Contents
- Type 1 diabetes
- How does insulin work?
- Is there a cure for type 1 diabetes?
- What happens if people with type 1 diabetes don’t receive insulin?
- What is an insulin pump?
- What is a smart insulin pen?
- What are blood sugar levels?
- Monitoring your blood sugar levels
- What happens when my blood sugar levels are too high?
- What happens when your blood sugar levels are too low?
- What happens if I don’t treat hypoglycemia?
- What is diabetic ketoacidosis?
- What is the difference between type 1 and type 2 diabetes?
- Type 1 diabetes pregnancy
- Type 1 diabetes causes
- Type 1 diabetes signs and symptoms
- Type 1 diabetes complications
- Type 1 diabetes prevention
- Type 1 diabetes diagnosis
- Type 1 diabetes treatment
- Type 1 diabetes prognosis
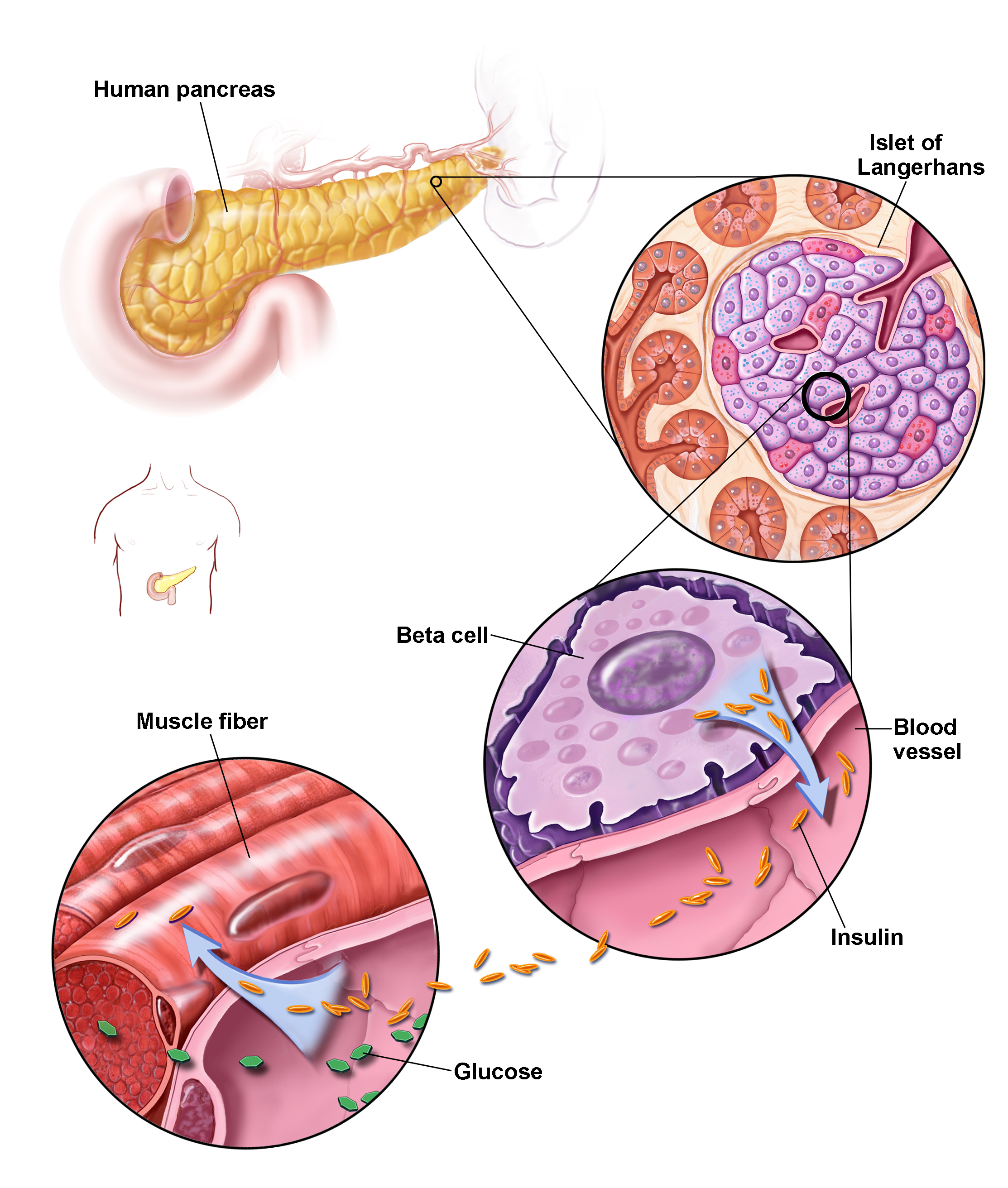
Type 1 diabetes
Type 1 diabetes previously known as juvenile diabetes or insulin-dependent diabetes mellitus (IDDM), is an autoimmune condition characterized by high blood sugar levels (high blood glucose or hyperglycemia) that occurs when your body’s immune system attacks the insulin-producing beta cells in your pancreas (an organ behind your stomach) and destroys them. The pancreas then produces little or no insulin. When you eat, your body breaks down sugar and starches from food into glucose (sugar) to use for energy. Your pancreas makes a hormone called insulin that controls the amount of glucose (sugar) in your blood. Insulin helps glucose (sugar) produced by the digestion of carbohydrates move from your blood into your body’s cells where it can be used for energy. When you have type 1 diabetes, your body doesn’t make enough insulin or no insulin, so the glucose (sugar) cannot enter your body’s cells and you end up with too much sugar in your blood (hyperglycemia). People with type 1 diabetes depend on insulin every day of their lives to replace the insulin their body cannot produce. People with type 1 diabetes must monitor their glucose levels throughout the day to ensure they stay within their target glucose range. This can be done using a blood glucose monitor or continuous glucose monitor.
The onset of type 1 diabetes occurs most frequently during childhood or adolescence, however you can also develop type 1 diabetes in adults. About 10 per cent of all cases of diabetes are type 1 diabetes. The latest World Health Organization (WHO) global estimate indicates that 40% of the 9 million patients diagnosed with type 1 diabetes are under the age of 40 1. The prevalence is about 10 times higher in high-income countries compared to low-income countries. The risk of developing type 1 diabetes in the general population is 6%, while in family members of a person already suffering from type 1 diabetes, the risk increases 15 times 2.
According to the Japan Diabetes Society diagnostic criteria, three pathogenic definitions of type 1 diabetes mellitus have been demonstrated: slowly progressive, acute‐onset and fulminant 3, 4, 5. In patients with acute‐onset and fulminant type 1 diabetes mellitus, lifelong insulin treatment initiation is required soon after the diagnosis because of the marked acute progression of insulin deficiency 4, 5. Conversely, patients with slowly progressive type 1 diabetes mellitus develop an insulin‐dependent state from 6 months to several years after onset because of a gradual decrease in insulin secretory capacity 3.
The exact cause of type 1 diabetes is still not known 6. Usually, the body’s own immune system — which normally fights harmful bacteria and viruses — destroys the insulin-producing (islet) cells in the pancreas. Scientists do not know what causes this autoimmune reaction however different factors, such as genetics and some viruses, may cause type 1 diabetes. People who develop type 1 diabetes may have one or a number of genes which make type 1 diabetes more likely, then some sort of environmental trigger occurs to start the autoimmune reaction. Examples of triggers include an infection or a high level of stress. Triggers are not always easy to identify. Despite many studies, the risk factors of type 1 diabetes in children and adolescents are not fully understood and remain a big challenge for researchers 6.
Your doctor is likely to do a blood test to check you have auto-antibodies to confirm the diagnosis of type 1 diabetes.
Experts know that type 1 diabetes has nothing to do with lifestyle, although maintaining a healthy lifestyle is very important in helping to manage all types of diabetes, including type 1 diabetes.
Even after a lot of research, at this stage nothing can be done to prevent or cure type 1 diabetes.
Treatment is directed toward managing the amount of sugar in the blood using insulin injections several times a day or the use of an insulin pump, diet and lifestyle to prevent complications.
Insulin can’t be taken as a tablet as it would be digested down to its building blocks, amino acids, by the body’s normal digestive process.
Untreated type 1 diabetes results in diabetic ketoacidosis (DKA), which is a medical emergency.
If you are very newly diagnosed with type 1 diabetes there is often a ‘honeymoon period’ after you begin taking insulin. This is where your body’s pancreas still produces some insulin, so your insulin needs may vary for a while. Eventually your pancreas will stop producing insulin completely. Your doctor may check how much insulin you are producing by ordering a laboratory test of C-peptide.
Type 1 diabetes keypoints:
- Type 1 diabetes occurs when your pancreas does not produce insulin
- Type 1 diabetes represents around 10 per cent of all cases of diabetes and is one of the most common chronic childhood conditions
- In children, type 1 diabetes onset is usually abrupt and the symptoms obvious
- In adults, type 1 diabetes onset is slower
- Type 1 diabetes symptoms can include excessive thirst (polydipsia) and urination (polyuria), unexplained weight loss, weakness and fatigue and blurred vision
- Type 1 diabetes is managed with insulin injections several times a day or the use of an insulin pump
- Untreated type 1 diabetes results in diabetic ketoacidosis (DKA), a medical emergency.
How does insulin work?
Insulin is a hormone that comes from the pancreas, a gland situated behind and below the stomach. Insulin regulates how your body uses sugar in the following ways:
- Sugar in the bloodstream triggers the pancreas to secrete insulin.
- Insulin circulates in the bloodstream, enabling sugar to enter your cells.
- The amount of sugar in your bloodstream drops.
- In response to this drop, the pancreas releases less insulin.
Is there a cure for type 1 diabetes?
In type 1 diabetes, insulin-producing beta cells in the pancreas are destroyed by the immune system. This means you can’t make the insulin you need to live. To stop type 1 diabetes scientists need to disrupt the immune system’s attack on beta cells. Currently scientists are working on it. They’re aiming to develop and test treatments – called immunotherapies – that target the immune system to stop it destroying beta cells.
What happens if people with type 1 diabetes don’t receive insulin?
Without insulin glucose builds up in your body. The kidneys attempt to wash the excess glucose out through the urine, resulting in dehydration. The body burns its own fat reserves through a process called ketosis to supply energy which releases chemical substances in the blood called ketone bodies. Without ongoing injections of insulin, these ketone bodies accumulate in your body. The high glucose and ketone levels along with dehydration can be life threatening if it is not treated. This is a condition called diabetic ketoacidosis or DKA.
