Contents
What is a fecal occult blood test
A fecal occult blood test (FOBT) also called guaiac fecal occult blood test (gFOBT) or fecal immunochemical test (FIT), looks at a sample of your poop (feces) to check for blood. Occult blood means that you can’t see it with the naked eye. Blood in the stool means there is likely some kind of bleeding in the digestive tract. It may be caused by a variety of conditions, including:
- Polyps
- Hemorrhoids
- Diverticulosis
- Ulcers
- Colitis, a type of inflammatory bowel disease
- Cancer
Blood in the stool may also be a sign of colorectal cancer, a type of cancer that starts in the colon or rectum. Colorectal cancer is the second leading cause of cancer-related deaths in the United States and the third most common cancer in men and in women. A fecal occult blood test is a screening test that may help find colorectal cancer early, when treatment is most effective.
Many people find these fecal occult blood tests easier to have than tests like colonoscopy, and fecal occult blood tests are typically done at home. But fecal occult blood tests need to be done more often. And if the result from one of these fecal occult blood tests is positive (abnormal), you’ll still need a colonoscopy to see if you have cancer.
Are there any risks to the home fecal occult blood test?
There is no known risk to having a fecal occult blood test.
Is there anything else I need to know about a fecal occult blood test?
Regular colorectal cancer screenings, such as the fecal occult blood test, are an important tool in the fight against cancer. Studies show that screening tests can help find cancer early, and may reduce deaths from the disease.
What is fecal occult blood test used for?
A fecal occult blood test is used as an early screening test for colorectal cancer. Fecal occult blood test (FOBT) may also be used to diagnose other conditions that cause bleeding in the digestive tract.
Types of fecal occult blood test
Fecal immunochemical test
One way to test for colorectal cancer is to look for occult (hidden) blood in stool. The idea behind this type of test is that blood vessels in larger colorectal polyps or cancers are often fragile and easily damaged by the passage of stool. The damaged vessels usually bleed into the colon or rectum, but only rarely is there enough bleeding for blood to be seen in the stool.
The fecal immunochemical test (FIT) is also called an immunochemical fecal occult blood test (iFOBT). It tests for hidden blood in the stool. This test reacts to part of the human hemoglobin protein, which is found in red blood cells.
For this test, small amounts of stool are collected on cards (or in tubes). You can do this in the privacy of your own home. Unlike the guaiac-based fecal occult blood test (gFOBT) (see below), there are no drug or dietary restrictions before the test (as vitamins and foods do not affect the fecal immunochemical test), and collecting the samples may be easier. This test is also less likely to react to bleeding from other parts of the digestive tract, such as the stomach.
This test must be done every year, unlike some other tests.
If the test results are positive (that is, if hidden blood is detected), a colonoscopy will be needed to investigate further. Although blood in the stool can be from cancers or polyps, it can also have other causes, such as ulcers, hemorrhoids, or other conditions.
Collecting the samples:
Be sure to follow the instructions that come with your kit, as different kits might have different instructions. Your health care provider will give you the supplies you need for testing. Have all of your supplies ready and in one place. Supplies typically include a test kit, test cards or tubes, long brushes or other collecting devices, waste bags, and a mailing envelope. The kit will give you detailed instructions on how to collect the samples. If you have any questions about how to use your kit, contact your health care provider’s office or clinic. Once you have collected the samples, return them as instructed in the kit.
Guaiac-based fecal occult blood test
The guaiac-based fecal occult blood test (gFOBT) detects occult (hidden) blood in the stool through a chemical reaction, in a different way than a fecal immunochemical test (FIT). But like the fecal immunochemical test (FIT), this test can’t tell if the blood is from the colon or from other parts of the digestive tract (such as the stomach).
The American Cancer Society recommends the more modern, highly sensitive versions of this test for screening.
This test must be done every year, unlike some other tests.
This test is done with a kit that you can use in the privacy of your own home that allows you to check more than one stool sample. A fecal occult blood test done during a digital rectal exam in the doctor’s office (which only checks one stool sample) is not enough for proper screening, as it is likely to miss most colorectal cancers.
If the test results are positive (that is, if hidden blood is detected), a colonoscopy will be needed to find the reason for the bleeding. It’s not enough to simply repeat this test or follow up with tests other than a colonoscopy.
Before the guaiac-based fecal occult blood test (gFOBT)
Some foods or drugs can affect the results of guaiac-based fecal occult blood test (gFOBT), so you may be instructed to avoid the following before this test:
- Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil), naproxen (Aleve), or aspirin, for 7 days before testing. (They can cause bleeding, which can lead to a false-positive result.) Note: People should try to avoid taking NSAIDs for minor aches prior to the test. But if you take these medicines daily for heart problems or other conditions, don’t stop them for this test without talking to your health care provider first.
