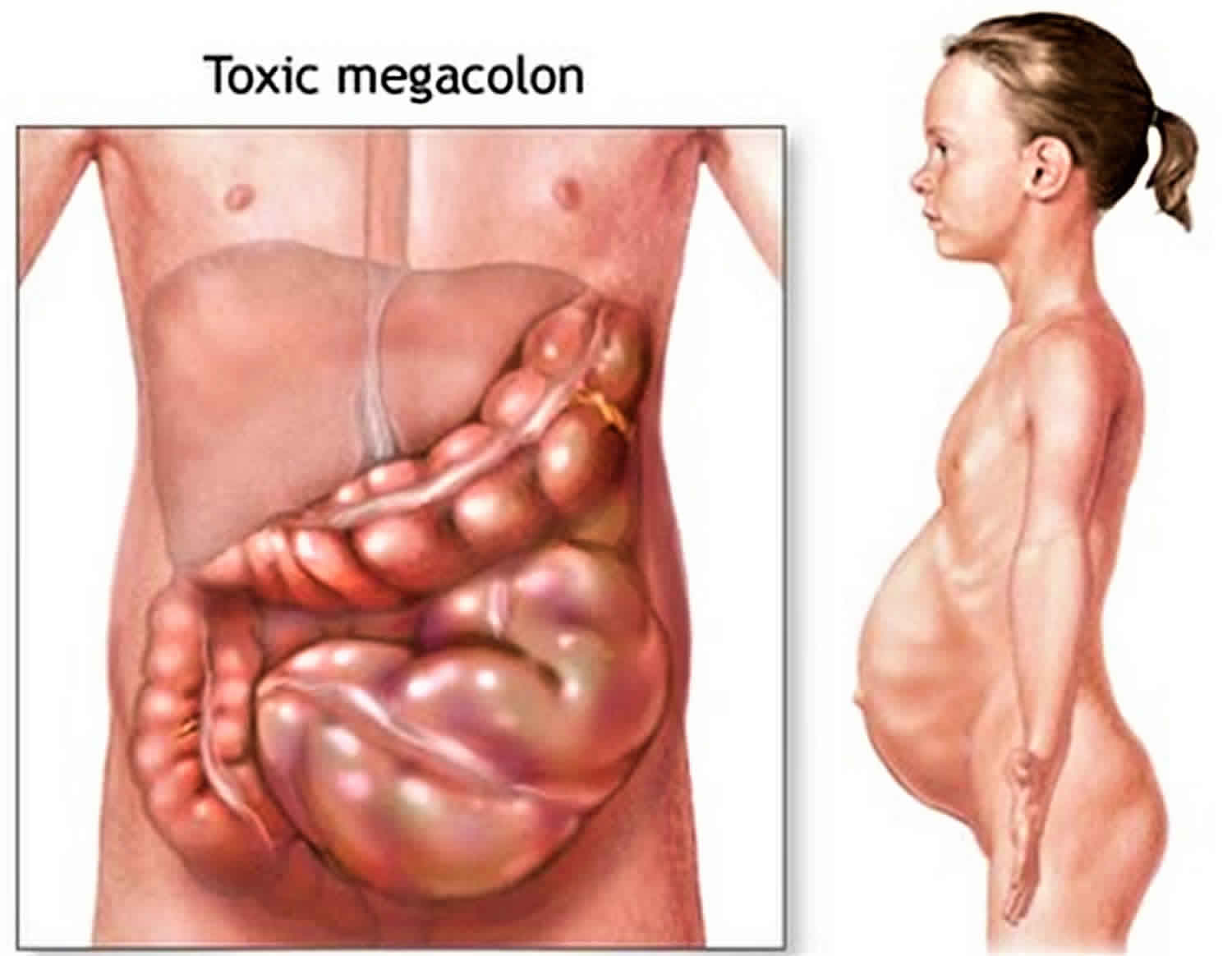
Toxic megacolon is characterized by extreme inflammation and distention of the colon. Toxic megacolon occurs when swelling and inflammation spread into the deeper layers of your colon. As a result, the colon stops working and widens. In severe cases, the colon may rupture. Toxic megacolon is a complication that can be seen in both types of inflammatory bowel disease, and less commonly in infectious colitis, as well as in some other types of colitis.
Common symptoms are pain, distention of the abdomen, fever, rapid heart rate, and dehydration.
