Contents
What is myotonic dystrophy
Myotonic dystrophy is part of a group of inherited disorders called muscular dystrophies. It is the most common form of muscular dystrophy that begins in adulthood. People who have myotonic dystrophy have progressive muscle wasting and weakness in their lower legs, hands, neck and face that get worse over time to the point of disability. Signs and symptoms of myotonic dystrophy usually develop when a person is in his or her twenties or thirties. Usually, disability does not become severe until fifteen to twenty years after the symptoms appear. The progression of muscle weakness is slower and is less serious in people who are older when the muscle weakness is first noticed. People with myotonic dystrophy often have prolonged muscle contractions (myotonia) and are not able to relax certain muscles after use. For example, a person may have difficulty releasing their grip on a doorknob or handle. Also, affected people may have slurred speech or temporary locking of their jaw.
Other signs and symptoms of myotonic dystrophy include clouding of the lens of the eye (cataracts) and abnormalities of the electrical signals that control the heartbeat (cardiac conduction defects). In affected men, hormonal changes may lead to early balding and an inability to father a child (infertility). The features of this disorder often develop during a person’s twenties or thirties, although they can occur at any age. The severity of myotonic dystrophy varies widely among affected people, even among members of the same family.
There are two major types of myotonic dystrophy: type 1 and type 2. The two types of myotonic dystrophy are caused by alterations (mutations) in two different genes. Their signs and symptoms overlap, although myotonic dystrophy type 2 tends to be milder than myotonic dystrophy type 1. The muscle weakness associated with myotonic dystrophy type 1 particularly affects the lower legs, hands, neck, and face. Muscle weakness in type 2 primarily involves the muscles of the neck, shoulders, elbows, and hips.
A severe type of myotonic dystrophy type 1 can be seen at birth, called congenital myotonic dystrophy, is apparent at birth. Congenital myotonic dystrophy characteristic features include weak muscle tone (hypotonia), an inward- and upward-turning foot (clubfoot), breathing problems, delayed development, and intellectual disability. Some of these health problems can be life-threatening. Congenital myotonic dystrophy has only been seen in type 1 myotonic dystrophy and not in type 2.
Below is a general comparison of the major features of myotonic dystrophy type 1 and myotonic dystrophy type 2.
Table 1. Comparison of myotonic dystrophy type 1 and myotonic dystrophy type 2
| Feature | Myotonic dystrophy type 1 | Myotonic dystrophy type 2 |
| age of onset | birth to adulthood | 8 to 60 years |
| earlier onset with each generation | often occurs | doesn’t appear to occur |
| facial weakness | prominent | mild |
| drooping eyelids | prominent | mild |
| neck muscle weakness | common, early | common, early |
| hip and thigh weakness | late | early |
| distal muscle weakness | prominent | mostly hands |
| weakness anywhere | can occur | can occur |
| muscle pain | can occur | often occurs |
| myotonia | occurs | occurs |
| enlargement of calf muscles | does not occur | occurs |
| early cataracts (of the eyes) | occurs | occurs |
| early balding in males | common | common |
| cardiac rhythm abnormalities | common | variable |
| cardiac muscle degeneration | can occur, especially late in disease course | not common |
| excessive daytime sleepiness | common | variable |
| cognitive impairment | occurs often; can be mild to severe | can occur; generally mild |
| respiratory abnormalities | common, particularly sleep-disordered breathing and inadequate breathing | not common |
| gastrointestinal disturbances | difficulty swallowing, constipation, diarrhea, gallstones can occur | not common |
| uterine dysfunction during labor and delivery | can occur | not common |
| high blood sugar because of insulin resistance | can occur | can occur |
Myotonic dystrophy is the most common form of muscular dystrophy that begins in adulthood. Myotonic dystrophy affects at least 1 in 8,000 people worldwide. The prevalence of the two types of myotonic dystrophy varies among different geographic and ethnic populations. In most populations, type 1 appears to be more common than type 2. However, recent studies suggest that type 2 may be as common as type 1 among people in Germany and Finland.
There is currently no cure or specific treatment for myotonic dystrophy. Ankle supports and leg braces can help when muscle weakness gets worse. There are also medications that can lessen the myotonia. Other symptoms of myotonic dystrophy such as the heart problems, and eye problems (cataracts) can also be treated.
Does myotonic dystrophy cause fatigue?
Yes. Sleepiness and fatigue are common features of myotonic dystrophy type 1. Medications to reduce fatigue are available. It’s recommend that you dicuss your treatment options with a healthcare provider.
In addition, heart block is a common and potentially dangerous complication of myotonic dystrophy type 1, that can cause light headedness, dizzy spells, near fainting, and fainting. These symptoms should be reported to your doctor right away.