- Vitamin C in excess of 250 mg daily from either supplements or citrus fruits and juices for 3 days before testing. (This can affect the chemicals in the test and make the result negative, even if blood is present.)
- Red meats (beef, lamb, or liver) for 3 days before testing. (Components of blood in the meat may cause a positive test result.)
Some people who are given the test never do it or don’t return it because they worry that something they ate may affect the test. Even if you are concerned that something you ate may alter the test, the most important thing is to get the test done.
Collecting the samples:
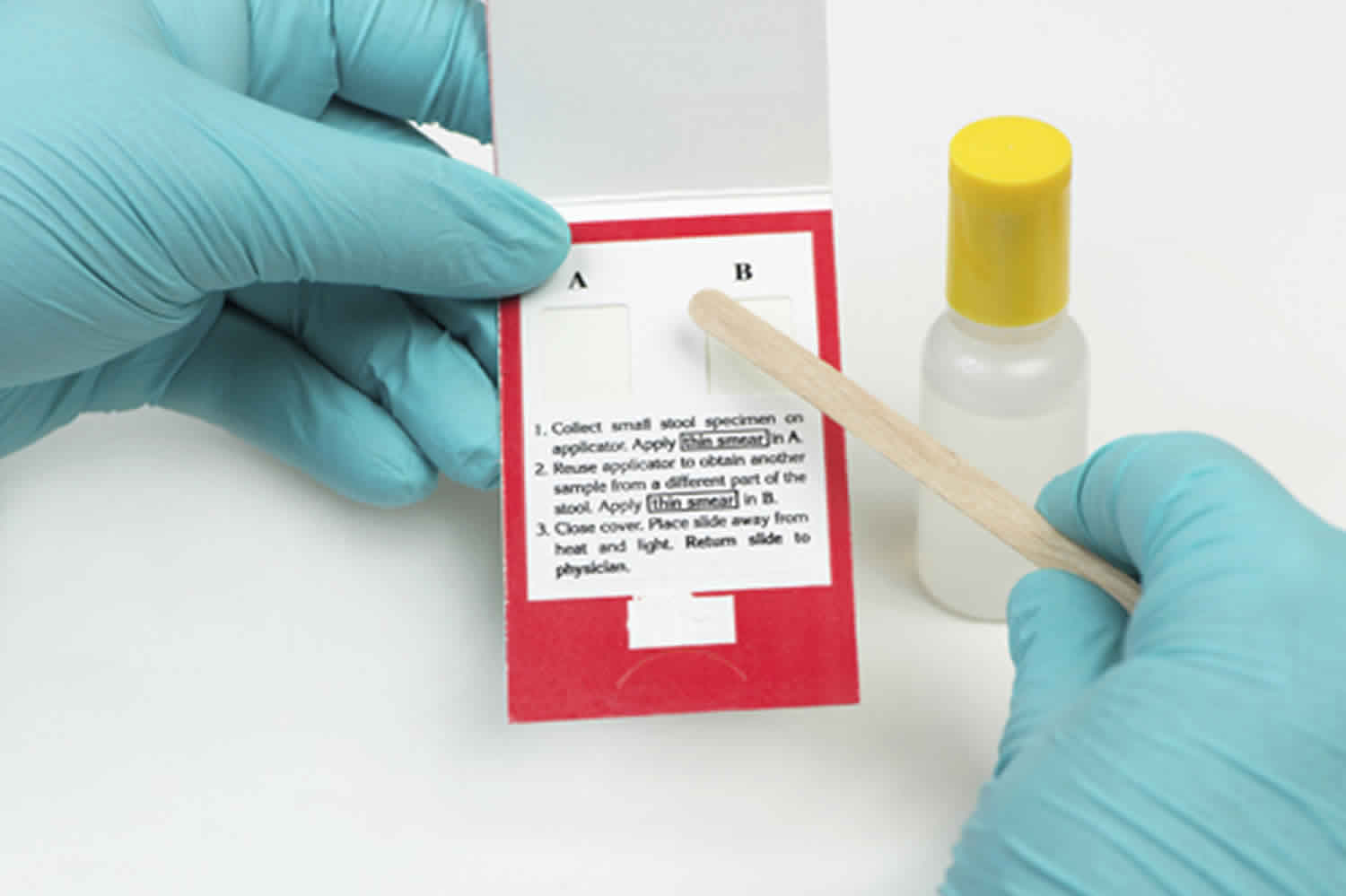
Be sure to follow the instructions that come with your kit, as different kits might have different instructions. People having this test will get a kit with instructions from their health care provider’s office or clinic. The kit will explain how to take stool samples at home (usually samples from 3 straight bowel movements are smeared onto small squares of paper). The kit is then returned to the doctor’s office or medical lab (usually within 2 weeks) for testing.
