What are night sweats
Night sweats are repeated episodes of extreme perspiration that may soak your nightclothes or bedding and are related to an underlying medical condition or illness. If you wake up with your pijamas and sheets soaked with perspiration, even if it’s not hot or you don’t have too many blankets on the bed, you may be having night sweats. Men, women and children can have night sweats.
You may occasionally awaken after having perspired excessively, particularly if you are sleeping under too many blankets or if your bedroom is too warm. Although uncomfortable, these episodes are usually not labeled as night sweats and typically aren’t a sign of a medical problem.
Night sweats are when you sweat so much that your night clothes and bedding are soaking wet, even though where you’re sleeping is cool.
In general, night sweats are also associated with fever, weight loss, localized pain, cough, diarrhea, or other symptoms of concern.
Night sweats and hot flashes are very common among women around the time of menopause. If you are around age 50 and are having irregular or absent menstrual periods, and have no other symptoms, this is likely the cause of your symptoms.
The most common reasons for night sweats are:
- menopause symptoms (“hot flushes”)
- anxiety
- medicines – some antidepressants, steroids and painkillers
- low blood sugar (hypoglycemia)
- alcohol or drug use
- a harmless condition called hyperhidrosis that makes you sweat too much all the time
Sometimes the cause of night sweats is unknown.
Schedule a doctor’s visit if night sweats:
- Occur on a regular basis
- Interrupt your sleep
- Are accompanied by a fever (or feel hot and shivery), weight loss, localized pain, cough, diarrhea, or other symptoms of concern
- Come on after your menopause symptoms have been absent for months to years
- You have night sweats regularly that wake you up or you’re worried
- You have night sweats and you’re losing weight for no reason
Night sweats causes
There are many causes of night sweats and most are not serious. In some cases, night sweats are a sign of a medical condition. In others, they may be caused by a medication that you are taking.
Medical conditions that can cause night sweats
Diseases and conditions that can cause night sweats include:
- Anxiety disorders
- Autoimmune disorders
- Autonomic neuropathy (damage to your autonomic nerves)
- Brucellosis (a bacterial infection)
- Cancers and tumors
- Carcinoid syndrome (a certain type of cancerous tumor in your intestines)
- Chronic eosinophilic pneumonia
- Chronic fatigue syndrome
- Diabetes insipidus 1
- Drug addiction (substance use disorder) or withdrawal (alcohol, opioids, cocaine, cannabis, benzodiazepines)
- Endocarditis (an infection of the inner lining of the heart)
- Endocrine
- Ovarian failure
- Hyperthyroidism
- Diabetes mellitus (nocturnal hypoglycemia)
- Endocrine tumors (pheochromocytoma, carcinoid tumor)
- Orchiectomy 2
- Gastroesophageal reflux disease
- Granulomatous disease 3
- HIV/AIDS
- Hodgkin’s lymphoma (Hodgkin’s disease)
- Hyperhidrosis — a condition in which the body continually produces too much sweat for no clear reason
- Hyperthyroidism (overactive thyroid)
- Infections
- Human immunodeficiency virus (HIV)
- Tuberculosis
- Mycobacterium avium complex
- Infectious mononucleosis
- Fungal infections (histoplasmosis, coccidioidomycosis)
- Lung abscess 4
- Endocarditis
- Other infection
- Leukemia
- Lymph node hyperplasia 5
- Menopause
- Myelofibrosis (a bone marrow disorder)
- Non-Hodgkin’s lymphoma
- Osteomyelitis (a bone infection)
- Pheochromocytoma (a rare adrenal gland tumor)
- Pregnancy 6
- Pyogenic abscess (a pus-filled cavity caused by an infection)
- Rheumatologic
- Takayasu’s arteritis
- Temporal arteritis 7
- Sleep disorders such as obstructive sleep apnea
- Stroke
- Syringomyelia (a fluid-filled cyst in the spinal cord)
- Thyroid disease
- Tuberculosis
Medications that can cause night sweats
Night sweats are a common side effect of many medications, such as:
- Antihypertensives
- Depression medications (antidepressants)
- Drugs used to treat diabetes (if the level of sugar in your blood gets too low) (hypoglycemic agents)
- Hormone-blocking drugs used to treat certain cancers (hormone therapy)
- Cortisones
- Drugs to reduce fevers (salicylates or aspirin, acetaminophen) can cause night sweats as a side effect.
