Contents
What is tabes dorsalis
Tabes dorsalis is a condition that results from the destruction of the dorsal columns in the spinal cord, normally responsible for position sense, due to late forms of neurosyphilis. Tabes dorsalis results in loss of position sense causes severe gait and leg ataxia (balance and motor control problems). Tabes dorsalis is a complication of untreated syphilis that involves muscle weakness and abnormal sensations. Late forms of neurosyphilis usually occur decades after untreated syphilis infection and the disease is more frequent in males than in females. Tabes dorsalis onset is commonly during mid-life. The incidence of tabes dorsalis is rising, in part due to co-associated HIV infection.
Tabes dorsalis is a slow degeneration of the nerve cells and nerve fibers in the dorsal columns in the spinal cord that carry sensory information to the brain. The degenerating nerves are in the dorsal columns of the spinal cord (the portion closest to the back of the body) and carry information that help maintain a person’s sense of position.
Tabes dorsalis is the result of an untreated syphilis infection. Symptoms may not appear for some decades after the initial infection and include weakness, diminished reflexes, unsteady gait, progressive degeneration of the joints, loss of coordination, episodes of intense pain and disturbed sensation, personality changes, dementia, deafness, visual impairment, and impaired response to light.
Syphilis is an infection caused by the bacterium Treponema pallidum that is most often spread by sexual contact, such as through direct contact with a syphilis sore (chancre), a firm, raised, painless sore.
Syphilis is easily treated with antibiotics but can cause severe health problems if left untreated. An infected mother can also pass the disease to her unborn child, with serious and potentially fatal consequences for the baby.
There are several possible stages with syphilis:
- Primary syphilis—the primary stage begins about 2-3 weeks after being infected. One or more chancres appear, usually on the part of the body exposed to the sexual partner’s chancre, such as on the penis or vagina. However, the chancre is usually painless and may go unnoticed, especially if it is in the rectum or on the cervix, and disappears within 4-6 weeks, healing regardless of whether the infected person is treated or not.
- Secondary syphilis—if primary syphilis is left untreated, secondary syphilis may occur from 6 weeks to 6 months after the chancre first appears. It is marked by a skin rash that often is rough, red, and spotted, appearing frequently on the palms of the hands and the bottoms of the feet (an unusual place for most other causes of rashes) and that usually does not itch. There may be other symptoms as well, such as fever, fatigue, swollen lymph nodes (“glands”), sore throat, and body aches.
- Late, tertiary syphilis—if untreated, secondary syphilis may continue into a latent stage, during which an infected person has no symptoms but continues to have the infection, and this stage can last for years. If still untreated, about 15% of people will develop the complications of late, or tertiary, syphilis. In these cases, the bacteria can damage the heart, eyes, brain, nervous system, bones, joints, or almost any other part of the body. When the central nervous system is affected, it is called neurosyphilis. Tertiary syphilis can last for years, with the final stage leading to mental illness, blindness, other neurological problems, heart disease, and death.
Syphilis is most infectious during the primary and secondary stages. In 2014, about one-third of over 63,000 new cases of syphilis reported to the Centers for Disease Control and Prevention (CDC) were primary or secondary stage syphilis. Eighty-three percent of these cases were among men who have sex with men.
Penicillin, administered intravenously, is the treatment of choice for tabes dorsalis. Associated pain can be treated with opiates, valproate, or carbamazepine. Patients may also require physical or rehabilitative therapy to deal with muscle wasting and weakness. Preventive treatment for those who come into sexual contact with an individual with tabes dorsalis is important.
Tabes dorsalis causes
Tabes dorsalis is a form of neurosyphilis, which is a complication of late stage syphilis infection. Syphilis is a bacterial infection that is spread sexually.
When syphilis is untreated, the bacteria damages the spinal cord and peripheral nervous tissue. This leads to the symptoms of tabes dorsalis.
Tabes dorsalis is now very rare because syphilis is usually treated early in the disease.
Tabes dorsalis symptoms
Symptoms of tabes dorsalis are caused by damage to the nervous system. Symptoms include any of the following:
- Abnormal sensations (paresthesia), often called “lightning pains”
- Problems walking such as with the legs far apart
- Loss of coordination and reflexes
- Joint damage, especially of the knees
- Muscle weakness
- Vision changes
- Bladder control problems
- Sexual function problems
Tabes dorsalis possible complications
Tabes dorsalis complications may include:
- Blindness
- Paralysis
- Dementia.
