Contents
What is melena
Melena refers to the passage of dark-colored, foul smelling, tarry stools and it is a sign of a problem in the upper digestive tract. Melena is caused by the presence of blood within the gastrointestinal lumen. The blood is broken down by bacteria in the colon into chemicals (hematin) which are black in color.
Eating black licorice, blueberries, blood sausage, or taking iron pills, activated charcoal, or bismuth medicines like Pepto-Bismol, can also cause black stools. Beets and foods with red coloring can sometimes make stools appear reddish. In all these cases, your doctor can test the stool with a chemical to rule out the presence of blood.
Bleeding in the esophagus or stomach (such as with peptic ulcer disease) can also cause you to vomit blood.
Call your health care provider right away if:
- You notice blood or changes in the color of your stool
- You vomit blood
- You feel dizziness or lightheadedness
- You notice black or pale stools often
- You notice changes in the stool related to diet
- You have chills
- You have cramping
- You have fever
- You have pain in your abdomen
- You have weight loss
In children, a small amount of blood in the stool is most often not serious. The most common cause is constipation. You should still tell your child’s provider if you notice this problem.
Hematochezia vs Melena
Hematochezia is also known as rectal bleeding, which refers to the passage of bright blood (often mixed with blood clots or stools) via the rectum. The rectum is the final 15cm of the colon (large intestine) where feces accumulate before being expelled from the body via the anal canal. Hematochezia (rectal bleeding) can be due to bleeding from anywhere in the lower gastrointestinal tract namely the colon, rectum or anus.
Hematochezia (rectal bleeding) is a very common complaint in the general population and affects up to 15% of adults. Unfortunately not all these people report their symptoms to their doctors, which is dangerous as a small proportion of hematochezia (rectal bleeding) is due to an underlying colorectal cancer. The majority of cases, however, will be due to a self-limiting condition affecting the anus or rectum, but it is still important that you see a doctor.
The severity of hematochezia (rectal bleeding) varies widely. Some people will only have a few small drops of blood that stain the toilet water or are detected on wiping, whilst others will pass several bowel motions containing large quantities of blood and clots. In some patients, the amount of blood loss is severe enough to cause weakness, light-headedness, low blood pressure and symptoms of anaemia. In these cases, hospital admission is often needed.
The color of the blood gives the doctor a clue to the likely site of origin of the gastrointestinal bleeding. Generally speaking, the closer the lesion is to the anus the brighter the blood lost. Bleeding from the first parts of the large intestine (the ascending and transverse colon) will cause passage of dark red or maroon blood. Bleeding from much further up the gastrointestinal tract such as the stomach doesn’t normally cause the loss of fresh blood, but produces black and tarry stools called melena.
Rectal bleeding is a symptom itself and should not be confused with the term fecal occult blood. The latter has similar causes to rectal bleeding, but does not result in any color changes to the stool or presence of fresh blood in the rectum. Fecal occult (hidden) blood is only detected when stool samples are examined at a laboratory. This may be done for the purpose of investigating the cause of iron deficiency anemia.
