Contents
- What are the ventricles of the brain
- Brain ventricles anatomy
- Brain ventricles function
- Enlarged ventricles brain
What are the ventricles of the brain
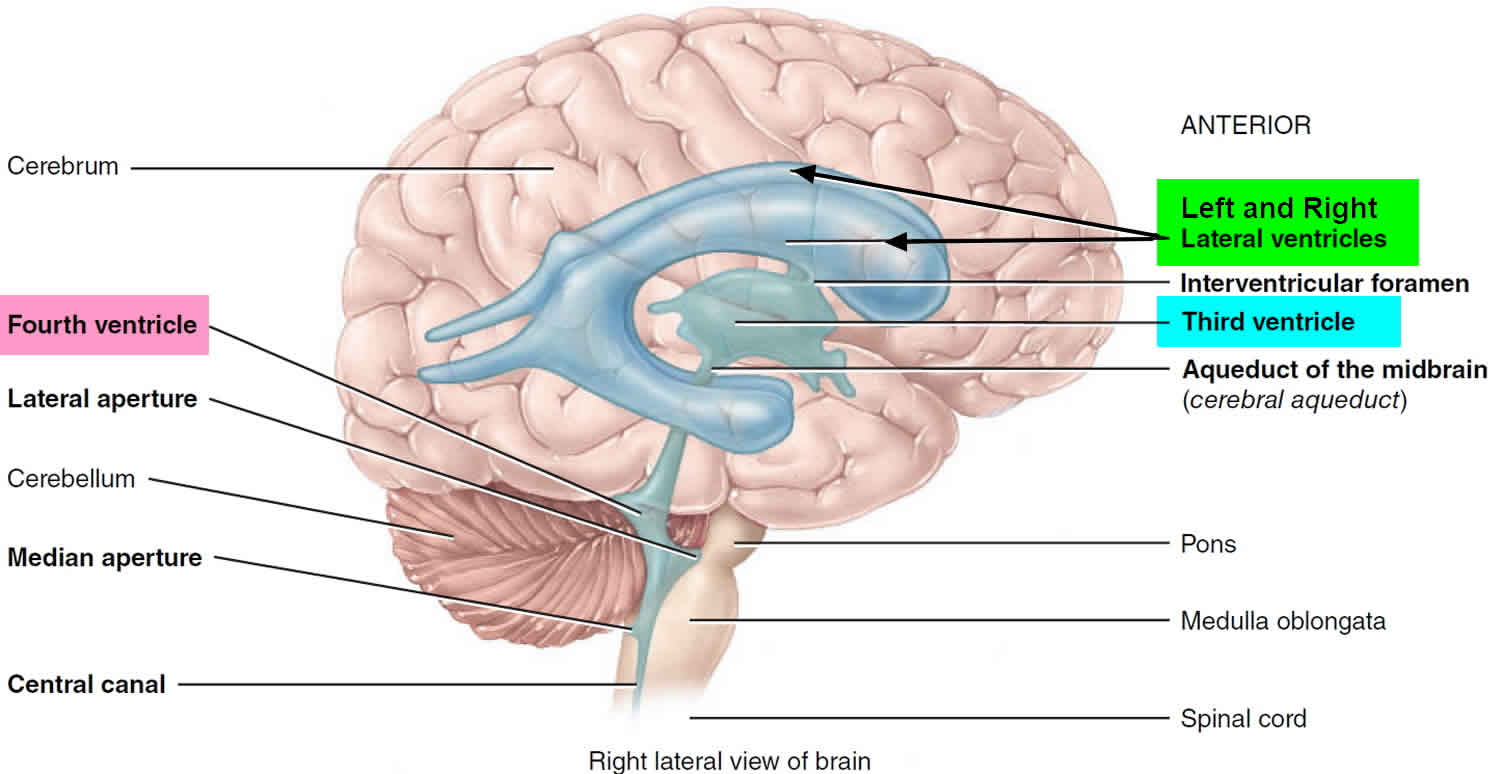
The brain has four ventricles or internal chambers. The largest and most frontal ones are the two lateral ventricles, which form an arc in each cerebral hemisphere. Through a tiny pore called the interventricular foramen, each lateral ventricle is connected to the third ventricle, a narrow median space inferior to the corpus callosum. From here, a canal called the cerebral aqueduct passes down the core of the midbrain and leads to the fourth ventricle, a small triangular chamber between the pons and cerebellum. Caudally, this space narrows and forms a central canal that extends through the medulla oblongata into the spinal cord.