Tabes dorsalis diagnosis
The health care provider will perform a physical exam, focusing on the nervous system.
If syphilis infection is suspected, tests may include the following:
- Cerebrospinal fluid (CSF) examination
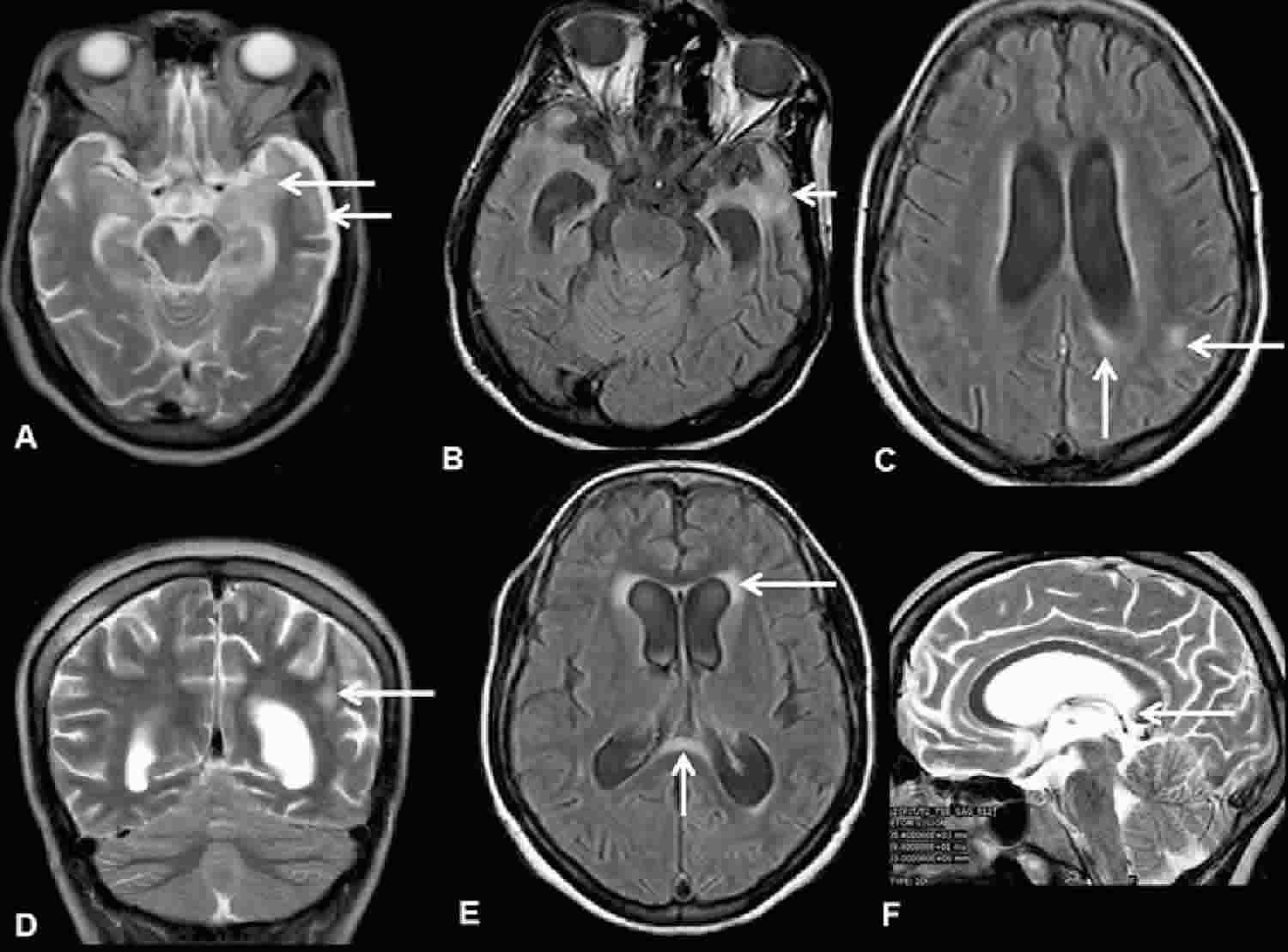
- Head CT, spine CT, or MRI scans of the brain and spinal cord to rule out other diseases
- Serum VDRL (Venereal Disease Research Laboratory) or serum RPR (Rapid Plasma Reagin) (used as a screening test for syphilis infection)
If the serum VDRL or serum RPR test is positive, one of the following tests will be needed to confirm the diagnosis:
- FTA-ABS (Fluorescent Treponemal Antibody Absorbed)
- MHA-TP (Microhemagglutination assay for Treponema pallidum antibodies)
- TP-EIA (Treponema pallidum-Enzyme immunoassay)
- TP-PA (Treponema pallidum-Particle agglutination)
The laboratory diagnosis of syphilis is challenging and requires using a combination of clinical and laboratory criteria to differentiate active infection, prior infection, and absence of infection 1. Treponema pallidum cannot be cultivated on artificial medium, but the organism can be grown using special techniques that involve inoculation in rabbits. In clinical samples, spirochetes can occasionally be visualized in specimens taken from cutaneous lesions using dark-field microscopy techniques. In addition, silver staining and immunohistochemical staining of tissue samples can demonstrate characteristic spirochetes on clinical biopsy specimens. Use of dark-field microscopy or immunohistochemical staining on oral specimens is not recommended due to the extremely poor specificity caused by abundant non-syphilitic oral Treponema species. Serologic testing remains the primary tool for diagnosis in most patients with syphilis and these tests include “nontreponemal” and “treponemal” tests. Although PCR testing is sometimes used for research purposes, there is no FDA-approved PCR test for syphilis at present. Research use of PCR detection of Treponema pallidum DNA has expanded the clinical sites from which Treponema pallidum can be detected.
The most common syphilis tests detect antibodies in the blood that are produced in response to a Treponema pallidum infection. Some methods that are used less commonly directly detect the bacterium or its genetic material (DNA).
Serologic testing for syphilis