Causes of melena
Melena (black or tarry stools) may be due to bleeding in the upper part of the GI (gastrointestinal) tract, such as the esophagus, stomach, or the first part of the small intestine. In this case, blood is darker because it gets digested on its way through the gastrointestinal tract.
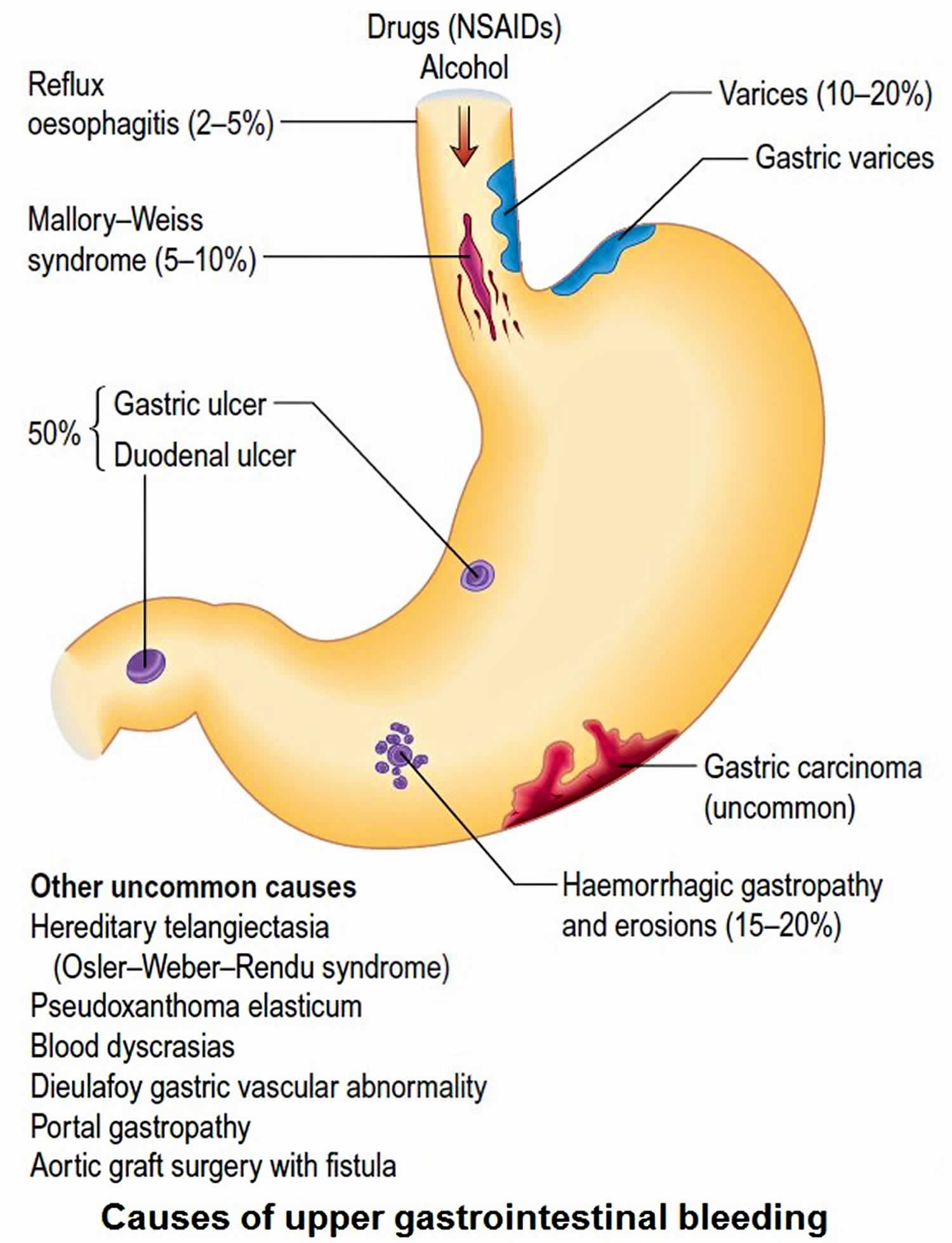
Upper gastrointestinal bleeding is a common problem with an annual incidence of approximately 80 to 150 per 100,000 population, with estimated mortality rates between 2% to 15% 1.
Peptic ulcers are the most common cause of acute upper gastrointestinal bleeding. Peptic ulcer disease accounts for 40% to 50% of the upper gastrointestinal bleeding cases 1. Of those, the majority is secondary to duodenal ulcers (30%). Peptic ulcers can be associated with nonsteroidal anti-inflammatory drugs (NSAIDs), Helicobacter pylori, and stress-related mucosal disease.
Melena may also occur due to:
- Abnormal blood vessels (vascular malformations 5%)
- A tear in the esophagus from violent vomiting (Mallory-Weiss tear 5% to 15%)
- Blood supply being cut off to part of the intestines
- Inflammation of the stomach lining (gastritis)
- Trauma or foreign body
- Erosive esophagitis accounts for 11%
- Duodenitis 10%
- Widened, overgrown veins (called varices) in the esophagus and stomach, commonly caused by liver cirrhosis. Varices 5% to 30% (depending if the population studied have a chronic liver disease)
- Cancer of the esophagus, stomach, or duodenum or ampulla
Figure 1. Causes of melena
Melena symptoms
Melena refers to the passage of dark-colored, foul smelling, tarry stools and it is a sign of a problem in the upper digestive tract. Melena is caused by the presence of blood within the gastrointestinal lumen. The blood is broken down by bacteria in the colon into chemicals (hematin) which are black in color.
Melena diagnosis
Your doctor will take a medical history and perform a physical exam. The exam will focus on your abdomen.
You may be asked the following questions:
- Are you taking blood thinners, such as aspirin, warfarin or clopidogrel, or similar medicines? Are you taking an NSAID, such as ibuprofen or naproxen?
- Have you had any trauma or swallowed a foreign object accidentally?
- Have you eaten black licorice, lead, Pepto-Bismol, or blueberries?
- Have you had more than one episode of blood in your stool? Is every stool this way?
- Have you lost any weight recently?
- Is there blood on the toilet paper only?
- What color is the stool?
- When did the problem develop?
- What other symptoms are present (abdominal pain, vomiting blood, bloating, excessive gas, diarrhea, or fever)?
You may need to have one or more tests to look for the cause:
- Angiography
- Bleeding scan (nuclear medicine)
- Blood studies must include a complete blood cell count (CBC) to look for current levels of hemoglobin, hematocrit, and platelets. A low MCV can point towards chronic blood loss and iron deficiency anemia. Chemistry should also be evaluated. Elevated BUN or elevated BUN/Creatinine can also be indicative of upper gastrointestinal bleeding. Coagulation studies should also be checked.
- Colonoscopy
- Esophagogastroduodenoscopy or EGD
- Stool culture
- Tests for the presence of Helicobacter pylori infection
- Capsule endoscopy (a pill with a built in camera that takes a video of the small intestine)
- Double balloon enteroscopy (a scope that can reach the parts of the small intestine that are not able to be reached with EGD or colonoscopy)
Severe cases of bleeding that cause excessive blood loss and a drop in blood pressure may require surgery or hospitalization.