Figure 1. Brain ventricles
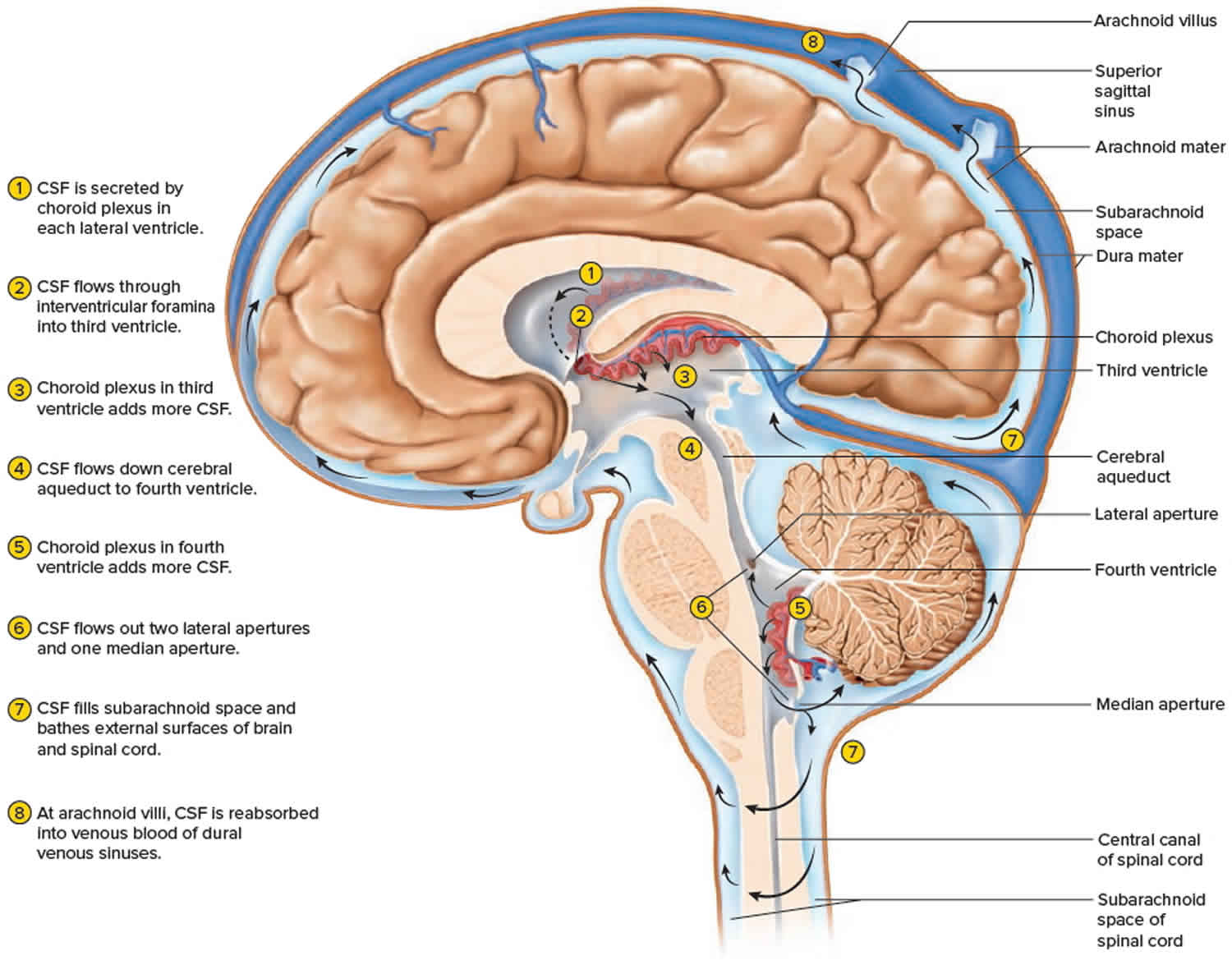
Figure 2. Cerebrospinal fluid formation, absorption and circulation around and within the brain
On the floor or wall of each ventricle is a spongy mass of blood capillaries called a choroid plexus, named for its histological resemblance to a fetal membrane called the chorion. Ependyma, a type of neuroglia that resembles a cuboidal epithelium, lines the ventricles and canals and covers the choroid plexuses. It produces cerebrospinal fluid (CSF).