Myotonic dystrophy type 1
Myotonic dystrophy type 1 the most common type of myotonic dystrophy, one of the two types of myotonic dystrophy, is an inherited type of muscular dystrophy that affects the muscles and other body systems (e.g., heart, eyes, endocrine system, and central nervous system) 1. Myotonic dystrophy type 1 results from an abnormal DNA expansion in the DMPK gene on chromosome 19.
Within myotonic dystrophy type 1 there are three additional subtypes that somewhat overlap, depending on a person’s age at onset of symptoms. The age of onset is roughly correlated with the size of the DNA expansion, with larger expansions associated with earlier disease onset.
The subtypes of myotonic dystrophy type 1 are:
- Congenital-onset myotonic dystrophy type 1 — begins at or around the time of birth and is characterized by severe muscle weakness, cognitive impairment and other developmental abnormalities
- Juvenile-onset myotonic dystrophy type 1 — begins during childhood (after birth but before adolescence) and is characterized by cognitive and behavioral symptoms, muscle weakness, myotonia (difficulty relaxing muscles after use) and other symptoms
- Adult-onset myotonic dystrophy type 1 — begins in adolescence or early adulthood and is characterized by slowly progressive weakness, myotonia, cardiac abnormalities and, sometimes, mild to moderate cognitive difficulties
Myotonic dystrophy type 1 is inherited in an autosomal dominant manner and is caused by mutations in the DMPK gene. Treatment is based on the signs and symptoms present 2.
People with myotonic dystrophy type 1 are at risk for complications involving the use of anesthesia. Close consultation among the medical team and the anesthesiologist should be recommended before a person with myotonic dystrophy type 1 undergoes any procedure that requires anesthesia. An anesthesiologist experienced with treating individuals with muscle disorders like myotonic dystrophy type 1 is recommended.
Adult Onset myotonic dystrophy type 1
This is the most common form of myotonic dystrophy. People may have mild disease or severe complications. Mild myotonic dystrophy type 1 may be associated with cataract, mild myotonia and sometimes diabetes. Men with the mild form have an increased likelihood of going bald. Affected individuals may have fully active lives with little impact on the lifespan or quality of life.
Individuals with a more severe form of myotonic dystrophy type 1 (commonly referred to as the classic form) have muscle weakness that most often affects certain muscles including a muscle that elevates the upper eyelid, a muscle that helps people to chew (masticate), a muscle that helps to move the neck, the muscles of the forearm closest to the hands, certain muscles in the hands, and muscles of the lower legs that help to move the ankles. Less often, muscles around the eyes (extraocular), a group of muscles located on the front of the thighs (quadriceps) and various muscles of the respiratory tract are affected. Muscle weakness and wasting is progressive. Muscle pain and fatigue are common.
For some people, it may take longer for their muscles to relax after using them (myotonia). This is often described as the muscles stiffening. Myotonia is usually mild or moderate in severity. Two common examples of myotonia are being unable to release a doorknob after opening or shutting a door, or taking a moment to be able to release a person’s hand after shaking hands.
Because of weakness of facial muscles, affected individuals may not have facial expressions or have a mask-like facial appearance. Because of weakness of the muscle that elevates the upper eyelids, the eyelids may droop and hang partially in front of the eyes (ptosis). Some individuals may have slurred speech because of weakness of muscles required to speak.
Many people with myotonic dystrophy type 1 have conduction defects of the heart. This means that there are problems with the transfer of electrical impulses (conduction) that regulate the normal, rhythmic pumping action of the heart. The normal heart has four chambers. The two upper chambers are the atria and the two lower chambers are the ventricles. Within the right atrium of a normal heart is a natural pacemaker that initiates and controls the heartbeat. The electrical stimulus travels from the pacemaker (sinoatrial or SA node) to the ventricles along a very specific path consisting of conducting tissue and known as the AV (atrioventricular) node. If the electrical impulse is transmitted normally, the heart behaves normally. If the transmission of the signal is impeded, the blocked transmission is known as a heart block or an AV block. People with myotonic dystrophy type 1 may have irregular heartbeats (arrhythmias), disease of the heart muscle (cardiomyopathy), overgrowth of the left ventricle (ventricular hypertrophy). The various heart abnormalities potentially associated with myotonic dystrophy type 1 can lead to life-threatening complications.
Weakness of muscles necessary for breathing can occur and can lead to hypoventilation, which is the insufficient exchange of carbon dioxide and oxygen in the lungs. People with hypoventilation breathe at a slower rate and there is an increased about of carbon dioxide in the blood. It is possible for respiratory failure to occur, particularly late in life.
