Contents
- What is a parathyroidectomy
- What are the parathyroid glands?
- What medications will I be taking after after parathyroidectomy?
- Do I need to donate blood (autologous or designated donor) prior to my surgery?
- Are there any restrictions after parathyroidectomy?
- When can I expect to return to work?
- Are there any dietary restrictions after parathyroidectomy?
- Indications for parathyroidectomy
- Parathyroidectomy surgery
- Parathyroidectomy recovery
- Life after parathyroidectomy
- Parathyroidectomy side effects
- Parathyroidectomy complications
What is a parathyroidectomy
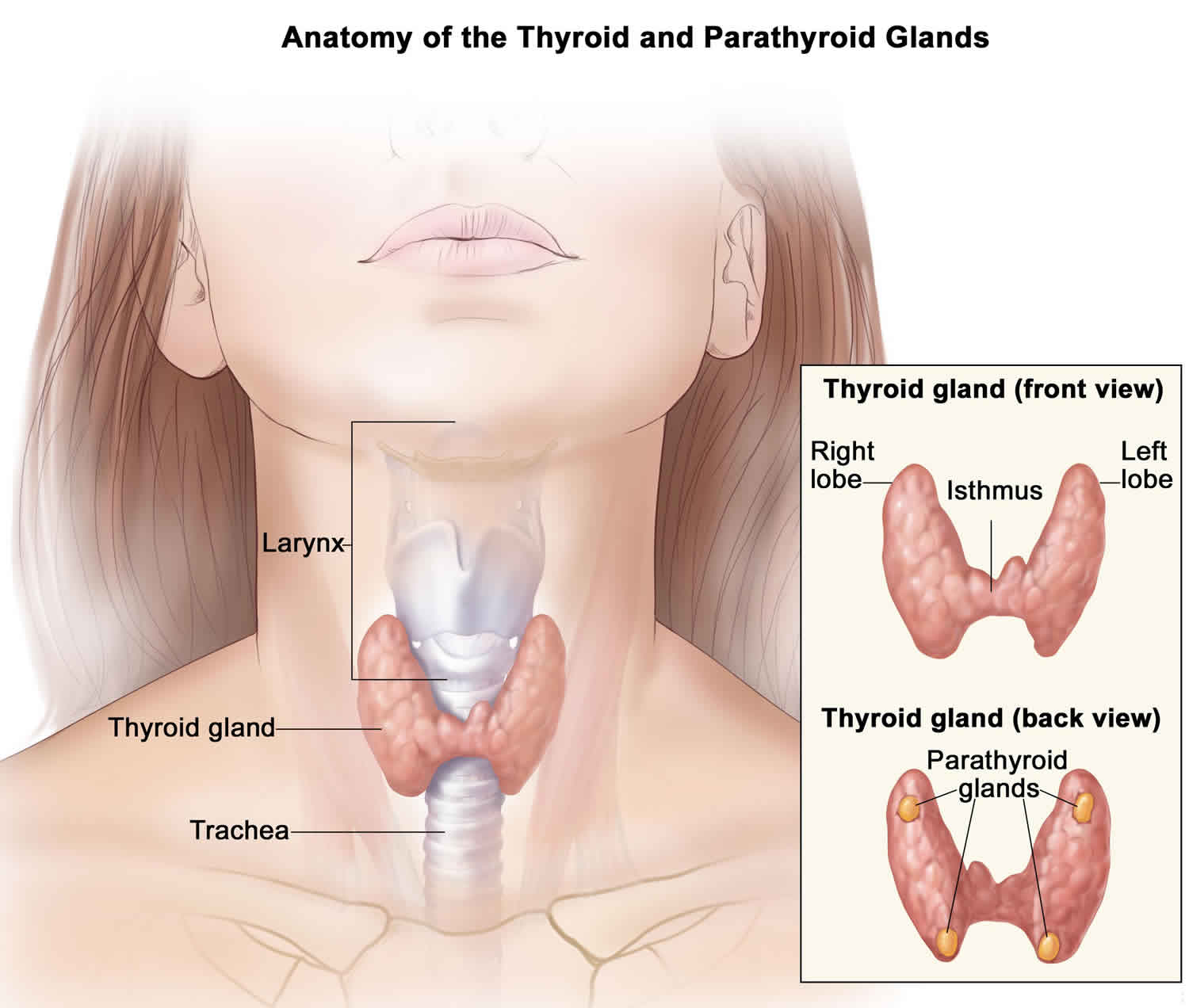
Parathyroidectomy is surgery to remove one or more of the four parathyroid glands in your neck. These small glands make parathyroid hormone (PTH), which controls the amount of calcium in your body. Parathyroid glands are found on the back of the thyroid gland. When they are too active, these glands cause high levels of calcium. This is called hyperparathyroidism. The parathyroid glands also are removed if they contain cancer.