Cerebrospinal fluid is a clear, colorless liquid that fills the ventricles and canals of the CNS and bathes its external surface. The brain produces about 500 mL of cerebrospinal fluid per day, but the fluid is constantly reabsorbed at the same rate and only 100 to 160 mL is normally present at one time. About 40% of it is formed in the subarachnoid space external to the brain, 30% by the general ependymal lining of the brain ventricles, and 30% by the choroid plexuses. Cerebrospinal fluid production begins with the filtration of blood plasma through the capillaries of the brain. Ependymal cells modify the filtrate as it passes through them, so the cerebrospinal fluid has more sodium chloride than blood plasma, but less potassium, calcium, and glucose and very little protein.
Cerebrospinal fluid serves three functions for the brain:
- Buoyancy. Because the brain and cerebrospinal fluid are similar in density, the brain neither sinks nor floats in the cerebrospinal fluid. It hangs from delicate specialized fibroblasts of the arachnoid meninx. A human brain removed from the body weighs about 1.5 kg, but when suspended in cerebrospinal fluid its effective weight is only about 50 g. This buoyancy allows the brain to attain considerable size without being impaired by its own weight. If the brain rested heavily on the floor of the cranium, the pressure would kill the nervous tissue.
- Protection. Cerebrospinal fluid also protects the brain from striking the cranium when the head is jolted. If the jolt is severe, however, the brain still may strike the inside of the cranium or suffer shearing injury from contact with the angular surfaces of the cranial floor. This is one of the common findings in head injuries (concussions) from contact sports like NFL, rugby and boxing.
- Chemical stability. Cerebrospinal fluid rinses metabolic wastes from the nervous tissue and regulates its chemical environment. Slight changes in cerebrospinal fluid composition can cause malfunctions of the nervous system. For example, a high glycine concentration disrupts the control of body temperature and blood pressure, and a high pH causes dizziness and fainting.
Cerebrospinal fluid continually flows through and around the brain and spinal cord, driven partly by its own pressure, partly by the beating of ependymal cilia, and partly by rhythmic pulsations of the brain produced by each heartbeat. The cerebrospinal fluid of the lateral ventricles flows through the interventricular foramina into the third ventricle, then down the cerebral aqueduct to the fourth ventricle. The third and fourth ventricles and their choroid plexuses add more cerebrospinal fluid along the way. A small amount of cerebrospinal fluid fills the central canal of the spinal cord, but ultimately, all of it escapes through three pores in the fourth ventricle—a median aperture and two lateral apertures. These lead into the subarachnoid space on the brain and spinal cord surface. From here, cerebrospinal fluid is reabsorbed by arachnoid granulations, extensions of the arachnoid meninx shaped like little sprigs of cauliflower, protruding through the dura mater into the superior sagittal sinus. Cerebrospinal fluid penetrates the walls of the granulations and mixes with blood in the sinus.
Brain ventricles anatomy
The 4 ventricles of the brain are a series of interconnected, cerebrospinal fluid (CSF)-filled spaces that lie in the core of the forebrain and brainstem (Figure 1). The presence of ventricular spaces in the various subdivisions of the brain reflects the fact that the ventricles are the adult derivatives of the open space or lumen of the embryonic neural tube 1. The largest of brain ventricles are the lateral ventricles (one within each of the cerebral hemispheres). The right and left lateral ventricles are best seen in frontal sections, where their ventral surface is usually defined by the basal ganglia, their dorsal surface by the corpus callosum, and their medial surface by the septum pellucidum, a membranous tissue sheet that forms part of the midline sagittal surface of the cerebral hemispheres. The third ventricle forms a narrow midline space between the right and left thalamus, and communicates with the lateral ventricles through a small opening at the anterior end of the third ventricle called the interventricular foramen. The third ventricle is continuous caudally with the cerebral aqueduct, which runs though the midbrain. At its caudal end, the aqueduct opens into the fourth ventricle, a larger space in the dorsal pons and medulla. The fourth ventricle narrows caudally to form the central canal of the spinal cord. The ventricles are filled with cerebrospinal fluid, and the lateral, third, and fourth ventricles are the site of the choroid plexus, which produces the cerebrospinal fluid. The cerebrospinal fluid percolates through the ventricular system and flows into the subarachnoid space through perforations in the thin covering of the fourth ventricle; it is eventually absorbed by specialized structures called arachnoid villi or granulations (see Figure 2), and returned to the venous circulation.
