Contents
What is Nipah virus
Nipah virus is a zoonotic virus (it is transmitted from animals to humans) and can also be transmitted through contaminated food or directly between people 1, 2, 3, 4, 5. Nipah virus is a paramyxovirus belonging to the genus Henipavirus of the family Paramyxoviridae 6, 7. Nipah virus was first discovered following an outbreak of febrile illness in pigs and encephalitis and respiratory illness among pig farmers, people with close contact with pigs and abattoir workers in Malaysia and neighboring Singapore between September 1998 and May 1999 8, 9, 10, 11, 12, 13, 14. The Nipah virus outbreak ended only after Malaysia established widespread surveillance of pigs, resulting in the culling of over one million animals 15. The clinical signs and symptoms of the Nipah virus disease include fever along with shortness of breath, cough and headache 2. Encephalitis along with seizures are the complications involved 16. Survivors of Nipah virus infection develop symptoms of neurological malfunction such as encephalopathy, cerebral atrophy, change in behavior, ocular motor palsies, cervical dystonia, weakness and facial paralysis, which remain for several years 17.
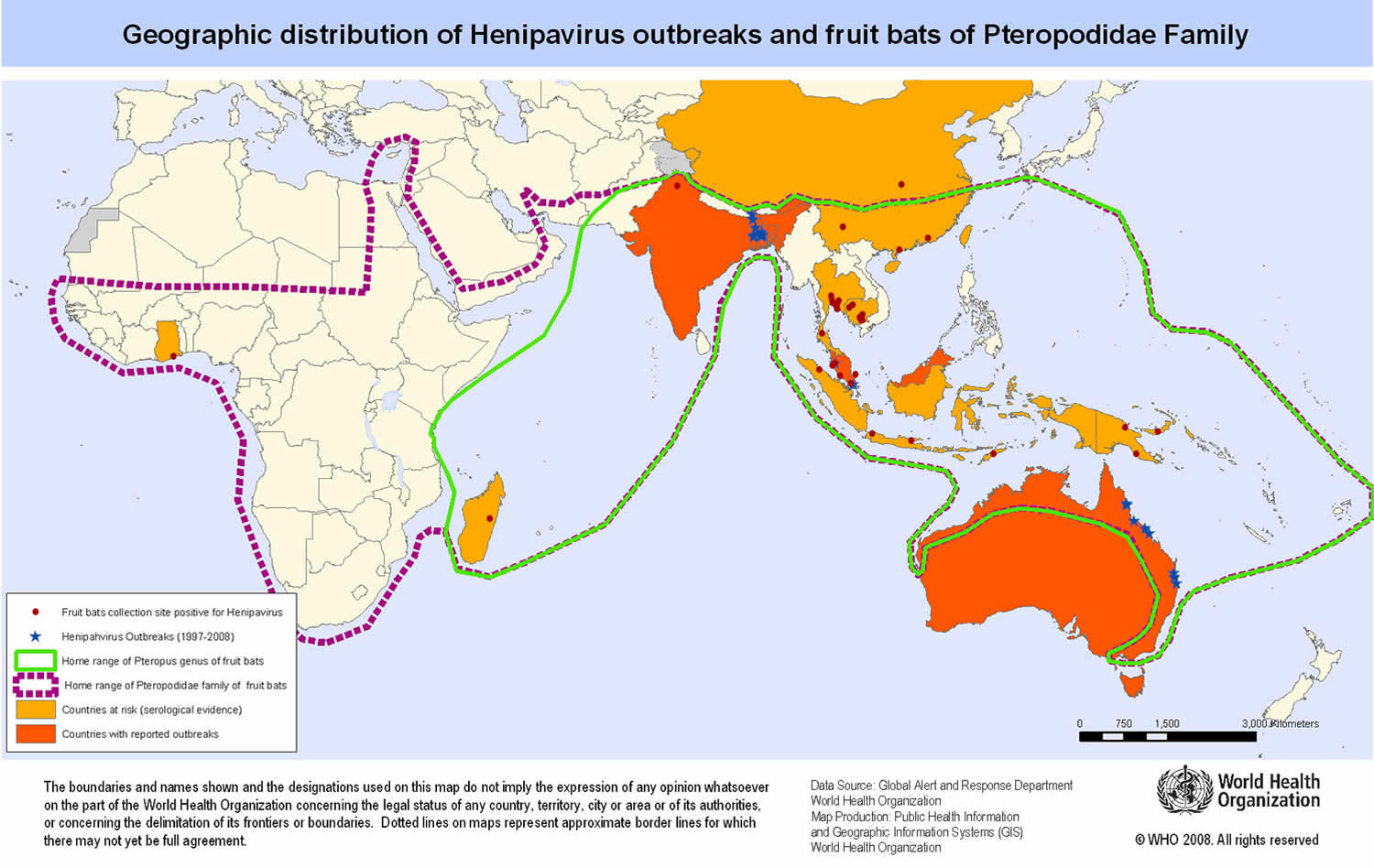
Nipah virus name originated from Sungai Nipah, a village in the Malaysian Peninsula where pig farmers became ill with encephalitis. Given the relatedness of Nipah virus to Hendra virus, bat species were quickly singled out for investigation and flying foxes (fruit bats) of the genus Pteropus were subsequently identified as the reservoir for Nipah virus (see Distribution Map) 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 6, 7, 31.
Fruit bats of Pteropus species act as natural reservoir of Nipah viruses and among various outbreaks documented from different geographical parts of the globe these bats have been associated in one or other way for transmission of Nipah virus and associated Nipah virus infection 32, 33. From bats, the virus has crossed its species-barrier frequently to several other species including man through spilled over transmission, but with limited transmission from person to person thereafter 34. Nipah virus transmission to human occurs mainly in places where human, pigs and bats come in close proximity. People rear pigs for economic benefits and fruit bearing trees are also cultivated in and around the farm for shade. Fruit bats of Pteropus spp. which are Nipah virus reservoirs, are attracted by the fruits, hence Nipah virus gets spilled over to pigs or animals and also to human. This combination of close surroundings of fruiting trees, fruits- like date palm, fruit bats, pigs and man altogether form the basis of emergence and spread of new deadly zoonotic virus infections like Nipah 35. Infected pig meat travels across continents which led to transmission of Nipah virus from animals in one part of the world to people in another part of globe.
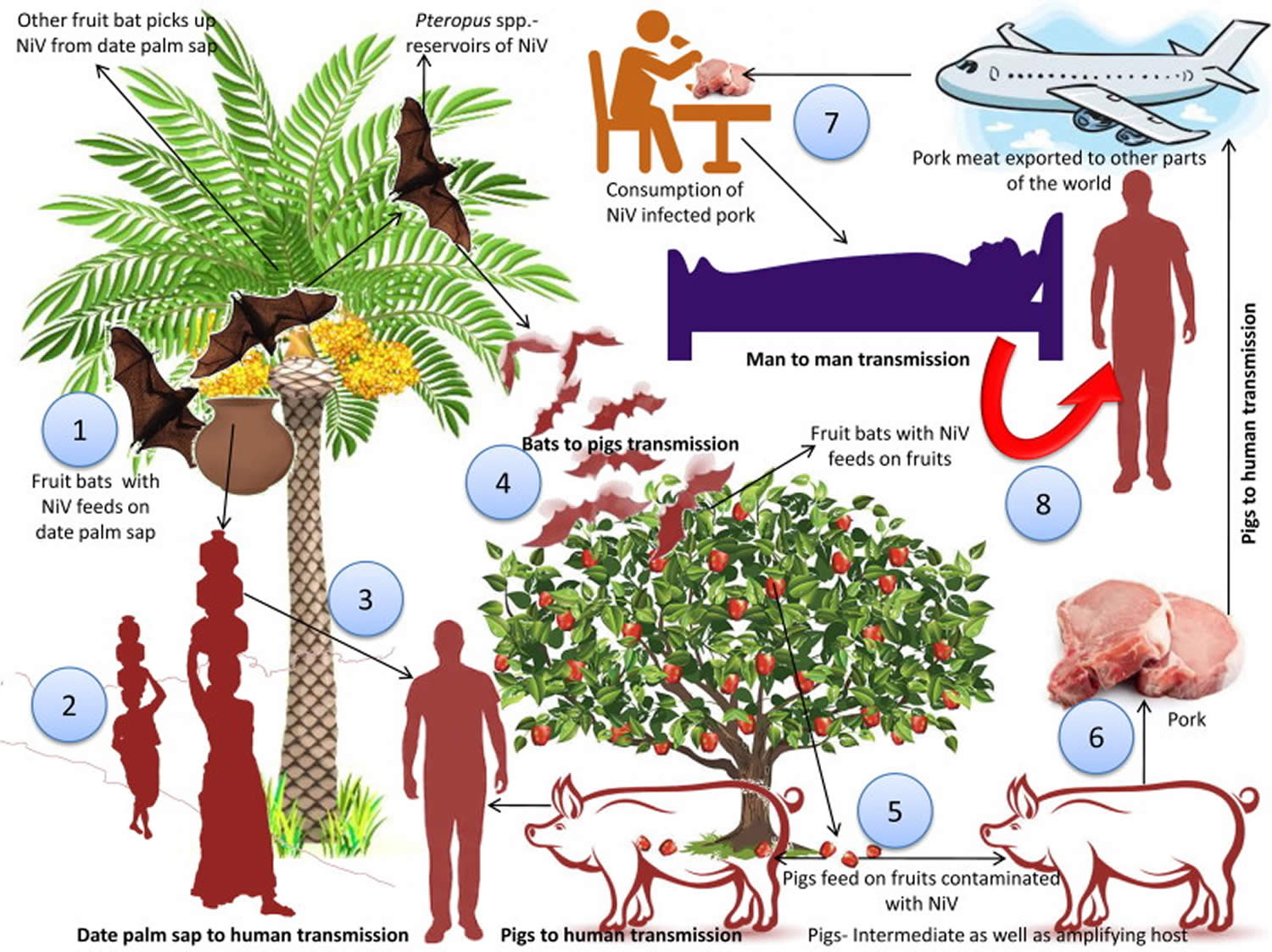
Nipah virus transmission occurs via consumption of virus-contaminated foods and contact with infected animals or human body fluids. Risk factors include close proximity viz., touching, feeding or attending virus infected person, thus facilitating contact to droplet Nipah virus infection. Recently, experimental studies with aerosolized Nipah virus in Syrian hamsters revealed that Nipah virus droplets (aerosol exposure) might play a role in transmitting Nipah virus during close contact (Escaffre et al. 2018). Three transmission pathways of the Nipah virus have been identified after investigation carried out in Bangladesh. Consumption of freshdate palm sap is the most frequent route, with the consumption of tari (fermented date palm juice) being a potential pathway of viral transmission. Nipah virus infection associated with tari can be prevented by prevention of the access of bat to date palm sap (Islam et al. 2016). Studies using infrared camera revealed that the date palm trees are often visited bats like Pteropus giganteus and during the process of collection of the sap, bats lick them. The virus can survive for days in sugar-rich solutions, viz., fruit pulp (Fogarty et al. 2008; Khan et al. 2008). The Nipah viral outbreak reported from Tangail district, Bangladesh was found to be associated with drinking of raw date palm sap. Notably, symptoms have been recognized in patients in Bangladesh during the season of collection of date palm sap, i.e. during December to March (Luby et al. 2006, 2009). Data also revealed high seroprevalence of anti-Nipah viral antibodies among Pteropusspp. This is suggestive of the fact that the virus has undergone adaptation well enough to get transmitted among Pteropus bats. The modes of transmission of the Nipah virus are depicted in Figure 2.