Toxic megacolon is a life-threatening complication that requires immediate medical treatment.
Go to the emergency room or call the local emergency number if you develop severe abdominal pain, especially if you also have:
- Bloody diarrhea
- Fever
- Frequent diarrhea
- Rapid heart rate
- Tenderness when the abdomen is pressed
- Abdominal distention
Toxic megacolon causes
The mechanisms involved in the development of toxic megacolon are not entirely clear, although chemical mediators such as nitric oxide and interleukins are thought to play a pivotal role in its pathogenesis 1.
The term “toxic” means that this problem is very dangerous. Toxic megacolon may occur in people with an inflamed colon due to:
- Ulcerative colitis, or Crohn disease that is not well controlled
- Infectious causes of toxic megacolon include:
Toxic megacolon may also be caused by:
- Radiation colitis
- Ischemic colitis
- Nonspecific colitis secondary to chemotherapy 7
- Rarely as a complication of collagenous colitis 8
- Behçet syndrome – Patients with this syndrome can rarely develop toxic megacolon as a complication 9
- Kaposi’s sarcoma 10
- Methotrexate therapy induced pseudomembranous colitis
Other forms of megacolon include pseudo-obstruction, acute colonic ileus, or congenital colonic dilation. These conditions do not involve an infected or inflamed colon. Toxic colitis is preferred by many now as the colon is not always dilated.
Figure 1. Toxic megacolon in Crohn disease
Toxic megacolon prevention
Treating diseases that cause toxic megacolon, such as ulcerative colitis or Crohn disease, can prevent this condition.
Toxic megacolon symptoms
The rapid widening of the colon may cause the following symptoms to occur over a short period of time:
- Painful, distended abdomen
- Fever
- Diarrhea (usually bloody)
Toxic megacolon possible complications
Toxic megacolon complications may include:
- Perforation of the colon
- Sepsis
- Shock
- Death
Toxic megacolon diagnosis
Your health care provider will perform a physical exam. Findings may include:
- Tenderness in the abdomen
- Reduced or absent bowel sounds
The exam may reveal signs of septic shock, such as:
- Increased heart rate
- Mental status changes
- Rapid heart rate
- Low blood pressure
Your health care provider may order any of the following tests:
- Abdominal x-ray, ultrasound, CT scan, or MRI scan
- Blood electrolytes
- Complete blood count
Toxic megacolon treatment
Treatment of toxic megacolon includes 3 main goals: (1) reduce colonic distention to prevent perforation, (2) correct fluid and electrolyte disturbances, and (3) treat toxemia and precipitating factors. Careful and frequent monitoring of the patient is required, and, initially, CBCs, electrolytes, and abdominal radiographs should be checked every 12 hours. If the patient is malnourished, consider parenteral nutrition.
Treatment of the disorder that led to toxic megacolon includes:
- Steroids and other medicines that suppress the immune system
- Antibiotics
If you have septic shock, you will be admitted to the intensive care unit of the hospital. Treatment may include:
- Breathing machine (mechanical ventilation)
- Dialysis for kidney failure
- Drugs to treat low blood pressure, infection, or poor blood clotting
- Fluids given directly into a vein
- Oxygen
If rapid widening is not treated, an opening or rupture can form in the colon. Therefore, most cases of toxic megacolon will need surgery to remove a part of or the entire colon.
You may receive antibiotics to prevent sepsis (a severe infection).
During the initial resuscitation, fluid replacement, electrolyte repletion, and transfusion should be aggressive. Broad-spectrum intravenous (IV) antibiotics with coverage equivalent to ampicillin, gentamicin, and metronidazole should be initiated. All medications that may affect colonic motility—including narcotics, antidiarrheals, and anticholinergic agents—must be stopped.
The patient with toxic megacolon should be put on bowel rest, and a nasogastric tube (NGT) or long intestinal tube should be placed to assist with gastrointestinal decompression. Long suction tubes may be more helpful for colonic decompression, but they should be placed into the ileum under fluoroscopic guidance.
The patient should be started on IV steroids. IV hydrocortisone is necessary for patients who are taking corticosteroids or who have been recently treated with corticosteroids.
It is important to recognize that although symptomatic improvement may correspond to improvement in the disease process, this is not always the case. Cessation of bowel movements may indicate worsening of the patient’s condition. Including repeated abdominal plain films in the evaluation of the clinical picture remains essential.