In the absence of dark-field microscopy, a probable diagnosis of syphilis is possible with the use of two types of serologic tests: nontreponemal and treponemal. Use of only one type of serologic test is insufficient for diagnosis since each test used alone has major limitations, including false-positive results in persons without syphilis and the inability for treponemal tests to distinguish between recent and distant infection. Both types of tests have several advantages and disadvantages as well as differing test characteristics.
Nontreponemal serologic tests
The nontreponemal tests include Venereal Disease Research Laboratory (VDRL), Rapid Plasma Reagin (RPR), Toluidine Red Unheated Serum Test (TRUST), and Unheated Serum Reagin (USR) 1. These tests measure IgM and IgG antibody and are not specific for Treponema pallidum. Nontreponemal test results are reported with a qualitative result and a quantitative titer, which usually correlates with disease activity 2. A fourfold change in titer, equivalent to a change of two dilutions (e.g., from 1:16 to 1:4 or from 1:8 to 1:32) is considered necessary to demonstrate a clinically significant difference 3. Sequential serologic tests in individual patients should be performed using the same testing method, preferably by the same laboratory. The Venereal Disease Research Laboratory (VDRL) and RPR tests are equally valid assays, but quantitative results from the two tests cannot be compared directly because RPR titers are often slightly higher than Venereal Disease Research Laboratory (VDRL) titers. TRUST is similar to RPR test whereas Unheated Serum Reagin (USR) is similar to VDRL, though in the United States TRUST and Unheated Serum Reagin (USR) are not often used. The nontreponemal tests have several drawbacks, including (1) they are labor intensive to perform, (2) results are typically not available for at least 7 days, (3) the tests have low sensitivity in certain stages, particularly early primary, late latent, and tertiary, and (4) false-positive reactions can occur. Nontreponemal tests usually become nonreactive with time after treatment. In some patients, however, nontreponemal antibodies can persist at a low titer (the definition “low” titer is dependent on laboratory and clinical context, but less than 1:8 is generally consider “low”) for a long period of time, sometimes for the life of the patient. This response is referred to as the “serofast reaction.” In addition, in some patients, nontreponemal tests may, with time, become nonreactive in the absence of therapy.