Nipah virus can spread to people from 36, 37, 38, 39:
- Direct contact with infected animals, such as bats or pigs, or their body fluids (such as blood, urine or saliva)
- Consuming food products that have been contaminated by body fluids of infected animals (such as palm sap or fruit contaminated by an infected bat)
- Close contact with a person infected with Nipah virus or their body fluids (including nasal or respiratory droplets, urine, or blood)
Nipah virus can survive for up to 3 days in some fruit juices or mango fruit, and for at least 7 days in artificial date palm sap (13% sucrose and 0.21% BSA in water, pH 7.0) kept at 22 °C 2. Nipah virus has a half-life of 18 hours in the urine of fruit bats. Nipah virus is relatively stable in the environment, and remains viable at 70 °C for 1 hour (only the viral concentration will be reduced) 2. Nipah virus can be completely inactivated by heating at 100 °C for more than 15 minutes 40. However, the viability of Nipah virus in its natural environment may vary depending on the different conditions. Nipah virus can be readily inactivated by soaps, detergents and commercially available disinfectants such as sodium hypochlorite 41.
In the first known Nipah virus outbreak, people were probably infected through close contact with infected pigs. The Nipah virus strain identified in that outbreak appeared to have been transmitted initially from bats to pigs, with subsequent spread within pig populations. Then people who worked closely with infected pigs began falling ill. No person-to-person transmission was reported in that outbreak.
However, person-to-person spread of Nipah virus is regularly reported in Bangladesh and India. This is most commonly seen in the families and caregivers of Nipah virus-infected patients, and in healthcare settings. Transmission also occurs from exposure to food products that have been contaminated by infected animals, including consumption of raw date palm sap or fruit that has been contaminated with saliva or urine from infected bats. Some cases of Nipah virus infection have also been reported among people who climb trees where bats often roost.
In the 1999 outbreak, Nipah virus caused a relatively mild disease in pigs, but nearly 300 human cases with over 100 deaths were reported. In order to stop the outbreak, more than a million pigs were euthanized, causing tremendous trade loss for Malaysia. Since this outbreak, no subsequent cases (in neither swine nor human) have been reported in either Malaysia or Singapore 14.
In 2001, Nipah virus was again identified as the causative agent in an outbreak of human disease occurring in Bangladesh 3, 14. Genetic sequencing confirmed this virus as Nipah virus, but a strain different from the one identified in 1999. In the same year, another outbreak was identified retrospectively in Siliguri, India with reports of person-to-person transmission in hospital settings (nosocomial transmission). Unlike the Malaysian Nipah virus outbreak, outbreaks occur almost annually in Bangladesh and have been reported several times in India.
Although Nipah virus has caused only a few known outbreaks in Asia, it infects a wide range of animals and causes severe disease and death in people, making it a public health concern. Nipah virus infection in people causes a range of illnesses from asymptomatic (subclinical) infection to acute respiratory illness and fatal encephalitis. Nipah virus can also cause severe disease in animals such as pigs, resulting in significant economic losses for farmers.
Infected people initially develop symptoms including fever, headaches, myalgia (muscle pain), vomiting and sore throat. This can be followed by dizziness, drowsiness, altered consciousness, and neurological signs that indicate acute encephalitis. Some people can also experience atypical pneumonia and severe respiratory problems, including acute respiratory distress. Encephalitis and seizures occur in severe cases, progressing to coma within 24 to 48 hours.
The incubation period (interval from infection to the onset of symptoms) is believed to range from 4 to 21 days 42, 43, 4. However, an incubation period as long as 45 days has been reported.
Most people who survive acute encephalitis make a full recovery, but long term neurologic conditions have been reported in survivors. Approximately 20% of patients are left with residual neurological consequences such as seizure disorder and personality changes. A small number of people who recover subsequently relapse or develop delayed onset encephalitis.
The case fatality rate is estimated at 40% to 75%. This rate can vary by outbreak depending on local capabilities for epidemiological surveillance and clinical management.
There are currently no drugs or vaccines specific for Nipah virus infection although WHO has identified Nipah as a priority disease for the WHO Research and Development Blueprint. Intensive supportive care is recommended to treat severe respiratory and neurologic complications.
Nipah virus key facts 44:
- Nipah virus infection in humans causes a range of clinical presentations, from asymptomatic infection (subclinical) to acute respiratory infection and fatal encephalitis.
- The case fatality rate is estimated at 40% to 75%. This rate can vary by outbreak depending on local capabilities for epidemiological surveillance and clinical management.
- Nipah virus can be transmitted to humans from animals (such as bats or pigs), or contaminated foods and can also be transmitted directly from human-to-human.
- Fruit bats of the Pteropodidae family are the natural host of Nipah virus.
- There is no treatment or vaccine available for either people or animals. The primary treatment for humans is supportive care.
- Patient education is important in preventing Nipah virus infection, especially in the context of the lack of an effective treatment. Patient education should focus on efforts to prevent the contamination or consumption of date palm sap. The WHO also recommends avoiding exposure to bats and pigs and avoiding exposure to bat-bitten fruits or raw date palm sap. Protective clothing is recommended for people involved in the slaughter of animals. Human-to-human transmission during an outbreak can be contained by limiting exposure and the use of personal protective equipment. Contact tracing and quarantining potential contacts form a large part of an outbreak response 4, 45, 46.
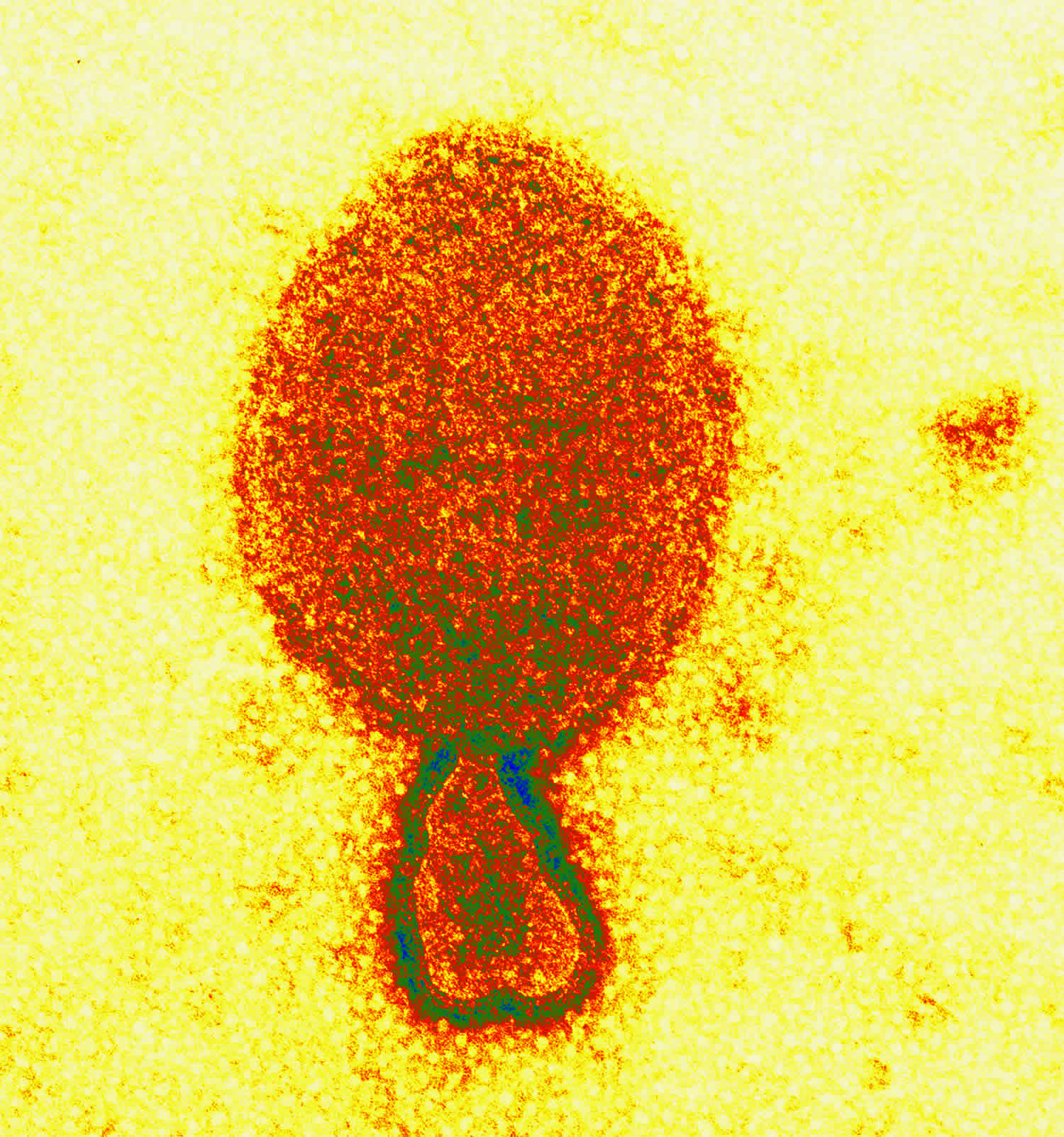
Figure 1. Nipah virus
Nipah virus
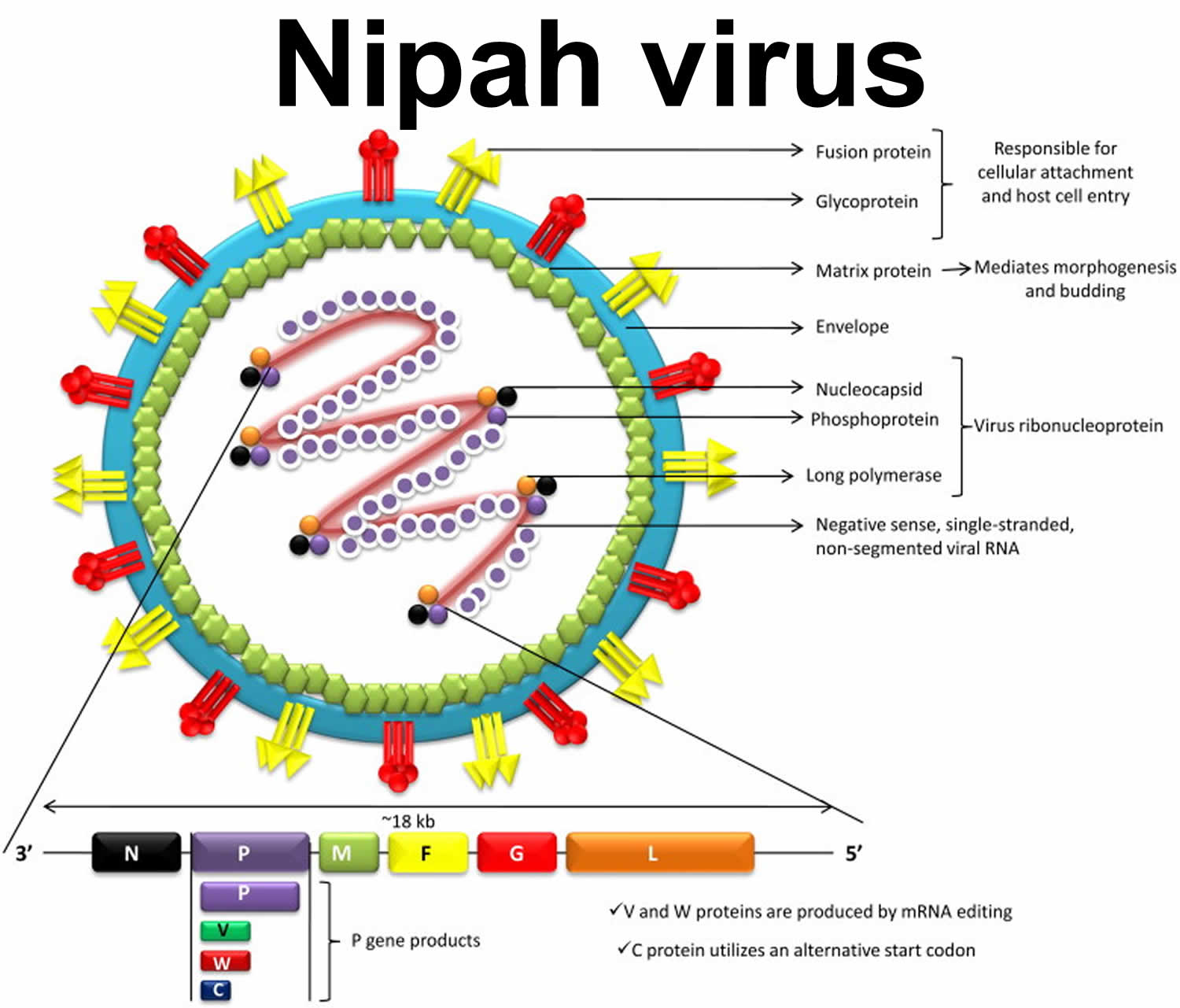