Individuals with myotonic dystrophy type 1 can develop problems in the gastrointestinal system. This involves the smooth muscle of the stomach and intestines. Affected individuals may have abdominal pain, gallstones, constipation, diarrhea, loss of bladder control (incontinence), and pseudo-obstruction, which is caused by abnormalities in the involuntary, coordinated muscle contractions (peristalsis) of the gastrointestinal tract. Peristalsis propels food and other material through the digestive system. Because of weakened muscles, peristalsis becomes altered and inefficient. Symptoms of pseudo-obstruction resemble those caused by mechanical obstruction of the small bowel. Mechanical obstruction refers to something (such as a tumor, scar tissue, etc.) physically blocking the passage of food and other material through the gastrointestinal tract. With pseudo-obstruction, no such physical obstruction is present. Common symptoms include nausea, vomiting, abdominal pain, abdominal swelling (distention) and constipation.
Some individuals with myotonic dystrophy type 1 have difficulty swallowing (dysphagia). Dysphagia may result in aspiration pneumonia, an infection that develops when food, saliva and bacteria are inhaled into the lungs. This can potentially be a life-threatening complication.
Men who have myotonic dystrophy type 1 have changes in hormones that cause balding. Some men are unable to father a child (infertility) due to underdevelopment of the testes (hypogonadism). People with the classic or adult form of myotonic dystrophy are also at a greater risk of developing diabetes. Some individuals have problems with their sleep including sleep apnea, and episodes of drowsiness, tiredness and lack of energy during the day (excessive daytime sleepiness). Some individuals have small, benign growths called pilomatrixomas and epitheliomas, particularly on the scalp. Behavioral issues including obsessive-compulsive disorder and passive-aggressive personality have been reported.
Juvenile myotonic dystrophy type 1
Some medical sources classify certain individuals with myotonic dystrophy type 1 as having juvenile myotonic dystrophy type 1. Onset is often before the age of 12. They may or may not have signs of muscle weakness or myotonia. Affected individuals usually have some intellectual and behavioral issues such as learning disabilities and difficulties with socialization at school. Difficulty with speech (dysarthria), hearing problems, and problems with coordination may also occur. Heart issues including heart rhythm disturbances and irregular heartbeats (arrhythmias) have been reported. Heart issues have occurred in adolescents who did not have any other symptoms.
Congenital myotonic dystrophy type 1
Congenital myotonic dystrophy type 1 is the most severe form of myotonic dystrophy. Infants show signs and symptoms of the disorder at birth (congenital) including severe muscle weakness and hypotonia. Hypotonia is when an infant lacks muscles tone; such infants are described as ‘floppy’. Some infants have muscle weakness affecting both sides of the face (facial diplegia). Clubfoot (talipes equinovarus), in which the foot appears to be turned in toward the body, is also common at birth.
Some infants have a low clarity of vision (visual acuity), farsightedness (hyperopia), and an abnormal curving of the lenses of the eye (astigmatism), which can contribute to poor or blurred vision. Mild to moderate intellectual disability can also occur in infants and children with congenital myotonic dystrophy type 1. Learning and behavioral disabilities may become apparent as children grow older. The intellectual disability seems to be related to abnormal development of parts of the brain, presumably caused by genetic abnormalities. Some experts have suggested that the very high incidence of labor and delivery complications in mothers with myotonic dystrophy also could be a contributing factor to the cognitive problems seen in these babies.
Poor feeding is common in affected infants and they often fail to grow and gain weight as expected (failure to thrive). Some infants have gastroparesis, a condition in which there is sluggish emptying of solid food (and more rarely, liquid nutrients) from the stomach. This can result in persistent digestive symptoms, especially nausea.
Infants and children with congenital myotonic dystrophy type 1 may have breathing difficulties due to muscle weakness. Breathing difficulties are often severe and can lead to respiratory failure, which is a common cause of mortality in congenital myotonic dystrophy type 1.
Infants and children with congenital myotonic dystrophy type 1 who survive early, severe complications will go on and develop symptoms of adult onset myotonic dystrophy type 1 including heart (cardiac) abnormalities. Cardiac issues can begin as early as the second decade of life. In rare instances, severely affected infants can have cardiac abnormalities in the newborn (neonatal) period.
Myotonic dystrophy type 1 cause
Myotonic dystrophy type 1 is caused by a mutation called a CTG trinucleotide repeat in the DMPK gene 1. It is made up of three DNA building blocks (CTG stands for cytosine, thymine, and guanine) that appear multiple times in a row. If the number of CTG repeats is more than 34, it creates an unstable region in the gene 1. Repeats between 35 and 49 are considered premutations. Individuals with CTG repeats in this range do not have symptoms themselves, but their children are at increased risk of inheriting a larger repeat size and thus having symptoms 2.
