Contents
What is esophageal manometry
Esophageal manometry test also called esophageal testing, measures the pressures, motility, function and the pattern of muscle contractions in your esophagus and lower esophageal sphincter (LES). A tube is usually inserted through your nose and passed into the esophagus. The pressure of the esophageal sphincter muscle is recorded and also the contraction waves of swallowing are recorded. Abnormalities in the contractions and strength of the muscle or in the sphincter at the lower end of the esophagus can result in pain, heartburn, and/or difficulty swallowing. Esophageal manometry is used to diagnose the conditions that can cause these symptoms.
Esophageal manometry test can also help evaluate swallowing disorders.
During the esophageal manometry test, you may experience some discomfort in your nose and/or throat. Esophageal manometry test will take approximately 30 minutes to complete and the results will be sent to your doctor’s office.
Risks of esophageal manometry test include:
- Slight nosebleed
- Sore throat
- Hole, or perforation, in the esophagus (this rarely happens)
The esophagus
The esophagus is a muscular tube that connects your throat to your stomach. With each swallow, the esophagus muscle contracts and pushes food into the stomach. At the lower end of the esophagus, a valve (a special sphincter muscle) remains closed except when food or liquid is swallowed or when you belch or vomit.
Figure 1. Esophagus
Why the esophageal manometry test is performed?
The esophagus is the tube that carries food from your mouth into the stomach. When you swallow, muscles in your esophagus squeeze (contract) to push food toward the stomach. Valves, or sphincters, inside the esophagus open to let food and liquid through. They then close to prevent food, fluids, and stomach acid from moving backward. The sphincter at the bottom of the esophagus is called the lower esophageal sphincter (LES).
Esophageal manometry is done to see if the esophagus is contracting and relaxing properly. The test helps diagnose swallowing problems. During the test, the doctor can also check the lower esophageal sphincter to see if it opens and closes properly.
Esophageal manometry test may be ordered if you have symptoms of:
- Heartburn or nausea after eating (gastroesophageal reflux disease, or GERD)
- Problems swallowing (feeling like food is stuck behind the breast bone)
Does esophageal manometry test hurt?
You may have a gagging sensation and discomfort when the tube passes through your nose and throat. You may also feel discomfort in your nose and throat during the test.
Esophageal manometry study preparation
An empty stomach allows for the best and safest examination, so do not eat or drink anything for 6 to 8 hours before the esophageal manometry test. Since many medications can affect esophageal pressure and the natural muscle contractions required for swallowing, be sure to discuss with your healthcare professional each medication you are taking. Your doctor may ask that you temporarily stop taking one or more medications before your test.
Esophageal manometry procedure
During esophageal manometry, a thin, flexible, pressure-sensitive tube is passed through your nose, down the esophagus, and into your stomach while you swallow sips of water.
Before the procedure, you receive numbing cream medicine inside your nostrils. This helps make the insertion of the tube less uncomfortable.
Mild, brief gagging may occur while the tube is passed through the throat. When the tube is in position, you will be sitting upright or lying on your back while the tube is connected to a computer.
After the tube is in the stomach, the tube is pulled slowly back into your esophagus. At this time, you are asked to swallow. The pressure of the muscle contractions is measured along several sections of the tube.
While the tube is in place, other studies of your esophagus may be done. The tube is removed after the tests are completed. The test takes about 30 minutes to complete.
What can I expect after the test?
After the esophageal manometry test, you may experience mild sore throat, stuffy nose, or a minor nosebleed; all typically improve within hours. Unless your physician has given you other instructions, you may resume normal meals, activities, and any interrupted medications.
Esophageal manometry results
Normal results
The lower esophageal sphincter (LES) pressure and muscle contractions are normal when you swallow.
Abnormal results may indicate:
- A problem with the esophagus that affects its ability to move food toward the stomach (achalasia)
- A weak lower esophageal sphincter (LES), which causes heartburn (GERD)
- Abnormal contractions of the esophagus muscles that do not effectively move food to the stomach (esophageal spasm)
Esophageal manometry interpretation
Interpretation of an esophageal manometry study requires interaction with software-generated esophageal pressure topography plots in order to examine manometric properties during the baseline period and each swallow, and synthesize these data to produce an esophageal motility diagnosis 1.
