Contents
What is uterine rupture
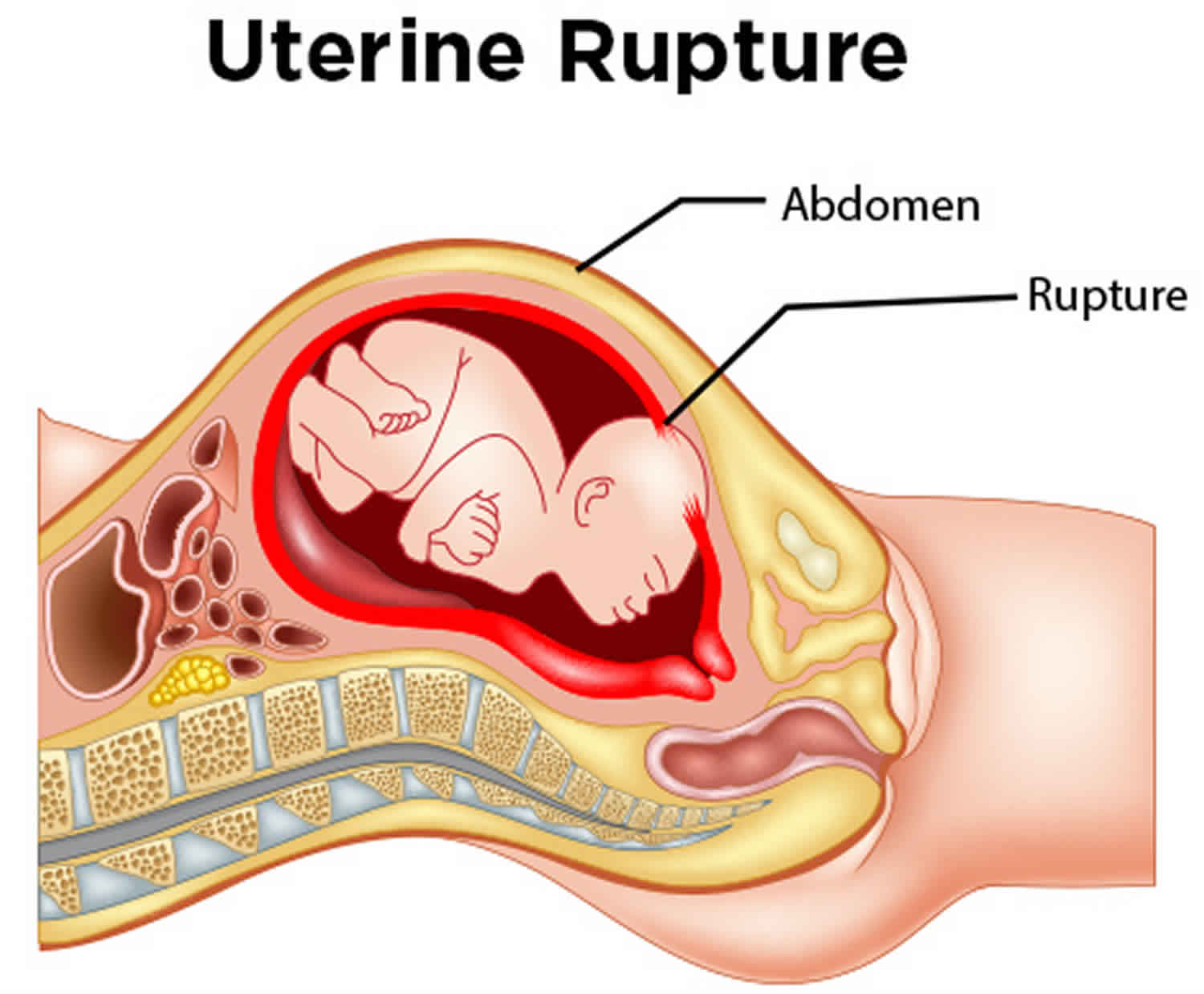
Uterine rupture is a rare but very dangerous complication in which your uterus tears open along the scar line from a prior C-section (cesarean section) or major uterine surgery during pregnancy or early labor 1. Very rarely, uterine rupture can also occur in women who had never had previous uterine surgery. Less than 1 percent of vaginal birth after C-sections lead to uterine rupture. But doctors cannot predict if uterine rupture is likely to occur in a woman. This risk, albeit very small, is unacceptable to some women. An emergency C-section is needed to prevent life-threatening complications for both the mother and the baby. Your uterus might need to be removed (hysterectomy). A World Health Organization (WHO) systematic review of uterine rupture worldwide, published in 2005, reported an overall median incidence of uterine rupture of 5.3 per 10,000 deliveries based on eight population-based studies identified 2.