Nipah virus is a paramyxovirus (Henipavirus genus, Paramyxovirinae subfamily, Paramyxoviridae family, order Mononegavirales), an emerging virus that can cause severe respiratory illness and deadly encephalitis in humans 2. Nipah virus is a negative sense, single-stranded, nonsegmented, enveloped RNA virus possessing helical symmetry 2. The RNA genome, from the 3´-5´, contains consecutive arrangement of six genes, such as nucleocapsid (N), phosphoprotein (P), matrix (M), fusion glycoprotein (F), attachment glycoprotein (G) and long polymerase (L) 2. The N, P and L attached to the viral RNA forming the virus ribonucleoprotein (vRNP). F and G proteins are responsible for cellular attachment of the virion and subsequent host cell entry 47, 48, 49. The newly produced precursor F protein (F0) is cleaved into two subunits, viz., F1 and F2, by host protease. The fusion peptide of the virus contained in the F1 subunit drives the viral and host cellular membrane fusion for the virus entry 50. Nipah virus M protein mediates morphogenesis and budding. Antibody to the G protein is essential for neutralization of the Nipah virus infectivity 51, 52. It is quite noteworthy that through the coordinated efforts of the fusion (F) (class I) and attachment (G) glycoproteins the target cell (i.e. host cell) is entered upon after binding by the enveloped Henipaviruses including Nipah virus. Interactions between Class B ephrins (viral receptors) on host cells and the Nipah virus glycoprotein (G) trigger conformational changes in the latter, leading to activation of F glycoprotein and membrane fusion 53. It is believed that the strategies of replication as well as fusion of the ephrin receptors are responsible for greater pathogenicity of these viruses. Multiple accessory proteins encoded by Henipaviruses aid in host immune evasion 54.
Nipah virus infects its host cells via two glycoproteins, i.e. G and F proteins. The G glycoprotein mediates attachment to host cell surface receptors and the fusion (F) protein makes fusion of virus-cell membranes for cellular entry. The G protein of Nipah virus binds to host ephrin B2/3 receptors and induces conformational changes in G protein that trigger the F protein refolding 55. Wong et al.56 have demonstrated that monomeric ephrinB2 binding leads to allosteric changes in Nipah virus G protein that pave the way to its full activation and receptor-activated virus entry into the host cells. Recently, viral regulation of host cell machinery has been revealed to target nucleolar DNA-damage response (DDR) pathway by causing inhibition of nucleolar Treacle protein that increases Henipavirus (Hendra and Nipha virus) production 57.
Nipah virus can survive for up to 3 days in some fruit juices or mango fruit, and for at least 7 days in artificial date palm sap (13% sucrose and 0.21% BSA in water, pH 7.0) kept at 22 °C. Nipah virus has a half-life of 18 h in the urine of fruit bats. Nipah virus is relatively stable in the environment, and remains viable at 70 °C for 1 hour (only the viral concentration will be reduced). Nipah virus can be completely inactivated by heating at 100 °C for more than 15 minutes 40. However, the viability of Nipah virus in its natural environment may vary depending on the different conditions. Nipah virus can be readily inactivated by soaps, detergents and commercially available disinfectants such as sodium hypochlorite 41.
Figure 2. Nipah virus structure
Foonote: The Nipah virus structure with six major targeted proteins with their nucleotide length is illustrated in Figure 2. Nipah virus encodes six structural proteins, out of which attachment glycoprotein (G) and fusion glycoprotein (F) are surface proteins of Nipah virus. Remaining four proteins are inner proteins comprising matrix protein (M), phosphoprotein (P), nucleoprotein (N), and the large protein or RNA polymerase protein (L). Meanwhile, the P gene also encodes to P, W, V, and C proteins. Furthermore, N, P and L are responsible for the attachment of viral RNA to form the virus ribonucleoprotein (vRNP), whereas F and G are responsible for the cellular attachment of the virion and the subsequent entry into the host cell.
[Source 2 ]Nipah virus transmission
Transmission of Nipah virus to humans may occur after direct contact with infected bats, infected pigs, or from other Nipah virus infected people or via consumption of Nipah virus-contaminated foods. However, detailed studies are needed to understand the mechanisms of Nipah virus transmission from bats-to-pigs, pigs-to-human, and from date palm sap to human and viral circulation between fruit bats, pigs and human beings 2. Consumption of freshdate palm sap is the most frequent route, with the consumption of tari (fermented date palm juice) being a potential pathway of viral transmission in Bangladesh. Nipah virus infection associated with tari can be prevented by prevention of the access of bat to date palm sap 58. Studies using infrared camera revealed that the date palm trees are often visited by bats like Pteropus giganteus and during the process of collection of the sap, bats lick them. Nipah virus can survive for days in sugar-rich solutions such as fruit pulp 59, 60. The Nipah viral outbreak reported from Tangail district, Bangladesh was found to be associated with drinking of raw date palm sap. Notably, symptoms have been recognized in patients in Bangladesh during the season of collection of date palm sap, i.e. during December to March 61, 62. Data also revealed high seroprevalence of anti-Nipah viral antibodies among Pteropus spp. This is suggestive of the fact that Nipah virus has undergone adaptation well enough to get transmitted among Pteropus bats. The modes of transmission of the Nipah virus are depicted in Figure 2.
During the first recognized outbreak of Nipah virus in Malaysia, which also affected Singapore, most human infections were apparently infected with Nipah virus only through close contact with infected sick pigs or their contaminated tissues 63, 64. Risk factors include touching, feeding or attending virus infected person, thus facilitating contact to droplet Nipah virus infection. Transmission is thought to have occurred via unprotected exposure to secretions from the pigs, or unprotected contact with the tissue of a sick animal. The Nipah virus strain identified in this outbreak appeared to have been transmitted initially from bats to pigs, with subsequent spread within pig populations. Incidental human infections resulted after exposure to infected pigs. No occurrence of person-to-person transmission was reported in this outbreak. Recently, experimental studies with aerosolized Nipah virus in Syrian hamsters revealed that Nipah virus droplets (aerosol exposure) might play a role in transmitting Nipah virus during close contact 65. Nipah virus is more likely to be transmitted from patients suffering from infection of the respiratory tract 66. A case-control study of risk factors for human infection with Nipah virus during the outbreak in Malaysia showed that direct close contact with pigs was the primary source of human Nipah virus infections, where only 8% of patients had no contact with pigs. The outbreak was stopped after pigs in the affected areas were slaughtered and proper disinfection measures were taken 67.
In subsequent outbreaks in Bangladesh and India, consumption of fruits or fruit products (such as raw date palm juice) contaminated with urine or saliva from infected fruit bats was the most likely source of infection. In Bangladesh, domestic animals represented another route of transmission of Nipah virus. Foraging for fruits (contaminated with infectious saliva) was observed among domestic animals in Bangladesh. There has been a report of spread of Nipah virus disease from sick cows during the year 2001 in a place called Meherpur in Bangladesh 68. Illness acquired from pigs or saliva of goats and secretions of bats infected with Nipah virus has also been recorded in Naogaon 69, 70. In ferrets, systemic disease was induced when the animals are exposed to certain doses of Nipah virus particles 32.