Treponemal serologic tests
The treponemal serologic tests include Treponema pallidum particle agglutination (TP-PA), fluorescent treponemal antibody absorption (FTA-ABS), and various enzyme immunoassays (EIAs) and chemiluminescence immunoassays 1. These tests measure antibody directed against Treponema pallidum antigens by particle agglutination, immunofluorescence, or enzyme immunoassay; some detect IgG only whereas others detect both IgM and IgG. These qualitative tests most often remain reactive for life, even after adequate treatment, but 15% to 25% of patients treated during the primary stage revert to being serologically nonreactive after two to three years 4. Treponemal antibody titers correlate poorly with disease activity, and they should not be used to assess treatment response.
Patterns of serologic reactivity and sensitivity of tests
The common patterns for serologic reactivity with syphilis tests depend on the specific test used, the stage of syphilis, and whether the patient has received treatment 5. The sensitivity of serologic testing also varies based on the test used and stage of syphilis (Table 1). Serologic testing for syphilis has the highest yield during secondary syphilis. Serologic tests for syphilis may be negative during very early primary syphilis. Thus, when serologic tests do not correspond with clinical findings suggestive of primary syphilis, presumptive treatment is recommended if the patient has known risk factors for syphilis; in this setting, use of other tests, such as dark-field microscopy, biopsy, or PCR, should be considered.
Table 1. Sensitivity and Specificity of common serological tests in Untreated Syphilis
| Sensitivity During Stage of Infection, % (range) | Specificity, % range | |||||
|---|---|---|---|---|---|---|
| Test | Primary | Secondary | Latent | Late | ||
| *FTA-ABS and TP-PA are generally considered equally sensitive in the primary stage of disease. Abbreviations: | ||||||