Any possible triggers for toxic megacolon should be stopped, including narcotics, antidiarrheals, and anticholinergics.
Rolling techniques (knee-elbow and prone) may be performed to assist in redistribution of colonic gas and decompression 11.
Cyclosporine
Some reports indicate that cyclosporine A may be beneficial in the treatment toxic megacolon or of severe ulcerative colitis, with data suggesting that cyclosporine may provide an initial response rate of as high as 80%. After a variable follow-up period, the durable response rate decreases to approximately 40%.
Although further studies are needed, cyclosporine therapy may obviate the need for urgent colectomy, allowing an elective subtotal colectomy or proctocolectomy to be performed under more controlled circumstances 12.
However, cyclosporine also has significant adverse effects, including immunosuppression and opportunistic infections, hypertension, renal toxicity, and neurologic complications.
Additional therapies
Some experimental therapies under study may help patients with toxic megacolon to avoid surgery. A case report showed that the use of infliximab, an anti–TNF-alpha monoclonal antibody, was successful in the treatment of toxic megacolon in a patient whose condition failed to respond to usual treatment and who refused surgery 13.
Leukocytapheresis has been reported to be effective against toxic megacolon. A series of 6 patients whose conditions had failed to improve after treatment with antibiotics and high-dose steroids were enrolled in a study 14. In 4 cases, the toxic megacolon resolved by the morning after initiation of treatment with leukocytapheresis. In 2 patients, the toxic megacolon resolved approximately 40 hours later. Improvement continued in 4 of the 6 patients 14.
Hyperbaric oxygen has also been reported to be of use in the treatment of toxic megacolon 15, but further studies are needed to confirm these results.
Shetler et al. 16 demonstrated that colonoscopic decompression and intracolonic vancomycin administration in the management of severe, acute, pseudomembranous colitis associated with ileus and toxic megacolon is feasible, safe, and effective in approximately 57-71% of cases.
Tacrolimus was successfully used in 1 case study in a patient with steroid-refractory ulcerative colitis complicated by toxic megacolon. Further studies are needed to validate the use 17.
Intravenous immune globulin (IVIG) may potentially be a last-line adjunct therapy in patients with severe complicated, refractory Clostridium difficile infection (eg, shock, ileus, megacolon), taking into account the possibility of adverse effects 18.
Colectomy
Early surgical consultation is essential for cases of toxic megacolon (toxic colitis). Indications for urgent operative intervention include free perforation, massive hemorrhage (6-8 units packed red blood cells), increasing toxicity, and progression of colonic dilatation. Most authors recommend colectomy if persistent dilatation is present or if no improvement is observed on maximal medical therapy after 24-72 hours.
The rationale for early intervention is based on a 5-fold increase in mortality after free perforation. The mortality rate for nonperforated, acute toxic colitis is about 4%; if perforation occurs, the mortality is approximately 20%. Significant independent predictors of mortality include Mannheim peritonitis index (MPI) class II and American Society of Anesthesiologists (ASA) classes 4-5 19.
Some physicians provide up to 7 days of medical therapy if the patient demonstrates clinical improvement despite persistent colonic dilatation. The authors recommend a strategy of early surgical intervention to minimize the incidence of colonic perforation. If no improvement occurs over 48-72 hours with medical therapy, perform surgical resection.
Whether to perform a total proctocolectomy or a subtotal colectomy with the rectum left behind is debated 20. The preference in the literature is to perform a subtotal colectomy; this is due to the following reasons:
- The patient is usually very ill, and not lengthening the operation is prudent if at all possible
- Subtotal colectomy preserves the possibility for an ileal pouch anal anastomosis
- Approximately 50% of patients with Crohn disease have minimal involvement of the rectum
Performing a total proctocolectomy in a patient who is acutely ill and toxic and on high-dose steroids increases the risk of complications, morbidity, and mortality.
Terminate the resection at the sacral promontory, and perform either a mucus fistula or a stapled rectal stump. If a stapled rectal stump is performed, keeping a rectal tube in place for 2-3 days may reduce the incidence of rectal stump blowout.
Because the surgical treatment of toxic megacolon requires an ostomy, the patient must give clear, informed consent. In addition, discussing the implications of an ostomy with the patient and the patient’s family is helpful. Also, it is important to tell the patient that surgical treatment may be staged such that reoperation is required in the future.
Toxic megacolon prognosis
If the condition does not improve, it can be fatal. Colon surgery is usually needed in such cases.