- Phenothiazines
- Substances of abuse: alcohol, heroin
Table 1. Drugs with the Labeled Side Effect of Night Sweats
| Drug | Incidence |
|---|---|
Donepezil (Aricept) | Infrequent |
Indinavir (Crixivan) | Infrequent |
Saquinavir (Fortovase, Invirase) | Less than 2 percent |
Zalcitabine (Hivid) | Less than 1 percent |
Cyclosporine (Neoral, Sandimmune) | Rare |
Pegaspargase (Oncaspar) | 1 to 5 percent |
Rituximab (Rituxan) | Among most frequent |
Interferon alfa-2a (Roferon) | 8 percent |
Daclizumab (Zenapax) | 2 to 5 percent |
Night sweats diagnosis
An extensive list of causes in patients with night sweats is provided above. The history and physical examination are aimed at revealing associated symptoms that will narrow this broad differential diagnosis and guide additional studies. Table 2 lists diagnostic actions to be considered based on findings from the history and physical.
Table 2. Evaluation of Night Sweats Based on Associated Symptoms or Signs
| Associated symptoms or signs | Action to consider |
|---|---|
Fever, TB exposure, HIV status or risk factors, cough, weight loss, immunocompromise | Purified protein derivative, chest radiograph, CBC, HIV test (CD4+ if known HIV positive), possibly blood cultures |
Menopausal | Hormone replacement therapy (an elevated FSH test if uncertain based on history, helps confirm the diagnosis) |
Firm lymphadenopathy in absence of current or recent infection | Lymph node biopsy |
Recent upper respiratory tract infection | CBC; heterophile antibodies or anti-VCA evaluation |
Diabetic | Rule out nocturnal hypoglycemia |
Overweight; excessive daytime sleepiness, partner reports loud snoring and gasping during sleep, small oropharynx | Sleep study |
Heartburn, indigestion | Trial of histamine H2 blocker |
Heat intolerance, exophthalmos, tremor, other symptoms or signs of hyperthyroidism | Thyroid function test |