In patients with hyperparathyroidism, one or more parathyroid glands become enlarged and oversecrete parathyroid hormone, causing levels of calcium to rise in the blood.
Parathyroidectomy surgery to remove the enlarged parathyroid gland (or glands) is the only definitive treatment for the disorder and cures it in 95 percent of cases.
The specific type of parathyroidectomy surgery depends on where the diseased parathyroid glands are. Types of parathyroidectomy surgery include:
- Minimally invasive parathyroidectomy. You may receive a shot of a very small amount of radioactive tracer before this surgery. This helps highlight the diseased glands. If you have this shot, your surgeon will use a special probe, like a Geiger counter, to locate the parathyroid gland. Your surgeon will make a small cut (1 to 2 inches; or 2.5 to 5 cm) on one side of your neck, and then remove the diseased gland through it. This procedure takes about 1 hour.
- Video-assisted parathyroidectomy. Your surgeon will make two small cuts in your neck. One is for instruments, and the other is for a camera. Your surgeon will use the camera to view the area and will remove the diseased glands with the instruments.
- Endoscopic parathyroidectomy. Your surgeon will make two or three small cuts in the front of your neck and one cut above the top of your collarbone. This reduces visible scarring, pain, and recovery time. This cut is less than 2 inches (5 cm) long. The procedure to remove any diseased parathyroid glands is similar to video-assisted parathyroidectomy.
With the use of accurate preoperative imaging studies and intraoperative parathyroid hormone measurement, minimally invasive parathyroidectomy via a 2-3 centimeter incision is possible in the majority of cases.
In 85-90% of patients with primary hyperparathyroidism, only one parathyroid gland is abnormal. This allows endocrine surgeons to perform a more limited, focused exploration where there is a high likelihood of having only a single abnormal gland.This approach is referred to as a “minimally invasive parathyroidectomy” and is the most common procedure performed today. The minimally invasive parathyroidectomy procedure has the following advantages for patients:
- Less post-operative pain
- Faster recovery from surgery
- Small or barely visible scar
- Shorter hospital stay
- A more rapid return to work and normal activities
Your surgeon will consider many factors when deciding whether to do parathyroidectomy surgery and what type of surgery would be best for you. Some of these factors are:
- Your age
- Calcium levels in your urine and blood
- Whether you have symptoms
The doctor will take out the parathyroid gland or glands through a cut in the front of your neck. This cut is called an incision. You may have a tube in your neck for 1 to 4 days. The tube drains fluid from the incision.
You may be able to go back to work or your normal routine after a few weeks. This depends on the kind of work you do and how you feel.
Be sure to make and go to all appointments, and call your doctor or nurse call line if you are having problems. It’s also a good idea to know your test results and keep a list of the medicines you take.
What are the parathyroid glands?
Most people have 4 parathyroid glands, which are in your neck and control the balance of calcium in your blood by making parathyroid hormone (PTH). One or more of the parathyroid glands can become overactive, causing an increase in the level of calcium. The most common symptom is bone pain.
What medications will I be taking after after parathyroidectomy?
Your blood calcium will be checked the night of your operation and in the morning following your operation. If your blood calcium level is low following your operation, you may experience hypocalcemia symptoms such as numbness/tingling and muscle cramping. These symptoms are relieved by taking calcium supplements (Tums, Oscal, etc) and, if needed, vitamin D (Rocaltrol). You can take 2 grams of calcium (4 tablets of 500mg Tums) every 4 hours as needed for your symptoms.
If you have persistent tingling despite taking calcium as directed, please call your doctor. Pain medication may be taken as necessary, and is usually only needed for three to four days following parathyroidectomy.
Do I need to donate blood (autologous or designated donor) prior to my surgery?
It is highly unlikely that you will require a blood transfusion during your parathyroidectomy, and therefore not medically necessary to donate (autologous or designated donor) blood prior to your surgery.
Are there any restrictions after parathyroidectomy?