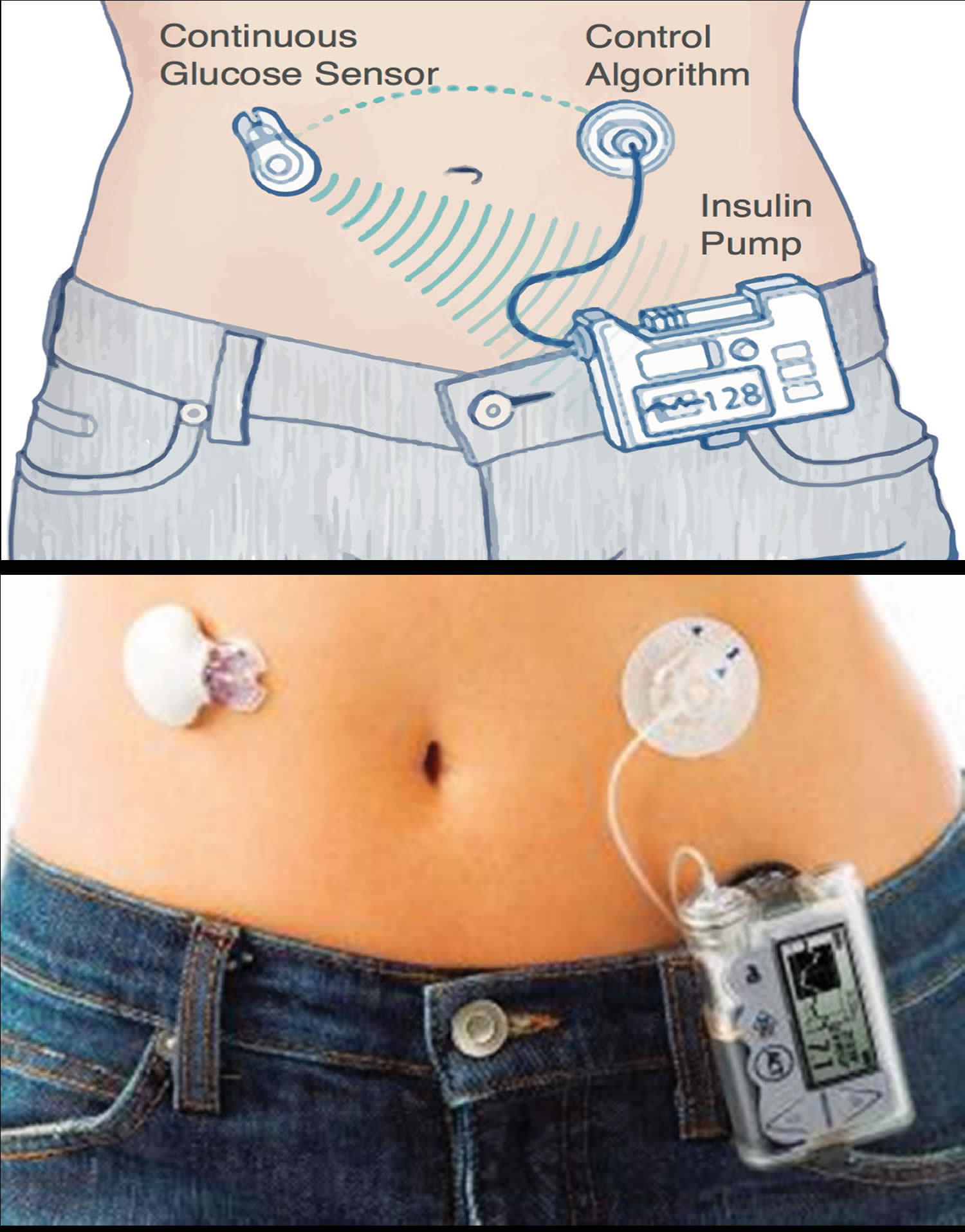
What is an insulin pump?
An insulin pump also known as continuous subcutaneous insulin infusion therapy (CSII) is a small device worn on the outside of your body that you program to deliver specific amounts of insulin throughout the day and when you eat to improve glucose control and/or reduce the risk of hypoglycemia (Figure 1) 7. A tube connects a reservoir of insulin to a catheter that’s inserted under the skin of your abdomen. There’s also a tubeless pump option that involves wearing a pod containing the insulin on your body combined with a tiny catheter that’s inserted under your skin.
Modern insulin pumps are portable and discrete (being similar in size to a mobile phone), and utilize smart technologies, such as Bluetooth transmission of capillary glucose level from glucometer to pump, and the ability to download pump data to a computer for analysis. However, contrary to the hopes of many individuals with type 1 diabetes, the pump is not a fully automatic ‘artificial pancreas’ and requires a high level of user involvement 8.
Figure 1. Insulin pump for type 1 diabetes
Who might use an insulin pump and why?
Insulin pump therapy can be considered for adults with type 1 diabetes who have problematic hypoglycemia (e.g., hypoglycemia unawareness or severe hypoglycemic episodes requiring third-party assistance) and/or inability to achieve target glycemic control despite best efforts 9. Before deciding on insulin pump or a continuous subcutaneous insulin infusion therapy as a treatment option, you should have tried multi-dose insulin (MDI) therapy with analogue insulins, undertake frequent self monitoring of capillary glucose and be proficient at carbohydrate counting (i.e, able to estimate the carbohydrate load of foods). Insulin pumps require a high level of self care, are more labor intensive than multi-dose insulin (MDI) (at least in the beginning) and have a greater potential for problems if used incorrectly; therefore, they are only suitable for motivated, appropriately educated individuals who engage with their diabetes healthcare team 8. The greatest improvement in glycemic control when changing from multi-dose insulin (MDI) to insulin pump is seen in those patients with the worst control pre-pump 10 but even individuals who do not see much change in their haemoglobin A1c show improved quality of life scores 7. In the UK, the use of insulin pump is subject to National Institute for Health and Clinical Excellence (NICE) guidance; current criteria do not include using insulin pump in people with type 2 diabetes 9.
What can go wrong with the insulin pump?
People using insulin pump for type 1 diabetes do not take any additional long-acting insulin. Therefore, any interruption to insulin delivery from the pump (e.g, if the tubing has an air block or the cannula is kinked or dislodged) will result in immediate insulin deficiency. Hyperglycemia (high blood sugar) and diabetic ketoacidosis (DKA) can develop quickly, unless the problem is identified and rectified, for example by re-siting the cannula, refilling the insulin reservoir, changing the tubing, or by starting alternative insulin, such as an intravenous infusion. Technical problems with the insulin pumps can occur; the pump manufacturing companies offer round-the-clock telephone support and are typically able to provide a replacement pump within 24 hour if required. All patients using insulin pumps are advised to retain a supply of their pre-pump insulin for use in an emergency situation, for example, in case of pump failure or damage 8.
What is a smart insulin pen?
A smart insulin pen is a reusable injector pen with an intuitive smartphone app that can help people with diabetes better manage insulin delivery. This smart system calculates and tracks doses and provides helpful reminders, alerts, and reports. They can come in the form of an add-on to your current insulin pen or a reusable form which uses prefilled cartridges instead of vials or disposable pens.
Many people with diabetes have a hard time correctly calculating insulin doses. This can result in insulin “stacking”—when you add more insulin while remaining insulin is still active from previous doses—which can lead to hypoglycemia (low blood sugar).
A smart insulin pen can:
- Calculate each dose based on current blood sugar level, carbohydrate amounts, meal size, active insulin, and settings prescribed by your doctor.
- Deliver accurate half-unit doses.
- Help prevent skipped or missed doses.
- Do the math for you when figuring out how to dose for a meal or correct a high blood sugar reading.
- Keep track of the time and amount of each dose, and remind you when it’s time for the next one.
- Notify you when your insulin has expired or exceeded its temperature range, so you can replace the cartridge.
- Send diabetes data to your health care team whenever needed.
- Work with your smart phone or watch and popular diabetes data tracking platforms.
The biggest challenges for many insulin pen (multiple daily injection) users are:
- Dose amount: How much to inject
- Dose timing: Shelf-life, temperature, and storage conditions
- Insulin quality: Shelf-life, temperature, and storage conditions
People with type 1 or type 2 diabetes on multiple daily injections of long or short acting insulin may benefit from a smart insulin pen. If you use an insulin pump, you may consider an insulin pen as a back-up delivery option. Your diabetes care team can help you find out if a smart insulin pen is a good choice for you and whether your insurance or Medicare will cover it. Some manufacturers offer co-pay assistance to make the device more affordable.
There are a few brands of smart insulin pens available now, and more are in development. You’ll need a prescription for both the pen and the insulin cartridges. Once available only from manufacturers, smart pens are now sold in pharmacies across the country.
According to most users, if you’ve used an insulin pen or pump before, you should have no trouble adapting to a smart pen. If new technology is sometimes hard for you to get used to, you can get help from your diabetes care team. They can train you on using it and make sure it’s set up properly for your needs.
Figure 2. Smart insulin pen
What are blood sugar levels?
Your blood sugar levels also known as blood glucose levels, are a measurement that show how much glucose (sugar) you have in your blood. Glucose is a sugar that you get from food and drink. Your blood sugar levels go up and down throughout the day and for people living with diabetes these changes are larger and happen more often than in people who don’t have diabetes.
Monitoring your blood sugar levels
You may measure your blood sugar levels or blood glucose levels regularly, up to six-eight times every day, in line with your doctor’s advice. Monitoring your blood glucose levels is important to make sure they’re as close as possible to your target range.
Your blood glucose level target range may vary depending on your personal circumstances. Your doctor, endocrinologist or diabetes educator can give the best advice for the range of blood glucose levels that’s safe for you.
Keeping your blood glucose levels in the optimum range requires a careful balance between what you eat, your physical activity and medication. Well-controlled blood glucose levels can help prevent both short- and long-term complications.
If your blood glucose levels are too high, it can result in hyperglycemia or diabetic ketoacidosis (DKA) . If too low, it can result in hypoglycemia. These can be difficult conditions to experience, so it’s important to know how to respond appropriately.
If experiencing Diabetes Ketoacidosis you may need to call emergency services if you have large ketones and not feeling well. Please follow any instructions that your diabetes health care team have given to you.
What happens when my blood sugar levels are too high?
If your blood sugar levels are slightly above your targets, there are usually no symptoms. But if your blood sugar levels become too high, you may experience some symptoms associated with a hyperglycemia (or hyper). High blood sugar levels are usually considered hyperglycemia when they are above 15mmol/L (270 mg/dL). Hyperglycemia can be caused by not enough insulin, eating too much carbohydrate food, sickness or infection, stress or reduced physical activity. If your blood sugar is persistently above 300 mg/dL (16.7 mmol/L), or if your urine ketones stays high in spite of taking correction doses of insulin, see your doctor or seek emergency care.
The blood sugar level at which symptoms begin to appear is different for everyone, but the common symptoms include passing more urine than normal, being very thirsty, having headaches and feeling tired and lethargic.
Symptoms of hyperglycemia:
- Excessive thirst
- Lethargy or fatigue
- Frequent urination
- Blurred vision
- Lack of concentration
- Change in behavior (usually irritable)
- Headache.
If you think you have hyperglycemia, check your blood sugar. If it is higher than your target range, you’ll likely need to administer a “correction.” A correction is an additional dose of insulin given to bring your blood sugar back to normal. High blood sugar levels don’t come down as quickly as they go up. Ask your doctor how long to wait until you recheck. If you use an insulin pump, random high blood sugar readings may mean you need to change the place where you put the pump on your body.
If you have a blood sugar reading above 240 mg/dL (13.3 mmol/L), test for ketones using a urine test stick. Don’t exercise if your blood sugar level is above 240 mg/dL or if ketones are present. If only a trace or small amounts of ketones are present, drink extra noncalorie fluids to flush out the ketones.
Over time, high blood glucose levels can lead to diabetes related complications. If your blood glucose levels are regularly above your target range, make an appointment to see your diabetes health team.
What happens when your blood sugar levels are too low?
Low blood sugar level also known as hypoglycemia, a ‘hypo’ or ‘low’, is when your blood glucose level is below 4 mmol/L (less than 72 mg/dL). Ask your doctor what’s considered a low blood sugar level for you. People taking insulin or certain types of diabetes medication are at risk of hypoglycemia. Hypos require immediate treatment with glucose to raise your blood glucose levels above 4mmol/L (above 72 mg/dL), otherwise your blood sugar levels will drop further. If this happens, you may experience a severe hypo and need emergency treatment.
Hypos can be caused by missing a meal, not eating enough carbohydrates for a given dose of insulin, unplanned physical activity, strenuous exercise, drinking alcohol, some medications or injecting too much insulin.
There are many different symptoms of a hypoglycemia, so it’s important that you are aware of the signs in case your blood sugar level gets too low. Test your blood sugar if you think your blood sugar levels are low. When in doubt, always test your blood sugar!
Symptoms of a hypo are:
- Weakness, trembling or shaking
- Sweating
- Light headedness/headache
- Lack of concentration or difficulty concentrating
- Behavior change
- Dizziness
- Tearfulness/crying
- Irritability or anxiety
- Tingling or numbness around the lips, tongue, cheek or fingers
- Hunger
- Looking pale (pallor)
- An irregular or fast heartbeat
- Feeling weak and having no energy (fatigue)
- Headache
Nighttime hypoglycemia may cause you to wake with sweat-soaked pajamas or a headache. Nighttime hypoglycemia sometimes might cause an unusually high blood sugar reading first thing in the morning.