How many ventricles are in the brain?
Four. The right and left lateral ventricles, third ventricle and the fourth ventricle. The ventricular system is made up of four ventricles connected by narrow passages. Normally, cerebrospinal fluid (CSF) flows through the ventricles, exits into cisterns (closed spaces that serve as reservoirs) at the base of the brain, bathes the surfaces of the brain and spinal cord, and then reabsorbs into the bloodstream.
Brain ventricles function
On the floor or wall of each ventricle is a spongy mass of blood capillaries called a choroid plexus, named for its histological resemblance to a fetal membrane called the chorion. Ependyma, a type of neuroglia that resembles a cuboidal epithelium, lines the ventricles and canals and covers the choroid plexuses. It produces cerebrospinal fluid (CSF).
Cerebrospinal fluid is a clear, colorless liquid that fills the ventricles and canals of the CNS and bathes its external surface. The brain produces about 500 mL of cerebrospinal fluid per day, but the fluid is constantly reabsorbed at the same rate and only 100 to 160 mL is normally present at one time. About 40% of it is formed in the subarachnoid space external to the brain, 30% by the general ependymal lining of the brain ventricles, and 30% by the choroid plexuses. Cerebrospinal fluid production begins with the filtration of blood plasma through the capillaries of the brain. Ependymal cells modify the filtrate as it passes through them, so the cerebrospinal fluid has more sodium chloride than blood plasma, but less potassium, calcium, and glucose and very little protein.
Cerebrospinal fluid serves three functions for the brain:
- Buoyancy. Because the brain and cerebrospinal fluid are similar in density, the brain neither sinks nor floats in the cerebrospinal fluid. It hangs from delicate specialized fibroblasts of the arachnoid meninx. A human brain removed from the body weighs about 1.5 kg, but when suspended in cerebrospinal fluid its effective weight is only about 50 g. This buoyancy allows the brain to attain considerable size without being impaired by its own weight. If the brain rested heavily on the floor of the cranium, the pressure would kill the nervous tissue.
- Protection. Cerebrospinal fluid also protects the brain from striking the cranium when the head is jolted. If the jolt is severe, however, the brain still may strike the inside of the cranium or suffer shearing injury from contact with the angular surfaces of the cranial floor. This is one of the common findings in head injuries (concussions) from contact sports like NFL, rugby and boxing.
- Chemical stability. Cerebrospinal fluid rinses metabolic wastes from the nervous tissue and regulates its chemical environment. Slight changes in cerebrospinal fluid composition can cause malfunctions of the nervous system. For example, a high glycine concentration disrupts the control of body temperature and blood pressure, and a high pH causes dizziness and fainting.
Enlarged ventricles brain
Enlarged ventricles of brain is also called hydrocephalus, which is derived from the Greek words “hydro” meaning water and “cephalus” meaning head. As the name implies, it is a condition in which the primary characteristic is excessive accumulation of fluid in the brain. Although hydrocephalus was once known as “water on the brain,” the “water” is actually cerebrospinal fluid (CSF) — a clear fluid that surrounds the brain and spinal cord. The excessive accumulation of CSF results in an abnormal widening of spaces in the brain called ventricles. This widening creates potentially harmful pressure on the tissues of the brain.
The ventricular system is made up of four ventricles connected by narrow passages. Normally, CSF flows through the ventricles, exits into cisterns (closed spaces that serve as reservoirs) at the base of the brain, bathes the surfaces of the brain and spinal cord, and then reabsorbs into the bloodstream.
Cerebrospinal fluid (CSF) has three important life-sustaining functions:
- To keep the brain tissue buoyant, acting as a cushion or “shock absorber”;
- To act as the vehicle for delivering nutrients to the brain and removing waste; and
- To flow between the cranium and spine and compensate for changes in intracranial blood volume (the amount of blood within the brain).
The balance between production and absorption of CSF is critically important. Because CSF is made continuously, medical conditions that block its normal flow or absorption will result in an over-accumulation of CSF. The resulting pressure of the fluid against brain tissue is what causes enlarged brain ventricles or hydrocephalus.