You can resume regular activity as tolerated. Walking outside, going up and down stairs, and performing light activities are all encouraged. Avoid strenuous activity or lifting anything that weighs 10 pounds or more until you feel up to it. If you are feeling well and are not taking any pain medication, you may drive (usually the third or fourth day after surgery).
When can I expect to return to work?
In general, you can return to work when you feel ready, usually within one to two weeks.
Are there any dietary restrictions after parathyroidectomy?
Resume a normal balanced diet as tolerated. Be sure to drink plenty of fluids.
Indications for parathyroidectomy
Parathyroidectomy is recommended when the parathyroid glands produce excessive amounts of parathyroid hormone (hyperparathyroidism). For example, patients with renal, gastrointestinal, or neuromuscular dysfunction 1. In patients with asymptomatic hyperparathyroidism, the National Institute of Health (NIH) has set the following parameters as indications for parathyroidectomy 1:
- Serum calcium 1.0 mg/dL above the upper limit of normal
- A 24-hour urinary calcium greater than 400 mg
- Creatinine clearance reduced by 30%
- Bone mineral density T score less than -2.5 standard deviation at any site
- Age younger than 50 years
Your symptoms should improve after parathyroidectomy. You should have less risk of permanent damage to your bones, kidneys or heart.
Are there any alternatives to parathyroidectomy surgery?
Sometimes you can have medication if the calcium level is not too high or if surgery would be too dangerous because of other medical problems you may have.
Parathyroidectomy surgery
Parathyroid glands are very small. You may need to have tests that show exactly where your glands are. This will help your surgeon find your parathyroid glands during surgery. Preoperative localization allows for the focused exploration and resection of the single offending gland without the need for bilateral four-gland exploration. Frequently utilized imaging modalities include parathyroid technetium-sestamibi (MIBI) scintigraphy, ultrasonography and 4-D computerized tomography (4D-CT). Dual isotope subtraction MIBI scanning with the utilization of single-photon emission computerized tomography (SPECT) and CT fusion has become the localization procedure of choice.
Before surgery, an anesthesiologist will review your medical history with you and decide what type of anesthesia to use. The anesthesiologist is the doctor who will give you the medicine that allows you to sleep and be pain free during surgery and who monitors you during surgery.
Tell your surgeon:
- If you are or might be pregnant
- What medicines, vitamins, herbs, and other supplements you’re taking, even ones you bought without a prescription
Preparing for parathyroidectomy surgery
- Understand exactly what surgery is planned, along with the risks, benefits, and other options.
- Tell your doctors ALL the medicines and natural health products you take. Some of these can increase the risk of bleeding or interact with anesthesia. If you take blood thinners, such as warfarin (Coumadin), clopidogrel (Plavix), or aspirin, be sure to talk to your doctor. He or she will tell you if you should stop taking these medicines before your surgery. Make sure that you understand exactly what your doctor wants you to do.
- Your doctor will tell you which medicines to take or stop before your surgery. You may need to stop taking certain medicines a week or more before surgery. So talk to your doctor as soon as you can.
- If you have an advance care plan, let your doctor know. Bring a copy to the hospital. If you don’t have one, you may want to prepare one. It lets your doctor and loved ones know your health care wishes. Doctors advise that everyone prepare these papers before any type of surgery or procedure.
During the week before your surgery:
- Fill any prescriptions for pain medicine and calcium you’ll need after surgery.
- You may be asked to stop taking blood thinners. These include NSAIDs (aspirin, ibuprofen), vitamin E, warfarin (Coumadin), dabigatran (Pradaxa), rivaroxaban (Xarelto), apixaban (Eliquis), and clopidegrel (Plavix).
- Ask your surgeon which drugs you should still take on the day of your surgery.
What happens on the day of parathyroidectomy surgery?
Follow the instructions exactly about when to stop eating and drinking. If you don’t, your surgery may be cancelled. If your doctor told you to take your medicines on the day of surgery, take them with only a sip of water.
Take a bath or shower before you come in for your surgery. Do not apply lotions, perfumes, deodorants, or nail polish.
Do not shave the surgical site yourself.
Take off all jewellery and piercings. And take out contact lenses, if you wear them.
You will be kept comfortable and safe by your anesthetist.
Parathyroidectomy surgery is usually performed under a general anesthetic. The operation usually takes about an hour, however, the parathyroidectomy surgery may take several hours, depending on how complex it is.
Your surgeon will make a a small horizontal cut usually a 2- to 4-inch (5- to 10-cm) incision on your neck in the line of one of your skin creases just under the Adam’s apple and remove any enlarged parathyroid glands.