Labile hypertension, paroxysms of headache or palpitations | Urine catecholamines or metanephrines measured in a 24-hour collection; if diagnosed, the tumor must be localized using radiologic imaging |
Attacks of cyanotic flushing, watery diarrhea, wheezing, hypotension, or edema | High levels of urinary 5-hydroxyindoleacetic acid (5-HIAA) confirms diagnosis. Certain foods and medications may cause false-positive results (Table 3). Once diagnosed, the tumor must be localized using radiologic imaging. |
Splinter hemorrhages, Janeway lesions, Osler’s nodes, new heart murmur | Blood cultures including HACEK organisms, echocardiogram |
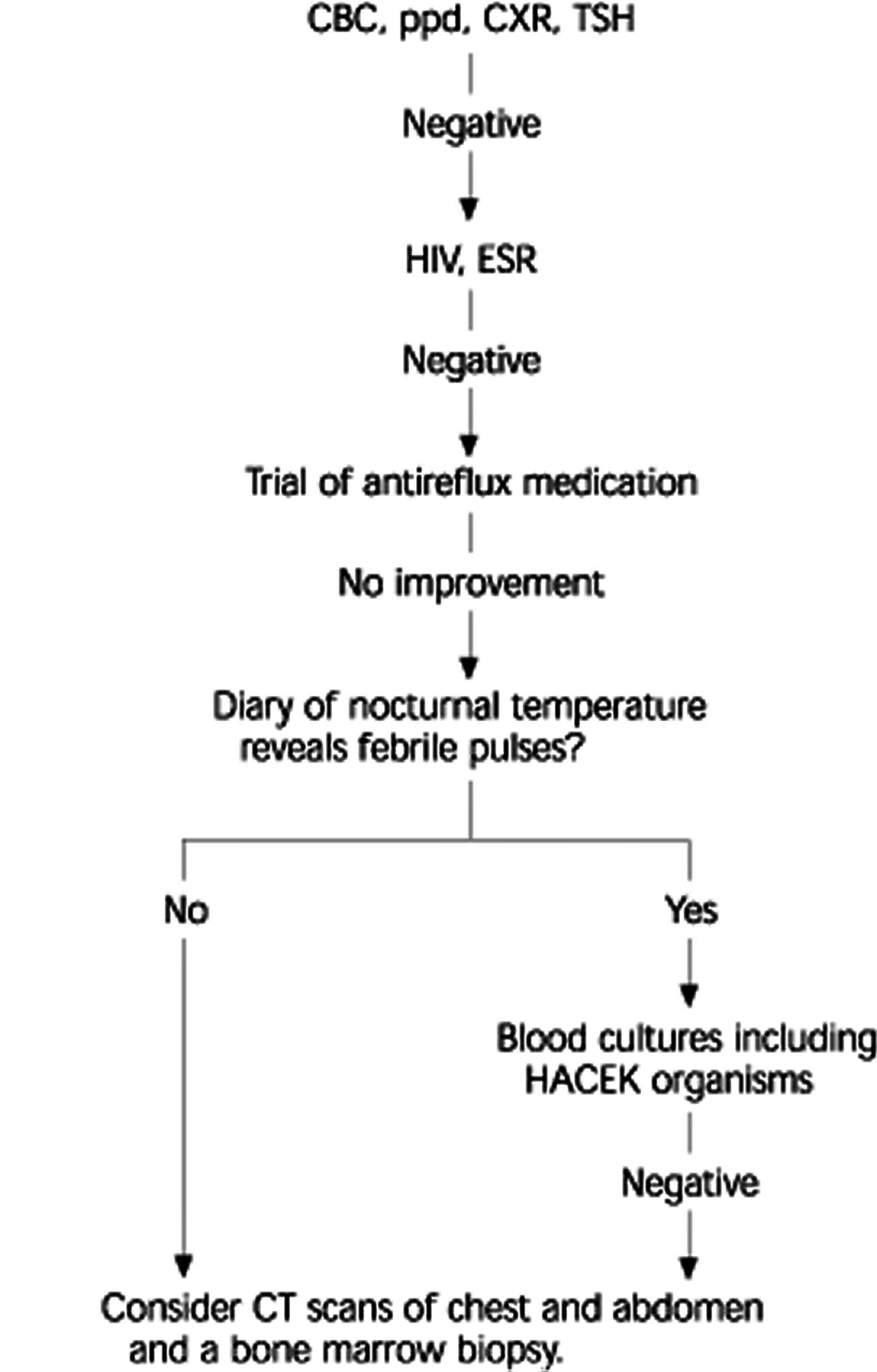
No associated symptoms or signs | See Figure 1. |
Abbreviations: TB = tuberculosis; HIV = human immunodeficiency virus; CBC = complete blood count; FSH = follicle-stimulating hormone; VCA = viral capsid antigen; HACEK = Haemophilus species; Actinobacillus;Cardiobacterium; Eikenella; Kingella.
[Source 8 ]Figure 3. Evaluating Night Sweats
Footnote: Evaluation of a patient with night sweats and no associated symptoms.
Abbreviations: CBC = complete blood count; ppd = purified protein derivative; CXR = chest radiograph, TSH = thyroid-stimulating hormone; HIV = human immunodeficiency virus; ESR = erythrocyte sedimentation rate; HACEK = Haemophilus species, Actinobacillus, Cardiobacterium, Eikenella, Kingella; CT = computed tomographic)
[Source 8 ]Table 3. Some foods and medications that may interfere with 5-hydroxyindoleacetic acid (5-HIAA) test
Tomatoes Red plums Pineapple Walnuts Avocado Eggplant Bananas | Acetaminophen Caffeine Methocarbamol (Robaxin) Diazepam (Valium) Glyceryl guaiacolate (many cough medicines) Phenothiazine* | Mephenasin carbamate (some muscle relaxants) Phenacetin Aspirin* Levodopa (Sinemet)* |
Footnote: *—May cause false-negative result.