Table 1. Pressure topography metrics utilized in the Chicago Classification v3.0. Unless otherwise specified, pressures are referenced to atmospheric. Metrics are listed alphabetically.
| Pressure Topography Metrics | |
|---|---|
| CDP (time, position)* Contractile Deceleration Point | Inflection point along the 30 mmHg isobaric contour (or pressure greater than intrabolus pressure in instances of compartmentalized pressurization) at which propagation velocity slows, demarcating peristalsis from ampullary emptying. The CDP must be localized within 3 cm of the proximal margin of the LES |
| DCI (mmHg·s·cm)† Distal Contractile Integral | Amplitude x duration x length (mmHg·s·cm) of the distal esophageal contraction exceeding 20 mmHg from the transition zone to the proximal margin of the LES (Clouse, 2nd and 3rd contractile segments) § |
| DL (s)* Distal Latency | Interval between UES relaxation and the CDP |
| IRP (mmHg)† Integrated Relaxation Pressure | Mean of the 4s of maximal deglutitive relaxation in the 10-s window beginning at UES relaxation. Contributing times can be contiguous or non-contiguous (eg interrupted by diaphragmatic contraction). Referenced to gastric pressure. |
Footnote:
*Normal values are independent of the manometric hardware utilized
†Normal values are dependent on the specific manometric hardware utilized
§In instances of suspected hypercontractility involving the LES, or even restricted to the LES, the DCI box should include the LES (Clouse, 4th contractile segment) as well
Abbreviations: CD= crural diaphragm; CDP = contractile deceleration point; EGJ= esophagogastric junction; UES= upper esophageal sphincter
[Source 2 ]Table 2. Pressure topography baseline esophagogastric junction (EGJ) morphology and tone derived from an overview of the study.
| Esophagogastric junction (EGJ) | ||
|---|---|---|
| EGJ morphology | Type I: | Complete overlap of CD and LES components with single peak on the spatial pressure variation plot |
| Type II: | Double-peaked pressure zone with the inter-peak nadir pressure greater than gastric pressure and a separation of 1–2 cm between peaks. This can vary or be present intermittently in which case the report should mention the range of observed LES-CD separation | |
| Type IIIa: | Double-peaked pressure zone with the inter-peak nadir pressure less than or equal to gastric pressure, but the pressure inversion point remains at the CD level. The range of observed LES-CD separation is reported | |
| Type IIIb: | Double-peaked pressure zone with the inter-peak nadir pressure equal to gastric pressure and the pressure inversion point at the LES level. The range of observed LES-CD separation is reported | |
| LES-CD separation | The EGJ pressure profile on a spatial pressure variation plot at peak inspiration can be a single or double peak. If a single peak, the LES-CD separation is 0; if a double peak, LES-CD separation is the axial distance between peaks | |
| Inspiratory EGJ pressure | Average of maximal inspiratory EGJ pressure reached during 3 respiratory cycles, ideally in a quiescent portion of recording, free of swallows | |
| Expiratory EGJ pressure | Average EGJ pressure midway between adjacent inspirations for 3 respiratory cycles, ideally in a quiescent portion of recording, free of swallows | |
Abbreviations: CD= crural diaphragm; CDP = contractile deceleration point; EGJ= esophagogastric junction; UES= upper esophageal sphincter
[Source 2 ]Table 3. Defintion of High resolution manometry metrics form the basis of the Chicago Classification
| Assessment | Metric | Classification | Definition |
|---|---|---|---|
| Contractile Vigor | Distal Contractile Integral |
|
|
| Latency Interval | Distal latency* |
|
|
| Peristaltic Integrity | Peristaltic break in 20mmHg isobaric contour* |
|
|
| Pressurization pattern | Pressurization in 30mmHg isobaric contour |
|
|
Footnote: A swallow is ineffective if either failed or weak.
*A distal contractile integral > 450 mmHg·s·cm is required for assessment of distal latency and peristaltic integrity.
Esophagogastric junction (EGJ); Upper esophageal sphincter (UES); Crural diaphragm (CD); Lower esophageal sphincter (LES).