| VDRL | 78 (74-87) | 100 | 95 (88-100) | 71 (37-94) | 98 (96-99) | |
| RPR | 86 (77-99) | 100 | 98 (95-100) | 73 | 98 (93-99) | |
| FTA-ABS | 84 (70-100) | 100 | 100 | 96 | 97 (94-100) | |
| TP-PA | 88 (86-100) | 100 | 100 | NA | 96 (95-100) | |
| ELISA (IgG) | 100 | 100 | 100 | NA | 100 | |
Prior Serologic Testing for Syphilis
The healthcare professional should determine the date and results of the patient’s most recent serologic test for syphilis, even if the patient reports no history of the disease. Prior results, if available, are particularly helpful when evaluating a patient that has a low titer serologic test for syphilis, no signs or symptoms that suggest a clinical diagnosis of syphilis, and no known contact with an early case of syphilis. Local health departments can often provide information on whether the patient has been reported as having had syphilis in the past, including reported serologic test results and treatment history.
Serologic testing algorithms
Given that treponemal and nontreponemal tests each have significant advantages and disadvantages, these lab tests are used together as part of a screening algorithm in order to maximize sensitivity and specificity for the detection of syphilis infection. Clinicians should be aware of their institution’s chosen method in order to most efficiently use serologic tests to screen for, diagnose, and monitor syphilis disease.
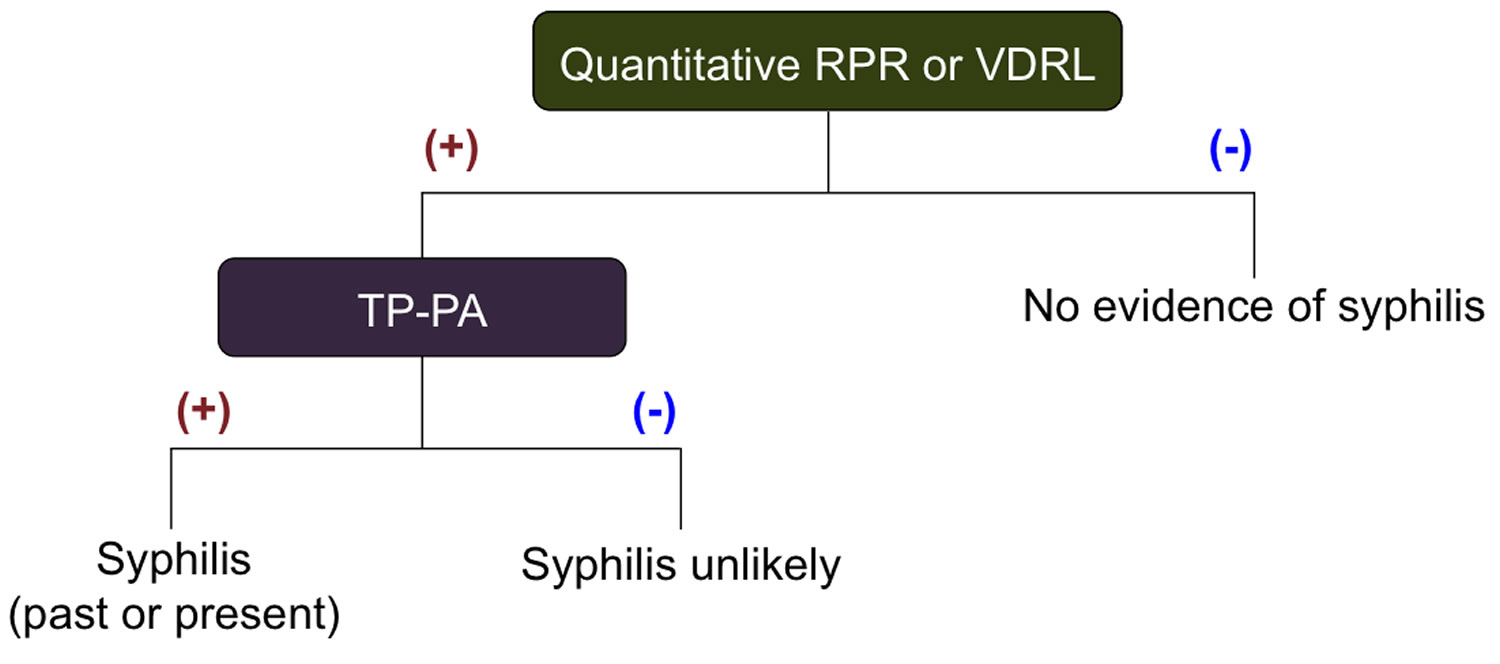
Standard (Traditional) Syphilis Screening Algorithm
Traditionally, the syphilis screening algorithm has consisted of initial screening with a nontreponemal test (VDRL or RPR), with further testing on a positive initial test with a treponemal test (TP-PA or EIA) (Figure 1). Patients with a negative screening test were relegated to periodic repeat screening whereas patients with positive results required a treponemal test to confirm a diagnosis of syphilis. The major limitations with using a nontreponemal test for initial screening include the personnel time required to perform a labor-intensive test, biologic false positives (i.e. pregnancy, medication use, and other conditions) and, as with all diagnostic tests for syphilis, the inability to detect early primary or latent infection.