When doing this test, have all of your supplies ready and in one place. Supplies typically include a test kit, test cards, either a brush or wooden applicator, and a mailing envelope. The kit will give you detailed instructions on how to collect the stool samples. If you have any questions about how to use your kit, contact your health care provider’s office or clinic. Once you have collected the samples, return them as instructed in the kit.
Stool DNA test
A stool DNA test (also known as a multitargeted stool DNA test, or MT-sDNA) looks for certain abnormal sections of DNA from cancer or polyp cells. Colorectal cancer or polyp cells often have DNA mutations (changes) in certain genes. Cells with these mutations often get into the stool, where tests may be able to detect them. Cologuard®, the only test currently available, tests for both DNA changes and blood in the stool.
Collecting the samples:
Be sure to follow the instructions that come with your kit. You’ll get a kit in the mail to use to collect your entire stool sample at home. The kit will have a sample container, a bracket for holding the container in the toilet, a bottle of liquid preservative, a tube, labels, and a shipping box. The kit has detailed instructions on how to collect the sample. If you have any questions about how to use your kit, contact your doctor’s office or clinic. Once you have collected the sample, return it as instructed in the kit.
Stool DNA test should be done every 3 years. If the stool DNA test is positive (if it finds DNA changes or blood), a colonoscopy will be needed.
Why do I need a fecal occult blood test?
The National Cancer Institute recommends that people get regular screenings for colorectal cancer starting at age 50. The screening may be a fecal occult test, a colonoscopy, or another test. Talk with your health care provider about which test is right for you.
If you choose a fecal occult blood test, you need to get it every year. If you have a colonoscopy, you only need it every ten years. But it is a more invasive procedure. You may need screening more often if you have certain risk factors. These include:
- A family history of colorectal cancer
- Cigarette smoking
- Obesity
- Excessive alcohol use
American Cancer Society Guideline for Colorectal Cancer Screening
For people at average risk
The American Cancer Society recommends that people at average risk* of colorectal cancer start regular screening at age 45. This can be done either with a sensitive test that looks for signs of cancer in a person’s stool (a stool-based test), or with an exam that looks at the colon and rectum (a visual exam). These options are listed below.
- People who are in good health and with a life expectancy of more than 10 years should continue regular colorectal cancer screening through the age of 75.
- For people ages 76 through 85, the decision to be screened should be based on a person’s preferences, life expectancy, overall health, and prior screening history.
- People over 85 should no longer get colorectal cancer screening.
*For screening, people are considered to be at average risk if they do not have:
- A personal history of colorectal cancer or certain types of polyps
- A family history of colorectal cancer
- A personal history of inflammatory bowel disease (ulcerative colitis or Crohn’s disease)
- A confirmed or suspected hereditary colorectal cancer syndrome, such as familial adenomatous polyposis (FAP) or Lynch syndrome (hereditary non-polyposis colon cancer or HNPCC)
- A personal history of getting radiation to the abdomen (belly) or pelvic area to treat a prior cancer
Test options for colorectal cancer screening
Several test options are available for colorectal cancer screening:
Stool-based tests
- Highly sensitive fecal immunochemical test (FIT) every year
- Highly sensitive guaiac-based fecal occult blood test (gFOBT) every year
- Multi-targeted stool DNA test (MT-sDNA) every 3 years
Visual (structural) exams of the colon and rectum
- Colonoscopy every 10 years
- CT colonography (virtual colonoscopy) every 5 years
- Flexible sigmoidoscopy (FSIG) every 5 years
There are some differences between these tests to consider, but the most important thing is to get screened, no matter which test you choose. Talk to your health care provider about which tests might be good options for you, and to your insurance provider about your coverage.
If a person chooses to be screened with a test other than colonoscopy, any abnormal test result should be followed up with colonoscopy.
For people at increased or high risk
People at increased or high risk of colorectal cancer might need to start colorectal cancer screening before age 45, be screened more often, and/or get specific tests. This includes people with:
- A strong family history of colorectal cancer or certain types of polyps
- A personal history of colorectal cancer or certain types of polyps
- A personal history of inflammatory bowel disease (ulcerative colitis or Crohn’s disease)
- A known family history of a hereditary colorectal cancer syndrome such as familial adenomatous polyposis (FAP) or Lynch syndrome (also known as hereditary non-polyposis colon cancer or HNPCC)
- A personal history of radiation to the abdomen (belly) or pelvic area to treat a prior cancer
The American Cancer Society does not have screening guidelines specifically for people at increased or high risk of colorectal cancer. However, some other professional medical organizations, such as the US Multi-Society Task Force on Colorectal Cancer, do put out such guidelines. These guidelines are complex and are best looked at along with your health care provider. In general, these guidelines divide people into several groups (although the details depend on each person’s specific risk factors).