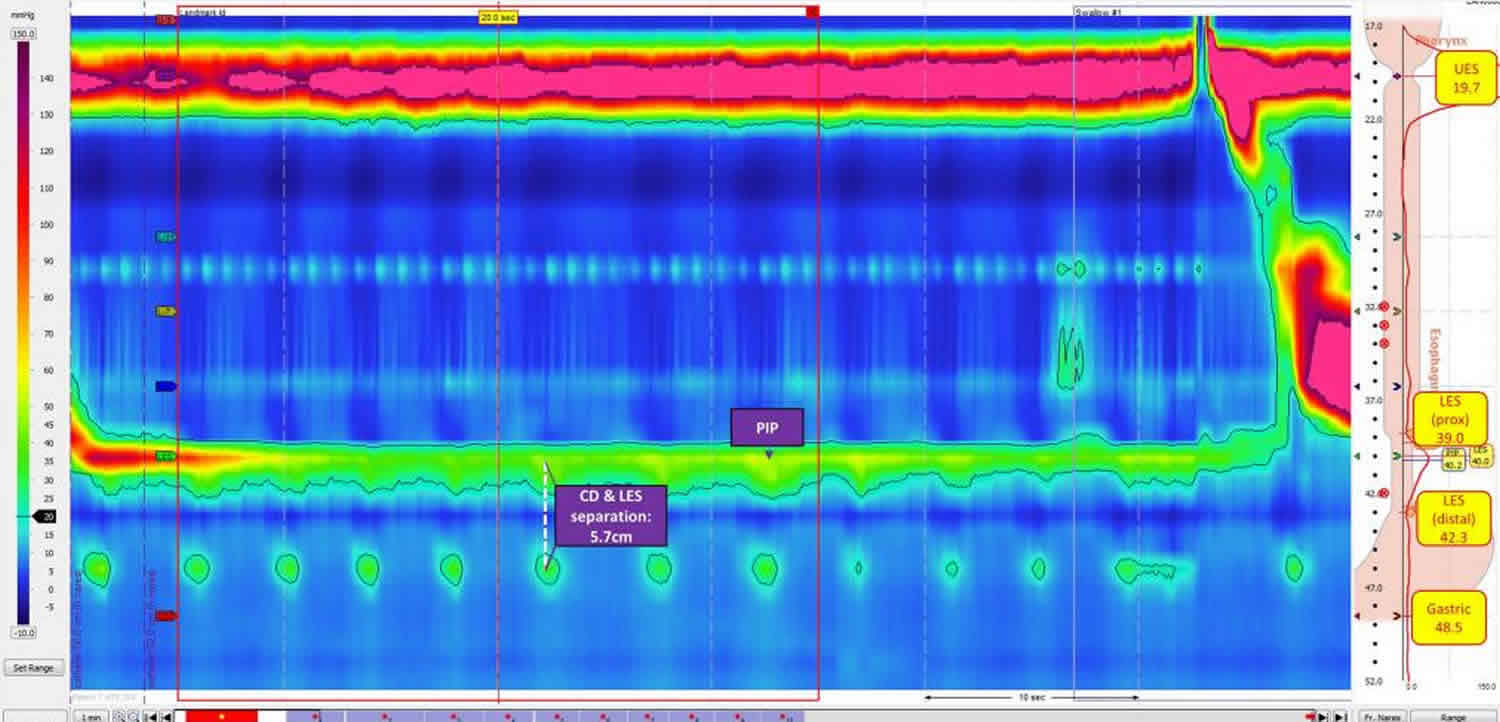
[Source 1 ]Baseline Assessment
Within the baseline window, the interpreter will position baseline landmarks, examine upper esophageal sphincter (upper esophageal sphincter) characteristics and basal esophagogastric junction pressures, identify the pressure inversion point ( pressure inversion point), and assess esophagogastric junction morphology (Figure 2) in order to gather important information regarding anatomic profiles and resting pressures 3.
The pressure inversion point (PIP) indicates the point of transition from the intraabdominal cavity to the intrathoracic cavity, and is manometrically displayed by an inverse directionality of the intraabdominal and intrathoracic pressure signals which magnifies with deep inspiration. The pressure inversion point is absent in cases where the manometry catheter does not traverse the lower esophageal sphincter (LES). Additionally, cases of a looped catheter in the esophageal body may manifest as a “butterfly” or mirror image. Assessment and documentation of the pressure inversion point is essential to esophageal manometry interpretation as the absence of the pressure inversion point indicates a technically inadequate study 3.
An added value of esophageal manometry is the ability to assess the spatial relationship between the crural diaphragm and lower esophageal sphincter (LES), referred to as the esophagogastric junction morphology. According to the Chicago Classification 3.0, there are three esophagogastric junction morphology type: type I indicates absence of hiatal hernia, type II indicates a small hernia and type III indicates a hiatal hernia greater than 2 cm and is further classified as type IIIa and IIIb based on pressure inversion point location 4.