The protein made by the DMPK gene is believed to play a role in communication and impulse transmission within and between cells. It appears to be important for the correct functioning of cells in the heart, brain, and skeletal muscles 1. The more than normal number of CTG repeats leads to the creation of longer and toxic RNA. This causes problems for cells mainly because it traps and disables important proteins 3. This prevents cells in muscles and other tissues from functioning normally, leading to the signs and symptoms of myotonic dystrophy type 1 2.
Myotonic dystrophy type 1 inheritance
Myotonic dystrophy type 1 is inherited in an autosomal dominant pattern, which means one copy of the mutated DMPK gene in each cell is sufficient to cause the disorder. In most cases, the person with myotonic dystrophy type 1 has a parent who also has the disorder 2. The children of a person with myotonic dystrophy type 1 have a 50% chance of inheriting the disorder 2.
As myotonic dystrophy is passed from one generation to the next, the disorder generally begins earlier in life and signs and symptoms become more severe. This phenomenon is called anticipation. It is caused by an increase in the length of the number of CTG repeats (unstable region) in the DMPK gene 1. The expansion of the unstable region causes the features of the disorder to become more severe with each successive generation.
Some people diagnosed with myotonic dystrophy type 1 have a parent who has the signs and symptoms of the disorder; others do not. A parent may appear to be unaffected because symptoms may be mild or absent. Genetic testing is available to confirm the presence of the condition 2.
Myotonic dystrophy type 1 symptoms
People with myotonic dystrophy type 1 have progressive muscle wasting and weakness beginning in their 20’s or 30’s. The muscle wasting and weakness develop in their lower legs, hands, neck and face. They also have stiffness and tightness of their muscles (called myotonia), so they are slow to relax certain muscles after using them. This condition is characterized by difficulty releasing the hand from a handshake or a doorknob. In addition to muscle weakness and wasting, people who have myotonic dystrophy type 1 may have fatigue, muscle pain, difficulty swallowing, clouding of the lens in their eyes (cataracts), and irregularities in the electrical control of their heartbeat (cardiac conduction defects). People with advanced disease may develop respiratory complications. Men with myotonic dystrophy type 1 have changes in their hormones that can cause balding and sometimes the inability to father a child (infertility) 2. The severity of symptoms varies among people with myotonic dystrophy type 1.
Myotonic dystrophy type 1 is associated with an increased risk for a variety of vision and eye problems, including 4:
- Drooping eyelids (ptosis)
- Cataracts
- Weakened eye muscles (affecting range of eye movement and ease of opening and closing eyes)
- Refractive error (often farsighted vision)
- Astigmatism
- Retinal changes
- Strabismus (eyes do not line up in the same direction)
Compared to myotonic dystrophy type 2, myotonic dystrophy type 1 is more severe and may affect lifespan 2.
Treatment of eye and vision problems must be individually tailored. Refractive error and astigmatism can be corrected with eyeglasses, contact lenses, or surgery. Special glasses with eye “crutches” can be used to improve vision in people with ptosis. Surgery can be done to treat ptosis and cataracts, however ptosis often recurs and special precautions must be taken with anesthesia. If severe, strabismus may also be treated with surgery.
Myotonic dystrophy type 2
Myotonic dystrophy type 2 was originally called PROMM for proximal myotonic myopathy, one of the two types of myotonic dystrophy, is an inherited muscular dystrophy that affects the muscles and other body systems (e.g., heart, eyes, and pancreas). It is characterized by prolonged muscle tensing (myotonia) as well as muscle weakness, pain, and stiffness. Signs and symptoms usually develop during a person’s twenties or thirties. Muscles in the neck, fingers, elbows, and hips are typically affected; facial and ankle muscles are less commonly involved 5. The severity of myotonic dystrophy type 2 varies widely among affected people, even among family members 6. It is inherited in an autosomal dominant pattern and is caused by mutations in the CNBP gene 6. Treatment is based on each person’s specific signs and symptoms.
Myotonic dystrophy type 2 cause
Mutations in the CNBP gene cause myotonic dystrophy type 2. The exact function of this gene is not known. The protein made by the CNBP gene (also called ZNF9 gene, a gene on chromosome 3) is mainly found in the heart and in skeletal muscles, where it probably helps regulate the function of other genes 1.
In people with myotonic dystrophy type 2, a short piece of DNA is abnormally repeated many times, forming an unstable area of the gene. The mutated gene makes an altered version of messenger RNA (mRNA), which is a copy of the gene that is normally used for protein production. The abnormal mRNA forms clumps inside the cell that interfere with the production of many proteins. These changes prevent cells in muscles and other tissues from functioning normally, leading to the signs and symptoms of myotonic dystrophy 6.