[Source 8 ]Medical history
Physicians should ask about fever, cough, and risk factors for tuberculosis (TB). In its pulmonary form, reactivation TB generally presents with cough in addition to the constitutional symptoms of weight loss and low-grade fever. Many patients experience night sweats several times per week. A history of (or risk factors for) human immunodeficiency virus (HIV) infection is important. The most common complaint with HIV infection is fever, with or without night sweats. This may be because of the virus or the result of HIV sequelae such as lymphoma or opportunistic infections.
Most patients with acquired immunodeficiency syndrome (AIDS)-related lymphoma have a history of fever, weight loss, and night sweats 9. AIDS-related infections might also cause night sweats, including Mycobacterium avium complex (MAC) infection and cytomegalovirus (CMV) syndromes. Mycobacterium avium complex infection in patients with HIV typically presents with fever, weight loss, and night sweats. It is a late complication of HIV infection that generally occurs in patients with CD4+ cell counts of less than 100 cells per mm³. Tuberculosis (TB) also can be present in a patient infected with HIV. In this population, patients often present in the classic manner with cough, fever, and night sweats.
Sometimes, travel history is helpful in evaluating the potential for other infectious diseases. Persons with the chronic pulmonary form of histoplasmosis present similarly to those who have tuberculosis (TB), with an increasing productive cough, weight loss, and night sweats 10. Persons with coccidioidomycosis may present with cough, fever, and night sweats 11. Risk factors for endocarditis also should be determined. The symptoms of infectious endocarditis are protean and include fever, chills, fatigue, sweats, and malaise. These night sweats may be related to nocturnal fever caused by transient bacteremia.
Low-grade fever that may be associated with night sweats is the most common systemic symptom of Hodgkin’s disease (Hodgkin’s lymphoma). High fluctuating fevers accompanied by drenching night sweats (Pel-Ebstein fevers) may persist for several weeks with Hodgkin’s disease. Night sweats may be the only presenting complaint for some patients. One study 12 of patients with Hodgkin’s disease who had sweating as their only symptom found a correlation with unperceived elevations in body temperature, or minor febrile pulses. Occasionally, patients with non-Hodgkin’s lymphoma also may experience night sweats.
A history of recent upper respiratory infection may be significant because infectious mononucleosis (IM), usually caused by Epstein-Barr virus, may cause night sweats, particularly during the acute phase. In a study 13 where the symptoms of infectious mononucleosis were compared with other upper respiratory infections, night sweats were significantly more common in patients with infectious mononucleosis 13. By the third week of illness, heterophile antibodies were positive in 90 percent of patients. If heterophile antibodies are not elevated, but the diagnosis is strongly suspected, IgM antibodies to Epstein-Barr virus viral capsid antigen (anti-VCA) may be measured, because they can be elevated for weeks to months after infection.
Women in the appropriate age range should be asked about symptoms of menopause, because patients with ovarian failure may experience hot flushes. Some women may experience a predominance of these during nocturnal hours 14. An elevated follicle-stimulating hormone test may be helpful in diagnosing menopause when the history is unclear.
Patients with diabetes experiencing nocturnal hypoglycemia may have night sweats without other hypoglycemic symptoms 15. This may be caused by missing a meal or performing unusually excessive exercise. Patients who are receiving large doses of evening insulin may be especially prone to nocturnal hypoglycemia 16. Risk factors for hypoglycemia may include tight diabetes control, renal insufficiency, polypharmacy, higher sulfonylurea or insulin doses, and advanced age 16.
An association between gastroesophageal reflux disease (GERD) and night sweats has been suggested. Informal observations suggest that patients treated for GERD often have dramatic relief of their night sweats 17.
Physicians should inquire about symptoms of hyperthyroidism, such as nervousness, palpitations, weight loss, and menstrual irregularity. The heat intolerance of hyperthyroidism may lead to night sweats, especially when combined with over-bundling or an overheated room.
Sleeping partners should be questioned about the patient’s sleeping habits (snoring, apneic spells, and daytime sleepiness). Obstructive sleep apnea is a relatively common disorder affecting up to 4 percent of middle-aged men 18. It may be a common cause of heavy night sweats 19.