Figure 3. Enlarged ventricles brain baby
Who gets enlarged brain ventricles?
The number of people who develop hydrocephalus or who are currently living with it is difficult to establish since the condition occurs in children and adults, and can develop later in life. A 2008 data review by the University of Utah found that, in 2003, hydrocephalus accounted for 0.6 percent of all pediatric hospital admissions in the United States. Some estimates report one to two of every 1,000 babies are born with hydrocephalus.
What causes enlarged brain ventricles?
The causes of enlarged ventricles of brain (hydrocephalus) are still not well understood. Hydrocephalus may result from inherited genetic abnormalities (such as the genetic defect that causes aqueductal stenosis) or developmental disorders (such as those associated with neural tube defects including spina bifida and encephalocele). Other possible causes include complications of premature birth such as intraventricular hemorrhage, diseases such as meningitis, tumors, traumatic head injury, or subarachnoid hemorrhage, which block the exit of CSF from the ventricles to the cisterns or eliminate the passageway for CSF within the cisterns.
What are the different types of enlarged ventricles of brain?
Hydrocephalus may be congenital or acquired. Congenital hydrocephalus is present at birth and may be caused by either events or influences that occur during fetal development, or genetic abnormalities. Acquired hydrocephalus develops at the time of birth or at some point afterward. This type of hydrocephalus can affect individuals of all ages and may be caused by injury or disease.
Hydrocephalus may also be communicating or non-communicating. Communicating hydrocephalus occurs when the flow of CSF is blocked after it exits the ventricles. This form is called communicating because the CSF can still flow between the ventricles, which remain open. Non-communicating hydrocephalus — also called “obstructive” hydrocephalus — occurs when the flow of CSF is blocked along one or more of the narrow passages connecting the ventricles. One of the most common causes of hydrocephalus is “aqueductal stenosis.” In this case, hydrocephalus results from a narrowing of the aqueduct of Sylvius, a small passage between the third and fourth ventricles in the middle of the brain.
There are two other forms of hydrocephalus which do not fit exactly into the categories mentioned above and primarily affect adults: hydrocephalus ex-vacuo and Normal Pressure Hydrocephalus.
Hydrocephalus ex-vacuo occurs when stroke or traumatic injury cause damage to the brain. In these cases, brain tissue may actually shrink. Normal Pressure Hydrocephalus is an abnormal increase of cerebrospinal fluid in the brain’s ventricles that may result from a subarachnoid hemorrhage, head trauma, infection, tumor, or complications of surgery. However, many people develop normal pressure hydrocephalus when none of these factors are present. An estimated 375,000 older Americans have normal pressure hydrocephalus.
Enlarged brain ventricles symptoms
Symptoms of hydrocephalus vary with age, disease progression, and individual differences in tolerance to the condition. For example, an infant’s ability to compensate for increased CSF pressure and enlargement of the ventricles differs from an adult’s. The infant skull can expand to accommodate the buildup of CSF because the sutures (the fibrous joints that connect the bones of the skull) have not yet closed.
In infancy, the most obvious indication of hydrocephalus is often a rapid increase in head circumference or an unusually large head size. Other symptoms may include vomiting, sleepiness, irritability, downward deviation of the eyes (also called “sun setting”), and seizures.
Older children and adults may experience different symptoms because their skulls cannot expand to accommodate the buildup of CSF. Symptoms may include headache followed by vomiting, nausea, blurred or double vision, sun setting of the eyes, problems with balance, poor coordination, gait disturbance, urinary incontinence, slowing or loss of developmental progress, lethargy, drowsiness, irritability, or other changes in personality or cognition including memory loss.
Symptoms of normal pressure hydrocephalus include problems with walking, impaired bladder control leading to urinary frequency and/or incontinence, and progressive mental impairment and dementia. An individual with this type of hydrocephalus may have a general slowing of movements or may complain that his or her feet feel “stuck.” Because some of these symptoms may also be experienced in other disorders such as Alzheimer’s disease, Parkinson’s disease, and Creutzfeldt-Jakob disease, normal pressure hydrocephalus is often incorrectly diagnosed and never properly treated. Doctors may use a variety of tests, including brain scans such as computed tomography (CT) and magnetic resonance imaging (MRI), a spinal tap or lumbar catheter, intracranial pressure monitoring, and neuropsychological tests, to help them accurately diagnose normal pressure hydrocephalus and rule out any other conditions.