During parathyroidectomy surgery:
- The cut is usually made in the center of your neck just under your Adam’s apple.
- Your surgeon will look for the four parathyroid glands and remove any that are diseased.
- You may have a special blood test during surgery that will tell if all the diseased glands were removed. Intraoperative parathyroid hormone (PTH) monitoring has a turnaround time of approximately 30 minutes or less and can therefore be utilized in the operating room to confirm resection of the offending parathyroid adenoma by demonstrating a rapid decline in parathyroid hormone (PTH) levels. This allows for highly accurate confirmation of surgical cure without the need for four-gland cervical exploration in patients with single adenomas. The accuracy of intraoperative parathyroid hormone (PTH) measurement has been widely verified and enthusiastically supported.
- In rare cases, when all four of these glands need to be removed, part of one is transplanted into the forearm. Or, it is transplanted into a muscle in the front of your neck next to the thyroid gland. This helps ensure your body’s calcium level stays at a healthy level.
After parathyroidectomy surgery, complete healing without complications usually occurs within 4 weeks. The long term outlook is excellent.
Parathyroidectomy recovery
You should be able to go home after 1 to 2 days. Recovery may be fastest when less invasive techniques are used.
You should be able to return to work and normal activities after about 2 weeks. It will take about 1 to 3 weeks for you to fully heal.
Regular exercise should help you to return to normal activities as soon as possible. Before you start exercising, ask the healthcare team or your doctor for advice.
A normal gland that was not removed may become overactive in the future.
You may leave the hospital with stitches in the cut the doctor made (incision). Your doctor will tell you if you need to come back to have these removed. You may still have a tube called a drain in your neck. Your doctor will take this out a few days after your surgery.
Going home
Be sure you have someone to drive you home. Anesthesia and pain medicine make it unsafe for you to drive.
You will be given more specific instructions about recovering from your surgery. They will cover things like diet, wound care, follow-up care, driving, and getting back to your normal routine.
You may have some trouble chewing and swallowing after you go home. Your voice probably will be hoarse, and you may have trouble talking. For most people, these problems get better within a few weeks, but it can take longer. In some cases, parathyroidectomy surgery causes permanent problems with chewing, speaking, or swallowing.
Wound care
- If your doctor told you how to care for your incision, follow your doctor’s instructions. If you did not get instructions, follow this general advice:
- After the first 24 to 48 hours, wash around the incision with clean water 2 times a day. Don’t use hydrogen peroxide or alcohol, which can slow healing.
- You may have a drain near your incision. Your doctor will tell you how to take care of it.
Medicines
- Your doctor will tell you if and when you can restart your medicines. He or she will also give you instructions about taking any new medicines.
- If you take blood thinners, such as warfarin (Coumadin), clopidogrel (Plavix), or aspirin, be sure to talk to your doctor. He or she will tell you if and when to start taking those medicines again. Make sure that you understand exactly what your doctor wants you to do.
- Take pain medicines exactly as directed.
- If the doctor gave you a prescription medicine for pain, take it as prescribed.
- If you are not taking a prescription pain medicine, ask your doctor if you can take an over-the-counter medicine.
- If you think your pain medicine is making you sick to your stomach:
- Take your medicine after meals (unless your doctor has told you not to).
- Ask your doctor for a different pain medicine.
- Your doctor may prescribe calcium to prevent problems after surgery from low calcium. Not having enough calcium can cause symptoms such as tingling around your mouth or in your hands and feet.
- Your doctor may have prescribed antibiotics. Take them as directed. Do not stop taking them just because you feel better. You need to take the full course of antibiotics.
Call your local emergency services number anytime you think you may need emergency care. For example, call if:
- You passed out (lost consciousness).
- You have sudden chest pain and shortness of breath, or you cough up blood.
- You have severe trouble breathing.
Call your doctor or seek immediate medical care if:
- You have loose stitches, or your incision comes open.
- You have blood leaking from your incision.
- You have signs of infection, such as:
- Increased pain, swelling, warmth, or redness.
- Red streaks leading from the incision.
- Pus draining from the incision.
- A fever.
- You have a tingling feeling around your mouth.
- You have cramping or tingling in your hands and feet.
Watch closely for changes in your health, and be sure to contact your doctor if:
- You have trouble talking.
- You are sick to your stomach or cannot keep fluids down.
- You do not have a bowel movement after taking a laxative.