Myotonic dystrophy type 2 inheritance
Myotonic dystrophy type 2 is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is enough to cause symptoms of the condition. In most cases, an affected person has one affected parent.
As myotonic dystrophy is passed from one generation to the next, it generally begins earlier in life and signs and symptoms become more severe. This phenomenon is called anticipation. The cause of the anticipation in families with myotonic dystrophy type 2 is unknown 6.
Myotonic dystrophy type 2 symptoms
Myotonic dystrophy type 2 is characterized by progressive muscle wasting and weakness. Symptoms typically begin in a person’s twenties. People with this condition often have prolonged muscle contractions (myotonia) and are not able to relax certain muscles after use. For example, a person may have difficulty releasing their grip on a doorknob or handle. Also, affected people may have slurred speech; temporary locking of their jaw; and muscle pain and weakness that mainly affects the neck, shoulders, elbows, and hips. Less common symptoms include abnormalities of the electrical signals that control the heartbeat (cardiac conduction defects); clouding of the lens in the eyes (cataracts); and diabetes. Males may experience balding and infertility. The severity of symptoms varies among affected people. Compared to myotonic dystrophy type 1, type 2 is milder and does not necessarily shorten a person’s lifespan 1.
Myotonic dystrophy type 2 diagnosis
Myotonic dystrophy is diagnosed by doing a physical exam. A physical exam can identify the typical pattern of muscle wasting and weakness and the presence of myotonia. A person with myotonic dystrophy may have a characteristic facial appearance of wasting and weakness of the jaw and neck muscles. Men may have frontal balding 6.
There are several laboratory tests that can be used to clarify the clinical diagnosis of myotonic dystrophy. One test, called electromyography (EMG), involves inserting a small needle into the muscle. The electrical activity of the muscle is studied and usually shows characteristic patterns of muscle electrical discharge 6. The definitive test for myotonic dystrophy type 2 is a genetic test. For this test, certain cells within the blood are analyzed to identify a change (mutation) in the CNBP gene 6.
The University of Washington provides more information on genetic testing for myotonic dystrophy type 2 in their publication titled, “Myotonic Dystrophy: Making an Informed Choice About Genetic Testing.” (https://depts.washington.edu/neurolog/images/neurogenetics/myotonic.pdf)
Myotonic dystrophy type 2 treatment
There is currently no treatment available to stop or slow the progression of myotonic dystrophy type 2. Management options depend on the symptoms that each affected person has, and aim to treat each specific symptom. For example 5:
- Ankle-foot braces, wheelchairs, or other assistive devices may be used as needed for weakness
- Defibrillator placement may be needed for arrhythmias
- Cataracts can be removed for those with impaired vision
- Testosterone replacement therapy may be useful for hypogonadism in males
Myotonia is usually mild and rarely requires treatment. Routine exercise appears to help with pain control, as well as with muscle strength and endurance. The effectiveness of most medications for pain management varies. Mexilitene, which is very effective for some forms of myotonia, has helped control muscle pain in some people with this condition. Other medications that have been used with some success include gabapentin, nonsteroidal anti-inflammatory drugs (NSAIDS), low-dose thyroid replacement, low-dose steroids, and tricyclic antidepressants. Cholesterol-lowering medications should be avoided when they are associated with increased weakness 5.
There are steps a person can take to prevent some secondary complications. Anesthetic risk may be increased, so careful assessment of heart and respiratory function before and after surgery are recommended. Affected people should also have a yearly electrocardiogram or cardiac MRI to detect possible conduction defects or cardiomyopathy 5.
Myotonic dystrophy cause
Myotonic dystrophy type 1 is caused by mutations in the DMPK gene (a gene on chromosome 19), while type 2 results from mutations in the CNBP gene (ZNF9) (a gene on chromosome 3). The specific functions of these genes are unclear. The protein produced from the DMPK gene may play a role in communication within cells. It appears to be important for the correct functioning of cells in the heart, brain, and skeletal muscles (which are used for movement). The protein produced from the CNBP gene is found primarily in the heart and in skeletal muscles, where it probably helps regulate the function of other genes.
Similar changes in the structure of the DMPK and CNBP genes cause the two forms of myotonic dystrophy. In each case, a segment of DNA is abnormally repeated many times, forming an unstable region in the gene. The mutated gene produces an expanded version of messenger RNA, which is a molecular blueprint of the gene that is normally used to guide the production of proteins. The abnormally long messenger RNA forms clumps inside the cell that interfere with the production of many other proteins. These changes prevent muscle cells and cells in other tissues from functioning normally, which leads to the signs and symptoms of myotonic dystrophy.