If diabetic hypoglycemia isn’t treated, symptoms of hypoglycemia worsen and can include:
- Confusion, unusual behavior or both, such as the inability to complete routine tasks
- Loss of coordination
- Difficulty speaking or slurred speech
- Blurry or tunnel vision
- Inability to eat or drink
- Muscle weakness
- Drowsiness
Severe hypoglycemia may cause:
- Convulsions or seizures
- Unconsciousness
- Death, rarely
You can raise your blood sugar quickly by eating or drinking a simple sugar source, such as glucose tablets, hard candy or fruit juice. Tell family and friends what symptoms to look for and what to do if you’re not able to treat the condition yourself.
If a blood glucose meter isn’t readily available, treat for low blood sugar anyway if you have symptoms of hypoglycemia, and then test as soon as possible.
Inform people you trust about hypoglycemia. If others know what symptoms to look for, they might be able to alert you to early symptoms. It’s important that family members and close friends know where you keep glucagon and how to give it so that a potentially serious situation can be easier to safely manage. Glucagon is a hormone that stimulates the release of sugar into the blood.
Here’s some emergency information to give to others. If you’re with someone who is not responding (loses consciousness) or can’t swallow due to low blood sugar:
- Don’t inject insulin, as this will cause blood sugar levels to drop even further
- Don’t give fluids or food, because these could cause choking
- Give glucagon by injection or a nasal spray
- Call your local emergency services number in your area for immediate treatment if glucagon isn’t on hand, you don’t know how to use it or the person isn’t responding
Hypoglycemia unawareness
Some people may lose the ability to sense that their blood sugar levels are getting low. This is called hypoglycemia unawareness. The body no longer reacts to a low blood sugar level with symptoms such as lightheadedness or headaches. The more you experience low blood sugar, the more likely you are to develop hypoglycemia unawareness.
If you can avoid having a hypoglycemic episode for several weeks, you may start to become more aware of coming lows. Sometimes increasing the blood sugar target (for example, from 80 to 120 mg/DL to 100 to 140 mg/DL) at least for a short time can also help improve low blood sugar awareness.
Hypoglycemia treatment
Hypoglycemia is treated by having quick-acting glucose, such as Lucozade, 6 to 7 jellybeans, 3 teaspoons of honey, 100mls of full-strength soft drink or 150-200mls of fruit juice.
Wait 15 minutes, re-check your blood glucose levels to see if your blood glucose level has risen above 4mmol/L (above 72 mg/dL). If your blood glucose level is still below 4mmol/L (less than 72 mg/dL), repeat Step 1 by having another quick-acting glucose.
If your blood glucose level has risen above 4mmol/L, eat a snack or meal with longer acting carbohydrate such as a slice of bread, 1 glass of milk, 1 piece of fruit, 2-3 pieces of dried apricots, figs or other dried fruit OR 1 tub of natural low-fat yogurt.
It’s important to tell your family, friends and colleagues about hypos, how to recognize the symptoms when you’re hypoglycemic and how to treat it. Make sure they know to call your local emergency services number if you become unconscious, drowsy or unable to swallow, stating that it is a diabetes emergency.
It is important that your support person does not try to feed you; instead they should lay you on your side and check that your airway is clear. Then they should wait with you until the ambulance arrives. It is recommended that you wear a medical alert ID. This will help emergency services personnel to act appropriately and quickly.
What happens if I don’t treat hypoglycemia?
If not treated quickly, your blood glucose level can continue to drop, which may result in the brain not getting enough glucose. This can cause unconsciousness or fitting.
If a person with diabetes is unconscious, drowsy or unable to swallow. THIS IS AN EMERGENCY.
Do not give them any food or drink by mouth, treat as follows:
- Place them on their side making sure their airway is clear
- Give an injection of Glucagon if available and you are trained to give it
- Phone for an ambulance stating the person is unconscious AND that the person has diabetes
- Wait with them until the ambulance arrives.
What is diabetic ketoacidosis?
Diabetic ketoacidosis or DKA is a life-threatening emergency and can occur if you have type 1 diabetes or in some circumstances when you have type 2 diabetes. Diabetic ketoacidosis occurs when your body starts breaking down fat at a rate that is much too fast. The fat is broken down by the liver into a fuel called ketones. Ketones are normally produced by the liver when the body breaks down fat after it has been a long time since your last meal (e.g., during fasting). These ketones are normally used by the muscles and the heart. When ketones are produced too quickly and build up in your blood, they can be toxic by making the blood acidic which can be dangerous if not treated promptly. This condition is known as ketoacidosis or diabetic ketoacidosis (DKA).
If you have diabetes, learn to recognize the signs and symptoms of diabetic ketoacidosis (DKA). Know when to test for ketones, such as when you are sick. If you use an insulin pump, check often to see that insulin is flowing through the tubing. Make sure the tube is not blocked, kinked or disconnected from the pump.
It is important to discuss ketoacidosis with your health care team to find out if you are at risk and develop a ketoacidosis management plan. If diabetic ketoacidosis (DKA) is not treated, it can lead to severe illness or death.
Diabetic ketoacidosis happens when the signal from insulin in the body is so low that:
- Glucose (blood sugar) can’t go into cells to be used as a fuel source.
- The liver makes a huge amount of blood sugar.
- Fat is broken down too rapidly for the body to process.
Diabetic ketoacidosis (DKA) is sometimes the first sign of type 1 diabetes in people who have not yet been diagnosed. Diabetic ketoacidosis (DKA) can also occur in someone who has already been diagnosed with type 1 diabetes. Infection, injury, a serious illness, missing doses of insulin shots, or the stress of surgery can lead to diabetic ketoacidosis (DKA) in people with type 1 diabetes.
In a person with type 1 diabetes, a ketone check is necessary when:
- You have a blood glucose meter reading of 15mmol/L (270mg/dL) or higher
- You are feeling unwell, even if your blood glucose levels are within your target range.
The ketone test is usually done using a urine sample or a blood sample. Ketone testing may be used in type 1 diabetes to screen for early ketoacidosis.
People with type 2 diabetes can also develop diabetic ketoacidosis (DKA), but it is less common and less severe. It is usually triggered by prolonged uncontrolled blood sugar, missing doses of medicines, or a severe illness or infection.
Common symptoms of diabetic ketoacidosis (DKA) can include:
- Decreased alertness
- Deep, rapid breathing or shortness of breath
- Dehydration
- Dry skin and mouth
- Flushed face
- Frequent urination or thirst that lasts for a day or more
- A sweet, fruity smell on your breath
- Headache
- Muscle stiffness or aches
- Weakness
- Nausea and vomiting
- Stomach pain
- Confusion
- Coma
Health problems that may result from diabetic ketoacidosis (DKA) include any of the following:
- Fluid buildup in the brain (cerebral edema)
- Heart stops working (cardiac arrest)
- Kidney failure
The goal of diabetic ketoacidosis (DKA) treatment is to correct the high blood sugar level with insulin. Another goal is to replace fluids lost through urination, loss of appetite, and vomiting if you have these symptoms.
If you have diabetes, it is likely your diabetes health team told you how to spot the warning signs of diabetic ketoacidosis (DKA). If you think you have diabetic ketoacidosis (DKA), check your urine for excess ketones with an over-the-counter ketones test kit. Some glucose meters can also measure blood ketones. If ketones are present, call your doctor or diabetes health team right away. Do not delay. Follow any instructions you are given.
It is likely that you will need to go to the hospital. There, you will receive insulin, fluids, and other treatment for diabetic ketoacidosis (DKA). Then your doctors will also search for and treat the cause of diabetic ketoacidosis (DKA), such as an infection. Most people respond to treatment within 24 hours. Sometimes, it takes longer to recover.
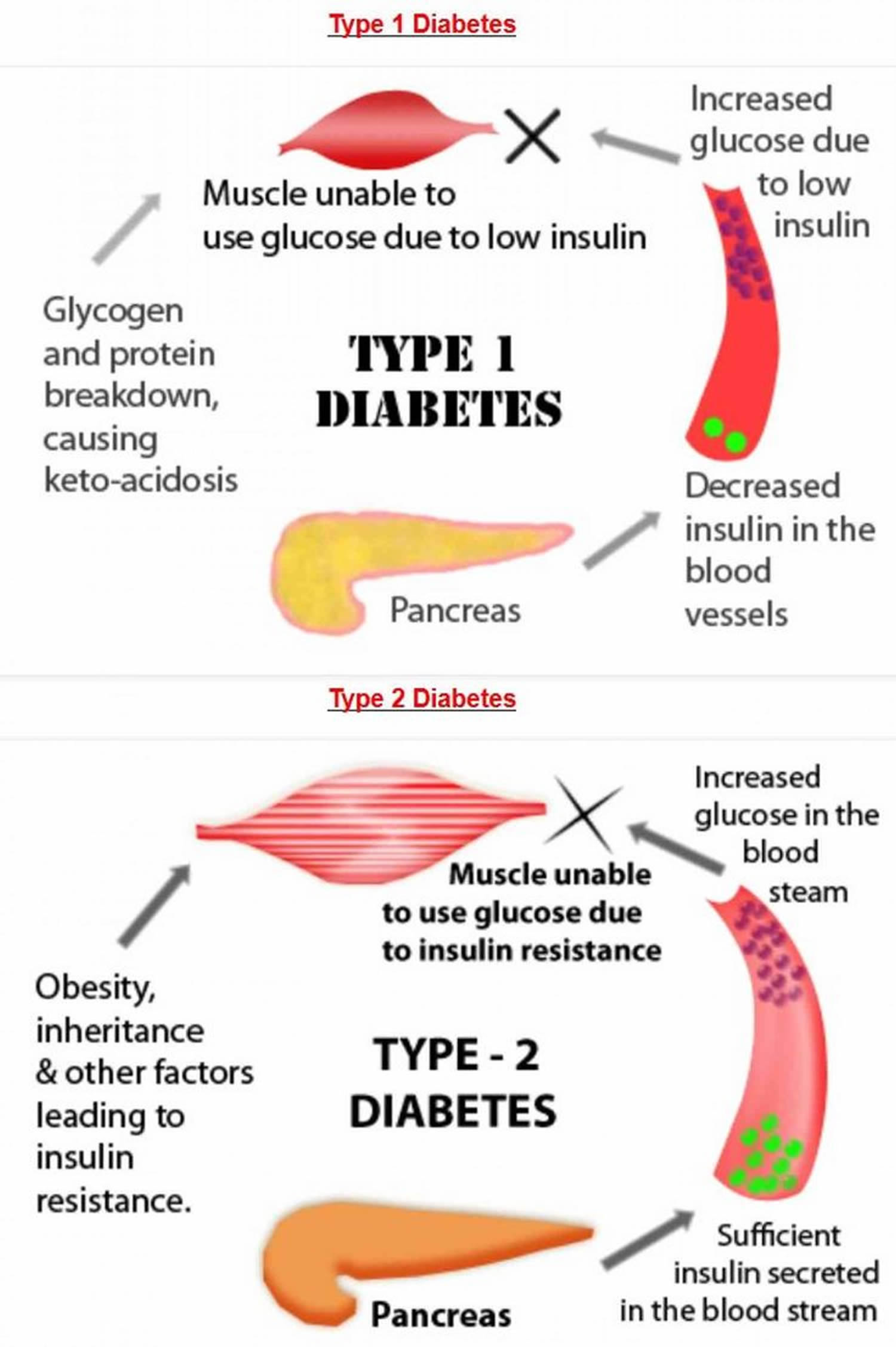
What is the difference between type 1 and type 2 diabetes?
The main difference between the type 1 and type 2 diabetes is that type 1 diabetes is a genetic condition that often shows up early in life, and type 2 is mainly lifestyle-related and develops over time. Type 1 diabetes is an auto-immune disease where your immune system is attacking and destroying the insulin-producing cells in your pancreas. In type 1 diabetes, people produce little or no insulin, as the insulin-producing cells have been destroyed by the body’s immune system. Approximately 5-10% of the people who have diabetes have type 1 diabetes. Currently, no one knows how to prevent type 1 diabetes.