Melena treatment
Management of the patient presenting with upper gastrointestinal bleeding should always follow a step-wise approach. The first step is to assess the hemodynamic status and initiate resuscitative efforts as needed (including fluids and blood transfusions). Patients should be risk stratified based on their initial presentation, hemodynamic status, comorbidities, age, and initial laboratory tests.
There are few scoring systems designed to predict which patients will likely need intervention and also to predict rebleeding and mortality. The Rockall score was designed to predict rebleeding and mortality and includes age, comorbidities, the presence of shock, and endoscopic stigmata. A pre-endoscopic Rockall is also available and can be used to stratify patient’s risk for rebleeding and mortality even before the endoscopic evaluation. When the Rockall score is used, patients with two or fewer points are considered low risk and have a 4.3% probability of rebleeding and 0.1% mortality. In contrast, patients with a score of six or more have a rebleeding rate of 15% and mortality of 39%.
Another scoring system that is traditionally used in upper gastrointestinal bleeding is the Blatchford Score. This scoring system was designed to predict the need for intervention. It includes hemoglobin levels, blood pressure, presentation of syncope, melena, liver disease, and heart failure. A score of six or higher is associated with a greater than 50% risk of needing an intervention.
If the patient is suspected of having upper gastrointestinal bleeding, endoscopy (esophagogastroduodenoscopy) must be performed to identify the cause and potentially treat the source of bleeding. Multiple studies have tried to identify the best timing to perform endoscopy. Until now, there is no evidence that emergency esophagogastroduodenoscopy is superior to routine esophagogastroduodenoscopy (done in 24 to 48 hours). The American College of Gastroenterology continues to recommend that all patients with upper gastrointestinal bleeding should undergo endoscopy within 24 hours of admission, following resuscitative efforts to optimize hemodynamic parameters and other medical problems. Per American College of Gastroenterology recommendations, endoscopy within 12 hours should be considered for all patients with higher risk clinical features (e.g., tachycardia, hypotension, bloody emesis or nasogastric aspirate in the hospital) to potentially improve clinical outcomes.
Patients must have a minimum of two large-bore peripheral access catheters (at least 18-gauge). Intravenous fluids should be administered to maintain adequate blood pressure and hemodynamic stability. If patients are not able to protect their airways or have ongoing severe hematemesis, elective endotracheal intubation is advised.
Blood transfusions should be given to target a hematocrit above 20%, with a hematocrit above 30% targeted in high-risk patients, such as the elderly and patients with coronary artery disease. There is no evidence that higher targets for hematocrit goals should be sought as that higher targets can even be deleterious.
Proton pump inhibitors are used to treat patients with nonvariceal upper gastrointestinal bleeding. The use of antacids has been shown to alter the natural history of patients with acute upper gastrointestinal bleeding. Patients with significant bleeding should be treated with an 80-mg bolus of proton pump inhibitor followed by a continuous infusion. The typical duration is 72 hours for patients with high-risk lesions visualized on esophagogastroduodenoscopy. If endoscopy was normal or only revealed low-risk lesion, proton pump inhibitor infusion can be discontinued and patient switch to a daily twice a day infusion or even to oral proton pump inhibitors .
Octreotide, a somatostatin analog, is a medication used when variceal bleeding is suspected. It is given as an intravenous bolus of 20 mcg to 50 mcg, followed by a continuous infusion at a rate of 25 mcg to 50 mcg per hour. Its use is not recommended in patients with acute nonvariceal upper gastrointestinal bleeding, but it can be used as adjunctive therapy in some cases. Its role is limited to settings in which endoscopy is unavailable or as a means to help stabilize patients before definitive therapy can be performed.
Endoscopic intervention might be warranted depending on the findings during the upper endoscopy. If a patient has an ulcer with a clean base, no intervention is needed. However, if a bleeding vessel is visualized or there is stigmata of recent bleeding, therapeutic options might include thermal coagulation to achieve hemostasis, local injection of epinephrine or use of clips. A combination of these methods might be needed based on the severity of the lesions.
If the patient is found to have H. pylori, eradication should be a target. If NSAIDs were likely the cause of the bleeding, they should be stopped, and if absolutely needed, alternative agents such as COX-2-selective NSAID plus a proton pump inhibitor should be used. Patients with established cardiovascular disease who require aspirin or other antiplatelet agents should be on proton pump inhibitor therapy and generally can have antiplatelet therapy reinstituted after bleeding ceases (ideally within 1 to 3 days and certainly within 7 days).
The natural history of patients who are treated with endoscopic therapy is that 80% to 90% of patients will have permanent control of their bleeding. However, 10% to 20% will rebleed. Patients who rebleed should have a second endoscopic procedure attempted. If bleeding persists despite endoscopic intervention or source of bleeding can not be identified, other modalities such as angiography or surgery should be considered.