Several medications may contribute to night sweats, but antipyretics are the most common. Acetaminophen and aspirin are cited as causes of night sweats. This is most likely a rebound effect as the antipyretic effects subside 20. Use of some antihypertensives, anti-depressants, tamoxifen (Nolvadex), leuprolide (Lupron), and niacin are possibly causal as well 21. Alcohol use, particularly alcohol dependence, also may cause night sweats. The Physicians’ desk reference search revealed 11 pharmaceutical agents that were labeled as having night sweats as a side effect (Table 1) 22.
Directed inquiry of symptoms suggestive of myocardial ischemia, anxiety, depression, and rheumatologic diseases may be useful. While not specifically revealed in the searches, it is likely that any disease that results in autonomic overactivity (e.g., congestive heart failure via neurohumoral activation) may result in night sweats.
Carcinoid syndrome should be a consideration if the patient (usually in the sixth to eighth decade of life) has a history of attacks of severe cyanotic flushing of the skin that lasts from minutes to days and is associated with other symptoms such as watery diarrhea, wheezing, hypotension, or edema. Symptoms are caused by a tumor that secretes serotonin and other biologically active substances.
The diagnosis of pheochromocytoma should be considered for patients with paroxysms of headache, palpitations, and sweating—especially in combination with hypertension. The paroxysms typically last from minutes to hours and may occur with varying frequency from once per month to multiple times in a 24-hour period.
Physical examination
On physical examination, the patient’s vital signs (particularly temperature and blood pressure) and body habitus should be noted. Lymphadenopathy or splenomegaly may prompt an evaluation for possible lymphoma or leukemia. Lymph nodes in either form of lymphoma are generally nontender and firm. Most patients with Hodgkin’s lymphoma present with cervical lymphadenopathy, while those with non-Hodgkin’s lymphoma present with peripheral lymphadenopathy. Biopsy is essential for diagnosis.
Signs of immunocompromise may include cachexia or oral candidiasis. The oropharynx should be examined for redundant tissue consistent with the findings in obstructive sleep apnea. A fine hand tremor, exophthalmos, eyelid lag, or hyperreflexia suggests hyperthyroidism. An elevated blood pressure in association with night sweats may prompt an evaluation for pheochromocytoma. Signs of endocarditis such as splinter hemorrhages (dark red linear streaks under the nails), Janeway lesions (small, nodular hemorrhages on palms and soles), Osler’s nodes (small, tender nodules on finger or toe pads), and a heart murmur should be sought as well.
Evaluation when history and physical are unrevealing
If the history and physical examination fail to reveal the possible etiology of the patient’s symptoms, consider obtaining a complete blood count, purified protein derivative test, chest radiograph, and thyroid-stimulating hormone test. These tests are widely available, not particularly costly, and help rule out many of the potential diagnoses. An HIV test and erythrocyte sedimentation rate (ESR) evaluation may be added if necessary (see Figure 1 above). The ESR evaluation helps rule out disorders that may cause night sweats but otherwise are relatively silent early in their course, such as endocarditis and Takayasu’s arteritis.
An elevated ESR and positive blood cultures are present in more than 90 percent of cases of endocarditis. An echocardiogram also may assist in the evaluation of a patient with suspected endocarditis.
Takayasu’s arteritis is a chronic inflammatory disease involving the aorta and its branches. Its cause is unknown. It also has been called pulseless disease because of the physical examination finding of diminished pulses in the upper extremities. A patient with Takayasu’s arteritis may present with malaise, fever, night sweats, arthralgias, and weight loss months before vessel involvement is noted. An elevated ESR is a characteristic, but nonspecific laboratory finding. Diagnosis would be confirmed by aortography.
If the screening tests are normal and nocturnal GERD is suspected, a trial of antireflux measures may be considered. If the patient continues to complain of night sweats, a diary of the patient’s temperature variations through the night may be helpful in revealing the presence or absence of febrile micropulses. Febrile pulses should reprompt a search for lymphoma or endocarditis. Blood cultures should be obtained to include cultures designated for the fastidious, gram-negative HACEK (Haemophilus species, Actinobacillus, Cardiobacterium, Eikenella, and Kingella) organisms, which are not found with routine culture methods. Computed tomographic scans of the chest and abdomen, and a bone marrow biopsy to evaluate for silent neoplastic or granulomatous disease would complete the work-up.