In type 2 diabetes, the body may make enough insulin early in the disease, but doesn’t respond to it effectively. As type 2 diabetes progresses, the pancreas gradually loses the ability to produce enough insulin. Type 2 diabetes is associated with inherited factors and lifestyle risk factors such as being overweight or obese, poor diet, and insufficient physical activity. Type 2 diabetes most often develops in people over age 45, but more and more children, teens, and young adults are also developing it because the increase in the number of children with obesity.
Type 1 diabetes affects 8% of everyone with diabetes. While type 2 diabetes affects about 90% of people with diabetes.
Although type 1 and type 2 diabetes both have things in common, there are lots of differences. Like what causes them, who they affect, and how you should manage them.
A big difference between the two is that type 1 diabetes isn’t affected by your lifestyle. Or your weight. That means you can’t affect your risk of developing type 1 diabetes by lifestyle changes.
It’s different for type 2 diabetes. Scientists know some things put you at more risk:
- If you’re overweight or obese. Being overweight or obese is a main risk.
- Fat distribution. Storing fat mainly in your abdomen (waist size is too large) — rather than your hips and thighs — indicates a greater risk. Your risk of type 2 diabetes rises if you’re a man with a waist circumference above 40 inches (101.6 centimeters) or a woman with a measurement above 35 inches (88.9 centimeters).
- How to measure your waist: Find the top of your hip bone and the bottom of your ribcage. In the middle of these two points is where you need to measure. For many people, the belly button is a good guide, but this might not be the case for you, so it’s best to find that midpoint between your ribcage and hip. If you’re still not sure, watch the video below.
- What is a healthy waist size? This all depends on your gender and ethnicity. For a healthy measurement you need to aim to be less than:
- 80 cm (31.5 in) for all women
- 94 cm (37 in) for most men
- 90cm (35in) for South Asian men. This is because you have a higher risk of type 2 diabetes if you are of black or South Asian background.
- Inactivity. The less active you are, the greater your risk. Physical activity helps control your weight, uses up glucose as energy and makes your cells more sensitive to insulin.
- Family history. The risk of type 2 diabetes increases if your parent, brother or sister has type 2 diabetes.
- Race and ethnicity. Although it’s unclear why, people of certain races and ethnicities — including African Caribbean, Black African, Hispanic, Native American and Asian people (Indian, Pakistani, Bangladeshi or Chinese), and Pacific Islanders — are more likely to develop type 2 diabetes than white people are.
- Blood lipid levels. An increased risk is associated with low levels of high-density lipoprotein (HDL) cholesterol — the “good” cholesterol — and high levels of triglycerides.
- Age. You’re more at risk if you’re white and over 40, or over 25 if you’re African Caribbean, Black African, or South Asian (Indian, Pakistani or Bangladeshi).
- Medical history. For example if you have a history of high blood pressure, heart attack or strokes, gestational diabetes or severe mental illness.
- Prediabetes. Prediabetes is a condition in which your blood sugar level is higher than normal, but not high enough to be classified as diabetes. Left untreated, prediabetes often progresses to type 2 diabetes.
- Pregnancy-related risks. Your risk of developing type 2 diabetes increases if you developed gestational diabetes when you were pregnant or if you gave birth to a baby weighing more than 9 pounds (4 kilograms).
- Polycystic ovary syndrome (PCOS). Having polycystic ovary syndrome — a common condition characterized by irregular menstrual periods, excess hair growth and obesity — increases the risk of diabetes.
- Smoking. Smoking is associated with a higher risk of type 2 diabetes, and also increases the risk of other health conditions such as heart disease and cancer.
- Areas of darkened skin, usually in the armpits and neck. This condition, called acanthosis nigricans. This condition often indicates insulin resistance. Acanthosis nigricans is most common in those who are overweight, have darker skin, and have diabetes or pre-diabetic conditions. Acanthosis nigricans is not contagious. It is not harmful. Acanthosis nigricans is a warning sign of a health problem that requires medical attention.
Scientists also know that there are things you can do to reduce your risk of developing type 2 diabetes. Things like eating healthily, being active and maintaining a healthy weight can help you to prevent type 2 diabetes.
Some people still get confused between type 1 and type 2 diabetes. Below is a guide to some of the main differences between type 1 and type 2 diabetes. The main thing to remember is that both are as serious as each other. Having high blood glucose (or sugar) levels can lead to serious health complications, no matter whether you have type 1 or type 2 diabetes. So if you have either condition, you need to take the right steps to manage it.
Figure 3. Differences between type 1 and type 2 diabetes
Table 1. Type 1 and type 2 diabetes differences
| Type 1 diabetes | Type 2 diabetes | |
|---|---|---|
| What is happening? | Your body attacks the cells in your pancreas which means it cannot make any insulin. | Your body is unable to make enough insulin or the insulin you do make doesn’t work properly. |
| Risk factors | Scientists don’t currently know what causes type 1 diabetes. | Scientists know some things can put you at risk of having type 2 like weight and ethnicity. |
| Symptoms | The symptoms for type 1 appear more quickly. | Type 2 symptoms can be easier to miss because they appear more slowly. |
| Management | Type 1 is managed by taking insulin to control your blood sugar. | You can manage type 2 diabetes in more ways than type 1. These include through medication, exercise and diet. People with type 2 can also be prescribed insulin. |
| Cure and Prevention | Currently there is no cure for type 1 but research continues. | Type 2 cannot be cured but there is evidence to say in many cases it can be prevented and put into remission. If you have obesity or overweight, your type 2 diabetes is more likely to go into remission if you lose a substantial amount of weight – 15kg (or 2 stone 5lbs) – as quickly and safely as possible following diagnosis. Type 2 diabetes remission is when your blood sugar levels are below the diabetes range and you don’t need to take diabetes medication anymore. Remission is when your HbA1c — a measure of long-term blood glucose levels — remains below 48mmol/mol or 6.5% for at least three months, without diabetes medication 11. |
Type 1 diabetes pregnancy
Preexisting diabetes also called pregestational diabetes means you have diabetes before you get pregnant. This is different from gestational diabetes, which is a kind of diabetes that some women get during pregnancy. In the United States, about 1 to 2 percent of pregnant women have preexisting diabetes. The number of women with diabetes during pregnancy has increased in recent years. The risk of complications during pregnancy is higher for people with type 1 diabetes. High blood sugar can be harmful to your baby during the first few weeks of pregnancy when his brain, heart, kidneys and lungs begin to form. There is a chance that some of the potential complications of diabetes, like eye disease (diabetic retinopathy), kidney disease (diabetic nephropathy) and diabetic ketoacidosis (DKA), may develop while you are pregnant. Your doctors will keep an eye on this. If you are pregnant or planning a pregnancy, visit an ophthalmologist during each trimester of your pregnancy, one year postpartum or as advised. There is also a risk of developing pregnancy-induced high blood pressure or preeclampsia, a condition involving high blood pressure during pregnancy, which can cause problems for the baby.
Experts recommend that you see your doctor before you get pregnant. Your A1C readings should be less than 6.5% before you try to get pregnant. The risk of diseases present at birth (congenital diseases), birth defects, miscarriage and stillbirth is higher for people with type 1 diabetes. The risk is also higher when your diabetes is poorly controlled during the first 6 to 8 weeks of pregnancy. Careful management of your diabetes during pregnancy can lower your risk of complications. And most women with diabetes have a healthy baby.
If you have type 1 or type 2 diabetes and are planning a family, you should plan your pregnancy as much as possible. Controlling your blood sugars before conception and throughout pregnancy gives you the best chance of having a trouble-free pregnancy and birth and a healthy baby.
Having diabetes means that you and your baby are more at risk of serious health complications during pregnancy and childbirth. The good news is that by planning ahead and getting support from your doctor and diabetes team, you can really reduce the risks involved. So you’re more likely to enjoy a healthy pregnancy and give birth to a healthy baby.
If you have diabetes and your pregnancy is unplanned, there’s still plenty you can do to give your baby the best start in life.
Signs of trouble
Regularly monitoring your blood sugar levels is important to avoid severe complications. Also, be aware of signs and symptoms that may suggest irregular blood sugar levels and the need for immediate care:
High blood sugar (hyperglycemia). Eating certain foods or too much food, being sick, or not taking medications at the right time can cause high blood sugar. Signs and symptoms include:
- Frequent urination
- Increased thirst
- Dry mouth
- Blurred vision
- Fatigue
- Headache
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS). This life-threatening condition includes a blood sugar reading higher than 600 mg/dL (33.3 mmol/L). Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) may be more likely if you have an infection, are not taking medicines as prescribed, or take certain steroids or drugs that cause frequent urination. Signs and symptoms of hyperglycemic hyperosmolar nonketotic syndrome (HHNS) include:
- Dry mouth
- Extreme thirst
- Drowsiness
- Confusion
- Dark urine
- Seizures
Diabetic ketoacidosis. Diabetic ketoacidosis occurs when a lack of insulin results in the body breaking down fat for fuel rather than sugar. This results in a buildup of acids called ketones in the bloodstream. Triggers of diabetic ketoacidosis include certain illnesses, pregnancy, trauma and medications — including the diabetes medications called SGLT2 inhibitors.
Although diabetic ketoacidosis is usually less severe in type 2 diabetes, the toxicity of the acids can be life-threatening. In addition to the signs and symptoms of low blood sugar (hypoglycemia), such as frequent urination and increased thirst, ketoacidosis may result in:
- Nausea
- Vomiting
- Abdominal pain
- Shortness of breath
- Fruity-smelling breath
Low blood sugar (hypoglycemia). If your blood sugar level drops below your target range, it’s known as low blood sugar (hypoglycemia). Your blood sugar level can drop for many reasons, including skipping a meal, unintentionally taking more medication than usual or being more physical activity than usual. Signs and symptoms include:
- Sweating
- Shakiness
- Weakness
- Hunger
- Irritability
- Dizziness
- Headache
- Blurred vision
- Heart palpitations
- Slurred speech
- Drowsiness
- Confusion
If you have signs or symptoms of low blood sugar, drink or eat something that will quickly raise your blood sugar level — fruit juice, glucose tablets, hard candy or another source of sugar. Retest your blood in 15 minutes. If levels are not at your target, repeat the sugar intake. Eat a meal after levels return to normal.
If you lose consciousness, you will need to be given an emergency injection of glucagon, a hormone that stimulates the release of sugar into the blood.
Type 1 diabetes causes
The exact cause of type 1 diabetes is still not known 6. Usually, the body’s own immune system — which normally fights harmful bacteria and viruses — destroys the insulin-producing (islet) cells in the pancreas. Scientists do not know what causes this autoimmune reaction however different factors, such as genetics and some viruses, may cause type 1 diabetes 12, 13, 14, 15, 16, 17. Previous studies have shown that genetic and environmental factors have a significant impact on the risk of developing type 1 diabetes 18, 19. People who develop type 1 diabetes may have one or a number of genes which make type 1 diabetes more likely, then some sort of environmental trigger occurs to start the autoimmune reaction 20. Examples of triggers include an infection or a high level of stress. Triggers are not always easy to identify. The risk of developing type 1 diabetes under the age of 20 is 1:300 in families without genetic burden, 1:50 in the case of a child whose mother has type 1 diabetes, and 1:15 in the case of type 1 diabetes in the child’s father. A family history of diabetes is an important indicator of the risk of the disease in children because it shows the coexistence of pro-diabetogenic factors, both genetic and environmental 21, 22. Despite many studies, the risk factors of type 1 diabetes in children and adolescents are not fully understood and remain a big challenge for researchers 6.
In the last few years, new factors have emerged that were not previously considered possible risk factors for the development of type 1 diabetes, such as particulate matter contamination or the microbiome 23, 24.
Your doctor is likely to do a blood test to check you have auto-antibodies to confirm the diagnosis of type 1 diabetes.