Human-to-human transmission of Nipah virus has also been reported among family and caregivers of Nipah virus-infected patients. Person-to-person transmission of Nipah virus in Bangladesh and India is regularly reported. Research based on detailed interview of Nipah virus infection survivors, medical practitioners and caretakers conducted in Bangladesh during May–December, 2004 showed that transmission occurred through both ways from bats-to-man and man-to-man. Secondary transmission between humans was observed during the outbreaks 71, 72, 73. Nipah virus shed from Pteropus species fruit bats may infect either single or multiple individuals and the chain of transmission may then continue in an epidemic form by person-to-person transmission 74. Risk factors associated with the infection include patient handling and contact with the secretion of infected person 75.
In Siliguri, India in 2001, transmission of the virus was also reported within a health-care setting, where 75% of cases occurred among hospital staff or visitors. From 2001 to 2008, around half of reported cases in Bangladesh were due to human-to-human transmission through providing care to infected patients.
Figure 3. Nipah virus transmission
Footnotes: (1) Fruit bats acts as natural reservoir of Nipah viruses. Fruit bats with Nipah virus feeds on date palm sap. Nipah virus can survive in solutions that are rich in sugar, such as fruit pulp. (2) Nipah virus transmitted to human through the consumption of date palm sap. (3) Fruit bats of Pteropus spp. which are Nipah virus reservoirs visited such fruit trees and got opportunity to naturally spill the drop containing virus in the farm to contaminate the farm soil and fruits. (4) Contaminated fruits are consumed by pigs and other animals. Pigs act as intermediate as well as amplifying host. Combination of close surroundings of fruiting trees, fruits-like date palm, fruit bats, pigs and human altogether form the basis of emergence and spread of new deadly zoonotic virus infection like Nipah virus. (5) Pork meat infected with Nipah virus are exported to other parts. (6) Consumption of infected pork can act as a source of infection to human. (7) Close contact with Nipah virus affected human can lead to spread of Nipah virus to other persons.
[Source 2 ]Nipah virus outbreak
Nipah virus was first recognized in 1999 during an outbreak among pig farmers in, Malaysia. No new outbreaks have been reported in Malaysia since 1999.
It was also recognized in Bangladesh in 2001, and nearly annual outbreaks have occurred in that country since. The disease has also been identified periodically in eastern India.
Other regions may be at risk for infection, as evidence of the virus has been found in the known natural reservoir (Pteropus bat species) and several other bat species in a number of countries, including Cambodia, Ghana, Indonesia, Madagascar, the Philippines, and Thailand.
Countries with reported outbreak of Nipah virus at risk based on serological evidence or molecular detection in Pteropus fruit bat species:
- Australia,
- Bangladesh,
- Cambodia,
- China,
- India,
- Indonesia,
- Madagascar,
- PNG,
- Taiwan,
- Thailand
Countries where Pteropus fruit bat species are known or likely present:
- Australia,
- Bangladesh,
- Bhutan,
- Brunei,
- Burma,
- Cambodia,
- China,
- Guam,
- India,
- Indonesia,
- Laos,
- Mariana Islands,
- Malaysia,
- Nepal,
- Pakistan,
- Palau,
- Papua New Guinea,
- Philippines,
- Singapore,
- Sri Lanka,
- Taiwan,
- Thailand,
- Timor-Leste,
- Vietnam
Natural host: fruit bats
Fruit bats of the family Pteropodidae – particularly species belonging to the Pteropus genus – are the natural hosts for Nipah virus 76, 77. There is no apparent disease in fruit bats. Pteropus species of bats in other countries (Cambodia, Thailand, Indonesia, and Madagascar) have anti–Nipah virus antibodies 78, 79, 80, 81. Rarely non-Pteropus species of bats can be reservoirs for Nipah virus 79, 82, 83. Pigs acted as intermediate hosts of the Nipah virus during the initial outbreak in Malaysia and Singapore and horses during the outbreak in the Philippines 84.
It is assumed that the geographic distribution of Henipaviruses overlaps with that of Pteropus species of fruit bats. This hypothesis was reinforced with the evidence of Henipavirus infection in Pteropus bats from Australia, Bangladesh, Cambodia, China, India, Indonesia, Madagascar, Malaysia, Papua New Guinea, Thailand and Timor-Leste.
African fruit bats of the genus Eidolon, family Pteropodidae, were found positive for antibodies against Nipah and Hendra viruses, indicating that these viruses might be present within the geographic distribution of Pteropodidae bats in Africa.
Transmission of the Nipah virus can occur from direct contact with infected animals (bats, pigs, horses) or their body fluids (blood, urine, or saliva), consuming contaminated food products (palm sap or fruit), or close contact with an infected person or their body fluids (nasal or respiratory droplets, urine, or blood) 5.
Nipah virus enters through the oro-nasal route into humans and other hosts. High concentrations of antigen in the lymphoid and respiratory tissue suggest that these are the probable sites of initial replication. Nipah virus infects the epithelium of the respiratory tract and induces inflammatory cytokines, leading to the development of an acute respiratory distress syndrome-like disease 85. Other than the lungs, the kidneys, spleen, and the brain may be involved, leading to multiple organ failure 2.
Nipah virus in domestic animals
Outbreaks of the Nipah virus in pigs and other domestic animals such as horses, goats, sheep, cats and dogs were first reported during the initial Malaysian outbreak in 1999.
Nipah virus is highly contagious in pigs. Pigs are infectious during the incubation period, which lasts from 4 to 14 days.
An infected pig can exhibit no symptoms, but some develop acute feverish illness, labored breathing, and neurological symptoms such as trembling, twitching and muscle spasms. Generally, mortality is low except in young piglets. These symptoms are not dramatically different from other respiratory and neurological illnesses of pigs. Nipah virus should be suspected if pigs also have an unusual barking cough or if human cases of encephalitis are present.
Figure 4. Nipah virus distribution map
Nipah virus outbreak prevention
Based on the experience gained during the outbreak of Nipah virus involving pig farms in 1999, routine and thorough cleaning and disinfection of pig farms with appropriate detergents may be effective in preventing infection.
If an outbreak is suspected, the animal premises should be quarantined immediately. Culling of infected animals – with close supervision of burial or incineration of carcasses – may be necessary to reduce the risk of transmission to people. Restricting or banning the movement of animals from infected farms to other areas can reduce the spread of the disease.
As Nipah virus outbreaks have involved pigs and/or fruit bats, establishing an animal health/wildlife surveillance system, using a One Health approach, to detect Nipah cases is essential in providing early warning for veterinary and human public health authorities.
Reducing the risk of infection in people
In the absence of a vaccine, the only way to reduce or prevent infection in people is by raising awareness of the risk factors and educating people about the measures they can take to reduce exposure to the Nipah virus.
Public health educational messages should focus on:
- Reducing the risk of bat-to-human transmission.
- Efforts to prevent transmission should first focus on decreasing bat access to date palm sap and other fresh food products. Keeping bats away from sap collection sites with protective coverings (such as bamboo sap skirts) may be helpful. Freshly collected date palm juice should be boiled, and fruits should be thoroughly washed and peeled before consumption. Fruits with sign of bat bites should be discarded.
- Reducing the risk of animal-to-human transmission.
- Gloves and other protective clothing should be worn while handling sick animals or their tissues, and during slaughtering and culling procedures. As much as possible, people should avoid being in contact with infected pigs. In endemic areas, when establishing new pig farms, considerations should be given to presence of fruit bats in the area and in general, pig feed and pig shed should be protected against bats when feasible.
- Reducing the risk of human-to-human transmission.
- Close unprotected physical contact with Nipah virus-infected people should be avoided. Regular hand washing should be carried out after caring for or visiting sick people.
Controlling infection in health-care settings
Health-care workers caring for patients with suspected or confirmed infection, or handling specimens from them, should implement standard infection control precautions at all times
As human-to-human transmission has been reported, in particular in health-care settings, contact and droplet precautions should be used in addition to standard precautions. Airborne precautions may be required in certain circumstances.
Samples taken from people and animals with suspected Nipah virus infection should be handled by trained staff working in suitably equipped laboratories.
Nipah virus prevention
Nipah virus infection can be prevented by avoiding exposure to sick pigs and bats in endemic areas and not drinking raw date palm sap.
In areas where Nipah virus outbreaks have occurred (Bangladesh, Malaysia, India, and Singapore), people should:
- Practice handwashing regularly with soap and water
- Avoid contact with sick bats or pigs
- Avoid areas where bats are known to roost
- Avoid eating or drinking products that could be contaminated by bats, such as raw date palm sap, raw fruit, or fruit that is found on the ground
- Avoid contact with the blood or body fluids of any person known to be infected with Nipah virus
Because Nipah virus can be spread from person-to-person, standard infection control practices and proper barrier nursing techniques are important in preventing hospital-acquired infections (nosocomial transmission) in settings where a patient has confirmed or suspected Nipah virus infection.
Other geographic locations may be at risk for Nipah virus outbreaks in the future, such as regions where flying foxes (bat genus Pteropus) live. These bats are currently found in Cambodia, Indonesia, Madagascar, the Philippines, and Thailand. People living in or visiting these areas should consider taking the same precautions as those living in areas where outbreaks have already occurred.
In addition to steps that individuals can take to lower their risk for Nipah virus infection, it will be critical for scientists, researchers, and communities at risk to continue learning about Nipah virus to prevent future outbreaks. Broader prevention efforts include:
- Increasing surveillance of animals and people in areas where Nipah virus is known to exist.
- Increasing research on the ecology of fruit bats to understand where they live and how they spread the virus to other animals and people.
- Evaluation of novel technologies or methods to minimize spread of the virus within bat populations.
- Improving tools to detect the virus early in communities and livestock.
- Reinforcing protocols for healthcare settings on standard infection control practices to prevent person-to-person spread.
- Raising awareness about the signs, symptoms, and risk of Nipah virus among populations at higher risk due to:
- Geographic location
- Contact with fruit bats or items contaminated by fruit bats
- Contact with pigs or animals that could come into contact with fruit bats
- Work in a healthcare setting or as a caregiver for people infected with Nipah virus
Nipah virus vaccine
Currently, there are no vaccines available against Nipah virus. A subunit vaccine, using the Hendra G protein, produces cross-protective antibodies against Hendra virus and Nipah virus has been recently used in Australia to protect horses against Hendra virus. This vaccine offers great potential for henipavirus protection in humans as well 86.
Nipah virus symptoms
Infection with Nipah virus can cause mild to severe disease, including asymptomatic infection to acute respiratory infection (mild, severe), inflammation of the brain (encephalitis) and potentially death 43, 87, 88, 89.
There are some differences in clinical features seen in the Malaysian and Indian Nipah virus outbreaks. Respiratory illness is seen in 70% of patients in India and Bangladesh 90, 91, whereas no significant respiratory involvement was seen in Malaysia 43. Respiratory involvement may present as a cough, respiratory distress and atypical pneumonia 92, 91.