People at increased risk for colorectal cancer
People with one or more family members who have had colon or rectal cancer
- Screening recommendations for these people depend on who in the family had cancer and how old they were when it was diagnosed. Some people with a family history will be able to follow the recommendations for average risk adults, but others might need to get a colonoscopy (and not any other type of test) more often, and possibly starting before age 45.
People who have had certain types of polyps removed during a colonoscopy
- Most of these people will need to get a colonoscopy again after 3 years, but some people might need to get one earlier (or later) than 3 years, depending on the type, size, and number of polyps.
People who have had colon or rectal cancer
- Most of these people will need to start having colonoscopies regularly within a year of surgery to remove the cancer. Other procedures like ultrasound might also be recommended for some people with rectal cancer, depending on the type of surgery they had.
People who have had radiation to the abdomen (belly) or pelvic area to treat a prior cancer
- Most of these people will need to start having colonoscopies at an earlier age (depending on how old they were when they got the radiation), and might need to be screened more often than normal (such as at least every 5 years).
People at high risk for colorectal cancer
- People with inflammatory bowel disease (Crohn’s disease or ulcerative colitis): These people generally need to get colonoscopies (not any other type of test) every 1 to 2 years, starting at an earlier age.
- People known or suspected to have certain genetic syndromes: These people generally need to have colonoscopy (not any of the other tests). Screening is often recommended to begin at a young age, possibly as early as the teenage years for some syndromes – and needs to be done much more frequently. Specifics depend on which genetic syndrome you have, and other factors.
If you’re at increased or high risk of colorectal cancer (or think you might be), talk to your health care provider to learn more. Your provider can suggest the best screening option for you, as well as determine what type of screening schedule you should follow, based on your individual risk.
Fecal occult blood test instructions
A fecal occult blood test is a noninvasive test that you can perform at home at your convenience. Your health care provider will give you a kit that includes instructions on how to do the test. There are two main types of fecal occult blood tests: the guaiac smear method (gFOBT) and the immunochemical method (iFOBT or FIT). Below are typical instructions for each test. Your instructions may vary slightly depending on the manufacturer of the test kit.
For a guaiac smear test (gFOBT), you will most likely need to:
- Collect samples from three separate bowel movements.
- For each sample, collect the stool and store in a clean container. Make sure the sample does not mix in with urine or water from the toilet.
- Use the applicator from your test kit to smear some of the stool on the test card or slide, also included in your kit.
- Label and seal all your samples as directed.
- Mail the samples to your health care provider or lab.
For a fecal immunochemical test (FIT), you will most likely need to:
- Collect samples from two or three bowel movements.
- Collect the sample from the toilet using the special brush or other device that was included in your kit.
- For each sample, use the brush or device to take the sample from the surface of the stool.
- Brush the sample onto a test card.
- Label and seal all your samples as directed.
- Mail the samples to your health care provider or lab.
Be sure to follow all the instructions provided in your kit, and talk to your health care provider if you have any questions.
Will I need to do anything to prepare for the fecal occult blood test?
Certain foods and drugs may affect the results of a guaiac smear method (gFOBT) test. Your health care provider may ask you to avoid the following:
- Nonsteroidal, anti-inflammatory drugs (NSAIDs) such as ibuprofen, naproxen, or aspirin for seven days prior to your test. If you take aspirin for heart problems, talk to your health care provider before stopping your medicine. Acetaminophen may be safe to use during this time, but check with your health care provider before taking it.
- More than 250 mg of vitamin C daily from supplements, fruit juices, or fruit for seven days prior to your test. Vitamin C can affect the chemicals in the test and cause a negative result even if there is blood present.
- Red meat, such as beef, lamb, and pork, for three days prior to the test. Traces of blood in these meats may cause a false-positive result.
There are no special preparations or dietary restrictions for a fecal immunochemical test (FIT).
What do the fecal occult blood test results mean?
If your results are positive for either type of fecal occult blood test, it means you likely have bleeding somewhere in your digestive tract. But it does not necessarily mean you have cancer. Other conditions that may produce a positive result on a fecal occult blood test include ulcers, hemorrhoids, polyps, and benign tumors. If your test results are positive for blood, your health care provider will likely recommend additional testing, such as a colonoscopy, to figure out the exact location and cause of your bleeding. If you have questions about your results, talk to your health care provider.