Figure 1. Standard syphilis screening algorithm
Abbreviation: TP-PA =Treponema pallidum-Particle agglutination
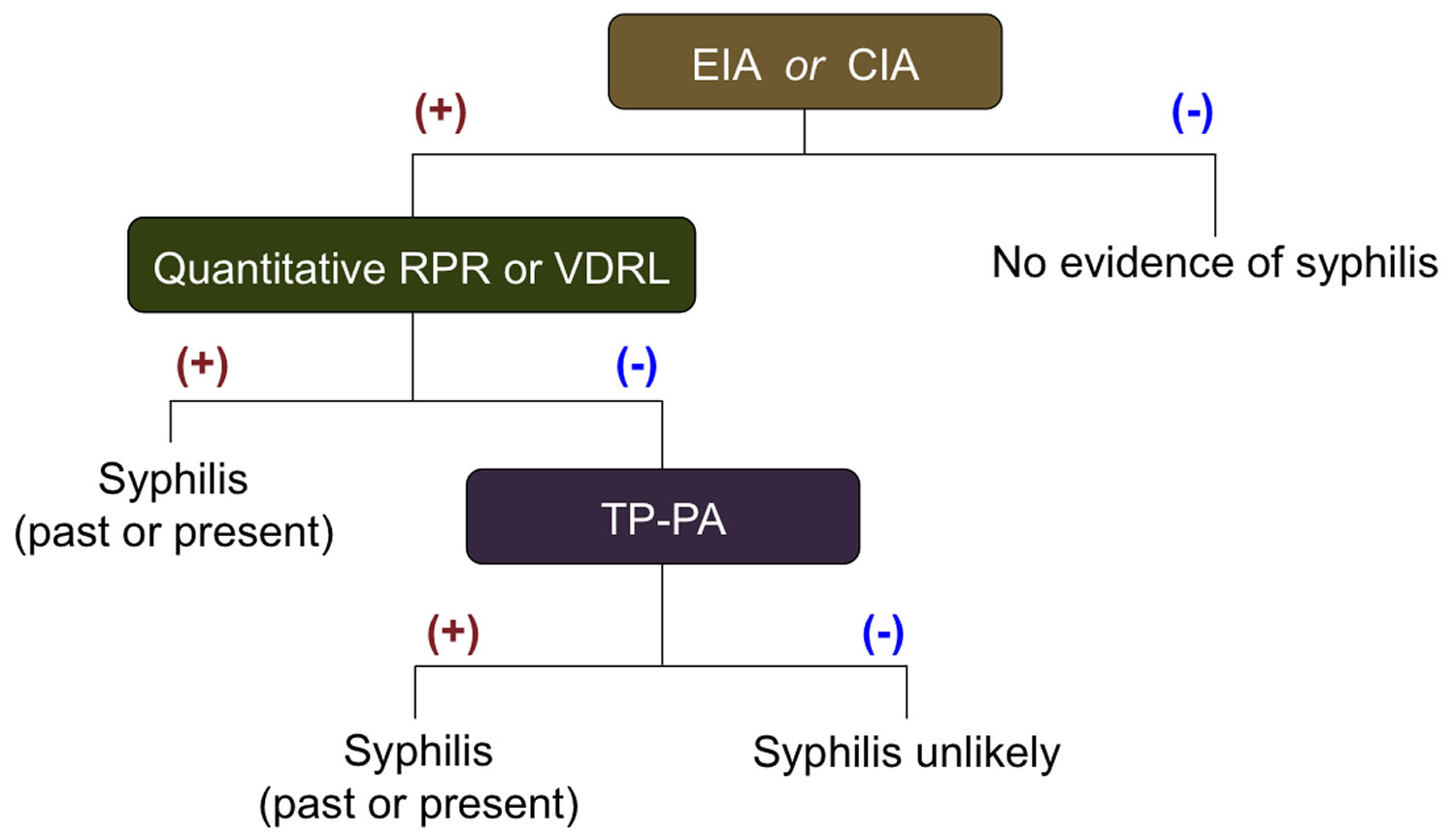
[Source 2 ]Reverse Sequence Syphilis Screening Algorithm
Another option for syphilis screening is to use Treponema pallidum-specific enzyme immunoassays (EIAs) or chemiluminescence immunoassays (CIAs) as an initial screening test. In recent years, increasing numbers of clinical laboratories and blood banks have begun using treponemal EIA or chemiluminescence immunoassays (CIAs) as the initial screening laboratory test for syphilis. With this approach, a positive enzyme immunoassay (EIA) or chemiluminescence immunoassay (CIA) test is followed by further testing with a nontreponemal test—often referred to as reverse screening (Figure 2). In the reverse screening algorithm, negative treponemal results are relegated to follow-up screening as with the standard (traditional) algorithm. Positive treponemal results undergo a confirmatory nontreponemal test (i.e. RPR) to guide management. In the event of a positive EIA and a negative nontreponemal test, a second confirmatory treponemal test (TP-PA) is performed. If either of the confirmatory tests is positive and there is no history of prior, treated syphilis, the patient is diagnosed with syphilis 7. This ‘reverse screening algorithm’ has several advantages and disadvantages distinguishing it from the standard (traditional) screening algorithm. Advantages of the reverse sequence algorithm include improved detection of early primary and treated infection, low cost, and reduced laboratory time and effort (much less pipetting and circumventing the manual dilutions of nontreponemal testing).