- Gan SI, Beck PL. A new look at toxic megacolon: an update and review of incidence, etiology, pathogenesis, and management. Am. J. Gastroenterol. 2003;98 (11): 2363-71. doi:10.1111/j.1572-0241.2003.07696.x[↩]
- Bartlett JG, Perl TM. The new Clostridium difficile–what does it mean?. N Engl J Med. 2005 Dec 8. 353(23):2503-5.[↩]
- Sidebotham EL, Sepkowitz K, Price AP, Steinherz PG, La Quaglia MP, Kayton ML. Eradication of cryptosporidium from a defunctionalized colon limb by refeeding stoma effluent. J Pediatr Surg. 2010 Jan. 45(1):E33-6.[↩]
- Shimada Y, Iiai T, Okamoto H, et al. Toxic megacolon associated with cytomegalovirus infection in ulcerative colitis. J Gastroenterol. 2003. 38(11):1107-8[↩]
- Hung CW, Wu WF, Wu CL. Rotavirus gastroenteritis complicated with toxic megacolon. Acta Paediatr. 2009 Nov. 98(11):1850-2[↩]
- Mohite U, Kell J, Haj MA, et al. Invasive aspergillosis localised to the colon presenting as toxic megacolon. Eur J Haematol. 2007 Mar. 78(3):270-3[↩]
- Hayes-Lattin BM, Curtin PT, Fleming WH, et al. Toxic megacolon: a life-threatening complication of high-dose therapy and autologous stem cell transplantation among patients with AL amyloidosis. Bone Marrow Transplant. 2002 Sep. 30(5):279-85[↩]
- Fitzgerald SC, Conlon S, Leen E, Walsh TN. Collagenous colitis as a possible cause of toxic megacolon. Ir J Med Sci. 2009 Mar. 178(1):115-7[↩]
- Umehara Y, Kudo M, Kawasaki M. Endoscopic findings of intestinal Behçet’s disease complicated with toxic megacolon. Endoscopy. 2010. 42 Suppl 2:E173-4[↩]
- Sheth SG, LaMont JT. Toxic megacolon. Lancet. 1998 Feb 14. 351(9101):509-13[↩]
- Panos MZ, Wood MJ, Asquith P. Toxic megacolon: the knee-elbow position relieves bowel distension. Gut. 1993 Dec. 34(12):1726-7[↩]
- Actis GC, Ottobrelli A, Pera A, et al. Continuously infused cyclosporine at low dose is sufficient to avoid emergency colectomy in acute attacks of ulcerative colitis without the need for high-dose steroids. J Clin Gastroenterol. 1993 Jul. 17(1):10-3.[↩]
- van Geenen EJ, Sachar DB. Infliximab in Crohn’s disease-associated toxic megacolon. J Clin Gastroenterol. 2012 Apr. 46(4):321-3[↩]
- Sawada K, Egashira A, Ohnishi K, et al. Leukocytapheresis (LCAP) for management of fulminant ulcerative colitis with toxic megacolon. Dig Dis Sci. 2005 Apr. 50(4):767-73.[↩][↩]
- Kuroki K, Masuda A, Uehara H, Kuroki A. A new treatment for toxic megacolon. Lancet. 1998 Sep 5. 352(9130):782[↩]
- Shetler K, Nieuwenhuis R, Wren SM, Triadafilopoulos G. Decompressive colonoscopy with intracolonic vancomycin administration for the treatment of severe pseudomembranous colitis. Surg Endosc. 2001 Jul. 15(7):653-9[↩]
- Pascu M, Muller AR, Wiedenmann B, Dignass AU. Rescue therapy with tacrolimus in a patient with toxic megacolon. Int J Colorectal Dis. 2003 May. 18(3):271-5[↩]
- Shah PJ, Vakil N, Kabakov A. Role of intravenous immune globulin in streptococcal toxic shock syndrome and Clostridium difficile infection. Am J Health Syst Pharm. 2015 Jun 15. 72(12):1013-9.[↩]
- Tapani MJ, Olavi KH. Surgical management of toxic megacolon. Hepatogastroenterology. 2014 May. 61(131):638-41[↩]
- Heppell J, Farkouh E, Dube S, et al. Toxic megacolon. An analysis of 70 cases. Dis Colon Rectum. 1986 Dec. 29(12):789-92[↩]