If all studies are negative, the patient can be reassured that the night sweats are most likely benign (may be the result of over-bundling). The patient should be taught to do self lymph node examinations and report any changes noted in the absence of active infection. The patient should report development of any new symptoms and continue annual health examinations.
How to stop night sweats
Most people sweat during the night. You should see your doctor if you’re having night sweats regularly — especially if you notice other symptoms such as unexplained weight loss.
The treatment your doctor recommends will depend on what’s causing your night sweats.
If medication is the cause, there may be an alternative that your doctor can prescribe.
- Raff SB, Gershberg H. Night sweats. A dominant symptom in diabetes insipidus. JAMA. 1975;234:1252–3[↩]
- Moore CB. Night sweats in prostatic cancer. JAMA. 1969;208:155[↩]
- Adlakha A, Kang E, Adlakha K, Ryu JH. Nonproductive cough, dyspnea, malaise, and night sweats in a 47-year-old woman. Chest. 1996;109:1385–7[↩]
- Levison ME. Pneumonia, including necrotizing pulmonary infections (lung abscess). In: Isselbacher KJ, ed. Harrison’s Principles of internal medicine. 13th ed. New York: McGraw-Hill, 1994:1184–91[↩]
- McCluskey DR, Buckley MR, McCluggage WG. Night sweats and swollen glands. Lancet. 1998;351:722[↩]
- Fred HL. Night sweats. Hosp Pract. 1993;28:88)
- Prinzmetal’s angina ((Fred HL. Night sweats. Hosp Pract. 1993;28:88[↩]
- Morris GC, Thomas TP. Night sweats—presentation of an often forgotten diagnosis. Br J Clin Pract. 1991;45:145[↩]
- Diagnosing Night Sweats. Am Fam Physician. 2003 Mar 1;67(5):1019-1024. https://www.aafp.org/afp/2003/0301/p1019.html[↩][↩][↩]
- Aboulafia DM, Mitsuyasu RT. Neoplasms in the acquired immunodeficiency syndrome. In: Kelley WN, Schlossberg D, eds. Textbook of internal medicine. 3d ed. Philadelphia: Lippincott-Raven, 1997: 1895–7[↩]
- Bennett JE. Histoplasmosis. In: Isselbacher KJ, ed. Harrison’s Principles of internal medicine. 13th ed. New York: McGraw-Hill, 1994:856–7[↩]
- El-Ani AS, Elwood CM. A case of coccidioidomycosis with unique clinical features. Arch Intern Med. 1978;138:1421–2[↩]
- Gobbi PG, Pieresca C, Ricciardi L, Vacchi S, Bertoloni D, Rossi A, et al. Night sweats in Hodgkin’s disease. A manifestation of preceding minor febrile pulses. Cancer. 1990;65:2074–7[↩]
- Lambore S, McSherry J, Kraus AS. Acute and chronic symptoms of mononucleosis. J Fam Pract. 1991;33:33–7[↩][↩]
- McAllister M. Menopause: providing comprehensive care for women in transition. Lippincotts Prim Care Pract. 1998;2:256–70[↩]
- Gale EA, Tattersall RB. Unrecognised nocturnal hypoglycaemia in insulin-treated diabetics. Lancet. 1979;1:1049–52[↩]
- Foster DW. Diabetes mellitus. In: Isselbacher KJ, ed. Harrison’s Principles of internal medicine. 13th ed. New York: McGraw-Hill, 1994:1979–2000[↩][↩]
- Reynolds WA. Are night sweats a sign of esophageal reflux? [Letter]. J Clin Gastroenterol. 1989;11:590–1[↩]
- Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5[↩]
- Duhon DR. Night sweats: two other causes. JAMA. 1994;271:1577.[↩]
- Fred HL. Night sweats. Hosp Pract. 1993;28:88[↩]
- Smetana GW. Diagnosis of night sweats. JAMA. 1993;270:2502–3.[↩]
- Physicians’ desk reference. 53rd ed. Montvale, N.J.: Medical Economics, 1999[↩]