In the UK national case-control study 1, two out of the 159 women with a uterine rupture died, a case fatality of 1.3%. 15 out of the 159 (9%) women had a hysterectomy following uterine rupture, ten (6%) women had one or more other organs damaged at rupture or removed during surgery, and 69 (43%) women had other or additional morbidity following their uterine rupture 1. This group included four women who required ventilation and 62 who received a blood transfusion. 50 (31%) of the woman with a uterine rupture were admitted to critical or high dependency care for a median duration of 2 days (range 1–12) 1.
Outcomes were known for 152 of the infants born to women with a uterine rupture. There were 15 stillbirths (12 antepartum, seven of which occurred prior to uterine rupture in women who were induced following intra-uterine death, and three intrapartum) and ten early neonatal deaths 1. Excluding the stillbirths that occurred prior to uterine rupture, the perinatal mortality rate was 124 per 1,000, significantly higher than the national rate of 7.5 per 1,000 3. Major complications were reported in an additional 19 infants, including nine infants diagnosed with neonatal encephalopathy and six diagnosed with respiratory distress syndrome. A total of 56/137 (41%) of the infants were admitted to a neonatal unit for a median duration of 3 days (range 1–48) 1.
The percent of vaginal birth after C-sections is dropping in the United States for many reasons. Some doctors, hospitals, and patients have concerns about the safety of vaginal birth after C-section. Some hospitals and doctors are unwilling to do vaginal birth after C-sections because of fear of lawsuits and insurance or staffing expenses. Many doctors, however, question if this trend is in the best interest of women’s health.
Choosing to try a vaginal birth after C-section is complex. If you are interested in a vaginal birth after C-section, talk to your doctor and read up on the subject. Only you and your doctor can decide what is best for you. vaginal birth after C-sections and planned c-sections both have their benefits and risks. Learn the pros and cons and be aware of possible problems before you make your choice.
What causes uterine rupture
Patients having had prior classical cesarean section (C-section) or prior incision into the contractile portion of the uterus have higher rates of uterine rupture. In a caesarean section, the baby is delivered through a cut made through the abdominal wall and the uterine wall. The stretching that occurs during pregnancy or the strong contractions of labor can tear the scar left by this cut, resulting in uterine rupture. Very rarely, uterine rupture can also occur in women who had never had previous uterine surgery. Likewise, the rate of uterine rupture is felt to increase with increasing number of prior cesarean sections. With 1 prior low transverse cesarean section, the rate of uterine rupture is less than 1%; whereas, the rate is slightly higher with 2 prior cesarean sections at 1% to 2% 4. Recent reports of an increased risk of morbidity, particularly due to uterine rupture, are thought to have contributed to a marked decrease in some countries in the number of women attempting vaginal birth after caesarean section 5. The rate of caesarean section delivery in the UK is increasing, with previous caesarean section being the most common primary obstetric indication for repeat section 6.
Risk of uterine rupture
A total of 139 (87%) of the uterine ruptures occurred in women who had previously delivered by caesarean section. Women who had two or more previous caesarean deliveries had a raised odds of having a uterine rupture compared to women with only one previous caesarean delivery, as did women who had an interval of less than 12 months compared to ≥24 months between their last cesarean section and their last menstrual period in their current pregnancy 1. There was no evidence to suggest a departure from linearity in the relationship between odds of rupture and number of caesarean deliveries, with the odds of rupture increasing by 3.02 for every one additional caesarean delivery. However, there was evidence of a departure in linearity in the association between uterine rupture and caesarean section-pregnancy interval, with the odds of rupture appearing to plateau for intervals beyond 12 months 1.
The presence of placenta previa also increased the odds of uterine rupture, although note that this finding is based on a very small number of women and should be interpreted with caution. The odds of uterine rupture was also raised in women who planned to have a vaginal delivery in their current pregnancy compared to women who planned to deliver by elective cesarean section. This finding was irrespective of whether the women who planned to have a vaginal delivery had their labour induced and/or received oxytocin in labor 1. However, the women who had prostaglandin labor induction and/or oxytocin used in labor appeared to have raised odds of uterine rupture compared to the women who labored without prostaglandin induction or oxytocin in labor 1. No significant interactions were found.
Characteristics of uterine rupture cases without a previous cesarean section
The characteristics of the 20 women who experienced a uterine rupture in the absence of a previous C-section when compared to a group of population-based control women, these women were more likely to be aged 35 years or older (40% versus 20% in control women) and were more likely to have a parity of three or more (30% versus 9% in control women). There was also a suggestion that the women who did not have a previous delivery by C-section and experienced a uterine rupture were more likely to have an infant with a birthweight of 4,000 g or more (26% versus 12%), although this was not statistically significant 1.
Uterine rupture signs and symptoms
Signs and symptoms of uterine rupture include fetal heart rate abnormalities, abdominal pain, and vaginal bleeding.