Symptoms typically appear in 4 to 14 days following exposure to Nipah virus. The illness initially presents as 3 to 14 days of fever and headache, and often includes signs of respiratory illness, such as cough, sore throat, and difficulty breathing. A phase of inflammation of the brain (encephalitis) may follow, where symptoms can include drowsiness, disorientation, and mental confusion, which can rapidly progress to coma within 24 to 48 hours. In fulminant illness, multiorgan dysfunction, gastrointestinal bleeding, and kidney failure are seen.
Nipah virus symptoms may initially include one or several of the following:
- Fever
- Headache
- Cough
- Sore throat
- Difficulty breathing
- Vomiting
Nipah virus severe symptoms may follow, such as:
- Disorientation, drowsiness, or confusion
- Seizures
- Coma
- Inflammation of the brain (encephalitis)
Death may occur in 40 to 75% of Nipah virus disease cases. Long-term neurologic effects from encephalitis in survivors of Nipah virus infection have been noted, including persistent convulsions, fatigue, encephalopathy, ocular motor palsies, cervical dystonia, focal weakness, facial paralysis and personality changes.
Infections that lead to symptoms and sometimes death much later after exposure (known as dormant or latent infections) have also been reported months and even years after exposure 93.
Nipah virus complications
There may be residual neurological deficits in survivors, including behavioral change, cervical dystonia, ocular motor palsies, weakness, and facial paralysis. In a small proportion of patients, there may be relapses after recovery from the acute infection 93.
Nipah virus diagnosis
Early diagnosis of Nipah virus infection can be challenging due to the non-specific early symptoms of Nipah virus infection. However, early detection and diagnosis are critical to increase chances of survival among infected individuals, to prevent transmission to other people, and to manage outbreak response efforts. Nipah virus should be considered for people with symptoms consistent with Nipah virus infection who have been in areas where Nipah is more common, such as Bangladesh or India—particularly if they have a known exposure.
Nipah virus infection can be diagnosed during illness or after recovery. Different tests are available to diagnose Nipah virus infection. During early stages of the illness, laboratory testing can be conducted using real time polymerase chain reaction (RT-PCR) from throat and nasal swabs, cerebrospinal fluid (CSF), urine, and blood. Real-time polymerase chain reaction (RT-PCR) is more sensitive than conventional assay 94, 95, 96, 97, 98. Serology is not helpful for acute infections but mostly useful for epidemiologic studies 99. Later in the course of illness and after recovery, testing for antibodies (IgG and IgM) is conducted using an enzyme-linked immunosorbent assay (ELISA). IgM antibody in serum or CSF is used for diagnosis 4. Detection of IgG antibodies is a good test for surveillance in humans and for the identification in reservoir animals during epidemiological investigations 4. It has also been used for diagnosis in humans during outbreaks.
In fatal cases, immunohistochemistry on tissues collected during autopsy may be the only way to confirm a diagnosis.
Initial signs and symptoms of Nipah virus infection are nonspecific, and the diagnosis is often not suspected at the time of presentation. This can hinder accurate diagnosis and creates challenges in outbreak detection, effective and timely infection control measures, and outbreak response activities.
In acute Nipah virus infection, virus-specific antibodies were present in the serum in more than 70% of samples but in less than one-third of cerebrospinal fluid (CSF) samples. The presence of the virus in CSF culture was strongly associated with mortality 100. EEG in encephalitis shows bilateral temporal periodic complexes of sharp and slow waves occurring every 1 or 2 seconds 101.
Other tests used include polymerase chain reaction (PCR) assay, and virus isolation by cell culture.
Nipah virus treatment
Currently Nipah virus treatment is limited to supportive care, including rest, hydration, and treatment of symptoms as they occur 5, 102. Because Nipah virus encephalitis can be transmitted person-to-person, standard infection control practices and proper barrier nursing techniques are important in preventing hospital-acquired infections (nosocomial transmission).
Ribavirin is an antiviral that is effective against other paramyxoviruses like respiratory syncytial virus (RSV). The drug ribavirin was used to treat a small number of patients in the initial Malaysian Nipah virus outbreak, but its efficacy in people is unclear, with conflicting reports showing a reduction in mortality and no effect. Chong et al. 103 reported a decrease in mortality while Goh et al. 43 found no decrease during the same outbreak. Ribavirin has been tested in animal models and found to be ineffective 104. However, in the absence of effective antivirals, the the Indian National Centre for Disease Control recommends the use of oral or parenteral Ribavirin for all confirmed Nipah virus cases 43, 4, 103. Ribavirin is not recommended for chemoprophylaxis 105. Acyclovir, chloroquine, and ephrin-B2 are under review as potential therapeutic options 92, 106, 107.
Acyclovir was used in Singapore but whether it was effective is unclear 92. Chloroquine was reported to be effective in cell culture but failed to prevent death in a hamster model in isolation or in combination with Ribavirin 106. The natural ligands of Ephrin-B2, as well as soluble Ephrin-B2, have been shown to be effective in vitro 107.
Favipiravir, a drug licensed in Japan for treatment of Influenza, was shown to be effective in hamsters 108.
The human monoclonal antibody has been shown to be useful in ferrets and non-human primates 109, 110. One such monoclonal antibody, m102.4, has completed phase 1 clinical trials and has been used on a compassionate use basis. Use of anti-G and anti-F monoclonal antibodies in an emergency setting is approved in India. In addition, the antiviral treatment remdesivir has been effective in nonhuman primates when given as post-exposure prophylaxis, and may be complementary to immunotherapeutic treatments.
Patients should be discharged only after a negative real time polymerase chain reaction (RT-PCR) is performed on a throat swab or blood. Discharged patients remain in isolation for 21 days following confirmation of the infection 4.
Nipah virus prognosis
Nipah virus case death rates can range between 40% and 100% 5. Risk factors for poor prognosis include old age, comorbidities, thrombocytopenia and raised aminotransferases on admission, brainstem involvement and seizures 43, 111.
Prognosis and case fatality rates also depend on the strain of the Nipah virus, with a higher mortality rate has been seen in India and Bangladesh (70%) as opposed to Malaysia (40%) 112, 90, 91.
- Nipah virus infection.https://www.who.int/csr/disease/nipah/en[↩]
- Singh RK, Dhama K, Chakraborty S, Tiwari R, Natesan S, Khandia R, Munjal A, Vora KS, Latheef SK, Karthik K, Singh Malik Y, Singh R, Chaicumpa W, Mourya DT. Nipah virus: epidemiology, pathology, immunobiology and advances in diagnosis, vaccine designing and control strategies – a comprehensive review. Vet Q. 2019 Dec;39(1):26-55. doi: 10.1080/01652176.2019.1580827[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- McKee CD, Islam A, Luby SP, Salje H, Hudson PJ, Plowright RK, Gurley ES. The Ecology of Nipah Virus in Bangladesh: A Nexus of Land-Use Change and Opportunistic Feeding Behavior in Bats. Viruses. 2021 Jan 23;13(2):169. doi: 10.3390/v13020169[↩][↩]
- Aditi, Shariff M. Nipah virus infection: A review. Epidemiol Infect. 2019 Jan;147:e95. doi: 10.1017/S0950268819000086[↩][↩][↩][↩][↩][↩][↩]
- Rathish B, Vaishnani K. Nipah Virus. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK570576[↩][↩][↩][↩]
- Halpin K, Young PL, Field HE, Mackenzie JS. 2000. Isolation of Hendra virus from pteropid bats: a natural reservoir of Hendra virus. J Gen Virol. 81(Pt 8):1927–1932. PMID 10900029. doi: 10.1099/0022-1317-81-8-1927[↩][↩]
- Vandali V, Biradar RB. 2018. Nipah virus (NiV) infection: a systematic review. JOJ Nursing & Health Care. 8(1):555729. doi: 10.19080/JOJNHC.2018.08.555729[↩][↩]