Type 1 diabetes genetic
The genes and the mode of inheritance for type 1 diabetes is complex and still not fully understood 20. A family history of diabetes is an important indicator of the risk of the disease in children because it shows the coexistence of pro-diabetogenic factors, both genetic and environmental 21, 22. The main genes predisposing to the development of type 1 diabetes are located within the genes of the HLA system on chromosome 6, although other genes may also be involved 25, 26. The genetic factor plays a significant role in the development of type 1 diabetes, which has been proven by studies on twins. In identical twins, the risk of diabetes is 50% compared to fraternal twins, where the risk ranges from 5 to 13% 27, 28. A study by Siewko et al. 29 showed that autoimmune markers were detected in the serum in more than 30% of first-degree relatives (parents, brothers and sisters) of diabetic patients. It was also revealed that these people, despite normal glucose tolerance, significantly decreased beta-cell secretory reserve and decreased insulin sensitivity 29.
The genetic predisposition to develop type 1 diabetes is associated with the HLA gene complex located in chromosome 6p21, which has been known since the 1970s 30. The associated HLA DR3 and DR4 haplotypes cause severe susceptibility 31, 32. In 90% of the Caucasian population, diabetes is strongly associated with DR3 antigens (DRB1 * 03: 01-DQB1 * 02: 01) and DR4 (DRB1 * 04: 01-DQB1 * 03: 02). In contrast, in Japan and most other East Asian populations, type 1 diabetes is associated with DR4 haplotypes (DRB1 * 04: haplotypes 05-DQB1 * 04: 01) and DR9 (DRB1 * 09: 01-DQB1 * 03: 03) 33. In Brazil, the most common haplotype is HLA-DRB1 * 03: 01 ~ DQA1 * 05: 01 g ~ DQB1 * 02: 01 32.
Analysis of the human genome by a mapping technique also identified other loci attributed to the presence of type 1 diabetes. One such site is the region associated with the insulin gene, which is located on the short arm of chromosome 11 (11p15.5) and is responsible for 10% inheritance of type 1 diabetes 34. So far, the risk of type 1 diabetes has been associated with nearly 30 different gene loci. However, few of the loci studied have been linked to specific genes 34. Research on the connection of genes with a genetic predisposition is still ongoing. Despite many years of research, the actual role of most of these genes in the pathogenesis of type 1 diabetes remains unclear 35, 36, 37. On the other hand, more and more studies indicate the role of environmental factors in the development and/or progression of type 1 diabetes 38, 24, 39, 40, 41, 38.
Risk factors for developing type 1 diabetes
Some factors that can raise your risk for type 1 diabetes include:
- Family history. Anyone with a parent or sibling with type 1 diabetes has a slightly higher risk of developing the condition.
- Genetics. Having certain genes increases the risk of developing type 1 diabetes.
- Geography. The number of people who have type 1 diabetes tends to be higher as you travel away from the equator.
- Age. Type 1 diabetes can appear at any age, but it appears at two noticeable peaks. The first peak occurs in children between 4 and 7 years old. The second is in children between 10 and 14 years old.
Type 1 diabetes signs and symptoms
Type 1 diabetes symptoms can appear suddenly and may include:
- Being excessively thirsty (polydipsia)
- Urinating a lot (polyuria)
- Bed-wetting in children who have never wet the bed during the night (enuresis)
- Always feeling hungry (polyphagia)
- Losing weight without trying
- Feeling irritable or having other mood changes
- Feeling tired and weak (fatigue)
- Having blurry vision
- Having cuts that heal slowly
- Itching, skin infections
- Headaches
- Feeling dizzy
- Leg cramps
These symptoms may occur suddenly. See your doctor if you notice any of the above symptoms in you or your child.
Untreated type 1 diabetes results in diabetic ketoacidosis (DKA), a medical emergency.
Type 1 diabetes complications
Over time, type 1 diabetes complications can affect major organs in the body. These organs include your heart, blood vessels, nerves, eyes and kidneys. Having a normal blood sugar level can lower your risk of many type 1 diabetes complications. Common diabetes health complications include heart disease, chronic kidney disease, nerve damage, and other problems with feet, oral health, vision, hearing, and mental health 42. Type 1 diabetes complications can lead to disabilities or even threaten your life.
- Heart and blood vessel disease. Diabetes increases the risk of some problems with the heart and blood vessels. These include coronary artery disease with chest pain (angina), heart attack, stroke, narrowing of the arteries (atherosclerosis) and high blood pressure. If you have diabetes, you’re more likely to have heart disease and stroke.
- Nerve damage (diabetic neuropathy). Too much sugar in the blood can injure the walls of the tiny blood vessels (capillaries) that feed the nerves. This is especially true in the legs. This can cause tingling, numbness, burning or pain. This usually begins at the tips of the toes or fingers and spreads upward. Poorly controlled blood sugar could cause you to lose all sense of feeling in the affected limbs over time. Many patients who develop neuropathy need to have regular foot exams to prevent infection from wounds that go unnoticed. Damage to the nerves that affect the digestive system can cause problems with nausea, vomiting, diarrhea or constipation. For men, erectile dysfunction may be an issue.
- Kidney damage (diabetic nephropathy). The kidneys have millions of tiny blood vessel clusters (glomeruli) that keep waste from entering the blood. Diabetes can damage this system. Severe damage can lead to kidney failure or end-stage kidney disease (ESRD) that can’t be reversed. End-stage kidney disease needs to be treated with mechanical filtering of the kidneys (dialysis) or a kidney transplant 43. If the albuminuria persists in the range of 30 to 300 mg/day (microalbuminuria), it seems to be a predictable earliest marker for the onset of diabetic neuropathy. Once macroalbuminuria (greater than 300 mg/24 hr) sets in, the progression to end-stage renal disease (ESRD) hastens up. The random spot urine specimen for measurement of the albumin-to-creatinine ratio is a quick, easy, predictable method that is the most widely used and preferred method to detect microalbuminuria. Two of three tests, done over a six month showing a persistent level greater than 30 mcg/mg creatinine, confirms the diagnosis of microalbuminuria.
- Eye damage. Diabetes can damage the blood vessels in the retina (part of the eye that senses light) (diabetic retinopathy). This could cause blindness. Diabetes also increases the risk of other serious vision conditions, such as cataracts and glaucoma. The duration of diabetes is the most crucial risk factor for the development of diabetic retinopathy. In people with type 1 diabetes, it typically sets in about 5 years after disease onset. Hence it is recommended to start the yearly retinal exams in these patients about five years after diagnosis. Diabetes is also a common cause of blindness in adults aged 20 to 74 years in the United States. Diabetic retinopathy contributes to 12,000 to 24,000 new cases of blindness annually, and treatments generally consist of laser surgery and glucose control 43.
- Foot damage. Nerve damage in the feet or poor blood flow to the feet increases the risk of some foot complications. Left untreated, cuts and blisters can become serious infections. These infections may need to be treated with toe, foot or leg removal (amputation). Diabetes is the leading cause of limb amputations in the United States; this is primarily due to vasculopathy and neuropathy associated with diabetes 43.
- Skin and mouth conditions. Diabetes may leave you more prone to infections of the skin and mouth. These include bacterial and fungal infections. Gum disease and dry mouth also are more likely.
- Pregnancy complications. High blood sugar levels can be dangerous for both the parent and the baby. The risk of miscarriage, stillbirth and birth defects increases when diabetes isn’t well-controlled. For the parent, diabetes increases the risk of diabetic ketoacidosis, diabetic eye problems (retinopathy), pregnancy-induced high blood pressure and preeclampsia.
- Hearing impairment. Hearing problems are more common in people with diabetes.
- Depression. Depression symptoms are common in people with type 1 and type 2 diabetes.
Type 1 diabetes prevention
At the present time, there’s no known way to prevent type 1 diabetes. But researchers are working on preventing the disease or further damage of the pancreatic islet cells in people who are newly diagnosed. Ask your doctor if you might be eligible for one of these clinical trials. It is important to carefully weigh the risks and benefits of any treatment available in a trial.
Type 1 diabetes diagnosis
If your doctor thinks you may have type 1 diabetes, you will probably need to have a blood test.
You may be asked to take a fasting blood glucose test, where you don’t eat for 8 hours before the test, or a random blood glucose test, where you don’t need to fast.
You may also need to have an oral glucose tolerance test (OGTT) where you have blood glucose tests after you drink a sugary drink.
You may also be asked to have your urine tested for ketones.
If you’re diagnosed with diabetes, your doctor may also run blood tests to check for autoantibodies that are common in type 1 diabetes. Autoantibodies are antibodies that attack your healthy tissues and cells by mistake. The tests help your doctor decide between type 1 and type 2 diabetes when the diagnosis isn’t certain. The presence of ketones — byproducts from the breakdown of fat — in your urine also suggests type 1 diabetes, rather than type 2.
Because type 1 diabetes can run in families, your health care professional can test your family members for autoantibodies. Type 1 diabetes TrialNet, an international research network, also offers autoantibody testing to family members of people diagnosed with the disease (https://www.trialnet.org). The presence of autoantibodies, even without diabetes symptoms, means the family member is more likely to develop type 1 diabetes. If you have a brother or sister, child, or parent with type 1 diabetes, you may want to get an autoantibody test. People age 20 or younger who have a cousin, aunt, uncle, niece, nephew, grandparent, or half-sibling with type 1 diabetes also may want to get tested.
A1C or HbA1C test
Type 1 diabetes is usually diagnosed using the glycated hemoglobin (A1C or HbA1C) test. The A1C test measures your average blood glucose for the past two to three months. Results are interpreted as follows 44:
- Below 5.7% is normal.
- 5.7% to 6.4% is diagnosed as prediabetes.
- 6.5% or higher on two separate tests indicates diabetes.
If the A1C test isn’t available, or if you have certain conditions — such as if you’re pregnant or have an uncommon form of hemoglobin (known as a hemoglobin variant) — that can make the A1C test inaccurate, your doctor may use the following tests to diagnose diabetes:
Random blood sugar test
Random blood sugar test also called casual plasma glucose test is a blood check at any time of the day when you have severe diabetes symptoms.
- Diabetes is diagnosed at blood glucose of greater than or equal to 11.1 mmol/L (200 mg/dL)
Blood sugar values are expressed in milligrams of sugar per deciliter (mg/dL) or millimoles of sugar per liter (mmol/L) of blood. Regardless of when you last ate, a level of 200 mg/dL (11.1 mmol/L) or higher suggests diabetes, especially if you also have signs and symptoms of diabetes, such as frequent urination and extreme thirst.
Fasting blood sugar test
A blood sample is taken after an overnight fast. Results are interpreted as follows:
- Less than 100 mg/dL (5.6 mmol/L) is normal.
- 100 to 125 mg/dL (5.6 to 6.9 mmol/L) is diagnosed as prediabetes.
- 126 mg/dL (7 mmol/L) or higher on two separate tests is diagnosed as diabetes.
Oral glucose tolerance test (OGTT)
Oral glucose tolerance test is less commonly used than the others, except during pregnancy. You’ll need to fast overnight and then drink a sugary liquid at the doctor’s office. Blood sugar levels are tested periodically for the next two hours. Results are interpreted as follows:
- Less than 140 mg/dL (7.8 mmol/L) is normal.
- 140 to 199 mg/dL (7.8 mmol/L and 11.0 mmol/L) is diagnosed as prediabetes.
- 200 mg/dL (11.1 mmol/L) or higher after two hours suggests diabetes.
Type 1 diabetes treatment
Treatment for type 1 diabetes includes:
- Insulin. Anyone who has type 1 diabetes needs insulin therapy throughout their life.
- Pramlintide. Some people who have trouble reaching their blood glucose targets with insulin alone also might need to take another type of diabetes medicine that works with insulin, such as pramlintide. Pramlintide, given by injection, helps keep blood glucose levels from going too high after eating. However, few people with type 1 diabetes take pramlintide. Another diabetes medicine, metformin (a medicine most commonly used in type 2 diabetes), may help decrease the amount of insulin you need to take, but more studies are needed to confirm this. Reseachers are also studying other diabetes pills that people with type 1 diabetes might take along with insulin.