Figure 2. Esophageal manometry baseline assessment
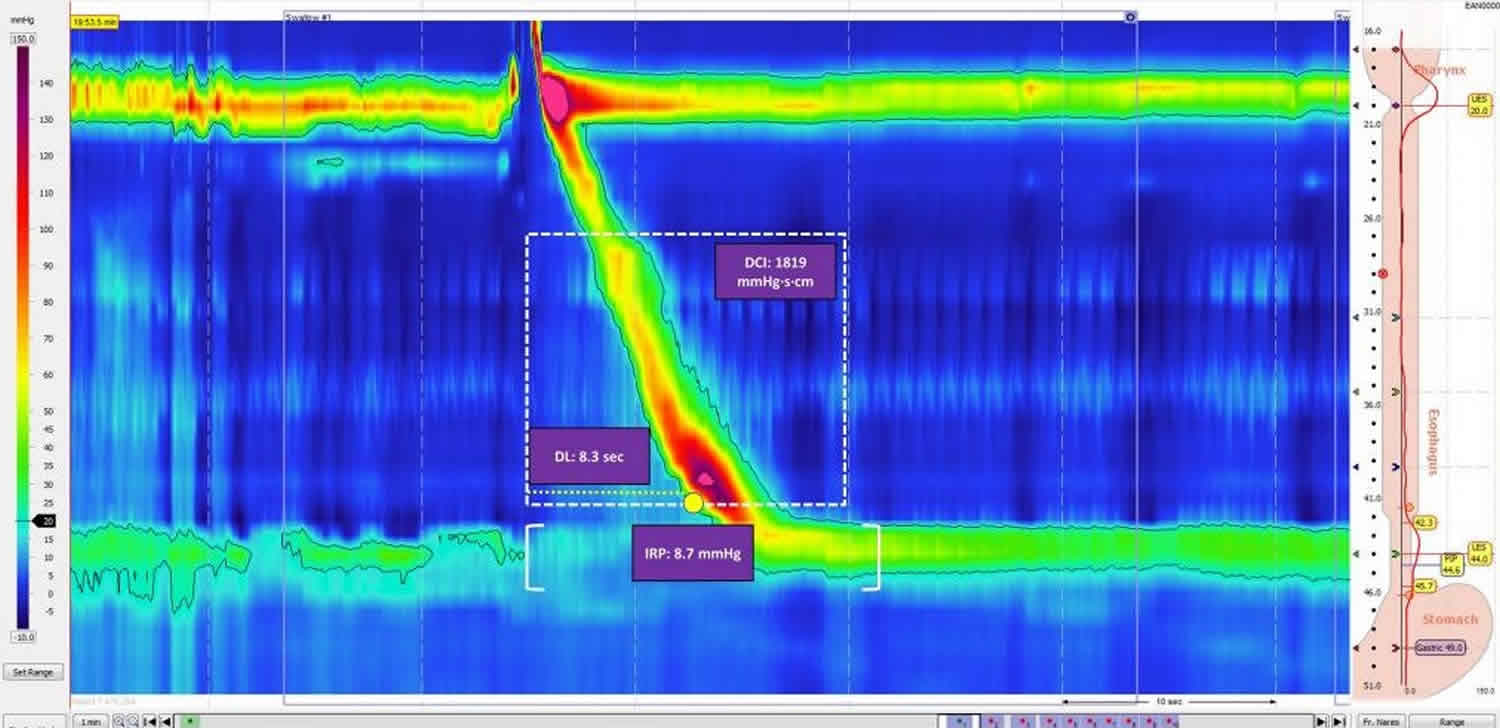
Swallow Assessment
Motility patterns during swallows provide valuable information about esophageal contractility and sphincter relaxation in response to bolus. Diagnosis of an esophageal motility disorder requires assessment of the integrated relaxation pressure (IRP), contractile function, and pressurization (Figure 3).
Figure 3. Esophageal manometry swallow assessment
[Source 1 ]Integrated Relaxation Pressure
The integrated relaxation pressure is the most discriminatory esophageal manometry metric according to the Chicago Classification. The integrated relaxation pressure is a measure of deglutitive relaxation based on four seconds of the lowest mean axial pressure, continuous or discontinuous, across the LES during the 10-second period after a swallow. An abnormal integrated relaxation pressure indicates abnormal transit across the esophagogastric junction 5. According to the Chicago Classification 3.0, the overall integrated relaxation pressure is expressed as the median integrated relaxation pressure of ten wet swallows 6. The reported range for normal integrated relaxation pressures differs across manometric systems. With the Sierra system (Sierra Scientific Instruments) integrated relaxation pressure values above 15mmHg indicate an esophagogastric junction outflow obstruction. However, in the setting of absent peristalsis, an integrated relaxation pressure cutoff of 10mmHg may indicate type I achalasia. In addition, absent peristalsis with at least 20% of swallows with panesophageal pressurization should raise suspicion for type II achalasia regardless of integrated relaxation pressure 7. Thus, the integrated relaxation pressure is an important metric to assess adequacy of esophagogastric junction relaxation, however integrated relaxation pressure values vary with different patterns of contractility and among manufacturers.