- Chua K.B., Goh K.J., Wong K.T., Kamarulzaman A., Tan P.S.K., Ksiazek T.G., Zaki S.R., Paul G., Lam S.K., Tan C.T. Fatal encephalitis due to Nipah virus among pig-farmers in Malaysia. Lancet. 1999;354:1257–1259. doi: 10.1016/S0140-6736(99)04299-3[↩]
- Paton N.I., Leo Y.S., Zaki S.R., Auchus A.P., Lee K.E., Ling A.E., Chew S.K., Ang B., Rollin P.E., Umapathi T., et al. Outbreak of Nipah-virus infection among abattoir workers in Singapore. Lancet. 1999;354:1253–1256. doi: 10.1016/S0140-6736(99)04379-2[↩]
- Goh K.J., Tan C.T., Chew N.K., Tan P.S.K., Kamarulzaman A., Sarji S.A., Wong K.T., Abdullah B.J.J., Chua K.B., Lam S.K. Clinical features of Nipah virus encephalitis among pig farmers in Malaysia. N. Engl. J. Med. 2000;342:1229–1235. doi: 10.1056/NEJM200004273421701[↩]
- Parashar U.D., Sunn L.M., Ong F., Mounts A.W., Arif M.T., Ksiazek T.G., Kamaluddin M.A., Mustafa A.N., Kaur H., Ding L.M., et al. Case-control study of risk factors for human infection with a new zoonotic paramyxovirus, Nipah virus, during a 1998–1999 outbreak of severe encephalitis in Malaysia. J. Infect. Dis. 2000;181:1755–1759. doi: 10.1086/315457[↩]
- Farrar JJ. 1999. Nipah-virus encephalitis-investigation of a new infection. Lancet. 354(9186):1222–1223. doi: 10.1016/S0140-6736(99)90124-1[↩]
- Rahman MA, Hossain MJ, Sultana S, Homaira N, Khan SU, Rahman M, Gurley ES, Rollin PE, Lo MK, Comer JA, et al. 2012. Date palm sap linked to Nipah virus outbreak in Bangladesh, 2008. Vector Borne Zoonotic Dis. 12(1):65–72. doi: 10.1089/vbz.2011.0656[↩]
- Nipah Virus (NiV). https://www.cdc.gov/vhf/nipah/index.html[↩][↩][↩]
- Chua K.B. Nipah virus outbreak in Malaysia. J. Clin. Virol. 2003;26:265–275. doi: 10.1016/S1386-6532(02)00268-8[↩]
- Broder CC, Xu K, Nikolov DB, Zhu Z, Dimitrov DS, Middleton D, Pallister J, Geisbert TW, Bossart KN, Wang L-F. 2013. A treatment for and vaccine against the deadly Hendra and Nipah viruses. Antiviral Res. 100(1):8–13. doi: 10.1016/j.antiviral.2013.06.012[↩]
- Sejvar JJ, Hossain J, Saha SK, Gurley ES, Banu S, Hamadani JD, Faiz MA, Siddiqui FM, Mohammad QD, Mollah AH, et al. 2007. Long-term neurological and functional outcome in Nipah virus infection. Ann Neurol. 62(3):235–242. doi: 10.1002/ana.21178[↩]
- Olival K.J., Latinne A., Islam A., Epstein J.H., Hersch R., Engstrand R.C., Gurley E.S., Amato G., Luby S.P., Daszak P. Population genetics of fruit bat reservoir informs the dynamics, distribution and diversity of Nipah virus. Mol. Ecol. 2020;29:970–985. doi: 10.1111/mec.15288[↩]
- Hsu V.P., Hossain M.J., Parashar U.D., Ali M.M., Ksiazek T.G., Kuzmin I., Niezgoda M., Rupprecht C., Bresee J., Breiman R.F. Nipah virus encephalitis reemergence, Bangladesh. Emerg. Infect. Dis. 2004;10:2082–2087. doi: 10.3201/eid1012.040701[↩]
- Chua K.B., Koh C.L., Hooi P.S., Wee K.F., Khong J.H., Chua B.H., Chan Y.P., Lim M.E., Lam S.K. Isolation of Nipah virus from Malaysian island flying-foxes. Microbes Infect. 2002;4:145–151. doi: 10.1016/S1286-4579(01)01522-2[↩]
- Rahman S.A., Hassan S.S., Olival K.J., Mohamed M., Chang L.-Y., Hassan L., Saad N.M., Shohaimi S.A., Mamat Z.C., Naim M.S., et al. Characterization of Nipah virus from naturally infected Pteropus vampyrus bats, Malaysia. Emerg. Infect. Dis. 2010;16:1990–1993. doi: 10.3201/eid1612.091790[↩]
- Sendow I., Field H.E., Adjid A., Ratnawati A., Breed A.C., Darminto, Morrissy C., Daniels P. Screening for Nipah virus infection in West Kalimantan province, Indonesia. Zoonoses Public Health. 2010;57:499–503. doi: 10.1111/j.1863-2378.2009.01252.x[↩]
- Breed A.C., Meers J., Sendow I., Bossart K.N., Barr J.A., Smith I., Wacharapluesadee S., Wang L., Field H.E. The distribution of henipaviruses in Southeast Asia and Australasia: Is Wallace’s line a barrier to Nipah virus? PLoS ONE. 2013;8:e61316. doi: 10.1371/journal.pone.0061316[↩]
- Breed A.C., Yu M., Barr J.A., Crameri G., Thalmann C.M., Wang L.-F. Prevalence of henipavirus and rubulavirus antibodies in pteropid bats, Papua New Guinea. Emerg. Infect. Dis. 2010;16:1997–1999. doi: 10.3201/eid1612.100879[↩]
- Field H., de Jong C.E., Halpin K., Smith C.S. Henipaviruses and fruit bats, Papua New Guinea. Emerg. Infect. Dis. 2013;19:670–671. doi: 10.3201/eid1904.111912[↩]
- Wacharapluesadee S., Boongird K., Wanghongsa S., Ratanasetyuth N., Supavonwong P., Saengsen D., Gongal G.N., Hemachudha T. A longitudinal study of the prevalence of Nipah virus in Pteropus lylei bats in Thailand: Evidence for seasonal preference in disease transmission. Vector Borne Zoonotic Dis. 2010;10:183–190. doi: 10.1089/vbz.2008.0105[↩]
- Wacharapluesadee S., Samseeneam P., Phermpool M., Kaewpom T., Rodpan A., Maneeorn P., Srongmongkol P., Kanchanasaka B., Hemachudha T. Molecular characterization of Nipah virus from Pteropus hypomelanus in Southern Thailand. Virol. J. 2016;13:53. doi: 10.1186/s12985-016-0510-x[↩]
- Reynes J.-M., Counor D., Ong S., Faure C., Seng V., Molia S., Walston J., Georges-Courbot M.C., Deubel V., Sarthou J.-L. Nipah virus in Lyle’s flying foxes, Cambodia. Emerg. Infect. Dis. 2005;11:1042–1047. doi: 10.3201/eid1107.041350[↩]
- Cappelle J., Hoem T., Hul V., Furey N., Nguon K., Prigent S., Dupon L., Ken S., Neung C., Hok V., et al. Nipah virus circulation at human–bat interfaces, Cambodia. Bull. World Health Organ. 2020;98:539–547. doi: 10.2471/BLT.20.254227[↩]
- Yob J.M., Field H., Rashdi A.M., Morrissy C., van der Heide B., Rota P., bin Adzhar A., White J., Daniels P., Jamaluddin A., et al. Nipah virus infection in bats (order Chiroptera) in peninsular Malaysia. Emerg. Infect. Dis. 2001;7:439–441. doi: 10.3201/eid0703.017312[↩]
- Ching P.K.G., de los Reyes V.C., Sucaldito M.N., Tayag E., Columna-Vingno A.B., Malbas F.F., Bolo G.C., Sejvar J.J., Eagles D., Playford G., et al. Outbreak of henipavirus infection, Philippines, 2014. Emerg. Infect. Dis. 2015;21:328–331. doi: 10.3201/eid2102.141433[↩]
- Clayton BA, Middleton D, Arkinstall R, Frazer L, Wang L-F, Marsh GA. 2016. The nature of exposure drives transmission of Nipah viruses from Malaysia and Bangladesh in ferrets. PLoS Negl Trop Dis. 10(6):e0004775. doi: 10.1371/journal.pntd.0004775[↩][↩]
- Yadav P, Sudeep A, Gokhale M, Pawar S, Shete A, Patil D, Kumar V, Lakra R, Sarkale P, Nichol S, Mourya D. 2018. Circulation of Nipah virus in Pteropus giganteus bats in northeast region of India, 2015. Indian J Med Res. 147(3):318–320. doi: 10.4103/ijmr.IJMR_1488_16[↩]
- Gurley ES, Hegde ST, Hossain K, Sazzad HMS, Hossain MJ, Rahman M, Sharker MAY, Salje H, Islam MS, Epstein JH, et al. 2017. Convergence of humans, bats, trees, and culturein Nipah virus transmission, Bangladesh. Emerg Infect Dis. 23(9):1446–1453. doi: 10.3201/eid2309.161922[↩]
- Pulliam JRC, Epstein JH, Dushoff J, Rahman SA, Bunning M, Jamaluddin AA, Hyatt AD, Field HE, Dobson AP, Daszak P. 2012. Agricultural intensification, priming for persistence and the emergence of Nipah virus: a lethal bat-borne zoonosis. J Royal Soc Interface. 9(66):89–101. doi: 10.1098/rsif.2011.0223[↩]
- Nipah Virus (NiV). https://www.cdc.gov/vhf/nipah/transmission/index.html[↩]
- Chatterjee P (2018) Nipah virus outbreak in India. The Lancet 391, 2200.[↩]
- Luby SP. The pandemic potential of Nipah virus. Antiviral Res. 2013 Oct;100(1):38-43. doi: 10.1016/j.antiviral.2013.07.011[↩]
- Luby SP, Rahman M, Hossain MJ, Blum LS, Husain MM, Gurley E, Khan R, Ahmed BN, Rahman S, Nahar N, Kenah E, Comer JA, Ksiazek TG. Foodborne transmission of Nipah virus, Bangladesh. Emerg Infect Dis. 2006 Dec;12(12):1888-94. doi: 10.3201/eid1212.060732[↩]
- de Wit E, Prescott J, Falzarano D, Bushmaker T, Scott D, Feldmann H, Munster VJ. 2014. Foodborne transmission of Nipah virus in Syrian hamsters. PLoS Pathog. 10(3):e1004001. doi: 10.1371/journal.ppat.1004001[↩][↩]
- Hassan MZ, Sazzad HMS, Luby SP, Sturm-Ramirez K, Bhuiyan MU, Rahman MZ, Islam MM, Ströher U, Sultana S, Kafi MAH, et al. 2018. Nipah virus contamination of hospital surfaces during outbreaks, Bangladesh, 2013-2014. Emerg Infect Dis. 24(1):15–21. doi: 10.3201/eid2401.161758[↩][↩]
- Parashar UD, Sunn LM, Ong F, Mounts AW, Arif MT, Ksiazek TG, Kamaluddin MA, Mustafa AN, Kaur H, Ding LM, Othman G, Radzi HM, Kitsutani PT, Stockton PC, Arokiasamy J, Gary HE Jr, Anderson LJ. Case-control study of risk factors for human infection with a new zoonotic paramyxovirus, Nipah virus, during a 1998-1999 outbreak of severe encephalitis in Malaysia. J Infect Dis. 2000 May;181(5):1755-9. doi: 10.1086/315457[↩]