- Counting carbohydrates, fats and protein
- Monitoring blood sugar often
- Eating healthy foods
- Exercising regularly and keeping a healthy weight
If you or your child is diagnosed with type 1 diabetes, you or your child will require a brief hospital stay while your blood sugars are bring controlled and a treatment plan is created. You or your child will need to take daily insulin injections to replace the insulin your body no longer makes on its own. A healthy diet and regular exercise also help control blood sugar levels. The goal is to keep the blood sugar level as close to normal as possible to delay or prevent complications. Generally, the goal is to keep the daytime blood sugar levels before meals between 80 and 130 mg/dL (4.44 to 7.2 mmol/L). After-meal numbers should be no higher than 180 mg/dL (10 mmol/L) two hours after eating.
Type 1 diabetes insulin
There are many types of insulin for type 1 diabetes and they include:
- Rapid-acting insulin. This type of insulin starts working within 15 minutes. It reaches peak effect at 60 minutes and lasts about 4 hours. This type is often used 15 to 20 minutes before meals. Examples are glulisine (Apidra), lispro (Humalog, Admelog and Lyumjev) and aspart (Novolog and FiAsp).
- Short-acting insulin also called regular insulin, this type starts working around 30 minutes after injection. It reaches peak effect at 90 to 120 minutes and lasts about 4 to 6 hours. Examples are Humulin R, Novolin R and Afrezza.
- Intermediate-acting insulin. Also called NPH insulin, this type of insulin starts working in about 1 to 3 hours. It reaches peak effect at 4 to 8 hours and lasts 12 to 24 hours. Examples are insulin NPH (Novolin N, Humulin N).
- Long-acting insulin and ultra-long-acting insulin. This type of insulin may provide coverage for as long as 14 to 40 hours. Examples are glargine (Lantus, Toujeo Solostar, Basaglar), detemir (Levemir) and degludec (Tresiba).
- Premixed insulin. Premixed insulin combines intermediate-acting insulin and short-acting insulin. Usually taken 10 to 30 minutes before breakfast and dinner. This type of insulin starts working in about 5 to 60 minutes. Its peak time varies depending on the mixture and lasts 10 to 16 hours.
Footnote:
- Onset is how quickly insulin lowers your blood sugar.
- Peak Time is when insulin is at maximum strength.
- Duration is how long insulin works to lower your blood sugar.
You’ll probably need several daily injections that include a combination of a long-acting insulin and a rapid-acting insulin. These injections act more like the body’s normal use of insulin than do older insulin regimens that only required one or two shots a day. A combination of three or more insulin injections a day has been shown to improve blood sugar levels.
Insulin delivery options
Insulin can’t be taken by mouth to lower blood sugar because stomach enzymes will break down the insulin, preventing it from working. You’ll need to either get shots (injections) or use an insulin pump.
- Insulin injections. You can use a fine needle and syringe or an insulin pen to inject insulin under the skin. Insulin pens look like ink pens and are available in disposable or refillable varieties. If you choose shots (injections), you’ll probably need a mixture of insulin types to use during the day and night.
- An insulin pump. This is a small device worn on the outside of your body that you program to deliver specific amounts of insulin throughout the day and when you eat. A tube connects a reservoir of insulin to a catheter that’s inserted under the skin of your abdomen. There’s also a tubeless pump option that involves wearing a pod containing the insulin on your body combined with a tiny catheter that’s inserted under your skin.
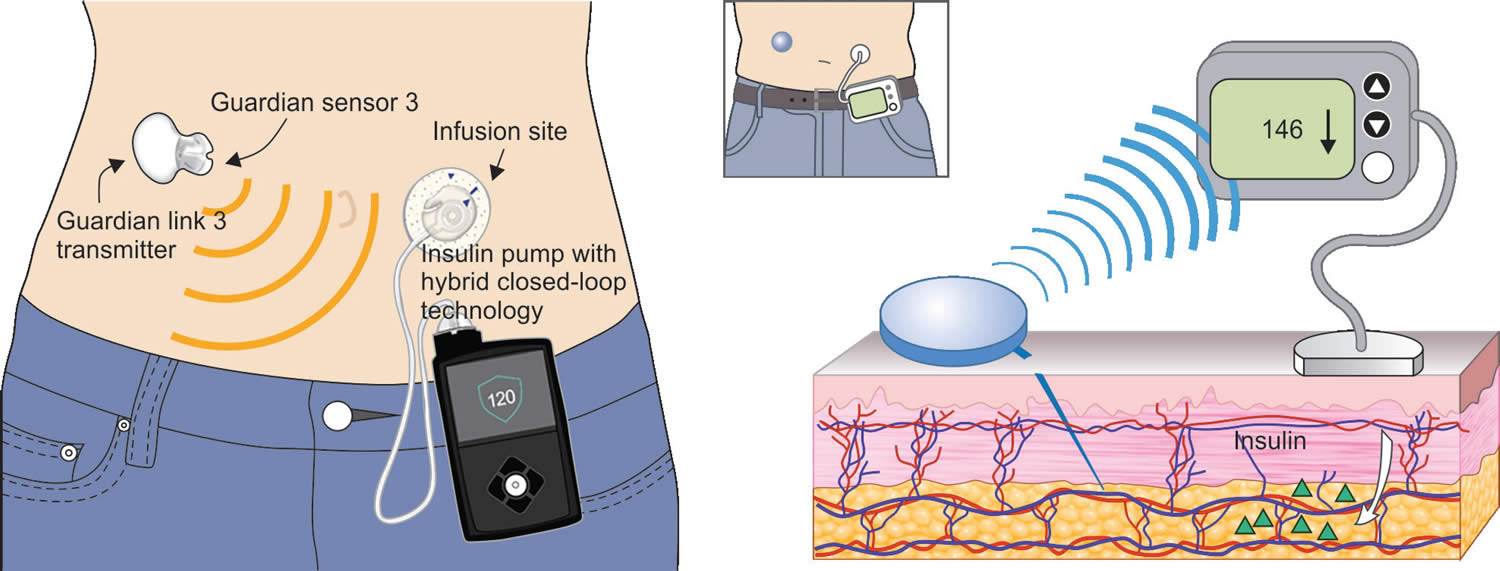
Artificial pancreas system
In 2016, the U.S. Food and Drug Administration (FDA) approved a type of “artificial pancreas” system called a hybrid closed-loop system or closed-loop insulin delivery system (the Medtronic MiniMed 670G hybrid closed-loop system) for use in people with type 1 diabetes who are age 14 and older 45. The “automated insulin delivery” system or an “autonomous system for glycemic control”, which is implanted in the body, links a continuous glucose monitor (CGM) to an insulin pump. The device tests your glucose level every 5 minutes throughout the day and night through a continuous glucose monitor (CGM), and automatically gives you the right amount of basal insulin, a long-acting insulin, through a separate insulin pump. The continuous glucose monitor sends information through a software program called a control algorithm. Based on your glucose level, the algorithm tells the insulin pump how much insulin to deliver. The software program could be installed on the pump or another device such as a cell phone or computer.
You still need to manually adjust the amount of insulin the pump delivers at mealtimes and when you need a correction dose. You also will need to test your blood with a glucose meter several times a day. Talk with your health care provider about whether the “artificial pancreas” system might be right for you.
Figure 4. Artificial pancreas system (closed-loop insulin delivery system)
Footnote: The glucose sensor contains a wire that is inserted under the skin on the abdomen and measures glucose values in the tissue fluid. The glucose values are wirelessly sent to the insulin pump, and displayed along with glucose trend information, alerts, and alarms on the pump screen. The insulin pump delivers a prescribed dosage of insulin through an infusion set. The insulin pump can automatically adjust the delivery of insulin using a mathematical equation, or algorithm that incorporates information from the continuous glucose monitor (CGM).
Type 1 diabetes future treatments
- Pancreas transplant. With a successful pancreas transplant, you would no longer need insulin. But pancreas transplants aren’t always successful — and the procedure poses serious risks. Because these risks can be more dangerous than the diabetes itself, pancreas transplants are generally used for those with very difficult-to-manage diabetes. They can also be used for people who also need a kidney transplant.
- Islet cell transplantation. Researchers are experimenting with islet cell transplantation. This provides new insulin-producing cells from a donor pancreas. This experimental procedure had some problems in the past. But new techniques and better drugs to prevent islet cell rejection may improve its chances of becoming a successful treatment.
Other medications
Other medications also may be prescribed for people with type 1 diabetes, such as:
- High blood pressure medications. Your provider may prescribe angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) to help keep your kidneys healthy. These medications are recommended for people with diabetes who have blood pressures above 140/90 millimeters of mercury (mm Hg).
- Aspirin. Your provider may recommend you take baby or regular aspirin daily to protect your heart. Your provider may feel that you have an increased risk of a cardiovascular event. Your provider will discuss the risk of bleeding if you take aspirin.
- Cholesterol-lowering drugs. Cholesterol guidelines are stricter for people with diabetes because of their higher risk of heart disease. The American Diabetes Association recommends that low-density lipoprotein (LDL, or “bad”) cholesterol be below 100 mg/dL (2.6 mmol/L). High-density lipoprotein (HDL, or “good”) cholesterol is recommended to be over 50 mg/dL (1.3 mmol/L) in women and over 40 mg/dL (1 mmol/L) in men. Triglycerides, another type of blood fat, should be less than 150 mg/dL (1.7 mmol/L).
Type 1 diabetes blood sugar monitoring
Depending on the type of insulin therapy you select or need, you may have to check and record your blood sugar level at least four times a day. The American Diabetes Association recommends testing blood sugar levels before meals and snacks, before bed, before exercising or driving, and whenever you think you have low blood sugar. Careful monitoring is the only way to make sure that your blood sugar level remains within your target range. More frequent monitoring can lower A1C levels.
Even if you take insulin and eat on a strict schedule, blood sugar levels can change. You’ll learn how your blood sugar level changes in response to food, activity, illness, medications, stress, hormonal changes and alcohol.
Continuous glucose monitoring
Continuous glucose monitoring (CGM) monitors blood sugar levels. It may be especially helpful for preventing low blood sugar. These devices have been shown to lower A1C.
Continuous glucose monitors attach to the body using a fine needle just under the skin. They check blood glucose levels every few minutes.
Time in range
Time in range is how long your blood sugar stays in your target range throughout the day. Most people with diabetes aim for 70% time in range, or between 16 and 17 hours out of 24.
Type 1 diabetes diet
There is no such thing as a ‘diabetic diet’ or a special diet exclusively for people with type 1 diabetes 46, 47. No two people with diabetes are the same. So there isn’t a one-size-fits-all way of eating for everyone with diabetes. In the past, people with type 1 diabetes were sent away after their diagnosis with a list of foods they weren’t allowed to eat, or often told to cut out sugar. But the best advice is to make healthier choices more often, and only have treats occasionally and in small portions. Because experts know that making healthier food choices is important to managing your diabetes and to reducing your risk of diabetes complications, like heart problems and strokes, and other health conditions including certain types of cancers.
Healthy eating centers around nutritious, low-fat, high-fiber foods such as:
- A regular schedule for meals and healthy snacks
- Smaller portion sizes
- More high-fiber foods, such as fruits, nonstarchy vegetables and whole grains
- Fewer refined grains, starchy vegetables and sweets
- Modest servings of low-fat dairy, low-fat meats and fish
- Healthy cooking oils, such as olive oil or canola oil
- Fewer calories
Your health care provider may recommend seeing a registered dietitian, who can help you:
- Identify healthy choices among your food preferences
- Plan well-balanced, nutritional meals
- Develop new habits and address barriers to changing habits
- Monitor carbohydrate intake to keep your blood sugar levels more stable
Try and make changes to your food choices that are realistic and achievable so you’ll stick with them. This will be different for everyone, depending on what you eat now and the goals you want to achieve.
Breakfast. Here are some healthy breakfast ideas to choose from:
- a bowl of wholegrain cereal with milk
- two slices of wholegrain toast with olive oil-based spread
- a pot of natural unsweetened yogurt and fruit
- two slices of avocado with a hardboiled egg.
Lunch. Here are some healthy lunch ideas to choose from:
- a chicken or tuna salad sandwich
- a small pasta salad
- soup with or without a wholegrain roll
- a piece of salmon or tuna steak and salad.
Think about having a piece of fruit or a pot of natural unsweetened yogurt afterwards too.