The symptoms described in this section account for the most typical ways in which progressive hydrocephalus is noticeable, but it is important to remember that symptoms vary significantly from person to person.
Enlarged brain ventricles diagnosis
Hydrocephalus is diagnosed through clinical neurological evaluation and by using cranial imaging techniques such as ultrasonography, CT, MRI, or pressure-monitoring techniques. A physician selects the appropriate diagnostic tool based on an individual’s age, clinical presentation, and the presence of known or suspected abnormalities of the brain or spinal cord.
Enlarged brain ventricles treatment
Hydrocephalus is most often treated by surgically inserting a shunt system. This system diverts the flow of CSF from the CNS to another area of the body where it can be absorbed as part of the normal circulatory process.
A shunt is a flexible but sturdy plastic tube. A shunt system consists of the shunt, a catheter, and a valve. One end of the catheter is placed within a ventricle inside the brain or in the CSF outside the spinal cord. The other end of the catheter is commonly placed within the abdominal cavity, but may also be placed at other sites in the body such as a chamber of the heart or areas around the lung where the CSF can drain and be absorbed. A valve located along the catheter maintains one-way flow and regulates the rate of CSF flow.
A limited number of individuals can be treated with an alternative procedure called third ventriculostomy. In this procedure, a neuroendoscope — a small camera that uses fiber optic technology to visualize small and difficult to reach surgical areas — allows a doctor to view the ventricular surface. Once the scope is guided into position, a small tool makes a tiny hole in the floor of the third ventricle, which allows the CSF to bypass the obstruction and flow toward the site of resorption around the surface of the brain.
What are the possible complications of a shunt system?
Shunt systems are imperfect devices. Complications may include mechanical failure, infections, obstructions, and the need to lengthen or replace the catheter. Generally, shunt systems require monitoring and regular medical follow up. When complications occur, subsequent surgery to replace the failed part or the entire shunt system may be needed.
Some complications can lead to other problems such as overdraining or underdraining. Overdraining occurs when the shunt allows CSF to drain from the ventricles more quickly than it is produced. Overdraining can cause the ventricles to collapse, tearing blood vessels and causing headache, hemorrhage (subdural hematoma), or slit-like ventricles (slit ventricle syndrome). Underdraining occurs when CSF is not removed quickly enough and the symptoms of hydrocephalus recur. Overdrainage and underdrainage of CSF are addressed by adjusting the drainage pressure of the shunt valve; if the shunt has an adjustable pressure valve these changes can be made by placing a special magnet on the scalp over the valve. In addition to the common symptoms of hydrocephalus, infections from a shunt may also produce symptoms such as a low-grade fever, soreness of the neck or shoulder muscles, and redness or tenderness along the shunt tract. When there is reason to suspect that a shunt system is not functioning properly (for example, if the symptoms of hydrocephalus return), medical attention should be sought immediately.
Enlarged brain ventricles prognosis
The prognosis for individuals diagnosed with hydrocephalus is difficult to predict, although there is some correlation between the specific cause of the hydrocephalus and the outcome. Prognosis is further clouded by the presence of associated disorders, the timeliness of diagnosis, and the success of treatment. The degree to which relief of CSF pressure following shunt surgery can minimize or reverse damage to the brain is not well understood.
Affected individuals and their families should be aware that hydrocephalus poses risks to both cognitive and physical development. However, many children diagnosed with the disorder benefit from rehabilitation therapies and educational interventions and go on to lead normal lives with few limitations. Treatment by an interdisciplinary team of medical professionals, rehabilitation specialists, and educational experts is critical to a positive outcome. Left untreated, progressive hydrocephalus may be fatal.
The symptoms of normal pressure hydrocephalus usually get worse over time if the condition is not treated, although some people may experience temporary improvements. While the success of treatment with shunts varies from person to person, some people recover almost completely after treatment and have a good quality of life. Early diagnosis and treatment improves the chance of a good recovery.
- Purves D, Augustine GJ, Fitzpatrick D, et al., editors. Neuroscience. 2nd edition. Sunderland (MA): Sinauer Associates; 2001. The Ventricular System. Available from: https://www.ncbi.nlm.nih.gov/books/NBK11083[↩]