- Goh KJ, Tan CT, Chew NK, Tan PS, Kamarulzaman A, Sarji SA, Wong KT, Abdullah BJ, Chua KB, Lam SK. Clinical features of Nipah virus encephalitis among pig farmers in Malaysia. N Engl J Med. 2000 Apr 27;342(17):1229-35. doi: 10.1056/NEJM200004273421701[↩][↩][↩][↩][↩][↩]
- Nipah virus. https://www.who.int/news-room/fact-sheets/detail/nipah-virus[↩]
- Wilson A, Warrier A, Rathish B. Contact tracing: a lesson from the Nipah virus in the time of COVID-19. Trop Doct. 2020 Jul;50(3):174-175. doi: 10.1177/0049475520928217[↩]
- Khan SU, Gurley ES, Hossain MJ, Nahar N, Sharker MA, Luby SP. A randomized controlled trial of interventions to impede date palm sap contamination by bats to prevent nipah virus transmission in Bangladesh. PLoS One. 2012;7(8):e42689. doi: 10.1371/journal.pone.0042689[↩]
- Ciancanelli MJ, Basler CF. 2006. Mutation of YMYL in the Nipah virus matrix protein abrogates budding and alters subcellular localization. J Virol. 80(24):12070–12078. doi: 10.1128/JVI.01743-06[↩]
- Ternhag A, Penttinen P. Nipahvirus–ännu en produkt från den asiatiska “virusfabriken” [Nipah virus–another product from the Asian “virus factory”]. Lakartidningen. 2005 Apr 4-10;102(14):1046-7. Swedish.[↩]
- Bossart KN, McEachern JA, Hickey AC, Choudhry V, Dimitrov DS, Eaton BT, Wang LF. 2007. Neutralization assays for differential henipa virus serology using Bio-Plex protein array systems. J Virol Meth. 142(1–2):29–40. doi: 10.1016/j.jviromet.2007.01.003[↩]
- Eaton BT, Broder CC, Middleton D, Wang LF. 2006. Hendra and Nipah viruses: different and dangerous. Nat Rev Microbiol. 4(1):23–35. doi: 10.1038/nrmicro1323[↩]
- Bossart KN, Crameri G, Dimitrov AS, Mungall BA, Feng Y-R, Patch JR, Choudhary A, Wang L-F, Eaton BT, Broder CC. 2005. Receptor binding, fusion inhibition and induction of cross-reactive neutralizing antibodies by a soluble G glycoprotein of Hendra virus. J Virol. 79(11):6690–6702. doi: 10.1128/JVI.79.11.6690-6702.2005[↩]
- White JR, Boyd V, Crameri GS, Duch CJ, van LRK, Wang LF, Eaton BT. 2005. Location of, immunogenicity of and relationships between neutralization epitopes on the attachment protein (G) of Hendra virus. J Gen Virol. 86(10):2839–2848. doi: 10.1099/vir.0.81218-0[↩]
- Steffen DL, Xu K, Nikolov DB, Broder CC. 2012. Henipavirus mediated membrane fusion, virus entry and targeted therapeutics. Viruses. 4(2):280–308. doi: 10.3390/v4020280[↩]
- Marsh GA, Wang LF. 2012. Hendra and Nipah viruses: why are they so deadly? Curr Opin Virol. 2(3):242–247. doi: 10.1016/j.coviro.2012.03.006[↩]
- Liu Q, Bradel-Tretheway B, Monreal AI, Saludes JP, Lu X, Nicola AV, Aguilar HC. 2015. Nipah virus attachment clycoprotein stalk C-terminal region links receptor binding to fusion triggering. J Virol. 89(3):1838–1850. doi: 10.1128/JVI.02277-14[↩]
- Wong JJW, Young TA, Zhang J, Liu S, Leser GP, Komives EA, Lamb RA, Zhou ZH, Salafsky J, Jardetzky TS. 2017. Monomeric ephrinB2 binding induces allosteric changes in Nipah virus G that precede its full activation. Nat Commun. 8(1):781. doi: 10.1038/s41467-017-00863-3[↩]
- Rawlinson SM, Zhao T, Rozario AM, Rootes CL, McMillan PJ, Purcell AW, Woon A, Marsh GA, Lieu KG, Wang LF, et al. 2018. Viral regulation of host cell biology by hijacking of the nucleolar DNA-damage response. Nat Commun. 9(1):3057. doi: 10.1038/s41467-018-05354-7[↩]
- Islam MS, Sazzad HM, Satter SM, Sultana S, Hossain MJ, Hasan M, Rahman M, Campbell S, Cannon DL, Ströher U, et al. 2016. Nipah virus transmission from bats to humans associated with drinking traditional liquor made from date palm sap, Bangladesh, 2011-2014. Emerg Infect Dis. 22(4):664–670. doi: 10.3201/eid2204.151747[↩]
- Fogarty R, Halpin K, Hyatt AD, Daszak P, Mungall BA. 2008. Henipavirus susceptibility to environmental variables. Virus Res. 132(1–2):140–144. doi: 10.1016/j.virusres.2007.11.010[↩]
- Khan M, Nahar N, Sultana R, Hossain M, Gurley ES, Luby S. 2008. Understanding bats access to date palm sap: identifying preventative techniques for Nipah virus transmission. New Orleans AmSocTrop Med Hyg. 4(3):331–333.[↩]
- Luby SP, Rahman M, Hossain MJ, Blum LS, Husain MM, Gurley E, Khan R, Ahmed BN, Rahman S, Nahar N, et al. 2006. Foodborne transmission of Nipah virus, Bangladesh. Emerging Infect Dis. 12(12):1888–1894. doi: 10.3201/eid1212.060732[↩]
- Luby SP, Hossain MJ, Gurley ES, Ahmed BN, Banu S, Khan SU, Homaira N, Rota PA, Rollin PE, Comer JA, et al. 2009. Recurrent zoonotic transmission of Nipah virus into humans, Bangladesh, 2001-2007. Emerg Infect Dis. 15(8):1229–1235. doi: 10.3201/eid1508.081237[↩]
- de Wit E, Munster VJ. 2015. Animal models of disease shed light on Nipah virus pathogenesis and transmission. J Pathol. 235(2):196–205. doi: 10.1002/path.4444[↩]
- Mohd Nor MN, Gan CH, Ong BL. Nipah virus infection of pigs in peninsular Malaysia. Rev Sci Tech. 2000 Apr;19(1):160-5. doi: 10.20506/rst.19.1.1202[↩]
- Escaffre O, Hill T, Ikegami T, Juelich TL, Smith JK, Zhang L, Perez DE, Atkins C, Park A, Lawrence WS, et al. 2018. Experimental infection of Syrian hamsters with aerosolized Nipah virus. J Infect Dis. 218(10):1602–1610. doi: 10.1093/infdis/jiy357[↩]
- Escaffre O, Borisevich V, Rockx B. 2013. Pathogenesis of Hendra and Nipah virus infection in humans. J Infect Dev Ctries. 7(4):308–311. doi: 10.3855/jidc.3648[↩]
- Chua KB. Epidemiology, surveillance and control of Nipah virus infections in Malaysia. Malays J Pathol. 2010 Dec;32(2):69-73. https://www.mjpath.org.my/2010.2/Nipah_virus_infections.pdf[↩]
- Hsu VP, Hossain MJ, Parashar UD, Ali MM, Ksiazek TG, Kuzmin I, Niezgoda M, Rupprecht C, Bresee J, Breiman RF, 2004. Nipah virus encephalitis reemergence, Bangladesh. Emerging Infect Dis. 10(12):2082–2087. doi: 10.3201/eid1012.040701[↩]
- Montgomery JM, Hossain MJ, Gurley E, Carroll GD, Croisier A, Bertherat E, Asgari N, Formenty P, Keeler N, Comer J, et al. 2008. Risk factors for Nipah virus encephalitis in Bangladesh. Emerging Infect Dis. 14(10):1526–1532. doi: 10.3201/eid1410.060507[↩]
- Hughes JM, Wilson ME, Luby SP, Gurley ES, Hossain MJ. 2009. Transmission of human infection with Nipah virus. Clin Infect Dis. 49(11):1743–1748. doi: 10.1086/647951[↩]
- Homaira N, Rahman M, Hossain MJ, Epstein JH, Sultana R, Khan MS, Podder G, Nahar K, Ahmed B, Gurley ES, et al. 2010. Nipah virus outbreak with person-to-person transmission in a district of Bangladesh, 2007. Epidemiol Infect. 138(11):1630–1636. doi: 10.1017/S0950268810000695[↩]
- Sazzad HMS, Jahangir Hossain M, Gurley ES, Ameen KMH, Parveen S, Saiful Islam M, Faruque LI, Podder G, Banu SS, Lo MK, et al. 2013. Nipah virus infection outbreak with nosocomial and corpse-to-human transmission, Bangladesh. Emerg Infect Dis. 19(2):210–217. doi: 10.3201/eid1902.120971[↩]
- Hegde ST, Sazzad HM, Hossain MJ, Alam MU, Kenah E, Daszak P, Rollin P, Rahman M, Luby SP, Gurley ES, 2016. Investigating rare risk factors for Nipah virus in Bangladesh: 2001-2012. Ecohealth. 13(4):720–728. doi: 10.1007/s10393-016-1166-0[↩]
- Gurley ES, Montgomery JM, Hossain MJ, Bell M, Azad AK, Islam MR, Molla MA, Carroll DS, Ksiazek TG, Rota PA, Lowe L, et al. 2007. Person-to-person transmission of Nipah virus in a Bangladeshi community. Emerg Infect Dis. 13(7):1031–1037. doi: 10.3201/eid1307.061128[↩]
- Stone R. 2011. Epidemiology. Breaking the chain in Bangladesh. Science. 331(6021):1128–1131. doi: 10.1126/science.331.6021.1128[↩]
- Hsu VP, Hossain MJ, Parashar UD, Ali MM, Ksiazek TG, Kuzmin I, Niezgoda M, Rupprecht C, Bresee J, Breiman RF. Nipah virus encephalitis reemergence, Bangladesh. Emerg Infect Dis. 2004 Dec;10(12):2082-7. doi: 10.3201/eid1012.040701[↩]
- Epstein JH, Prakash V, Smith CS, Daszak P, McLaughlin AB, Meehan G, Field HE, Cunningham AA. Henipavirus infection in fruit bats (Pteropus giganteus), India. Emerg Infect Dis. 2008 Aug;14(8):1309-11. doi: 10.3201/eid1408.071492[↩]
- Reynes JM, Counor D, Ong S, Faure C, Seng V, Molia S, Walston J, Georges-Courbot MC, Deubel V, Sarthou JL. Nipah virus in Lyle’s flying foxes, Cambodia. Emerg Infect Dis. 2005 Jul;11(7):1042-7. doi: 10.3201/eid1107.041350[↩]
- Wacharapluesadee S, Lumlertdacha B, Boongird K, Wanghongsa S, Chanhome L, Rollin P, Stockton P, Rupprecht CE, Ksiazek TG, Hemachudha T. Bat Nipah virus, Thailand. Emerg Infect Dis. 2005 Dec;11(12):1949-51. doi: 10.3201/eid1112.050613[↩][↩]