Contractile Function
Esophageal manometry assessment of esophageal contractile function is based on the distal contractile integral (DCI), distal latency (DL) and peristaltic integrity. The distal contractile integral measures the vigor of peristalsis in the smooth muscle esophagus. The distal contractile integral is determined by summing pressures exceeding 20mmHg within the time/length field spanning the smooth muscle transition zone to the proximal aspect of the esophagogastric junction. distal contractile integral values are calculated as units of mmHg·s·cm. According to Chicago Classification 3.0, a distal contractile integral greater than 8,000 mmHg·s·cm indicates hypercontractility, whereas distal contractile integral values below 450 mmHg·s·cm signify weak peristalsis, with values below 100 mmHg·s·cm representing a failed swallow. distal contractile integral values between 450 to 8000 mmHg·s·cm are within normal range, though values at the upper limit of normal (5,000 to 8,000 mmHg·s·cm) may indicate a degree of increased contractile vigor 8. Latency and peristaltic integrity should only be assessed in the context of distal contractile integral values above 450 mmHg·s·cm.
The distal latency is a time measurement from the start of swallow-induced upper esophageal sphincter opening to arrival of esophageal contraction at the contractile deceleration point, the inflection point in the wavefront velocity proximal to the esophagogastric junction. A swallow is considered premature or spastic if the distal latency is less than 4.5 seconds. 6,19 Borderline normal distal latency values (e.g., 4.5 to 5.5 seconds) may indicate a spastic disorder in evolution.
Peristaltic integrity is evaluated by the presence of spatial breaks or gaps in the peristaltic contraction across the upper esophageal sphincter to the esophagogastric junction under a 20mmHg isobaric contour. According to Chicago Classification v3.0, breaks longer than 5cm indicate a fragmented swallow 8.
Esophageal Pressurization
An added advantage of esophageal manometry is the ability to assess intrabolus pressurization patterns. Esophageal pressurization occurs when swallowed liquid is trapped between two contracting segments of the esophagus, and is abnormal when pressurization exceeds 30mmHg. Pressurization spanning the upper esophageal sphincter to the esophagogastric junction is considered panesophageal pressurization, and is the defining feature of type II achalasia. Compartmentalized pressurization extending from the contractile deceleration point to the esophagogastric junction may indicate a distal outflow obstruction. esophagogastric junction pressurization spanning the zone between the LES and crural diaphragm may be encountered with a hiatal hernia 8.
Esophageal manometry risks
As with any medical procedure, there are certain risks. While serious side effects of esophageal manometry procedure are extremely rare, it is possible that you could experience irregular heartbeats, aspiration (when stomach contents flow back into the esophagus and are breathed into the lung), or perforation (a hole in the esophagus). During insertion, the tube may be misdirected into the windpipe before being repositioned. Precautions are taken to prevent such risks, and your physician believes the risks are outweighed by the benefits of this test.
- Yadlapati R. High-resolution esophageal manometry: interpretation in clinical practice. Curr Opin Gastroenterol. 2017;33(4):301–309. doi:10.1097/MOG.0000000000000369 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5568812/[↩][↩][↩][↩]
- Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2014;27(2):160–174. doi:10.1111/nmo.12477 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4308501/[↩][↩]
- Gyawali CP, Patel A. Esophageal motor function: technical aspects of manometry. Gastrointest Endosc Clin N Am. 2014;24:527–43[↩][↩]
- Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–74. Chicago Classification version 3.0 is the most recently updated version of the Chicago Classification, the analytic scheme for esophageal motility disorders based on high-resolution manometry.[↩]
- Ghosh SK, Pandolfino JE, Rice J, Clarke JO, Kwiatek M, Kahrilas PJ. Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitative analysis of 400 patients and 75 controls. Am J Physiol Gastrointest Liver Physiol. 2007;293:G878–85[↩]
- Roman S, Gyawali CP, Xiao Y, Pandolfino JE, Kahrilas PJ. The Chicago classification of motility disorders: an update. Gastrointest Endosc Clin N Am. 2014;24:545–61[↩]
- Lin Z, Kahrilas PJ, Roman S, Boris L, Carlson D, Pandolfino JE. Refining the criterion for an abnormal Integrated Relaxation Pressure in esophageal pressure topography based on the pattern of esophageal contractility using a classification and regression tree model. Neurogastroenterol Motil. 2012;24:e356–63.[↩]
- Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–74. Chicago Classification version 3.0 is the most recently updated version of the Chicago Classification, the analytic scheme for esophageal motility disorders based on high-resolution manometry[↩][↩][↩]