Dinner. Here are some healthy dinner ideas to choose from:
- lasagne and salad
- roast chicken and vegetables, with or without potatoes
- beef stir-fry and vegetables, with or without brown rice
- chicken tortillas and salad
- salmon and vegetables, with or without noodles
- curry with chickpeas and brown rice
Physical activity
Everyone needs regular aerobic exercise, including people who have type 1 diabetes. First, get your doctor’s OK to exercise. Then choose activities you enjoy, such as walking or swimming, and do them every day when you can. Try for at least 150 minutes of moderate aerobic exercise a week, with no more than two days without any exercise.
Remember that physical activity lowers blood sugar. If you begin a new activity, check your blood sugar level more often than usual until you know how that activity affects your blood sugar levels. You might need to adjust your meal plan or insulin doses because of the increased activity.
Activities of concern
Certain life activities may be of concern for people who have type 1 diabetes.
- Driving. Low blood sugar can occur at any time. It’s a good idea to check your blood sugar anytime you’re getting behind the wheel. If it’s below 70 mg/dL (3.9 mmol/L), have a snack with 15 grams of carbohydrates. Retest again in 15 minutes to make sure it has risen to a safe level before you start driving.
- Working. Type 1 diabetes can pose some challenges in the workplace. For example, if you work in a job that involves driving or operating heavy machinery, low blood sugar could pose a serious risk to you and those around you. You may need to work with your provider and your employer to ensure that certain adjustments are made. You may need additional breaks for blood sugar testing and fast access to food and drink. There are federal and state laws that require employers to provide these adjustments for people with diabetes.
- Being older or having other conditions. For those who are weak or sick or have difficulty thinking clearly, tight control of blood sugar may not be practical. It could also increase the risk of low blood sugar. For many people with type 1 diabetes, a less strict A1C goal of less than 8% may be appropriate.
Managing diabetes at school
Getting back into the routine of school takes a little more preparation for kids with diabetes, but it pays off over and over as the weeks and months go by. And since kids spend nearly half their waking hours in school, reliable diabetes care during the school day really matters. Some older students will be comfortable testing their blood sugar, injecting insulin, and adjusting levels if they use an insulin pump. Younger students and those who just found out they have diabetes will need help with everyday diabetes care. In a perfect world, all teachers and other school staff would understand how to manage diabetes so they could support your child as needed. But here in the real world, you’ll want to provide information to the school and work with staff to keep your son or daughter safe and healthy, no matter what the school day brings.
Diabetes Management Plan
No two kids handle their diabetes exactly the same way. Before the school year begins, meet with your child’s diabetes health care team to develop a personalized Diabetes Medical Management Plan. Then visit the school and review the Diabetes Medical Management Plan with the principal, office secretary, school nurse, nutrition service manager, teachers, and other staff who may have responsibility for your son or daughter during the day and after school.
The Diabetes Medical Management Plan explains everything about diabetes management and treatment, including:
- Target blood sugar range and whether your child needs help checking his or her blood sugar
- Your child’s specific low blood sugar (hypoglycemia) symptoms (see the list on this page) and how to treat low blood sugar
- Insulin or other medication used
- Meal and snack plans, including for special events
- How to manage physical activity/sports
The Diabetes Medical Management Plan works with your child’s daily needs and routine. Make sure to update it every year or more often if treatment changes.
To get a copy of the American Diabetes Association’s Diabetes Medical Management Plan please click here: https://diabetes.org/sites/default/files/2022-11/DMMP-updated-11-11-22.pdf
Type 1 diabetes follow up care
It takes a health care team to help you manage diabetes. And you’re the most important member of the team because you’re the one managing diabetes every day. You’ll regularly visit your doctor to talk about managing your diabetes. During these visits, the doctor will check your A1C levels. Your target A1C goal may vary depending on your age and various other factors. The American Diabetes Association generally recommends that A1C levels be below 7%, or an average glucose level of about 154 mg/dL (8.5 mmol/L).
A1C testing shows how well the diabetes treatment plan is working better than daily blood sugar tests. A high A1C level may mean you need to change the insulin amount, meal plan or both.
Once a year, you will need to have extra screening tests to look for early signs of other complications. These tests include:
- Dilated eye exam for diabetic retinopathy
- Fasting lipid profile for high cholesterol
- Urine test for albuminuria
- Thyroid function tests
- Celiac panel
Your doctor will also take blood and urine samples. They will use these samples to check cholesterol levels, as well as thyroid, liver and kidney function. Your doctor will also take your blood pressure and check the sites where you test your blood sugar and deliver insulin.
Living with type 1 diabetes
Careful management of type 1 diabetes can lower your risk of serious — even life-threatening — complications. Consider these tips:
- For Parents. If your child has type 1 diabetes—especially a young child—you’ll handle diabetes care on a day-to-day basis. Daily care will include serving healthy foods, giving insulin injections, and watching for and treating hypoglycemia (low blood sugar). You’ll also need to stay in close contact with your child’s health care team. They will help you understand the treatment plan and how to help your child stay healthy.
- Make a commitment to manage your diabetes. Take your medications as recommended. Learn all you can about type 1 diabetes. Make healthy eating and physical activity part of your daily routine. Establish a relationship with a diabetes educator. Ask your health care team for help.
- Wear a tag or bracelet that says you are living with type 1 diabetes. Keep a glucagon kit nearby in case of a low blood sugar emergency. Make sure your friends and loved ones know how to use the kit.
- Schedule a yearly physical exam and regular eye exams. Your regular diabetes checkups aren’t meant to replace yearly physicals or routine eye exams. During the physical, your doctor will look for any diabetes-related complications. Your doctor will also look for other medical problems. Your eye care specialist will check for signs of eye complications, such as retina damage, cataracts and glaucoma.
- Keep your vaccinations up to date. High blood sugar can weaken the immune system. The Centers for Disease Control and Prevention (CDC) recommends hepatitis B vaccination if you haven’t had it before and you’re an adult between the ages of 19 and 59 years with type 1 or type 2 diabetes. The CDC recommends vaccination as soon as possible after diagnosis with type 1 or type 2 diabetes. If you are age 60 or older and have diabetes and haven’t received the vaccine, talk to your doctor about whether it’s right for you.
- Pay attention to your feet. Wash your feet daily in lukewarm water. Dry them gently, especially between the toes. Moisturize your feet with lotion. Check your feet every day for blisters, cuts, sores, redness or swelling. Consult your provider if you have a sore or other foot problem that doesn’t heal.
- Keep your blood pressure and cholesterol under control. Eating healthy foods and exercising regularly can help control high blood pressure and cholesterol. Medication also may be needed.
- Quit smoking. If you smoke or use other forms of tobacco, ask your doctor to help you quit. Smoking increases your risk of diabetes complications. These include heart attack, stroke, nerve damage and kidney disease. Talk to your provider about ways to stop smoking or to stop using other types of tobacco.
- If you drink alcohol, do so responsibly. Alcohol can cause either high or low blood sugar. It depends on how much you drink and if you eat at the same time. If you choose to drink, do so only in moderation and always with a meal. Check your blood sugar levels before going to sleep.
- Manage stress. The hormones the body produces when you’re under long-term stress may prevent insulin from working properly. This can stress and frustrate you even more. Take a step back and set some limits. Prioritize your tasks. Learn ways to relax. Get plenty of sleep.
Type 1 diabetes prognosis
The prognosis of type 1 diabetes gets significantly influenced by the degree of glucose management. Chronic hyperglycemia significantly increases the risk of type 1 diabetes complications. Study after study has shown that reasonable blood sugar control favorably affected the onset and progression of diabetic complications. The Diabetes Control and Complications Trial and the United Kingdom Prospective Diabetes Study found that individuals with type 1 diabetes and type 2 diabetes respectively had increased microvascular complications with chronic hyperglycemia 48, 49. Uncontrolled blood pressure is an added risk factor for macular edema. Lowering the blood pressure in patients with diabetes thus also affects the risk of progression of the retinopathy. Injection of antibodies vascular endothelial growth factor (anti-VEGF) agents are generally in use as the initial therapy in cases of macular edema. In cases of nonproliferative diabetic retinopathy, pan-retinal photocoagulation is being used. In cases of diabetic proliferative retinopathy, combined modalities of anti-VEGF agents and pan-retinal photocoagulation are now in use. Sudden loss of vision can occur for several reasons in patients with diabetes mellitus, the most common being vitreous hemorrhage. Less common causes that merit consideration include vascular occlusion (central retinal vein or branch vein occlusion involving the macula), retinal detachment, end-stage glaucoma, and ischemic optic neuropathy.
Patients who can revert to normal glucose during the progression from pre-diabetes to frank diabetes had a good prognosis and may be able to slow disease progression 50.