- Sendow I, Field HE, Curran J, Darminto, Morrissy C, Meehan G, Buick T, Daniels P. Henipavirus in Pteropus vampyrus bats, Indonesia. Emerg Infect Dis. 2006 Apr;12(4):711-2. doi: 10.3201/eid1204.051181[↩]
- Iehlé C, Razafitrimo G, Razainirina J, Andriaholinirina N, Goodman SM, Faure C, Georges-Courbot MC, Rousset D, Reynes JM. Henipavirus and Tioman virus antibodies in pteropodid bats, Madagascar. Emerg Infect Dis. 2007 Jan;13(1):159-61. doi: 10.3201/eid1301.060791[↩]
- Yob JM, Field H, Rashdi AM, Morrissy C, van der Heide B, Rota P, bin Adzhar A, White J, Daniels P, Jamaluddin A, Ksiazek T. Nipah virus infection in bats (order Chiroptera) in peninsular Malaysia. Emerg Infect Dis. 2001 May-Jun;7(3):439-41. doi: 10.3201/eid0703.010312[↩]
- Hayman DT, Suu-Ire R, Breed AC, McEachern JA, Wang L, Wood JL, Cunningham AA. Evidence of henipavirus infection in West African fruit bats. PLoS One. 2008 Jul 23;3(7):e2739. doi: 10.1371/journal.pone.0002739[↩]
- Ching PK, de los Reyes VC, Sucaldito MN, Tayag E, Columna-Vingno AB, Malbas FF Jr, Bolo GC Jr, Sejvar JJ, Eagles D, Playford G, Dueger E, Kaku Y, Morikawa S, Kuroda M, Marsh GA, McCullough S, Foxwell AR. Outbreak of henipavirus infection, Philippines, 2014. Emerg Infect Dis. 2015 Feb;21(2):328-31. doi: 10.3201/eid2102.141433[↩]
- Rockx B, Brining D, Kramer J, Callison J, Ebihara H, Mansfield K, Feldmann H. Clinical outcome of henipavirus infection in hamsters is determined by the route and dose of infection. J Virol. 2011 Aug;85(15):7658-71. doi: 10.1128/JVI.00473-11[↩]
- Nipah Virus (NiV) Prevention. https://www.cdc.gov/vhf/nipah/prevention/index.html[↩]
- Chong HT, Kunjapan SR, Thayaparan T, Tong J, Petharunam V, Jusoh MR, Tan CT. Nipah encephalitis outbreak in Malaysia, clinical features in patients from Seremban. Can J Neurol Sci. 2002 Feb;29(1):83-7. doi: 10.1017/s0317167100001785[↩]
- M. Jahangir Hossain, Emily S. Gurley, Joel M. Montgomery, Michael Bell, Darin S. Carroll, Vincent P. Hsu, P. Formenty, A. Croisier, E. Bertherat, M. A. Faiz, Abul Kalam Azad, Rafiqul Islam, M. Abdur Rahim Molla, Thomas G. Ksiazek, Paul A. Rota, James A. Comer, Pierre E. Rollin, Stephen P. Luby, Robert F. Breiman, Clinical Presentation of Nipah Virus Infection in Bangladesh, Clinical Infectious Diseases, Volume 46, Issue 7, 1 April 2008, Pages 977–984, https://doi.org/10.1086/529147[↩]
- Lee, K.-E., Umapathi, T., Tan, C.-B., Tjoei-Lian Tjia, H., Chua, T.-S., Oh, H.M.-L., Fock, K.-M., Kurup, A., Das, A., Tan, A.K.-Y. and Lee, W.-L. (1999), The neurological manifestations of Nipah virus encephalitis, a novel paramyxovirus. Ann Neurol., 46: 428-432. https://doi.org/10.1002/1531-8249(199909)46:3<428::AID-ANA23>3.0.CO;2-I[↩]
- Chadha MS, Comer JA, Lowe L, Rota PA, Rollin PE, Bellini WJ, Ksiazek TG, Mishra A. Nipah virus-associated encephalitis outbreak, Siliguri, India. Emerg Infect Dis. 2006 Feb;12(2):235-40. doi: 10.3201/eid1202.051247[↩][↩]
- Hossain MJ, Gurley ES, Montgomery JM, Bell M, Carroll DS, Hsu VP, Formenty P, Croisier A, Bertherat E, Faiz MA, Azad AK, Islam R, Molla MA, Ksiazek TG, Rota PA, Comer JA, Rollin PE, Luby SP, Breiman RF. Clinical presentation of nipah virus infection in Bangladesh. Clin Infect Dis. 2008 Apr 1;46(7):977-84. doi: 10.1086/529147[↩][↩][↩]
- Paton NI, Leo YS, Zaki SR, Auchus AP, Lee KE, Ling AE, Chew SK, Ang B, Rollin PE, Umapathi T, Sng I, Lee CC, Lim E, Ksiazek TG. Outbreak of Nipah-virus infection among abattoir workers in Singapore. Lancet. 1999 Oct 9;354(9186):1253-6. doi: 10.1016/S0140-6736(99)04379-2[↩][↩][↩]
- Sejvar JJ, Hossain J, Saha SK, Gurley ES, Banu S, Hamadani JD, Faiz MA, Siddiqui FM, Mohammad QD, Mollah AH, Uddin R, Alam R, Rahman R, Tan CT, Bellini W, Rota P, Breiman RF, Luby SP. Long-term neurological and functional outcome in Nipah virus infection. Ann Neurol. 2007 Sep;62(3):235-42. doi: 10.1002/ana.21178[↩][↩]
- Chow VT, Tambyah PA, Yeo WM, Phoon MC, Howe J. Diagnosis of nipah virus encephalitis by electron microscopy of cerebrospinal fluid. J Clin Virol. 2000 Dec;19(3):143-7. doi: 10.1016/s1386-6532(00)00094-9[↩]
- Wacharapluesadee S, Hemachudha T. Duplex nested RT-PCR for detection of Nipah virus RNA from urine specimens of bats. J Virol Methods. 2007 Apr;141(1):97-101. doi: 10.1016/j.jviromet.2006.11.023[↩]
- Bossart KN, McEachern JA, Hickey AC, Choudhry V, Dimitrov DS, Eaton BT, Wang LF. Neutralization assays for differential henipavirus serology using Bio-Plex protein array systems. J Virol Methods. 2007 Jun;142(1-2):29-40. doi: 10.1016/j.jviromet.2007.01.003[↩]
- Zhu Z, Bossart KN, Bishop KA, Crameri G, Dimitrov AS, McEachern JA, Feng Y, Middleton D, Wang LF, Broder CC, Dimitrov DS. Exceptionally potent cross-reactive neutralization of Nipah and Hendra viruses by a human monoclonal antibody. J Infect Dis. 2008 Mar 15;197(6):846-53. doi: 10.1086/528801[↩]
- Guillaume V, Lefeuvre A, Faure C, Marianneau P, Buckland R, Lam SK, Wild TF, Deubel V. Specific detection of Nipah virus using real-time RT-PCR (TaqMan). J Virol Methods. 2004 Sep 15;120(2):229-37. doi: 10.1016/j.jviromet.2004.05.018[↩]
- Chua KB, Lam SK, Goh KJ, Hooi PS, Ksiazek TG, Kamarulzaman A, Olson J, Tan CT. The presence of Nipah virus in respiratory secretions and urine of patients during an outbreak of Nipah virus encephalitis in Malaysia. J Infect. 2001 Jan;42(1):40-3. doi: 10.1053/jinf.2000.0782[↩]
- Chua, K.B., Lam, S.K., Tan, C.T., Hooi, P.S., Goh, K.J., Chew, N.K., Tan, K.S., Kamarulzaman, A. and Wong, K.T. (2000), High mortality in Nipah encephalitis is associated with presence of virus in cerebrospinal fluid. Ann Neurol., 48: 802-805. https://doi.org/10.1002/1531-8249(200011)48:5<802::AID-ANA17>3.0.CO;2-M[↩]
- Chua KB. Nipah virus outbreak in Malaysia. J Clin Virol. 2003 Apr;26(3):265-75. doi: 10.1016/s1386-6532(02)00268-8[↩]
- Nipah Virus (NiV) Treatment. https://www.cdc.gov/vhf/nipah/treatment/index.html[↩]
- Chong HT, Kamarulzaman A, Tan CT, Goh KJ, Thayaparan T, Kunjapan SR, Chew NK, Chua KB, Lam SK. Treatment of acute Nipah encephalitis with ribavirin. Ann Neurol. 2001 Jun;49(6):810-3. doi: 10.1002/ana.1062[↩][↩]
- Georges-Courbot MC, Contamin H, Faure C, Loth P, Baize S, Leyssen P, Neyts J, Deubel V. Poly(I)-poly(C12U) but not ribavirin prevents death in a hamster model of Nipah virus infection. Antimicrob Agents Chemother. 2006 May;50(5):1768-72. doi: 10.1128/AAC.50.5.1768-1772.2006[↩]
- NIPAH Virus Guidelines. https://ncdc.mohfw.gov.in/index4.php?lang=1&level=0&linkid=113&lid=228[↩]
- Freiberg AN, Worthy MN, Lee B, Holbrook MR. Combined chloroquine and ribavirin treatment does not prevent death in a hamster model of Nipah and Hendra virus infection. J Gen Virol. 2010 Mar;91(Pt 3):765-72. doi: 10.1099/vir.0.017269-0[↩][↩]
- Negrete OA, Levroney EL, Aguilar HC, Bertolotti-Ciarlet A, Nazarian R, Tajyar S, Lee B. EphrinB2 is the entry receptor for Nipah virus, an emergent deadly paramyxovirus. Nature. 2005 Jul 21;436(7049):401-5. doi: 10.1038/nature03838[↩][↩]
- Dawes BE, Kalveram B, Ikegami T, Juelich T, Smith JK, Zhang L, Park A, Lee B, Komeno T, Furuta Y, Freiberg AN. Favipiravir (T-705) protects against Nipah virus infection in the hamster model. Sci Rep. 2018 May 15;8(1):7604. doi: 10.1038/s41598-018-25780-3[↩]
- Geisbert TW, Mire CE, Geisbert JB, Chan YP, Agans KN, Feldmann F, Fenton KA, Zhu Z, Dimitrov DS, Scott DP, Bossart KN, Feldmann H, Broder CC. Therapeutic treatment of Nipah virus infection in nonhuman primates with a neutralizing human monoclonal antibody. Sci Transl Med. 2014 Jun 25;6(242):242ra82. doi: 10.1126/scitranslmed.3008929[↩]
- Mire CE, Chan YP, Borisevich V, Cross RW, Yan L, Agans KN, Dang HV, Veesler D, Fenton KA, Geisbert TW, Broder CC. A Cross-Reactive Humanized Monoclonal Antibody Targeting Fusion Glycoprotein Function Protects Ferrets Against Lethal Nipah Virus and Hendra Virus Infection. J Infect Dis. 2020 May 11;221(Suppl 4):S471-S479. doi: 10.1093/infdis/jiz515[↩]
- Banerjee S, Gupta N, Kodan P, Mittal A, Ray Y, Nischal N, Soneja M, Biswas A, Wig N. Nipah virus disease: A rare and intractable disease. Intractable Rare Dis Res. 2019 Feb;8(1):1-8. doi: 10.5582/irdr.2018.01130[↩]
- Thomas B, Chandran P, Lilabi MP, George B, Sivakumar CP, Jayadev VK, Bindu V, Rajasi RS, Vijayan B, Mohandas A, Hafeez N. Nipah Virus Infection in Kozhikode, Kerala, South India, in 2018: Epidemiology of an Outbreak of an Emerging Disease. Indian J Community Med. 2019 Oct-Dec;44(4):383-387. doi: 10.4103/ijcm.IJCM_198_19[↩]