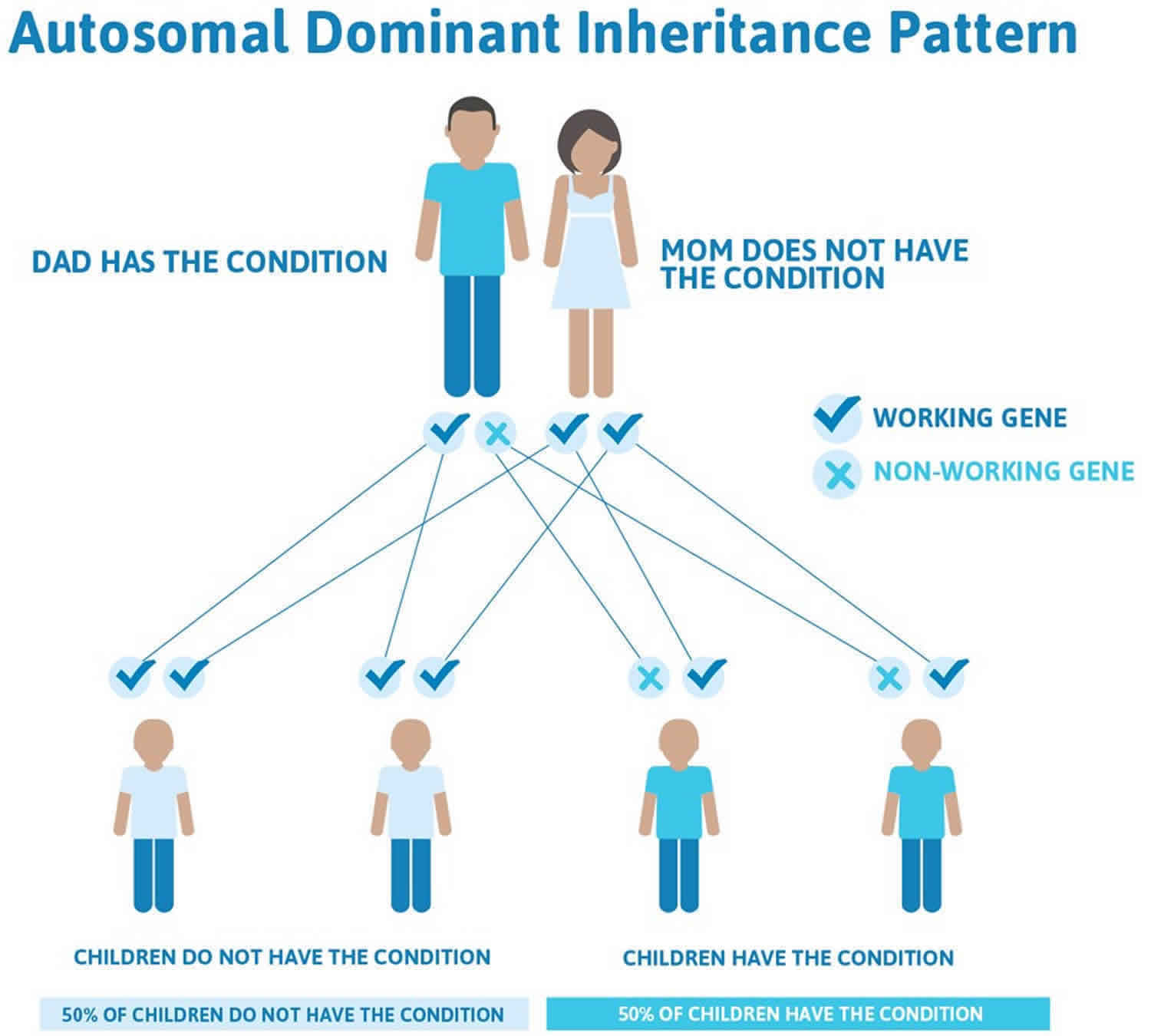
Myotonic dystrophy inheritance
Both types of myotonic dystrophy are inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder. In most cases, an affected person has one parent with the condition.
In cases where the autosomal dominant condition does run in the family, the chance for an affected person to have a child with the same condition is 50% regardless of whether it is a boy or a girl. These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
- When one parent has the abnormal gene, they will pass on either their normal gene or their abnormal gene to their child. Each of their children therefore has a 50% (1 in 2) chance of inheriting the changed gene and being affected by the condition.
- There is also a 50% (1 in 2) chance that a child will inherit the normal copy of the gene. If this happens the child will not be affected by the disorder and cannot pass it on to any of his or her children.