- Chobot A., Polanska J., Deja G., Jarosz-Chobot P. Incidence of type 1 diabetes among Polish children ages 0–14 years from 1989–2012. Acta Diabetol. 2015;52:483–488. doi: 10.1007/s00592-014-0682-z[↩]
- Patterson C.C., Dahlquist G.G., Gyürüs E., Green A., Soltész G. Incidence trends for childhood type 1 diabetes in Europe during 1989–2003 and predicted new cases 2005–20: A multicentre prospective registration study. Lancet. 2009;373:2027–2033. doi: 10.1016/S0140-6736(09)60568-7[↩]
- Tanaka S, Ohmori M, Awata T, et al. Diagnostic criteria for slowly progressive insulin‐dependent (type 1) diabetes mellitus (SPIDDM) (2012): report by the Committee on Slowly Progressive Insulin‐Dependent (Type 1) Diabetes Mellitus of the Japan Diabetes Society. Diabetol Int 2015; 6: 1–7.[↩][↩]
- Kawasaki E, Maruyama T, Imagawa A, Awata T, Ikegami H, Uchigata Y, Osawa H, Kawabata Y, Kobayashi T, Shimada A, Shimizu I, Takahashi K, Nagata M, Makino H, Hanafusa T. Diagnostic criteria for acute-onset type 1 diabetes mellitus (2012): Report of the Committee of Japan Diabetes Society on the Research of Fulminant and Acute-onset Type 1 Diabetes Mellitus. J Diabetes Investig. 2014 Feb 12;5(1):115-8. doi: 10.1111/jdi.12119[↩][↩]
- Imagawa A, Hanafusa T, Awata T, Ikegami H, Uchigata Y, Osawa H, Kawasaki E, Kawabata Y, Kobayashi T, Shimada A, Shimizu I, Takahashi K, Nagata M, Makino H, Maruyama T. Report of the Committee of the Japan Diabetes Society on the Research of Fulminant and Acute-onset Type 1 Diabetes Mellitus: New diagnostic criteria of fulminant type 1 diabetes mellitus (2012). J Diabetes Investig. 2012 Dec 20;3(6):536-9. doi: 10.1111/jdi.12024[↩][↩]
- Zorena K, Michalska M, Kurpas M, Jaskulak M, Murawska A, Rostami S. Environmental Factors and the Risk of Developing Type 1 Diabetes-Old Disease and New Data. Biology (Basel). 2022 Apr 16;11(4):608. doi: 10.3390/biology11040608[↩][↩][↩][↩]
- Misso ML, Egberts KJ, Page M, O’Connor D, Shaw J. Continuous subcutaneous insulin infusion (CSII) versus multiple insulin injections for type 1 diabetes mellitus. Cochrane Database Syst Rev. 2010 Jan 20;(1):CD005103. doi: 10.1002/14651858.CD005103.pub2[↩][↩]
- Evans K. Insulin pumps in hospital: a guide for the generalist physician. Clin Med (Lond). 2013 Jun;13(3):244-7. doi: 10.7861/clinmedicine.13-3-244[↩][↩][↩]
- National Institute for Health and Clinical Excellence. Technology Appraisal Guidance 151 (review of Technology Appraisal Guidance 57) London: NICE; 2008. Continuous subcutaneous insulin infusion for the treatment of diabetes mellitus.[↩][↩]
- Pickup JC, Sutton AJ. Severe hypoglycaemia and glycaemic control in type 1 diabetes: meta-analysis of multiple daily insulin injections versus continuous subcutaneous insulin infusion. Diabet Med. 2008;25:765–74. doi: 10.1111/j.1464-5491.2008.02486.x[↩]
- Diabetes remission. https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/treating-your-diabetes/type2-diabetes-remission[↩]
- Hugerth L.W., Larsson J., Alneberg J., Lindh M.V., Legrand C., Pinhassi J., Andersson A.F. Metagenome-assembled genomes uncover a global brackish microbiome. Genome Biol. 2015;16:279. doi: 10.1186/s13059-015-0834-7[↩]
- Mogensen T.H., Paludan S.R. Molecular pathways in virus-induced cytokine production. Microbiol. Mol. Biol. Rev. 2001;65:131–150. doi: 10.1128/MMBR.65.1.131-150.2001[↩]
- Cheon C.K. Understanding of type 1 diabetes mellitus: What we know and where we go. Korean J. Pediatr. 2018;61:307–314. doi: 10.3345/kjp.2018.06870[↩]
- Myśliwiec M., Balcerska A., Zorena K., Jędrzejczyk A., Malinowska E., Myśliwska J. Increasing incidence of diabetes mellitus type 1 in children: The role of environmental factors. Pol. J. Environ. Stud. 2007 16:109–112.[↩]
- Ibrahim Saber A.-Z.A.-B., Mohammed A.H. The role of Human Cytomegalovirus and Epstein-Barr virus in type 1 Diabetes Mellitus. Ann. Trop Public Health. 2019;22:S267. doi: 10.36295/ASRO.2019.220912[↩]
- Murdaca G., Greco M., Borro M., Gangemi S. Hygiene hypothesis and autoimmune diseases: A narrative review of clinical evidences and mechanisms. Autoimmun. Rev. 2021;20:102845. doi: 10.1016/j.autrev.2021.102845[↩]
- Altobelli E., Petrocelli R., Verrotti A., Chiarelli F., Marziliano C. Genetic and environmental factors affect the onset of type 1 diabetes mellitus. Pediatr. Diabetes. 2016;17:559–566. doi: 10.1111/pedi.12345[↩]
- Pang H., Luo S., Huang G., Xia Y., Xie Z., Zhou Z. Advances in Knowledge of Candidate Genes Acting at the Beta-Cell Level in the Pathogenesis of T1DM. Front. Endocrinol. 2020;11:119. doi: 10.3389/fendo.2020.00119[↩]
- Strollo R., Vinci C., Napoli N., Pozzilli P., Ludvigsson J., Nissim A. Antibodies to post-translationally modified insulin as a novel biomarker for prediction of type 1 diabetes in children. Diabetologia. 2017;60:1467–1474. doi: 10.1007/s00125-017-4296-1[↩][↩]
- Rewers M., Ludvigsson J. Environmental risk factors for type 1 diabetes. Lancet. 2016;387:2340–2348. doi: 10.1016/S0140-6736(16)30507-4[↩][↩]
- Cieślak M., Cieślak M. Role of purinergic signalling and proinflammatory cytokines in diabetes. Clin. Diabetol. 2017;6:90–100. doi: 10.5603/DK.2017.0015[↩][↩]
- Michalska M., Zorena K., Wąż P., Bartoszewicz M., Brandt-Varma A., Ślęzak D., Robakowska M. Gaseous Pollutants and Particulate Matter (PM) in Ambient Air and the Number of New Cases of Type 1 Diabetes in Children and Adolescents in the Pomeranian Voivodeship, Poland. Biomed. Res. Int. 2020;2020:1648264. doi: 10.1155/2020/1648264[↩]
- Bedi S., Richardson T.M., Jia B., Saab H., Brinkman F.S.L., Westley M. Similarities between bacterial GAD and human GAD65: Implications in gut mediated autoimmune type 1 diabetes. PLoS ONE. 2022;17:e0261103. doi: 10.1371/journal.pone.0261103[↩][↩]
- Principi N., Berioli M.G., Bianchini S., Esposito S. Type 1 diabetes and viral infections: What is the relationship? J. Clin. Virol. Off. Publ. Pan Am. Soc. Clin. Virol. 2017;96:26–31. doi: 10.1016/j.jcv.2017.09.003[↩]
- Singh S., Sonkar S.K., Sonkar G.K., Mahdi A.A. Diabetic kidney disease: A systematic review on the role of epigenetics as diagnostic and prognostic marker. Diabetes. Metab. Res. Rev. 2019;35:e3155. doi: 10.1002/dmrr.3155[↩]
- Hyttinen V., Kaprio J., Kinnunen L., Koskenvuo M., Tuomilehto J. Genetic liability of type 1 diabetes and the onset age among 22,650 young Finnish twin pairs: A nationwide follow-up study. Diabetes. 2003;52:1052–1055. doi: 10.2337/diabetes.52.4.1052[↩]
- Paschou S., Papadopoulou-Marketou N., Chrousos G., Kanaka-Gantenbein C. On type 1 diabetes mellitus pathogenesis. Endocr. Connect. 2018;7:R38–R46. doi: 10.1530/EC-17-0347[↩]
- Siewko K., Popławska-Kita A., Telejko B., Maciulewski R., Zielińska A., Nikołajuk A., Górska M., Szelachowska M. Prognostic markers for the development of type 1 diabetes in first-degree relatives of diabetic patients. Endokrynol. Pol. 2014;65:176–180. doi: 10.5603/EP.2014.0024[↩][↩]
- Nerup J., Platz P., Andersen O.O., Christy M., Lyngsoe J., Poulsen J.E., Ryder L.P., Nielsen L.S., Thomsen M., Svejgaard A. HL-A antigens and diabetes mellitus. Lancet. 1974;2:864–866. doi: 10.1016/S0140-6736(74)91201-X[↩]
- Farina F., Picascia S., Pisapia L., Barba P., Vitale S., Franzese A., Mozzillo E., Gianfrani C., Del Pozzo G.G. HLA-DQA1 and HLA-DQB1 Alleles, Conferring Susceptibility to Celiac Disease and Type 1 Diabetes, Are More Expressed Than Non-Predisposing Alleles and Are Coordinately Regulated. Cells. 2019;8:751. doi: 10.3390/cells8070751[↩]
- Santos D.C., Porto L.C., Oliveira R.V., Secco D., Hanhoerderster L., Pizarro M.H., Barros B.S.V., Mello L.G.N., Muniz L.H., Silva D.A., et al. HLA class II genotyping of admixed Brazilian patients with type 1 diabetes according to self-reported color/race in a nationwide study. Sci. Rep. 2020;10:6628. doi: 10.1038/s41598-020-63322-y[↩][↩]
- Ikegami H., Noso S., Babaya N., Kawabata Y. Genetics and pathogenesis of type 1 diabetes: Prospects for prevention and intervention. J. Diabetes Investig. 2011;2:415–420. doi: 10.1111/j.2040-1124.2011.00176.x[↩]
- Pugliese A. Genetics of type 1 diabetes. Endocrinol. Metab. Clin. N. Am. 2004;33:1–16. doi: 10.1016/S0889-8529(03)00082-3[↩][↩]
- Antosik K., Gnyś P., Jarosz-Chobot P., Myśliwiec M., Szadkowska A., Małecki M., Młynarski W., Borowiec M. An analysis of the sequence of the BAD gene among patients with maturity-onset diabetes of the young (MODY) J. Pediatr. Endocrinol. Metab. 2017;30:97–100. doi: 10.1515/jpem-2016-0239[↩]
- Yalcıntepe S., Ozguc Comlek F., Gurkan H., Demir S., Atlı E.I., Atlı E., Eker D., Tutunculer Kokenli F. The Application of Next Generation Sequencing Maturity Onset Diabetes of the Young Gene Panel in Turkish Patients from Trakya Region. J. Clin. Res. Pediatr. Endocrinol. 2021;13:320–331. doi: 10.4274/jcrpe.galenos.2021.2020.0285[↩]
- Ivanoshchuk D.E., Shakhtshneider E.V., Rymar O.D., Ovsyannikova A.K., Mikhailova S.V., Fishman V.S., Valeev E.S., Orlov P.S., Voevoda M.I. The Mutation Spectrum of Maturity Onset Diabetes of the Young (MODY)-Associated Genes among Western Siberia Patients. J. Pers. Med. 2021;11:57. doi: 10.3390/jpm11010057[↩]
- Di Ciaula A., Portincasa P. Relationships between emissions of toxic airborne molecules and type 1 diabetes incidence in children: An ecologic study. World J. Diabetes. 2021;12:673–684. doi: 10.4239/wjd.v12.i5.673[↩][↩]
- Ilonen J., Lempainen J., Veijola R. The heterogeneous pathogenesis of type 1 diabetes mellitus. Nat. Rev. Endocrinol. 2019;15:635–650. doi: 10.1038/s41574-019-0254-y[↩]
- Michalska M., Bartoszewicz M., Wąż P., Korzeniowska K., Myśliwiec M., Zorena K. The relation between concentration of particulate matter PM10 and the number of new cases of type 1 diabetes mellitus in children and adolescents in the Pomeranian Voivodeship. Med. Srod. 2018;21:25–27. doi: 10.19243/2018303[↩]
- Kowalewska B., Zorena K., Szmigiero-Kawko M., Wąż P., Myśliwiec M. High Interleukin-12 Levels May Prevent an Increase in the Amount of Fungi in the Gastrointestinal Tract during the First Years of Diabetes Mellitus Type 1. Dis. Markers. 2016;2016:4685976. doi: 10.1155/2016/4685976[↩]
- Nanayakkara N, Curtis AJ, Heritier S, Gadowski AM, Pavkov ME, Kenealy T, Owens DR, Thomas RL, Song S, Wong J, Chan JC, Luk AO, Penno G, Ji L, Mohan V, Amutha A, Romero-Aroca P, Gasevic D, Magliano DJ, Teede HJ, Chalmers J, Zoungas S. Impact of age at type 2 diabetes mellitus diagnosis on mortality and vascular complications: systematic review and meta-analyses. Diabetologia. 2021 Feb;64(2):275-287. doi: 10.1007/s00125-020-05319-w[↩]
- Forbes JM, Cooper ME. Mechanisms of diabetic complications. Physiol Rev. 2013 Jan;93(1):137-88. doi: 10.1152/physrev.00045.2011[↩][↩][↩]
- Understanding A1C. https://diabetes.org/diabetes/a1c/diagnosis[↩]
- The Artificial Pancreas Device System. https://www.fda.gov/medical-devices/consumer-products/artificial-pancreas-device-system[↩]
- Evert AB, Dennison M, Gardner CD, Garvey WT, Lau KHK, MacLeod J, Mitri J, Pereira RF, Rawlings K, Robinson S, Saslow L, Uelmen S, Urbanski PB, Yancy WS Jr. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Diabetes Care. 2019 May;42(5):731-754. doi: 10.2337/dci19-0014[↩]
- Food for Thought. Key Takeaways from ADA’s Nutrition Consensus Report. https://diabetes.org/sites/default/files/2019-10/ADV_2019_Consumer_Nutrition_One%20Pager.pdf[↩]
- Albers JW, Herman WH, Pop-Busui R, Feldman EL, Martin CL, Cleary PA, Waberski BH, Lachin JM; Diabetes Control and Complications Trial /Epidemiology of Diabetes Interventions and Complications Research Group. Effect of prior intensive insulin treatment during the Diabetes Control and Complications Trial (DCCT) on peripheral neuropathy in type 1 diabetes during the Epidemiology of Diabetes Interventions and Complications (EDIC) Study. Diabetes Care. 2010 May;33(5):1090-6. doi: 10.2337/dc09-1941[↩]
- Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998 Sep 12;352(9131):837-53. Erratum in: Lancet 1999 Aug 14;354(9178):602.[↩]
- Perreault L, Pan Q, Mather KJ, Watson KE, Hamman RF, Kahn SE; Diabetes Prevention Program Research Group. Effect of regression from prediabetes to normal glucose regulation on long-term reduction in diabetes risk: results from the Diabetes Prevention Program Outcomes Study. Lancet. 2012 Jun 16;379(9833):2243-51. doi: 10.1016/S0140-6736(12)60525-X[↩]