Figure 2. Reverse Sequence Syphilis Screening Algorithm
Abbreviations:
- Treponema pallidum-specific enzyme immunoassay (EIA) or chemiluminescence immunoassay (CIA)
- VDRL = Venereal Disease Research Laboratory
- RPR = Rapid Plasma Reagin
- FTA-ABS = Fluorescent Treponemal Antibody Absorbed
- TP-PA =Treponema pallidum-Particle agglutination
- ELISA= Enzyme Linked Immunoassay
Discordant Test Results Using Reverse Screening
In the scenario where a patient has a positive treponemal screening test (EIA), a negative nontreponemal test, and a positive second treponemal test (TP-PA), there are several possible scenarios: prior treated syphilis, early syphilis, untreated latent syphilis, or false-positive test. If the patient has received prior treatment for syphilis and has no evidence by history or examination for recent infection with Treponema pallidum, then the patient does not require further evaluation or management 2. Patients without prior treatment and no evidence for recent infection are considered to have latent syphilis and require further evaluation and treatment. If recent infection possibly occurred, then repeat nontreponemal testing should take place 2 to 3 weeks later; if this repeat testing is positive the patient likely has early syphilis and if the test is negative then further evaluation is usually not needed.
Tabes dorsalis treatment
The goals of treatment are to cure the infection and slow the disease. Treating the infection helps prevent new nerve damage and may reduce symptoms. Treatment does not reverse existing nerve damage.
Medicines likely to be given include:
- Penicillin or other antibiotics for a long time to make sure the infection goes away
- Painkillers to control pain
The recommended regimen for both neurosyphilis and ocular syphilis is aqueous crystalline penicillin G 18-24 million units per day, given as 3-4 million units intravenously (IV) every 4 hours (or as continuous infusion), for a total of 10 to 14 days 8. If adherence to therapy can be ensured, an acceptable alternative regimen is procaine penicillin G 2.4 million units IM once daily with probenecid 500 mg orally four times a day. Both agents are given for 10 to 14 days. It is important to note that some experts believe the duration of neurosyphilis therapy is not sufficient for treatment of late latent syphilis. Therefore, benzathine penicillin G 2.4 million units IM once per week for up to 3 weeks can be considered after completion of a neurosyphilis regimen in order to provide a comparable total duration of therapy. In addition, systemic corticosteroids have been used by some experts or specialists as adjunctive therapy for otologic syphilis, but data are insufficient to support the use of systemic corticosteroid therapy for otologic syphilis or any other form of syphilis.
Treatment of Neurosyphilis in Penicillin-Allergic Patients: Limited data suggest that ceftriaxone 2 g daily either IM or IV for 10 to 14 days can be used as an alternative treatment for persons with neurosyphilis 8. Other regimens have not been adequately studied for use in patients with neurosyphilis.
Symptoms of existing nervous system damage need to be treated. People who are unable to eat, dress themselves, or take care of themselves may need help. Rehabilitation, physical therapy, and occupational therapy may help with muscle weakness.
Tabes dorsalis prognosis
If left untreated, tabes dorsalis can lead to paralysis, dementia, and blindness. Existing nerve damage cannot be reversed.
- Association of Public Health Laboratories (APHL) and Centers for Disease Control and Prevention (CDC). Laboratory diagnostic testing for Treponema pallidum, Expert Consultation Meeting Summary Report, January 13-15, 2009, Atlanta, GA. https://www.aphl.org/programs/infectious_disease/std/Documents/ID_2009Jan_Laboratory-Guidelines-Treponema-pallidum-Meeting-Report.pdf[↩][↩][↩]
- Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. Syphilis. MMWR Recomm Rep. 2015;64(No. RR-3):1-137.[↩][↩][↩]
- Syphilis. https://www.std.uw.edu/go/pathogen-based/syphilis/core-concept/all[↩]
- Romanowski B, Sutherland R, Fick GH, Mooney D, Love EJ. Serologic response to treatment of infectious syphilis. Ann Intern Med. 1991;114:1005-9.[↩]
- Peeling RW, Ye H. Diagnostic tools for preventing and managing maternal and congenital syphilis: an overview. Bull World Health Organ. 2004;82:439-46.[↩]
- Seña AC, White BL, Sparling PF. Novel Treponema pallidum serologic tests: a paradigm shift in syphilis screening for the 21st century. Clin Infect Dis. 2010;51:700-8.[↩]
- Centers for Disease Control and Prevention (CDC). Discordant results from reverse sequence syphilis screening–five laboratories, United States, 2006-2010. MMWR Morb Mortal Wkly Rep. 2011;60:133-7.[↩][↩]
- 2015 Sexually Transmitted Diseases Treatment Guidelines. Syphilis. https://www.cdc.gov/std/tg2015/syphilis.htm[↩][↩]