As myotonic dystrophy is passed from one generation to the next, the disorder generally begins earlier in life and signs and symptoms become more severe. This phenomenon, called anticipation, has been reported with both types of myotonic dystrophy. However, the evidence for anticipation appears to be strongest in myotonic dystrophy type 1. In this form of the disorder, anticipation is caused by an increase in the length of the unstable region in the DMPK gene. It is less clear whether anticipation occurs in myotonic dystrophy type 2, and the mechanism is unknown. A longer unstable region in the CNBP gene does not appear to influence the age of onset of the disorder.
Figure 1. Myotonic dystrophy autosomal dominant inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Myotonic dystrophy symptoms
Myotonic dystrophy is a very complicated condition. The symptoms and disease progression can vary widely. The effects can be quite different even among members of the same family, so it is difficult to predict just how myotonic dystrophy will affect you and your family. One person may only have mild muscle pain or cataracts that develop in later years, while someone else with the condition may be born with serious breathing problems.
The most common people who have myotonic dystrophy have progressive muscle weakness (myopathy), trouble relaxing a muscle (myotonia), and muscle wasting (atrophy) that gets worse over time beginning in their 20’s or 30’s. The muscle wasting and weakness develop in their lower legs, hands, neck and face. They also have stiffness and tightness of their muscles (called myotonia), so they are slow to relax certain muscles after using them. Not being able to release their grip on in a handshake or a doorknob is one example of this problem.
In addition to muscle weakness and wasting, people who have myotonic dystrophy have clouding of the lens in their eyes (cataracts), and irregularities in the electrical control of their heartbeat (cardiac conduction defects).
Men who have myotonic dystrophy have changes in their hormones that can cause balding and sometimes the inability to father a child (infertility).
Myotonic dystrophy can also cause problems with heart, lungs, gastrointestinal (GI) system, cognitive function, personality, and vision. Not everyone with myotonic dystrophy will have all or even most of the possible symptoms.
Babies who are born with signs and symptoms of myotonic dystrophy have congenital myotonic dystrophy. They have weakness of all their muscles, breathing problems, and developmental delays including mental retardation. Sometimes these medical conditions are so severe they may cause death.
Myotonic dystrophy diagnosis
Myotonic dystrophy is diagnosed by doing a physical exam. A physical exam can identify the typical pattern of muscle wasting and weakness and the presence of myotonia. A person with myotonic dystrophy may have a characteristic facial appearance of wasting and weakness of the jaw and neck muscles. Men may have frontal balding.
There are several laboratory tests that can be used to clarify the clinical diagnosis of myotonic dystrophy. One test, called electromyography (EMG), involves inserting a small needle into the muscle. The electrical activity of the muscle is studied and usually shows characteristic patterns of muscle electrical discharge.
The definitive test for myotonic dystrophy is a genetic test. For this test, a blood sample is taken to identify the altered gene (mutation) within the chromosomes which are contained within the white blood cells. Gene alterations in two genes – CNBP and DMPK – cause myotonic dystrophy. Myotonic dystrophy Type 1 is caused by a mutation in the DMPK gene. Type 2 myotonic dystrophy is caused by a mutation in the CNBP gene (also called the ZNF9 gene). Mutations in each of these genes involve a short segment of DNA that is abnormally repeated many times. This abnormal repetition forms an unstable region of the gene. These changes keep cells in the muscles and other body tissues from functioning normally, leading to signs and symptoms of myotonic dystrophy.
Myotonic dystrophy treatment
There is currently no cure or specific treatment for myotonic dystrophy 6. Treatment is aimed at managing symptoms of the disease 7. Routine physical activity appears to help maintain muscle strength and endurance and to control musculoskeletal pain 5. Canes, braces, walkers, and scooters can help as muscle weakness progresses 6.
There are also medications that can lessen pain associated with myotonic dystrophy 6. Pain management can be achieved through the use of medications prescribed by a doctor 2. A variety of medications have been used including nonsteroidal anti-inflammatories (NSAIDs), gabapentin, tricyclic antidepressants, mexiletine, and low-doses of glucocorticoids such as prednisone.
Heart problems associated with myotonic dystrophy can be treated through the insertion of a pacemaker, medications, and regular monitoring of cardiac function. A pacemaker sends pulses to speed up a heart when there is an abnormally slow heartbeat or rhythm. An implantable cardioverter defibrillator (ICD) sends a shock to the heart if it is beating irregularly in order to return the heartbeat to normal.
Testosterone replacement therapy may be used to treat infertility in males 8.
Cataracts can be removed surgically if they affect vision. However, there have been reports that cataracts can recur after removal.
Drooping of the upper eyelid (ptosis) can be treated by an eyelid crutch, which is a small device added onto to existing glasses to prop the eyelid up. Sometimes blepharoplasty is required. This surgery involves removing excess muscle, fat and other tissue.