Parathyroidectomy diet
- If swallowing is painful, start out with cold drinks, flavored ice pops, and ice cream. Next, try soft foods like pudding, yogurt, canned or cooked fruit, scrambled eggs, and mashed potatoes. Avoid eating hard or scratchy foods like chips or raw vegetables. Avoid orange or tomato juice and other acidic foods that can sting the throat.
- If you cough right after drinking, try drinking thicker liquids, such as a smoothie.
- You may notice that your bowel movements are not regular right after your surgery. This is common. Try to avoid constipation and straining with bowel movements. You may want to take a fiber supplement every day. If you have not had a bowel movement after a couple of days, ask your doctor about taking a mild laxative.
Activity
- Rest when you feel tired. Getting enough sleep will help you recover. When you lie down, put two or three pillows under your head to keep it raised.
- Try to walk each day. Start by walking a little more than you did the day before. Bit by bit, increase the amount you walk. Walking boosts blood flow and helps prevent pneumonia and constipation.
- Avoid strenuous physical activity and lifting heavy objects for 3 weeks after surgery or until your doctor says it is okay.
- Do not over-extend your neck backwards for 2 weeks after surgery.
- Ask your doctor when you can drive again.
- You may take a shower, unless you still have a drain. Pat the incision dry. If you have a drain coming out of your incision, follow your doctor’s instructions to care for it.
Life after parathyroidectomy
Call your surgeon if you have any numbness or tingling around your mouth in the 24 to 48 hours after surgery. This is caused by low calcium. Follow instructions about how to take your calcium supplements.
After this procedure, you should have routine blood tests to check your calcium level.
Sometimes, another surgery is needed to remove more of the parathyroid glands.
Parathyroidectomy side effects
Risks for anesthesia and surgery in general are:
- Reactions to medicines or breathing problems
- Bleeding, blood clots, or infection
Risks for parathyroidectomy are:
- Injury to the thyroid gland or the need to remove part of the thyroid gland.
- Hypoparathyroidism. This can lead to low calcium levels that are dangerous to your health.
- Injury to the nerves going to the muscles that move your vocal cords. You may have a hoarse or weaker voice which could be temporary or permanent.
- Difficulty breathing. This is very rare and almost always goes away several weeks or months after surgery.
Parathyroidectomy complications
Parathyroidectomy should be a relatively straightforward surgical procedure devoid of complications when carried out by an endocrine surgeon with appropriate training 2. Complications relating to the wound and damage caused to nearby structures should be of very low incidence. Complications relating to operative strategy, pathology (hyperplastic disease versus multiple adenomas) and failure to find an adenoma are much more complex and difficult to correct.
General complications
- pain
- infection of the surgical site (wound)
- unsightly scarring
- blood clots
Specific complications
- Bleeding. There is a 1/300 risk of bleeding with your operation. This is the main reason you stay overnight in the hospital.
- Recurrent laryngeal nerve injury
- Superior laryngeal nerve injury
- Change in your voice
- Breathing difficulties
- Drop in calcium levels (hypocalcemia)
- Failure of the operation or persistent disease
Post parathyroidectomy problems
Recurrent laryngeal nerve injury
Recurrent laryngeal nerve controls your vocal cords and if injured you will have a hoarse voice. There is a 1% chance of permanent hoarseness and a 5% chance of temporary hoarseness (<6months).
The recurrent laryngeal nerve will be vulnerable to injury when dissection and removal of adenomas occurs close to the branches of the inferior thyroid artery 2. The development of an intraneural hematoma can readily occur through disruption of the fine feeding vessels which run throughout the substance of the nerve. The nerve is especially vulnerable in removal of superior adenomas which “grow” inferiorly and “drop into” the upper posterior mediastinum behind the inferior thyroid artery 3.
Golden rules to help avoid nerve injury are:
- Stay close to the adenoma surface during dissection.
- Be exceedingly careful if diathermy is used – remember the circumference of thermal injury extends well beyond the points of the forceps, especially if monopolar diathermy is used.
- Be thoroughly conversant with the course of the nerve and if the adenoma overlies or comes in close proximity be sure that the nerve is seen and preserved throughout mobilization and dissection.
- Do not sling the nerve on tapes or threads and avoid handling or palpating the nerve.