Two hundred nine (86.4%) of mothers were diagnosed with uterine rupture preoperatively, 33 (13.6%) of cases were diagnosed intraoperatively. One hundred fourty-two (58.7%) of mothers had abdominal pain and or tenderness, 148 (61.2%) had cessation of uterine contraction, and 177 (73.1%) didn’t have fetal heart sounds, 102 (42.1%) mothers had multiple fetal palpable part, 83 (34.3%) mothers presented with hypovolemic shock, and 37 (15.3%) mothers came with vaginal bleeding. Two hundred eighteen (90.1%) of mothers had preoperative hematocrit of ≥34, 17(7%) mothers had preoperative hematocrit value of 22–33% and 7 (2.9%) mothers had preoperative hematocrit value of < 22% 7.
Uterine rupture complications
Uterine rupture is associated with a number of acute and long term complications. These include anemia, need for transfusion, bladder injury, wound infection, sepsis and death 8. Complications like obstetric fistula, foot drop, psychological trauma, permanent loss of fertility are some of the long term outcomes 8. Acute renal failure from pre-renal azotemia is also possible following massive hemorrhage 9. Among these, the most commonly encountered complication is hemorrhage leading to anemia 10.
Uterine rupture treatment
If uterine rupture happens during labor, the woman must have an immediate C-section (surgical delivery of her baby) to save both her life and that of her baby. The woman’s womb and nearby organs can be damaged at uterine rupture or removed during surgery and she may need a blood transfusion because of severe bleeding. Moreover, her baby may develop respiratory distress syndrome and other life-threatening complications 1.
The type of surgical intervention on the uterus is dependent on the type and extent of uterine rupture, hemodynamic status of the mother, desire for future fertility, presence of gross infection and experience of the surgeon 11. This could be total or subtotal abdominal hysterectomy, uterine repair with or without tubal ligation 12. Uterine repair should be reserved for women who have low transverse rupture, no extension of the tear to broad ligaments, cervix or vagina, easily controllable hemorrhage, good general condition, desire for future child bearing and no evidence of gross infection. Hysterectomy is appropriate for those with one of the above intra operative findings 13.
- Fitzpatrick KE, Kurinczuk JJ, Alfirevic Z, Spark P, Brocklehurst P, Knight M. Uterine rupture by intended mode of delivery in the UK: a national case-control study. PLoS Med. ;9(3):e1001184. doi:10.1371/journal.pmed.1001184 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3302846[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- WHO systematic review of maternal mortality and morbidity: the prevalence of uterine rupture. Hofmeyr GJ, Say L, Gülmezoglu AM. BJOG. 2005 Sep; 112(9):1221-8.[↩]
- Centre for Maternal and Child Enquiries. Perinatal mortality 2008. London: Centre for Maternal and Child Enquiries; 2010[↩]
- Habak PJ, Kole M. Pregnancy, Vaginal Birth After Cesarean Delivery (VBAC) [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507844[↩]
- Planned elective repeat caesarean section versus planned vaginal birth for women with a previous caesarean birth. Dodd JM, Crowther CA, Huertas E, Guise JM, Horey D. Cochrane Database Syst Rev. 2004 Oct 18; (4):CD004224.[↩]
- RCOG Clinical Effectiveness Support Unit. The National Sentinel Caesarean Section Audit Report. London: RCOG; 2001.[↩]
- Astatikie G, Limenih MA, Kebede M. Maternal and fetal outcomes of uterine rupture and factors associated with maternal death secondary to uterine rupture. BMC Pregnancy Childbirth. 2017;17(1):117. Published 2017 Apr 12. doi:10.1186/s12884-017-1302-z https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5389173[↩]
- Yasmeen Khooharo JZY, Malik SH, Amber A, Majeed N, Malik NH, Pervez H, Majeed I, Majeed N. Incidence and management of rupture uterus in obstructed labour. J Ayub Med Coll Abbottabad. 2013;25:1–2[↩][↩]
- Sunitha K, Indira I, Suguna P. Clinical Study of Rupture Uterus – Assessment of Maternal and Fetal Outcome. J Dental Med Scie. 2015;14(3):39–45[↩]
- Astatikie G, Limenih MA, Kebede M. Maternal and fetal outcomes of uterine rupture and factors associated with maternal death secondary to uterine rupture. BMC Pregnancy Childbirth. 2017;17:117. doi: 10.1186/s12884-017-1302-z[↩]
- Ahmed DM, Mengistu TS, Endalamaw AG. Incidence and factors associated with outcomes of uterine rupture among women delivered at Felegehiwot referral hospital, Bahir Dar, Ethiopia: cross sectional study. BMC Pregnancy Childbirth. 2018;18(1):447. Published 2018 Nov 16. doi:10.1186/s12884-018-2083-8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6240227[↩]
- Uterine rupture in Mekelle, northern Ethiopia, between 2009 and 2013. Berhe Y, Gidey H, Wall LL. Int J Gynaecol Obstet. 2015 Aug; 130(2):153-6.[↩]
- Gerard G, Nahum M, FACS. Uterine Rupture in Pregnancy: FACOG, FACS; 2016.[↩]