Some people with breathing problems during sleep may require non-invasive ventilation, which involves breathing support with a mask or similar device.
Some infants with congenital myotonic dystrophy type 1 require ongoing breathing support with a machine. Some infants require a gastronomy tube, which is a thin tube that is inserted directly into the stomach through a small surgical opening. This ensures that infants receive the required nutrients, but avoid the risk of aspiration.
Some affected individuals may develop hypothyroidism, a condition characterized by underactivity of the thyroid gland. This means that the thyroid produces low levels of thyroid hormone. Hypothyroidism has been shown to worsen myotonic dystrophy. Hypothyroidism is treated by medications that replace the activity of the underproduced hormones.
Current research is focusing on how scientists might be able to one day use gene-editing technology or other treatments to remove the clumps of RNA that cause the symptoms of myotonic dystrophy. However, this therapy is not yet possible in humans 9.
Myotonic dystrophy life expectancy
The long-term outlook (prognosis) for each person with myotonic dystrophy including life expectancy may depend on the type of myotonic dystrophy and the specific medical problems present. Myotonic dystrophy is a progressive disease, meaning that symptoms worsen as a person gets older 10.
Although evidence is limited, life expectancy appears to be reduced for people with myotonic dystrophy type 1. The most common causes of death in people with myotonic dystrophy type 1 are respiratory and cardiac (heart) symptoms. An increased risk of death may be associated with younger age of onset, more severe muscle weakness, and cardiac conduction defects. People with more mild symptoms of myotonic dystrophy type 1 may have a normal lifespan 11.
Definitive information about prognosis in people with myotonic dystrophy type 2 is limited, but the condition generally runs a milder course. In general, people with myotonic dystrophy type 2 have a better long-term outlook (prognosis) than those with type 1. Symptoms are usually relatively mild. People with myotonic dystrophy type 2 may have a normal lifespan 11. While the rate of progression can vary among affected people, symptoms generally progress slowly 12. While mobility may be impaired at an earlier age, the ability to walk is often retained until around 60 years of age 12.
The prognosis for affected people can depend on the extent of heart (cardiac) involvement 12. While definitive information is not available, it appears there is relatively little shortening of the lifespan in people with myotonic dystrophy type 2 11.
- Myotonic dystrophy. https://ghr.nlm.nih.gov/condition/myotonic-dystrophy[↩][↩][↩][↩][↩][↩][↩]
- Bird TD. Myotonic Dystrophy Type 1. 1999 Sep 17 [Updated 2018 Dec 6]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1165[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- MMD Research: Seeking to Free Proteins from a ‘Toxic Web’ https://www.mda.org/quest/article/mmd-research-seeking-to-free-proteins-from-a-toxic-web[↩]
- Ekström AB et al. Visual function in congenital and childhood myotonic dystrophy type 1. Ophthalmology. 2010 May;117(5):976-82; http://www.ncbi.nlm.nih.gov/pubmed/20346513[↩]
- Dalton JC, Ranum LPW, Day JW. Myotonic Dystrophy Type 2. 2006 Sep 21 [Updated 2013 Jul 3]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1466[↩][↩][↩][↩][↩]
- About Myotonic Dystrophy. https://www.genome.gov/Genetic-Disorders/Myotonic-Dystrophy[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- O’Sullivan Smith C, Bennett RL, and Bird TD. Myotonic Dystrophy: Making an Informed Choice About Genetic Testing. Department of Neurology, University of Washington School of Medicine. http://depts.washington.edu/neurolog/images/neurogenetics/myotonic.pdf[↩]
- Myotonic Dystrophy (DM). https://www.mda.org/disease/myotonic-dystrophy/medical-management/adult-dm1-dm2-juvenile-dm1[↩]
- Batra R, Nelles DA, Pirie E, Blue SM, Marina RJ, Wang H, Chaim IA, Thomas JD, Zhang N, Nguyen V, Aigner S, Markmiller S, Xia G, Corbett KD, Swanson MS, and Yeo GW. Elimination of Toxic Microsatellite Repeat Expansion RNA by RNA-Targeting Cas9. Cell. August 8, 2017; https://www.ncbi.nlm.nih.gov/pubmed/28803727[↩]
- Managing DM: FAQs. Myotonic Dystrophy Foundation. http://www.myotonic.org/what-dm/faqs[↩]
- Myotonic dystrophy: Etiology, clinical features, and diagnosis. https://www.uptodate.com/contents/myotonic-dystrophy-etiology-clinical-features-and-diagnosis[↩][↩][↩]
- Myotonic Dystrophy (DM). https://www.mda.org/disease/myotonic-dystrophy[↩][↩][↩]