Superior laryngeal nerve injury
Superior laryngeal nerve will be vulnerable in dissections close to the upper thyroid pole. Adenomas will not be close to the main nerve trunk but the external branch (to the cricothyroid muscle) might be damaged, especially if a superior adenoma is closely applied to the upper thyroid pole or entwined within superior thyroid vessels 2. Carefully develop the space between the medial surface of the upper pole and the cricothyroid muscle and, if superior thyroid vessels have to be divided to allow access to the adenoma, be sure to divide them individually and on the surface of the thyroid gland and not above the upper pole.
Persistent disease
If hypercalcemia persists after first exploration then the diagnosis of primary hyperparathyroidism has to be reconfirmed by establishing (a) positive or confirmatory markers such as inappropriately high parathyroid hormone (PTH), hypercalciuria, hypophosphataemia, etc, and (b) negative markers – be sure to have excluded familial hypocalciuric hypercalcemia and occult malignancy or other causes of hypercalcemia.
If a diagnosis of persistent primary hyperparathyroidism is confirmed then be sure that the patient warrants re-exploration with its attendant increased morbidity. For example, you might not wish to re-explore the neck of an 85 year old woman with cerebro-vascular disease and mild asymptomatic hypercalcemia. You would want to re-explore a 35 year old man with a serum calcium of 3.00 mmol/l who continues to produce renal calculi. If the diagnosis is confirmed and re-exploration is warranted then localization should be carried out before surgery. The operation note should be reviewed to see if the localization coincides with a likely uncovered adenoma. For example – if three normal glands had been found but the left inferior gland had not been seen and Sestimibi and MRI scans suggest a mediastinal gland in the upper left quadrant, then exploration should be directed initially in this area. The adenoma is likely to be in the upper horn of the left thymic lobe.
The histopathology and frozen section reports pertaining to the first exploration must be reviewed. Frozen section errors “allow” premature and in approprite cessation of exploration. Failure to recognize hyperplasia on frozen section, for example, leads to inadequate resection. A false call of an adenoma instead of hyperplasia “allows” three hyperplastic glands to remain in situ 4. More appropriate surgery would have been 3_ gland resection. Surgical errors “allow” multiple adenomas to be left in situ because the condition is not known about or because not all glands were visualized. A danger of scan directed unilateral neck exploration is that in 10% of patients the existence of hyperplasia and/or double or multiple adenomas will not be recognized by preoperative scans or by the surgeon only opening one compartment of the neck 5.
Low blood calcium (hypocalcemia)
Currently most surgeons remove only the abnormal parathyroid gland(s) and at most might take a sliver biopsy of one of the other glands. The other parathyroid glands can, of course, be inadvertently bruised or devascularized, thereby leading to hypocalcemia. This would require you to take calcium and vitamin D supplementation. There is a 1% chance of permanent calcium supplementation and 5% chance of temporary calcium supplementation.
Further contributions to the incidence and severity of hypocalcemia include the atrophy of residual parathyroid glands in the face of a single hyperfunctioning adenoma (especially if there has been longstanding and significant hypercalcemia), so called hungry bone syndrome and previous parathyroid or thyroid surgery 2. It may need treating with vitamin D and/or calcium supplements. Very rarely a patient may need vitamin D and calcium supplements in the long term especially after reoperative parathyroid surgery or after resection of multiple gland disease 6.
- Wolfe SA, Fingeret A. Parathyroid Minimally Invasive Surgery. [Updated 2019 Mar 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507834[↩][↩]
- Farndon JR. Postoperative complications of parathyroidectomy. In: Holzheimer RG, Mannick JA, editors. Surgical Treatment: Evidence-Based and Problem-Oriented. Munich: Zuckschwerdt; 2001. Available from: https://www.ncbi.nlm.nih.gov/books/NBK6967[↩][↩][↩][↩]
- Sinclair I S R. The risk to the recurrent laryngeal nerves in thyroid and parathyroid surgery. JR Coll Surg Edinb. (1994);39:253–257[↩]
- Thompson N W, Sandelin K. Primary hyperparathyroidism caused by multiple gland disease (hyperplasia) long-term results in familial and sporadic cases. Acta Chir Aust. (1994);26 (S112):44–47.[↩]
- Szabo E, Lundgren E, Juhlin C, Ljunghall S, Akerstrom G, Rastad J. Double parathyroid adenoma, a clinically nondistinct entity of primary hyperparathyroidism. World J Surg. (1998);22:708–713[↩]
- Wong W K, Wong N A C S, Farndon J R. Early postoperative plasma calcium concentration as a predictor of the need for calcium supplement after parathyroidectomy. Br J Surg. (1996);83:532–534.[↩]